3D Bioprinting Revolution: How Nanoparticle Bioinks Are Advancing Tissue Engineering and Drug Development
This article provides a comprehensive overview of 3D bioprinting utilizing nanoparticle-laden bioinks, tailored for researchers and drug development professionals.
3D Bioprinting Revolution: How Nanoparticle Bioinks Are Advancing Tissue Engineering and Drug Development
Abstract
This article provides a comprehensive overview of 3D bioprinting utilizing nanoparticle-laden bioinks, tailored for researchers and drug development professionals. It explores the foundational principles of nanoparticle-enhanced hydrogels, detailing the methodological integration of metallic, polymeric, and ceramic nanoparticles for improved printability, mechanical strength, and bioactivity. The content addresses key challenges in rheology, cell viability, and sterilization, while offering optimization strategies for ink formulation and printing parameters. A critical evaluation covers the validation techniques, comparative performance against traditional bioinks, and the translational potential of these advanced constructs in creating physiologically relevant tissue models, drug screening platforms, and regenerative implants.
Nanoparticle Bioinks Explained: Core Concepts, Components, and Rationale for 3D Bioprinting
Nanoparticle bioinks represent an advanced class of materials for 3D bioprinting, engineered by incorporating functional nanoparticles (NPs) into traditional hydrogel-based bioinks. These composites are designed to enhance the physicochemical, biological, and mechanical properties of the printed constructs, thereby addressing critical challenges in tissue engineering and regenerative medicine. Within the broader thesis of 3D bioprinting research, nanoparticle bioinks are pivotal for creating biomimetic, bioactive, and structurally stable living tissues for applications in disease modeling, drug screening, and organ regeneration.
Composition and Key Functions
Nanoparticle bioinks typically consist of a hydrogel matrix (e.g., alginate, gelatin methacryloyl (GelMA), hyaluronic acid) infused with nanoparticles such as ceramic NPs (e.g., hydroxyapatite), polymeric NPs, metallic NPs (e.g., gold, silver), carbon-based NPs (e.g., graphene oxide), or drug-loaded liposomes. The nanoparticles confer multifunctionality.
Table 1: Primary Nanoparticle Types, Properties, and Functions in Bioinks
| Nanoparticle Type | Example Materials | Key Properties Imparted | Primary Function in Bioprinted Construct |
|---|---|---|---|
| Ceramic | Hydroxyapatite, Bioglass | Enhanced osteoconductivity, mechanical stiffness | Bone and cartilage tissue engineering |
| Metallic | Gold NPs, Silver NPs | Electrical conductivity, antimicrobial activity | Neural/ cardiac tissue interfaces, infection control |
| Polymeric | PLGA, Chitosan NPs | Controlled drug/protein delivery, improved shear-thinning | Sustained growth factor release, printability |
| Carbon-Based | Graphene Oxide, CNTs | High electrical conductivity, tensile strength | Electrically active tissues (muscle, nerve) |
| Lipid-Based | Liposomes, Extracellular Vesicles | High biocompatibility, efficient cell signaling molecule delivery | Enhanced cell-cell communication, wound healing |
Application Notes: Enhancing Bioink Performance
Note 1: Mechanical Reinforcement
Hydrogels alone often lack the mechanical integrity for printing load-bearing tissues. The incorporation of rigid nanoparticles like hydroxyapatite or cellulose nanocrystals creates nanocomposite networks. Recent studies show that adding 2% (w/v) cellulose nanocrystals to alginate bioinks increased compressive modulus by approximately 300%, from ~15 kPa to ~60 kPa.
Table 2: Quantitative Impact of Nanoparticles on Bioink Properties
| Bioink Formulation | Nanoparticle Load (wt%) | Key Outcome Measurement | Result (Mean ± SD) | Reference Year |
|---|---|---|---|---|
| GelMA + Graphene Oxide | 0.1% | Electrical Conductivity (S/m) | 0.18 ± 0.02 | 2023 |
| Alginate + HAp | 1.5% | Compressive Modulus (kPa) | 85 ± 7 | 2024 |
| Hyaluronic Acid + PLGA NPs | 3.0% | Sustained VEGF Release Duration (days) | 28 | 2023 |
| Collagen + Gold NPs | 0.05% | Printability Fidelity Score (%) | 94 ± 3 | 2024 |
Note 2: Biofunctionalization and Stimuli-Responsiveness
Nanoparticles can be surface-functionalized with peptides (e.g., RGD) to improve cell adhesion. Furthermore, magnetic nanoparticles (e.g., Fe₃O₄) enable non-contact manipulation of printed constructs or remote stimulation of cells. A 2023 protocol demonstrated that MNPs aligned endothelial cells in printed vessels under a magnetic field, increasing angiogenesis marker expression (CD31) by 2.5-fold.
Note 3: Controlled Therapeutic Delivery
Nanoparticles act as reservoirs for growth factors, antibiotics, or siRNA, protecting them from degradation and enabling localized, sustained release. This is crucial for creating instructive microenvironments. For instance, bioinks containing vascular endothelial growth factor (VEGF)-loaded mesoporous silica nanoparticles showed a sustained, linear release profile over 21 days, significantly enhancing vascular network formation in printed dermal grafts.
Experimental Protocols
Protocol 1: Synthesis and Characterization of a Nanocomposite Bioink for Bone Tissue Engineering
Title: Preparation and Rheological Assessment of GelMA-Hydroxyapatite Nanocomposite Bioink. Objective: To synthesize a osteogenic bioink by incorporating hydroxyapatite nanoparticles (nHAp) into GelMA hydrogel and characterize its printability and mechanical properties. Materials:
- GelMA polymer
- Photoinitiator (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, LAP)
- Hydroxyapatite nanoparticles (<200 nm)
- Phosphate Buffered Saline (PBS)
- UV light source (365 nm, 5-10 mW/cm²)
- Rheometer
- Extrusion bioprinter
Methodology:
- GelMA Solution Preparation: Dissolve GelMA in PBS at 10% (w/v) concentration at 37°C. Add LAP photoinitiator at 0.25% (w/v).
- Nanoparticle Incorporation: Gradually add nHAp powder to the GelMA solution to achieve a final concentration of 2% (w/v). Use probe sonication (5 cycles of 30s ON, 30s OFF, 40% amplitude) to ensure homogeneous dispersion. Avoid bubble formation.
- Rheological Characterization:
- Shear-thinning: Perform a steady-state flow sweep test from 0.1 to 100 s⁻¹ shear rate. The viscosity should decrease with increasing shear rate.
- Recovery Test: Apply high shear (100 s⁻¹ for 30s), then switch to low shear (0.1 s⁻¹ for 60s) to measure structural recovery (G' and G'' moduli).
- Printability Assessment: Load bioink into a sterile syringe. Print a 15x15 mm grid structure (22G nozzle, 150 kPa pressure, 8 mm/s speed). Assess filament uniformity, fusion, and strand diameter consistency.
- Crosslinking & Mechanical Testing: Expose printed structures to UV light (365 nm, 10 mW/cm², 60s). Perform unconfined compression tests on cylindrical samples (n=5) to determine compressive modulus.
Protocol 2: Bioprinting a Vascularized Construct with Drug-Releasing Nanoparticles
Title: Bioprinting a Vasculogenic Construct Using Bioinks Containing VEGF-Loaded Nanoparticles. Objective: To fabricate a cell-laden, prevascularized construct using a bioink containing VEGF-releasing PLGA nanoparticles. Materials:
- Human Umbilical Vein Endothelial Cells (HUVECs)
- Normal Human Dermal Fibroblasts (NHDFs)
- Fibrinogen, Thrombin, Aprotinin
- VEGF-loaded PLGA nanoparticles (VEGF-NPs)
- Multi-material extrusion bioprinter
Methodology:
- Bioink Preparation:
- Bioink A (Vascular Channels): Mix HUVECs (5x10⁶ cells/mL) with fibrinogen (10 mg/mL) and VEGF-NPs (1 mg/mL) in cell culture medium.
- Bioink B (Stromal Matrix): Mix NHDFs (3x10⁶ cells/mL) with fibrinogen (15 mg/mL).
- Prepare a crosslinking solution of thrombin (2 U/mL) and aprotinin (150 KIU/mL).
- Coaxial Bioprinting Setup: Load Bioink A into the core syringe and the thrombin/aprotinin solution into the sheath syringe of a coaxial printhead.
- Printing Process: Co-print a branching vascular tree structure into a pre-printed layer of Bioink B. The simultaneous extrusion crosslinks the fibrinogen in Bioink A upon contact with thrombin.
- Post-Print Culture: Transfer constructs to an incubator (37°C, 5% CO₂) for 15 minutes for complete gelation. Add endothelial growth medium.
- Analysis: At days 3, 7, and 14, fix samples and immunostain for CD31 to visualize endothelial network formation. Quantify total tube length and branch points per field of view.
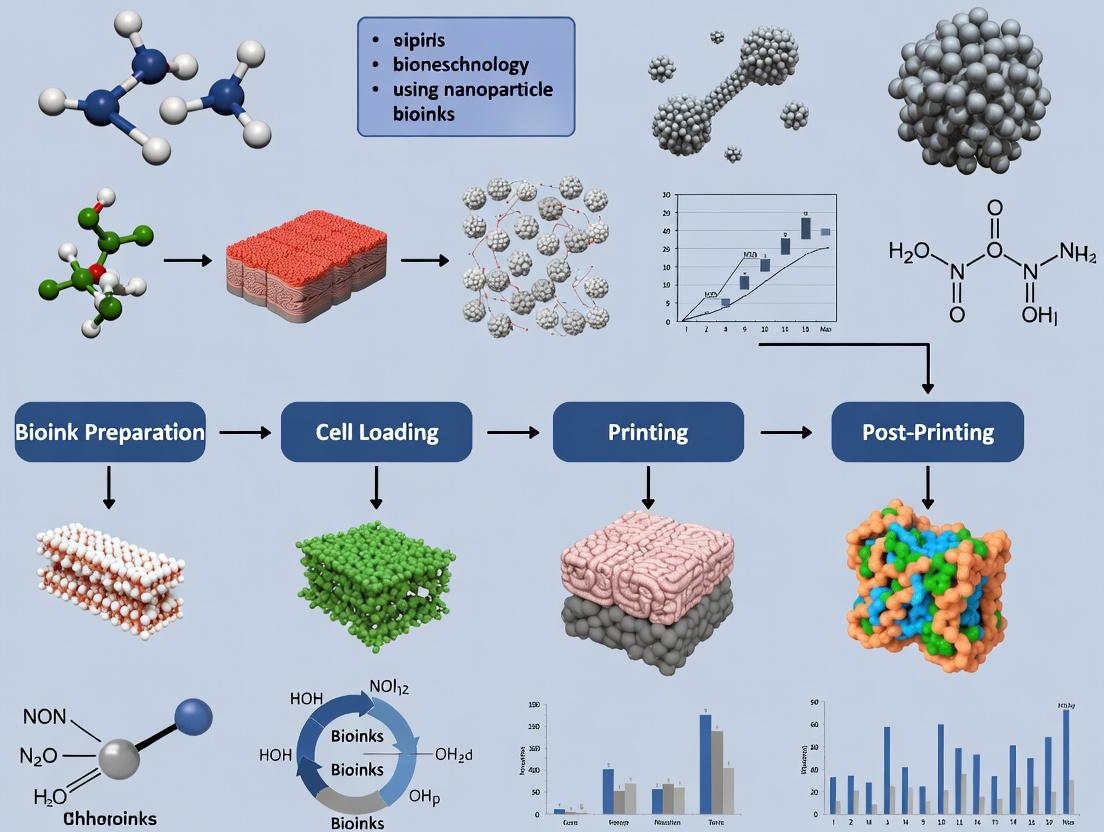
Visualization of Key Concepts
Title: Nanoparticle Bioink Engineering Workflow
Title: Nanoparticle-Induced Angiogenic Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Bioink Research
| Item | Function in Research | Example Vendor/Product Note |
|---|---|---|
| Methacrylated Hydrogels (GelMA, Hyaluronic Acid-MA) | Provides photo-crosslinkable, tunable base matrix with inherent biocompatibility. | Advanced BioMatrix, GelMA Kit; EngiMaTrix, HAMA. |
| Functional Nanoparticles (HAp, GO, PLGA NPs) | Core additive for imparting mechanical, electrical, or drug-delivery properties. | Sigma-Aldrich (nHAp), Graphenea (GO), PolySciTech (PLGA NPs). |
| Photoinitiators (LAP, Irgacure 2959) | Enables rapid UV-mediated crosslinking of bioinks for shape fidelity. | Tokyo Chemical Industry (LAP); CIBA (Irgacure 2959). |
| Rheometer with Temperature Control | Critical for characterizing shear-thinning, recovery, and gelation kinetics of bioinks. | TA Instruments DHR series, Malvern Kinexus. |
| Sterile, Temperature-Controlled Bioprinter | For precise deposition of cell-laden nanocomposite bioinks. | Allevi 3, CELLINK BIO X, Regemat 3D. |
| Cell-Compatible Crosslinkers (CaCl₂, Thrombin) | For ionic (alginate) or enzymatic (fibrin) crosslinking post-printing. | Thermo Fisher Scientific. |
| Live/Dead Viability Assay Kit | Standard for assessing post-printing cell viability in 3D constructs. | Thermo Fisher Scientific (Calcein AM / Ethidium homodimer-1). |
Application Notes
Nanoparticles (NPs) are engineered into bioinks to transcend their traditional role as passive scaffold reinforcements. They impart bioactive, electrical, and diagnostic functionalities, enabling the creation of sophisticated, biomimetic, and intelligent tissue constructs.
1. Mechanical Reinforcement & Printability Nanoparticles like cellulose nanocrystals (CNCs), silica nanoparticles (SiNPs), and graphene oxide (GO) enhance the rheological properties of bioinks. They improve viscosity, yield stress, and shear-thinning behavior, enabling the printing of high-fidelity, self-supporting structures. This is critical for fabricating complex architectures with high shape fidelity.
2. Bioactivation & Signaling Nanoparticles functionalized with growth factors, peptides, or drugs provide sustained, localized biochemical cues. For example, hydroxyapatite nanoparticles (nHA) in bone bioinks adsorb bone morphogenetic protein-2 (BMP-2), promoting osteogenic differentiation. Lipid nanoparticles (LNPs) can deliver mRNA or siRNA to direct stem cell fate within the printed construct.
3. Electrically Conductive Networks NPs such as gold nanorods (AuNRs), graphene, and carbon nanotubes (CNTs) create percolating networks within insulating hydrogels (e.g., GelMA, alginate). This enables the fabrication of cardiac patches or neural tissues that can conduct electrical signals, synchronizing cell contraction and promoting maturation.
4. Real-Time Monitoring & Theranostics Fluorescent, magnetic, or plasmonic nanoparticles (e.g., quantum dots, superparamagnetic iron oxide nanoparticles - SPIONs) can be embedded as biosensors. They allow non-invasive monitoring of tissue maturation, oxygen tension, or specific biomarkers post-printing, merging fabrication with diagnostic capability.
5. Crosslinking & Structural Integrity Photocatalytic nanoparticles like titanium dioxide (TiO₂) or gold nanoparticles (AuNPs) can initiate or enhance crosslinking upon exposure to specific light wavelengths (e.g., visible light vs. UV), leading to deeper, more uniform hydrogel curing and improved cell viability.
Quantitative Data Summary
Table 1: Mechanical Enhancement by Nanoparticles in Alginate/GelMA Bioinks
| Nanoparticle Type | Concentration (w/v %) | Storage Modulus Increase (%) | Compression Modulus (kPa) | Reference Bioink |
|---|---|---|---|---|
| Cellulose Nanocrystals (CNC) | 1.5% | ~220% | 45 ± 3 | 3% Alginate |
| Graphene Oxide (GO) | 0.2% | ~180% | 68 ± 5 | 5% GelMA |
| Silica Nanoparticles (SiNP) | 2.0% | ~150% | 52 ± 4 | 4% Alginate/GelMA Blend |
| n-Hydroxyapatite (nHA) | 2.5% | ~120% | 95 ± 8 | 7% GelMA for Bone |
Table 2: Functional Outcomes in Bioprinted Constructs with NPs
| NP Function | NP Type & Model | Key Outcome Metric | Result vs. Control |
|---|---|---|---|
| Osteogenic Induction | BMP-2 loaded nHA / hMSCs | Alkaline Phosphatase Activity (Day 14) | 3.2-fold increase |
| Cardiac Conduction | AuNRs in GelMA / Cardiomyocytes | Conduction Velocity (cm/s) | 18.5 ± 1.2 vs. 9.8 ± 0.9 |
| Neural Guidance | GO-PEDOT in Hyaluronic Acid / Neural Progenitors | Neurite Length (µm, Day 7) | 350 ± 25 vs. 210 ± 30 |
| Angiogenic Induction | VEGF-loaded PLGA NPs in Bioink / HUVECs | Tubule Formation (Total Length mm/mm²) | 22.5 ± 2.1 vs. 11.3 ± 1.5 |
Experimental Protocols
Protocol 1: Formulation and Characterization of a Mechanically Reinforced CNF/GelMA/GO Bioink for Neural Tissue
Aim: To formulate a bioink with enhanced shear-thinning and electrical conductivity for neural tissue models.
Materials:
- GelMA (Methacryloyl gelatin)
- Photoinitiator (LAP, Lithium phenyl-2,4,6-trimethylbenzoylphosphinate)
- Graphene Oxide (GO) dispersion (2 mg/mL in water)
- Cellulose Nanofibrils (CNF) suspension (1% w/w)
- Phosphate Buffered Saline (PBS)
- Primary Rat Neural Stem Cells (NSCs)
Procedure:
- Bioink Preparation: a. Dissolve GelMA to 7% (w/v) in PBS containing 0.25% (w/v) LAP at 37°C. b. Homogenize CNF suspension (final 0.5% w/v) into the GelMA solution using a dual asymmetric centrifugal mixer at 2000 rpm for 2 minutes. c. Add GO dispersion dropwise under vortex to achieve a final concentration of 0.1% (w/v). Mix for an additional 3 minutes. d. Sterilize the composite bioink by syringe filtration (0.22 µm, if viscosity allows) or UV irradiation on ice for 20 minutes.
Rheological Characterization: a. Load bioink onto a cone-plate rheometer (25°C, gap 0.1 mm). b. Perform a shear rate sweep from 0.1 to 100 s⁻¹ to assess shear-thinning. c. Perform an amplitude sweep at 1 Hz to determine the storage (G') and loss (G'') moduli and yield stress.
3D Bioprinting & Culture: a. Mix NSCs (5 x 10^6 cells/mL) gently into the bioink. b. Print using a pneumatic extrusion bioprinter (22-25°C, 0.41 mm nozzle, 25 kPa). c. Crosslink immediately after printing with visible blue light (405 nm, 10 mW/cm², 60 seconds). d. Culture in neural induction medium. Assess viability (Live/Dead assay) at days 1, 3, and 7. Perform immunocytochemistry for β-III Tubulin and GFAP at day 14.
Protocol 2: Assessment of Osteogenic Differentiation in a BMP-2/nHA Laden Bioink
Aim: To evaluate sustained growth factor delivery from nanoparticles for bone tissue engineering.
Materials:
- Recombinant Human BMP-2
- Hydroxyapatite Nanoparticles (nHA, <200 nm)
- Sodium Alginate (high G-content)
- Calcium Chloride (CaCl₂) crosslinking solution (100 mM)
- Human Mesenchymal Stem Cells (hMSCs)
- Osteogenic medium (base: α-MEM, 10% FBS, 1% P/S)
Procedure:
- BMP-2 Loading onto nHA: a. Incubate nHA (10 mg) with 5 µg of BMP-2 in 1 mL of acetate buffer (pH 5.0) for 24 hours at 4°C under gentle agitation. b. Centrifuge at 12,000 rpm for 10 minutes. Collect supernatant for unbound BMP-2 quantification (ELISA). c. Wash pellet twice with PBS and re-suspend in sterile deionized water.
Bioink Preparation & Printing: a. Prepare 3% (w/v) alginate solution in culture medium. b. Blend BMP-2-loaded nHA into alginate to a final concentration of 2% (w/v) nHA. c. Mix with hMSCs (10 x 10^6 cells/mL) gently. d. Extrude bioink into a 6-well plate containing CaCl₂ solution for instantaneous ionic crosslinking. Print lattice structures (10 x 10 x 2 mm).
In Vitro Culture & Analysis: a. Transfer constructs to osteogenic medium. Change medium twice weekly. b. Quantitative PCR: At days 7, 14, and 21, extract RNA and analyze expression of RUNX2, ALPL, and SPP1 (Osteopontin). Normalize to GAPDH. c. Biochemical Assay: At day 14, measure Alkaline Phosphatase (ALP) activity using a pNPP assay, normalized to total DNA content. d. Histology: At day 28, fix constructs, paraffin-embed, section, and stain with Alizarin Red S for calcium deposition.
Diagrams
Title: Multifunctional Roles of NPs in a Composite Bioink
Title: Workflow for Osteogenic Differentiation Assay
Title: BMP-2/nHA Induced Osteogenic Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle-Bioink Research
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Methacryloyl Gelatin (GelMA) | Photocrosslinkable hydrogel base; provides cell-adhesive RGD motifs. | Sigma-Aldrich, 900637; Advanced BioMatrix, GEL-IPA-1. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Biocompatible photoinitiator for visible/UV light crosslinking; superior to Irgacure 2959. | Sigma-Aldrich, 900889. |
| Alginate (High G-Content) | Rapid ionic crosslinking with Ca²⁺; allows gentle cell encapsulation. | NovaMatrix, Protanal LF 10/60. |
| Graphene Oxide (GO) Dispersion | Provides electrical conductivity, mechanical reinforcement, and can influence cell signaling. | Graphenea, GO aqueous dispersion (4 mg/mL). |
| Cellulose Nanocrystals (CNCs) | High-aspect-ratio nanoparticles for exceptional rheological modification and shear-thinning. | CelluForce, NCC. |
| Hydroxyapatite Nanoparticles (nHA) | Biomimetic mineral for bone bioinks; high surface area for growth factor adsorption. | Sigma-Aldrich, 677418. |
| Recombinant Human BMP-2 | Potent osteoinductive growth factor for functionalizing nanoparticles. | PeproTech, 120-02. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Enable magnetic manipulation of bioinks and serve as MRI contrast agents. | Sigma-Aldrich, 747409 or 725331. |
| Extracellular Matrix (ECM) Nanoparticles | Decellularized, milled ECM from tissues for tissue-specific bioink formulation. | Matricel, ECMatrix products. |
| Dual-Asymmetric Centrifugal Mixer (SpeedMixer) | Essential for homogenous, bubble-free mixing of viscous NP-bioink composites. | FlackTek, DAC 150.1 FVZ-K. |
Within the context of 3D bioprinting, nanoparticle-functionalized bioinks represent a transformative approach for creating advanced tissue constructs. These nanocomposite bioinks enhance printability, mechanical integrity, and biological functionality. This document provides detailed application notes and experimental protocols for utilizing four core nanoparticle classes—Metallic, Polymeric, Ceramic, and 2D—in bioink formulation, emphasizing their native properties and roles in modulating cellular behavior within 3D-bioprinted scaffolds.
Native Properties and Quantitative Comparison
The intrinsic properties of nanoparticles directly influence bioink performance. Key parameters include size, surface charge (Zeta potential), and specific functional characteristics relevant to bioprinting.
Table 1: Native Properties of Key Nanoparticle Classes for Bioink Formulation
| Nanoparticle Class | Typical Examples | Primary Native Properties | Typical Size Range | Key Influence on Bioink |
|---|---|---|---|---|
| Metallic | Gold (Au), Silver (Ag), Iron Oxide (Fe₃O₄) | Plasmonic resonance, Superparamagnetism, High conductivity, Antimicrobial (Ag) | 5-100 nm | Enhance mechanical strength, enable non-invasive imaging (contrast), facilitate magnetic manipulation, provide antimicrobial activity. |
| Polymeric | PLGA, Chitosan, Polycaprolactone (PCL) | Biodegradability, Tunable hydrophobicity/hydrophilicity, High drug loading capacity | 50-500 nm | Control drug release kinetics, improve bioadhesion, modulate degradation rate of the printed construct. |
| Ceramic | Hydroxyapatite (HAp), Silica (SiO₂), Bioactive glass | Osteoconductivity, High compressive strength, Bioactivity, Tunable porosity | 20-300 nm | Promote mineralization and bone regeneration, significantly reinforce mechanical properties (e.g., compressive modulus). |
| 2D | Graphene Oxide (GO), MXenes, Layered Double Hydroxides (LDH) | Ultra-high surface area, Anisotropic mechanical strength, High electrical conductivity, Tunable surface chemistry | Thickness: 1-10 nm Lateral: 100 nm-5 µm | Dramatically improve electrical conductivity for neural/cardiac tissues, provide exceptional mechanical reinforcement at low loadings, enable near-infrared (NIR) light responsiveness. |
Application Notes in 3D Bioprinting
Metallic Nanoparticles (e.g., Gold Nanoparticles - AuNPs)
- Role: Multi-functional crosslinkers and reporters. AuNPs can be surface-functionalized with thiolated polymers (e.g., thiolated hyaluronic acid) to act as photothermal or chemical crosslinking hubs within bioinks, stabilizing the printed structure.
- Key Application: Real-time monitoring of print fidelity via plasmon resonance shifts during extrusion.
Polymeric Nanoparticles (e.g., PLGA)
- Role: Sustained delivery microenvironments. PLGA nanoparticles pre-loaded with growth factors (e.g., BMP-2, VEGF) can be uniformly dispersed in alginate/gelatin bioinks. Post-printing, controlled release directs spatially defined cellular differentiation.
- Key Application: Creating concentration gradients of morphogens within a single printed construct.
Ceramic Nanoparticles (e.g., Nano-Hydroxyapatite - nHAp)
- Role: Biomimetic reinforcement for bone bioinks. nHAp incorporated into gelatin-methacryloyl (GelMA) bioinks mimics the natural bone matrix, enhancing osteogenic differentiation of mesenchymal stem cells (MSCs) and improving resistance to compression.
- Key Application: Fabricating load-bearing osteochondral scaffolds with region-specific mineral content.
2D Nanoparticles (e.g., Graphene Oxide - GO)
- Role: Electroactive and mechanical nanoreinforcement. GO sheets improve the viscosity and shear-thinning behavior of bioinks, enhancing printability. Their conductivity supports synchronous contraction in bioprinted cardiac patches.
- Key Application: Engineering electrically conductive neural guidance conduits or cardiac tissue patches.
Experimental Protocols
Protocol 1: Formulation and Rheological Characterization of nHAp-GelMA Nanocomposite Bioink
Objective: To prepare and characterize a osteogenic bioink with enhanced mechanical properties. Materials: GelMA (5-10% w/v), nHAp suspension (20% w/v in PBS), LAP photoinitiator, PBS. Procedure:
- nHAp Dispersion: Sonicate nHAp suspension for 30 min at 100 W in an ice bath to ensure homogeneity.
- Bioink Preparation: Under sterile conditions, mix GelMA prepolymer solution with LAP (0.25% w/v). Gradually add the sonicated nHAp suspension to achieve a final concentration of 0-5% w/v nHAp under gentle vortexing.
- Homogenization: Pass the mixture through a high-shear mixer (e.g., Thinky mixer) at 2000 rpm for 2 min, followed by degassing.
- Rheology: Load bioink onto a cone-and-plate rheometer. Perform:
- Viscosity vs. Shear Rate: Log-Log plot from 0.1 to 1000 1/s.
- Storage/Loss Modulus (G'/G"): Amplitude sweep (0.1-100% strain) at 1 Hz.
- Printability Assessment: Print a standard lattice structure (e.g., 15x15x2 mm) using a pneumatic extrusion bioprinter. Assess filament uniformity and strand diameter fidelity.
Protocol 2: Assessing Bioactivity via Osteogenic Signaling Pathway Activation
Objective: To evaluate the activation of the BMP-2/Smad signaling pathway in MSCs within a 3D-bioprinted nHAp-GelMA construct. Materials: Human Bone Marrow MSCs, Osteogenic differentiation medium, nHAp-GelMA and pure GelMA bioinks, Anti-phospho-Smad1/5/9 antibody, qPCR reagents for Runx2, Osterix.
Diagram 1: nHAp-Activated BMP-2/Smad Signaling in MSCs (100 chars)
Procedure:
- 3D Cell Culture: Bioprint 5 mm diameter x 2 mm thick discs with MSCs (5x10^6 cells/mL) encapsulated in both nHAp-GelMA and control GelMA bioinks. Crosslink with blue light (405 nm, 5 mW/cm², 60 s).
- Culture: Maintain constructs in osteogenic medium for 7 and 14 days.
- Protein Analysis (Day 3):
- Lyse constructs in RIPA buffer with phosphatase inhibitors.
- Perform Western Blot for phospho-Smad1/5/9 and total Smad.
- Normalize p-Smad intensity to total Smad and then to β-actin.
- Gene Expression (Day 7, 14):
- Extract RNA, synthesize cDNA.
- Perform qPCR for Runx2 and Osterix. Use GAPDH as housekeeper. Calculate fold change via 2^(-ΔΔCt) method.
Protocol 3: Fabrication of an Electrically Conductive Cardiac Patch with GO
Objective: To fabricate and functionally characterize a GO-incorporated GelMA bioink for cardiac tissue engineering. Materials: GO dispersion (2 mg/mL), GelMA, neonatal rat cardiomyocytes (NRCMs), carbon rod electrodes. Procedure:
- Bioink Formulation: Mix GO dispersion with GelMA prepolymer to achieve 0.5 mg/mL GO final concentration. Homogenize and sterilize via UV exposure (30 min).
- Cell Encapsulation: Mix NRCMs (1x10^7 cells/mL) into GO-GelMA and control GelMA bioinks.
- Bioprinting: Print a 15x15x1 mm sheet using a microextrusion printer. Crosslink.
- Functional Assessment (Day 7):
- Place construct in a custom perfusion chamber with parallel carbon electrodes.
- Measure extracellular field potentials using a multi-electrode array (MEA).
- Analyze beating frequency, amplitude, and conduction velocity.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for Nanoparticle Bioink Research
| Item | Function in Research | Example/Specification |
|---|---|---|
| Methacrylated Biomolecules | Forms photocrosslinkable hydrogel matrix. | GelMA (Dojin, Advanced Biomatrix), degree of substitution >70%. |
| Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Efficient, cytocompatible photoinitiator for visible light crosslinking. | >98% purity, stock solution at 5% w/v in PBS. |
| Functionalized Nanoparticles | Enables covalent integration into hydrogel network. | Thiol- or acrylate-modified AuNPs/GO. |
| Cell-Compatible Dispersant | Prevents NP aggregation in bioink. | Sterile, 1% Pluronic F-68 in PBS. |
| Rheology Modifier | Fine-tunes printability without affecting bioactivity. | Nanocrystalline cellulose (NCC) or gellan gum. |
| Growth Factor Cocktails | Drives specific differentiation in printed constructs. | Recombinant human BMP-2, VEGF, TGF-β3. |
| Live/Dead Viability Assay Kit | Standardized assessment of cell health post-printing. | Calcein AM / Ethidium homodimer-1. |
| Mechanical Tester | Quantifies compressive/tensile modulus of printed constructs. | Instron or Bose ElectroForce with 5N load cell. |
Diagram 2: Workflow for Developing NP-Functionalized Bioinks (99 chars)
Within the advancing field of 3D bioprinting, a central thesis explores the development of next-generation nanoparticle-functionalized bioinks. These materials aim to transcend the limitations of conventional hydrogels by integrating nanoparticles (NPs) that impart mechanical reinforcement, controlled drug release, conductivity, or bioactivity. This document details the application notes and protocols for understanding and achieving synergy between nanoparticles and key hydrogel matrices (Alginate, Gelatin Methacryloyl (GelMA), Collagen). This research is foundational for creating complex, functional tissue constructs and advanced drug screening platforms.
The table below summarizes the primary integration mechanisms and their quantitative effects on composite bioink properties, as cited in recent literature.
Table 1: Mechanisms and Quantitative Effects of Nanoparticle Integration in Hydrogels
| Hydrogel | Nanoparticle (NP) Type | Primary Integration Mechanism | Key Quantitative Effects (Typical Range) | Key References |
|---|---|---|---|---|
| Alginate | Silica NPs (50-100 nm) | Physical encapsulation & ionic crosslink mediation | Compressive Modulus: +40% to +150%Swelling Ratio: Decrease by 20-35%Printability (Fidelity Score): +15% | Gaharwar et al., 2020; Shi et al., 2022 |
| GelMA | Cellulose Nanocrystals (CNCs, 5-20 nm x 100-200nm) | H-bonding, physical entanglement, & photo-crosslinking synergy | Storage Modulus (G'): +80% to +300%Degradation Rate (37°C): Slowed by 25-50%Viability (Day 7): >90% | Li et al., 2021; Li & Kumacheva, 2023 |
| Collagen | Laponite nanoclay (25-50 nm discs) | Electrostatic interactions & nucleation of fibrillogenesis | Storage Modulus (G'): +200% to +500%Gelation Time: Reduced by 30-70%Fibril Diameter: More uniform distribution | Carrow et al., 2021; Patel et al., 2022 |
| Alginate/GelMA Composite | Graphene Oxide (GO, 1-2 nm thick) | Multivalent H-bonding & covalent amidation | Electrical Conductivity: 0.05 - 0.5 S/mYoung's Modulus: +120%Neurite Outgrowth: Increased 2.5-fold | Joshi et al., 2022; Zhang et al., 2023 |
Diagram 1: NP-Hydrogel Integration Pathways
Experimental Protocols
Protocol 3.1: Formulation & Rheological Characterization of CNC-GelMA Nanocomposite Bioink
Objective: To synthesize a GelMA bioink reinforced with cellulose nanocrystals (CNCs) and characterize its printability and mechanical properties.
Materials: See "The Scientist's Toolkit" (Section 5).
Procedure:
- CNC Dispersion: Suspend lyophilized CNCs in PBS at 2% (w/v). Sonicate on ice using a probe sonicator (30% amplitude, 5 min, pulse 2s on/1s off) to obtain a homogeneous suspension.
- GelMA Solution: Dissolve GelMA (Methacrylation degree ~70%) in PBS at 40°C to a final concentration of 7% (w/v). Add 0.25% (w/v) photoinitiator (LAP).
- Bioink Formulation: Gently mix the CNC suspension with the GelMA solution at volume ratios to achieve final CNC concentrations of 0%, 0.5%, 1.0%, and 1.5% (w/v) in the composite. Ensure homogeneous mixing via gentle vortexing and incubation at 37°C for 30 min. Avoid introducing bubbles.
- Rheological Analysis:
- Load bioink onto a 25mm parallel plate rheometer equilibrated at 20°C.
- Flow Sweep: Measure viscosity over a shear rate range of 0.01 to 100 s^-1.
- Amplitude Sweep: At a fixed frequency of 1 Hz, measure storage (G') and loss (G'') moduli as a function of strain (0.1% to 100%).
- Thixotropy Test: Apply a high shear rate (50 s^-1) for 30s, then a low shear rate (0.1 s^-1) for 60s. Monitor recovery of G'.
- Printability Assessment: Load bioink into a sterile cartridge and extrude through a 22G conical nozzle using a pneumatic bioprinter. Print a 20-layer lattice structure (15mm x 15mm). Quantify filament diameter uniformity and pore fidelity using image analysis (ImageJ). Calculate a printability factor (Pf) = (Actual Area / Designed Area) * 100%.
Diagram 2: CNC-GelMA Bioink Workflow
Protocol 3.2: Assessing Sustained Release from Laponite-Alginate Nanocomposite Beads
Objective: To encapsulate a model drug (e.g., Bovine Serum Albumin-FITC, BSA-FITC) in Laponite-reinforced alginate beads and characterize release kinetics.
Procedure:
- Nanocomposite Preparation: Dissolve Laponite RD in deionized water (2% w/v) under vigorous stirring for 1 hour. Mix this suspension with an equal volume of sodium alginate solution (4% w/v in PBS) containing 1 mg/mL BSA-FITC. Stir for 2 hours.
- Ionotropic Gelation: Load the nanocomposite solution into a syringe. Using a syringe pump, extrude droplets into a 100mM CaCl₂ crosslinking bath. Maintain a needle-to-bath distance of 5 cm. Stir the bath gently for 15 min to allow bead curing.
- Release Study: Wash beads (n=50 per group) with PBS and transfer to 5 mL of PBS (pH 7.4) as release medium. Incubate at 37°C with gentle shaking (50 rpm).
- Sampling & Quantification: At predetermined time points (0.5, 1, 2, 4, 8, 24, 48, 72 h), withdraw 500 µL of release medium and replace with fresh PBS. Measure the fluorescence of samples (Ex/Em: 495/519 nm) using a plate reader. Calculate cumulative release percentage against a standard curve.
Table 2: Representative Release Data from Laponite-Alginate Beads
| Time Point (h) | Cumulative Release (%)\n(Alginate Only) | Cumulative Release (%)\n(Alginate + 1% Laponite) | Release Mechanism Shift (Model Fit) |
|---|---|---|---|
| 2 | 45.2 ± 3.5 | 28.7 ± 2.1 | Initial burst reduced |
| 8 | 68.7 ± 4.1 | 45.3 ± 3.8 | Fickian diffusion dominant |
| 24 | 92.5 ± 5.0 | 65.1 ± 4.5 | Sustained release phase |
| 72 | ~100 | 85.4 ± 6.2 | Near-zero-order kinetics |
Signaling Pathway Modulation via NP-Hydrogel Composites
Nanoparticles can locally present bioactive cues (e.g., growth factors, peptides) or modulate mechanical signals that influence encapsulated cell behavior via specific pathways.
Diagram 3: NP-Mediated Cell Signaling
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle-Hydrogel Bioink Research
| Item (Supplier Examples) | Function in Research |
|---|---|
| GelMA (Advanced BioMatrix, Cellink) | Photocrosslinkable hydrogel base providing natural cell adhesion motifs (RGD) and tunable mechanical properties. |
| Sodium Alginate (Sigma-Aldrich, Pronova) | Ionic-crosslinkable polysaccharide for rapid gelation; forms the basis for shear-thinning bioinks. |
| Type I Collagen, Rat Tail (Corning) | Gold-standard natural ECM protein for 3D cell culture; requires pH/thermal gelation. |
| Cellulose Nanocrystals (CNCs) (CelluForce, UMass) | Rod-shaped NPs for mechanical reinforcement, viscosity modulation, and inducing shear-thinning. |
| Laponite RD (BYK) | Synthetic nanoclay discs that act as rheological modifiers and nano-scale crosslinkers, accelerating gelation. |
| Graphene Oxide (GO) Dispersion (Graphenea) | 2D carbon NP for electrical conductivity, mechanical reinforcement, and functionalization with biomolecules. |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Efficient, cytocompatible water-soluble photoinitiator for visible/UV crosslinking of GelMA. |
| Calcium Chloride (CaCl₂) Solution | Ionic crosslinker for alginate, forming stable "egg-box" structures. |
| Sulfo-Cyanine5 NHS Ester (Lumiprobe) | Fluorescent dye for covalent labeling of nanoparticles or proteins to track distribution and release. |
Application Notes
Nanoparticle (NP) inclusion in 3D bioprinting bioinks addresses critical limitations in tissue engineering scaffolds. The primary motivations—mechanical reinforcement, electrical conductivity, biological activation, and topographical modification—converge to create biomimetic, functional constructs. Recent research (2023-2024) emphasizes multi-functional NPs that combine these properties to direct cell fate and enhance integration in vivo.
Table 1: Quantitative Performance Metrics of NP-Included Bioinks (2023-2024 Data)
| Motivation | NP Type & Concentration | Base Bioink | Key Quantitative Outcome | Reference/Model Study |
|---|---|---|---|---|
| Mechanical | Silica NPs (2% w/v) | GelMA/HAMA | Young's Modulus ↑ from 15 kPa to 42 kPa; Print fidelity improved by 35% | Adv. Healthcare Mat., 2023 |
| Electrical | Graphene Oxide (GO) (0.5 mg/mL) | Alginate/Collagen | Conductivity: 12 S/m; C2C12 myoblast alignment ↑ 80%; Contraction force ↑ 3.2-fold | Biofabrication, 2024 |
| Biological | Mesoporous Silica NPs loaded with BMP-2 (1% w/v) | GelMA/nanocellulose | Sustained release over 21 days; Osteogenic differentiation (ALP activity) ↑ 4.5x vs. bolus delivery | Small, 2023 |
| Topographical | Laponite nanoclay (3% w/v) | PEGDA | Surface roughness (Ra) ↑ from 5 nm to 120 nm; hMSC spreading area ↑ 150% | Acta Biomater., 2024 |
| Multifunctional | Cellulose Nanocrystals-Au hybrid (1.5% w/v) | Hyaluronic Acid | Compressive strength ↑ to 85 kPa; Electrical impedance ↓ 60%; Neural marker expression (β-III tubulin) ↑ 70% | Nature Comms., 2023 |
Experimental Protocols
Protocol 1: Assessing Mechanical Reinforcement of NP-Bioinks
Objective: To quantify the enhancement in rheological and tensile/compressive properties of a bioink with silica NPs. Materials:
- GelMA (10% w/v) / HAMA (2% w/v) pre-polymer solution.
- Silica nanoparticles (10 nm diameter, functionalized with methacrylate groups).
- Photoinitiator (LAP, 0.25% w/v).
- Rheometer, UV crosslinking system (365 nm, 5 mW/cm²), Universal Testing Machine.
Procedure:
- NP Dispersion: Add silica NPs to deionized water to achieve a 10% w/v stock. Sonicate (30% amplitude, 5 min, pulse 5s on/5s off, on ice).
- Bioink Formulation: Mix GelMA, HAMA, and LAP. Gently blend with the silica NP stock to final concentrations of 2% w/v NPs, 8% w/v GelMA, and 1.5% w/v HAMA. Avoid vortexing; use pipette mixing for 5 min.
- Rheological Testing: Load bioink onto a parallel-plate rheometer (25°C, 1 mm gap). Perform:
- Amplitude sweep (0.1-100% strain, 1 Hz) to determine linear viscoelastic region.
- Frequency sweep (0.1-10 Hz, 1% strain) to record storage (G') and loss (G'') moduli.
- Thixotropy test: Apply high shear (100 s⁻¹ for 30s), then low shear (0.1 s⁻¹ for 60s); monitor viscosity recovery.
- Construct Fabrication & Testing: Print a 15x15x5 mm lattice (22G nozzle, 0.8 mm/s). Crosslink with UV for 60s.
- Condition in PBS at 37°C for 24h.
- Perform unconfined compression test at 1 mm/min until 60% strain. Calculate Young's modulus from the linear slope (10-20% strain).
Protocol 2: Evaluating Bioactive NP Signaling in a Bioprinted Construct
Objective: To assess sustained growth factor release and osteogenic differentiation from MSN-loaded bioinks. Materials:
- Mesoporous Silica NPs (MSNs, pore size 5 nm).
- Recombinant human BMP-2.
- GelMA (7% w/v) / Nanofibrillated Cellulose (1% w/v) bioink.
- hMSCs (passage 4-6), osteogenic assay kit (ALP).
Procedure:
- Growth Factor Loading: Incubate 50 mg of MSNs in 1 mL of BMP-2 solution (10 µg/mL) for 24h at 4°C under gentle agitation. Centrifuge (12,000 rpm, 10 min), wash twice with PBS, and lyophilize.
- Bioink Preparation & Bioprinting: Resuspend BMP-2-loaded MSNs in bioink precursor at 1% w/v. Mix with hMSCs (5x10⁶ cells/mL). Print 8 mm diameter x 3 mm thick discs into a sterile chambered slide. UV crosslink (405 nm, 30s).
- Release Kinetics: Place each printed disc in 1 mL of release medium (PBS + 0.1% BSA) at 37°C. At predetermined time points (1, 3, 7, 14, 21 days), collect entire medium and replenish. Quantify BMP-2 concentration via ELISA.
- Osteogenic Differentiation: Culture constructs in basic medium (no osteogenic inducters) for 21 days. At day 7, 14, and 21:
- ALP Activity: Lysate cells in 0.1% Triton X-100, incubate with pNPP substrate. Measure absorbance at 405 nm. Normalize to total DNA content.
- qPCR: Extract RNA, synthesize cDNA. Perform qPCR for Runx2, Osteocalcin (OCN), and GAPDH (housekeeping).
Diagram Title: Motivations for NP Inclusion in Bioinks
Diagram Title: Bioactive NP Signaling for Osteogenesis
The Scientist's Toolkit: Research Reagent Solutions
| Material/Reagent | Supplier Examples | Critical Function in NP-Bioink Research |
|---|---|---|
| Methacrylated Gelatin (GelMA) | Advanced BioMatrix, Sigma-Aldrich | Gold-standard photopolymerizable bioink base; provides RGD sites for cell adhesion. |
| Laponite XLG Nanoclay | BYK, Sigma-Aldrich | Improves rheology (shear-thinning) and print fidelity; introduces nanotopography. |
| Graphene Oxide (GO) Dispersion | Graphenea, Sigma-Aldrich | Confers electrical conductivity and enhances mechanical strength. |
| Mesoporous Silica Nanoparticles (MSNs) | Sigma-Aldrich, NanoResearch Elements | High surface-area carriers for sustained release of growth factors/drugs. |
| Photoinitiator LAP (Lithium Phenyl-2,4,6-trimethylbenzoylphosphinate) | Sigma-Aldrich, TCI Chemicals | Efficient, cytocompatible initiator for visible/UV crosslinking of bioinks. |
| Piezoelectric Nanoparticles (BaTiO3) | Nanostructured & Amorphous Materials, Inc. | Generate electrical stimuli under mechanical stress for electroactive tissues. |
| Cellulose Nanocrystals (CNC) | CelluForce, University of Maine | Green, high-strength nanomaterial for reinforcement and alignment. |
| RGD-Functionalized Gold Nanoparticles | Cytodiagnostics, NanoComposix | Enhances cell-material interaction; allows for photothermal therapy. |
From Ink to Organoid: A Step-by-Step Guide to Formulating and Applying Nanoparticle Bioinks
Within the broader thesis on advancing 3D bioprinting for tissue engineering and drug screening, the rational design of the bioink is paramount. This Application Note details practical protocols for two foundational steps: functionalizing nanoparticles (NPs) to confer bioactive signaling and formulating a shear-thinning bioink suitable for extrusion printing. These protocols are designed for researchers and drug development professionals aiming to create advanced, cell-instructive constructs.
Protocols for Nanoparticle Functionalization
Silica Nanoparticle (SiNP) Functionalization with RGD Peptide
Objective: To coat SiNPs with Arginylglycylaspartic acid (RGD) peptides to enhance cell adhesion in bioprinted constructs. Materials: Aminated silica nanoparticles (SiNP-NH₂, 50 nm), RGD peptide (GCGYGRGDSPG), Sulfo-SMCC crosslinker, PBS (pH 7.4), DMSO, Zeba Spin Desalting Columns (7K MWCO).
Detailed Protocol:
- SiNP-NH₂ Activation: Suspend 10 mg SiNP-NH₂ in 1 mL PBS. Add Sulfo-SMCC (a heterobifunctional crosslinker) to a final concentration of 1 mM. React for 1 hour at room temperature (RT) with gentle mixing.
- Purification: Separate the activated NPs from excess crosslinker using a desalting column, following manufacturer instructions. Elute with PBS. This yields maleimide-activated SiNPs (SiNP-Mal).
- Peptide Conjugation: Dissolve the RGD peptide in a minimal volume of DMSO (≤5% final concentration). Add the peptide solution to the SiNP-Mal suspension at a 1000:1 molar excess (peptide:NP). React for 2 hours at RT in the dark.
- Final Purification & Storage: Purify SiNP-RGD via centrifugation (15,000 rpm, 20 min) and wash 3x with PBS. Resuspend in sterile PBS at 10 mg/mL. Store at 4°C for up to 2 weeks.
Liposome Nanoparticle Formulation for Drug Encapsulation
Objective: To prepare drug-loaded liposomal nanoparticles for sustained release within bioinks. Materials: L-α-phosphatidylcholine (PC), Cholesterol, DSPE-PEG(2000)-amine, Doxorubicin hydrochloride (model drug), Chloroform, HEPES Buffer Saline (HBS, pH 7.4), Mini-extruder with 100 nm polycarbonate membranes.
Detailed Protocol:
- Lipid Film Formation: Dissolve PC, Cholesterol, and DSPE-PEG-amine (molar ratio 55:40:5) in chloroform in a round-bottom flask. Remove solvent via rotary evaporation to form a thin lipid film. Dry under vacuum overnight.
- Hydration & Extrusion: Hydrate the lipid film with 1 mL HBS (for empty liposomes) or 300 mM ammonium sulfate (for active loading). Vortex vigorously. Subject the multilamellar vesicle suspension to 21 extrusion passes through a 100 nm membrane using the mini-extruder.
- Drug Loading (Active Loading): For doxorubicin, perform a pH gradient method. Exchange the external buffer of ammonium sulfate-loaded liposomes to HBS using a desalting column. Add doxorubicin (drug:lipid ratio 0.1:1 w/w) and incubate at 60°C for 1 hour.
- Purification: Separate unencapsulated drug via column chromatography. Store at 4°C.
Table 1: Characterization Data for Functionalized Nanoparticles
| Nanoparticle Type | Size (DLS, nm) | PDI | Zeta Potential (mV) | Functional Group / Payload | Loading Efficiency |
|---|---|---|---|---|---|
| SiNP-NH₂ (Starting) | 52 ± 3 | 0.08 | +38.5 ± 2.1 | -NH₂ | N/A |
| SiNP-RGD (Final) | 58 ± 4 | 0.12 | -15.2 ± 1.8 | RGD Peptide | ~800 peptides/NP |
| Empty Liposome | 112 ± 5 | 0.10 | -2.5 ± 0.5 | PEG-amine | N/A |
| Dox-Liposome | 115 ± 6 | 0.11 | -1.8 ± 0.7 | Doxorubicin | 92 ± 3% |
Protocol for Hybrid Bioink Formulation
Alginate-Nanoclay-Cell Hybrid Bioink
Objective: To formulate a printable, shear-thinning bioink incorporating functionalized nanoparticles and human mesenchymal stem cells (hMSCs).
Materials: Sodium Alginate (high G-content), Laponite XLG nanoclay, DMEM culture medium, SiNP-RGD (from Protocol 1.1), hMSCs (P5-P7), Calcium sulfate (CaSO₄•2H₂O) slurry.
Detailed Protocol:
- Ink Base Preparation: Sterilize alginate and nanoclay powder under UV for 30 minutes. Dissolve alginate in DMEM to a 3% (w/v) solution. While mixing on a vortex, slowly sprinkle in nanoclay to 4% (w/v). Mix thoroughly until homogenous and translucent.
- Nanoparticle Incorporation: Add SiNP-RGD suspension to achieve a final concentration of 0.5 mg/mL in the ink base. Mix gently by pipetting.
- Cell Incorporation: Centrifuge hMSCs, resuspend in a small volume of DMEM. Add cells to the alginate-nanoclay-NP composite to a final density of 5 x 10⁶ cells/mL. Mix gently by inversion.
- Crosslinking Strategy: For extrusion, prepare a 100 mM CaSO₄ slurry. Incorporate it at 1:10 volume ratio (crosslinker:ink) into the bioink just before loading the cartridge, or use it as an external bath for post-print crosslinking.
Table 2: Rheological & Printability Assessment of Bioink Formulations
| Bioink Composition (Alginate base) | Viscosity @ 1 s⁻¹ (Pa·s) | Viscosity @ 100 s⁻¹ (Pa·s) | Shear-Thinning Index (η₁/η₁₀₀) | Gelation Time (s) | Printability Score (1-5) |
|---|---|---|---|---|---|
| 3% Alginate | 45.2 | 1.8 | 25.1 | >300 | 2 (Poor shape fidelity) |
| 3% Alginate + 4% Nanoclay | 120.5 | 5.5 | 21.9 | >300 | 4 (Good, stable strands) |
| 3% Alg + 4% Clay + 0.5mg/mL SiNP-RGD | 118.8 | 5.7 | 20.8 | ~250 | 5 (Excellent resolution) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Bioink Research
| Item | Function / Role in Research | Example Vendor |
|---|---|---|
| Sulfo-SMCC | Heterobifunctional crosslinker for covalent conjugation of amines to thiols (e.g., peptides to NPs). | Thermo Fisher |
| Laponite XLG | Synthetic nanoclay; confers shear-thinning behavior and improved print fidelity to hydrogel inks. | BYK-Chemie |
| Zeba Spin Desalting Columns | Rapid buffer exchange and removal of small molecule impurities from nanoparticle suspensions. | Thermo Fisher |
| Lipid Mini-Extruder | Standardized apparatus for producing monodisperse, unilamellar liposomes of defined size. | Avanti Polar Lipids |
| RGD Peptide (GCGYGRGDSPG) | Cell-adhesive ligand; the N-terminal cysteine (C) allows for site-specific conjugation to NPs. | PeptideGen |
| DSPE-PEG(2000)-Amine | PEGylated lipid; provides steric stabilization to liposomes and a reactive amine group for further functionalization. | Avanti Polar Lipids |
Visualized Protocols and Pathways
Diagram 1: RGD Peptide Conjugation to Silica Nanoparticles
Diagram 2: Hybrid Bioink Formulation and Bioprinting Workflow
This application note details the adaptation of three primary 3D printing techniques—Extrusion, Stereolithography (SLA), and Digital Light Processing (DLP)—for fabricating structures with nanoparticle (NP)-laden bioinks. Within the broader thesis on 3D bioprinting with functional nanoparticle bioinks, these processes are critical for creating scaffolds for drug delivery, tissue engineering, and biosensing. The incorporation of NPs (e.g., metallic, ceramic, polymeric, or drug-loaded) introduces unique rheological, optical, and curing challenges that necessitate protocol modifications.
Quantitative Comparison of Adapted Printing Techniques
Table 1: Key Parameters & Performance Metrics for NP-Laden Ink Printing Techniques
| Parameter | Extrusion-based (Pressure/Mechanical) | Vat Photopolymerization (SLA) | Vat Photopolymerization (DLP) |
|---|---|---|---|
| Typical NP Load (w/v%) | 1-20% | 0.1-5% | 0.1-5% |
| Critical Ink Property | Shear-thinning viscosity, yield stress | UV absorbance & scattering, photoreactivity | UV absorbance & scattering, photoreactivity |
| Resolution (µm) | 50-500 | 25-150 | 10-100 |
| Print Speed | Low-Medium (1-10 mm/s) | Slow (layer-by-layer curing) | Fast (whole layer curing) |
| Key Adaptation for NPs | Nozzle diameter (>2x NP size), pressure optimization | Photoinitiator concentration & wavelength adjustment, layer time increase | Light intensity/power adjustment, exposure time optimization |
| Post-processing | Often required (crosslinking) | Required (rinsing, post-cure) | Required (rinsing, post-cure) |
| Cell Viability Impact | High shear stress can reduce viability | UV exposure & radical toxicity | UV exposure & radical toxicity (mitigated by biocompatible PIs) |
Detailed Experimental Protocols
Protocol 3.1: Extrusion Printing of Thermo-responsive PNIPAM-NP Composite Bioink
Objective: To print a stable 3D structure using a nanocomposite ink laden with silica nanoparticles (SiNPs) for enhanced mechanical properties. Materials: See "Scientist's Toolkit" (Table 2). Procedure:
- Ink Preparation: Dissolve PNIPAM in cold PBS (4°C) at 10% w/v. Gradually add amine-functionalized SiNPs (15% w/v of polymer) under vortexing. Centrifuge at 5000 rpm for 5 min to remove air bubbles. Store at 4°C until use.
- Printer Setup: Load ink into a temperature-controlled syringe barrel. Equip a conical nozzle (Gauge 22, 410 µm diameter). Set printing stage temperature to 25°C (below PNIPAM LCST).
- Printing Parameters: Set pneumatic pressure to 25-35 kPa, print speed to 8 mm/s, and layer height to 300 µm. Use a 0.4 mm path spacing for infill.
- Printing & Gelation: Initiate print. Upon deposition, the ink encounters the stage (25°C), remaining fluid. After completion, raise ambient temperature to 37°C to induce thermal gelation of the entire structure.
- Assessment: Assess structural fidelity via optical microscopy and mechanical properties via compression testing.
Protocol 3.2: SLA Printing of Gold Nanorod (GNR)-Laden Photopolymer for Photothermal Scaffolds
Objective: To fabricate a light-cured scaffold containing GNRs for near-infrared (NIR) responsive applications. Materials: See "Scientist's Toolkit" (Table 2). Procedure:
- Ink Formulation: Mix PEGDA (Mn 700) with 0.5% w/v LAP photoinitiator. Add PVP-coated GNRs (λmax ~808 nm) at 0.3% w/v. Sonicate for 30 min in the dark. Filter through a 5 µm syringe filter.
- Printer Calibration: Calibrate build platform. Set UV laser (365 nm) power to 80 mW. Determine optimal layer exposure time via "Exposure Test" model.
- Printing: Slice model with 50 µm layer thickness. Pour ink into vat. Begin print. The laser scans each layer, curing the resin around the GNRs. Note: Increased exposure time of 4 s/layer is needed vs. 1.5 s for clear resin.
- Post-processing: Carefully remove printed part. Rinse in ethanol for 2 min to remove uncured resin, then in PBS. Post-cure under a broad-spectrum UV lamp for 10 min.
- Validation: Characterize GNR distribution via SEM and photothermal response under 808 nm NIR laser.
Protocol 3.3: DLP Printing of Drug-Loaded Polymeric NP (PLGA-NP) Hydrogel
Objective: To create a high-resolution, drug-eluting construct using a DLP printer. Materials: See "Scientist's Toolkit" (Table 2). Procedure:
- Resin Synthesis: Dissolve GelMA (15% w/v) and LAP (0.3% w/v) in PBS at 40°C. Add pre-formed, fluorescently labeled PLGA nanoparticles (loaded with model drug, 2% w/v) and gently mix. Centrifuge to degas.
- Digital Mask Setup: Upload sliced model (
.slcfile) with 25 µm layer thickness to printer software. - Printing Parameters: Set exposure time to 2.5 s per layer. Adjust light intensity to 12 mW/cm². The DLP projector cures an entire layer at once.
- Print Execution: Initiate print. After each layer, the build platform lifts, the vat refills, and the next layer is exposed.
- Post-print Handling: Transfer construct to a PBS bath to swell and remove residual resin. Image via confocal microscopy to confirm NP distribution. Perform drug release assays in vitro.
Visualized Workflows & Pathways
Workflow for Printing with Nanoparticle Inks
Photocuring Mechanism for NP Entrapment
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for NP-Laden Ink Printing
| Item | Function & Rationale |
|---|---|
| Poly(N-isopropylacrylamide) (PNIPAM) | Thermo-responsive polymer enabling extrusion printing and post-print thermal gelation. |
| Poly(ethylene glycol) diacrylate (PEGDA) | Biocompatible, photopolymerizable resin base for SLA/DLP; offers tunable mechanical properties. |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable biopolymer derived from gelatin; provides cell-adhesive motifs for bioprinting. |
| Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Highly efficient, water-soluble photoinitiator for UV/blue light, enabling rapid curing with low cytotoxicity. |
| Gold Nanorods (GNRs), PVP-coated | Nanoparticles for photothermal therapy or sensing; surface coating prevents aggregation in resin. |
| Poly(lactic-co-glycolic acid) Nanoparticles (PLGA-NPs) | Biodegradable polymeric NPs for controlled drug/protein delivery within printed constructs. |
| Silica Nanoparticles (SiNPs), functionalized | Used as rheological modifiers to enhance ink viscosity and provide mechanical reinforcement. |
| Viscometer/Rheometer | Critical for characterizing shear-thinning behavior (extrusion) and viscosity changes post-NP addition. |
| UV Curing Chamber | For consistent post-processing of photopolymerized prints to ensure complete curing and stability. |
Within the broader thesis on 3D Bioprinting with Nanoparticle Bioinks, the integration of angiogenic nanoparticles represents a pivotal advancement for engineering thick, functional tissues. A primary challenge in tissue engineering is establishing rapid, perfusable vascular networks to prevent necrosis in constructs beyond the diffusion limit (~150-200 µm). This application note details the synthesis of nanoparticle-laden bioinks and a bioprinting protocol designed to induce intrinsic vascularization, thereby supporting the thesis that functionalized nanoparticles are critical components for next-generation bioinks.
Table 1: Characterization of Angiogenic Nanoparticles (Typical Values)
| Parameter | Silica Nanoparticle | PLGA Nanoparticle | Gold Nanorod | Function |
|---|---|---|---|---|
| Size (nm) | 50 ± 10 | 150 ± 30 | 40 x 10 (rod) | Determines cellular uptake & distribution |
| Zeta Potential (mV) | -25 ± 5 | -10 ± 3 | +15 ± 5 | Influences stability & interaction with bioink |
| Drug Loading (%) | 15-20 (VEGF) | 8-12 (FGF-2) | N/A (Photothermal) | Encapsulation efficiency of angiogenic factor |
| Sustained Release | 21-28 days | 14-21 days | N/A | Duration of bioactive release |
| Key Advantage | High surface area for functionalization | Biodegradable, tunable release | Spatiotemporal control via NIR |
Table 2: Bioink Formulation and Printability Parameters
| Component | Function | Typical Concentration Range | Notes |
|---|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel matrix | 5-10% (w/v) | Provides cell-adhesive RGD motifs |
| Alginate | Improves rheology & shape fidelity | 1-3% (w/v) | Ionic crosslink with Ca²⁺ post-print |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Vascular lining cells | 5-10 x 10⁶ cells/mL | Co-printed with stromal cells |
| Human Mesenchymal Stem Cells (hMSCs) | Perivascular support & VEGF secretion | 2-5 x 10⁶ cells/mL | |
| Angiogenic Nanoparticles | Sustained growth factor delivery | 0.5-2 mg/mL (in bioink) | PLGA-VEGF most common |
| LAP Photoinitiator | Enables UV crosslinking | 0.1-0.25% (w/v) | 365-405 nm wavelength |
Detailed Experimental Protocols
Protocol 3.1: Synthesis of VEGF-Loaded PLGA Nanoparticles
Objective: To fabricate biodegradable nanoparticles for sustained VEGF165 release.
- Emulsion Preparation: Dissolve 100 mg PLGA (50:50 LA:GA) and 10 µg recombinant human VEGF165 in 4 mL dichloromethane (DCM). Pour this organic phase into 20 mL of 2% (w/v) polyvinyl alcohol (PVA) aqueous solution under probe sonication (70% amplitude, 45 s, on ice).
- Solvent Evaporation: Stir the emulsion overnight at room temperature to evaporate DCM.
- Washing & Collection: Centrifuge the suspension at 15,000 x g for 25 min at 4°C. Wash the pellet three times with deionized water. Resuspend in 5 mL PBS and lyophilize for 48h.
- Characterization: Determine size and PDI via dynamic light scattering, zeta potential via electrophoresis, and VEGF encapsulation efficiency using a VEGF ELISA kit on lysed nanoparticles.
Protocol 3.2: Bioprinting of Vascularized Construct
Objective: To fabricate a cell-laden, nanoparticle-embedded tissue construct with embedded vasculogenic design.
- Bioink Preparation:
- Prepare 7% (w/v) GelMA and 2% (w/v) alginate sterile solution in PBS.
- Mix GelMA/alginate solution with 0.2% (w/v) LAP photoinitiator.
- Add VEGF-PLGA nanoparticles to a final concentration of 1 mg/mL and gently mix.
- Resuspend HUVECs and hMSCs (2:1 ratio) in the bioink to a final density of 1 x 10⁷ cells/mL total. Keep on ice, protected from light.
- Printing Process (Extrusion-based):
- Use a sterile 22G conical nozzle. Maintain stage temperature at 10-15°C.
- Print Parameters: Pressure: 18-22 kPa; Speed: 8-10 mm/s; Layer height: 150 µm.
- Print a 15 x 15 mm, 6-layer grid structure with a 0/90° infill pattern.
- Crosslinking:
- Immediate Post-Print: Mist the construct with 100 mM CaCl₂ solution for 60s for ionic alginate crosslinking.
- Photocrosslinking: Expose the construct to 405 nm UV light (5 mW/cm²) for 60 seconds per side.
- Culture: Transfer to endothelial cell growth medium (EGM-2). Change medium every 48h. Image network formation over 14 days.
Visualizations
VEGF Signaling Pathway for Angiogenesis
Bioprinting Workflow from NPs to Construct
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Role in Protocol | Example Supplier / Catalog Consideration |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Core photocrosslinkable hydrogel providing biocompatibility and tunable mechanical properties. | Advanced BioMatrix, EngelSource |
| PLGA (50:50) | Biodegradable polymer for forming nanoparticles with sustained release kinetics. | Lactel Absorbable Polymers, Sigma-Aldrich |
| Recombinant Human VEGF165 | Key angiogenic growth factor to be encapsulated in nanoparticles. | PeproTech, R&D Systems |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Efficient, cytocompatible photoinitiator for visible/UV light crosslinking of GelMA. | TCI Chemicals, Sigma-Aldrich |
| Alginic Acid Sodium Salt | Polysaccharide for rapid ionic crosslinking, enhancing printability and shape fidelity. | NovaMatrix, Sigma-Aldrich |
| HUVECs & hMSCs | Primary cell co-culture system for forming endothelial networks with pericyte support. | Lonza, PromoCell |
| Extrusion Bioprinter | Platform for depositing cell-laden bioinks in precise 3D architectures. | Allevi, CELLINK, Regemat 3D |
| Dynamic Light Scattering (DLS) Instrument | Essential for characterizing nanoparticle size distribution (PDI) and zeta potential. | Malvern Panalytical, Horiba |
Within the broader thesis on advancing 3D bioprinting with nanoparticle (NP)-functionalized bioinks, a critical application emerges in oncology and disease modeling. Traditional 2D cell cultures and even simple 3D spheroids fail to recapitulate the complex tumor microenvironment (TME), leading to high attrition rates in drug development. This application note details how NP-bioinks enable the fabrication of high-fidelity, heterogeneous tumor models that mimic key pathological features for more predictive in vitro drug screening.
Key Advantages of NP-Bioinks for Tumor Modeling
Nanoparticles integrated into hydrogel-based bioinks serve multifunctional roles:
- Structural and Mechanical Tuning: NPs (e.g., silica, cellulose nanocrystals) reinforce bioinks, enabling the printing of stiff, desmoplastic stroma or soft necrotic cores.
- Controlled Signaling: NPs can be loaded with growth factors (e.g., VEGF, TGF-β) and engineered for sustained release to guide angiogenesis and immune cell recruitment.
- Cellular Microenvironment Engineering: Conductive NPs (e.g., graphene oxide) mimic electrical synapses in neural models, while magnetic NPs allow for spatial organization of cells post-printing.
- Biosensing and Monitoring: Fluorescent or plasmonic NPs can act as embedded sensors for real-time monitoring of metabolite (e.g., pH, O₂) changes in response to therapeutics.
Table 1: Comparison of Tumor Model Platforms for Drug Screening
| Feature | 2D Monolayer | 3D Spheroid | 3D Bioprinted Model (Standard Bioink) | 3D Bioprinted Model (NP-Bioink) |
|---|---|---|---|---|
| ECM Complexity | None | Low, homogeneous | Moderate, tunable | High, biomimetic & tunable |
| Cell-Cell/ECM Interactions | Limited | Good in core | Guided by structure | Spatially programmed & enhanced |
| Hypoxia & Gradients | None | Central hypoxia, limited gradients | Possible | Precisely induced & controlled |
| Stromal Co-culture | Difficult | Random | Layered | Spatially organized & functional |
| Throughput & Reproducibility | Very High | Moderate | Moderate-High | High (with automation) |
| Predictive Value for In Vivo | ~5% | ~25% | ~40% | >70% (estimated) |
Table 2: Commonly Used Nanoparticles in Tumor Model Bioinks
| Nanoparticle Type | Core Function | Example in Tumor Modeling |
|---|---|---|
| Silica NPs | Mechanical reinforcement, drug delivery | Mimicking desmoplastic fibrosis in pancreatic cancer |
| Cellulose Nanocrystals | Thixotropic rheology modifier, alignment | Creating anisotropic stroma for invasion studies |
| Gold NPs (AuNPs) | Photothermal, conductive, biosensing | Thermal ablation studies, neural tumor electrophysiology |
| Graphene Oxide (GO) | Conductivity, stem cell differentiation | Glioblastoma models with neural network activity |
| Magnetic NPs (Fe₃O₄) | Remote cell patterning, MRI contrast | Post-print organization of immune cells in TME |
| PLGA NPs | Sustained growth factor/drug release | Gradual release of chemoattractants for angiogenesis |
Experimental Protocols
Protocol 4.1: Formulation of a Multi-Cellular Glioblastoma (GBM) Model Bioink with VEGF-Releasing NPs
Aim: To create a bioprintable GBM model containing glioma stem cells (GSCs), astrocytes, and microglia, with sustained VEGF signaling to induce endothelial network formation.
Materials:
- Base Bioink: Hyaluronic acid (HA)-Gelatin methacryloyl (GelMA) composite.
- NPs: PLGA nanoparticles loaded with VEGF₁₆₅.
- Cells: Patient-derived GSCs (U87), human astrocytes, HMC3 microglia, HUVECs.
- Crosslinker: LAP photoinitiator.
Method:
- NP Preparation: Prepare VEGF-loaded PLGA NPs via double emulsion. Characterize size (target: 150-200 nm) and encapsulation efficiency (HPLC). Resuspend in PBS at 10 mg/mL.
- Bioink Formulation: Mix sterile HA-GelMA prepolymer (5% w/v HA, 7% w/v GelMA) with 0.3% (w/v) LAP. Add PLGA-VEGF NPs to final concentration of 0.5 mg/mL. Gently mix.
- Cell Preparation: Trypsinize and centrifuge GSCs, astrocytes, and microglia. Resuspend in bioink-NP mixture at final densities of 5x10⁶ cells/mL (GSCs), 2x10⁶ cells/mL (astrocytes), and 1x10⁶ cells/mL (microglia).
- Bioprinting: Load bioink into a temperature-controlled (20-22°C) cartridge. Using a extrusion bioprinter, print a concentric circle structure (22G nozzle, 9 mm diameter, 2 mm height) onto a petri dish. Crosslink with 405 nm light (15 mW/cm², 30 seconds per layer).
- Culture and Maturation: Transfer constructs to advanced DMEM/F-12 media with growth factors (excluding VEGF). Culture for 14 days, with media change every 2 days.
- Analysis: At day 14, assess endothelial network formation (CD31 immunofluorescence), hypoxia (pimonidazole staining), and cytokine secretion (multiplex ELISA).
Protocol 4.2: Drug Screening on a Bioprinted Desmoplastic Pancreatic Ductal Adenocarcinoma (PDAC) Model
Aim: To evaluate the efficacy and penetration of a standard chemotherapeutic (gemcitabine) versus a novel nanoparticle-drug conjugate in a stromal-rich model.
Materials:
- Model: Pre-bioprinted PDAC model using a collagen I bioink reinforced with silica NPs (2% w/v) and containing pancreatic cancer cells (PANC-1) and pancreatic stellate cells (PSCs) at a 1:1 ratio.
- Therapeutics: Gemcitabine hydrochloride (1 mM stock), Gemcitabine-loaded Chitosan NPs (Gem-CS-NPs, 10 mg/mL stock).
- Viability Assay: PrestoBlue or ATP-based 3D cell viability assay.
Method:
- Model Preparation: Bioprint 24 identical PDAC constructs (6 mm diameter, 1.5 mm height) in a 48-well plate format using Protocol 4.1 as a reference, substituting the appropriate bioink and cells. Culture for 7 days to mature.
- Treatment: Prepare treatment groups in triplicate: (A) Control (media only), (B) Free Gemcitabine (10 µM), (C) Gem-CS-NPs (equivalent to 10 µM gemcitabine), (D) Blank CS-NPs. Add 500 µL of treatment/media to each well.
- Incubation: Incubate constructs for 72 hours.
- Viability Assessment: Aspirate treatment media. Add 300 µL of PrestoBlue reagent (diluted 1:10 in PBS) to each well. Incubate for 2 hours at 37°C protected from light.
- Quantification: Transfer 100 µL of supernatant from each well to a black 96-well plate. Measure fluorescence (Ex/Em: 560/590 nm). Calculate relative viability normalized to control.
- Penetration Analysis (Parallel Experiment): Fix, section, and stain treated constructs for cleaved caspase-3. Use image analysis to quantify apoptosis depth from the construct periphery.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Bioprinting High-Fidelity Tumor Models
| Item | Function | Example Brand/Type |
|---|---|---|
| Tunable Hydrogel Precursor | Provides the foundational, printable ECM. | GelMA, Thiolated HA, PEGDA |
| Functional Nanoparticles | Enhances mechanics, adds sensing/delivery functions. | Silica NPs, PLGA-NPs (custom synthesized) |
| Photoinitiator (Visible Light) | Enables cytocompatible crosslinking of bioinks. | LAP (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate) |
| Multi-Cell Type Suspensions | Creates heterogeneous tumor-stroma interactions. | Primary patient-derived cells, immortalized lines, iPSCs |
| Bioprinter (Extrusion-based) | Enables precise spatial deposition of NP-bioinks. | Allevi 3, BIO X, custom research systems |
| Advanced Culture Media | Supports multiple co-cultured cell types long-term. | DMEM/F-12 + specific growth factor cocktails |
| Live-Cell Analysis System | Monitors viability, metabolism, and morphology over time. | Incucyte, confocal microscopy with environmental control |
Visualizations
Title: Workflow for Drug Screening Using Bioprinted NP-Bioink Tumor Models
Title: Key Signaling Pathways Recapitulated in NP-Bioink Tumor Models
Application Notes
Within the broader thesis on 3D bioprinting with nanoparticle bioinks, the development of mineral-doped inks represents a strategic advancement for regenerative orthopedics. These inks are engineered to direct stem cell fate and stimulate endogenous repair mechanisms for bone and cartilage defects. The core innovation lies in the inclusion of bioactive mineral nanoparticles—such as nano-hydroxyapatite (nHA), bioactive glass (BAG), or calcium phosphate (CaP) derivatives—within a printable hydrogel matrix (e.g., alginate, gelatin methacryloyl, hyaluronic acid). These nanoparticles provide topographical, chemical, and ionic cues that mimic the native extracellular matrix of mineralized tissues, promoting osteogenic or chondrogenic differentiation without excessive reliance on exogenous growth factors.
Recent research focuses on overcoming the historical limitations of polymer scaffolds, such as poor mechanical strength and limited bioactivity. The strategic doping of inks with specific minerals addresses these challenges: nHA enhances osteoconductivity and compressive modulus, while silicate-based BAG nanoparticles can upregulate pro-angiogenic and osteogenic genes (e.g., RUNX2, VEGF). For cartilage, sulfated mineral compounds or layered double hydroxides are being explored to stabilize the chondrogenic phenotype and inhibit hypertrophy. The printability-composability trade-off is a key research frontier, where mineral content and particle size distribution are optimized against rheological properties to ensure shape fidelity during extrusion-based printing.
Table 1: Characteristics and Performance of Common Mineral Dopants in Bioinks
| Mineral Dopant | Typical Size (nm) | Optimal Ink Concentration (w/v%) | Key Biological Effect (in vitro) | Resultant Compressive Modulus Increase (vs. base hydrogel) | Primary Target Tissue |
|---|---|---|---|---|---|
| Nano-Hydroxyapatite (nHA) | 50-200 | 1-5% | Upregulation of ALP activity (2-3 fold), Enhanced calcium deposition | 150-300% | Bone |
| Bioactive Glass (BAG, 4555) | 20-100 | 0.5-3% | Sustained release of Si⁴⁺ and Ca²⁺ ions, Angiogenic VEGF secretion | 100-250% | Bone, Osteochondral |
| Tricalcium Phosphate (β-TCP) | 100-500 | 2-7% | High osteoconductivity, supports cell adhesion and proliferation | 200-400% | Bone |
| Strontium-doped HA (SrHA) | 50-150 | 1-4% | Dual osteogenic and anti-osteoclastic activity | 120-220% | Bone (Osteoporotic) |
| Laponite (Clay Nanosilicate) | 25-50 | 1-6% | Shear-thinning for printability, induces chondrogenic gene expression (SOX9, COL2A1) | 80-600% (rheology-dependent) | Cartilage, Bone |
Table 2: In Vivo Outcomes of Implants from Mineral-Doped Inks (Rodent Critical-Sized Defect Models)
| Implant Composition (Ink Base + Dopant) | Animal Model | Defect Site | Time Point (weeks) | Key Metric vs. Control | Outcome Summary |
|---|---|---|---|---|---|
| GelMA + 3% nHA | Rat | Calvarial | 8 | Bone Volume/Tissue Volume (BV/TV): ~35% vs. ~10% (base GelMA) | Significant bridged bone formation, minimal inflammation. |
| Alginate + 2% BAG nanoparticles | Mouse | Femoral Condyle | 6 | New Bone Area: ~2.5x higher than alginate alone. | Enhanced bone regeneration with early vascular infiltration. |
| Hyaluronic Acid-MA + 4% Laponite | Rat | Trochlear Groove | 12 | Histologic Scoring (ICRS II): ~80% of normal cartilage score. | Improved cartilage matrix uniformity, reduced fibrocartilage. |
| Collagen/Pluronic + 5% β-TCP | Rabbit | Radial | 12 | Bending Strength: ~70% of native cortical bone. | Implant integrated, supporting load-bearing remodeling. |
Experimental Protocols
Protocol 1: Synthesis and Characterization of nHA-Doped Gelatin Methacryloyl (GelMA) Bioink
Objective: To prepare a sterile, printable, and osteogenic bioink containing 3% (w/v) nano-hydroxyapatite in 10% (w/v) GelMA.
Materials:
- GelMA (degree of substitution >70%)
- Nano-hydroxyapatite powder (≤200 nm)
- Photoinitiator (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, LAP)
- Dulbecco’s Phosphate Buffered Saline (DPBS)
- Sterile 50 mL conical tubes
- Centrifuge
- Sonicator (probe type)
- 3D bioprinter (extrusion-based) with UV crosslinking module
- Rheometer
Method:
- GelMA Solution Preparation: Dissolve GelMA powder in DPBS at 40°C to make a 10% (w/v) solution. Filter sterilize using a 0.22 µm syringe filter.
- nHA Suspension: Weigh 0.15 g of nHA powder per 5 mL of final ink volume. Disperse in a small volume of sterile DPBS using a probe sonicator on ice (30% amplitude, 5 min, pulsed 5s on/5s off) to create a homogeneous suspension.
- Ink Formulation: Slowly add the nHA suspension to the warm GelMA solution under gentle magnetic stirring. Add LAP photoinitiator to a final concentration of 0.25% (w/v).
- Mixing and De-aeration: Mix the composite for 2 hours at 37°C. Centrifuge the ink at 2000 x g for 5 minutes to remove air bubbles.
- Rheological Characterization: Load ink onto a parallel-plate rheometer. Perform a shear rate sweep (0.1 to 100 s⁻¹) to assess shear-thinning. Conduct a time-dependent recovery test to evaluate self-healing.
- Printability Assessment: Load ink into a sterile cartridge. Print a 10x10x2 mm grid structure (22G nozzle, 15 mm/s speed, 25 kPa pressure). Expose to 405 nm UV light (5 mW/cm², 60 s) for crosslinking. Assess filament uniformity and strand fusion.
Protocol 2: In Vitro Osteogenic Differentiation Assay with Mineral-Doped Constructs
Objective: To evaluate the osteoinductive potential of printed mineral-doped constructs using human bone marrow-derived mesenchymal stem cells (hBM-MSCs).
Materials:
- hBM-MSCs (passage 3-5)
- Osteogenic medium: α-MEM, 10% FBS, 50 µg/mL ascorbic acid, 10 mM β-glycerophosphate, 100 nM dexamethasone
- Control medium: Growth medium (α-MEM, 10% FBS)
- Alizarin Red S (ARS) staining kit
- Alkaline Phosphatase (ALP) activity assay kit
- qPCR reagents (TRIzol, cDNA synthesis kit, SYBR Green)
- Sterile 24-well plate
Method:
- Cell Seeding on Constructs: Sterilize printed 5x5x2 mm constructs under UV light for 30 min per side. Seed hBM-MSCs at a density of 1x10⁵ cells/construct in 50 µL medium. Allow cell attachment for 2 hours before adding 1 mL of medium.
- Culture Conditions: Maintain cultures for 21 days in either osteogenic or control medium, with medium changes every 3 days. Use triplicate constructs per condition.
- Alkaline Phosphatase Activity (Day 7, 14): Lyse constructs in 0.1% Triton X-100. Measure ALP activity using p-nitrophenyl phosphate as substrate. Normalize to total protein content (BCA assay). Report as nmol pNP/min/µg protein.
- Mineralization Analysis (Day 21): Fix constructs in 4% PFA for 30 min. Wash and incubate with 2% ARS solution (pH 4.2) for 30 min. For quantification, destain with 10% cetylpyridinium chloride and measure absorbance at 562 nm.
- Gene Expression (Day 14): Homogenize constructs in TRIzol. Extract RNA, synthesize cDNA, and perform qPCR for osteogenic markers (RUNX2, SP7 (Osterix), BGLAP (Osteocalcin)). Normalize to GAPDH using the 2^(-ΔΔCt) method.
Diagrams
Diagram Title: Mineral-Doped Ink Bioactivity Signaling Pathways
Diagram Title: Experimental Workflow for Mineral-Doped Implant Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Developing Mineral-Doped Bioinks
| Item | Function in Research | Example Product/Brand (for reference) |
|---|---|---|
| Methacrylated Hydrogel Precursor | Forms the primary, photocrosslinkable network of the bioink, providing cell encapsulation capability and structural integrity. | GelMA (Gelatin Methacryloyl, System Bio); Hyaluronic Acid-MA (ESI Bio) |
| Bioactive Mineral Nanoparticles | Provides osteoconductive/chondroinductive signals, enhances mechanical properties, and modulates ion release. | Nano-Hydroxyapatite (nHA, Sigma-Aldrich); Bioactive Glass 4555 (Mo-Sci Corp); Laponite XLG (BYK) |
| Photoinitiator (Visible Light) | Initiates radical polymerization of methacrylated polymers under cytocompatible light exposure. | Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP); Irgacure 2959 |
| Rheometer | Characterizes the viscoelastic properties (viscosity, shear-thinning, yield stress, recovery) critical for printability. | Discovery Hybrid Rheometer (TA Instruments); MCR Series (Anton Paar) |
| Sterile, Temperature-Controlled Bioprinter | Precisely deposits bioink in a layer-by-layer fashion under aseptic conditions, often with integrated crosslinking. | BIO X (CELLINK); 3D-Bioplotter (EnvisionTEC) |
| Mesenchymal Stem Cells (MSCs) | Primary cell model for evaluating the osteogenic/chondrogenic differentiation potential of the printed constructs. | Human Bone Marrow-derived MSCs (Lonza); AD-MSCs (ATCC) |
| Osteo/Chondro Differentiation Media Kits | Provides standardized, quality-controlled supplements for directing stem cell fate in vitro. | StemPro Osteogenesis/Chondrogenesis Differentiation Kit (Thermo Fisher) |
| Micro-Computed Tomography (μCT) Scanner | Non-destructive, 3D quantitative analysis of bone mineral density, volume, and microstructure in explanted implants. | Skyscan 1272 (Bruker); Xradia 620 Versa (Zeiss) |
Overcoming Critical Hurdles: Solutions for Printability, Cell Viability, and Sterilization Challenges
Application Notes
Within 3D bioprinting of nanoparticle bioinks, precise rheological control is paramount for fabricating structurally and biologically viable constructs. Nanoparticle incorporation (e.g., carbon nanotubes, silica, cellulose nanocrystals) into polymeric hydrogels (like alginate, gelatin methacryloyl, or hyaluronic acid) aims to enhance mechanical properties, conductivity, or bioactivity. However, this introduces significant rheology roadblocks: elevated zero-shear viscosity can hinder extrusion; inadequate shear-thinning risks cell damage; and nanoparticle aggregation leads to frequent nozzle clogging, disrupting print fidelity and viability.
This protocol details methodologies to characterize, troubleshoot, and optimize these key parameters. The core thesis is that systematic rheological profiling and nozzle dynamics analysis are prerequisites for successful bioprinting with complex nanocomposite bioinks.
Protocols
Protocol 1: Comprehensive Rheological Profiling of Nanoparticle Bioinks
Objective: To quantitatively measure zero-shear viscosity (η₀), shear-thinning exponent (n), yield stress (τ₀), and viscoelastic moduli (G', G'') for bioink formulation optimization.
Materials:
- Rheometer (cone-plate or parallel plate geometry, 25-40 mm diameter).
- Temperature-controlled Peltier plate.
- Bioink samples (e.g., 2% w/v alginate with 0.5% w/v cellulose nanocrystals).
- Solvent trap or humidification chamber to prevent drying.
Method:
- Loading: Load ~150 µL of bioink onto the lower plate. Lower the upper geometry to a measuring gap of 0.1-0.5 mm (depending on particle size). Trim excess.
- Flow Sweep: Perform a steady-state shear rate sweep from 0.01 to 1000 s⁻¹ at 20°C (or printing temperature). Record viscosity (η) versus shear rate (˙γ).
- Data Fitting: Fit the data to the Herschel-Bulkley model: τ = τ₀ + K(˙γ)ⁿ, where τ is shear stress, K is consistency index. Extract τ₀ and n. η₀ is approximated as the viscosity at the lowest measured shear rate (e.g., 0.01 s⁻¹).
- Oscillatory Sweep: Perform an amplitude sweep (stress or strain) at a fixed frequency (e.g., 1 Hz) to determine the linear viscoelastic region (LVR). Then, perform a frequency sweep (e.g., 0.1 to 100 rad/s) within the LVR to record G' (elastic/storage modulus) and G'' (viscous/loss modulus).
Data Interpretation: A viable bioink typically shows n < 1 (shear-thinning), a moderate η₀ for shape retention, and G' > G'' at low frequencies indicating solid-like behavior pre-extrusion.
Protocol 2: Nozzle Clogging Probability Assessment via Extrusion Force Monitoring
Objective: To quantify the propensity for nozzle clogging by measuring extrusion pressure over time and correlating it with nanoparticle concentration and size distribution.
Materials:
- Bioprinter with pressure-based extrusion system and in-line pressure sensor.
- Cylindrical cartridges (3 mL).
- Standardized nozzles (e.g., 22G-27G, inner diameter 0.1-0.4 mm).
- Test bioinks with varying nanoparticle loadings (0%, 0.25%, 0.5%, 1.0% w/v).
Method:
- Setup: Load 2 mL of bioink into a cartridge, attach the nozzle, and mount onto the printer. Purge a small amount to fill the nozzle tip.
- Constant-Pressure Run: Set a standard extrusion pressure (e.g., 15 kPa for alginate-based inks). Extrude continuously for 10 minutes, recording the volumetric flow rate (or mass of extruded ink) every 30 seconds.
- Constant-Flow Rate Run: Set a target flow rate (e.g., 1 mm/s filament speed). Record the required extrusion pressure over a 10-minute period.
- Analysis: Calculate the coefficient of variation (CV) of flow rate (for constant pressure) or pressure (for constant flow). A rising trend or high CV indicates instability and clogging onset. Post-experiment, inspect nozzle bore under a microscope for aggregate deposition.
Table 1: Quantitative Rheological and Clogging Data for Model Nanoparticle Bioinks
| Bioink Formulation (2% Alginate base) | Zero-Shear Viscosity, η₀ (Pa·s) | Shear-Thinning Exponent, n | Yield Stress, τ₀ (Pa) | Clogging Probability Index (CV of Pressure, %) @ 27G nozzle |
|---|---|---|---|---|
| 0% Nanoparticles (Pure) | 12.5 ± 1.8 | 0.41 ± 0.03 | 8.2 ± 0.9 | 2.1 ± 0.5 |
| + 0.25% w/v Cellulose Nanocrystals | 48.3 ± 5.2 | 0.35 ± 0.02 | 15.7 ± 1.5 | 5.8 ± 1.2 |
| + 0.5% w/v Cellulose Nanocrystals | 125.7 ± 15.6 | 0.29 ± 0.04 | 28.4 ± 3.1 | 18.4 ± 3.7* |
| + 0.5% w/v Silica Nanoparticles (50nm) | 89.4 ± 10.1 | 0.32 ± 0.03 | 21.3 ± 2.4 | 45.6 ± 8.9* |
*Indicates frequent full clogging within test duration.
Protocol 3: Mitigation of Clogging via Ultrasonic Nozzle Agitation
Objective: To apply low-power, high-frequency ultrasonic vibration to the nozzle assembly to disrupt nanoparticle aggregation proximal to the orifice.
Materials:
- Custom-modified bioprinthead with integrated piezoelectric ultrasonic transducer (e.g., 40 kHz, < 2W).
- Function generator and amplifier.
- High-speed camera for flow visualization.
Method:
- Integration: Mount the ultrasonic transducer in direct contact with the stainless-steel nozzle hub.
- Parameter Optimization: For a given bioink (e.g., 0.5% silica-alginate), extrude at constant pressure while applying ultrasonic pulses (e.g., 50 ms pulse every 500 ms) or continuous wave. Vary amplitude and frequency.
- Efficacy Measurement: Conduct the constant-flow rate test from Protocol 2, with and without ultrasonic agitation. Compare the stability of extrusion pressure.
- Viability Check: For cell-laden versions, assess post-printing cell viability (e.g., Live/Dead assay) to ensure ultrasonic energy does not cause significant damage.
Diagrams
Title: Roadblock Identification and Mitigation Workflow
Title: Nozzle Clogging Assessment Protocol
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions & Materials
| Item | Function in Rheology & Clogging Management |
|---|---|
| Herschel-Bulkley Model Fitting Software (e.g., Rheometer native software, MATLAB) | Quantifies key parameters: yield stress (τ₀), consistency index (K), and shear-thinning exponent (n) from flow sweep data. |
| In-line Pneumatic Pressure Sensor (e.g., 0-100 kPa range) | Critical for real-time monitoring of extrusion pressure during printing, enabling clog detection and feedback control. |
| Piezoelectric Ultrasonic Transducer (20-100 kHz, low power) | Integrated into printhead to deliver vibrational energy that disrupts nanoparticle networks at the nozzle orifice. |
| PEGylated or PEG-Silane Reagents | Used for surface modification of nanoparticles (e.g., silica) to introduce steric hindrance, reduce aggregation, and improve dispersion stability in bioinks. |
| Cellulose Nanocrystals (CNCs) | A common rheological modifier; increases viscosity and yield stress while providing excellent shear-thinning. Serves as a model nanoparticle for studies. |
| Humidified Environmental Enclosure | Prevents bioink drying at the nozzle tip, a significant contributor to clogging, especially for high-viscosity inks. |
| Tapered or Coated Nozzles (e.g., silicon-coated glass) | Reduce wall adhesion and shear stress gradients within the nozzle, facilitating smoother extrusion of particle-laden fluids. |
Application Notes
Within the burgeoning field of 3D bioprinting, the integration of functional nanoparticles (NPs) into bioinks presents a transformative approach for creating advanced tissue constructs. NPs can impart electrical conductivity (e.g., carbon nanotubes), provide mechanical reinforcement (e.g., nanoclay), or enable controlled drug release (e.g., polymeric NPs). However, a primary barrier to their adoption is inherent cytotoxicity, which compromises cell viability and undermines the functionality of bioprinted tissues. This document outlines practical strategies to mitigate NP toxicity, framed within the specific context of preparing and characterizing nanoparticle-laden bioinks for 3D bioprinting applications. The focus is on actionable surface modification techniques, precise dispersion protocols, and rigorous in vitro assessment methods to ensure high cell viability in final constructs.
Table 1: Summary of Nanoparticle Toxicity Mitigation Strategies & Efficacy Data
| Strategy | Mechanism of Action | Typical Materials/Approaches | Reported Improvement in Cell Viability (vs. Unmodified NPs) | Key Considerations for Bioinks |
|---|---|---|---|---|
| Surface Coating | Creates a physical barrier; reduces direct cell-membrane interaction; prevents ion leaching. | PEGylation, Polysaccharides (alginate, chitosan), Serum Proteins. | 40-60% increase (e.g., PEG-AuNPs) | Can alter bioink viscosity & crosslinking kinetics. |
| Functionalization with Biomolecules | Enhances biocompatibility; promotes specific cell interactions. | Peptides (RGD), Laminin, Collagen, Heparin. | 50-70% increase (e.g., RGD-coated SiO2 NPs) | May introduce immunogenic responses; cost. |
| Size & Shape Control | Optimizes cellular uptake pathways; reduces membrane disruption. | Synthesis of sub-50 nm spherical vs. high-aspect-ratio rods. | 30-50% variance based on size/shape | Smaller NPs may have higher inflammatory potential. |
| Charge Neutralization | Reduces electrostatic disruption of cell membranes. | Coating cationic NPs with anionic polymers (e.g., PAA). | ~35% increase for cationic particles | Near-neutral zeta potential is target. |
| Improved Dispersion | Prevents cytotoxic localized agglomeration. | Sonication, use of biocompatible surfactants (Pluronic F-127). | 25-45% increase | Surfactants must be cytocompatible; sonication can damage bioink polymers. |
Protocol 1: Synthesis and Characterization of PEGylated Gold Nanoparticles (AuNPs) for Conductive Bioinks
Objective: To synthesize cytocompatible, PEG-coated AuNPs for integration into gelatin methacryloyl (GelMA) bioinks to enhance electrical conductivity without compromising viability.
Materials:
- Chloroauric acid (HAuCl4)
- Sodium citrate dihydrate
- Methoxy-PEG-Thiol (MW 5000 Da)
- Ultrapure water
- GelMA, Photoinitiator (LAP)
Procedure:
- Synthesis of Citrate-capped AuNPs: Heat 100 mL of 1 mM HAuCl4 to boiling under reflux. Rapidly add 10 mL of 38.8 mM sodium citrate with vigorous stirring. Continue heating until solution color changes to deep red (~10 min). Cool to room temperature.
- PEGylation: Add methoxy-PEG-Thiol to the AuNP solution at a 10,000:1 PEG:NP molar ratio. Stir gently for 24 hours at room temperature.
- Purification: Centrifuge the PEG-AuNP solution at 14,000 x g for 30 min. Discard supernatant and resuspend the soft pellet in PBS. Repeat twice.
- Characterization: Use UV-Vis spectroscopy (Surface Plasmon Resonance peak ~520 nm), Dynamic Light Scattering (for hydrodynamic diameter and zeta potential), and TEM (for core size and morphology).
- Bioink Formulation: Mix purified PEG-AuNPs into 5% (w/v) GelMA solution at desired concentration (e.g., 0-50 µg/mL). Add 0.25% (w/v) LAP photoinitiator. Homogenize by gentle vortexing.
- Sterilization: Pass the final bioink through a 0.22 µm syringe filter (if viscosity permits) or expose to UV light for 20 minutes prior to cell mixing.
Protocol 2: Assessment of Cell Viability in 3D Bioprinted NP-Bioink Constructs
Objective: To quantitatively assess the short- and long-term cytotoxicity of nanoparticle bioinks in a 3D bioprinted environment.
Materials:
- NIH/3T3 fibroblasts or human mesenchymal stem cells (hMSCs)
- NP-laden bioink (from Protocol 1)
- Live/Dead Viability/Cytotoxicity Kit (Calcein AM/EthD-1)
- Cell culture medium, PBS
- Confocal microscope
- 3D bioprinter (e.g., extrusion-based)
Procedure:
- Cell-Laden Bioink Preparation: Trypsinize and centrifuge cells. Resuspend cell pellet in the sterile NP-bioink to a final density of 5 x 10^6 cells/mL. Keep on ice.
- 3D Bioprinting: Load bioink into a sterile cartridge. Print a standardized grid structure (e.g., 10x10x2 mm) into a culture dish. Crosslink immediately (e.g., 405 nm light for 60 sec for GelMA).
- Culture: Add complete medium and incubate at 37°C, 5% CO2. Change medium every 2-3 days.
- Live/Dead Staining (Day 1, 3, 7): a. Prepare staining solution: 2 µM Calcein AM and 4 µM Ethidium homodimer-1 in PBS. b. Wash constructs with PBS. c. Incubate constructs in staining solution for 45 minutes at 37°C, protected from light. d. Image using a confocal microscope (ex/em ~488/515 nm for Calcein, ~561/635 nm for EthD-1). Take z-stacks from at least 3 random locations per construct.
- Quantitative Analysis: Use image analysis software (e.g., ImageJ/Fiji) to count live (green) and dead (red) cells. Calculate percentage viability: [Live cells / (Live+Dead cells)] * 100%.
Signaling Pathways in Nanoparticle-Induced Cytotoxicity & Mitigation
Pathways of NP Toxicity and Mitigation
Experimental Workflow for NP-Bioink Development & Testing
NP-Bioink Development Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function in NP-Bioink Research | Example Product/Catalog |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel base for bioinks; provides cell-adhesive motifs. | GelMA, Sigma-Aldrich (MASTERGEL) or synthesizable. |
| Polyethylene Glycol-Thiol (PEG-SH) | Gold-standard polymer for creating stealth coatings on NPs to reduce opsonization and toxicity. | Methoxy-PEG-Thiol, 5kDa, BroadPharm. |
| LAP Photoinitiator | Biocompatible photoinitiator for visible light (405 nm) crosslinking of bioinks like GelMA. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP). |
| Pluronic F-127 | Non-ionic, biocompatible surfactant used to improve NP dispersion in hydrophobic polymers. | Poloxamer 407, Sigma-Aldrich P2443. |
| Live/Dead Viability/Cytotoxicity Kit | Two-color fluorescence assay for simultaneous determination of live (calcein-AM) and dead (EthD-1) cells in 3D constructs. | Thermo Fisher Scientific L3224. |
| AlamarBlue/Resazurin | Cell-permeant redox indicator used for quantitative, non-destructive measurement of metabolic activity over time. | Thermo Fisher Scientific DAL1025. |
| Zetasizer Nano System | Instrument for measuring NP hydrodynamic size, size distribution (DLS), and zeta potential (surface charge). | Malvern Panalytical Zetasizer Nano ZS. |
Within the emerging field of 3D bioprinting with nanoparticle-laden bioinks, achieving and maintaining a uniform dispersion of nanoparticles is paramount. These composite bioinks integrate functional nanoparticles (e.g., drug carriers, imaging contrast agents, conductive nanomaterials, or reinforcing agents) within a biocompatible hydrogel matrix. Aggregation of nanoparticles during bioink formulation, storage, or the printing process itself leads to nozzle clogging, heterogeneous print fidelity, and critically, non-uniform biological or functional performance in the final bioprinted construct. This application note details protocols and techniques to ensure nanoparticle colloidal stability, enabling reproducible fabrication of advanced, functional tissue constructs.
Core Stabilization Mechanisms and Quantitative Data
Nanoparticle dispersion stability is governed by interparticle forces. The primary strategies to prevent aggregation work by introducing repulsive forces to counteract van der Waals attraction.
Table 1: Core Stabilization Mechanisms for Nanoparticles in Aqueous Bioinks
| Mechanism | Agent Type | How it Works | Optimal For | Key Parameter (Typical Range) | ||
|---|---|---|---|---|---|---|
| Electrostatic | Ionic surfactants (SDS), citrate, charged polymers (PSS). | Creates surface charge, generating repulsive electrostatic double-layer. | Inorganic NPs (Au, SiO₂, Fe₃O₄) in simple buffers. | Zeta Potential: > | ±30 | mV for good stability. |
| Steric | Non-ionic surfactants (Pluronic F-68, Tween 80), polymers (PEG, PVA). | Physically obstructs particle approach via adsorbed polymer chains. | Hydrophobic NPs, long-term storage, physiological ionic strength. | Polymer MW: 2-10 kDa; Grafting Density: > 0.5 chains/nm². | ||
| Electrosteric | Charged polymers (chitosan, polylysine), PEGylated lipids. | Combines electrostatic and steric repulsion. | Highest stability for bioinks; withstands ionic bio-fluids. | Zeta Potential: > | ±20 | mV + dense polymer layer. |
Table 2: Impact of Dispersion Quality on Bioink Printability
| Dispersion State | Average Hydrodynamic Diameter (DLS) | Polydispersity Index (PDI) | Bioink Viscosity (at 10 s⁻¹) | Printing Outcome |
|---|---|---|---|---|
| Well-dispersed | Close to primary particle size (e.g., 50 nm). | < 0.1 | Consistent, predictable. | Smooth extrusion, uniform struts, high resolution. |
| Moderately aggregated | 2-5x primary size (e.g., 100-250 nm). | 0.1 - 0.25 | Slightly elevated, shear-thinning. | Minor inconsistencies, potential for clogging. |
| Heavily aggregated | > 10x primary size (e.g., >500 nm). | > 0.3 | Unpredictable, can gel or separate. | Nozzle clogging, failed prints, heterogeneous structure. |
Detailed Experimental Protocols
Protocol 3.1: Formulating a Sterically-Stabilized PLGA Nanoparticle Bioink
Objective: Incorporate drug-loaded Poly(lactic-co-glycolic acid) (PLGA) nanoparticles into a gelatin-methacryloyl (GelMA) bioink with high dispersion fidelity.
Materials: See "The Scientist's Toolkit" below. Procedure:
- NP Synthesis & Stabilization: Prepare PLGA NPs via single emulsion. Add 200 mg PLGA and hydrophobic drug (e.g., Paclitaxel, 5 mg) in 4 mL dichloromethane. Emulsify in 20 mL of 2% (w/v) aqueous poly(vinyl alcohol) (PVA, MW 30-70 kDa) using a probe sonicator (70% amplitude, 60 s on ice). Stir overnight to evaporate solvent. Centrifuge at 15,000 x g for 20 min and resuspend pellet in 10 mL of 1% (w/v) Pluronic F-127 solution. Sonicate (bath, 5 min) and filter (0.8 µm).
- Characterization: Measure hydrodynamic diameter and PDI via Dynamic Light Scattering (DLS). Confirm stability by monitoring size over 72h at 4°C.
- Bioink Integration: Mix the purified NP suspension with 10% (w/v) GelMA prepolymer solution at a 1:9 volume ratio (NP suspension:GelMA). Gently vortex for 30 s.
- Rheological Assessment: Perform a shear rate sweep (0.1 to 100 s⁻¹) to confirm viscosity profile is unchanged versus pure GelMA, indicating no macroscopic aggregation.
- Printability Test: Load bioink into a pneumatic bioprinter (22G nozzle, 20°C). Extrude a 15 x 15 mm grid structure. Assess strand continuity and uniformity under microscope.
Protocol 3.2: Assessing Dispersion Fidelity Post-Printing via Microscopy
Objective: Quantify nanoparticle aggregation within a bioprinted hydrogel construct.
Procedure:
- Print and Crosslink: Bioprint a thin, single-layer lattice using the formulated bioink. Crosslink with UV light (365 nm, 5 mW/cm², 60 s).
- Sectioning: Cryo-section the printed construct to 20 µm thickness.
- Imaging: Use confocal microscopy (if NPs are fluorescent) or dark-field microscopy (for metallic NPs like gold) to image multiple random fields within the section.
- Image Analysis (Using FIJI/ImageJ):
- Convert image to 8-bit and apply a threshold to highlight NP clusters.
- Run "Analyze Particles" function to count clusters and measure their cross-sectional area.
- Calculate Aggregation Index = (Area of all clusters / Total image area) x 100%. Compare this index between different stabilization methods.
Diagrams
Nanoparticle Stabilization Pathways for Bioinks
Bioink Formulation and Assessment Workflow
The Scientist's Toolkit: Key Reagents & Materials
| Item | Function in Preventing Aggregation | Example Product/Chemical |
|---|---|---|
| Pluronic F-127 / F-68 | Non-ionic triblock surfactant. Provides steric hindrance, reduces interfacial tension during NP formation, biocompatible. | Sigma-Aldrich P2443 / P1300 |
| Poly(vinyl alcohol) (PVA) | Steric stabilizer. Commonly used as an emulsion stabilizer in NP synthesis, forms protective colloidal layer. | MW 30-70 kDa, 87-89% hydrolyzed |
| Polyethylene glycol (PEG) thiol/amine | For "PEGylation." Creates a hydrophilic, steric barrier, dramatically increases circulation time and stability. | Methoxy-PEG-SH, 5 kDa |
| Citrate | Electrostatic stabilizer for metallic NPs. Provides negative surface charge via adsorption/reduction. | Trisodium citrate dihydrate |
| Dynamic Light Scattering (DLS) Instrument | Measures hydrodynamic diameter and Polydispersity Index (PDI), the gold standard for assessing aggregation state. | Malvern Zetasizer Nano |
| Zeta Potential Analyzer | Measures surface charge. Predicts electrostatic stability; > |±30| mV indicates high stability. | Integrated in DLS instruments |
| Bath Sonicator | Provides gentle, uniform energy to resuspend NP pellets and break up loose aggregates in solution. | Branson 2800 |
| Syringe Filters (0.22, 0.45 µm) | Removes large aggregates and contaminants from NP suspensions or bioinks prior to printing. | PVDF or cellulose acetate membrane |
| Gelatin-Methacryloyl (GelMA) | A widely used photopolymerizable hydrogel bioink. Serves as the dispersing matrix for NPs. | Advanced BioMatrix 900633 |
Within the broader thesis on developing advanced 3D bioprinting platforms for tissue engineering and drug screening, the formulation of sterile, functional nanoparticle bioinks is a critical bottleneck. Nanoparticles (e.g., polymeric, liposomal, ceramic) are integrated into bioinks to enhance mechanical properties, control drug release, or impart conductivity. However, standard sterilization methods can induce aggregation, degrade polymers, or inactivate biological cargo. These Application Notes compare three compatible sterilization techniques—UV irradiation, filtration, and antibiotic addition—detailing protocols, efficacy data, and impact on nanoparticle and cell viability.
Comparative Efficacy & Impact Data
Table 1: Sterilization Method Efficacy and Nanoparticle Bioink Compatibility
| Method | Typical Log Reduction | Key Impact on Nanoparticle Bioinks | Recommended Max Exposure/Concentration |
|---|---|---|---|
| UV-C Irradiation | 3-4 log (bacteria), variable (spores) | Potential polymer cross-linking/ degradation; free radical generation. | 15-30 mJ/cm² (254 nm) |
| Sterile Filtration | >7 log (bacteria) | Loss of particles > pore size; shear stress may deform soft nanoparticles. | 0.22 µm PES membrane |
| Antibiotic Cocktail | Bacteriostatic/Bactericidal | Minimal direct physical impact; risk of masking low-level contamination. | 1% Pen-Strep or equivalent |
Table 2: Post-Sterilization Bioink Properties (Example: PLGA Nanoparticle-Alginate Bioink)
| Sterilization Method | Avg. Particle Size (nm) Δ | PDI Δ | Encapsulant (BSA) Retention (%) | Post-print Cell Viability (%)* |
|---|---|---|---|---|
| Unsterilized Control | 215 ± 12 | 0.08 | 100 (Ref) | 92 ± 3 |
| UV (30 mJ/cm²) | 223 ± 15 | 0.12 | 95 ± 4 | 88 ± 5 |
| Filtration (0.22 µm) | 205 ± 10 | 0.07 | 98 ± 2 | 91 ± 4 |
| Antibiotics (1%) | 216 ± 13 | 0.08 | 99 ± 1 | 90 ± 3 |
Viability measured at 24h post-bioprinting with NIH/3T3 fibroblasts. *Indicates potential loss of larger aggregates.
Detailed Experimental Protocols
Protocol 1: UV-C Sterilization of Nanoparticle Bioink Precursor Objective: To sterilize a nanoparticle suspension prior to mixing with thermosensitive bioink polymers.
- Preparation: In a laminar flow hood, aliquot 5 mL of nanoparticle suspension (e.g., PEG-PLGA NPs in PBS) into a sterile, UV-transparent quartz cuvette or shallow Petri dish. Leave lid open.
- UV Exposure: Place sample under a calibrated UV-C germicidal lamp (254 nm). Use a radiometer to confirm dose. Gently agitate every 5 minutes to ensure uniform exposure.
- Dosage: Apply a total fluence of 25 mJ/cm². Calculate exposure time: Time (s) = Dose (J/m²) / Irradiance (W/m²). (e.g., 0.25 W/m² for 100 seconds).
- Post-Processing: Aseptically combine the sterilized nanoparticle suspension with filter-sterilized polymer solution (e.g., gelatin methacryloyl) to form the final bioink.
Protocol 2: Aseptic Filtration of Composite Bioink Objective: To sterilize a low-viscosity, final composite bioink by membrane filtration.
- Membrane Selection: Pre-wet a 0.22 µm pore size, low protein-binding PES syringe filter with 5 mL of sterile water or buffer.
- Bioink Preparation: Formulate bioink ensuring nanoparticles are well-dispersed. Pre-filter through a 5 µm pore size filter to remove large aggregates and prevent clogging.
- Filtration: Using a sterile luer-lock syringe, gently pass the pre-filtered bioink through the 0.22 µm PES filter into a sterile collection tube. Do not exceed manufacturer-recommended pressure.
- Validation: Assess post-filtration particle size and distribution via dynamic light scattering (DLS) to confirm no significant fraction loss or size alteration.
Protocol 3: Incorporation of Antibiotic/Antimycotic Agents Objective: To supplement bioink with antimicrobials as a secondary sterilization barrier.
- Stock Solution: Use commercial 100X antibiotic-antimycotic solution (e.g., containing penicillin, streptomycin, and amphotericin B).
- Aseptic Addition: Under laminar flow, add the antibiotic solution to the sterile bioink (prepared via filtration or UV) to achieve a 1X working concentration. Final bioink concentration: 100 U/mL penicillin, 100 µg/mL streptomycin.
- Mixing: Gently vortex or pipette mix to ensure homogeneous distribution without introducing bubbles.
- Note: This method is not a substitute for primary sterilization. Use in conjunction with other methods for long-term culture.
Visualizations
Sterilization Workflow for Bioink
UV Sterilization: Mechanisms & Risks
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Bioink Sterilization Studies
| Item | Function & Rationale |
|---|---|
| Polyethylene Glycol-b-Poly(Lactic-co-Glycolic Acid) (PEG-PLGA) | A common copolymer for forming "stealth" nanoparticles with controlled release; assesses sterilization impact on biodegradable polymers. |
| 0.22 µm PES Syringe Filter (Low Protein Binding) | Standard for sterile filtration; PES minimizes nanoparticle adhesion compared to cellulose acetate. |
| UV-C Crosslinker (254 nm) with Radiometer | Provides controlled, quantifiable UV dosage for reproducible sterilization studies. |
| Dynamic Light Scattering (DLS) Instrument | Critical for measuring nanoparticle hydrodynamic diameter (size) and polydispersity index (PDI) pre- and post-sterilization. |
| Tryptic Soy Broth (TSB) & Agar Plates | For sterility validation via microbial growth turbidity assays and colony formation. |
| AlamarBlue or MTT Assay Kit | To quantify the impact of sterilized bioinks on encapsulated or bioprinted cell viability. |
| Antibiotic-Antimycotic (100X) Solution | Broad-spectrum prophylactic against bacterial and fungal contamination in final bioink. |
| Low-Adhesion Sterile Centrifuge Tubes | For bioink storage; prevents nanoparticle and polymer loss on container walls. |
Within the broader thesis on 3D bioprinting with nanoparticle (NP)-laden bioinks, this application note addresses the critical interdependence of three core parameters: bioink concentration, crosslinking strategy, and printing speed. Nanoparticles, such as cellulose nanocrystals (CNCs), silica nanoparticles, or extracellular vesicle-loaded carriers, modify bioink rheology, gelation kinetics, and post-printing cell behavior. Isolating and optimizing these parameters is essential for achieving structurally stable, biologically functional constructs. This document provides a standardized protocol for systematic parameter screening.
The printability window is defined by the delicate balance between bioink viscosity (governed by polymer and NP concentration), crosslinking density, and shear forces applied during dispensing (governed by speed). The following tables summarize target ranges and outcomes based on recent literature.
Table 1: Optimization Matrix for Alginate-Gelatin-Nanoparticle Bioinks
| Parameter | Low Range | Optimal Target Range | High Range | Primary Outcome Measure |
|---|---|---|---|---|
| Total Polymer Conc. | 2-3% w/v | 4-6% w/v | >7% w/v | Shape Fidelity (Filament Collapse) |
| NP Loading (e.g., CNC) | 0-1% w/v | 2-4% w/v | >5% w/v | Storage Modulus (G'), Shear-Thinning |
| Ionic Crosslink (CaCl₂) | 50-100 mM | 150-300 mM | >500 mM | Gelation Time, Compression Modulus |
| Print Speed | 1-5 mm/s | 6-15 mm/s | >20 mm/s | Filament Uniformity, Cell Viability |
Table 2: Printability Assessment Scoring (Schwartzman Scale)
| Score | Filament Morphology | Pore Integrity | Dimensional Accuracy |
|---|---|---|---|
| 1 (Poor) | Continuous extrusion failed | No pore definition | >30% deviation from design |
| 2 (Fair) | Irregular, bulging/breaking | Pores partially collapsed | 15-30% deviation |
| 3 (Good) | Consistent, slight spreading | Pores visible, some merging | 5-15% deviation |
| 4 (Excellent) | Sharp, smooth filaments | Square pores, minimal spreading | <5% deviation |
Experimental Protocols
Protocol 1: Rheological Characterization for Parameter Bounding
Objective: Determine the shear-thinning profile and gelation kinetics to establish printable concentration and crosslinking ranges. Materials: Rheometer (cone-plate or parallel plate), NP-bioink samples, crosslinking agent (e.g., CaCl₂ solution). Method:
- Shear-Thinning Test: Load bioink. Perform a shear rate sweep from 0.1 to 100 s⁻¹ at 20°C. Record apparent viscosity. Optimal bioinks show >80% viscosity drop.
- Amplitude Sweep: At a fixed frequency (1 Hz), strain from 0.1% to 100%. Determine the linear viscoelastic region (LVR) and yield stress.
- Gelation Kinetics: For UV or ionic crosslinking, initiate gelation on the plate and monitor storage (G') and loss (G'') modulus over time at 1 Hz. Report time-to-gel (G' > G'').
Protocol 2: Grid-Based Printability Assay
Objective: Empirically test combinations of printing speed and pressure/concentration. Materials: Extrusion bioprinter, sterile printing cartridges, 24-well plate. Method:
- Design: Create a 10x10mm single-layer grid in slicing software.
- Parameter Array: Prepare bioinks with 3 concentrations (e.g., 4, 5, 6%). For each, set 4 pressures and 4 speeds (e.g., 5, 10, 15, 20 mm/s) in a crossed array.
- Print & Image: Print grids into wells. Capture overhead images immediately.
- Analyze: Use ImageJ to measure filament diameter consistency and pore area fidelity. Assign a Printability Score (Table 2).
Protocol 3: Post-Printing Construct Integrity & Cell Viability Assessment
Objective: Evaluate the long-term outcome of optimized parameters. Materials: Crosslinked constructs, live/dead assay kit, confocal microscope, mechanical tester. Method:
- Culture: Maintain printed constructs in culture for 1, 7, and 14 days.
- Viability: At each timepoint, incubate with Calcein-AM (2µM) and EthD-1 (4µM) for 45 min. Image via confocal microscopy. Calculate viability as (live cells / total cells) * 100.
- Integrity: Perform unconfined compression test to determine elastic modulus at day 1. Report modulus relative to acellular controls.
Visualizations
Title: Parameter Optimization Workflow
Title: From Print Parameters to Cell Fate
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in NP-Bioink Optimization |
|---|---|
| Alginate (High G-Content) | Provides primary polymer backbone for ionic (Ca²⁺) crosslinking, enabling rapid gelation. |
| Gelatin or GelMA | Adds cell-adhesive RGD motifs and enables thermal or photochemical crosslinking. |
| Cellulose Nanocrystals (CNCs) | Nanoparticle additive that enhances shear-thinning, improves print fidelity, and reinforces matrix. |
| Photoinitiator (LAP) | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate for UV crosslinking of GelMA; offers cytocompatibility. |
| Calcium Chloride (CaCl₂) | Ionic crosslinker for alginate; concentration tunes gelation speed and final stiffness. |
| Rheology Modifier (Hyaluronic Acid) | Can be used to further modulate zero-shear viscosity and water retention. |
| Fluorescent Nanobeads | Tracers for visualizing nanoparticle distribution and dispersion within printed filaments. |
| Live/Dead Viability Kit | Standard assay (Calcein-AM/EthD-1) for quantifying post-printing cell survival over time. |
Benchmarking Performance: Analytical Validation and Comparative Analysis of Nanoparticle Bioinks
Within the broader thesis on "Advancing 3D Bioprinting with Nanoparticle-Enhanced Bioinks for Controlled Drug Delivery," validating the engineered constructs is paramount. This document provides detailed application notes and protocols for essential assays to analyze the structural integrity, mechanical properties, and degradation kinetics of 3D bioprinted scaffolds. These analyses are critical for correlating scaffold performance with in vitro and eventual in vivo outcomes in drug release and tissue regeneration.
Structural and Morphological Analysis
Application Note: Characterization of pore architecture, strut morphology, and nanoparticle distribution within the bioink matrix directly influences nutrient diffusion, cell migration, and drug release profiles.
Protocol 1.1: Scanning Electron Microscopy (SEM) for Microarchitecture
- Objective: To visualize surface and internal microstructure, pore interconnectivity, and nanoparticle integration.
- Materials: Critical point dryer, sputter coater, high-resolution SEM.
- Methodology:
- Fixation: Immerse printed constructs (5x5x2 mm) in 4% paraformaldehyde for 2 hours at 4°C.
- Dehydration: Subject samples to an ethanol series (50%, 70%, 90%, 100% x3), 15 minutes per step.
- Drying: Process samples using a critical point dryer to prevent structural collapse.
- Mounting & Coating: Mount samples on aluminum stubs with conductive carbon tape and sputter-coat with a 10 nm gold-palladium layer.
- Imaging: Image at accelerating voltages of 5-15 kV. For internal structure, freeze-fracture samples in liquid nitrogen prior to dehydration.
Protocol 1.2: Micro-Computed Tomography (μCT) for 3D Porosity Analysis
- Objective: To non-destructively quantify porosity, pore size distribution, and wall thickness.
- Methodology:
- Calibration: Calibrate the μCT system using a phantom with known density.
- Scanning: Mount the hydrated construct in a radiolucent holder. Scan with an isotropic voxel size of ≤10 μm, voltage 50 kV, current 200 μA.
- Reconstruction & Analysis: Reconstruct 3D models using filtered back-projection. Apply a global threshold to binarize images. Use built-in software to calculate porosity (%) and pore size (μm).
Quantitative Data from Structural Assays:
| Assay | Measured Parameter | Typical Target for Drug Delivery Scaffolds | Instrument |
|---|---|---|---|
| SEM Analysis | Average Pore Size (μm) | 100 - 300 μm | Scanning Electron Microscope |
| μCT Analysis | Total Porosity (%) | 70 - 90% | Micro-CT Scanner |
| μCT Analysis | Pore Interconnectivity (%) | > 95% | Micro-CT Scanner |
| SEM/EDS | Nanoparticle Distribution | Homogeneous dispersion | SEM with EDS Detector |
Mechanical Characterization
Application Note: Mechanical properties dictate scaffold handling, surgical suturability, and in vivo performance under physiological loads. Nanoparticles (e.g., cellulose nanocrystals, silica) are often incorporated to modulate these properties.
Protocol 2.1: Uniaxial Compression Testing for Elastic Modulus
- Objective: To determine the compressive modulus and strength of cylindrical bioprinted constructs.
- Materials: Universal mechanical tester, 500 N load cell, phosphate-buffered saline (PBS) at 37°C.
- Methodology:
- Sample Prep: Print cylindrical constructs (Ø8mm x 4mm height, n=5). Incubate in PBS at 37°C for 24 hours prior to testing.
- Testing: Place the hydrated sample between parallel plates. Apply a pre-load of 0.01 N. Compress at a constant strain rate of 1 mm/min until 60% strain is reached.
- Analysis: Calculate the compressive modulus (MPa) as the slope of the linear (elastic) region (typically 10-20% strain) on the stress-strain curve.
Quantitative Mechanical Data:
| Bioink Formulation | Compressive Modulus (kPa) | Yield Strength (kPa) | Key Finding |
|---|---|---|---|
| Alginate-Gelatin (Baseline) | 45.2 ± 5.1 | 32.1 ± 3.8 | Baseline hydrogel |
| Baseline + 1.5% w/v Laponite NP | 118.7 ± 12.3 | 85.4 ± 9.1 | ~2.6x increase in modulus |
| Baseline + 2% w/v Cellulose NC | 156.4 ± 18.9 | 101.5 ± 11.7 | ~3.5x increase in modulus |
Degradation and Drug Release Kinetics
Application Note: Understanding scaffold degradation and its correlation with controlled drug release is the core of the thesis. Assays must simulate physiological conditions.
Protocol 3.1: In Vitro Mass Loss Degradation Study
- Objective: To monitor mass loss over time in simulated physiological conditions.
- Materials: Lyophilizer, analytical balance, degradation buffer (PBS with 10 U/mL lysozyme, pH 7.4, 37°C).
- Methodology:
- Dry Weight (Initial): Lyophilize constructs (n=5) to constant mass. Record dry weight (Wᵢ).
- Incubation: Immerse samples in 5 mL degradation buffer under gentle agitation (60 rpm) at 37°C.
- Time Points: At predetermined intervals (e.g., days 1, 3, 7, 14, 21), remove samples, rinse with DI water, lyophilize, and record dry weight (Wₜ).
- Calculation: Calculate mass remaining (%) = (Wₜ / Wᵢ) * 100.
Protocol 3.2: Cumulative Drug Release Profiling
- Objective: To quantify the release kinetics of a model drug (e.g., bovine serum albumin - BSA) from nanoparticle-loaded bioinks.
- Methodology:
- Loading: Incorporate 0.1 mg/mL fluorescein-isothiocyanate-labeled BSA (FITC-BSA) into the bioink prior to printing.
- Release Study: Immerse printed constructs in 5 mL PBS (pH 7.4) at 37°C under gentle agitation.
- Sampling: At each time point, collect 1 mL of release medium and replace with fresh pre-warmed PBS.
- Quantification: Measure FITC-BSA concentration via fluorescence microplate reader (Ex/Em: 495/519 nm) against a standard curve.
Degradation & Release Data:
| Time (Days) | Mass Remaining (%) | Cumulative BSA Release (%) |
|---|---|---|
| 1 | 98.5 ± 1.2 | 15.3 ± 2.1 |
| 7 | 85.4 ± 3.8 | 48.7 ± 3.5 |
| 14 | 62.1 ± 5.6 | 82.9 ± 4.2 |
| 21 | 40.8 ± 6.3 | 96.5 ± 1.8 |
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Function in Validation Assays |
|---|---|
| Critical Point Dryer | Preserves delicate 3D hydrogel microstructure by replacing solvent with CO₂ for SEM. |
| Lysozyme (in PBS) | Enzyme added to degradation buffer to simulate enzymatic hydrolysis in the body. |
| FITC-Bovine Serum Albumin | A stable, fluorescent model protein drug used to track release kinetics from scaffolds. |
| Laponite XLG Nanoparticles | Synthetic silicate clay nanoparticles used as rheological modifiers and mechanical reinforcers in bioinks. |
| Cellulose Nanocrystals | Rod-like nanoparticles derived from biomass used to enhance mechanical strength and control degradation. |
Visualization: Experimental Workflow & Signaling Impact
Diagram 1: Integrated Validation Workflow for 3D Bioprinted Constructs (75 chars)
Diagram 2: NP Impact on Scaffold Properties & Cellular Signaling (78 chars)
The integration of functional nanoparticles (e.g., carbon nanotubes for conductivity, bioactive glass for mineralization, or drug-loaded polymeric NPs) into hydrogel bioinks presents a transformative approach in 3D bioprinting. These nanocomposite bioinks aim to direct cell fate and enhance tissue maturation. Rigorous biological validation across in vitro and in vivo models is paramount to confirm that the printed constructs support physiologically relevant cell behavior and functional tissue formation. This document outlines standardized protocols and analytical methods for this critical validation phase.
Application Note: Assessing Cell Viability and Proliferation in 3D Bioprinted Constructs
Objective: To quantify the impact of nanoparticle bioinks on initial cell survival and subsequent proliferative capacity within 3D printed structures.
Key Assays:
- Live/Dead Staining (Day 1-3): Assesses immediate biocompatibility and cytotoxicity of the bioink and printing process.
- Metabolic Activity (AlamarBlue/CCK-8) (Time Course): Tracks proliferative trends.
- DNA Quantification (PicoGreen) (Endpoint): Provides direct measure of total cell number.
Protocol 1.1: Live/Dead Viability/Cytotoxicity Assay for 3D Constructs
- Preparation: Prepare constructs in 24-well plates. Prepare working solution by adding 2 µL of ethidium homodimer-1 (EthD-1) and 0.5 µL of calcein AM to 1 mL of PBS or culture medium.
- Staining: Aspirate culture medium from the well. Add 300-500 µL of working solution to completely cover the construct. Incubate for 30-45 minutes at room temperature, protected from light.
- Imaging: Rinse gently with PBS. Image immediately using a confocal microscope. Use filters for calcein (ex/em ~495/~515 nm, green/live) and EthD-1 (ex/em ~495/~635 nm, red/dead).
- Analysis: Calculate viability percentage: (Number of live cells / Total number of cells) × 100 from multiple z-stack images.
Protocol 1.2: Quantification of Metabolic Activity using AlamarBlue
- Reagent Prep: Dilute AlamarBlue (resazurin) reagent 1:10 in complete culture medium (e.g., 100 µL reagent + 900 µL medium per well of a 24-well plate).
- Incubation: Aspirate culture medium from constructs. Add the diluted reagent solution. Incubate for 2-4 hours at 37°C, protected from light.
- Measurement: Transfer 100 µL of the reacted solution from each well to a 96-well plate in triplicate. Measure fluorescence at excitation 560 nm / emission 590 nm using a plate reader.
- Analysis: Subtract background fluorescence from blank (reagent + medium, no cells). Normalize data to a control group (e.g., cells in standard bioink without NPs).
Table 1: Typical Proliferation Data from a 3D Bioprinted Osteogenic Construct with Silica Nanoparticles
| Time Point (Days) | Live/Dead Viability (%) | Metabolic Activity (RFU, Relative to Day 1) | DNA Content (ng/construct) |
|---|---|---|---|
| Day 1 | 92.5 ± 3.1 | 1.00 ± 0.08 | 150 ± 12 |
| Day 3 | 95.2 ± 2.4 | 1.35 ± 0.11 | 210 ± 18 |
| Day 7 | 93.8 ± 4.0 | 1.89 ± 0.14 | 380 ± 25 |
| Day 14 | 90.1 ± 5.2 | 2.45 ± 0.21 | 650 ± 45 |
RFU: Relative Fluorescence Units. Data are mean ± SD, n=6.
Application Note: Evaluating Lineage-Specific Differentiation
Objective: To verify that the biochemical and biophysical cues from the nanoparticle bioink drive stem cells (e.g., MSCs) toward the intended lineage (e.g., osteogenic, chondrogenic, neuronal).
Key Methods:
- Gene Expression (qRT-PCR): For early and mid-term markers.
- Protein Expression (Immunohistochemistry - IHC/Immunofluorescence - IF): For mid-to-late term markers and spatial distribution.
- Biochemical Assays (Endpoint): Quantify functional matrix deposition.
Protocol 2.1: RNA Isolation and qRT-PCR from 3D Bioprinted Constructs
- Homogenization: Transfer construct to a microfuge tube. Add 500 µL of TRIzol Reagent. Homogenize using a micro-pestle or tissue grinder on ice. Incubate 5 min.
- Phase Separation: Add 100 µL chloroform. Shake vigorously, incubate 3 min. Centrifuge at 12,000 × g, 15 min, 4°C.
- RNA Precipitation: Transfer aqueous phase to a new tube. Add 250 µL isopropanol. Incubate 10 min, centrifuge at 12,000 × g, 10 min, 4°C.
- Wash & Resuspend: Wash pellet with 75% ethanol. Air dry, resuspend in 20-30 µL RNase-free water.
- cDNA Synthesis & qPCR: Use 500 ng-1 µg RNA for reverse transcription. Perform qPCR using SYBR Green master mix and primer sets for target genes (e.g., RUNX2, COL1A1, SOX9, ACAN). Normalize to housekeeping genes (GAPDH, HPRT1). Analyze via ∆∆Ct method.
Protocol 2.2: Immunofluorescence Staining of Cryosectioned Constructs
- Sectioning: Fix constructs in 4% PFA for 24 hours. Cryoprotect in 30% sucrose overnight. Embed in OCT, section at 10-20 µm thickness.
- Staining: Permeabilize with 0.1% Triton X-100. Block with 5% normal serum. Incubate with primary antibody (e.g., anti-Osteocalcin, anti-Collagen II) overnight at 4°C.
- Visualization: Incubate with fluorophore-conjugated secondary antibody. Counterstain nuclei with DAPI. Mount and image with confocal microscopy.
Table 2: Example qRT-PCR Fold Change for MSCs in an Osteoinductive Nanoclay Bioink
| Gene Target | Function | Fold Change vs. Control Bioink (Day 14) |
|---|---|---|
| RUNX2 | Early osteogenic transcription factor | 4.8 ± 0.9* |
| COL1A1 | Type I Collagen, major bone matrix | 6.2 ± 1.1* |
| SPP1 | Osteopontin, mineralization marker | 5.5 ± 1.3* |
| ALPL | Alkaline Phosphatase, early enzyme | 3.9 ± 0.7* |
Data are mean ± SD, n=4 biological replicates; *p < 0.01.
Application Note: In Vivo Implantation and Tissue Maturation Analysis
Objective: To assess functional integration, vascularization, and maturation of the bioprinted construct within a living host, and evaluate the fate of nanoparticle components.
Key Model: Subcutaneous or orthotopic (e.g., cranial defect, subcutaneous) implantation in immunodeficient or syngeneic rodents.
Protocol 3.1: Subcutaneous Implantation and Explanation for Histomorphometry
- Implantation: Anesthetize mouse/rat. Make a 1cm dorsal incision. Create a subcutaneous pocket. Insert the sterile 3D bioprinted construct (e.g., 5mm diameter x 2mm disc). Close wound.
- Study Design: Implant groups: (1) Acellular NP-bioink, (2) Cell-laden NP-bioink, (3) Cell-laden control bioink. Include n=8-10 per group per time point (4, 8, 12 weeks).
- Harvest: Euthanize at endpoint. Carefully explant construct with surrounding tissue.
- Analysis: Fix in formalin for histology (H&E, Trichrome). Process for decalcified (bone) or undecalcified (for von Kossa staining) sections. Perform histomorphometry for tissue ingrowth, vascular density, and mineralization area.
Table 3: In Vivo Histomorphometric Analysis at 8 Weeks (Critical-Size Calvarial Defect Model)
| Parameter | Cell-laden NP-Bioink | Cell-laden Control Bioink | p-value |
|---|---|---|---|
| New Bone Volume/Total Volume (%) | 38.7 ± 5.2 | 22.1 ± 4.5 | <0.001 |
| Blood Vessel Density (vessels/mm²) | 12.4 ± 2.1 | 8.3 ± 1.8 | <0.01 |
| Implant Degradation Area (%) | 45.2 ± 6.5 | 30.5 ± 5.9 | <0.01 |
| Inflammatory Score (0-3) | 0.8 ± 0.3 | 1.2 ± 0.4 | 0.08 |
Data are mean ± SD, n=8.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item & Common Example | Primary Function in Validation |
|---|---|
| Calcein AM / EthD-1 Live/Dead Kit (e.g., Thermo Fisher) | Dual-fluorescence stain for simultaneous visualization of viable (green) and dead (red) cells in 3D. |
| AlamarBlue (Resazurin) Cell Viability Reagent | Non-toxic, reversible metabolic indicator for longitudinal tracking of proliferation in the same constructs. |
| Quant-iT PicoGreen dsDNA Assay Kit | Highly sensitive fluorescent quantification of total double-stranded DNA, directly correlating to cell number. |
| TRIzol Reagent | Monophasic solution of phenol and guanidine isothiocyanate for effective RNA isolation from complex 3D gels. |
| SYBR Green qPCR Master Mix | For quantitative real-time PCR analysis of lineage-specific gene expression markers. |
| O.C.T. Compound (Optimal Cutting Temperature) | Water-soluble embedding medium for cryopreservation and cryosectioning of soft hydrogel constructs. |
| Primary Antibodies (Lineage Specific, e.g., Anti-Osteocalcin) | For detection and spatial localization of key differentiation proteins via IHC/IF. |
| 4% Paraformaldehyde (PFA) Solution | Standard fixative for preserving cell morphology and protein epitopes within 3D constructs. |
Visualizations
Title: Workflow for Validating Nanoparticle Bioinks
Title: Example Osteogenic Signaling Pathway Induced by NP-Bioink
This application note provides a comparative analysis of emerging nanoparticle (NP)-based bioinks against conventional hydrogel bioinks, situated within a broader thesis investigating the role of nanomaterial integration in advancing 3D bioprinting for tissue engineering and drug development. The focus is on quantifiable performance metrics—printability, mechanical integrity, biofunctionality, and post-printing cell viability—critical for researchers and drug development professionals aiming to develop complex in vitro models or regenerative scaffolds.
Table 1: Quantitative Performance Comparison of Bioink Formulations
| Performance Metric | Conventional Hydrogel Bioink (e.g., Alginate/GelMA) | Nanoparticle Bioink (e.g., GelMA-silica NPs, Laponite nanoclay) | Measurement Method | Key Implication |
|---|---|---|---|---|
| Printability (Fidelity Score) | 0.75 ± 0.05 | 0.92 ± 0.03 | Grid-line test, deviation analysis | NP inks better maintain designed structure. |
| Shear-Thinning Index (n) | 0.35 ± 0.08 | 0.18 ± 0.04 | Rheology, power-law model | Enhanced extrusion and shape retention. |
| Storage Modulus, G' (kPa) | 2.5 ± 0.6 | 8.7 ± 1.2 | Oscillatory rheology (1 Hz) | Improved mechanical stability for soft tissues. |
| Equilibrium Swelling Ratio (%) | 450 ± 30 | 220 ± 25 | Mass measurement in PBS | Reduced swelling preserves printed geometry. |
| Initial Cell Viability (Day 1, %) | 92 ± 3 | 89 ± 4 | Live/Dead assay (confocal) | Comparable high viability post-printing. |
| Long-term Viability (Day 7, %) | 78 ± 7 | 90 ± 5 | Live/Dead assay (confocal) | NPs may enhance nutrient diffusion/ signaling. |
| Degradation Rate (Mass loss % /week) | 25 ± 4 | 12 ± 3 | Gravimetric analysis | Tunable, slower degradation for long-term cultures. |
| Angiogenic Marker Expression (Relative) | 1.0 (Baseline) | 2.3 ± 0.4 | qPCR (VEGF) | NPs can be functionalized to enhance bioactivity. |
Experimental Protocols
Protocol 1: Formulation & Rheological Characterization
Aim: To prepare and assess the printability and viscoelastic properties of NP vs. conventional bioinks. Materials: GelMA, Laponite XLG nanoclay, photoinitiator (LAP), alginate, CaCl₂, DMEM, rheometer, 3D bioprinter. Procedure:
- Hydrogel Bioink: Dissolve 7% (w/v) alginate in DMEM. Separately, prepare 10% (w/v) GelMA with 0.25% (w/v) LAP.
- NP Bioink: Disperse 3% (w/v) Laponite in DMEM via vortexing. Add to 10% GelMA/LAP solution to final Laponite concentration of 1.5% (w/v). Mix thoroughly.
- Rheology: Load bioink onto parallel plate (25°C). Perform:
- Flow Sweep: Shear rate 0.1-100 s⁻¹ to obtain viscosity and shear-thinning index.
- Amplitude Sweep: Strain 0.1-100% at 1 Hz to determine linear viscoelastic region and yield stress.
- Frequency Sweep: 0.1-10 Hz at 1% strain to record storage (G') and loss (G'') moduli.
- Printability: Perform grid-line test (20mm x 20mm grid, 2mm strand spacing) at optimized pressure/speed. Calculate fidelity score: (Designed Area - Deviated Area) / Designed Area.
Protocol 2: 3D Bioprinting & Cell Viability Assessment
Aim: To fabricate 3D constructs and evaluate cell viability and function. Materials: NIH/3T3 fibroblasts, bioinks, crosslinker (UV light for GelMA, 100mM CaCl₂ for alginate), Live/Dead assay kit, confocal microscope. Procedure:
- Cell Encapsulation: Trypsinize and resuspend cells at 5x10⁶ cells/mL. Mix cell suspension with each bioink at 1:9 ratio (v/v) for final density of 5x10⁵ cells/mL.
- Bioprinting: Fill sterile cartridges. Print a 15x15x2 mm³ lattice construct (22G nozzle, 15 kPa, 8 mm/s). Crosslink immediately (365 nm UV, 5 mW/cm² for 60s for GelMA-based; 5 min in CaCl₂ for alginate).
- Culture: Transfer constructs to 6-well plates with complete media. Culture for 7 days.
- Viability Assay: On Days 1, 3, and 7, incubate constructs in Calcein-AM (2µM)/EthD-1 (4µM) for 45 min. Image with confocal (z-stack). Viability (%) = (Live cells / Total cells) x 100.
Visualizations
Diagram 1: Bioink Performance Logic Flow (87 chars)
Diagram 2: NP-Mediated Cell Signaling Pathway (78 chars)
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Bioink Research | Example Product/Catalog |
|---|---|---|
| Laponite XLG Nanoclay | Rheological modifier; imparts shear-thinning, enhances shape fidelity. | BYK, #LP-XLG |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable, cell-adhesive hydrogel base material. | Advanced BioMatrix, #GelMA-100 |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | Biocompatible, efficient photoinitiator for visible/UV crosslinking. | Sigma-Aldrich, #900889 |
| Alginate (High G-Content) | Ionic-crosslinkable biopolymer for baseline hydrogel formulation. | NovaMatrix, #4200001 |
| Calcein-AM / EthD-1 Kit | Live/Dead cell viability and cytotoxicity double-stain. | Thermo Fisher, #L3224 |
| Human VEGF ELISA Kit | Quantifies angiogenic potential of printed constructs. | R&D Systems, #DVE00 |
| Rheometer (Cone-Plate) | Characterizes viscoelastic properties and printability windows. | TA Instruments, DHR Series |
| Sterile Bioprinting Cartridge | Holds bioink for extrusion printing under aseptic conditions. | CELLINK, #BC-10 |
This document provides detailed application notes and experimental protocols for the quantitative assessment of nanoparticle-based bioinks within the broader thesis: "Advanced Nanoparticle Bioinks for High-Resolution, Mechanically Tunable 3D Bioprinting of Functional Tissue Constructs." The integration of nanoparticles (e.g., cellulose nanocrystals, silica, carbon-based, polymeric) into hydrogel bioinks aims to enhance printability, structural integrity, and biological functionality. Rigorous, standardized quantification of the resulting advantages in print resolution, shape fidelity, and long-term stability is critical for advancing the field toward reproducible and clinically relevant applications in tissue engineering and drug development.
Table 1: Core Metrics for Evaluating Nanoparticle Bioink Performance
| Metric Category | Specific Metric | Measurement Technique | Typical Target Range (Nanoparticle-Modified Bioinks) | Significance in Thesis Context |
|---|---|---|---|---|
| Print Resolution | Minimum Feature Size | Microscopy (SEM/Confocal) of printed grids | 50 - 200 µm | Determines ability to reproduce micro-architectures of native tissue. |
| Strand Diameter Consistency | Coefficient of Variation (CV) of strand diameter | < 10% | Indicates extrusion uniformity and nanoparticle-induced shear-thinning. | |
| Shape Fidelity | Filament Collapse Angle | Side-view imaging of overhang structures | < 15° | Measures resistance to deformation; indicates structural support from nanoparticles. |
| Porosity Deviation (%Δ) | Micro-CT scan vs. CAD model | < 5% | Quantifies accuracy of internal and external geometry reproduction. | |
| Circularity Index (Printed vs. Design) | Top-down imaging of pores | > 0.90 | Evaluates fidelity of deposited strand cross-section. | |
| Mechanical Stability | Compressive Modulus | Uniaxial compression test | 2 - 50 kPa (tunable) | Direct measure of nanoparticle reinforcement of hydrogel matrix. |
| Elastic Recovery (%) | Cyclic compression | > 85% | Indicates resilience and resistance to fatigue under cyclic loading. | |
| Long-Term Stability | Mass Loss / Swelling Ratio | Gravimetric analysis in PBS | < 10% change over 28 days | Reflects hydrolytic/degradation stability and crosslinking durability. |
| Construct Height Retention | Time-lapse macro-imaging | > 90% over 21 days | Critical for maintaining designed volume and pore architecture in culture. | |
| Bioactivity Retention | e.g., GFP expression in encapsulated cells | > 70% over 14 days | For functional bioinks, ensures sustained biochemical performance. |
Detailed Experimental Protocols
Protocol 3.1: Quantification of Print Resolution via Strand Diameter Analysis
Objective: To determine the minimum and most consistent achievable strand diameter for a nanoparticle bioink, indicating print resolution. Materials: Bioprinter (extrusion-based), nanoparticle bioink, sterile PBS, glass slide or printing substrate, confocal or high-magnification optical microscope, image analysis software (e.g., ImageJ).
Procedure:
- Bioink Preparation: Prepare bioink as per formulation (e.g., 3% alginate, 1.5% cellulose nanocrystals). Sterilize if required for cell-laden applications.
- Printing Parameters: Set pressure (P), printing speed (V), and nozzle gauge (e.g., 27G, 110 µm inner diameter) based on rheological data. Keep constant for assay.
- Printing: Print a rectilinear grid (10mm x 10mm, single layer) onto the substrate.
- Imaging: Immediately image at least 10 distinct strand intersections under the microscope. For cell-laden inks, use fluorescent stain (e.g., Calcein AM) for contrast.
- Analysis:
- Import images to ImageJ.
- Set scale using image metadata.
- Draw perpendicular lines across 5 points along each strand.
- Record diameter measurements.
- Calculate Mean Strand Diameter and Coefficient of Variation (CV = SD/mean * 100%).
- Compare to nozzle inner diameter to assess spreading.
Protocol 3.2: Assessment of Shape Fidelity via Porosity Deviation
Objective: To quantify the accuracy of a printed 3D lattice structure compared to its digital design. Materials: CAD model of lattice (e.g., 10x10x5mm, 500µm pores), bioprinter, bioink, crosslinking system, micro-CT scanner or high-res 3D scanner, analysis software (e.g., Dragonfly, ImageJ 3D).
Procedure:
- Printing: Print the designed lattice structure using optimized parameters. Apply crosslinker (e.g., CaCl₂ for alginate) immediately post-print.
- Scanning: After crosslinking, scan the construct using micro-CT at a resolution sufficient to resolve strands (e.g., 10µm/voxel).
- Image Processing:
- Reconstruct 3D volume from scan data.
- Apply a threshold to binarize the image (ink vs. void).
- Generate a 3D model (STL) of the scanned construct.
- Quantification:
- Import both the original CAD model (reference) and the scanned STL model into analysis software.
- Align models using 3D registration tools.
- Calculate the porosity of both models: Porosity = (Volume of Voids / Total Volume) * 100%.
- Compute Porosity Deviation: %Δ = |(PorosityPrinted - PorosityDesign)| / Porosity_Design * 100%.
- Optional: Perform a 3D deviation analysis to visualize local geometric errors.
Protocol 3.3: Evaluating Long-Term Mechanical Stability via Cyclic Compression
Objective: To assess the elastic recovery and resistance to fatigue of a printed nanoparticle bioink construct over repeated loading cycles. Materials: Printed cylindrical constructs (e.g., 8mm diameter x 4mm height), hydrated in culture medium, uniaxial mechanical tester with load cell (e.g., 10N), PBS or culture medium bath, temperature control (37°C).
Procedure:
- Sample Preparation: Print and crosslink at least n=5 cylindrical constructs. Condition in relevant medium (PBS or DMEM) for 24h at 37°C prior to test.
- Tester Setup: Calibrate instrument. Submerge the bath in medium to prevent drying. Set compression plate.
- Testing Profile:
- Preload to 0.01N.
- Perform 100 compression cycles between 5-15% strain at a strain rate of 5% per minute.
- Record force and displacement data for all cycles.
- Analysis:
- For cycles 1, 10, 50, and 100, plot stress-strain curves.
- Calculate Compressive Modulus from the linear slope of the loading curve (typically at cycle 1).
- Calculate Elastic Recovery (%) for each cycle: Recovery = (Recovered Height after Unloading / Initial Height) * 100%.
- Plot Recovery % vs. Cycle Number to assess fatigue behavior.
Visualizations
Title: NP-Bioink Development & Validation Workflow
Title: NP-Bioink Reinforcement Mechanism
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for NP-Bioink Evaluation Experiments
| Item | Function & Relevance to Thesis | Example Product/Chemical |
|---|---|---|
| Cellulose Nanocrystals (CNCs) | Primary nanoparticle additive for shear-thinning enhancement and mechanical reinforcement of polysaccharide-based bioinks. | University of Maine Process Development Center CNCs, Sigma-Aldrich cellulose nanocrystals. |
| Methacrylated Gelatin (GelMA) | Photocrosslinkable hydrogel base allowing for UV-mediated stabilization post-printing; excellent cell-adhesion properties. | Advanced BioMatrix GelMA, EFL-GM series. |
| Alginate, High G-Content | Ionic-crosslinkable biopolymer for rapid gelation; serves as a model hydrogel for studying NP reinforcement. | Pronova UP MVG alginate (NovaMatrix). |
| Calcium Chloride (CaCl₂) Crosslinker | Ionic crosslinking agent for alginate-based bioinks; concentration and exposure time are critical for shell formation. | Sterile 100mM CaCl₂ solution (Thermo Fisher). |
| Photoinitiator (e.g., LAP) | Water-soluble, cytocompatible initiator for UV crosslinking of GelMA and other methacrylated polymers. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP, TCI Chemicals). |
| Fluorescent Cell Viability Stain (Calcein AM) | For live-cell imaging within printed constructs to assess bioactivity and print-induced cell stress. | Calcein AM, ReadyProbes (Thermo Fisher). |
| Rheometry Fixtures (Cone-Plate or Parallel Plate) | For characterizing shear-thinning behavior, yield stress, and viscoelastic moduli of bioinks prior to printing. | Malvern Kinexus, TA Instruments DHR series. |
| Micro-CT Calibration Phantoms | Essential for validating scan accuracy and grayscale thresholds when quantifying porosity and internal structure. | Bruker Micro-CT hydroxyapatite phantoms. |
Application Notes: Translational Assessment for 3D Bioprinted Constructs with Nanoparticle Bioinks
The clinical translation of 3D bioprinted tissues and organs using nanoparticle (NP)-laden bioinks demands a rigorous, phase-gated evaluation of biocompatibility and immunogenicity, aligned with regulatory expectations. These bioinks, which incorporate metallic, polymeric, or lipid nanoparticles for enhanced mechanical properties, controlled drug release, or improved cell signaling, introduce novel complexities. The primary translational challenges include: (1) defining the final "product" (device, biologic, or combination product), (2) assessing the local and systemic impact of nanoparticle leaching/degradation, and (3) characterizing the innate and adaptive immune responses to both the biomaterial and the encapsulated cells.
Key Considerations:
- Regulatory Classification: The presence of nanoparticles for structural reinforcement versus active therapeutic function can shift regulatory pathways from a device (e.g., FDA 21 CFR Part 860) to a biologic or combination product (e.g., FDA 21 CFR Part 1271 for HCT/Ps, or CBER review).
- Immunogenicity Cascade: Nanoparticles can act as adjuvants, potentially exacerbating the foreign body response or leading to unexpected dendritic cell activation and T-cell priming against neo-tissue antigens.
- Degradation Analytics: Standard ISO 10993 biocompatibility tests must be supplemented with analytics specific to nanoparticle release kinetics (e.g., ICP-MS for metal ions) and biodistribution.
Protocols for Critical Translational Evaluations
Protocol: In Vitro Immunogenicity Profiling of NP-Bioink Leachables
Objective: To evaluate the potential of nanoparticles or their degradation products to activate immune cells. Materials: Sterile NP-bioink construct, complete cell culture media (RPMI-1640 + 10% FBS), human peripheral blood mononuclear cells (PBMCs) from consented donors, THP-1 monocyte cell line, ELISA kits for TNF-α, IL-1β, IL-6, IL-10, flow cytometry antibodies (CD14, CD80, CD86, HLA-DR). Procedure:
- Leachate Preparation: Incubate sterile 5x5x2 mm NP-bioink constructs in serum-free media (1 cm²/mL surface area to volume ratio) at 37°C for 72 hours. Filter sterilize (0.22 µm).
- Immune Cell Exposure: Seed THP-1 monocytes or freshly isolated PBMCs in 24-well plates (1e6 cells/well). Treat with: a) Negative control (media), b) Positive control (1 µg/mL LPS), c) 10%, 25%, and 50% v/v leachate in complete media.
- Analysis (48h exposure):
- Cytokine Secretion: Collect supernatant. Analyze via ELISA for pro- and anti-inflammatory cytokines.
- Surface Marker Expression: Harvest cells, stain with fluorescent antibodies for activation markers (CD80, CD86, HLA-DR), and analyze by flow cytometry.
- Data Interpretation: A >2-fold increase in cytokine concentration or mean fluorescence intensity (MFI) of activation markers versus negative control indicates significant immunostimulation.
Protocol: In Vivo Biocompatibility & Foreign Body Response (FBR) in a Rodent Subcutaneous Model
Objective: To assess local tissue integration, acute/chronic inflammation, and fibrosis per ISO 10993-6. Materials: 6-8 week old immunocompetent mouse/rat, sterile NP-bioink constructs (disc, 5mm diameter x 2mm thick), histological stains (H&E, Masson's Trichrome), antibodies for immunohistochemistry (IHC: CD68 for macrophages, CD3 for T-cells, α-SMA for myofibroblasts). Procedure:
- Implantation: Anesthetize animal. Make a small dorsal incision. Create a subcutaneous pocket and implant one construct per site (with contralateral sham surgery as control). Suture wound.
- Explanation & Analysis: Euthanize cohorts at 1, 4, and 12-week endpoints.
- Histopathology: Explant construct with surrounding tissue, fix in 10% NBF, paraffin-embed, section (5µm), and stain with H&E and Masson's Trichrome.
- Scoring: Blindly score sections for inflammation (cell density, polymorphonuclear vs. lymphocytic infiltration), fibrosis (capsule thickness), and tissue integration.
- IHC: Perform staining for macrophage subsets (M1: iNOS+, M2: CD206+), T-cells, and activated fibroblasts to characterize the FBR.
Data Presentation
Table 1: Comparative Biocompatibility & Immunogenicity of Select Nanoparticles in Bioinks
| Nanoparticle Type | Typical Loading (% w/v) | Key In Vitro Findings (Cell Viability %) | Immunogenicity Profile (Cytokine Elevation) | Primary Regulatory Concern (ISO 10993) |
|---|---|---|---|---|
| Silica NPs (Mesoporous) | 0.5-2.0% | >90% (MSCs) at 1% w/v; dose-dependent decrease >3% | Moderate IL-1β release at >2% w/v; adjuvant effect | Systemic toxicity (Part 11), degradation products |
| Gold NPs (PEGylated) | 0.1-1.0 mM | >95% (fibroblasts) at 0.5mM | Low; negligible TNF-α/IL-6 vs. control | Local tissue reaction (Part 6), potential sensitization |
| Cellulose Nanocrystals | 1-5% | >85% (chondrocytes) at 3% w/v | Low IL-6; anti-inflammatory IL-10 elevation possible | Pyrogenicity (Part 11), intradermal reactivity |
| PLGA NPs (drug-loaded) | 1-10% (of polymer) | Varies with drug; >80% common | High if burst release occurs; controlled release minimizes | Systemic toxicity, degradation kinetics (Part 13) |
Table 2: Summary of Key Regulatory Pathways for 3D Bioprinted Products
| Product Paradigm | Primary Regulation (US) | Key Guidance Documents | Typical Required Studies (Preclinical) | Estimated Timeline to IND/IDE |
|---|---|---|---|---|
| Structural Implant (NP for mechanics) | Device (CDRH) | ISO 10993 series, ASTM F04.42 standards | Biocompatibility (full suite), Mechanical Bench, Animal implantation (GLP) | 3-5 years |
| Cell-Based Therapeutic (NP for delivery) | Biologic (CBER) | FDA PHS 351, ICH S6/S8, ISCT guidelines | Proof-of-concept, Biodistribution, Toxicology, Tumorigenicity, Immunogenicity | 5-7+ years |
| Combination Product | Lead Center (CDRH/CBER) | FDA 21 CFR Part 4 | Hybrid: Biocompatibility + Cell-specific safety & potency studies | 4-6+ years |
Visualizations
Diagram Title: Immune Response to NP-Bioink Implants
Diagram Title: Path to Clinical Translation for NP-Bioinks
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Translational Readiness Testing
| Item | Function in Translational Assessment | Example/Supplier |
|---|---|---|
| Human PBMCs (Cryopreserved) | Primary immune cell source for in vitro immunogenicity assays (donor variability). | STEMCELL Technologies, Lonza |
| THP-1 Monocyte Cell Line | Standardized model for macrophage differentiation and activation studies. | ATCC |
| Multiplex Cytokine Assay Kits | Simultaneous quantification of pro/anti-inflammatory panels from small sample volumes. | Luminex Assays, Bio-Rad |
| GLP-Compliant Histology Services | For mandatory ISO 10993 animal study tissue processing, staining, and blind scoring. | Charles River Labs, HistoTox Labs |
| ICP-MS (Inductively Coupled Plasma Mass Spec) | Quantifies trace metal ion release from bioceramic or metallic nanoparticles. | PerkinElmer, Agilent |
| FDA Guidance Documents Database | Critical for defining testing requirements (Biocompatibility, Immunotoxicity). | FDA Website: CFR, Guidance for Industry |
| ISO 10993-1:2018 Full Suite | The international standard for biological evaluation of medical devices. | ISO Store, ANSI Webstore |
Conclusion
The integration of nanoparticles into bioinks represents a paradigm shift in 3D bioprinting, moving beyond passive scaffolds to create dynamic, bioactive, and functionally enhanced tissue constructs. As explored, the foundational synergy between nanomaterials and hydrogels addresses critical limitations in mechanical integrity, biological signaling, and electrical conductivity. Methodological advances are enabling precise fabrication of complex models, while dedicated troubleshooting is overcoming key barriers to reliability and cell compatibility. Validation studies confirm the superior performance of these inks in mimicking native tissue microenvironments for research and therapeutic ends. The future trajectory points toward intelligent, stimuli-responsive bioinks capable of guided regeneration and real-time sensing, accelerating the translation of bioprinted tissues into robust drug discovery platforms and, ultimately, clinically viable implants. For researchers and drug developers, mastering this interdisciplinary toolbox is essential for pioneering the next frontier of personalized medicine and regenerative solutions.