Breaking Barriers: BBB Disruption Strategies for Glioblastoma Therapy in 2024
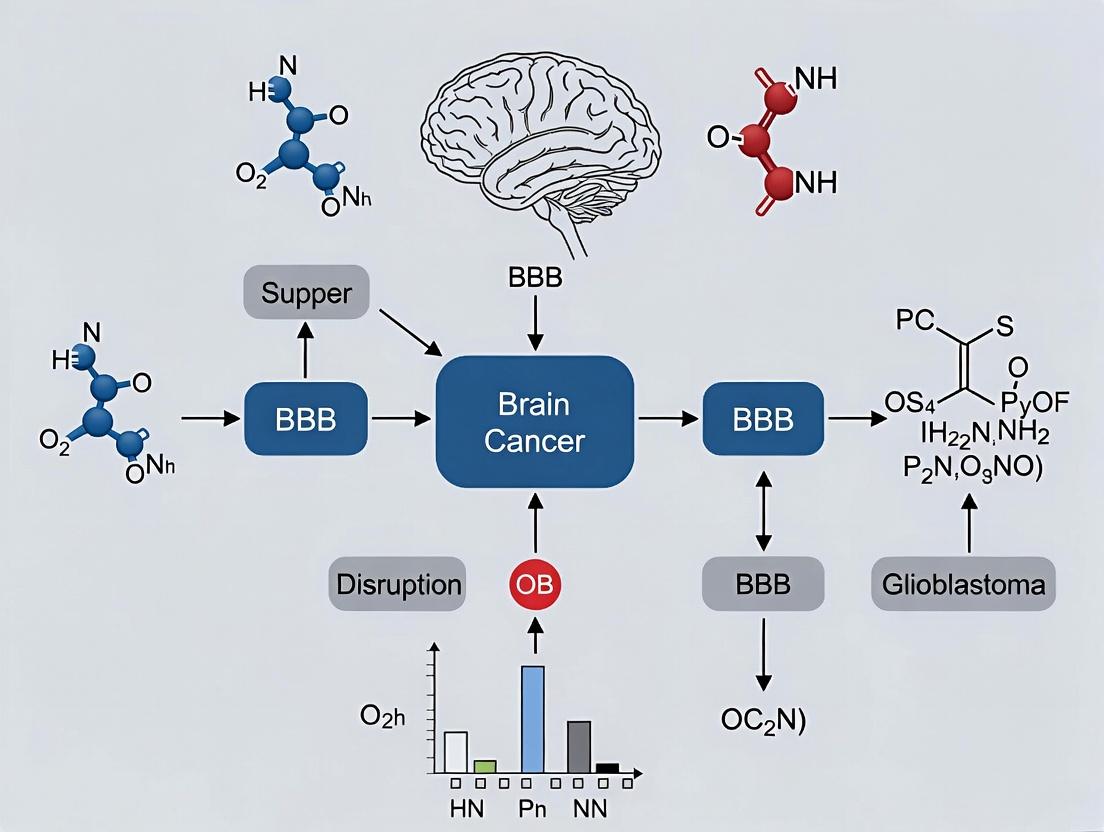
This article provides a comprehensive review for researchers and drug development professionals on the critical role of Blood-Brain Barrier (BBB) disruption in brain cancer and glioblastoma treatment.
Breaking Barriers: BBB Disruption Strategies for Glioblastoma Therapy in 2024
Abstract
This article provides a comprehensive review for researchers and drug development professionals on the critical role of Blood-Brain Barrier (BBB) disruption in brain cancer and glioblastoma treatment. It explores the foundational biology of the intact and compromised BBB in tumors, examines current and emerging methodologies for intentional disruption and drug delivery, addresses key challenges in clinical translation, and validates approaches through comparative analysis of preclinical and clinical data. The synthesis aims to inform the development of next-generation therapeutic strategies that effectively navigate this formidable biological barrier.
The Glioblastoma Fortress: Understanding the BBB's Dual Role in Protection and Obstruction
The intact blood-brain barrier (BBB) represents the single greatest physiological obstacle to therapeutic delivery in brain cancer and glioblastoma (GBM). Understanding its sophisticated structure and regulatory physiology is not merely an academic exercise in neurovascular biology but a prerequisite for devising strategies to overcome it. This whitepaper details the anatomy and physiology of the neurovascular unit (NVU), the functional core of the BBB, providing a baseline from which its pathological disruption in GBM can be understood and potentially therapeutically exploited.
The Neurovascular Unit: A Cellular Consortium
The BBB is not a passive barrier but a dynamic interface governed by the NVU, a multicellular ensemble. Its integrity is maintained through precise cell-cell communication.
Table 1: Cellular Components of the Neurovascular Unit and Their Primary Functions
| Cell Type | Primary Functions in BBB Integrity | Relevance to Brain Cancer Research |
|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | - Form continuous, non-fenestrated capillary walls.- Express tight junction (TJ) and adherens junction (AJ) complexes.- Exhibit low rates of pinocytosis and transcytosis.- Express efflux transporters (e.g., P-gp, BCRP). | - Primary physical and transport barrier to chemotherapeutics.- Efflux pumps actively remove drugs.- TJ disruption is a hallmark of GBM-associated BBB. |
| Pericytes | - Embedded within the endothelial basement membrane.- Regulate capillary diameter and cerebral blood flow.- Contribute to TJ formation and stability.- Modulate endothelial transcytosis. | - Loss of pericyte coverage correlates with BBB leakage in GBM.- Potential target for vascular normalization therapy. |
| Astrocytes (End-feet) | - Terminal "end-feet" processes ensheath >99% of the abluminal capillary surface.- Release factors (e.g., GDNF, Ang-1) that induce and maintain BBB properties.- Contribute to ion and water homeostasis. | - Reactive astrogliosis around tumors alters BBB function.- Can release both protective and disruptive signals. |
| Microglia | - Resident immune sentinels.- Survey the microenvironment.- Release cytokines that can modulate BBB permeability. | - Pro-tumoral (M2) polarization can promote angiogenesis and immunosuppression. |
| Neurons | - Modulate blood flow and BBB function via neurotransmitter release.- Couple metabolic demand to supply. | - Tumor-induced neuronal activity influences the peritumoral microenvironment. |
| Basement Membrane | - Extracellular matrix synthesized by endothelia and pericytes.- Provides structural support and cell anchoring.- Reservoir for signaling molecules. | - Remodeled and degraded in GBM invasion, facilitating metastasis. |
Molecular Anatomy of the BBB
Tight and Adherens Junctions
The paracellular barrier is sealed by junctional complexes. Key proteins include:
- Tight Junctions: Claudins (esp. CLDN-5), Occludin, Junctional Adhesion Molecules (JAMs), linked to the actin cytoskeleton via Zonula Occludens (ZO-1, ZO-2) proteins.
- Adherens Junctions: Vascular endothelial (VE)-cadherin, linked via catenins.
Table 2: Key Junctional Proteins and Quantitative Expression
| Protein | Primary Role | Approx. Molecular Weight (kDa) | Notes on Expression/Function |
|---|---|---|---|
| CLDN-5 | Primary sealing protein, creates charge-selective pores. | ~23 | Critical for barrier; deletion in mice leads to lethal BBB breakdown. |
| Occludin | Regulatory, modulates barrier and signaling. | ~65 | Phosphorylation state regulates junction assembly/function. |
| ZO-1 | Scaffold, links transmembrane proteins to actin. | ~220 | Essential for junction assembly; displacement is an early sign of BBB disruption. |
| VE-cadherin | Mediates endothelial cell-cell adhesion. | ~130 | Stabilizes junctions; cleavage by MMPs in GBM promotes permeability. |
Transport Machinery
- Influx Transporters: (e.g., GLUT1 for glucose, LAT1 for large neutral amino acids).
- Efflux Transporters: P-glycoprotein (P-gp/ABCB1), Breast Cancer Resistance Protein (BCRP/ABCG2).
- Transcytosis: Minimal in healthy BBB via receptor-mediated (RMT) and adsorptive-mediated (AMT) pathways. GBM co-opts these pathways (e.g., via LRP1 RMT) for nutrient uptake.
Signaling Physiology of the NVU
Barrier function is dynamically regulated by intercellular signaling within the NVU.
Diagram 1: Wnt/β-catenin Signaling in BBB Induction and Maintenance
Diagram 2: Angiopoietin-1/Tie2 Signaling for Barrier Stabilization
Experimental Protocols for Assessing Intact BBB/NVU Function
Protocol 1: In Vitro Transendothelial Electrical Resistance (TEER) Measurement
Aim: Quantify real-time barrier integrity of BMEC monolayers. Method:
- Cell Culture: Seed primary human BMECs or induced pluripotent stem cell (iPSC)-derived BMECs onto collagen/fibronectin-coated permeable transwell inserts (0.4 μm pores).
- Measurement: Use an epithelial voltohmmeter with "chopstick" electrodes.
- Procedure: Equilibrate system in cell culture medium. Place electrode in outer (basolateral) well, then inner (apical) well. Record resistance (Ω).
- Calculation: Subtract blank insert resistance. Multiply net resistance (Ω) by effective membrane area (cm²) to obtain TEER (Ω×cm²). Acceptance Criterion: TEER > 1500 Ω×cm² for rodent cells, >500 Ω×cm² for human cells, indicates significant barrier formation.
- Validation: Perform concurrently with permeability assay using fluorescent tracers (e.g., 4 kDa FITC-dextran).
Protocol 2: Immunofluorescence Analysis of Junctional Proteins
Aim: Visualize and localize TJ/AJ proteins in an in vitro NVU model. Method:
- Culture: Grow BMECs in co-culture with pericytes/astrocytes or monoculture on glass coverslips.
- Fixation: Fix cells with 4% paraformaldehyde (PFA) for 15 min at RT.
- Permeabilization/Blocking: Permeabilize with 0.1% Triton X-100, block with 5% normal goat serum.
- Staining: Incubate with primary antibodies (e.g., anti-CLDN5, anti-ZO-1, anti-VE-cadherin) overnight at 4°C.
- Detection: Incubate with fluorophore-conjugated secondary antibodies. Counterstain nuclei with DAPI. Mount.
- Imaging: Acquire high-resolution Z-stacks using confocal microscopy. Analyze for continuous, linear staining at cell borders.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BBB/NVU Research
| Reagent/Material | Provider Examples | Primary Function in Research |
|---|---|---|
| Primary Human BMECs | ScienCell, Cell Systems | Gold-standard primary cells for in vitro BBB models. |
| iPSC-derived BMEC Kits | STEMCELL Technologies, Cedarlane Labs | Reproducible, scalable source of human BMECs with high TEER. |
| Transwell Permeable Supports | Corning, Greiner Bio-One | Physical supports for culturing polarized endothelial monolayers for TEER/permeability assays. |
| EVOM3 Voltohmmeter | World Precision Instruments | Instrument for accurate, standardized TEER measurement. |
| Claudin-5 Antibody | Invitrogen, Abcam | Key antibody for immunofluorescence and Western blot analysis of tight junctions. |
| Fluorescent Tracers (FITC-dextran) | Sigma-Aldrich, TdB Labs | Used in permeability assays to quantify paracellular leak (e.g., 4 kDa for BBB integrity). |
| Recombinant Human Angiopoietin-1 | R&D Systems, PeproTech | Used to stimulate Tie2 signaling and promote barrier stabilization in experiments. |
| DAPT (γ-secretase inhibitor) | Tocris, Selleckchem | Inhibits Notch signaling; used to study its role in BBB differentiation and function. |
This whitepaper provides an in-depth technical guide to the pathological disruption of the blood-brain barrier (BBB) within the glioblastoma (GBM) microenvironment. The content is framed within the broader thesis of understanding BBB dysregulation as a central, yet paradoxical, feature of brain cancer: while the BBB remains a significant obstacle to therapeutic delivery, the tumor core and peritumoral regions exhibit severe, heterogeneous vascular leakiness. This disruption is not a passive breakdown but an active, multifaceted process driven by dynamic crosstalk between glioma cells, endothelial cells, pericytes, astrocytes, and immune cells. Understanding the molecular and cellular mechanisms of this "leaky vasculature" is critical for developing novel strategies to normalize the tumor vasculature or selectively enhance drug delivery across the compromised BBB.
Core Mechanisms of BBB Disruption in GBM
GBM-induced BBB disruption involves coordinated pathological signaling.
Diagram Title: Key Pathways in GBM-Driven BBB Disruption
Quantitative Alterations in BBB Components
Table 1: Quantifiable Changes in BBB Integrity Markers in GBM vs. Normal Brain
| BBB Component | Specific Marker | Normal Brain Expression/Level | GBM Tumor Core Expression/Level | Measurement Method | Key Reference |
|---|---|---|---|---|---|
| Tight Junctions | Claudin-5 | High (Continuous) | Reduced by 60-80% (Discontinuous) | IHC, WB | Agarwal et al., 2019 |
| Occludin | High | Reduced by ~70% | IHC, WB | ||
| Adherens Junctions | VE-cadherin | High | Reduced by ~50% | IHC | |
| Basement Membrane | Collagen IV | Thick, continuous | Fragmented, ~40% thinning | EM, IHC | |
| Laminin | Intact | Degraded, irregular | IHC | ||
| Pericyte Coverage | PDGFR-β, NG2 | >80% coverage | <30% coverage | IHC co-staining (CD31/NG2) | |
| Transcytosis | Caveolin-1 (CAV1) | Low | Increased 5-7 fold | IHC, mRNAseq | |
| Efflux Transporters | P-glycoprotein (ABCB1) | High at luminal membrane | Heterogeneous, often reduced | IHC, Functional assay |
Experimental Protocols for Assessing BBB Disruption
Protocol: In Vitro BBB Permeability Assay Using a Transwell Model
Objective: To quantitatively measure paracellular permeability in a human brain microvascular endothelial cell (HBMEC) monolayer under GBM-conditioned media exposure.
- Coat Transwells: Coat polyester Transwell inserts (3.0 µm pore, 12-well format) with 150 µL of rat tail collagen type I (100 µg/mL). Incubate at 37°C for 1 hr.
- Seed HBMECs: Plate primary HBMECs (passage 3-5) at a density of 1.0 x 10^5 cells/insert in EGM-2MV medium. Culture for 5-7 days until Transendothelial Electrical Resistance (TEER) >150 Ω·cm².
- Apply Conditioned Media: Replace medium in the upper chamber with 0.5 mL of conditioned media from patient-derived GBM stem-like cells (GSCs) or U87-MG cells (72-hr collection, centrifuged). Control uses fresh EGM-2MV.
- Measure TEER: Monitor TEER daily using a volt-ohm meter. Calculate TEER as (Sample - Blank) x Membrane Area.
- Fluorescent Tracer Permeability Assay: At experimental endpoint (e.g., 48 hrs), add 0.5 mL of 1 mg/mL FITC-Dextran (70 kDa or 4 kDa) in HBSS to the upper chamber. Collect 100 µL from the lower chamber at T=0, 30, 60, 90, 120 min.
- Quantification: Measure fluorescence (Ex/Em: 490/520 nm). Calculate Apparent Permeability (Papp): Papp = (dQ/dt) / (A * C0), where dQ/dt is flux rate, A is membrane area, C0 is initial upper chamber concentration.
Protocol: In Vivo Assessment of Vascular Leakiness (Evans Blue Extravasation)
Objective: To visualize and quantify BBB disruption in an orthotopic GBM mouse model.
- Tumor Implantation: Implant 2x10^5 luciferase-tagged GL261 cells or patient-derived xenograft cells into the right striatum of C57BL/6 mice (coordinates: 2 mm lateral, 0.5 mm anterior to bregma, 3 mm depth).
- Dye Administration: At day 14-21 post-implantation, inject 2% (w/v) Evans Blue dye (EB) in saline (4 mL/kg) via tail vein. Allow circulation for 1 hour.
- Perfusion and Tissue Collection: Deeply anesthetize mouse. Perfuse transcardially with 50 mL ice-cold PBS at 10 mL/min to clear intravascular dye. Extract brain.
- Qualitative Imaging: Photograph the whole brain under brightfield to visualize blue staining.
- Quantitative Extraction: Weigh the tumor-containing hemisphere. Homogenize in 1 mL of 50% trichloroacetic acid (TCA). Centrifuge at 10,000xg for 20 min. Collect supernatant.
- Spectrophotometry: Dilute supernatant 1:3 in ethanol (1:1:0.5 ratio of sample:ethanol:TCA). Measure absorbance at 610 nm. Calculate EB content (µg/g brain) against a standard curve.
The Tumor Microenvironment's Role
The leaky vasculature exists within a hostile TME that perpetuates its dysfunction.
Diagram Title: TME Feedback Loop Driving BBB Leakiness
Quantitative Data on TME Factors
Table 2: Key TME Parameters in Glioblastoma Affecting BBB Integrity
| TME Parameter | Normal Brain | GBM Tumor Core | Measurement Technique | Impact on BBB |
|---|---|---|---|---|
| Partial Pressure of O2 (pO2) | ~30-35 mm Hg | <10 mm Hg (Severe Hypoxia) | Oxygen-sensitive electrodes, Hypoxyprobe | Induces HIF-1α → VEGF |
| Interstitial Fluid Pressure (IFP) | 0-1 mm Hg | 15-25 mm Hg | Wicket catheter, MRI-based | Collapses vessels, hinders convection |
| Extracellular pH | ~7.3 | 6.7-7.0 (Acidic) | pH-sensitive MRI, microelectrodes | Activates cathepsins, MMPs |
| Stiffness (Elastic Modulus) | 0.1-0.5 kPa | 1-10 kPa | Atomic Force Microscopy (AFM) | Activates mechanosensitive integrin pathways |
| Immune Cell Infiltrate | Resting Microglia | 30-50% of cells are TAMs (Macrophages + Microglia) | Flow cytometry (CD11b+, CD45high/low) | Source of VEGF, MMP-9, TGF-β |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying BBB Disruption in GBM
| Reagent/Catalog # | Supplier Example | Function in BBB/GBM Research |
|---|---|---|
| Primary Human Brain Microvascular Endothelial Cells (HBMECs) | Cell Systems (ACBRI 376), ScienCell (1000) | Gold standard for in vitro BBB models; express key TJ proteins and transporters. |
| Transwell Permeable Supports (3.0 µm, polyester) | Corning (3460) | Physical scaffold for growing endothelial monolayers for permeability assays. |
| EVOM3 Voltohmmeter with STX2 Electrodes | World Precision Instruments | Accurately measures Transendothelial Electrical Resistance (TEER) as a proxy for junctional integrity. |
| FITC-Dextran, 70 kDa and 4 kDa | Sigma-Aldrich (FD70S, FD4) | Fluorescent tracer molecules for quantifying paracellular (70 kDa) and broader (4 kDa) permeability. |
| Recombinant Human VEGF165 | PeproTech (100-20) | Positive control for inducing pathological angiogenesis and vascular permeability in vitro and in vivo. |
| Anti-Claudin-5 Antibody [4C3C2] | Invitrogen (35-2500) | Validated antibody for detecting tight junction protein localization/disruption via IF/IHC. |
| MMP-9 Activity Assay Kit (Fluorometric) | Abcam (ab197752) | Quantifies active MMP-9 levels in conditioned media or tissue lysates, key for BM degradation. |
| Hypoxyprobe-1 (Pimonidazole HCl) | Hypoxyprobe Inc. | Forms protein adducts in hypoxic tissues (<10 mm Hg O2) detectable by IHC, linking hypoxia to BBB disruption. |
| GL261-Luc2 Mouse Glioma Cells | PerkinElmer (124336) | Syngeneic, luciferase-expressing cell line for orthotopic models allowing tumor growth and BBB leakiness monitoring. |
| Evans Blue Dye (E2129) | Sigma-Aldrich | Classic albumin-binding dye for macroscopic and quantitative assessment of vascular leakiness in vivo. |
The blood-brain barrier (BBB) represents a formidable obstacle in the treatment of primary brain tumors like glioblastoma (GBM). While BBB disruption is a central therapeutic aim, the phenomenon of heterogeneous permeability creates a paradoxical landscape: regions of leaky vasculature coexist with intact, treatment-resistant sanctuaries. This spatial and temporal heterogeneity in barrier function is a critical determinant of therapeutic failure. This whitepaper explores the mechanistic basis of this paradox, its implications for drug delivery, and outlines contemporary experimental approaches for its investigation within the broader thesis of optimizing BBB disruption in neuro-oncology.
Mechanistic Foundations of Heterogeneous Permeability
Heterogeneous BBB permeability in GBM is driven by dynamic tumor-host interactions.
Key Drivers:
- Angiogenic Dysregulation: GBM-secreted VEGF leads to chaotic, immature vasculature with aberrant tight junction (TJ) protein expression (e.g., claudin-5, ZO-1).
- Inflammatory Mediators: Tumor-associated macrophages and microglia release TNF-α, IL-1β, and MMPs (particularly MMP-9), which degrade basement membrane and modulate TJ integrity.
- Cellular Stress: Hypoxia and acidosis within the tumor microenvironment further destabilize endothelial cell biology.
- Heterogeneous Expression of Transporters: P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) remain functional in pockets of vasculature, actively excluding chemotherapeutics.
Quantitative Data on Permeability Heterogeneity
Data synthesized from recent studies (2022-2024) utilizing dynamic contrast-enhanced MRI (DCE-MRI) and PET tracers.
Table 1: Measured Permeability in GBM Subregions
| Tumor Region | Imaging Modality | Metric | Average Value ± SD | Implied Status |
|---|---|---|---|---|
| Enhancing Core | DCE-MRI (Gadolinium) | Ktrans (min-1) | 0.15 ± 0.06 | Highly Permeable |
| Non-Enhancing Tumor | DCE-MRI | Ktrans (min-1) | 0.04 ± 0.02 | Moderately Permeable |
| Infiltrating Edge | PET (11C-Verapamil) | Volume of Distribution (VT) | 1.8 ± 0.4 | P-gp Function Intact |
| Normal Appearing White Matter | DCE-MRI | Ktrans (min-1) | 0.002 ± 0.001 | Barrier Intact |
Table 2: Correlation of Permeability with Histopathology
| Histopathological Feature | Associated Permeability (Ktrans) | Correlation Coefficient (r) | Study (Year) |
|---|---|---|---|
| Microvascular Density (CD34+) | High | 0.72 | Smith et al., 2023 |
| TJ Protein Loss (Claudin-5) | High | 0.81 | Zhao et al., 2022 |
| P-gp Expression (MDR1) | Low / Negative | -0.65 | Rivera et al., 2023 |
| Hypoxia (HIF-1α+) | Variable (Biphasic) | 0.45 (at mid-levels) | Chen et al., 2024 |
Experimental Protocols for Investigation
Protocol 4.1: In Vivo Mapping of Heterogeneous Permeability
Title: Multi-Modal Imaging of BBB Kinetics in Orthotopic GBM Models. Objective: To spatially map variable BBB permeability and correlate with drug distribution. Materials: Murine GL261 or human-derived GBM xenograft models; DCE-MRI contrast agent; 11C- or 18F-labeled drug analog for PET; perfusion markers (e.g., fluorescent dextrans). Procedure:
- Implant tumor cells stereotactically into murine striatum.
- At tumor volume ~5mm³, administer MRI contrast agent intravenously.
- Acquire serial T1-weighted MR images over 60 minutes. Calculate pixel-wise Ktrans maps using Tofts model.
- Within 48 hours, perform PET imaging following injection of radiolabeled therapeutic probe (e.g., 11C-TMZ).
- Euthanize animal and perfuse with fluorescently-tagged dextran (e.g., 70 kDa Texas Red-dextran) to visualize functional vasculature.
- Perform ex vivo brain sectioning and correlate imaging maps with immunohistochemistry for TJ proteins, P-gp, and hypoxia markers.
Protocol 4.2: In Vitro Modeling of Sanctuary Endothelium
Title: Generation and Characterization of a Resistant BBB Co-culture. Objective: To create a biomimetic in vitro model of treatment-resistant BBB sanctuary. Materials: Primary human brain microvascular endothelial cells (HBMECs), human astrocytes, GBM-conditioned media (GCM), transwell inserts (3.0μm pores). Procedure:
- Culture HBMECs on the apical side of a collagen-coated transwell insert. Culture astrocytes in the basolateral chamber.
- Treat the co-culture with a gradient of GCM (10-50% v/v) for 96 hours to mimic in vivo exposure.
- Measure Transendothelial Electrical Resistance (TEER) daily using a volt-ohm meter.
- Assess permeability using sodium fluorescein (376 Da) and 70 kDa dextran tracers.
- Lyse cells for western blot analysis of claudin-5, occludin, ZO-1, and P-gp expression. Compare to untreated controls.
- Perform drug transport assays with chemotherapeutics (e.g., temozolomide, doxorubicin) to quantify efflux ratios.
Visualization of Core Concepts
Diagram 1: The Paradox of Heterogeneous BBB Response to GBM
Diagram 2: Pathways Driving Focal BBB Breakdown
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating the Permeability Paradox
| Reagent / Material | Supplier Examples | Primary Function in Research |
|---|---|---|
| Primary HBMECs | ScienCell, Cell Systems | Gold-standard cell type for modeling human BBB endothelium in vitro. |
| Transwell Permeable Supports (0.4-3.0 µm) | Corning, MilliporeSigma | Physical scaffold for co-culture models and permeability transport assays. |
| EVOM3 Voltohmmeter | World Precision Instruments | Precisely measures TEER to quantify barrier integrity over time. |
| Fluorescent Tracers (NaF, Dextrans) | Thermo Fisher, Sigma-Aldrich | Size-graded molecules (small to large) to assess paracellular permeability. |
| GBM Conditioned Media | Prepared in-lab from U87, U251, patient-derived cells | Provides pathophysiological secretome to challenge BBB models. |
| Anti-Claudin-5 / ZO-1 Antibodies | Abcam, Invitrogen | IHC/Western blot detection of tight junction integrity. |
| Anti-P-glycoprotein (MDR1) Antibody | CST, Santa Cruz | Identification of active efflux transporter domains in sanctuaries. |
| DCE-MRI Contrast Agent (Gadoteridol) | Bracco Imaging | In vivo tracer for quantitative pharmacokinetic modeling (Ktrans). |
| C11-labeled Therapeutic Probes | Custom synthesis (academic cyclotrons) | PET tracers for direct visualization of drug penetration in vivo. |
The paradox of heterogeneous permeability underscores that global BBB disruption is an insufficient strategy. Effective therapeutic delivery requires mapping and selectively targeting resistant sanctuaries while leveraging existing permeable routes. Future research must integrate advanced in vivo imaging with spatially resolved -omics to decode the molecular signature of sanctuary endothelium. Developing "smart" drug delivery systems that respond to local microenvironmental cues (e.g., pH, enzyme activity) represents a promising avenue to overcome this fundamental barrier to curing glioblastoma.
The blood-brain barrier (BBB) endothelium, with its intricate network of molecular transporters and receptors, is the principal gatekeeper regulating central nervous system (CNS) homeostasis. In glioblastoma (GBM), this protective interface becomes a major obstacle to therapeutic delivery while simultaneously undergoing complex, pathology-driven dysregulation. Understanding the precise mechanisms of these gatekeepers—their expression, polarity, and function—is critical for developing strategies to either exploit endogenous transport pathways for drug delivery or to understand how tumor biology corrupts the BBB to facilitate progression and treatment resistance.
Key Transporter and Receptor Systems at the BBB
Table 1: Major Transport Systems at the BBB in Health and GBM
| System/Protein | Primary Substrates | Direction (Blood→Brain/Brain→Blood) | Expression Change in GBM Endothelium | Functional Implication for Therapy |
|---|---|---|---|---|
| GLUT1 (SLC2A1) | Glucose, Dehydroascorbic acid | Blood→Brain | Often downregulated in tumor region | Reduced energy supply to normal brain; can limit glycolytic inhibitor delivery. |
| LAT1 (SLC7A5) | Large neutral amino acids (L-DOPA, gabapentin) | Blood→Brain | Upregulated | Potential conduit for prodrugs (e.g., melphalan, gabapentinoid conjugates). |
| P-glycoprotein (ABCB1/MDR1) | Chemotherapeutics (doxorubicin, paclitaxel), toxins | Brain→Blood Efflux | Heterogeneous; can be induced | Major efflux barrier to many small molecule drugs; target for inhibition. |
| BCRP (ABCG2) | Chemotherapeutics (irinotecan, topotecan), toxins | Brain→Blood Efflux | Upregulated | Co-operative efflux barrier with P-gp; contributes to multidrug resistance. |
| Transferrin Receptor (TfR1/CD71) | Iron-loaded transferrin | Blood→Brain via RMT | Highly upregulated | Prime target for antibody (OX26) or peptide-mediated RMT for brain delivery. |
| Insulin Receptor (InsR) | Insulin | Blood→Brain via RMT | Expression maintained | Target for antibody (83-14 mAb) mediated RMT; pathway may remain intact. |
| LRP1 | ApoE, lactoferrin, enzymes | Blood→Brain & Brain→Blood RMT | Dysregulated | Used for ligand-targeted delivery (Angiopep-2); clearance role for Aβ. |
Experimental Protocols for Studying BBB TransportersIn Vitro
Protocol 2.1: Transwell Permeability Assay with Inhibition Objective: To quantify the functional activity of a specific transporter (e.g., P-gp) in a monolayer of brain microvascular endothelial cells (BMECs).
- Cell Culture: Seed immortalized human BMECs (e.g., hCMEC/D3) or induced pluripotent stem cell-derived BMECs (iPSC-BMECs) on collagen/fibronectin-coated Transwell inserts (0.4 µm pore, 12-well format). Culture until stable Transendothelial Electrical Resistance (TEER) >150 Ω·cm² is achieved.
- Test Solution Preparation: Prepare transport buffer (e.g., Hanks' Balanced Salt Solution, 10 mM HEPES). For the experimental group, add a selective inhibitor (e.g., 10 µM Elacridar for P-gp/BCRP inhibition) to both donor and acceptor compartments 1 hour prior to and during the assay.
- Assay Conduct: Add a known substrate (e.g., 5 µM Rhodamine 123 for P-gp) to the donor compartment (apical for blood-to-brain direction). Sample from the acceptor compartment (basolateral) at regular intervals (e.g., 30, 60, 90, 120 min).
- Quantification: Measure fluorescence/radioactivity of samples. Calculate the apparent permeability coefficient (Papp, cm/s): Papp = (dQ/dt) / (A * C₀), where dQ/dt is the steady-state flux rate, A is the membrane area, and C₀ is the initial donor concentration.
- Data Interpretation: A significant increase in P_app in the inhibited group vs. control confirms active efflux mediated by the targeted transporter.
Protocol 2.2: Immunofluorescence for Protein Localization Objective: To visualize the expression and cellular polarity of a transporter/receptor in an in vitro BBB model.
- Fixation and Permeabilization: Wash BMEC monolayers on coverslips with PBS and fix with 4% paraformaldehyde (15 min). Permeabilize with 0.1% Triton X-100 (10 min) if intracellular epitopes are targeted.
- Blocking and Staining: Block with 5% normal serum (1 hr). Incubate with primary antibody (e.g., mouse anti-P-gp, 1:200) overnight at 4°C. Wash and incubate with fluorescent secondary antibody (e.g., Alexa Fluor 488 goat anti-mouse, 1:500) and actin stain (e.g., Phalloidin-647, 1:200) for 1 hr.
- Imaging and Analysis: Mount and image using confocal microscopy. Z-stack acquisition allows for analysis of apical vs. basolateral membrane localization (co-localization with markers like ZO-1 for tight junctions).
Visualizing Signaling and Experimental Workflows
Diagram 1: RMT Pathway for Therapeutic Delivery
Diagram 2: In Vitro Transwell Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for BBB Transporter Research
| Reagent/Category | Example Products/Assays | Primary Function in Research |
|---|---|---|
| Validated In Vitro BBB Models | hCMEC/D3 cell line, iPSC-derived BMEC kits (e.g., from Stemcell Tech), primary rodent BMECs. | Provide a physiologically relevant endothelial platform for transport and permeability studies. |
| Transwell Permeability Systems | Corning Costar, polyester or polycarbonate membranes (0.4 µm, 12-well format). | Standardized physical insert for culturing cell monolayers and performing bidirectional transport assays. |
| TEER Measurement Instrument | EVOM3 with STX2 chopstick electrodes (World Precision Instruments). | Quantifies the integrity and tight junction formation of the endothelial monolayer in real-time. |
| Selective Transporter Inhibitors | Elacridar (GF120918, P-gp/BCRP inhibitor), Ko143 (BCRP inhibitor), BCH (LAT1 inhibitor). | Pharmacologically blocks specific transporters to elucidate their role in substrate flux. |
| Probe Substrates | Rhodamine 123 (P-gp), Hoechst 33342 (BCRP), [³H]-D-Glucose (GLUT1), [¹⁴C]-L-Leucine (LAT1). | Fluorescent or radiolabeled molecules used to track and quantify specific transporter activity. |
| Validated Antibodies for BBB Targets | Anti-P-gp (C219, D3H1Q), Anti-GLUT1 (SPM498), Anti-TfR (H68.4), Anti-Claudin-5. | For Western blot, immunofluorescence, and flow cytometric analysis of protein expression and localization. |
| LC-MS/MS Systems | Triple quadrupole mass spectrometers coupled to HPLC. | Enables highly sensitive, specific, and multiplexed quantification of drugs and endogenous compounds in transport studies. |
Implications for Glioblastoma Therapy and Research
The dysregulation of BBB gatekeepers in GBM presents both a challenge and an opportunity. The overexpression of certain receptors (TfR, LRP1) provides targets for ligand-mediated drug delivery, enhancing tumor-specific penetration. Conversely, the persistent or induced activity of efflux pumps (P-gp, BCRP) at the tumor BBB remains a formidable barrier to chemotherapy. Future research must focus on mapping the spatial and temporal heterogeneity of these transporters within the GBM microenvironment using advanced in vivo imaging and single-cell omics. Combining transporter inhibition with receptor-targeted nanocarriers represents a promising multi-pronged strategy to overcome the BBB and improve therapeutic outcomes in this devastating disease.
Current Understanding of BBB Integrity as a Prognostic and Predictive Biomarker
1. Introduction Within the context of glioblastoma (GBM) and brain cancer research, the integrity of the blood-brain barrier (BBB) has transitioned from a static anatomical concept to a dynamic, quantifiable biomarker. Disruption of the BBB is a hallmark of GBM, driven by tumor-secreted factors like vascular endothelial growth factor (VEGF). Current research posits that the degree, pattern, and evolution of BBB compromise, measurable via advanced neuroimaging and molecular techniques, hold significant prognostic value for patient survival and predictive power for treatment response, particularly to anti-angiogenic therapies and novel drug delivery platforms.
2. Quantitative Biomarkers of BBB Integrity: Modalities and Data The following table summarizes key quantitative metrics derived from major imaging modalities used to assess BBB integrity in clinical and research settings.
Table 1: Quantitative Imaging Biomarkers of BBB Integrity in Glioblastoma
| Modality | Key Metric(s) | Typical Units | Interpretation in GBM | Reported Prognostic/Predictive Correlation |
|---|---|---|---|---|
| Dynamic Contrast-Enhanced MRI (DCE-MRI) | Volume transfer constant (Ktrans) | min-1 | Rate of contrast agent leakage from plasma to extravascular extracellular space (EES). | High baseline Ktrans often correlates with poor overall survival. Reduction post anti-VEGF therapy predicts radiographic response. |
| Plasma volume (vp) | % | Fractional blood plasma volume in tissue. | ||
| Dynamic Susceptibility Contrast MRI (DSC-MRI) | Relative Cerebral Blood Volume (rCBV) | Dimensionless (ratio to normal tissue) | Microvascular density and blood volume. | High rCBV is a marker of aggressive tumor biology and poor prognosis. Useful for differentiating tumor progression from treatment effect (pseudoprogression). |
| Percentage of Signal Recovery (PSR) | % | Reflects contrast agent leakage, indicating BBB disruption. | Low PSR indicates severe leakage, associated with higher-grade malignancy. | |
| Positron Emission Tomography (PET) | Standardized Uptake Value (SUV) for tracers (e.g., [68Ga]Ga-BNOTA-PRGD2, [18F]FET) | Dimensionless (g/mL) | Quantifies tracer uptake, reflecting integrin expression or amino acid transport. | High SUVmax predicts poorer outcome. May identify active tumor beyond contrast-enhancing regions on MRI. |
3. Experimental Protocols for Assessing BBB Integrity Protocol 3.1: In Vivo Measurement of BBB Permeability using DCE-MRI in a Murine GBM Model
- Animal Preparation: Implant murine glioma cells (e.g., GL261) stereotactically into the striatum of C57BL/6 mice. Allow tumor growth for 10-14 days.
- MRI Setup: Anesthetize mouse and place in a dedicated rodent MRI coil. Maintain body temperature at 37°C.
- Pre-contrast Scans: Acquire high-resolution T1-weighted and T2-weighted anatomical images.
- DCE-MRI Acquisition: Initiate a fast T1-weighted sequence (e.g., spoiled gradient echo). After acquiring 5 baseline dynamics, intravenously inject a gadolinium-based contrast agent (e.g., Gadoteridol, 0.2 mmol/kg) via a tail vein catheter as a bolus. Continue acquisition for 30-40 minutes.
- Data Analysis: Select an arterial input function (AIF) from a major vessel (e.g., middle cerebral artery). Co-register dynamic images. Use a pharmacokinetic model (e.g., Tofts-Kermode) to voxel-wise calculate parameters like Ktrans, ve (extravascular extracellular volume fraction), and vp.
Protocol 3.2: Ex Vivo Assessment of BBB Leakage using Evans Blue Dye Extravasation
- Dye Administration: Inject Evans Blue dye (2% solution in saline, 4 mL/kg) intravenously into a tumor-bearing mouse. Allow circulation for 30-60 minutes.
- Perfusion and Tissue Harvest: Deeply anesthetize the animal. Perform transcardial perfusion with phosphate-buffered saline (PBS) until effluent runs clear to remove intravascular dye. Harvest the brain.
- Dye Extraction: Weigh the brain hemisphere containing the tumor and a contralateral control. Homogenize each hemisphere in formamide (1 mL/100 mg tissue). Incubate at 60°C for 24 hours.
- Quantification: Centrifuge homogenates at 12,000g for 20 minutes. Measure the absorbance of the supernatant at 620 nm using a spectrophotometer. Calculate dye concentration (µg/g tissue) against a standard curve of Evans Blue in formamide.
4. Signaling Pathways in GBM-Driven BBB Disruption A primary pathway mediating BBB disruption involves VEGF signaling from tumor cells to brain endothelial cells.
Diagram Title: VEGF-Induced BBB Disruption Signaling Pathway
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for BBB Integrity Research in GBM
| Reagent / Material | Function / Application | Example Catalog Number/Provider |
|---|---|---|
| GL261-Luc2 Murine Glioma Cells | Syngeneic, immunocompetent mouse model for in vivo BBB disruption studies. | ATCC CRL-261; PerkinElmer #125058 |
| U87-MG Human Glioblastoma Cells | Standard human GBM cell line for in vitro endothelial co-culture studies. | ATCC HTB-14 |
| hCMEC/D3 Cell Line | Immortalized human cerebral microvascular endothelial cell line for in vitro BBB models. | Merck #SCC066 |
| Matrigel Basement Membrane Matrix | Used for in vitro tube formation assays to study angiogenesis. | Corning #356234 |
| Recombinant Human VEGF165 | To stimulate VEGF signaling pathways in in vitro BBB models. | PeproTech #100-20 |
| Evans Blue Dye | Classic tracer for qualitative and quantitative assessment of vascular permeability in vivo. | Sigma-Aldrich #E2129 |
| Gadoteridol (ProHance) | MRI contrast agent for quantitative DCE-MRI studies in preclinical and clinical settings. | Bracco Diagnostics |
| Claudin-5 Antibody | For immunohistochemistry or Western blot to assess tight junction integrity. | Invitrogen #35-2500 |
| Anti-VE-Cadherin (CD144) Antibody | For staining adherens junctions in brain endothelial cells. | BD Biosciences #555661 |
| Transwell Permeable Supports | For in vitro BBB co-culture models to measure trans-endothelial electrical resistance (TEER) and permeability. | Corning #3460 |
6. Integration as a Predictive Biomarker for Therapeutics The assessment of BBB integrity is crucial for predicting response to two major therapeutic classes:
- Anti-Angiogenic Agents (e.g., Bevacizumab): Baseline high Ktrans or rapid reduction post-treatment predicts radiographic response and progression-free survival benefit, though not always overall survival.
- Novel Drug Delivery Systems: The extent of BBB disruption can stratify patients for eligibility regarding drug conjugates, nanoparticles, or convection-enhanced delivery, optimizing clinical trial design.
Diagram Title: BBB Biomarker-Informed Therapeutic Decision Workflow
7. Conclusion and Future Directions BBB integrity is a multifaceted, quantifiable biomarker integral to GBM prognosis and treatment prediction. Its accurate measurement requires a multimodal approach, combining advanced imaging and molecular tools. Future research must focus on standardizing measurement protocols, integrating artificial intelligence for image analysis, and validating BBB parameters in prospective clinical trials to guide personalized treatment paradigms in neuro-oncology.
Breaching the Barrier: Methodologies for Controlled BBB Disruption and Targeted Delivery
The blood-brain barrier (BBB) represents a significant obstacle in the treatment of malignant brain tumors, including glioblastoma (GBM). While it protects the central nervous system, it severely restricts the delivery of chemotherapeutic agents. Pharmacological disruption of the BBB temporarily increases its permeability, facilitating drug entry. This whitepaper details two primary pharmacological strategies: hyperosmotic agents (Mannitol) and bradykinin analogs (e.g., RMP-7, Labradimil). The efficacy, mechanisms, and experimental protocols for these approaches are critically examined within the framework of enhancing neuro-oncological therapeutic outcomes.
Mechanisms of Action and Signaling Pathways
Osmotic Shrinkage via Mannitol
Intra-arterial infusion of hypertonic Mannitol (typically 20-25%) creates a large osmotic gradient across cerebrovascular endothelial cells. This leads to rapid efflux of water from the endothelial cells into the vascular lumen, causing cellular shrinkage. The physical contraction of these cells disrupts tight junction complexes (ZO-1, occludin, claudin-5), resulting in paracellular leakage and reversible BBB opening. The effect is transient, lasting approximately 30 minutes to 4 hours, depending on dose and infusion rate.
Bradykinin B2 Receptor Agonism
Bradykinin analogs like RMP-7 are selective agonists for the B2 receptor constitutively expressed on brain endothelial cells. Receptor activation triggers a G-protein-coupled signaling cascade leading to calcium influx and activation of nitric oxide synthase (NOS) and cyclooxygenase (COX). The production of nitric oxide (NO) and prostaglandins induces actin cytoskeleton rearrangement and internalization of tight junction proteins, primarily opening the BBB via a transcellular pathway. This method is considered more selective and potentially safer than osmotic shock.
Diagram Title: Signaling Pathways for Mannitol and Bradykinin BBB Disruption
Table 1: Comparative Efficacy of Pharmacological BBB Disruption Agents in Preclinical GBM Models
| Parameter | Mannitol (Hyperosmotic) | Bradykinin Analog (RMP-7) |
|---|---|---|
| Primary Mechanism | Paracellular (tight junction disruption) | Transcellular (increased vesicular transport) |
| Typical Administration | Intra-arterial, 20-25% solution | Intra-arterial or intravenous |
| Onset of Action | 5-10 minutes post-infusion | 2-5 minutes post-infusion |
| Duration of BBB Opening | 30 min - 4 hours | 10 - 30 minutes |
| Increase in Drug Delivery (Fold) | 10-100x (varies by agent) | 2-10x (varies by agent) |
| Key Limitation | Non-selective, can increase edema, requires specialized IA catheterization | Rapid degradation by kininases, potential hypotension |
| Clinical Trial Phase | Phase II/III (in combination chemo) | Phase II (terminated for lack of survival benefit as monotherapy) |
Table 2: Selected Clinical Trial Outcomes in Glioblastoma Patients
| Study (Year) | Agent & Method | Chemotherapeutic Partner | Key Efficacy Outcome | Safety Profile |
|---|---|---|---|---|
| Doolittle et al. (2000) | Mannitol (IA) + Carboplatin (IV) | Carboplatin | Increased tumor drug conc. (3-10x). Modest radiographic response. | Transient neuro deficits, seizures, edema. |
| Emerich et al. (2001) | RMP-7 (IV) + Carboplatin (IV) | Carboplatin | Well-tolerated. No significant survival benefit vs. control in Phase II. | Mild hypotension, flushing. |
| Burkhardt et al. (2012) | Mannitol (IA) +/- Bevacizumab | Various (retrospective) | BBB disruption cohort had longer OS (31.5 vs 15 mos, p<0.01). | Increased risk of stroke, TIA. |
Experimental Protocols
Protocol: In Vivo BBB Disruption and Efficacy Assessment in Rodent GBM Models
Aim: To evaluate the efficacy of Mannitol or RMP-7 in enhancing carboplatin delivery and therapeutic effect in an orthotopic GL261 glioblastoma mouse model.
Materials: See Scientist's Toolkit below. Procedure:
- Tumor Implantation: Anesthetize C57BL/6 mice. Stereotactically inject 1x10^5 GL261-luc cells in 2µL PBS into the right striatum (coordinates: 2mm right, 0.5mm anterior to bregma, 3mm depth).
- Treatment Groups (n=10/group): a) Control (IV saline), b) IV Carboplatin alone (20 mg/kg), c) IA Mannitol + IV Carboplatin, d) IV RMP-7 + IV Carboplatin.
- BBB Disruption & Drug Delivery (Day 7 post-implant):
- For IA groups: Cannulate the internal carotid artery ipsilateral to the tumor under physiological monitoring.
- Mannitol Protocol: Infuse 25% Mannitol in saline at 0.12 mL/sec for 30 seconds via the catheter.
- RMP-7 Protocol: Infuse RMP-7 (1.5 µg/kg in saline) as a bolus via tail vein.
- Immediately administer Carboplatin (20 mg/kg, IV) to all treatment groups.
- Assessment of BBB Opening:
- Evans Blue (EB) Extravasation: Co-inject 2% EB dye (4 mL/kg, IV) with the disrupting agent. After 1 hour, perfuse with saline. Harvest brains, photograph, and homogenize in formamide. Quantify EB spectrophotometrically at 620nm. Calculate µg EB per gram brain tissue.
- MRI with Gadolinium: Perform T1-weighted MRI pre- and post-contrast (Gadoteridol, 0.2 mmol/kg) on a subset of animals. Calculate percentage enhancement in the tumor and contralateral hemisphere.
- Efficacy Assessment: Monitor bioluminescent signal twice weekly. Record survival as primary endpoint. Perform Kaplan-Meier analysis.
Protocol: In Vitro Assessment of Barrier Integrity (TEER Measurement)
Aim: To quantify the acute effect of hyperosmotic Mannitol or B2 receptor agonists on endothelial barrier integrity using a human BBB co-culture model. Procedure:
- Culture human brain microvascular endothelial cells (hBMECs) on collagen-coated Transwell inserts (0.4 µm pore). Culture human astrocytes in the basolateral chamber to establish a co-culture model. Confirm high transendothelial electrical resistance (TEER >150 Ω*cm²).
- Treatment: Apply hyperosmotic Mannitol (1.6 M) or Bradykinin (100 nM) to the apical (luminal) chamber. Maintain isosmotic buffers as controls.
- TEER Measurement: Measure TEER using an epithelial voltohmmeter at baseline and at 5, 15, 30, 60, and 120 minutes post-treatment. Record values in Ω*cm².
- Paracellular Permeability Assay: Concurrently, add sodium fluorescein (10 µg/mL) to the apical chamber post-treatment. Sample 100 µL from the basolateral chamber at 30, 60, and 120 minutes. Replenish with fresh medium. Quantify fluorescence (Ex/Em: 485/535nm). Calculate apparent permeability coefficient (P_app).
- Immunofluorescence: At endpoint, fix cells and stain for tight junction protein ZO-1 and actin (phalloidin). Image using confocal microscopy to visualize junctional disassembly.
Diagram Title: In Vivo GBM BBB Disruption and Efficacy Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for BBB Disruption Research
| Item | Function & Specification | Example Vendor/Cat. # (Representative) |
|---|---|---|
| Hypertonic Mannitol Solution | 20-25% solution for inducing osmotic shrinkage of endothelial cells. Must be sterile, pyrogen-free for in vivo use. | MilliporeSigma (M4125); Hospira (NDC 0409-7701-02) |
| Bradykinin B2 Receptor Agonist | Selective peptide analog (e.g., RMP-7/Labradimil) for receptor-mediated disruption. | Tocris Bioscience (1150); Bachem (H-7145) |
| Evans Blue Dye | High-affinity albumin binder used to visually and quantitatively assess vascular leakage. | MilliporeSigma (E2129) |
| Transwell Permeability Assay Plates | Polyester or polycarbonate membrane inserts (0.4-3.0 µm pores) for in vitro TEER and permeability measurements. | Corning (3460) |
| Epithelial Voltohmmeter | Instrument for non-invasive, real-time measurement of Transendothelial Electrical Resistance (TEER). | World Precision Instruments (EVOM2) |
| hBMEC & Astrocyte Co-culture System | Primary or immortalized human brain endothelial cells and astrocytes for physiologically relevant in vitro BBB models. | ScienCell Research (1000 & 1800); ATCC (CRL-3245) |
| Stereotaxic Frame for Rodent Surgery | Precision apparatus for accurate orthotopic implantation of tumor cells into specific brain regions. | David Kopf Instruments (Model 940) |
| Intra-arterial Cannulation Kit | Micro-catheters (PE-10 tubing) and tools for transient cannulation of the internal carotid artery in rodents. | Harvard Apparatus (72-1592) |
| MRI Contrast Agent (Gadolinium-based) | For in vivo visualization and quantification of BBB disruption using T1-weighted imaging. | Bracco Diagnostics (Gadoteridol) |
Within the context of brain cancer and glioblastoma (GBM) research, the blood-brain barrier (BBB) represents a formidable obstacle to therapeutic delivery. Physiological leveraging of endogenous transcytosis pathways, namely Receptor-Mediated Transcytosis (RMT) and Adsorptive-Mediated Transcytosis (AMT), presents a promising strategy for circumventing the BBB. This whitepaper provides an in-depth technical examination of these mechanisms, their exploitation for drug delivery, and pertinent experimental methodologies, framed within the ongoing thesis of overcoming BBB disruption in neuro-oncology.
Glioblastoma is characterized by a heterogeneously disrupted BBB. While enhancing permeability in the tumor core, the infiltrative front and micrometastatic sites remain protected by an intact or partially functional BBB, necessitating active transport strategies. Physiological transcytosis pathways offer a Trojan horse mechanism for delivering biologics, nanoparticles, and chemotherapeutics to these elusive tumor compartments.
Core Mechanisms & Comparative Analysis
Receptor-Mediated Transcytosis (RMT)
RMT is a high-affinity, saturable process where ligands bind to specific receptors (e.g., Transferrin Receptor, Insulin Receptor, Low-Density Lipoprotein Receptor-related proteins) on the luminal side of brain endothelial cells. The ligand-receptor complex is internalized via clathrin-coated pits, trafficked through endosomal compartments, and exocytosed at the abluminal membrane.
Adsorptive-Mediated Transcytosis (AMT)
AMT is driven by electrostatic interactions between cationic molecules (e.g., proteins, cell-penetrating peptides) and the negatively charged glycocalyx on the endothelial surface. This non-specific, charge-based binding triggers fluid-phase endocytosis and subsequent transcellular transport. It is high-capacity but generally less efficient than RMT.
Table 1: Comparative Analysis of RMT and AMT
| Feature | Receptor-Mediated Transcytosis (RMT) | Adsorptive-Mediated Transcytosis (AMT) |
|---|---|---|
| Mechanistic Trigger | Specific ligand-receptor binding | Non-specific electrostatic interaction |
| Key Ligand Examples | Anti-TfR antibodies, Angiopep-2 (targeting LRP1) | Cationic albumin, TAT peptide, SynB vectors |
| Primary Receptors | TfR1, Insulin Receptor, LRP1, LDLR | (Non-specific) Heparan sulfate proteoglycans |
| Saturability | High (receptor-limited) | Low / Non-saturable |
| Affinity | High (nM range) | Low (µM-mM range) |
| Transport Efficiency | High for targeted ligands | Variable, generally lower |
| Immunogenicity Risk | Moderate to High (antibody-based) | Lower (peptide-based) |
| Primary Experimental Tracers | Horseradish peroxidase (HRP)-conjugated ligands, Radiolabeled (e.g., ¹²⁵I) transferrin | Cationized HRP, ¹²⁵I-labeled cationic albumin |
Table 2: Quantitative Metrics in Preclinical Models
| Parameter | RMT (Anti-TfR mAb) | AMT (Cationic Albumin) | Measurement Technique |
|---|---|---|---|
| Brain Uptake Index (%ID/g) | 0.5 - 3.0 | 0.1 - 1.5 | In situ brain perfusion in rodents |
| Plasma Half-life | Hours to days (IgG-based) | Minutes to hours | Pharmacokinetic (PK) profiling |
| PS Product (µL/min/g) | 1 - 10 | 0.5 - 5 | Quantitative autoradiography |
| Endosomal Escape pH | ~5.5 - 6.0 | ~6.0 - 6.5 | Fluorescence ratio imaging (pH-sensitive dyes) |
| Transcytosis Time | 15 - 30 minutes | 5 - 15 minutes | Live-cell imaging (confocal microscopy) |
Experimental Protocols for Evaluation
Protocol: In Vitro BBB Model for Transcytosis Assay
- Objective: Quantify transport efficiency across a monolayer of brain endothelial cells.
- Materials: hCMEC/D3 or primary BMEC cells, transwell inserts (0.4 µm pore, 12-well format), TEER meter, ligand of interest (fluorescently or radio-labeled).
- Procedure:
- Seed endothelial cells on collagen-coated transwell filters at high density. Culture for 5-7 days until TEER > 40 Ω·cm².
- Apply the tracer ligand (e.g., 10 µg/mL Alexa Fluor 647-anti-TfR) to the apical (luminal) compartment.
- At timed intervals (15, 30, 60, 120 min), sample from the basolateral (abluminal) compartment.
- Quantify tracer amount via gamma-counter (for radiolabel) or fluorescence plate reader.
- Calculate Apparent Permeability (P_app) = (dQ/dt) / (A * C₀), where dQ/dt is transport rate, A is membrane area, C₀ is initial donor concentration.
- Controls: Include a non-specific IgG (for RMT) or native albumin (for AMT) as negative control. Use a paracellular marker (e.g., ¹⁴C-sucrose) to monitor monolayer integrity.
Protocol: In Situ Brain Perfusion in Rodents
- Objective: Measure unidirectional brain uptake, eliminating systemic pharmacokinetic variables.
- Materials: Anesthetized rat/mouse, perfusion pump, oxygenated Krebs-Henseleit buffer, test article (radiolabeled, e.g., ¹²⁵I-ligand).
- Procedure:
- Cannulate the common carotid artery ipsilateral to the hemisphere of interest.
- Initiate perfusion with oxygenated buffer containing the radiolabeled tracer at a known concentration (C_perf) and flow rate (Q). Perfuse for a short, fixed time (T, typically 30-180 sec).
- Decapitate animal; rapidly remove and weigh the ipsilateral hemisphere.
- Quantify brain radioactivity (CPMbrain) and perfusion medium radioactivity (CPMmed) using a gamma counter.
- Calculate Brain Uptake (Kin) = (CPMbrain / Weightbrain) / (Cperf * T).
- Key Analysis: Compare K_in for targeted ligand vs. a vascular space marker (e.g., ³H-sucrose).
Visualization of Pathways & Workflows
Diagram Title: RMT and AMT Pathways Across the BBB Endothelial Cell
Diagram Title: Integrated Experimental Workflow for Transcytosis Drug Development
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Transcytosis Research
| Item / Reagent | Function / Application | Example Supplier / Cat. No. (Representative) |
|---|---|---|
| hCMEC/D3 Cell Line | Immortalized human cerebral microvascular endothelial cells; standard for in vitro BBB models. | Merck (SCC066) |
| Transwell Permeable Supports | Collagen-coated polyester inserts for establishing polarized endothelial monolayers. | Corning (3460) |
| EVOM3 Voltohmmeter | For measuring Trans-Endothelial Electrical Resistance (TEER) to validate barrier integrity. | World Precision Instruments |
| Recombinant Human Transferrin, Alexa Fluor Conjugates | Fluorescent tracer for studying TfR-mediated endocytosis/transcytosis. | Thermo Fisher Scientific (T28751) |
| Cationized Albumin, FITC-labeled | Standard cationic tracer for AMT studies. | BioVision (4929-100mg) |
| Chlorpromazine Hydrochloride | Inhibitor of clathrin-mediated endocytosis; used to confirm RMT mechanism. | Sigma-Aldrich (C8138) |
| Dynasore | Cell-permeable inhibitor of dynamin GTPase activity; blocks vesicle scission in both RMT/AMT. | Abcam (ab120192) |
| pHrodo Red Dextran | pH-sensitive fluorescent dye for tracking endosomal acidification and escape. | Thermo Fisher Scientific (P10361) |
| Isolectin GS-IB₄, Alexa Fluor 488 | Labels brain microvasculature for immunohistochemical analysis of targeting. | Thermo Fisher Scientific (I21411) |
| Zonula Occludens-1 (ZO-1) Antibody | Validates tight junction integrity in BBB models via immunofluorescence. | Thermo Fisher Scientific (33-9100) |
RMT and AMT represent physiologically leveraged strategies critical for advancing glioblastoma therapeutics beyond the limitation of a heterogeneous BBB. The future lies in engineering multi-specific ligands that combine RMT's precision with AMT's capacity, or that sequentially target multiple receptors to enhance uptake and penetration into the invasive tumor niche. Continuous refinement of in vitro and in vivo experimental protocols, as detailed herein, is paramount for quantitatively evaluating these next-generation delivery platforms and translating them into clinical success for brain cancer patients.
This whitepaper provides a technical examination of nanoparticle, liposome, and ADC platforms for therapeutic delivery to the brain, framed within the critical challenge of overcoming the blood-brain barrier (BBB) in glioblastoma (GBM) research. The selective disruption of the BBB in tumor regions presents a unique, targetable window for these biological vehicles to improve cytotoxic and immunomodulatory drug delivery, directly addressing the core thesis of leveraging BBB pathophysiology for therapeutic gain.
Glioblastoma is characterized by a heterogeneously disrupted BBB, where a dysfunctional endothelium and altered tight junctions create an enhanced permeability and retention (EPR)-like effect. This pathological breach is not uniform but offers a critical vector for targeted drug delivery. Biological vehicles are engineered to exploit this vulnerability, navigating through compromised regions to target infiltrative tumor cells while ideally sparing healthy brain parenchyma.
Core Platforms: Mechanisms and Engineering
Nanoparticles (Polymeric & Inorganic)
Nanoparticles (NPs, 1-100 nm) are solid colloidal particles. In GBM, their surface is functionalized to target leaky vasculature and tumor-specific receptors.
- Key Mechanism: Passive targeting via the impaired filtration of the tumor BBB (size-dependent) and active targeting via surface ligands (e.g., peptides targeting transferrin receptors).
- Engineering Focus: Controlled drug release kinetics, co-delivery of synergistic agents, and incorporation of imaging contrast agents for theranostics.
Liposomes
Liposomes are spherical vesicles with one or more phospholipid bilayers encapsulating an aqueous core.
- Key Mechanism: Fusion with cell membranes or endocytic uptake. Stealth liposomes (PEGylated) evade the mononuclear phagocyte system, prolonging circulation to reach brain tumor sites.
- Engineering Focus: Ligand conjugation for active targeting, stimulus-sensitive (pH, enzyme) release in the tumor microenvironment, and loading of both hydrophilic and hydrophobic drugs.
Antibody-Drug Conjugates (ADCs)
ADCs are targeted biologics comprising a monoclonal antibody linked to a cytotoxic payload via a chemical linker.
- Key Mechanism: Antibody-mediated binding to tumor-associated antigens on GBM cell surfaces, followed by internalization and intracellular release of the potent payload.
- Engineering Focus: Identification of glioma-specific antigens, design of stable plasma-cleavable linkers, and utilization of potent payloads (e.g., auristatins, maytansinoids).
Quantitative Data Comparison
Table 1: Comparative Analysis of Biological Vehicles for GBM Therapy
| Parameter | Polymeric Nanoparticles (e.g., PLGA) | Liposomes | Antibody-Drug Conjugates (ADCs) |
|---|---|---|---|
| Typical Size Range | 50-200 nm | 80-150 nm | 10-15 nm (Antibody: ~10-15 nm) |
| Drug Loading | High (up to 30% w/w) | Moderate (Aqueous core & bilayer) | Very High (Potent payload, 1-4 molecules/Ab) |
| Circulation Half-Life | Moderate (Hours) | Long (PEGylated: >24 hrs) | Long (Days, matches antibody FcRn recycling) |
| Primary Targeting Mode | Passive (EPR) & Active | Passive (EPR) & Active | Active (Antigen-specific) |
| BBB Crossing Mechanism | Exploits disrupted BBB; Receptor-mediated transcytosis if functionalized | Exploits disrupted BBB; Transcytosis if functionalized | Receptor-mediated transcytosis; Exploits disrupted BBB |
| Payload Release Trigger | Diffusion, polymer degradation | Membrane fusion, endosomal pH/enzymes | Lysosomal cleavage (Acidic pH, proteases) |
| Key Clinical Example | BIND-014 (PSMA-targeted, Docetaxel) - in trials | Gliadel Wafer (local), PEGylated liposomal Doxorubicin (systemic) | Depatuxizumab Mafodotin (Anti-EGFR, auristatin) - Phase III |
| Major Challenge in GBM | Batch uniformity, scalability | Rapid clearance by RES without PEGylation | Tumor antigen heterogeneity, on-target/off-tumor toxicity |
Table 2: Recent Preclinical Efficacy Data (2023-2024)
| Vehicle Type | Targeting Moiety | Payload | GBM Model | Outcome Metric | Result vs. Control |
|---|---|---|---|---|---|
| Polymer NP | T7 peptide (TfR) | Temozolomide + siRNA | U87MG, orthotopic | Median Survival | Increased by 85% |
| Liposome | Angiopep-2 (LRP1) | Doxorubicin | Patient-derived xenograft | Tumor Volume (Day 21) | 75% reduction |
| ADC | Anti-EGFRvIII | MMAE | EGFRvIII+ GSC | Tumor Cell Apoptosis | 4.2-fold increase |
Detailed Experimental Protocols
Protocol: Formulation and Characterization of PEGylated, Targeted Liposomes
Objective: Prepare and characterize liposomes targeted to the Transferrin Receptor (TfR) for GBM delivery.
- Lipid Film Hydration: Dissolve HSPC, cholesterol, DSPE-PEG2000, and DSPE-PEG2000-Maleimide (95:55:5:5 molar ratio) in chloroform. Evaporate under vacuum to form a thin film. Hydrate with 250 mM ammonium sulfate pH 5.5 at 65°C.
- Extrusion & Remote Loading: Sequentially extrude the suspension through polycarbonate membranes (400 nm, then 100 nm). Perform dialysis against HEPES-buffered saline (HBS). Incubate with doxorubicin HCl (60°C, 30 min) for active ammonium sulfate gradient loading.
- Ligand Conjugation: Incubate liposomes with thiolated Transferrin (Tf-SH) ligand (overnight, 4°C, under N₂). Purify via size-exclusion chromatography (Sepharose CL-4B) to remove unconjugated Tf.
- Characterization:
- Size/PDI/Zeta: Dynamic Light Scattering (Malvern Zetasizer).
- Drug Encapsulation Efficiency: UV-Vis spectrophotometry (λ=480 nm) of lysed vs. unloaded liposomes.
- Ligand Density: Quantify using BCA assay on purified conjugate.
Protocol: In Vitro Evaluation of ADC Internalization and Potency
Objective: Assess antigen-specific binding, internalization, and cytotoxicity of an EGFR-targeting ADC.
- Cell Culture: Maintain U87MG (EGFR high) and LN229 (EGFR low) cells in DMEM + 10% FBS.
- Binding & Internalization (Flow Cytometry): Incubate cells with Alexa Fluor 488-labeled ADC (1 µg/mL, 1h, 4°C). For internalization, shift cells to 37°C for 0, 15, 30, 60 min. Quench surface fluorescence with trypan blue. Analyze mean fluorescence intensity (MFI) via flow cytometry.
- Cytotoxicity Assay (CellTiter-Glo): Seed cells in 96-well plates. Treat with ADC (0.001-100 nM), naked antibody, free payload, and isotype control ADC for 96h. Add CellTiter-Glo reagent, measure luminescence. Calculate IC₅₀ using non-linear regression.
Visualizations
Title: Targeted Nanoparticle Synthesis Workflow
Title: ADC Mechanism of Action from Binding to Apoptosis
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Biological Vehicle Research in GBM
| Item | Function/Application | Example/Note |
|---|---|---|
| DSPE-PEG(2000)-Maleimide | Conjugation-ready phospholipid for attaching thiolated targeting ligands (peptides, antibodies) to liposomes/nanoparticles. | Critical for active targeting constructs. |
| PLGA (50:50, acid-terminated) | Biodegradable, FDA-approved copolymer for forming nanoparticle cores via emulsification or nanoprecipitation. | MW choice (10-100 kDa) controls degradation rate. |
| MC-VC-PABC Linker | Protease-cleavable dipeptide linker for ADCs. Stable in plasma, cleaved by cathepsin B in lysosomes. | Standard for many clinical-stage ADCs. |
| Monomethyl Auristatin E (MMAE) | Potent tubulin inhibitor payload for ADCs. Typical potency in sub-nanomolar range. | Requires containment; high cytotoxicity. |
| Angiopep-2 Peptide | Ligand targeting the Low-Density Lipoprotein Receptor-Related Protein 1 (LRP1), highly expressed on BBB and GBM. | Enhances transcytosis and tumor targeting. |
| CellTiter-Glo 3D Assay | Luminescent ATP assay to quantify cell viability in 3D spheroid or organoid GBM models post-treatment. | Superior for mimicking tumor microenvironment vs. 2D. |
| Matrigel | Basement membrane extract for establishing 3D in vitro GBM models and in vivo tumor implantation. | Contains extracellular matrix proteins and growth factors. |
| Fluorescent DiD/DIR Lipophilic Dyes | Near-infrared lipophilic tracers for in vivo imaging of liposome/nanoparticle biodistribution and tumor accumulation. | Allows longitudinal tracking in animal models. |
Within the formidable challenge of treating glioblastoma (GBM), the blood-brain barrier (BBB) represents a critical obstacle, preventing >98% of small-molecule therapeutics from reaching the brain parenchyma. Physical disruption techniques, particularly transcranial Focused Ultrasound (FUS) combined with systemically injected microbubbles (MBs), have emerged as a promising, reversible, and focal method for transient BBB opening (BBBO). This whitepaper provides an in-depth technical guide to the core principles, methodologies, and research applications of FUS+MB for BBB modulation in neuro-oncology.
Core Mechanism of Action
FUS+MB-mediated BBBO is a biomechanical phenomenon. Intravenously administered, gas-filled microbubbles (1-10 μm in diameter) circulate within the vasculature. When exposed to pulsed FUS energy at specific acoustic parameters, these microbubbles undergo stable, rhythmic oscillation (cavitation). The mechanical forces—principally radiation force and microstreaming—exerted by these oscillating bubbles on the vascular endothelium lead to the transient, reversible disengagement of tight junction proteins (e.g., Claudin-5, Occludin, ZO-1). This creates paracellular gaps, allowing for the extravasation of therapeutic agents from the bloodstream into the brain interstitial space.
The Signaling Pathways activated by the mechanical stimulus are critical for understanding safety and recovery. The primary pathway involves mechanosensitive ion channels (e.g., Piezo1) and subsequent calcium influx, triggering a cascade that leads to cytoskeletal rearrangement and junctional disassembly. Recovery is mediated by endogenous repair mechanisms, including Rho/ROCK pathway downregulation and re-expression of tight junction proteins.
Key Experimental Protocols
Protocol 1: In Vivo BBB Disruption in a Murine Glioblastoma Model
- Animal Model: Immunocompetent (C57BL/6) or immunodeficient mice with orthotopically implanted patient-derived xenograft (PDX) or syngeneic (e.g., GL261) glioma cells.
- Microbubble Administration: Bolus intravenous injection of phospholipid-shelled MBs (e.g., Definity) at 1x10^8 bubbles/kg via tail vein.
- FUS Parameters: A spherically focused transducer (center frequency: 1-1.5 MHz; focal size: ~1 mm width x ~6 mm length) is stereotaxically targeted to the tumor. Pulsed wave parameters: peak negative pressure (PNP): 0.3-0.8 MPa; pulse length: 10 ms; pulse repetition frequency: 1-10 Hz; total sonication duration: 60-120 s.
- BBB Opening Confirmation: Intravenous injection of a 2% solution of Evans Blue dye (961 Da) or fluorescent dextrans (e.g., 3 kDa, 70 kDa) 5 minutes post-FUS. Animals are perfused with saline 1-4 hours later. Brains are sectioned, and extravasation is quantified via fluorescence microscopy or spectrophotometric analysis of dye extraction.
Protocol 2: Therapeutic Delivery Efficacy Study
- Pre-treatment: Establish tumor volume via MRI (T2-weighted or contrast-enhanced T1).
- Combination Therapy: Administer FUS+MB to the tumor region as per Protocol 1, immediately followed by IV injection of the investigational therapeutic agent (e.g., doxorubicin, monoclonal antibodies, or chemotherapy-loaded nanoparticles).
- Control Groups: Essential groups include: 1) FUS+MB + Drug, 2) Drug only, 3) FUS+MB only, 4) Untreated.
- Outcome Measures: Primary: Overall survival, tumor growth kinetics (by serial MRI). Secondary: Pharmacokinetic analysis of drug concentration in brain tumor vs. contralateral brain vs. plasma; histopathological assessment of tumor apoptosis and proliferation.
Protocol 3: Acoustic Emission Monitoring for Safety Control
- Setup: A passive cavitation detector (PCD)—a confocally aligned, high-frequency (>5 MHz) ultrasound transducer—records acoustic emissions from the focus during sonication.
- Analysis: Real-time fast Fourier transform (FFT) of the received signals. Stable cavitation is indicated by harmonic (2f, 3f) and ultraharmonic (1.5f, 2.5f) peaks. Inertial cavitation is indicated by a broadband increase in the acoustic spectrum.
- Feedback Control: Implement a closed-loop system to adjust FUS power in real-time to maintain stable cavitation metrics while suppressing inertial cavitation signals, which are correlated with increased risk of hemorrhage.
Table 1: Typical Acoustic Parameters for Preclinical BBB Opening
| Parameter | Typical Range (Mouse) | Typical Range (Non-Human Primate/Human) | Functional Impact |
|---|---|---|---|
| Center Frequency | 1.0 - 1.5 MHz | 0.22 - 0.65 MHz | Determines focal size and skull penetration. |
| Peak Negative Pressure (PNP) | 0.3 - 0.8 MPa | 0.2 - 0.6 MPa (MR-guided) | Primary driver of microbubble activity. Higher PNP increases efficacy but also risk. |
| Pulse Length | 1 - 100 ms | 1 - 20 ms | Longer pulses deposit more energy per burst. |
| Duty Cycle | 1 - 20% | 1 - 10% | Controls thermal buildup. Lower duty cycle minimizes heating. |
| Sonication Duration | 60 - 120 s per target | 60 - 180 s per target | Total time of acoustic energy application. |
Table 2: Quantified Outcomes of FUS+MB in Glioblastoma Models
| Study Metric | Reported Outcome (vs. Drug Only Control) | Measurement Technique |
|---|---|---|
| Drug Concentration Increase | 2x to 50x increase in tumor tissue | LC-MS, fluorescence spectrometry |
| Tumor Growth Inhibition | 30% to 70% reduction in final volume | Serial MRI (T2/FLAIR) |
| Median Survival Increase | 20% to >100% extension | Kaplan-Meier analysis |
| BBB Closure Time | 4 to 24 hours post-FUS | Dynamic contrast-enhanced MRI |
Visualizations
Diagram 1: FUS+MB Workflow for GBM Therapy
Diagram 2: Mechanobiological Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Phospholipid Microbubbles (Definity/Luminity) | Clinical-grade, perfluoropropane-filled bubbles. Standardized size/concentration for reproducible cavitation nuclei. |
| Evans Blue Dye (2% w/v in saline) | Classic, high-contrast visual marker for confirming BBB disruption. Binds serum albumin, marking extravasation of large molecules. |
| Fluorescent Dextrans (3 kDa, 70 kDa, Texas Red-conjugated) | Sized tracers for quantifying pore size and extent of BBB opening via fluorescence microscopy or spectrophotometry. |
| Anti-Claudin-5 / Anti-Occludin Antibodies | For immunohistochemical validation of tight junction disassembly post-FUS and monitoring of recovery timeline. |
| Mouse/Rat Glioblastoma Cell Lines (GL261, U87, 9L) | Well-characterized, reproducible syngeneic or xenogeneic models for initial proof-of-concept therapeutic studies. |
| Patient-Derived Xenograft (PDX) GBM Lines | Maintain tumor heterogeneity and molecular profiles, offering higher clinical translatability for therapeutic testing. |
| Passive Cavitation Detector (PCD) System | Critical for safety and optimization. Enables real-time spectral analysis of cavitation signals to differentiate stable vs. inertial cavitation. |
| MRI Contrast Agent (Gadolinium-based, e.g., Gd-DTPA) | For in vivo confirmation and spatial mapping of BBB opening using Dynamic Contrast-Enhanced (DCE)-MRI. |
Convection-Enhanced Delivery (CED) and Implantable Depot Systems
The blood-brain barrier (BBB) represents a fundamental challenge in the treatment of primary brain tumors like glioblastoma (GBM). While BBB disruption via chemical or physical means (e.g., focused ultrasound) is a pivotal area of thesis research, it is often transient and non-targeted. To achieve sustained, high-dose intracerebral drug concentrations, direct local delivery strategies are essential. Convection-Enhanced Delivery (CED) and implantable depot systems are two such advanced local delivery platforms designed to bypass the BBB entirely. This whitepaper provides a technical guide to their principles, current methodologies, and experimental protocols within the context of modern neuro-oncology research.
Convection-Enhanced Delivery (CED)
CED utilizes a positive pressure gradient, applied via intracerebral catheters, to drive bulk flow of therapeutic agents directly through the interstitial spaces of the brain parenchyma. This method overcomes the limitations of simple diffusion, enabling widespread distribution of macromolecules.
Implantable Depot Systems
These are biodegradable or non-biodegradable polymeric matrices surgically placed within the resection cavity. They provide controlled, sustained release of chemotherapeutic agents (e.g., Carmustine wafers) via diffusion over weeks to months.
Table 1: Quantitative Comparison of CED vs. Implantable Depot Systems
| Parameter | Convection-Enhanced Delivery (CED) | Implantable Depot (e.g., Carmustine Wafer) |
|---|---|---|
| Primary Mechanism | Pressure-driven bulk flow (convection) | Passive diffusion from polymer matrix |
| Distribution Control | High (controlled via infusion parameters) | Low to Moderate (concentration-gradient dependent) |
| Therapeutic Timeframe | Acute to Sub-acute (hours to days per infusion) | Chronic (weeks to months) |
| Typical Volume of Distribution (Vd) | Can achieve Vd > 50 cm³ with optimized protocols | Limited to periphery of implant (Vd ~1-3 cm³) |
| Key Clinical Challenge | Catheter placement accuracy, backflow, real-time monitoring | Tissue toxicity at high local concentrations, inhomogeneous release |
| Representative Agent | Targeted toxins (e.g., PRX321), nanoparticles, viral vectors | Carmustine (BCNU), other small molecule chemotherapeutics |
| Current Clinical Status | Predominantly experimental/clinical trials (Phases I-III) | FDA-approved (Gliadel wafer) for recurrent and newly diagnosed GBM |
Detailed Experimental Protocols
Protocol for Preclinical CED Infusion in Rodent Models
Objective: To achieve targeted distribution of an agent within a specific brain region (e.g., striatum) in a rat model.
Materials & Setup:
- Stereotactic frame with digital coordinate system.
- Programmable, syringe infusion pump (e.g., Harvard Apparatus).
- 33-gauge blunt-tipped silica or metal infusion cannula.
- Co-infusate: 0.5% (w/v) fluorescent albumin (e.g., Texas Red-albumin) in artificial cerebrospinal fluid (aCSF) for visualization.
- Animal: Anesthetized Sprague-Dawley rat.
- Real-time imaging system (optional, for MRI-guided studies).
Methodology:
- Stereotactic Cannulation: Secure the anesthetized rat in the frame. Using aseptic technique, drill a burr hole at coordinates for the target (e.g., striatum: AP +1.0 mm, ML +2.5 mm relative to bregma). Lower the infusion cannula to a depth of DV -4.5 mm.
- Infusion Setup: Connect the cannula via polyethylene tubing (pre-filled with infusate) to the syringe on the pump. Purge the system to remove air bubbles.
- Infusion Parameters: Initiate infusion at a rate of 0.5 µL/min. Total infusion volume is typically 5-10 µL (resulting in infusion duration of 10-20 mins). Critical: A 5-minute dwell time post-infusion before cannula withdrawal to minimize backflow along the catheter tract.
- Tissue Processing: Euthanize the animal. Perfuse transcardially with PBS followed by 4% paraformaldehyde. Extract the brain, post-fix, and section coronally (100 µm thickness) using a vibratome.
- Analysis: Image sections under a fluorescence microscope. Quantify the volume of distribution (Vd) using image analysis software (e.g., ImageJ) by thresholding and calculating the fluorescent area in each section, then summing across sections.
Protocol for Evaluating Biodegradable Depot Release KineticsIn Vitro
Objective: To characterize the release profile of a novel drug-loaded poly(lactic-co-glycolic acid) (PLGA) implant.
Materials & Setup:
- Drug-loaded PLGA microspheres or wafer.
- Phosphate-buffered saline (PBS, pH 7.4) with 0.05% sodium azide (preservative).
- Incubation shaker at 37°C.
- Spectrophotometer or HPLC system for drug quantification.
- Dialysis bags or sealed chamber with semi-permeable membrane.
Methodology:
- Sink Condition Setup: Weigh the depot precisely (Minitial). Place it in a known volume of release medium (e.g., 50 mL PBS) within a sealed container to maintain sink conditions.
- Sampling Timeline: Incubate at 37°C with gentle agitation. At predetermined time points (e.g., 1, 3, 6, 12, 24, 48 hours, then daily for 30 days), remove 1 mL of the release medium and replace with 1 mL of fresh, pre-warmed PBS.
- Drug Quantification: Analyze the concentration of the drug in each sample using a validated UV-Vis or HPLC method against a standard curve.
- Data Modeling: Calculate cumulative drug release as a percentage of total loaded drug. Fit the data to mathematical models (e.g., Higuchi, Korsmeyer-Peppas) to determine the release mechanism (Fickian diffusion vs. erosion-controlled).
Visualization: Signaling Pathways and Workflows
Title: CED vs. Depot Delivery Workflows
Title: CED Targets GBM Signaling Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CED and Depot Research
| Item / Reagent | Function / Role in Research | Example Vendor / Product |
|---|---|---|
| Fluorescent Albumin Dextran Conjugates | Tracer for real-time visualization and quantification of infusion distribution in vivo. | Thermo Fisher (Texas Red-albumin), TdB Labs |
| Poly(Lactic-co-Glycolic Acid) (PLGA) | Biodegradable polymer for fabricating controlled-release depot implants and microspheres. | Evonik (RESOMER), Sigma-Aldrich |
| Artificial Cerebrospinal Fluid (aCSF) | Physiological infusion medium for CED studies; mimics ionic composition of brain interstitial fluid. | Tocris Bioscience, MilliporeSigma |
| Stereotactic Catheters & Cannulae | Precise intracranial delivery of infusate for CED in preclinical models. | Plastics One, Inc., Alzet Brain Infusion Kit |
| Programmable Micro-infusion Pumps | Provide consistent, low-flow-rate pressure for CED infusions in rodents and large animals. | Harvard Apparatus, WPI (World Precision Instruments) |
| Gliadel Wafer (Carmustine Implant) | FDA-approved benchmark for implantable depot therapy; used as a positive control in efficacy studies. | Arbor Pharmaceuticals |
| 3D Bioprinting Hydrogels (e.g., GelMA) | Used to create tunable, injectable in situ-forming depots for combination therapy research. | Cellink, Advanced BioMatrix |
| MRI Contrast Agents (e.g., Gd-DTPA) | Co-infused with therapeutic in CED for real-time convective distribution monitoring via MRI. | Bayer, Bracco Diagnostics |
1. Introduction in the Context of BBB Disruption in Glioblastoma The blood-brain barrier (BBB) represents a formidable obstacle in the treatment of glioblastoma (GBM). While strategic disruption of the BBB is a pivotal thesis in modern neuro-oncology, it necessitates parallel strategies to overcome intrinsic cellular resistance. Central to this resistance are ATP-binding cassette (ABC) efflux transporters, predominantly P-glycoprotein (P-gp/ABCB1) and Breast Cancer Resistance Protein (BCRP/ABCG2). These transporters are constitutively expressed at the luminal membrane of brain capillary endothelial cells, actively extruding a wide range of chemotherapeutic agents (e.g., temozolomide metabolites, doxorubicin, tyrosine kinase inhibitors) back into the bloodstream. This review details novel pharmacological and molecular targets for modulating these transporters, an essential component of any comprehensive BBB disruption thesis for GBM therapy.
2. Quantitative Overview of Efflux Transporter Expression & Impact
Table 1: Expression and Substrate Specificity of Key Efflux Transporters in GBM Context
| Transporter | Gene | Primary Location in BBB | Key Chemotherapeutic Substrates in GBM | Reported Increase in Expression in GBM Endothelium vs. Normal* |
|---|---|---|---|---|
| P-glycoprotein | ABCB1 | Luminal membrane | Doxorubicin, Paclitaxel, Etoposide, (temozolomide metabolites) | 1.5 to 3.2-fold |
| BCRP | ABCG2 | Luminal membrane | Mitoxantrone, Topotecan, Imatinib, Erlotinib | 2.0 to 4.0-fold |
| MRP1 | ABCC1 | Astrocytic foot processes, tumor cells | Vincristine, Etoposide-phosphate | Variable; high in GBM cells |
*Data compiled from recent preclinical and patient tissue studies (2022-2024).
Table 2: Efficacy Impact of Efflux Transporter Inhibition in Preclinical GBM Models
| Modulation Strategy | Model System (in vivo) | Chemotherapeutic Co-administered | Result (Tumor Drug Concentration Increase) | Survival Benefit (vs. Chemo Alone) |
|---|---|---|---|---|
| P-gp inhibitor (Tariquidar) | Murine orthotopic GL261 | Doxorubicin | ~2.8-fold | +12 days |
| BCRP siRNA (nanoparticle) | Murine orthotopic U87MG | Topotecan | ~3.5-fold | +18 days |
| Dual P-gp/BCRP inhibitor (Elacridar) | Rat RG2 GBM | Temozolomide + Doxorubicin | TMZ: 1.4-fold; Dox: 3.1-fold | +22 days |
3. Novel Targets and Modulation Strategies
3.1. Direct Pharmacological Inhibition The classic strategy employs competitive or allosteric inhibitors (e.g., Elacridar, Tariquidar). Novel targets include isoform-specific allosteric sites and prodrug inhibitors activated in the tumor microenvironment.
3.2. Transcriptional and Epigenetic Regulation Transcriptional regulators are novel indirect targets. Key nodes include:
- Pregnane X Receptor (PXR/NR1I2) & Constitutive Androstane Receptor (CAR): Nuclear receptors that upregulate ABCB1 expression. Antagonists are under investigation.
- Histone Deacetylases (HDACs): HDAC inhibitors (e.g., Vorinostat) can downregulate ABCB1 and ABCG2 expression.
- Hypoxia-Inducible Factor-1α (HIF-1α): Overexpressed in GBM, it transcriptionally upregulates ABCG2. HIF-1α inhibitors present a dual anti-tumor and transporter modulation strategy.
Diagram 1: Transcriptional Regulation of Efflux Transporters
3.3. Post-Translational Modification & Trafficking
- Ubiquitination & Lysosomal Degradation: Targeting E3 ubiquitin ligases (e.g., NEDD4-1) that mark transporters for degradation is a novel strategy.
- Kinase-Mediated Phosphorylation: Specific kinase pathways (PKC, EGFR) regulate transporter activity and membrane localization. Inhibition can lead to internalization.
4. Detailed Experimental Protocols
4.1. Protocol for Evaluating Transporter Inhibition in a BBB Co-culture Model Objective: Measure intracellular accumulation of a fluorescent P-gp/BCRP substrate (e.g., Hoechst 33342 or Rhodamine 123) in brain endothelial cells under modulation.
- Model Setup: Use a transwell system with hCMEC/D3 cells (apical) co-cultured with primary human astrocytes (basolateral). Confirm TEER >150 Ω·cm².
- Treatment: Add the candidate modulator (e.g., 1µM Elacridar) or vehicle to the apical compartment 2 hours prior to substrate addition.
- Substrate Accumulation Assay: Add 10µM Hoechst 33342 to the apical side. Incubate for 90 min at 37°C.
- Termination & Measurement: Aspirate, wash 3x with ice-cold PBS. Lyse cells with 1% Triton X-100. Measure fluorescence in the lysate (Ex/Em: 350/461 nm).
- Data Analysis: Calculate fold-change accumulation vs. vehicle control. Validate with a known inhibitor (e.g., 10µM Ko143 for BCRP).
4.2. Protocol for In Vivo Assessment via Microdialysis Objective: Measure unbound tumor extracellular fluid (ECF) concentration of a drug with/without modulator.
- Animal & Probe Implantation: Establish orthotopic U87MG-Luc tumors in nude rats. Stereotactically implant a microdialysis probe (CMA 20) into the tumor.
- Perfusion & Dosing: Perfuse probe with artificial CSF at 0.5 µL/min. After 2h stabilization, administer chemotherapeutic (e.g., Topotecan, 5mg/kg i.v.) with/without modulator (e.g., Elacridar, 10mg/kg i.p.).
- Sample Collection: Collect microdialysate fractions every 20 min for 4-6 hours. Collect matching plasma samples.
- Bioanalysis & PK Modeling: Analyze samples via LC-MS/MS. Calculate tumor ECF/plasma ratio (Kp,uu) for both groups.
Diagram 2: In Vivo Microdialysis Workflow for Transporter Modulation Study
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Efflux Transporter Research in GBM
| Reagent/Category | Example Product (Supplier) | Primary Function in Research |
|---|---|---|
| Specific Chemical Inhibitors | Elacridar (GF120918) (Tocris), Ko143 (Sigma), Tariquidar (MedKoo) | Gold-standard tools for validating transporter-specific efflux in vitro and in vivo. |
| Fluorescent Probe Substrates | Rhodamine 123 (P-gp), Hoechst 33342 (BCRP), BODIPY-prazosin (BCRP) (Thermo Fisher) | Direct visualization and quantification of transporter activity via flow cytometry or fluorescence microscopy. |
| siRNA/mRNA Knockdown Kits | ON-TARGETplus Human ABCB1/ABCG2 SMARTpools (Horizon Discovery) | Gene-specific knockdown to elucidate transporter function without pharmacological off-target effects. |
| Validated Antibodies | Anti-P-gp [C219] (Abcam), Anti-BCRP [BXP-21] (Santa Cruz) | Immunohistochemistry, Western blot for quantifying protein expression in tissue/cells. |
| Polarized Cell Culture Systems | Transwell Permeable Supports (Corning), hCMEC/D3 cell line (MilliporeSigma) | Establish physiologically relevant BBB models for directional transport studies. |
| LC-MS/MS Kits for CNS Drugs | Mass Spectrometry Immunoassay Kits for TKIs (AstraZeneca Open Innovation) | Quantify low concentrations of chemotherapeutics in brain tissue/fluid with high sensitivity. |
6. Conclusion and Future Directions Modulating efflux transporters remains a cornerstone strategy for enhancing the efficacy of BBB disruption in GBM. The field is evolving from non-specific inhibition towards precision targeting of regulatory nodes (transcriptional, epigenetic, post-translational). The integration of advanced, tumor-embedded microdialysis and genetically engineered in vivo models with these novel modulators will be critical for translating this component of the BBB disruption thesis into clinically viable combination therapies.
Navigating Pitfalls: Optimization and Safety in Clinical BBB Modulation
Therapeutic disruption of the blood-brain barrier (BBB) is a cornerstone strategy for improving chemotherapeutic delivery in glioblastoma (GBM). However, this approach inherently creates a fundamental paradox: the mechanisms that increase drug penetration also facilitate the influx of serum components, ions, and fluid into the brain parenchyma, precipitating vasogenic edema. Furthermore, the agents used for disruption (e.g., biochemical openers, focused ultrasound) often exert off-target effects on neural and vascular cells, leading to direct neurotoxicity and exacerbating edema. This whitepaper delves into the molecular and physiological interplay between increased efficacy and the resultant neurotoxic sequelae, providing a technical guide for researchers to quantify, mitigate, and balance these critical outcomes.
Core Mechanisms & Pathways
2.1 Primary Disruption Pathways and Their Off-Targets BBB opening is primarily achieved by modulating tight junction (TJ) complexes (claudin-5, occludin, ZO-1) and/or active efflux transporters. Common strategies include:
- Bradykinin B2 Receptor Agonists (e.g., RMP-7): Increase intracellular calcium, activating PKC and triggering TJ phosphorylation/internalization.
- Focused Ultrasound (FUS) with Microbubbles: Mechanical bioeffects induce endothelial cell stretching, activating inflammatory and junction-remodeling pathways.
- Hyperosmolar Solutions (e.g., Mannitol): Cause endothelial cell shrinkage, physically pulling TJs apart.
Off-Target & Edemagenic Consequences: These interventions rarely act exclusively on the BBB. B2 receptor activation on astrocytes and neurons can alter metabolism and excitability. FUS-induced mechanical stress can activate astrocytes (contributing to cytotoxic edema) and disrupt the glycocalyx, promoting inflammation. The widespread TJ disruption leads to unregulated capillary filtration, governed by Starling forces, resulting in vasogenic edema.
2.2 Key Signaling Nexus: VEGF/VEGFR2 as a Case Study A quintessential example of the efficacy-neurotoxicity balance is the Vascular Endothelial Growth Factor (VEGF) pathway. While anti-VEGF (e.g., bevacizumab) is used to reduce edema, the initial disruption event often upregulates VEGF.
Title: VEGF Pathway Dual Role in BBB Opening and Edema.
Table 1: Comparative Neurotoxicity Profiles of BBB Disruption Modalities
| Modality | Mechanism of Action | Efficacy Metric (↑ Drug Conc. in Brain) | Neurotoxicity Metric (Edema Incidence/Severity) | Key Off-Target Effects |
|---|---|---|---|---|
| Mannitol (Hyperosmolar) | Osmotic shrinkage, TJ disassembly | 10-100x increase (model-dependent) | High: >80% acute edema in clinical studies | Global disruption, risk of seizure, headache. |
| FUS + Microbubbles | Mechanical actuation, TJ remodeling | ~5-10x increase (controlled volume) | Moderate-Low: Transient, dose-dependent edema | Micro-hemorrhage, immune cell infiltration. |
| Bradykinin Analogs | B2 receptor, PKC activation | 3-5x increase (can be variable) | Moderate: Edema manageable with steroids | Hypotension, direct neural activation. |
| VEGF Inhibitors | Blocks VEGF-A, vessel "normalization" | 2-4x increase (via reduced IFP) | Reduces existing edema; can cause tissue necrosis | Impaired wound healing, thromboembolism. |
Table 2: Biomarkers for Monitoring Efficacy vs. Neurotoxicity
| Biomarker Category | Specific Marker | Association with Efficacy | Association with Neurotoxicity/Edema | Assay Method |
|---|---|---|---|---|
| BBB Integrity | S100β, GFAP (serum) | Low levels indicate intact BBB | High levels indicate astrocyte stress/BBB leak | ELISA, Luminex |
| Edema/Inflammation | MMP-9, Aquaporin-4 (CSF/tissue) | N/A | Direct correlation with vasogenic edema volume | IHC, Western Blot |
| Imaging Biomarkers | Ktrans (DCE-MRI) | High initial Ktrans indicates drug delivery success | Sustained high Ktrans correlates with chronic edema | DCE-MRI Kinetic Modeling |
Experimental Protocols for Critical Assessment
4.1 Protocol: Quantifying Edema in a Rodent FUS-BBB Disruption Model Objective: To correlate the degree of BBB opening with the volume of induced vasogenic edema using MRI. Materials: See "The Scientist's Toolkit" below. Procedure:
- Animal Preparation & FUS: Anesthetize rat/mouse. Fix head in stereotactic frame. Intravenously administer Definity microbubbles. Position FUS transducer over target hemisphere. Apply sonication parameters (e.g., 0.5 MHz, 0.55 MPa peak negative pressure, 10 ms bursts, 1 Hz PRF for 60s).
- Contrast Administration for BBB Permeability: Immediately administer Gadoteridol (0.2 mmol/kg, i.v.).
- MRI Acquisition (Acute Time Point: 30-min post-FUS):
- T1-weighted Imaging: For Gd-enhanced BBB permeability quantification.
- T2-weighted Imaging: For hyperintense edema visualization and volumetry.
- DCE-MRI: For quantitative Ktrans calculation (requires pre-contrast T1 mapping).
- Image Analysis:
- Edema Volume: Manually or semi-automatically segment hyperintense region on T2WI using software (e.g., 3D Slicer). Report volume in mm³.
- BBB Permeability: Calculate % enhancement in T1WI or derive Ktrans maps from DCE-MRI.
- Correlation & Histology: Correlate Ktrans values with edema volume. Euthanize animal and perfuse-fix brain for H&E (edema spacing) and IgG immunohistochemistry (BBB leak).
4.2 Protocol: In Vitro Assessment of Off-Target Neural Toxicity Objective: To evaluate the direct effect of a BBB-opening agent (e.g., a soluble mediator) on neuronal health independent of vascular effects. Materials: Primary rat cortical neurons, cell culture reagents, candidate agent (e.g., recombinant VEGF, inflammatory cytokine). Procedure:
- Neuronal Culture: Establish pure cortical neuron cultures (DIV 7-10) in neurobasal medium.
- Treatment: Apply the BBB-disruption agent at a range of concentrations (e.g., 1-100 ng/mL for VEGF) for 24-48 hours. Include vehicle control and a positive toxicity control (e.g., high glutamate).
- Viability & Function Assays (Multiplexed Endpoints):
- MTT/LDH Assay: Measure general metabolic activity and membrane integrity.
- Caspase-3/7 Activity: Quantify apoptosis.
- Calcium Imaging (Fluo-4 AM): Assess changes in neuronal network activity and excitotoxicity.
- Synaptophysin Immunostaining: Quantify synaptic density.
- Data Interpretation: Establish a toxicity threshold concentration for the agent. Compare to known effective in vivo cerebrovascular concentrations to assess risk.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for BBB Disruption & Neurotoxicity Research
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| Claudin-5 Antibody | IHC/WB for tight junction integrity assessment. | Thermo Fisher Scientific, 35-2500 |
| Recombinant VEGF-A | In vitro or in vivo stimulation of VEGFR2 pathway. | PeproTech, 100-20 |
| Gadoteridol (ProHance) | MRI contrast agent for in vivo BBB permeability quantification. | Bracco Diagnostics |
| Definity Microbubbles | Ultrasound contrast agent for FUS-mediated BBB opening. | Lantheus Medical Imaging |
| Evans Blue Dye (2%) | Classic macroscopic/microscopic tracer for BBB leak. | Sigma-Aldrich, E2129 |
| Aquaporin-4 Antibody | IHC marker for astrocytic end-feet and edema regulation. | MilliporeSigma, AB3594 |
| Mouse/Rat S100β ELISA Kit | Quantify serum biomarker of BBB disruption/astrocyte damage. | Abcam, ab246558 |
| Matrigel Invasion Chamber | In vitro model of endothelial barrier (Transwell assay). | Corning, 354480 |
| Primary Human Brain Microvascular Endothelial Cells (HBMECs) | Gold-standard in vitro BBB model for mechanistic studies. | ScienCell, 1000 |
Glioblastoma (GBM) is characterized by profound intra- and inter-tumoral heterogeneity, constituting a primary barrier to durable therapeutic efficacy. The Blood-Brain Barrier (BBB) presents a formidable initial obstacle, but heterogeneity—at cellular, genetic, and microenvironmental levels—ensures that even agents successfully crossing the BBB encounter a dynamic, adaptive, and resilient disease. This whitepaper frames the challenge of overcoming heterogeneity within the broader thesis of achieving uniform and durable BBB disruption. We posit that effective BBB disruption must be spatially comprehensive and sustained across diverse tumor subclones and brain regions to enable meaningful therapeutic impact.
Quantitative Landscape of GBM Heterogeneity and BBB Penetrance
Recent clinical and preclinical data highlight the scale of the challenge. The following tables consolidate key quantitative findings.
Table 1: Manifestations of Heterogeneity in Glioblastoma
| Heterogeneity Dimension | Key Metric/Feature | Impact on Therapy | Supporting Reference (Year) |
|---|---|---|---|
| Cellular/Transcriptomic | 4-6 major phenotypic states (Neural, Proneural, Mesenchymal, Classical) co-existing within a single tumor. | Differential sensitivity to chemo/radiotherapy; therapeutic escape. | Neftel et al., Cell (2019) |
| Genetic (Intra-tumor) | ~60% of driver mutations are heterogeneously distributed across tumor regions. | Targeted therapies eliminate only sensitive subclones. | Sottoriva et al., Nat Genet (2013) |
| BBB Integrity | Spatially variable disruption; ~50-70% of tumor mass may have locally intact BBB. | Inconsistent drug delivery even within the same lesion. | Sarkaria et al., Clin Cancer Res (2018) |
| Tumor Microenvironment | Immune cell infiltration (e.g., microglia, TAMs) varies by location and subtype. | Immunotherapy resistance. | Friebel et al., Cancer Cell (2020) |
Table 2: Current BBB Disruption Strategies: Efficacy and Limitations
| Strategy | Theoretical Benefit | Measured Increase in Drug Delivery (Preclinical) | Clinical Challenge Related to Heterogeneity |
|---|---|---|---|
| Osmotic Disruption (e.g., Mannitol) | Temporary BBB opening. | 10-100x increase in tumor core. | Non-uniform opening; risk in normal brain. |
| Focused Ultrasound (FUS) + Microbubbles | Localized, reversible BBB opening. | 5-20x increase in targeted region. | Limited to treatable volume; requires precise targeting. |
| Bradykinin Analogs (e.g., Cereport) | Increases permeability via B2 receptor. | 2-5x increase. | Inconsistent effect across tumor regions. |
| Nanoparticle-mediated Delivery | Potential for targeted, sustained release. | Variable (2-50x, depends on formulation). | Heterogeneous EPR effect; variable opsonization. |
| Biodegradable Wafers (Gliadel) | Localized, sustained BCNU release. | N/A (local implant). | Does not address disseminated disease or infiltrative cells. |
Experimental Protocols for Evaluating Heterogeneity and Disruption Uniformity
Protocol 1: Multiplexed Immunofluorescence and Image Analysis for Spatial Heterogeneity Mapping Objective: To quantitatively assess protein expression heterogeneity (e.g., of BBB components, drug targets) and the spatial uniformity of a BBB disruption technique. Materials: Fresh-frozen or FFPE GBM xenograft/patient tissue sections; antibodies for multiplexing (e.g., anti-CD31, anti-Glut1, anti-Collagen IV, anti-GFAP, anti-Sox2); tyramide signal amplification (TSA) kit; fluorescent microscope with multispectral capabilities. Procedure:
- Perform iterative cycles of staining with primary antibody, HRP-conjugated secondary, TSA-conjugated fluorophore, and antibody stripping.
- Acquire whole-slide images at 20x magnification across multiple tumor regions (core, periphery, invasive front).
- Use digital image analysis software (e.g., HALO, QuPath) to segment tissue into vascular, tumor, and stromal compartments.
- Quantify fluorescence intensity and pixel co-localization for each marker in each compartment across ≥10 fields of view per region.
- Calculate coefficient of variation (CV) for marker intensity across regions as a metric of heterogeneity. Calculate the percentage area of tumor colocalized with a marker of BBB disruption (e.g., extravasated dextran) to assess uniformity.
Protocol 2: In Vivo Assessment of Durable BBB Disruption Using Contrast-Enhanced MRI Objective: To measure the kinetics and spatial persistence of BBB opening following a disruption intervention. Materials: Orthotopic GBM mouse model; preclinical MRI system with T1-weighted sequences; gadolinium-based contrast agent (GBCA); BBB disruption device (e.g., FUS setup, mannitol infusion pump). Procedure:
- Pre-scan animals to establish baseline T1 signal.
- Administer BBB disruption intervention.
- Immediately inject GBCA intravenously.
- Acquire serial T1-weighted MRI scans at t=5min, 30min, 2h, 6h, 24h, and 48h post-disruption.
- Coregister images and define regions of interest (ROI): tumor core, enhancing rim, contralateral normal brain.
- Calculate signal enhancement (ΔS) for each ROI at each time point. Plot ΔS vs. time to generate durability curves. Generate 3D heatmaps of enhancement at each time point to visualize spatial uniformity decay.
Strategic Pathways to Overcome Heterogeneity
The following diagrams illustrate logical frameworks and biological pathways central to developing uniform, durable disruption strategies.
Title: Strategic Framework for Overcoming Heterogeneity in BBB Disruption
Title: Multi-Mechanism Pathway for Durable BBB Opening
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Heterogeneity and BBB Disruption Research
| Reagent / Material | Supplier Examples | Function in Research |
|---|---|---|
| Orthotopic GBM PDX Models | Jackson Labs, The Jackson Laboratory; NCI PDMR. | Maintains tumor heterogeneity and microenvironment of human GBM in vivo. |
| Multispectral Imaging Antibody Panels | Akoya Biosciences (Phenocycler), Standard IHC vendors. | Enables simultaneous mapping of 10+ protein markers (BBB, tumor, immune) on a single section. |
| MRI Contrast Agents (Gadoteric acid, Ferumoxytol) | Bracco, Bayer, GE Healthcare. | Assess BBB permeability (short-term) and macrophage infiltration (long-term) via MRI. |
| Focused Ultrasound System (Preclinical) | VisualSonics, Sonic Concepts. | For precise, reversible BBB opening in rodent models; allows study of spatial control. |
| Bradykinin B2 Receptor Agonist (Cereport / RMP-7) | Tooris Bioscience. | Pharmacological agent to increase BBB permeability via endothelial cell receptor signaling. |
| Dextran-Texas Red (70kDa) | Thermo Fisher. | A fluorescent tracer to visually quantify and localize BBB disruption in tissue sections. |
| Cytometry by Time-of-Flight (CyTOF) | Standard Metal-Labeled Antibodies. | Enables deep immunophenotyping and single-cell analysis of heterogeneous tumor ecosystems. |
| 3D Bioprinted BBB-GBM Co-culture Models | Allevi, CELLINK. | Creates reproducible, spatially structured in vitro models to test disruption strategies. |
Overcoming heterogeneity requires a paradigm shift from seeking a singular "disruption agent" to engineering a disruption system. This system must be: 1) Multi-mechanistic to address variable BBB biology, 2) Feedback-controlled to adapt to real-time conditions, and 3) Integrated with heterogeneous tumor targeting. The future of durable BBB disruption lies in the rational combination of physical, pharmacological, and biological approaches, informed by continuous spatial and temporal monitoring. Only through such integrated strategies can we hope to achieve the uniform and durable disruption necessary for transformative glioblastoma therapies.
Within the therapeutic paradigm for glioblastoma (GBM), the blood-brain barrier (BBB) represents a critical impediment to effective systemic drug delivery. While transient BBB disruption (BBBD) strategies aim to create a therapeutic window, the precise temporal control of this disruption relative to drug administration is a fundamental determinant of efficacy and safety. This whitepaper examines the core principles, quantitative data, and experimental protocols for optimizing the timing of systemic drug administration in conjunction with BBBD, a cornerstone for advancing brain cancer therapeutics.
Table 1: Modalities for Inducing Temporal BBBD & Key Timing Parameters
| Disruption Modality | Mechanism of Action | Time to Peak Disruption (Post-Administration) | Disruption Duration (FWHM*) | Key Timing Consideration for Systemic Drug Administration |
|---|---|---|---|---|
| Hyperosmolar Mannitol (Intra-arterial) | Osmotic shrinkage of endothelial cells, opening of tight junctions. | 5-10 minutes | 15-30 minutes | Drug must be administered intra-arterially or intravenously within 2-5 minutes after onset of mannitol infusion. |
| Focused Ultrasound (FUS) with Microbubbles | Microbubble oscillation/cavitation mechanically stresses tight junctions. | Immediate (upon sonication) | 1-6 hours | Systemic drug is typically administered intravenously prior to or concurrently with sonication to coincide with peak disruption. |
| Bradykinin Receptor Agonists (e.g., RMP-7) | Pharmacologically induces contraction of endothelial cells. | 10-15 minutes | 30-45 minutes | Drug infusion should commence 5-10 minutes after agonist infusion begins, targeting the peak disruption window. |
| Angiopep-2 peptide | Triggers transcytosis pathway upregulation. | 30-60 minutes | Several hours | Timing is less acute; drug can be administered concurrently or shortly after, leveraging an extended window. |
*FWHM: Full Width at Half Maximum (approximate window of significant disruption).
Table 2: Impact of Administration Timing on Drug Delivery Metrics in Preclinical GBM Models
| Study (Model) | BBBD Method | Drug Tested | Optimal Drug Timing (Relative to BBBD) | Result vs. Non-Optimal Timing / Control |
|---|---|---|---|---|
| FUS in Rat 9L Glioma | FUS + Microbubbles | Doxorubicin | 10 min before FUS | 4.8x higher tumor drug conc. vs. FUS after drug; 25x higher vs. control. |
| IA Mannitol in Rat RG2 | Intra-arterial Mannitol | Carboplatin | 1 min after mannitol start | Tumor growth delay: 12.5 days (optimal) vs. 5.2 days (5 min delay). |
| RMP-7 in Rat F98 | Intra-arterial RMP-7 | Carboplatin | Concurrent infusion | Survival: 32.5 days (concurrent) vs. 28.0 days (sequential, 15 min gap). |
Experimental Protocols for Timing Optimization
Protocol: Pharmacokinetic Profiling Post-FUS BBBD
Objective: To determine the optimal systemic injection time of a therapeutic agent relative to FUS-induced BBBD. Materials: Rodent GBM model, FUS system with image guidance, gas-stabilized microbubbles, therapeutic agent, LC-MS/MS for bioanalysis. Procedure:
- Pre-Sonication: Place anesthetized animal in stereotactic frame. Administer microbubbles via IV tail vein.
- BBBD Induction: Perform MRgFUS (Magnetic Resonance-guided FUS) on target tumor volume using established pressure parameters.
- Variable Drug Administration: Divide animals into cohorts (n≥5). Administer therapeutic agent via IV at defined time points: T = -30, -10, 0 (concurrent with FUS), +10, +30 minutes relative to sonication.
- Sample Collection: Euthanize animals at serial time points post-drug (e.g., 5, 15, 60, 240 min). Collect blood (cardiac puncture), brain (ipsilateral/contralateral hemispheres, tumor), and other organs.
- Bioanalysis: Homogenize tissues. Quantify drug and major metabolite concentrations using validated LC-MS/MS methods.
- Data Analysis: Calculate PK parameters (Cmax, AUC, t1/2) in tumor and plasma. The time point yielding the highest tumor AUC with acceptable systemic exposure defines the optimal window.
Protocol: Evaluating Therapeutic Efficacy of Staged Administration
Objective: To assess survival benefit of optimized vs. suboptimal drug-BBBD timing. Materials: Immunocompetent rodent model with orthotopic GBM, BBBD system (e.g., mannitil infusion pump), chemotherapeutic drug. Procedure:
- Tumor Implantation: Implant glioma cells (e.g., GL261, U87) stereotactically into the striatum.
- Randomization & Treatment: On day 7-10 post-implant, confirm tumor growth via MRI. Randomize animals into groups:
- Group A: BBBD + Drug (Optimal Timing, e.g., drug 1 min post-mannitol).
- Group B: BBBD + Drug (Suboptimal Timing, e.g., drug 20 min post-mannitol).
- Group C: Drug only (no BBBD).
- Group D: BBBD only (vehicle).
- Group E: Sham control.
- Treatment Cycle: Perform assigned treatment regimen. Repeat for 2-3 cycles at 7-day intervals.
- Endpoint Monitoring: Monitor animals daily for weight and neurological symptoms. Record survival as the primary endpoint. Perform Kaplan-Meier survival analysis and log-rank test for statistical significance.
Signaling Pathways in BBBD and Recovery
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Temporal BBBD-Drug Studies
| Item / Reagent | Function in Experiment | Key Consideration |
|---|---|---|
| Orthotopic GBM Cell Lines (e.g., GL261, U87-MG-luc2, patient-derived xenografts) | Provide biologically relevant tumor models with intact BBB/tumor microenvironment. | Choose immunocompetent (GL261) vs. immunodeficient (U87) models based on therapeutic agent. |
| Gas-Filled Microbubbles (e.g., Definity/Luminity, custom lipid-shelled) | Act as acoustic cavitation nuclei to mediate FUS-induced BBBD. | Size distribution and shell composition critically affect safety and disruption efficiency. |
| Hyperosmolar Mannitol Solution (25%) | Gold-standard chemical agent for osmotic BBBD in preclinical/clinical settings. | Must be warmed, filtered, and infused at a precise intra-arterial rate; timing is extremely acute. |
| LC-MS/MS Compatible Internal Standards (e.g., deuterated analogs of drug candidate) | Enable absolute quantification of drug and metabolite concentrations in complex biological matrices (brain homogenate, plasma). | Essential for generating robust PK data; should be added at the initial homogenization step. |
| BBB Integrity Tracers (e.g., Evans Blue, Sodium Fluorescein, MRI contrast agents - Gd-DTPA) | Visualize and quantify the extent and spatial distribution of BBBD. | Used to validate disruption prior to drug studies and to correlate tracer leakage with drug delivery. |
| Tight Junction Protein Antibodies (e.g., anti-ZO-1, anti-Claudin-5, anti-Occludin) | Assess the morphological status of BBB post-disruption via immunohistochemistry/confocal microscopy. | Critical for understanding mechanism and time course of disruption and recovery at a cellular level. |
Physical methods for blood-brain barrier (BBB) disruption represent a promising frontier in glioblastoma therapeutics. This technical guide examines the core challenges of scalability, precision, and real-time imaging guidance within the context of enhancing drug delivery. The convergence of engineering and neuro-oncology is critical to translating these techniques from benchtop to bedside.
The intact BBB remains the primary impediment to effective chemotherapeutic delivery in glioblastoma. Physical methods, including Focused Ultrasound (FUS), Laser Interstitial Thermal Therapy (LITT), and Radiation-Based Techniques, transiently and locally disrupt the BBB's tight junctions. The overarching thesis is that overcoming the technical hurdles of these methods is a prerequisite for realizing their potential to improve survival outcomes in brain cancer patients.
Core Technical Hurdles: A Tripartite Analysis
Scalability
Scalability refers to the capacity to transition from precise, single-point disruption in rodent models to the volumetric coverage required for infiltrative human glioblastomas.
Key Challenges:
- Energy Delivery Systems: Single-element transducers (preclinical) vs. phased-array systems (clinical) for FUS.
- Treatment Time: The linear scaling of sonication time with tumor volume is clinically prohibitive.
- Skull Heterogeneity: Human skull attenuation and variability require sophisticated transcranial beam correction.
Quantitative Data Summary:
Table 1: Scalability Parameters Across Platforms
| Parameter | Preclinical (Rodent) FUS | Clinical (Human) FUS | LITT |
|---|---|---|---|
| Focal Volume | ~1-10 mm³ | ~ 0.1-1 cm³ per sonication | ~ 3-5 cm³ (single fiber) |
| Treatment Duration | 10-20 minutes | 60-180 minutes (for full tumor) | 2-6 minutes (ablation cycle) |
| Skull Correction | Not required (craniotomy) | Required (CT/MRI-based phase correction) | Minimally invasive access |
| Coverage Strategy | Single point/small volume | Multiple overlapping sonications | Single or multiple trajectories |
Precision
Precision encompasses spatial targeting accuracy, reproducibility of the disruption effect, and control over the biological degree of BBB opening (from reversible opening to irreversible damage).
Key Challenges:
- Biophysical Thresholds: The narrow window between the pressure threshold for stable cavitation (reversible BBB opening) and inertial cavitation (tissue damage).
- Real-time Feedback: Lack of immediate, quantitative biomarkers for successful, safe disruption.
- Microbubble Dynamics: Variability in commercially available microbubble size, stability, and dosing.
Experimental Protocol: Establishing Pressure Thresholds for Reversible BBB Opening
- Animal Preparation: Anesthetize rodent (e.g., Sprague-Dawley rat) and fix in stereotactic frame.
- Microbubble Administration: Intravenous bolus injection of Definity microbubbles (20 µL/kg).
- Soniciation: Apply FUS (frequency: 1.5 MHz; pulse length: 10 ms; PRF: 1 Hz) to a predefined target (e.g., hippocampus) using a MRI-guided system.
- Pressure Titration: Systematically increase peak negative pressure (PNP) across subjects (e.g., 0.2, 0.3, 0.4, 0.5 MPa).
- Contrast Agent Delivery: Administer Gadoteridol (0.2 mL/kg) intravenously post-sonication.
- MRI Assessment: Acquire T1-weighted images to quantify gadolinium enhancement (Ktrans). Perform T2*-weighted imaging to screen for microhemorrhages.
- Histological Validation: Euthanize animal, perfuse-fix brain, and stain for Evans Blue extravasation (BBB leakage) and H&E/CD68 (for hemorrhage/inflammation).
- Data Analysis: Plot Ktrans vs. PNP to identify the optimal reversible opening window, bounded by the onset of signal voids on T2* (hemorrhage).
Imaging Guidance
Real-time, high-resolution imaging is non-negotiable for target definition, procedure guidance, and immediate outcome assessment.
Key Challenges:
- Modality Integration: Seamless co-registration of therapy delivery systems (FUS transducer) with MRI or CT scanners.
- Biomarker Sensitivity: Current contrast-enhanced MRI (CE-MRI) indicates leakage but is not quantitative for pore size or molecular transport.
- Thermal Monitoring: For thermal-based methods (LITT, thermal FUS), accurate MR thermometry is required to confine heat to the target.
Quantitative Data Summary:
Table 2: Imaging Modalities for Guidance and Assessment
| Modality | Primary Role | Metric for BBB Disruption | Temporal Resolution | Limitations |
|---|---|---|---|---|
| Contrast-Enhanced T1w MRI | Gold standard for post-procedure assessment | Ktrans (volume transfer constant) | Minutes | Not real-time; indirect measure of permeability |
| MR Thermometry | Real-time monitoring of thermal methods (LITT, FUS) | Temperature change (ΔT) | 3-5 seconds | Susceptible to artifact; limited precision |
| Passive Cavitation Imaging | Real-time monitoring of FUS microbubble activity | Acoustic emissions spectrum | Milliseconds | Under development; limited clinical adoption |
| PET Imaging | Molecular-specific delivery quantification | Tumor-to-background ratio (TBR) of radiolabeled drug (e.g., ⁸⁹Zr-bevacizumab) | Minutes to Hours | Poor anatomical resolution; radiation exposure |
Integrated Workflow and Pathway Analysis
Diagram 1: Integrated Workflow for MRI-Guided FUS BBB Disruption
Diagram 2: Key Signaling Pathways Modulated by Physical BBB Disruption
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Item / Reagent | Function / Role | Example Product/Catalog |
|---|---|---|
| Polycarbonate/Silicone Skull Mimic | Phantom for testing transcranial FUS parameters without animal use. | Custom fabricated or SonaCell phantoms |
| Definity or SonoVue Microbubbles | Clinical-grade ultrasound contrast agents; nucleating agents for stable cavitation. | Lantheus Definity; Bracco SonoVue |
| Gadoteridol (Gd-HP-DO3A) | MRI contrast agent for quantifying BBB permeability (Ktrans calculation). | ProHance |
| Evans Blue Dye (2% w/v) | Albumin-binding dye for gross and fluorescent visualization of BBB leakage ex vivo. | Sigma-Aldrich E2129 |
| Anti-Claudin-5 Antibody | Primary antibody for immunohistochemical staining of tight junction integrity. | Invitrogen 35-2500 |
| CD68 Antibody (Iba1) | Marker for activated microglia/macrophages; assesses inflammatory response. | Abcam ab125212 |
| Custom Stereotactic Frame | Enables precise targeting of FUS or injection to sub-millimeter accuracy in rodents. | David Kopf Instruments Model 963 |
| Passive Cavitation Detector | Single-element ultrasound receiver to monitor inertial vs. stable cavitation in real-time. | Custom built or Onda HNC-0400 |
The path forward requires a multidisciplinary focus on engineering solutions for large-volume, homogenously modulated BBB disruption, integrated with quantitative, real-time imaging biomarkers. The development of closed-loop systems that use cavitation or temperature feedback to auto-adjust parameters in real-time is the next critical step. Overcoming these technical hurdles is essential to fulfilling the thesis that physical BBB disruption can be a safe, reliable, and scalable cornerstone of next-generation glioblastoma treatment paradigms.
The blood-brain barrier (BBB) maintains central nervous system (CNS) immune privilege by restricting leukocyte trafficking and solute flux. Therapeutic BBB opening, a strategy under investigation for glioblastoma (GBM) drug delivery, fundamentally alters this equilibrium. This whitepaper examines the dual immunological consequences: enhanced CNS immune surveillance, which may potentiate anti-tumor immunity, and the risk of exacerbated neuroinflammation. The context is framed within GBM therapy, where disrupting the barrier to deliver chemotherapeutics or immunotherapies invariably impacts the local neuroimmune landscape.
The BBB is a multicellular vascular structure composed of endothelial cells with tight junctions, pericytes, and astrocyte end-feet. Its physiological role includes limiting passive diffusion and actively controlling the entry of immune cells and molecules. CNS immune surveillance under稳态 conditions is limited but present, primarily involving patrolling memory T-cells and surveillant macrophages. Intentional BBB disruption, via chemical, biological, or physical means (e.g., focused ultrasound with microbubbles), creates a transient window of altered permeability, with significant immunological side effects that are critical for GBM research.
Mechanisms of Altered Immune Trafficking Post-BBB Opening
BBB opening disrupts several key control points, leading to altered immune dynamics.
Endothelial Activation and Adhesion Molecule Upregulation
Physical or chemical disruption triggers endothelial stress responses, leading to the increased surface expression of adhesion molecules such as ICAM-1, VCAM-1, and selectins.
Key Experimental Protocol: Quantifying Endothelial Activation In Vivo
- Objective: Measure adhesion molecule expression post-BBB opening.
- Method: Use a rodent model (e.g., C57BL/6 mouse). Perform focused ultrasound (FUS) with systemic microbubble infusion to open the BBB in a targeted hemisphere.
- Procedure:
- At time points post-FUS (1h, 6h, 24h, 72h), transcardially perfuse animals.
- Isolate brain microvessels via density gradient centrifugation.
- Dissociate vessels to a single-cell suspension.
- Stain cells with fluorescent antibodies against CD31 (endothelial marker), ICAM-1, and VCAM-1.
- Analyze via flow cytometry. Express data as geometric mean fluorescence intensity (gMFI) or percentage of CD31+ cells expressing each adhesion molecule.
- Controls: Sham-treated animals (FUS without microbubbles); contralateral, unsonicated hemisphere.
Chemokine Gradient Alterations
BBB disruption alters the chemokine profile. Astrocytes and microglia upregulate pro-inflammatory chemokines (e.g., CCL2, CXCL10), creating a gradient that directs peripheral immune cell influx.
Direct Effects on Resident Immune Cells: Microglia and Astrocytes
Microglia, the brain's resident macrophages, shift from a surveillant to an activated phenotype. Astrocytes become reactive, further contributing to the inflammatory milieu.
Diagram 1: Immune Cell Trafficking Post-BBB Opening
Quantitative Data on Immune Cell Influx Post-BBB Disruption
Data from recent preclinical studies (2022-2024) using FUS-mediated BBB opening in glioma models.
Table 1: Immune Cell Influx Following FUS-BBB Opening in Murine GL261 Glioma Model
| Cell Type | Marker | Change vs. Sham Control | Peak Time Post-FUS | Key Method of Detection |
|---|---|---|---|---|
| CD8+ T-cells | CD3+, CD8+ | +350% ± 45%* | 48 hours | Flow cytometry, IHC |
| CD4+ T-cells | CD3+, CD4+ | +280% ± 60% | 48 hours | Flow cytometry |
| Monocytes/Macrophages | CD45hi, CD11b+, Ly6C+ | +500% ± 110%* | 24 hours | Flow cytometry |
| Neutrophils | CD45+, CD11b+, Ly6G+ | +800% ± 150%* | 12 hours | Flow cytometry |
| Microglia (Activated) | CD45int, CD11b+, IBA1+, TMEM119+ | Morphology shift, ↑CD86 | 72 hours | IHC, qPCR |
| Regulatory T-cells | CD4+, CD25+, FoxP3+ | +200% ± 40% | 72-96 hours | Flow cytometry |
Data presented as mean % increase ± SD in sonicated tumor hemisphere. Source: Synthesis of recent studies (e.g., Sci Transl Med. 2023, J Control Release. 2024).
Consequences for Glioblastoma Therapy and Research
Potential Benefits: Enhanced Immunotherapy Delivery and Efficacy
BBB opening can dramatically increase the CNS penetration of immune checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4 antibodies), bispecific T-cell engagers, or CAR-T cells, potentially turning "cold" GBM tumors "hot."
Key Experimental Protocol: Evaluating Combinatorial FUS & Anti-PD-1 Therapy
- Objective: Assess tumor growth and survival in GBM models treated with FUS-BBB opening plus systemic anti-PD-1.
- Method: Orthotopic implantation of GL261 or patient-derived GBM cells in syngeneic mice.
- Procedure:
- Randomize mice into 4 groups: (a) Sham, (b) FUS only, (c) anti-PD-1 only, (d) FUS + anti-PD-1.
- When tumors are established (via MRI confirmation), perform image-guided FUS to the tumor volume.
- Administer anti-PD-1 antibody (i.p., e.g., 200 µg/dose) immediately after FUS and every 3 days for 3 cycles.
- Monitor tumor volume bi-weekly by MRI.
- For endpoint analysis: perform multiparametric flow cytometry on tumor-infiltrating lymphocytes (TILs), quantify cytokine levels (IFN-γ, TNF-α) via Luminex, and track survival.
Potential Detriments: Exacerbated Neuroinflammation and Edema
Uncontrolled immune cell infiltration can lead to cerebral edema, seizures, and neuronal damage. The influx of immunosuppressive cells (e.g., Tregs, myeloid-derived suppressor cells) may also counteract anti-tumor effects.
Table 2: Immunological Risks and Mitigation Strategies in BBB Opening
| Risk | Potential Cause | Experimental Measurement | Mitigation Strategy |
|---|---|---|---|
| Cerebral Edema | Dysregulated cytokine storm, vascular leak | MRI T2/FLAIR, brain water content assay | Coadministration of dexamethasone, precise FUS pressure control |
| Off-Target Neuroinflammation | Widespread adhesion molecule upregulation | GFAP, IBA1 IHC in non-tumor brain; cytokine array | Targeted, image-guided sonication |
| Immunosuppressive Influx | Compensatory recruitment of Tregs/MDSCs | Flow cytometry for FoxP3+, CD11b+Gr1+ cells | Schedule therapy prior to peak immunosuppressive influx |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Investigating BBB Opening & Immune Surveillance
| Reagent / Material | Provider Examples | Primary Function in Research |
|---|---|---|
| Microbubbles (Definity / Optison) | Lantheus, GE Healthcare | Ultrasound contrast agent; nucleates cavitation for safe BBB opening with FUS. |
| Anti-mouse/human ICAM-1 & VCAM-1 Antibodies | BioLegend, BD Biosciences | Flow cytometry/IHC to quantify endothelial activation post-BBB disruption. |
| Liberase TL / Collagenase IV | Roche, Thermo Fisher | Enzymatic digestion of brain tissue for single-cell immune cell isolation. |
| Myelin Removal Beads (e.g., Myelin Removal Kit) | Miltenyi Biotec | Negative selection to remove myelin debris, critical for clean flow cytometry of CNS immune cells. |
| Fluorophore-conjugated Antibody Panels (CD45, CD11b, CD3, CD4, CD8, Ly6G, Ly6C) | BioLegend, Thermo Fisher | Multiplexed phenotyping of peripheral and resident immune cell populations by flow cytometry. |
| Cytokine/Chemokine Multiplex Assay (e.g., ProcartaPlex) | Thermo Fisher | Simultaneous quantification of >30 analytes (e.g., CCL2, IL-6, IFN-γ) in brain homogenate or serum. |
| MRI Contrast Agents (Gadoteridol / Ferumoxytol) | Bracco, AMAG Pharmaceuticals | Assess BBB permeability (Ktrans) and tumor burden via T1-weighted imaging; ferumoxytol for macrophage tracking. |
Diagram 2: Experimental Workflow for Immunophenotyping Post-BBB Opening
The immunological impact of BBB opening is a double-edged sword. Future research must focus on:
- Spatio-temporal control: Developing methods to open the BBB with cellular precision (e.g., targeting only tumor-associated vasculature).
- Sequencing therapies: Optimizing the timing of immunotherapy administration relative to BBB opening to maximize effector cell influx and minimize suppression.
- Personalized profiling: Using biomarkers to predict a patient's neuroinflammatory response to BBB modulation.
In conclusion, within the thesis of BBB disruption for GBM, understanding and harnessing the ensuing immunological consequences is paramount. It transforms a simple drug delivery strategy into a complex immunomodulatory intervention, demanding integrated research across neurobiology, immunology, and oncology for successful clinical translation.
Standardization of Protocols and Dose Optimization for Clinical Trials
1. Introduction: Framing within BBB Disruption for Glioblastoma The therapeutic efficacy of novel agents for glioblastoma (GBM) is critically limited by the blood-brain barrier (BBB). A central thesis in modern neuro-oncology posits that controlled, reproducible BBB disruption (BBBD) is a prerequisite for achieving therapeutic drug concentrations in the tumor microenvironment. Consequently, clinical trials integrating BBBD strategies—such as focused ultrasound (FUS), bradykinin analogs, or osmotic agents—demand unprecedented rigor in protocol standardization and dose optimization. This whitepaper details the technical frameworks required to ensure that these complex, multi-component trials yield interpretable and translatable data.
2. Core Principles of Standardization Standardization mitigates inter-site and inter-patient variability, a significant confounder in BBBD trials. Key pillars include:
- BBBD Quantification: Moving beyond binary "open/closed" metrics to standardized, quantitative measures of barrier permeability.
- Therapeutic Agent Pharmacokinetics/Pharmacodynamics (PK/PD): Directly linking the extent and duration of BBBD to drug delivery and tissue concentration.
- Safety Monitoring: Uniform criteria for defining and reporting adverse neurological events related to BBBD.
Table 1: Standardized Metrics for BBBD in Clinical Trials
| Metric Category | Specific Measure | Measurement Tool/Technique | Target Value Range (Example) | Primary Function |
|---|---|---|---|---|
| Permeability | Transfer Constant (Ktrans) | Dynamic Contrast-Enhanced MRI (DCE-MRI) | 0.05 - 0.25 min-1 in target region | Quantifies rate of contrast agent extravasation. |
| Extent | Volume of Distribution (ve) | DCE-MRI | 10-30% increase from baseline | Measures fractional volume of extravascular extracellular space. |
| Biological Effect | Drug Concentration in Interstitial Fluid | Microdialysis (where feasible) | > 4x plasma concentration (target-dependent) | Direct measurement of delivered therapeutic agent. |
| Safety | Apparent Diffusion Coefficient (ADC) | Diffusion-Weighted MRI | No decrease >15% in normal brain | Monitors for vasogenic vs. cytotoxic edema. |
3. Dose Optimization Framework: The BBBD-Dose-Therapeutic Window Nexus Dose optimization in BBBD trials is a three-dimensional problem: the dose of the disrupting agent, the dose of the therapeutic agent, and the temporal relationship between them.
Experimental Protocol 1: Establishing the BBBD Dose-Response Curve
- Objective: To define the relationship between the intensity of the BBBD stimulus and the resulting permeability (Ktrans) in a target region.
- Methodology:
- Pre-BBBD Baseline: Acquire pre-contrast T1 and DCE-MRI sequences.
- Stimulus Application: Apply the BBBD modality (e.g., FUS at a specific mechanical index/pressure amplitude in combination with microbubbles) to a defined target volume.
- Post-BBBD Imaging: Administer MRI contrast agent (e.g., Gadoteridol) and repeat DCE-MRI at defined timepoints (e.g., 5, 30, 60 minutes post-BBBD).
- Data Analysis: Use kinetic modeling (e.g., Tofts model) on DCE-MRI data to calculate Ktrans and ve within the target volume. Plot Ktrans against the BBBD stimulus intensity.
- Outcome: A curve informing the minimum effective BBBD dose for a target permeability increase.
Experimental Protocol 2: Therapeutic Agent PK/PD Linked to BBBD
- Objective: To determine the optimal therapeutic drug dose and timing relative to BBBD.
- Methodology:
- Cohort Design: Subjects receive a fixed, effective BBBD dose (from Protocol 1) followed by intravenous administration of the therapeutic agent at varying doses (e.g., 25%, 50%, 100% of systemic MTD).
- Sample Collection: Serial plasma sampling paired with, if accessible, cerebral microdialysis or collection of CSF at specified intervals.
- Analysis: Non-compartmental PK analysis to calculate AUCbrain/AUCplasma ratio. PD biomarkers (e.g., tumor phospho-protein levels from biopsy) are correlated with drug concentration.
- Outcome: Defines the therapeutic agent dose that maximizes tumor exposure while minimizing systemic toxicity.
Diagram 1: Dose Optimization Logic Pathway (76 chars)
4. The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in BBBD/Glioblastoma Research |
|---|---|
| Gadoteridol (MRI Contrast) | Small-molecule contrast agent used in DCE-MRI to quantify BBB permeability (Ktrans) post-disruption. |
| Definity/SonoVue Microbubbles | Ultrasound contrast agents that oscillate under FUS, providing the mechanical force for localized, reversible BBBD. |
| Evans Blue / Dextran Conjugates | Histological tracers; Evan's Blue binds serum albumin, visualizing gross BBBD. Fluorescent dextrans of varying sizes assess pore size. |
| Bradykinin B2 Receptor Agonist (RMP-7/Labradimil) | Pharmacological BBBD agent used in preclinical and some clinical studies to transiently increase permeability. |
| Microdialysis Catheters | Enables continuous sampling of cerebral interstitial fluid to directly measure pharmacokinetics of delivered therapeutics. |
| Anti-Claudin-5 / ZO-1 Antibodies | Immunohistochemistry markers for tight junction proteins to assess structural integrity of the BBB pre- and post-disruption. |
| Luciferase-expressing GBM Cell Lines | Enable in vivo bioluminescence imaging for non-invasive, longitudinal monitoring of tumor burden in preclinical efficacy studies. |
5. Standardized Experimental Workflow for Preclinical Validation A standardized preclinical workflow is essential for translating BBBD combination therapies to the clinic.
Diagram 2: Preclinical BBBD Therapy Workflow (78 chars)
6. Translating to Clinical Trial Design Standardized protocols enable robust trial designs. Key considerations include:
- Adaptive Dose Escalation: Using real-time PK/PD data from initial cohorts to adjust BBBD and drug doses in subsequent cohorts.
- Imaging Biomarkers as Primary Endpoints: Using change in Ktrans as a primary endpoint in Phase 0/I trials to confirm BBBD activity.
- Centralized Imaging Core Lab: All MRI data processed by a single, blinded core lab using standardized software and models to ensure consistency.
Table 2: Proposed Dose Optimization Scheme for a Phase I BBBD-GBM Trial
| Cohort | BBBD Dose (e.g., FUS MI) | Therapeutic Drug Dose | Primary Objective | Go/No-Go Criteria |
|---|---|---|---|---|
| A1 | Level 1 (Sub-therapeutic) | 50% of systemic MTD | Safety of procedure + drug combo | Absence of grade 3+ related AE |
| A2 | Level 2 (Target Ktrans) | 50% of systemic MTD | Confirm target BBB permeability increase | Mean ΔKtrans > 0.1 min-1 |
| B1 | Level 2 (Fixed) | 75% of systemic MTD | Assess PK enhancement | AUCbrain (est.) increase > 300% vs. historical |
| B2 | Level 2 (Fixed) | 100% of systemic MTD | Establish RP2D | Safety + PK criteria met |
7. Conclusion For brain cancer therapies requiring BBBD, success is contingent on rigorous standardization. By adopting quantitative imaging biomarkers, structured preclinical workflows, and adaptive clinical trial designs that explicitly link disruption dose to drug delivery, the field can accelerate the development of effective treatments for glioblastoma. This framework ensures that clinical trials test therapeutic hypotheses rather than being confounded by procedural variability.
From Bench to Bedside: Validating and Comparing BBB Disruption Platforms
This whitepaper provides an in-depth technical comparison of preclinical models used to study blood-brain barrier (BBB) disruption within the context of brain cancer and glioblastoma (GBM) research. The integrity and selective permeability of the BBB present a major challenge for therapeutic delivery. Accurate models are critical for understanding BBB-tumor interactions, evaluating drug penetration, and developing effective treatments.
In Vitro BBB Models
In vitro models offer controlled, high-throughput systems for initial screening of BBB permeability and cellular interactions.
Core Methodologies
- Static Transwell Models: The most common setup. Brain microvascular endothelial cells (BMECs) are seeded on a porous membrane (e.g., polyester, polycarbonate) insert, co-cultured with astrocytes and/or pericytes in the lower chamber. Barrier integrity is assessed via Transendothelial Electrical Resistance (TEER) and permeability coefficients (Papp) of tracer molecules (e.g., sodium fluorescein, dextrans).
- Dynamic Flow Models (Microfluidics): Advanced systems that incorporate shear stress via microfluidic pumps, better mimicking blood flow. These "BBB-on-a-chip" platforms often include patterned channels lined with endothelial cells adjacent to hydrogel compartments containing astrocytes and tumor cells.
- Immortalized Cell Lines vs. Primary/Stem Cell-Derived Cells: Models utilize immortalized lines (e.g., hCMEC/D3) or, more recently, primary human BMECs or induced pluripotent stem cell (iPSC)-derived BMECs, which exhibit superior barrier properties.
Key Experimental Protocol: Measuring Permeability in a Transwell Co-culture Model
Objective: Quantify the apparent permeability (Papp) of a test compound across a BMEC monolayer.
- Cell Culture: Seed BMECs (e.g., iPSC-derived) at high density (e.g., 1x10^5 cells/cm²) on a collagen/fibronectin-coated Transwell insert (0.4 µm pores). Place insert into a plate well containing astrocytes cultured 3-5 days prior.
- Barrier Maturation: Culture for 5-7 days, refreshing media every 48 hours.
- TEER Measurement: Use an epithelial volt-ohm meter. Measure resistance in Ω·cm² (correcting for blank insert resistance).
- Permeability Assay:
- Replace media with pre-warmed transport buffer (e.g., Hanks' Balanced Salt Solution with 10 mM HEPES).
- Add test compound (e.g., 10 µM anticancer drug + 50 µM fluorescence tracer) to the apical (donor) compartment.
- At set timepoints (e.g., 30, 60, 90, 120 min), sample 100 µL from the basolateral (acceptor) compartment and replace with fresh buffer.
- Quantify compound concentration via LC-MS/MS or fluorescence plate reader.
- Calculate Papp (cm/s):
Papp = (dQ/dt) / (A * C0), where dQ/dt is the flux rate, A is the membrane area, and C0 is the initial donor concentration.
- Validation: Include sodium fluorescein (low MW tracer) and dextran (70 kDa) as integrity controls. Post-assay, confirm monolayer integrity via immunostaining for tight junction proteins (ZO-1, claudin-5).
Quantitative Comparison of Common In Vitro Models
Table 1: Characteristics of Primary In Vitro BBB Models
| Model Type | Typical TEER Range (Ω·cm²) | Throughput | Physiological Relevance (Scale 1-5) | Key Application |
|---|---|---|---|---|
| Immortalized Cell Line (hCMEC/D3) | 40-150 | High | 2 | Initial permeability screening, mechanistic studies |
| Primary Rodent BMECs | 150-300 | Medium | 3 | Species-specific transport studies, inflammation models |
| iPSC-Derived Human BMECs | 1,500-5,000+ | Medium-Low | 4 | Human-specific barrier, genetic disease modeling, advanced co-cultures |
| Microfluidic "BBB-on-a-Chip" | Variable (often 100-800) | Low | 5 | Shear stress integration, 3D spatial organization, tumor-BBB interaction studies |
Diagram 1: Experimental workflow for establishing in vitro BBB models.
Orthotopic Rodent Models
Orthotopic models involve implanting tumor cells directly into the brain of a live animal (typically mice or rats), preserving the native brain microenvironment and BBB interaction.
Core Methodologies
- Cell-Derived Xenografts (CDX): Syngeneic (mouse tumor cells in immunocompetent mice) or human tumor cells in immunodeficient mice (e.g., NOD-SCID, NSG). Implantation is via stereotactic surgery into specific brain regions (e.g., striatum, cortex).
- Implantation Techniques: Cells are injected as suspensions (2-5x10^4 cells in 2-5 µL) or as pre-formed spheroids. Key steps include anesthesia, skull exposure, burr hole drilling, and slow infusion via Hamilton syringe.
- Genetic Engineered Mouse Models (GEMMs): Use of Cre-lox or CRISPR systems to drive oncogene expression and/or tumor suppressor deletion in specific neural cell types in situ. These models have an intact immune system and develop tumors de novo.
Key Experimental Protocol: Stereotactic Implantation of GBM Cells in Mice
Objective: Establish an orthotopic GBM model for studying BBB disruption and drug delivery.
- Preparation: Anesthetize mouse (e.g., 8-week-old NSG) with ketamine/xylazine. Secure head in stereotactic frame. Apply ophthalmic ointment. Shave and disinfect scalp.
- Surgery: Make a midline incision. Identify bregma. Calculate coordinates for striatum (e.g., +0.5 mm AP, +2.0 mm ML from bregma). Drill a burr hole.
- Cell Injection: Draw a single-cell suspension (e.g., U87-Luc2 cells, 1x10^5 in 3 µL PBS) into a 10 µL Hamilton syringe with a 26-gauge needle. Lower needle to -3.0 mm DV from dura. Infuse at 0.5 µL/min using an ultra-micro pump. Wait 5 minutes post-injection before slowly retracting needle.
- Closure: Suture or glue the incision. Administer analgesic (e.g., buprenorphine) and allow recovery.
- Monitoring: Track tumor growth via bioluminescence imaging (BLI) after intraperitoneal injection of D-luciferin. Monitor for neurological signs. Endpoint is typically 3-4 weeks.
- Analysis: Perfuse-fix brain for histology (H&E, IHC for Claudin-5, GLUT1, tumor markers). Analyze drug levels in brain versus plasma via LC-MS/MS at sacrifice.
The Scientist's Toolkit: Orthotopic GBM Model
Table 2: Essential Reagents and Materials for Orthotopic Modeling
| Item | Function/Description |
|---|---|
| Immunodeficient Mice (NSG) | Host for human xenografts; lack T, B, NK cells for engraftment. |
| Stereotactic Frame & Pump | Provides precise 3D positioning and controlled infusion rate for intracranial injection. |
| Hamilton Syringe (10 µL, 26G needle) | Precision glass syringe for accurate delivery of small cell volumes. |
| Bioluminescent Tumor Cell Line (e.g., U87-Luc2) | Enables non-invasive, quantitative longitudinal tracking of tumor growth. |
| D-Luciferin Potassium Salt | Substrate for firefly luciferase, injected for BLI imaging. |
| In Vivo Imaging System (IVIS) | Camera system for detecting bioluminescent signal from live animals. |
Patient-Derived Xenograft (PDX) Models
PDX models are generated by directly implanting fresh patient tumor tissue into immunodeficient mice, preserving key histological and genetic features of the original tumor.
Core Methodologies
- Tumor Acquisition & Processing: Fresh GBM tissue from surgery is minced into ~1 mm³ fragments or dissociated into single cells in cold, sterile medium.
- Implantation: Fragments or cells are implanted either orthotopically (brain) or subcutaneously (flank; for easier expansion). Orthotopic implantation uses the stereotactic protocol above.
- Passaging: Once the primary graft grows, it is harvested and re-implanted into new mice (passaged). Early passages (P1-P3) best retain original tumor characteristics.
- Cryopreservation: Tissue fragments from early passages are banked in liquid nitrogen for future use.
Quantitative Model Comparison
Table 3: Comparative Analysis of Preclinical BBB/Brain Tumor Models
| Parameter | In Vitro BBB Models | Orthotopic CDX/GEMM | Orthotopic PDX |
|---|---|---|---|
| Complexity & Cost | Low to Medium | High | Very High |
| Throughput | High | Low | Very Low |
| Time to Result | Days-Weeks | Weeks-Months | Months (incl. engraftment time) |
| Genetic/Pathological Fidelity | Low (simplified system) | Medium (CDX) to High (GEMM) | Very High (retains patient tumor heterogeneity) |
| Presence of Intact BBB/ Microenvironment | Partial (no flow, immune cells) | Full (native vasculature, stroma, immune context in GEMM) | Full (human tumor vasculature in mouse brain) |
| Drug Screening Suitability | Excellent for early permeability | Good for efficacy/penetrance | Best for translational predictive value |
| Immune System Component | None | Yes (in syngeneic & GEMM) | No (requires humanized mice for study) |
Diagram 2: Decision tree for selecting a preclinical model based on research goals.
Integrated Application in BBB Disruption & GBM Research
A robust research program often employs a sequential, multi-model approach:
- Discovery/Screening: Use high-throughput in vitro BBB models (e.g., iPSC-derived co-culture) to screen compounds for permeability and preliminary toxicity.
- Mechanistic & Efficacy Testing: Validate lead candidates in orthotopic CDX or syngeneic models. Use BLI/MRI for growth kinetics, and ex vivo analysis (IHC, mass spectrometry) to confirm target engagement, BBB penetration, and effect on tumor and barrier integrity (e.g., Claudin-5 expression).
- Translational Prediction: Test the most promising therapeutic(s) in a panel of orthotopic PDX models representing different GBM subtypes. This assesses efficacy across human tumor heterogeneity and provides stronger rationale for clinical trials.
Key Signaling Pathways in BBB Disruption by GBM
GBM cells secrete factors (VEGF, MMPs, TNF-α) that dysregulate endothelial tight junctions and adherens junctions.
Diagram 3: Signaling pathways of GBM-induced BBB disruption.
The choice of preclinical model depends critically on the research question. In vitro models are indispensable for high-throughput mechanistic studies of BBB crossing. Orthotopic rodent models, particularly GEMMs and PDXs, provide the necessary in vivo complexity to evaluate therapeutic efficacy, pharmacokinetics, and pharmacodynamics within the brain microenvironment. For glioblastoma research focused on overcoming the BBB, an integrated approach leveraging the strengths of each model system offers the most powerful path toward developing effective clinical therapies.
The integrity of the blood-brain barrier (BBB) is a critical determinant in the pathophysiology and treatment of brain cancers, particularly glioblastoma (GBM). The BBB, a selective endothelial interface, is frequently compromised in GBM, leading to characteristic contrast enhancement on imaging. This disruption is not merely a diagnostic hallmark but a central therapeutic target and a gateway for drug delivery. Accurate characterization of the degree, pattern, and kinetics of BBB disruption via advanced imaging biomarkers is fundamental to diagnosis, treatment planning, therapeutic response assessment, and the development of novel agents. This whitepaper provides an in-depth technical guide to three core imaging modalities—Contrast-Enhanced MRI, PET Tracers, and Sonography—within the thesis context of BBB disruption in brain cancer research.
Core Modalities & Technical Principles
Contrast-Enhanced MRI
Dynamic Contrast-Enhanced (DCE) and Dynamic Susceptibility Contrast (DSC) MRI are the clinical mainstays for assessing BBB permeability. They rely on the longitudinal (T1) or transverse (T2/T2*) effects of gadolinium-based contrast agents (GBCAs) leaking from the intravascular space into the interstitial space where the BBB is compromised.
- DCE-MRI: Quantifies permeability via pharmacokinetic modeling (e.g., Tofts model). The transfer constant Ktrans (min-1) is the primary biomarker, representing the rate of contrast agent extravasation from blood plasma to the extravascular extracellular space (EES).
- DSC-MRI: Measures relative cerebral blood volume (rCBV) and flow by tracking the first-pass T2* signal drop. Leakage correction algorithms are essential to derive accurate perfusion metrics in the context of a permeable BBB.
PET Tracers
Positron Emission Tomography provides molecular-level insights into BBB disruption by utilizing radiolabeled ligands that target specific physiological processes.
- [68Ga]Ga-EDTA / [82Rb]RbCl: Small molecules that passively cross a disrupted BBB, acting as non-specific markers of increased permeability.
- Amino Acid Tracers (e.g., [11C]MET, [18F]FET, [18F]FDOPA): Utilize upregulated amino acid transporters (LAT1) at the BBB of tumor cells, providing biomarkers of both disruption and increased metabolic demand. They offer superior tumor-to-background contrast compared to MRI GBCAs, especially for non-enhancing infiltrative regions.
- Transporter-Specific Tracers (e.g., [11C]Verapamil for P-glycoprotein): Probe the functional activity of efflux transporters, whose dysfunction contributes to BBB disruption and treatment resistance.
Sonography (with Microbubbles)
Focuses Ultrasound (FUS) paired with intravascular microbubbles is both a biomarker and a modulator of the BBB. Diagnostic ultrasound can image microbubble kinetics to assess vascular perfusion. When combined with FUS, it induces temporary, localized BBB disruption (sonopermeation) for targeted drug delivery. Contrast-enhanced ultrasound (CEUS) can quantify relative blood flow and volume in brain lesions through the intact skull using advanced signal processing.
Table 1: Key Quantitative Biomarkers by Modality
| Modality | Key Biomarker(s) | Typical Units | Range in GBM (Approx.) | Physiological Correlate |
|---|---|---|---|---|
| DCE-MRI | Ktrans | min-1 | 0.05 - 0.30 | Endothelial transfer coefficient (permeability x surface area) |
| ve (extravascular volume) | % | 10% - 60% | Extravascular extracellular space fraction | |
| DSC-MRI | rCBV | Ratio to contralateral NAWM | 1.5 - 5.0 | Tumor neovascularization |
| rCBF | Ratio to contralateral NAWM | 1.2 - 4.0 | Cerebral blood flow | |
| Amino Acid PET | TBRmax (Tumor-to-Background) | Ratio | 1.5 - 3.5+ | Amino acid transporter activity |
| TTP (Time-to-Peak) | Minutes | Early (~10-20 min) vs. Late | Differential uptake kinetics | |
| CEUS | PE (Peak Enhancement) | dB or a.u. | Variable | Relative blood volume |
| AUC (Area Under Curve) | dB*sec or a.u. | Variable | Relative blood flow |
Table 2: Comparison of Modality Characteristics
| Characteristic | CE-MRI (DCE/DSC) | Amino Acid PET | Sonography (CEUS/FUS) |
|---|---|---|---|
| Spatial Resolution | High (~1 mm) | Moderate (~4-7 mm) | Low/Moderate (~1-2 mm with FUS) |
| Temporal Resolution | High (Seconds) | Low (Minutes) | Very High (Milliseconds) |
| Primary Biomarker | Vascular Permeability (Ktrans), Blood Volume (rCBV) | Transporter Activity (TBR) | Microvascular Perfusion (PE), Disruption Control |
| Key Advantage | High-resolution anatomic & physiologic data | High sensitivity for infiltrative tumor | Can actively induce/control BBB opening |
| Key Limitation | Non-specific; relies on post-contrast kinetics | Radioactive tracer; limited availability | Requires a craniotomy or specialized acoustic window for therapy |
Experimental Protocols
Protocol: DCE-MRI forKtransQuantification in a Rodent GBM Model
Objective: To quantitatively assess BBB permeability in an orthotopic GL261 murine glioblastoma model. Materials: See "The Scientist's Toolkit" below. Procedure:
- Animal Preparation: Anesthetize tumor-bearing mouse (e.g., Day 14 post-implantation). Secure in MRI-compatible stereotactic holder with temperature and respiration monitoring.
- Baseline Scans: Acquire high-resolution T2-weighted anatomical images for tumor localization. Acquire pre-contrast T1 mapping sequences (variable flip angle or inversion recovery) to establish baseline T1 values.
- Dynamic Acquisition: Initiate a fast T1-weighted gradient-echo sequence (e.g., 3D SPGR) with temporal resolution of 5-15 seconds. After 30 seconds (baseline phase), manually inject a bolus of Gd-DTPA (0.2 mmol/kg) via tail vein catheter, followed by saline flush.
- Post-Processing: Continue dynamic acquisition for 15-20 minutes. Co-register all dynamic images. Define Region of Interest (ROI) for an arterial input function (AIF, e.g., in the sagittal sinus) and for the tumor (enhancing core and peritumoral region).
- Pharmacokinetic Modeling: Convert signal intensity-time curves to contrast concentration-time curves using the baseline T1 map. Fit the data to the Extended Tofts Model using software (e.g., nordicICE, MITK) to generate voxel-wise parametric maps of Ktrans, ve, and kep (Ktrans/ve).
Protocol: [18F]FET-PET Imaging in a Preclinical GBM Model
Objective: To visualize and quantify amino acid transporter uptake in a rat F98 GBM model. Procedure:
- Tracer Injection: Anesthetize the rat. Inject ~15-20 MBq of [18F]FET via a tail vein or catheter.
- Dynamic Acquisition: Place the animal in the PET/CT scanner. Initiate a 60-minute dynamic PET acquisition list-mode, simultaneously acquiring a low-dose CT for attenuation correction.
- Image Reconstruction: Reconstruct dynamic data into frames (e.g., 6 x 30s, 4 x 60s, 5 x 300s, 1 x 600s). Apply all corrections (attenuation, scatter, randoms, decay).
- Kinetic Analysis: Co-register PET frames to a structural MRI. Draw ROIs on the tumor (based on MRI) and a contralateral healthy brain reference region (e.g., cerebellum). Generate time-activity curves (TACs). Calculate standard uptake values (SUV) and Tumor-to-Background Ratios (TBR). Perform kinetic modeling (e.g., Logan plot) if an arterial input function is available to derive distribution volume ratios.
Visualizations
Title: DCE-MRI Pharmacokinetic Modeling Pathway
Title: Multi-Modal Imaging Workflow for BBB Disruption
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials
| Item | Function in BBB Disruption Imaging | Example/Note |
|---|---|---|
| Gadolinium-Based Contrast Agent (GBCA) | T1-shortening agent for CE-MRI. Leakage indicates BBB disruption. | Gadoterate meglumine (Dotarem), Gadobutrol (Gadavist). Preclinical: Gd-DTPA. |
| Amino Acid PET Tracer | Radiolabeled substrate for LAT1 transporter; highlights tumor infiltration. | [18F]Fluoroethyltyrosine ([18F]FET) – most common in research. |
| Phospholipid-shelled Microbubbles | Ultrasound contrast agent. Oscillate in an acoustic field, enabling CEUS and mediating sonopermeation. | Definity (clinically approved), custom-targeted bubbles for research. |
| Focusing Ultrasound Transducer | Applies precise acoustic energy to target brain regions to temporarily disrupt the BBB with microbubbles. | Image-guided FUS systems (e.g., RK series, Insightec Exablate Neuro). |
| Pharmacokinetic Modeling Software | Converts dynamic imaging data into quantitative parametric maps (e.g., Ktrans, rCBV). | nordicICE, OsiriX MD, PMOD, in-house MATLAB/Python scripts. |
| Orthotopic GBM Cell Lines | Preclinical models with reproducible BBB disruption patterns. | Human: U87MG, U251. Murine: GL261, CT-2A. Rat: F98, C6. |
| MRI-Compatible Animal Monitoring System | Maintains physiology (temp, respiration) during long scans for data stability. | SA Instruments, MR-compatible isoflurane anesthesia system. |
The blood-brain barrier (BBB) presents a formidable challenge in treating primary brain tumors like glioblastoma (GBM). The core thesis framing this analysis posits that effective, transient, and safe BBB disruption is the critical rate-limiting step for delivering therapeutic agents to brain tumors. This whitepaper provides a head-to-head comparison of two principal disruption strategies—pharmacological and physical—evaluating their mechanisms, clinical efficacy, and practical implementation in contemporary trials for brain cancer.
Pharmacological Disruption: Utilizes biochemical agents to transiently modulate BBB integrity. This primarily involves targeting tight junction proteins (e.g., claudin-5, occludin, ZO-1) or inducing vasoactive responses. Physical Disruption: Employs energy-based modalities to create temporary, localized openings in the BBB. This includes techniques like focused ultrasound (FUS) with microbubbles, laser interstitial thermal therapy (LITT), or radiation.
Table 1: High-Level Comparison of Disruption Strategies
| Aspect | Pharmacological Disruption | Physical Disruption |
|---|---|---|
| Primary Mechanism | Biochemical modulation of tight junctions/transporters | Energy-induced biomechanical opening or thermal effect |
| Typical Agents/Devices | Bradykinin analogs (e.g., Cereport), VEGF, Mannitol | MRI-guided FUS systems (e.g., Exablate), LITT systems |
| Spatial Specificity | Low to moderate (often global or hemispheric) | High (MRI-guided to tumor volume) |
| Temporal Control | Moderate (minutes to hours post-infusion) | High (immediate, duration controllable) |
| Key Limitation | Systemic side effects, lack of tumor specificity | Skull heating (FUS), invasive procedures (some methods) |
| Therapeutic Window | 15-30 minutes to several hours | 4-8 hour window post-procedure |
Detailed Methodologies & Experimental Protocols
Protocol: Pharmacological Disruption with Intra-Arterial Mannitol
This classic method induces osmotic shrinkage of endothelial cells, physically pulling tight junctions apart.
- Patient Preparation: General anesthesia, femoral artery catheterization.
- Selective Cannulation: A microcatheter is advanced into the internal carotid or vertebral artery supplying the tumor region.
- Hyperosmolar Agent Infusion: 20-25% Mannitol solution is warmed to body temperature and infused via the arterial line at a rate of 3-12 mL/sec for 30 seconds. Total volume: 120-250 mL based on vessel territory.
- Chemotherapy Administration: Intra-arterial chemotherapeutic agent (e.g., Carboplatin, Melphalan) is administered 5-10 minutes post-mannitol infusion.
- Monitoring: Neurological assessment upon awakening; MRI with contrast at 24 hours to assess drug delivery (enhancement pattern) and edema.
Protocol: MRI-Guided Focused Ultrasound (MRgFUS) with Microbubbles
This non-invasive method uses ultrasound energy combined with intravenous microbubbles to mechanically disrupt the BBB.
- Patient Preparation: Head shaving, stereotactic frame fixation, or flexible transducer coupling.
- Treatment Planning: Pre-procedural MRI (T1, T2, FLAIR) is loaded into the FUS system. Target tumor and surrounding infiltrative margin are delineated.
- Sonications: Systemically administered FDA-approved microbubbles (e.g., Definity) circulate. Low-frequency ultrasound pulses (220-650 kHz) are targeted sequentially to multiple points within the planned volume. Each sonication (duration: 20-60 sec) is synchronized with the microbubble circulation.
- Real-Time Monitoring: MRI thermometry monitors for undesired heating (<2°C increase tolerated). Immediate post-sonication T1-weighted contrast MRI confirms BBB opening via new contrast enhancement.
- Therapeutic Infusion: The targeted therapeutic (e.g., checkpoint inhibitor, antibody-drug conjugate) is administered intravenously during the ~6-hour window of BBB opening.
Quantitative Data & Clinical Trial Outcomes
Table 2: Summary of Recent Clinical Trial Data (2019-2024)
| Trial/Study (PMID/ClinicalTrials.gov) | Method | Agent Delivered | Primary Outcome | Key Metric Result |
|---|---|---|---|---|
| NCT03744026 (Phase I/II) | MRgFUS + Microbubbles | Pembrolizumab (anti-PD1) | Safety & Drug Delivery | ~5x increase in tumor drug concentration (vs. contralateral). Safe in 25 recurrent GBM patients. |
| NCT03616860 | Intra-Arterial Mannitol | Carboplatin + Etoposide | Progression-Free Survival (PFS) | mPFS: 9.1 months in newly diagnosed GBM (n=42) vs. historical 6.9 months. |
| NCT02343991 | Laser Interstitial Thermal Therapy (LITT) | N/A (disruption only) | Permeability Change | Local BBB permeability (Ktrans) increased by 300-400% for 4-6 weeks post-LITT. |
| Cereport (RMP-7) Studies (Meta-analysis) | Pharmacological (Bradykinin analog) | Carboplatin | Tumor Drug Uptake | Inconsistent results; average 1.5-2x uptake increase, but high patient variability. |
| NCT04446416 (Phase 0/1) | MRgFUS + Microbubbles | Panobinostat (HDAC inhibitor) | Tumor Drug Concentration | Achieved therapeutic target concentration (≥ 50 nM) in 4 of 6 patients. |
Table 3: Safety & Practicality Comparison
| Parameter | Pharmacological (IA Mannitol) | Physical (MRgFUS) |
|---|---|---|
| Procedure Invasiveness | High (endovascular intervention) | Low (non-invasive) |
| Anesthesia Requirement | General anesthesia required | Usually conscious sedation |
| Duration of BBB Opening | ~15-30 minutes | 4-8 hours |
| Common Adverse Events | Seizures (8-12%), neurological deficits (5%), headache | Transient headache (20-30%), MRI contrast enhancement (expected), hemorrhage (<2%) |
| Treatment Cost/Complexity | High (angiography suite, interventional team) | Very High (capital equipment, multi-hour MRI slot) |
| Potential for Repeated Use | Limited by arterial access complications | High (can be repeated weekly) |
Signaling Pathways & Mechanistic Diagrams
Diagram Title: Pharmacological BBB Disruption Signaling Pathways
Diagram Title: MRgFUS Microbubble Disruption Mechanism
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents & Materials for BBB Disruption Research
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| In Vitro BBB Models | Co-culture systems to screen disruption agents. | Millicell Hanging Cell Culture Inserts with human brain microvascular endothelial cells (HBMECs), astrocytes, and pericytes. |
| Anti-Claudin-5 Antibody | Immunofluorescence/Western Blot to assess tight junction integrity. | Invitrogen Anti-Claudin-5 (4C3C2), Cat# 35-2500. |
| Anti-ZO-1 Antibody | Labels tight junction protein ZO-1 for permeability assessment. | Thermo Fisher Scientific ZO-1 Monoclonal Antibody (ZO1-1A12), Cat# 33-9100. |
| FITC-Dextran (4-70 kDa) | Tracer molecule to quantify paracellular permeability in vitro/vivo. | Sigma-Aldrich FD4 (4 kDa) & FD70 (70 kDa). |
| Mannitol (Hyperosmolar Agent) | Positive control for pharmacological BBB disruption in vivo. | Sterile 25% Mannitol injection solution for pre-clinical IA studies. |
| Definity or SonoVue Microbubbles | Clinical-grade ultrasound contrast agents for FUS-BBB disruption studies. | Lantheus Definity; Bracco SonoVue. |
| Gd-Based MRI Contrast Agent | In vivo visualization of BBB opening via contrast-enhanced T1w MRI. | Gadoteridol (ProHance) or Gadobutrol (Gadavist). |
| LC-MS/MS Kits | Quantification of therapeutic agent concentration in brain tissue post-disruption. | Waters MassTrak TDM kits or custom LC-MS/MS assay development. |
| Matrigel for In Vivo Studies | For establishing orthotopic glioblastoma mouse models for disruption testing. | Corning Matrigel Matrix, Phenol Red-free. |
The evaluation of therapeutic index (TI), defined as the ratio between the toxic dose and the therapeutic dose (TD50/ED50), is a cornerstone of preclinical and clinical oncology development. Within the specific and challenging domain of brain cancer, particularly glioblastoma (GBM), this evaluation is critically complicated by the presence of the blood-brain barrier (BBB). The BBB severely restricts the delivery of most systemic therapeutics to the tumor site, creating a profound disconnect between systemic toxicity and intracranial efficacy. This whitepaper frames the comparison of therapeutic indices across treatment modalities within the context of a broader thesis: that intentional, transient, and targeted BBB disruption (BBBD) is a necessary strategy to improve the TI for GBM therapies. By enabling greater drug delivery to the tumor, BBBD can potentially increase the effective dose (ED) at the target site without a proportional increase in systemic toxic dose (TD), thereby widening the TI and improving the overall risk-benefit profile for patients.
Quantitative Comparison of Therapeutic Modalities in GBM
The following tables summarize key quantitative data on efficacy, toxicity, and therapeutic index considerations for major GBM treatment modalities, with and without BBBD strategies.
Table 1: Standard & Emerging Modalities: Efficacy and Systemic Toxicity
| Modality | Common Agents/Techniques | Typical Reported Median Overall Survival (OS) in Newly Diagnosed GBM | Major Dose-Limiting Toxicities (Systemic) | Estimated TI (Qualitative/Notes) |
|---|---|---|---|---|
| Systemic Chemotherapy | Temozolomide (TMZ) | ~14.6 months (with RT) | Myelosuppression, nausea, hepatotoxicity | Narrow; Limited by systemic exposure and inherent resistance (MGMT). |
| Radiotherapy (RT) | Fractionated external beam | ~12-15 months (as monotherapy) | Radionecrosis, neurocognitive decline, alopecia. | Localized, but toxicity to healthy brain tissue limits dose. |
| Targeted Molecular Therapy | Bevacizumab (Anti-VEGF) | ~9-11 months (recurrent) | Hypertension, hemorrhage, thrombosis, proteinuria. | Very Narrow; Poor BBB penetration, systemic anti-angiogenic effects. |
| Immunotherapy | Immune checkpoint inhibitors (ICIs) | Varied; limited success in trials | Immune-related adverse events (irAEs: colitis, hepatitis, pneumonitis). | Narrow; Limited by poor CNS T-cell infiltration and systemic autoimmunity. |
| Tumor-Treating Fields (TTFields) | Alternating electric fields | ~20.9 months (with TMZ) | Localized skin reactions beneath arrays. | High; Non-invasive, primarily local, minimal systemic toxicity. |
Table 2: BBBD-Enhanced Modalities: Impact on Delivery and TI
| BBBD Method | Compatible Modality | Key Mechanism | Evidence of Increased Intratumoral Drug Concentration | Impact on TI Rationale |
|---|---|---|---|---|
| Chemical (e.g., Mannitol) | Intra-arterial Chemotherapy (Carboplatin, MTX) | Osmotic shrinkage of endothelial cells. | 2-10x increase in tumor drug levels post-infusion. | Potential to improve; Higher local CNS ED, but systemic TD (e.g., nephrotoxicity, neurotoxicity) remains a concern. |
| Biochemical (e.g., Bradykinin analogs) | Systemic Chemotherapy | B2 receptor-mediated opening of tight junctions. | Preclinical models show ~2x increase. | Theoretical improvement; More selective opening may spare global CNS exposure. |
| Focused Ultrasound (FUS) with Microbubbles | Systemic Doxorubicin, TMZ, Antibodies | Mechanical sonoporation of BBB. | Preclinical: 5-20x increase in drug delivery. Clinical: Evidence of gadolinium enhancement. | High potential to widen; Targeted, reversible, image-guided disruption to specific tumor regions, minimizing systemic and off-target CNS toxicity. |
| Laser Interstitial Thermal Therapy (LITT) | Adjuvant Chemotherapy | Thermal effects increase local permeability. | Local hyperthermia may increase TMZ efficacy. | Localized effect; Primarily a surgical debulking tool with adjunctive BBBD potential at cavity margins. |
Experimental Protocols for Key Evaluations
Protocol 1: In Vivo Assessment of TI with FUS-BBBD
- Objective: To determine the TI of Doxorubicin (Dox) with and without FUS-mediated BBBD in an orthotopic GL261 murine GBM model.
- Materials: GL261-luc cells, C57BL/6 mice, ultrasound system with FUS transducer, Definity microbubbles, Doxorubicin IV formulation, In Vivo Imaging System (IVIS).
- Methodology:
- Tumor Implantation: Stereotactically inject GL261-luc cells into the right striatum. Monitor tumor growth via bioluminescence weekly.
- Treatment Groups (n=10/group): a) Saline control, b) Dox alone (3 mg/kg, IV), c) FUS-BBBD alone, d) FUS-BBBD + Dox (3 mg/kg).
- FUS-BBBD Procedure: On treatment days, anesthetize mouse, inject Definity bolus. Position FUS transducer over the tumor (MRI-guided). Apply sonication parameters (0.5 MPa, 10 ms bursts, 1 Hz PRF for 60s). Immediately administer Dox IV.
- Efficacy Endpoint (ED50): Monitor survival. Calculate the dose required to achieve a 50% increase in median survival relative to control.
- Toxicity Endpoint (TD50): A separate cohort receives escalating Dox doses (± FUS) without tumors. TD50 is defined as the dose causing ≥20% body weight loss or lethal cardiotoxicity in 50% of animals within 30 days.
- TI Calculation: TI = TD50 (with/without FUS) / ED50 (with/without FUS). Compare ratios between Dox-alone and FUS+Dox groups.
- Key Analysis: HPLC-MS/MS on plasma and brain homogenates to quantify systemic vs. intracranial drug levels.
Protocol 2: In Vitro Screening for TI of BBBD-Adjuvant Compounds
- Objective: High-throughput screening of compound libraries to identify agents whose therapeutic index improves under BBB-disrupted conditions simulated in vitro.
- Materials: Primary human brain microvascular endothelial cells (HBMECs), U87-MG GBM cells, Transwell co-culture system, compound library, CellTiter-Glo viability assay.
- Methodology:
- Co-culture Model: Seed HBMECs on the apical side of a collagen-coated Transwell insert. Culture U87 cells in the basolateral chamber. Confirm BBB integrity via TEER >150 Ω·cm² and low FITC-dextran permeability.
- Simulated "BBBD": Treat apical side with a chemical disruptor (e.g., 100 ng/mL TNF-α) for 6h to reversibly compromise tight junctions (reduced TEER).
- Dose-Response Testing: Add a gradient of test compounds to the apical chamber under both intact BBB and disrupted BBB conditions.
- Dual Readout: After 72h, measure:
- Toxicity (TD): Viability of HBMECs (apical chamber).
- Efficacy (ED): Viability of U87 GBM cells (basolateral chamber).
- TI Index Calculation: For each compound and condition, calculate an in vitro TI index: IC50 (HBMEC Toxicity) / IC50 (U87 Efficacy). A compound favorable for BBBD will show a greater TI index in the "disrupted BBB" condition.
Visualizations: Pathways and Workflows
Diagram Title: Mechanism of TI Improvement via Focused Ultrasound BBBD.
Diagram Title: In Vivo Therapeutic Index Experiment Workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for BBBD and TI Research
| Item/Category | Example Product/Specifics | Primary Function in Research |
|---|---|---|
| In Vitro BBB Model | - Primary Human Brain Microvascular Endothelial Cells (HBMECs)- hCMEC/D3 Cell Line- Transwell Permeable Supports | Forms a confluent monolayer with tight junctions to screen compound permeability and toxicity in vitro under controlled conditions. |
| BBB Integrity Assays | - Millicell ERS-2 Voltohmmeter (for TEER)- FITC-Dextran (4-70 kDa)- Lucifer Yellow | Quantifies the integrity and permeability of the BBB model pre- and post-disruption (TEER = electrical resistance; tracers = flux measurement). |
| In Vivo BBBD Agents | - 25% Mannitol Solution (chemical)- Definity or SonoVue Microbubbles (FUS)- Bradykinin B2 Agonist (RMP-7) | Used in animal models to induce reversible BBB opening via osmotic, mechanical, or biochemical mechanisms. |
| Drug Concentration Analysis | - LC-MS/MS Systems (e.g., Waters Xevo TQ-S)- Fluorescently-tagged Therapeutics (e.g., DOXIL-Cy5.5) | Gold-standard for quantifying drug levels in plasma, brain, and tumor tissue homogenates. Fluorescent tags enable spatial visualization. |
| Toxicity & Viability Assays | - CellTiter-Glo 3D (for co-culture)- Annexin V/PI Apoptosis Kits- Clinical Chemistry Analyzers (for serum markers) | Measures cell death and viability in both target tumor cells and off-target endothelial/healthy cells to derive in vitro TI metrics. |
| Animal Model & Imaging | - Orthotopic GL261 or U87 GBM Models- IVIS Spectrum (bioluminescence)- High-Field MRI (7T/9.4T) with contrast (Gd-DTPA) | Provides a physiologically relevant model for GBM. Imaging is critical for tumor placement, monitoring growth, and confirming BBBD (via contrast enhancement). |
The treatment of glioblastoma (GBM) and other primary brain cancers remains profoundly limited by the blood-brain barrier (BBB). This selective barrier prevents approximately 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from reaching therapeutic concentrations in the brain parenchyma. Within the broader thesis of brain cancer research, transient and targeted BBB disruption has emerged as a pivotal strategy to enhance drug delivery. Two leading technological paradigms have advanced to clinical trials: Focused Ultrasound (FUS) with microbubbles, a physical disruption method, and Receptor-Mediated Transcytosis (RMT)-Based Therapies, a biological Trojan horse approach. This analysis provides a technical examination of recent Phase I/II trials utilizing these modalities, detailing protocols, outcomes, and the essential toolkit for preclinical and clinical investigation.
Table 1: Recent Phase I/II Trials of FUS for BBB Disruption in Glioma
| Trial Identifier / Name | Phase | Target Population | FUS Device / Parameters | Concomitant Agent(s) | Primary Endpoints & Key Results |
|---|---|---|---|---|---|
| NCT03712293 | I/II | Recurrent GBM (n=~17) | Exablate Neuro (670 kHz), sonications at ~0.7-1.0 MPa | IV Microbubbles (Definity), +/- IV Carboplatin | Feasibility/Safety: MR-guided BBB opening achieved in 100% of sonications. Efficacy: Median OS from first sonication: 8.9 months. 35% increase in drug concentration in sonicated regions. |
| NCT04446416 (BOREALIS) | I | Recurrent GBM (n=~15) | NaviFUS system (250 kHz) | IV Microbubbles (SonoVue), +/- IV Doxorubicin | Safety: No serious device-related adverse events (AEs). BBB Opening: Confirmed via MRI-Ktrans. Preliminary tumor volume reduction observed. |
| NCT03616860 | I | Recurrent GBM (n=5) | Insightec Exablate | IV Microbubbles, IV Pembrolizumab | Safety: Well-tolerated. Immunologic: Increased CD8+ T-cell tumor infiltration in some patients. Imaging: Post-sonication hyperintensity on T1w MRI confirming localized BBB opening. |
Table 2: Recent Phase I/II Trials of Novel RMT-Based Therapies in Brain Cancer
| Therapeutic Agent / Platform | Phase | Target Population | RMT Target / Payload | Key Results & Findings |
|---|---|---|---|---|
| ABBV-321 (EGFRvIII-ADC) | I | EGFRvIII+ Solid Tumors, inc. GBM (n=~50) | Anti-EGFRvIII mAb / Auristatin payload | Preliminary data showed antitumor activity in systemic EGFRvIII+ cancers. Brain penetration data pending. Dose escalation ongoing. |
| BRAIN SHUTTLE-Anti-BACE1 (Roche) | I | Healthy Volunteers / Alzheimer's | Transferrin Receptor (TfR1) / Anti-BACE1 Antibody | Pharmacodynamic: >50% reduction of CSF Aβ. Modeling: 55-fold increase in brain exposure vs. parent antibody. Demonstrates platform proof-of-concept. |
| MTX110 (Panobinostat) + Convection-Enhanced Delivery | I/II | DIPG / Recurrent GBM | Not RMT - Direct infusion | Safety: Manageable. Pharmacokinetics: Sustained drug levels in brain tissue. Efficacy: Some cases of radiographic response in DIPG. |
Detailed Experimental Protocols
Protocol for MR-Guided FUS BBB Disruption (NCT03712293)
Objective: To safely induce localized BBB disruption and enhance carboplatin delivery in recurrent GBM.
- Patient Preparation & Simulation: A stereotactic frame is affixed. Pre-treatment MRI (T1, T2, FLAIR, perfusion) is performed. Treatment targets are delineated on gadolinium-enhanced tumor margins.
- Microbubble & Drug Administration: Definity microbubbles are activated and administered via continuous IV infusion (20 μL/kg/min). Carboplatin (AUC 4-6 dose) is prepared for IV infusion.
- FUS Sonication: Patient is positioned in the Exablate Neuro device integrated with a 3T MRI. Using neuronavigation, low-intensity (0.7-1.0 MPa peak negative pressure), pulsed FUS (10 Hz pulse rate, 1% duty cycle) is applied to target locations. Real-time acoustic monitoring ensures stable cavitation.
- BBB Opening Verification: Immediate post-sonication T1-weighted MRI with gadoteridol contrast confirms BBB opening via new focal enhancement.
- Drug Infusion & Pharmacokinetics: Carboplatin infusion begins during sonication. Blood and, where feasible, cerebrospinal fluid (CSF) samples are collected at scheduled intervals for LC-MS/MS analysis of drug concentration.
- Follow-up & Safety Monitoring: Daily neurological exams for 3 days post-procedure. MRI at 24 hours to assess resolution of BBB opening and monitor for edema or hemorrhage (safety).
Protocol for Evaluating RMT-Based Antibody CNS Penetration
Objective: To quantify brain uptake of a TfR1-targeting BRAIN SHUTTLE antibody in non-human primates (NHP), a standard precursor to clinical trials.
- Radiolabeling: The test antibody (e.g., Anti-BACE1 BRAIN SHUTTLE) and a control IgG are labeled with Iodine-125 (¹²⁵I) or Zirconium-89 (⁸⁹Zr) using established methods (Iodogen or site-specific conjugation). Radiochemical purity is confirmed (>95%).
- Dosing & Biodistribution: NHPs (n=3/group) receive a single IV dose of 3-10 mg/kg of the radiolabeled antibody. Animals are monitored for clinical signs.
- Tissue Harvest & Gamma Counting: At predetermined timepoints (e.g., 1, 3, and 7 days), animals are euthanized. Blood, major organs, and brain are collected. The brain is dissected into regions (cortex, striatum, cerebellum, etc.). Tissue samples are weighed and radioactivity measured in a gamma counter.
- Autoradiography (Optional): Coronal brain sections are prepared and exposed to a phosphorimaging plate to visualize the spatial distribution of the antibody.
- Data Analysis: The percentage of injected dose per gram of tissue (%ID/g) is calculated for each sample. The brain-to-plasma ratio (or brain concentration) of the BRAIN SHUTTLE antibody is compared to the control antibody, with a >10-fold increase considered significant for platform validation.
Pathway and Workflow Visualizations
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for FUS & RMT BBB Research
| Item / Reagent | Supplier Examples | Function in Research |
|---|---|---|
| Definity or SonoVue Microbubbles | Lantheus, Bracco | Ultrasound contrast agents; oscillate in FUS field to mechanically disrupt BBB tight junctions. |
| Exablate Neuro or NaviFUS System | Insightec, NaviFUS Corp. | Integrated MRgFUS devices for precise, image-guided BBB disruption in clinical/preclinical settings. |
| Species-Specific Anti-TfR1 Antibodies | Bio-Techne, Sino Biological | Tool antibodies for validating TfR1 expression and screening shuttle candidates in vitro and in vivo. |
| Brain Shuttle or similar bsAb Platform | Roche (in-house), IONTAS, OmniAb | Bispecific antibody platforms for engineering RMT-enabled therapeutics. |
| hCMEC/D3 Cell Line | Merck Millipore | Immortalized human cerebral microvascular endothelial cells; standard for in vitro BBB models. |
| In Vivo Imaging Agents: MRI Gadoteridol, ¹²⁵I, ⁸⁹Zr | Bracco, PerkinElmer, 3D Imaging | Used to quantify BBB permeability (Ktrans) and perform biodistribution studies of RMT therapeutics. |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Waters, Sciex, Agilent | Gold standard for quantifying small molecule drug (e.g., carboplatin) concentrations in brain tissue and plasma. |
| Cynomolgus or Rhesus Non-Human Primates | Charles River, Covance | Critical preclinical model for assessing RMT therapeutic brain penetration due to similar TfR1 biology to humans. |
Cost, Accessibility, and Clinical Workflow Integration of Different Technologies
Thesis Context: Evaluating technologies for studying the blood-brain barrier (BBB) and its therapeutic disruption is a cornerstone of modern brain cancer and glioblastoma research. This guide provides a technical analysis of key methodologies, framed within the imperative to deliver effective therapeutics across the BBB.
The following table summarizes core technologies for BBB and glioblastoma research, focusing on cost, throughput, and clinical integration potential.
Table 1: Comparative Analysis of Key BBB/Glioblastoma Research Technologies
| Technology | Approx. Cost (Setup) | Approx. Cost per Sample/Run | Throughput | Clinical Integration Feasibility | Primary Application in BBB Research |
|---|---|---|---|---|---|
| Static In Vitro Transwell Models | $1K - $5K | $50 - $200 | Medium-High | Low (screening) | Permeability screening, basic transport studies |
| Dynamic In Vitro Models (Microfluidics) | $10K - $50K | $200 - $1000 | Low-Medium | Medium (niche) | Shear stress studies, advanced BBB mimicry |
| In Vivo Models (Rodent) | $50K+ (vivarium) | $500 - $5K per subject | Low | High (preclinical gold standard) | Full organism physiology, therapeutic efficacy |
| Medical Imaging (MRI/PET) | $500K - $3M+ | $500 - $5K per scan | Low | High (diagnostic standard) | Non-invasive BBB integrity mapping (e.g., Ktrans) |
| Next-Gen Sequencing (scRNA-seq) | $100K - $1M+ | $1K - $10K per library | Medium | Medium (biomarker discovery) | Tumor & BBB endothelial cell heterogeneity |
| Mass Spectrometry Imaging | $500K - $1.5M+ | $500 - $2K per slide | Low | Medium (pathology adjunct) | Spatial distribution of drugs and metabolites |
Experimental Protocols for Key Methodologies
Protocol: Establishing a Microfluidic BBB-on-a-Chip for Disruption Studies
Objective: To model the BBB and assess glioblastoma-conditioned media-induced disruption.
Materials: See "Scientist's Toolkit" below. Method:
- Chip Priming: Sterilize the PDMS microfluidic chip (e.g., two-channel, collagen-coated) with UV for 30 minutes. Prime all channels with 1X PBS.
- Hydrogel Seeding: Prepare a 4 mg/mL collagen I solution. Fill the central gel chamber. Polymerize at 37°C for 45 minutes.
- Endothelial Seeding: Trypsinize and resuspend hCMEC/D3 cells (or primary HBMECs) at 5 x 106 cells/mL. Introduce 50 µL into the "vascular" channel. Allow adhesion for 15 minutes before connecting to medium flow.
- Pericyte Differentiation & Seeding: Differentiate human pericytes from stem cells or use primary cultures. Resuspend at 2 x 106 cells/mL and seed into the opposing side of the gel chamber (abluminal side) after 24 hours.
- Culture & Barrier Maturation: Connect chips to a perfusion system. Flow endothelial growth medium (EGM-2) through the vascular channel at 10 µL/hour. Flow astrocyte/pericyte medium through the abluminal channel. Culture for 3-5 days to form a mature barrier.
- Integrity Assessment: Measure TEER daily using integrated or chopstick electrodes. Perform sodium fluorescein (376 Da) or dextran (3kDa-70kDa) permeability assays.
- Disruption Experiment: Replace the abluminal medium with conditioned media from patient-derived glioblastoma stem-like cells (GSCs). Monitor TEER and permeability over 24-72 hours. Collect effluent for cytokine analysis (ELISA).
Protocol:In VivoAssessment of BBB Disruption via Dynamic Contrast-Enhanced MRI (DCE-MRI)
Objective: To quantify the extent of BBB disruption in an orthotopic glioblastoma mouse model using a clinical imaging modality.
Method:
- Animal Model: Establish an orthotopic GL261 or patient-derived xenograft (PDX) glioblastoma model in immunocompetent or immunodeficient mice, respectively.
- MRI Preparation: Anesthetize mouse with 1-2% isoflurane. Place in MRI-compatible holder with physiological monitoring (respiration, temperature).
- Pre-contrast Scans: Acquire high-resolution T2-weighted images for tumor volume. Acquire T1 mapping sequences (variable flip angles) to establish baseline T1 values.
- Contrast Agent Administration: Intravenously inject a bolus of Gadobutrol (0.1 mmol/kg) via a tail vein catheter connected to an automated pump.
- DCE-MRI Acquisition: Immediately initiate a fast T1-weighted gradient-echo sequence (e.g., SPGR or FLASH) with high temporal resolution (~10-15 sec/phase) for 20-30 minutes.
- Data Analysis: Use dedicated software (e.g., Olea Sphere, Horos) to align images. Select an arterial input function (AIF) from a major vessel (e.g., sagittal sinus). Fit the signal intensity curves to a pharmacokinetic model (e.g., Tofts model) on a voxel-by-voxel basis to generate parametric maps of Ktrans (volume transfer constant), a key metric of BBB permeability.
Visualization of Key Concepts
Diagram: Signaling in BBB Disruption by Glioblastoma
Diagram Title: GBM-Secreted Factors Disrupt BBB Integrity
Diagram: Integrated Workflow for Evaluating BBB Disruption
Diagram Title: Translational Workflow for BBB Disruption Studies
The Scientist's Toolkit
Table 2: Essential Research Reagents & Materials for BBB Disruption Experiments
| Item | Function & Application | Example Product/Catalog | |
|---|---|---|---|
| hCMEC/D3 Cell Line | Immortalized human cerebral microvascular endothelial cell line; standard for in vitro BBB models. | Merck, SCC066 | |
| Collagen I, Rat Tail | Extracellular matrix protein for coating transwell inserts or forming hydrogel in microfluidic chips. | Corning, 354236 | |
| Transwell Permeable Supports | Polyester or polycarbonate inserts with defined pore size (e.g., 0.4 µm) for static co-culture models. | Corning, 3460 | |
| TEER Voltohmmeter | Instrument to measure Trans-Endothelial Electrical Resistance, a critical quantitative metric of barrier integrity. | World Precision Instruments, EVOM3 | |
| Sodium Fluorescein (376 Da) | Low molecular weight tracer for measuring paracellular permeability in in vitro and in vivo models. | Sigma-Aldrich, 46960 | |
| Gadobutrol (MRI Contrast Agent) | Macrocylic gadolinium-based contrast agent used in DCE-MRI to calculate Ktrans in vivo. | Bayer, Gadavist | |
| Mouse Anti-ZO-1 Antibody | Primary antibody for immunofluorescence staining of the critical tight junction protein Zonula Occludens-1. | Thermo Fisher, 33-9100 | |
| Luminex Multiplex Assay (Human Cytokine) | Multiplex panel to quantify a suite of inflammatory cytokines (VEGF, TNF-α, IL-6) in conditioned media. | R&D Systems, LXSAHM | |
| Patient-Derived GSC Lines | Biologically relevant glioblastoma stem cell lines that secrete key factors for inducing BBB disruption. | Commercial biorepositories (e.g., ATCC) or institutional banks. | |
| Microfluidic Chip (Two-Channel) | PDMS or plastic device for generating shear stress and modeling the neurovascular unit dynamically. | Emulate, Brain-Chip | Syngene, SynTwin |
Conclusion
Effective disruption of the Blood-Brain Barrier represents a cornerstone for advancing glioblastoma therapy, transitioning from a serendipitous pathological feature to a deliberately targeted therapeutic parameter. Foundational research continues to reveal the barrier's complex biology, informing smarter methodological approaches—from biologically inspired nanoparticle engineering to image-guided focused ultrasound. However, significant challenges in safety, uniformity, and clinical translation persist, demanding rigorous comparative validation. The future lies in personalized, combinatorial, and temporally controlled strategies that integrate disruption mechanisms with advanced therapeutics (e.g., immunotherapies, targeted molecular agents). Success will depend on interdisciplinary collaboration between neuro-oncologists, pharmacologists, biomedical engineers, and imaging scientists to transform BBB modulation from a formidable obstacle into a controllable gateway for curative treatments.