Controlled Drug Release from Nanocarriers: Mechanisms, Methods, and Clinical Translation
This article provides a comprehensive analysis of the methods and mechanisms for achieving controlled drug release from pharmaceutical nanocarriers.
Controlled Drug Release from Nanocarriers: Mechanisms, Methods, and Clinical Translation
Abstract
This article provides a comprehensive analysis of the methods and mechanisms for achieving controlled drug release from pharmaceutical nanocarriers. Tailored for researchers and drug development professionals, it explores the foundational principles of drug release kinetics, details advanced methodological approaches including stimuli-responsive and targeted systems, addresses key challenges in optimization and biocompatibility, and evaluates the current landscape of preclinical and clinical validation. The synthesis of these four core intents offers a state-of-the-art resource for designing next-generation nanocarriers that enhance therapeutic efficacy and accelerate clinical application.
The Fundamentals of Controlled Release: Understanding Drug Release Mechanisms and Kinetics
A drug's therapeutic window is the specific concentration range in which it is effective without causing excessive toxicity. Concentrations below this window are ineffective, while those above it are toxic. For researchers in nanocarrier development, controlled release is the engineering discipline that actively shapes and maintains drug concentration within this critical window. It moves beyond simple drug encapsulation to the precise programming of drug release kinetics, which is fundamental to enhancing therapeutic efficacy and safety.
Conventional drug delivery systems, such as immediate-release tablets, often cause significant fluctuations in plasma drug levels. This leads to a cycle of brief therapeutic effect followed by sub-therapeutic troughs and potential peak-related side effects [1] [2]. Controlled release systems are designed to overcome these limitations by releasing the active pharmaceutical ingredient (API) at a predetermined rate to maintain stable concentrations within the therapeutic window over an extended period [3]. This capability is particularly critical in fields like oncology, where many chemotherapeutic agents have a very narrow therapeutic index [4].
Troubleshooting Guide: Common Challenges in Controlled Release Experimentation
This section addresses frequent experimental hurdles and provides evidence-based solutions.
Table 1: Troubleshooting Common Controlled Release Experimental Issues
| Problem | Possible Root Cause | Potential Solutions & Investigations |
|---|---|---|
| Bursted Release Profile | • Insufficient polymer matrix density or cross-linking [2].• Poor drug-carrier compatibility or surface adsorption [5].• Damage to the nanocarrier coating (reservoir systems) [1]. | • Increase polymer concentration or cross-linker density.• Use a different polymer or incorporate hydrophobic modifiers.• Characterize nanocarrier integrity post-synthesis via TEM/SEM [6]. |
| Incomplete or Slow Release | • Overly dense or thick polymer matrix/coating [2].• Drug instability or precipitation at local pH.• Inadequate sink conditions in release media [5]. | • Optimize polymer molecular weight or coating thickness.• Verify sink conditions (ensure volume ≥ 5-10x saturation solubility).• Incorporate enzyme or pH-responsive excipients for targeted sites [7]. |
| High Polydispersity Index (PDI) in Nanocarriers | • Aggregation or instability of nanocarriers [6].• Inconsistent mixing during synthesis.• Unoptimized purification process. | • Adjust surface charge (Zeta potential) to > ±30 mV for electrostatic stabilization [6].• Use surfactants or steric stabilizers (e.g., PEG).• Introduce a fractionation step like AF4 before DLS measurement [6]. |
| Poor Correlation Between In Vitro and In Vivo Release | • Over-simplified in vitro release media not mimicking in vivo conditions (enzymes, flow, pH gradients) [8].• Failure to account for protein binding in vivo. | • Develop a biorelevant dissolution media (correct pH, enzymes, surfactants).• Use a model that accounts for hydrodynamic conditions and binding proteins.• Consider advanced modeling (e.g., machine learning) to bridge the gap [9]. |
Experimental Protocols for Characterizing Release Kinetics
Protocol: Establishing a Standard In Vitro Release Study
Objective: To determine the drug release profile of a pH-responsive polymeric nanocarrier under simulated physiological and tumor microenvironment conditions.
Materials:
- Research Reagent Solutions: Phosphate Buffered Saline (PBS) at pH 7.4, Acetate Buffer at pH 6.5 and pH 5.0, PBS with 0.1% w/v Tween 80 (to maintain sink conditions), dialysis membranes with appropriate molecular weight cut-off (MWCO), nanocarrier suspension.
- Equipment: USP Type II (paddle) dissolution apparatus, HPLC system with UV-Vis detector, dynamic light scattering (DLS) instrument.
Methodology:
- Nanocarrier Characterization: Prior to release studies, characterize the nanocarrier batch for particle size, PDI, and zeta potential using DLS to ensure quality and reproducibility [6].
- Sink Condition Validation: Determine the solubility of the drug in each release medium. The volume of medium used should be at least 5-10 times the volume required to create a saturated solution of the drug dose.
- Release Study Setup:
- Place a precise volume of nanocarrier suspension (equivalent to a known drug dose) into a dialysis tube sealed at both ends.
- Immerse the dialysis tube in the release vessel containing a known volume (e.g., 500 mL) of pre-warmed (37°C) release medium, stirred at 50 rpm.
- Perform the study in triplicate for each pH condition (pH 7.4, 6.5, and 5.0) to simulate blood, tumor microenvironment, and endolysosomal conditions, respectively [4] [7].
- Sampling and Analysis:
- At predetermined time intervals, withdraw a known aliquot (e.g., 1 mL) from the release medium and replace it with an equal volume of fresh, pre-warmed medium to maintain sink conditions.
- Filter the withdrawn samples (0.45 µm filter) and analyze the drug concentration using a validated HPLC method.
- Continue the experiment until at least 80% of the drug has been released or a plateau is reached.
Protocol: Data Analysis and Release Kinetics Modeling
Objective: To fit experimental release data to mathematical models to identify the predominant release mechanism.
Methodology:
- Data Compilation: Calculate the cumulative percentage of drug released versus time.
- Model Fitting: Fit the release data to the following key mathematical models using statistical software. The table below summarizes the models and their interpretations [5].
Table 2: Key Mathematical Models for Analyzing Drug Release Kinetics
| Model Name | Equation | Mechanistic Interpretation |
|---|---|---|
| Zero-Order | ( Qt = Q0 + k_0 t ) | Constant release rate over time, ideal for controlled release systems. ( Qt ) is the amount of drug released at time ( t ), ( k0 ) is the rate constant. |
| First-Order | ( \log Qt = \log Q0 + \frac{k_1 t}{2.303} ) | Release rate is concentration-dependent. Common for water-soluble drugs in porous matrices. |
| Higuchi | ( Qt = kH \sqrt{t} ) | Drug release from an insoluble matrix is controlled by Fickian diffusion. ( k_H ) is the Higuchi dissolution constant. |
| Korsmeyer-Peppas (Power Law) | ( \frac{Mt}{M\infty} = k t^n ) | Empirically describes drug release from polymeric systems. The release exponent ( n ) indicates the release mechanism (e.g., Fickian diffusion, Case-II transport, anomalous transport) [5]. |
- Model Selection: The best-fit model is typically selected based on the highest correlation coefficient (R²) and the lowest Akaike Information Criterion (AIC). The Korsmeyer-Peppas model is particularly useful for identifying the underlying release mechanism in the initial 60% of release.
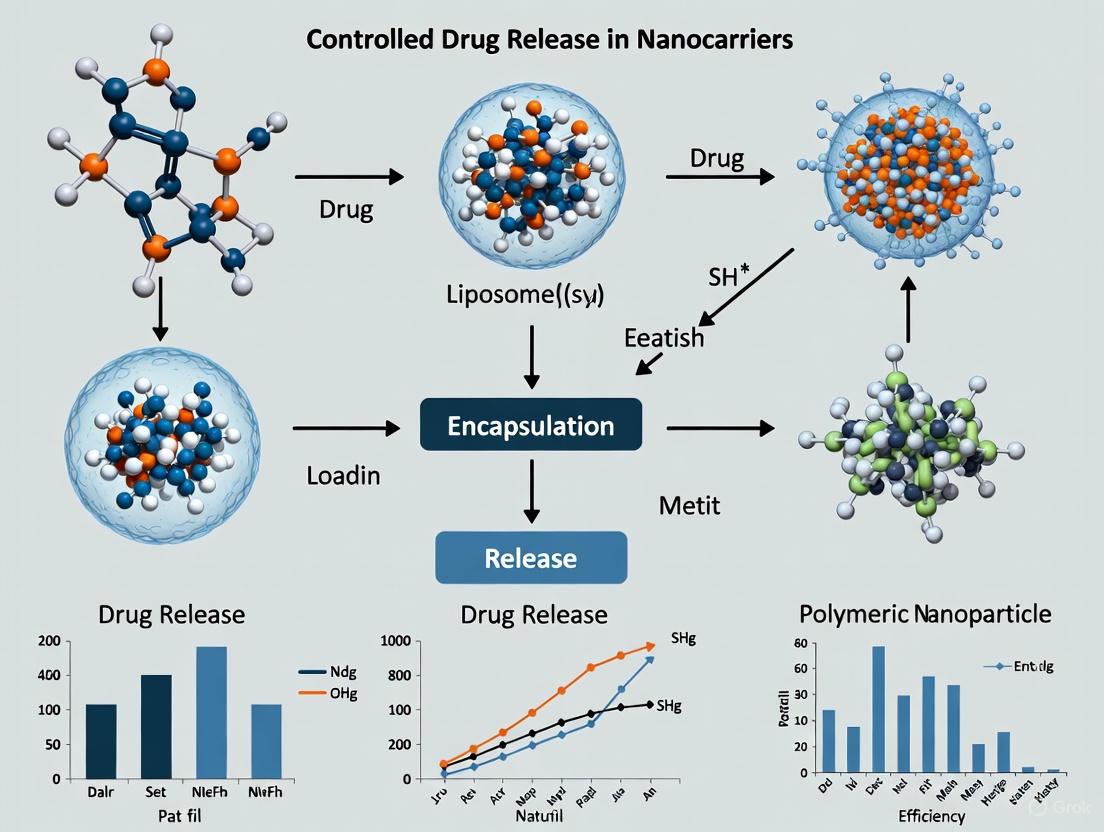
Visualizing the Experimental Workflow
The following diagram illustrates the logical workflow for developing and characterizing a controlled-release nanocarrier system, from formulation to data interpretation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Controlled Release Nanocarrier Development
| Reagent / Material | Function & Rationale | Common Examples |
|---|---|---|
| pH-Sensitive Polymers | Backbone of nanocarriers that degrade or swell in response to acidic pH (e.g., tumor microenvironment, endosomes). Enable targeted drug release [4] [7]. | Poly(L-histidine), Eudragit series (S100, L100), Poly(β-amino esters). |
| Ionizable Lipids | Critical component of lipid nanoparticles (LNPs). Their headgroup protonation/deprotonation in different pH environments can facilitate endosomal escape and content release [4] [10]. | DLin-MC3-DMA, ALC-0315. |
| Hydrophilic Polymers | Used to create gel-forming matrix tablets or as stealth coatings on nanocarriers to reduce opsonization and prolong circulation half-life [1] [2]. | Hydroxypropyl methylcellulose (HPMC), Polyethylene glycol (PEG), Polyvinyl alcohol (PVA). |
| Enzyme-Sensitive Linkers | Cross-linkers or building blocks that are cleaved by enzymes overexpressed in disease sites (e.g., matrix metalloproteinases in tumors). Provide a biological trigger for release [7]. | MMP-cleavable peptides (e.g., GPLG↓VRG), hyaluronic acid (cleaved by hyaluronidase). |
| Osmotic Agents | Core component in osmotic pump systems. They generate osmotic pressure to push the drug solution out through a laser-drilled orifice at a constant rate, independent of environmental pH [1]. | Sodium chloride, potassium phosphate, sucrose. |
| Targeting Ligands | Molecules attached to the nanocarrier surface to facilitate active targeting to specific cell types via receptor-mediated endocytosis, enhancing site-specific release [4] [7]. | Folate, monoclonal antibodies, transferrin, peptides (e.g., RGD). |
Advanced Topics: Integrating Machine Learning and Pathway Analysis
Machine Learning in Release Kinetics Prediction
Traditional mathematical models are powerful but can struggle with the complexity of multi-stimuli responsive systems. Machine learning (ML) is emerging as a robust tool for modeling and predicting drug release. A recent study demonstrated that ML regression models like Decision Tree Regression (DTR) can achieve exceptional predictive accuracy (R² > 0.99) for drug release from complex polymeric matrices by learning from large datasets generated via computational fluid dynamics (CFD) [9]. This data-driven approach can significantly accelerate the formulation optimization process.
Molecular Pathways in Colorectal Cancer and Nanocarrier Design
Understanding disease-specific molecular pathways is crucial for designing intelligent, targeted nanocarriers. The following diagram outlines key pathways in Colorectal Cancer (CRC) that can be exploited for controlled release, illustrating the connection between molecular biology and delivery system engineering.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between "Extended Release" (ER) and "Controlled Release" (CR)? While often used interchangeably, there is a technical distinction. Extended-release (ER) is a broad term for any dosage form that prolongs the release of an API. Controlled-release (CR) is a specific type of ER designed to release the drug at a constant, predetermined rate (zero-order kinetics) by using advanced mechanisms like osmotic pumps, maintaining plasma levels within the therapeutic window with minimal fluctuation [1].
Q2: Why is my nanocarrier formulation showing high batch-to-batch variability in release profiles? Inconsistent physicochemical properties like particle size and PDI are the most common culprits. Strict control over synthesis parameters (e.g., mixing speed, solvent addition rate, temperature) and purification processes is essential. Implement rigorous in-process controls and characterize every batch for size, PDI, and zeta potential using DLS before proceeding to release studies [6].
Q3: How can I determine if my nanocarrier's release mechanism is diffusion- or erosion-controlled? Fit your release data to the Korsmeyer-Peppas model. The release exponent (n) value provides insight. For spherical matrices, an n ≈ 0.43 suggests Fickian diffusion, while n ≈ 0.85 indicates Case-II transport (relaxation/erosion controlled). An n value between 0.43 and 0.85 signifies anomalous transport, a combination of both diffusion and erosion [5].
Q4: Our in vitro release data looks excellent, but the in vivo efficacy is poor. Where should we focus our investigation? This disconnect often arises from biological barriers not accounted for in in vitro tests. Key areas to investigate are:
- Protein Corona: Serum proteins adsorb onto nanocarriers in vivo, altering their surface properties and targeting capability [6] [10].
- Premature Clearance: The mononuclear phagocyte system (MPS) may rapidly clear nanocarriers. Consider modifying the surface with "stealth" coatings like PEG.
- Biological Sink: The drug may be rapidly distributed, metabolized, or cleared in vivo, preventing local accumulation.
Q5: Are there strategies to create a multi-pulsed (chronotherapeutic) release profile from a single nanocarrier system? Yes, this is an advanced area of research. Strategies include:
- Multi-layered Systems: Coating drug cores with polymers of different thicknesses and degradation rates.
- Pulsatile Systems: Using a rupturable coating that dissolves after a specific time lag.
- Multi-Material Nanocarriers: Designing particles with a core-shell structure where each compartment responds to a different stimulus (e.g., pH then enzyme), resulting in staged release [2].
In pharmaceutical nanotechnology, controlling the release of an active pharmaceutical ingredient (API) is fundamental to enhancing therapeutic efficacy and reducing systemic side effects. Controlled-release nanocarriers are designed to deliver drugs in a spatiotemporally controlled manner, which helps maintain drug concentration within the therapeutic window—between the minimum effective concentration (MEC) and the minimum toxic concentration (MTC) [11]. The primary mechanisms governing this controlled release are diffusion-controlled, solvent-controlled, and degradation-controlled release. For researchers developing nanocarrier-based drug delivery systems (DDS), a deep understanding of these mechanisms is critical for rational design and overcoming common experimental challenges. This guide provides a technical foundation and practical troubleshooting support for investigating these core release mechanisms.
Core Drug Release Mechanisms: Principles and Analysis
The following table summarizes the key characteristics, driving forces, and typical release profiles of the three primary drug release mechanisms.
Table 1: Fundamental Drug Release Mechanisms in Nanocarriers
| Mechanism | System Design | Driving Force | Release Kinetics | Key Influencing Factors |
|---|---|---|---|---|
| Diffusion-Control [11] [12] | Reservoir system (drug core surrounded by polymer membrane) or Matrix system (drug dispersed in polymer matrix) | Concentration gradient across the polymer barrier [11] | First-order (matrix); Zero-order (reservoir, ideal case) [11] | Membrane thickness, drug solubility, polymer porosity, diffusion coefficient [11] |
| Solvent-Control [11] | Osmotic pumps (semi-permeable membrane) or Swelling systems (glassy hydrophilic polymers) | Osmotic pressure gradient or Water absorption/polymer swelling [11] | Zero-order (osmosis); Often complex, can be zero-order (swelling) [11] | Membrane permeability, osmotic pressure, polymer relaxation rate, cross-link density [11] |
| Degradation-Control [11] | Systems comprising biodegradable polymers (e.g., polyesters, polyamides) | Chemical or enzymatic cleavage of polymer chains [11] | Often correlated with degradation rate (e.g., first-order, biphasic) | Polymer crystallinity, molecular weight, pH, enzyme concentration [11] |
Diffusion-Controlled Release
Diffusion is a mass transport process where particles move from a region of higher concentration to a region of lower concentration [13]. In nanocarriers, this mechanism is governed by Fick's laws of diffusion [13].
- Fick's First Law describes the steady-state flux (J):
J = -D (dC/dx), whereDis the diffusion coefficient, anddC/dxis the concentration gradient [13]. - Fick's Second Law describes how the concentration changes with time at a definite location:
∂C/∂t = D (∂²C/∂x²)[13].
Two main types of diffusion-controlled systems are prevalent:
- Reservoir Systems (Membrane Systems): The drug is contained in a core surrounded by a polymeric membrane. Drug release is controlled by diffusion through this rate-controlling membrane [11] [12].
- Matrix Systems (Monolithic Systems): The drug is uniformly dispersed or dissolved throughout a polymer matrix. Release occurs as the drug diffuses from the matrix to the surrounding medium [11] [12].
The following diagram illustrates the fundamental principles of the diffusion-controlled release mechanism.
Solvent-Controlled Release
This mechanism relies on the transport of solvent (typically water) into the drug carrier. It is subdivided into two categories:
- Osmosis-Controlled Release: The system is encapsulated by a semi-permeable membrane. Water flows into the core due to an osmotic gradient, building up internal pressure that pushes the drug solution out through a laser-drilled orifice [11] [12]. This mechanism can achieve a constant (zero-order) release rate [11].
- Swelling-Controlled Release: This involves glassy, hydrophilic polymers. Upon contact with water, the polymer swells as water diffuses in, transitioning from a glassy to a rubbery state. The drug then diffuses out through the swollen polymer network. The release rate depends on both the water diffusion rate and the polymer chain relaxation rate [11].
The diagram below outlines the sequential process of solvent-controlled release.
Degradation-Controlled Release
In this mechanism, drug release is regulated by the chemical breakdown of the carrier material itself. Biodegradable polymers, such as poly(lactic-co-glycolic acid) (PLGA) and other polyesters, are commonly used. Degradation can occur via:
- Bulk Erosion: The polymer degrades uniformly throughout the matrix.
- Surface Erosion: Degradation is confined to the surface of the device, which can lead to a more constant release rate.
The degradation process itself can be driven by hydrolysis (cleavage of chemical bonds by water) or by enzymatic activity in the target environment [11].
Essential Experimental Protocols for Mechanism Investigation
Protocol: In Vitro Drug Release Kinetics Study
Objective: To characterize and model the drug release profile from a nanocarrier formulation under simulated physiological conditions.
Materials:
- Phosphate Buffered Saline (PBS), pH 7.4: Standard dissolution medium simulating physiological pH [11].
- Dialysi s Bag or Membrane: Acts as a barrier between the nanocarrier suspension and the release medium, simulating a diffusion path [6].
- UV-Vis Spectrophotometer or HPLC: For quantitative analysis of drug concentration in the release medium [6].
- Stirring Plate and Water Bath: To maintain constant temperature (e.g., 37°C) and hydrodynamics (sink conditions) [6].
Methodology:
- Sample Preparation: Place a known volume of nanocarrier suspension (with precise drug content) into a pre-hydrated dialysis bag. Seal the bag securely.
- Dissolution Setup: Immerse the dialysis bag in a vessel containing a sufficient volume of pre-warmed PBS (37°C) to maintain sink conditions. Ensure constant, gentle agitation.
- Sampling: At predetermined time intervals, withdraw a fixed aliquot of the release medium from the vessel.
- Replenishment: Immediately replace the withdrawn volume with fresh, pre-warmed PBS to maintain a constant volume and sink conditions.
- Analysis: Quantify the drug concentration in each aliquot using a pre-validated analytical method (e.g., UV-Vis at λ_max, HPLC).
- Data Processing: Calculate the cumulative drug release (%) versus time. Plot the release profile and fit the data to various mathematical models (e.g., Zero-order, First-order, Higuchi, Korsmeyer-Peppas) to identify the predominant release mechanism [11].
Protocol: Nanocarrier Physicochemical Characterization
Objective: To determine key physical properties of the nanocarrier that directly influence its release behavior and performance.
Materials:
- Dynamic Light Scattering (DLS) Instrument: For measuring particle size, size distribution (PDI), and zeta potential [6].
- Transmission Electron Microscopy (TEM) or Scanning Electron Microscopy (SEM): For visualizing particle morphology, size, and structure [6].
- Atomic Force Microscopy (AFM): For high-resolution topographical imaging of nanocarriers [6].
Methodology:
- Particle Size & PDI: Dilute the nanocarrier suspension appropriately with a filtered solvent (e.g., water). Measure the hydrodynamic diameter and PDI using DLS. A PDI value <0.3 is generally considered acceptable for a monodisperse system [6].
- Zeta Potential: Dilute the sample and measure the electrophoretic mobility to determine zeta potential, which indicates colloidal stability. Values greater than ±30 mV typically suggest good physical stability [6].
- Morphology: Deposit a diluted drop of nanocarrier suspension onto a TEM grid or SEM stub. Allow to dry and image under the microscope to confirm the DLS size data and observe the shape and surface characteristics [6].
Troubleshooting Guide: Common Experimental Challenges
Table 2: Frequently Encountered Problems and Solutions in Release Studies
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Burst Release [11] | Drug adsorbed on or near the particle surface; Inadequate encapsulation; Fast water penetration. | Modify preparation method to enhance encapsulation efficiency; Increase polymer wall thickness; Use a hydrophobic coating or cross-linking [11]. |
| Incomplete Release | Poor drug solubility in release medium; Insufficient degradation of polymer; Drug-polymer interactions. | Incorporate solubilizing agents (e.g., surfactants) in the release medium; Use polymers with faster degradation kinetics; Optimize drug-polymer compatibility [11]. |
| Irreproducible Release Profiles | Inconsistent nanocarrier batch quality (size, PDI); Aggregation during release study; Variable experimental conditions. | Standardize nanocarrier synthesis and purification protocols; Include stabilizers to prevent aggregation; Strictly control temperature, pH, and agitation speed [6]. |
| Deviation from Expected Kinetics | Complex, overlapping release mechanisms (e.g., diffusion and swelling); Changes in carrier structure during release. | Conduct release studies under different conditions (e.g., pH, enzyme presence) to deconvolute mechanisms; Use microscopy (SEM/TEM) to observe structural changes post-release [11] [6]. |
| Nanocarrier Instability | Low zeta potential leading to aggregation; Chemical degradation during storage; Ostwald ripening. | Optimize formulation to increase surface charge; Lyophilize with appropriate cryoprotectants; Store under inert conditions and appropriate temperature [6]. |
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Controlled-Release Nanocarrier Development
| Reagent/Material | Function | Example Use Cases |
|---|---|---|
| Biodegradable Polymers (e.g., PLGA, PLA) | Form the degradable matrix or membrane of the nanocarrier, controlling release rate [11]. | Matrix systems for sustained release; Micro/Nanospheres for encapsulation [11]. |
| Polyethylene Glycol (PEG) | Surface coating agent to impart "stealth" properties, reducing opsonization and extending circulation half-life [11]. | PEGylation of liposomes, polymeric nanoparticles to enhance passive targeting via the EPR effect [11]. |
| Lipids (Phospholipids, Cholesterol) | Building blocks for lipid-based nanocarriers like liposomes and solid lipid nanoparticles (SLNs) [6]. | Forming biocompatible vesicles for encapsulating hydrophilic and hydrophobic drugs [6]. |
| Targeting Ligands (e.g., Folate, Antibodies, Peptides) | Surface functionalization moieties for active targeting to receptors overexpressed on specific cells [11] [7]. | Functionalizing nanoparticles for targeted delivery to cancer cells (e.g., folate for CRC cells) [11] [7]. |
| Disintegrants & Porogens (e.g., Crospovidone, NaCl) | Agents that create channels or cause the structure to break apart, facilitating drug release [14]. | Incorporated into matrix systems to modify release profiles from diffusion-controlled to erosion-controlled [14]. |
FAQ: Addressing Critical Research Questions
Q1: How can I differentiate between diffusion-controlled and degradation-controlled release in my experimental data? A: Fit your release data to mathematical models. A good fit to the Higuchi model (cumulative release ∝ √time) often suggests a diffusion-controlled mechanism from a matrix system. For degradation control, monitor both mass loss of the polymer and drug release; if they correlate closely, degradation is likely the primary driver. Additionally, observe the carrier morphology post-release—significant structural disintegration points toward degradation-control [11].
Q2: My nanocarrier formulation shows high initial burst release. How can I mitigate this? A: Burst release is often caused by poorly encapsulated drug or drug crystals on the surface. Solutions include: 1) Optimizing your preparation method (e.g., double emulsion for hydrophilic drugs) to improve encapsulation efficiency. 2) Applying a sealing or coating layer (e.g., with a polyelectrolyte or polymer shell). 3) Washing the final nanocarrier product thoroughly to remove surface-bound drug [11].
Q3: Why is achieving zero-order (constant rate) release kinetics challenging with nanocarriers? A: The high surface-area-to-volume ratio of nanocarriers makes them prone to initial rapid release. True zero-order release requires the release area and the concentration gradient to remain constant, which is difficult to maintain in a shrinking or degrading nanoparticle. Reservoir systems (nanocapsules) and swelling-controlled systems that exhibit a constant moving diffusion front are your best candidates for approaching zero-order kinetics [11].
Q4: How does the nanocarrier's size and surface charge influence drug release? A: Size: Smaller particles have a larger surface area for diffusion, which can lead to a faster initial release rate. Surface Charge (Zeta Potential): A high zeta potential (positive or negative) improves colloidal stability by preventing aggregation. If particles aggregate during the release study, the effective surface area changes, leading to altered and irreproducible release kinetics [6].
Frequently Asked Questions (FAQs)
Q1: What is the primary goal of achieving zero-order release kinetics in a drug delivery system?
Zero-order release describes a system where the drug is released at a constant rate, independent of its concentration [15]. This is the ultimate goal for many controlled-release systems because it maintains a stable, therapeutic concentration of the drug in the blood for a prolonged period [15] [5]. This leads to better patient compliance, reduces the frequency of drug administration, and minimizes the risk of side effects caused by plasma concentration fluctuations, which is especially critical for drugs with a narrow therapeutic index [15].
Q2: When should I use the Korsmeyer-Peppas model over other release kinetic models?
The Korsmeyer-Peppas model is particularly useful when the exact drug release mechanism from a polymeric system is unknown or when multiple release phenomena are involved [16] [17] [18]. It is a semi-empirical model that is often applied to analyze the first 60% of the release curve to understand the underlying transport mechanism [17]. Its strength lies in its ability to analyze non-Fickian diffusion, which is common in polymeric systems, by using a diffusional exponent, 'n', to provide insight into the release mechanism [15] [18].
Q3: My release data shows an initial burst release. Is this normal for nanocarrier systems?
Yes, an initial burst release is a common characteristic of many nanocarrier systems, including those made from polymers like PLGA [17]. This often occurs due to the rapid release of drug molecules attached to the surface or residing in the peripheral layers of the nanoparticle [17]. Following this initial burst, a slower, more sustained release phase is typically observed, which is often dominated by the diffusion of the drug through the polymer matrix and the subsequent degradation of the polymer itself [17].
Q4: How do I determine if my drug release is controlled by Fickian diffusion or other mechanisms using the Korsmeyer-Peppas model?
The value of the release exponent 'n' in the Korsmeyer-Peppas model is used to interpret the release mechanism. For a thin film formulation, the general interpretation is as follows [15] [19]:
- n = 0.5: Indicates Fickian diffusion, where release is controlled by the concentration gradient.
- 0.5 < n < 1.0: Indicates non-Fickian or anomalous transport, where release is governed by a combination of diffusion and polymer relaxation.
- n = 1.0: Indicates Case-II transport, which is purely relaxation-controlled.
- n > 1.0: Indicates super Case-II transport. It is crucial to consult literature for the specific 'n' values corresponding to your delivery system's geometry (e.g., spherical, cylindrical) [16].
Q5: Why is my drug release profile not fitting well with any standard kinetic model?
Poor model fitting can occur for several reasons. The release process may be complex, involving a combination of diffusion, swelling, and erosion mechanisms that a single model cannot capture [19]. The model might be applied outside its valid range; for example, the Korsmeyer-Peppas model is recommended only for the first 60% of the release data [17]. Furthermore, specific experimental conditions, such as changes in osmotic stress or ionic strength in the release medium, can significantly alter the release kinetics, leading to non-linear profiles that are difficult to fit with simple models [16].
Troubleshooting Guides
Issue 1: Failure to Achieve Zero-Order Release Profile
Problem: The drug release rate from your matrix system decreases over time, showing first-order kinetics instead of the desired constant, zero-order release.
| Possible Cause | Solution |
|---|---|
| Insufficient multi-diffusion pathways | Incorporate a combination of release-controlling polymers with different characteristics. For example, use methacrylic acid copolymers (e.g., Eudragit) in combination with a swellable polymer like HPMC to create a homogenous, intermeshing gel structure that provides a multi-step diffusion system [15]. |
| Poorly controlled reservoir system | For reservoir-type devices, ensure the coating membrane is uniform and acts as a true rate-controlling barrier. The core should function as a saturated drug reservoir. Optimize the coating process and the permeability of the polymer membrane [15] [19]. |
| Rapid erosion of the matrix | If using an erodible system, adjust the polymer composition and ratio to slow down the erosion process. Using a non-eroding polymer network that is formed by heat curing can provide a more stable structure for constant release [15]. |
Issue 2: Interpreting the Diffusional Exponent (n) in the Korsmeyer-Peppas Model
Problem: You have calculated the 'n' value but are unsure how to interpret it for your specific drug delivery system.
| System Geometry | n value for Fickian Diffusion | n value for Case-II Transport (Polymer Relaxation) | Reference |
|---|---|---|---|
| Thin Film | 0.5 | 1.0 | [15] [19] |
| Cylinder | 0.45 | 0.89 | [19] |
| Sphere | 0.43 | 0.85 | [19] |
Action Plan:
- Confirm Geometry: First, correctly identify the geometry of your drug delivery system (e.g., a spherical nanoparticle, a cylindrical implant, or a thin film).
- Refer to Table: Use the table above to find the critical 'n' values for your system's geometry.
- Interpret Mechanism: Compare your calculated 'n' value to the reference values.
- If n is equal to the Fickian diffusion value, release is diffusion-controlled.
- If n is between the Fickian and Case-II values, release is anomalous (a combination of diffusion and relaxation).
- If n is equal to the Case-II value, release is controlled by polymer relaxation/swelling [19].
Issue 3: Managing Burst Release from Polymeric Nanoparticles
Problem: Your polymeric nanoparticle formulation exhibits a significant initial burst release, depleting a large portion of the drug too quickly.
| Possible Cause | Solution |
|---|---|
| Drug adsorbed on the surface | Modify the synthesis technique or include a washing step after nanoparticle formation to remove surface-bound drug molecules [17]. |
| High porosity and fast water penetration | Optimize the formulation by adjusting the polymer molecular weight, lactide/glycolide (LA:GA) ratio in PLGA, or adding excipients to reduce initial porosity and slow down water ingress [17]. |
| Low drug-polymer interaction | Consider functionalizing the polymer or the drug to promote stronger interactions, thereby reducing the diffusion of drug molecules near the surface [17]. |
Key Mathematical Models for Release Kinetics
The table below summarizes the most common mathematical models used to analyze in-vitro drug release data.
| Model Name | Equation | Application & Release Mechanism |
|---|---|---|
| Zero-Order | Q<sub>t</sub> = Q<sub>0</sub> + K<sub>0</sub>t [15] |
Describes systems where drug release is constant over time (ideal for controlled release). Release rate is independent of drug concentration [15] [5]. |
| First-Order | ln Q<sub>t</sub> = ln Q<sub>0</sub> + K<sub>1</sub>t [17] |
Describes systems where the release rate is concentration-dependent. The release rate declines over time as the drug concentration in the dosage form decreases [15] [5]. |
| Higuchi | Q = K<sub>H</sub>t<sup>1/2</sup> [15] [5] |
Describes drug release from an insoluble matrix as a square root of time-dependent process based on Fickian diffusion. It is often used for systems where the drug is dispersed in a solid matrix [15] [5]. |
| Korsmeyer-Peppas | M<sub>t</sub>/M<sub>∞</sub> = Kt<sup>n</sup> [16] [17] |
A semi-empirical model used to analyze the release mechanism from polymeric systems when the mechanism is unknown or more than one phenomenon is involved. The diffusional exponent 'n' characterizes the release mechanism [15] [16]. |
| Hixson-Crowell | Q<sub>0</sub><sup>1/3</sup> - Q<sub>t</sub><sup>1/3</sup> = K<sub>HC</sub>t [15] |
Describes release from systems where the surface area and diameter of the drug particles change over time, such as in erodible systems [15]. |
Experimental Protocols
Protocol 1: Preparation of Multi-Step Diffusion-Based Matrix Tablets for Zero-Order Release
This protocol is adapted from a study aiming to achieve pH-independent, zero-order release for a freely water-soluble drug [15].
1. Materials and Equipment:
- Active Pharmaceutical Ingredient (API): Freely water-soluble model drug.
- Release-Controlling Polymers: Eudragit RS/RL and hydroxypropyl methylcellulose (HPMC) K100M.
- Excipients: Colloidal silicon dioxide (glidant), calcium phosphate dibasic dihydrate (disintegrant), microcrystalline cellulose and lactose monohydrate (diluents), magnesium stearate (lubricant).
- Granulating Solution: Polyvinyl pyrolidone (PVP) K30 (binder) and triethyl citrate (TEC, plasticizer) in solvent.
- Equipment: Planetary mixer, wet granulation equipment, drying oven, tablet compression machine, coating pan.
2. Methodology:
- Step 1: Dry Blending. Screen the API, polymers (Eudragit RS/RL, HPMC), and all excipients (except lubricant) through a 20-mesh sieve. Dry blend them in a planetary mixer [15].
- Step 2: Wet Granulation. Wet the blended mixture with a binder solution comprising PVP K30 and triethyl citrate. This aids in granule formation [15].
- Step 3: Drying and Lubrication. Dry the resulting wet granules. Afterwards, blend the dried granules with the lubricant (magnesium stearate) [15].
- Step 4: Compression. Compress the final blend into round tablets with a target hardness of approximately 15 KP [15].
- Step 5: Heat Curing. Heat cure the core tablets at 35°C for two hours. This critical step allows the methacrylic acid copolymers to form a structure that entraps the drug molecules, creating a multi-diffusional network [15].
- Step 6: (Optional) Coating. For further release control, the core tablets can be coated with a minimal weight gain (e.g., 5% w/w) of a controlled-release polymer membrane (e.g., Eudragit RS/RL). The coated tablets must also be dried and cured at 35°C for two hours [15].
3. Release Kinetics Analysis:
- Use USP Apparatus II (paddle method) at 100 rpm with sequential dissolution media (e.g., 2 hours at pH 1.2 followed by 10 hours at pH 6.8) to obtain the drug release profile [15].
- Fit the cumulative release data to various kinetic models (Zero-order, First-order, Higuchi, Korsmeyer-Peppas) to analyze the release mechanism and confirm the achievement of zero-order kinetics [15].
Protocol 2: Analyzing Drug Release from Liposomes using the Korsmeyer-Peppas Model
This protocol outlines the use of the Korsmeyer-Peppas model to interpret non-linear drug release data from liposomes, which can be affected by the external environment [16].
1. Materials and Equipment:
- Liposomal Formulation: Large unilamellar vesicle (LUV) dispersions.
- Drugs: Hydrophilic (e.g., caffeine) and lipophilic (e.g., hydrocortisone) drugs.
- Release Media: Phosphate buffered saline (PBS) of varying ionic strengths/tonicity (e.g., 65 mOsm/kg and 300 mOsm/kg) to simulate osmotic stress.
- Dialysis Barriers: Low-retention barriers (e.g., regenerated cellulose membrane) and high-retention barriers (e.g., Permeapad).
- Equipment: Dialysis apparatus, UV-Vis spectrophotometer or HPLC for drug quantification.
2. Methodology:
- Step 1: Liposome Preparation and Characterization. Prepare LUV dispersions using a method like thin-film hydration and extrusion. Characterize the liposomes for size, polydispersity index (PDI), zeta potential (ZP), and encapsulation efficiency (EE) [16].
- Step 2: In Vitro Release Study. Place the liposomal dispersion in the donor compartment of a dialysis device. The acceptor compartment contains the release medium (PBS). Maintain the system under sink conditions where possible [16].
- Step 3: Sampling. At predetermined time intervals, withdraw samples from the acceptor compartment and replace with fresh medium to maintain volume. Analyze the samples for drug concentration [16].
- Step 4: Data Collection. Calculate the cumulative amount of drug released (
M_t) and the fractional release (M_t / M_∞) over time, whereM_∞is the total amount of drug released at the end of the experiment.
3. Data Fitting with Korsmeyer-Peppas Model:
- Input the fractional release (
M_t / M_∞) and time (t) data into non-linear regression software. - Fit the data to the Korsmeyer-Peppas equation:
M_t / M_∞ = K * t^n[16]. - Obtain the release constant (K) and the release exponent (n).
- Interpret the value of 'n' to understand the drug release mechanism from the liposomes under different osmotic conditions [16].
Experimental Workflow and Model Selection
The following diagram illustrates a logical workflow for selecting and applying kinetic models to analyze drug release data.
Research Reagent Solutions
The table below lists key materials used in the featured experiments for developing controlled release dosage forms.
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Methacrylic Acid Copolymers (Eudragit RS/RL) | Non-eroding, pH-independent release-controlling polymers that form a permeable membrane for drug diffusion. RL is more permeable than RS [15]. | Used in matrix tablets to create a multi-diffusional network for zero-order release of freely soluble drugs [15]. |
| Hydroxypropyl Methylcellulose (HPMC) | A swellable hydrophilic polymer that forms a gel layer upon hydration, controlling drug release through diffusion and erosion [15]. | Combined with Eudragit polymers to form a homogenous, intermeshing gel structure in matrix tablets [15]. |
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer used in nanocarriers. Release kinetics can be controlled by adjusting its molecular weight and LA:GA ratio [17]. | Used in nanoparticles for sustained release; shows biphasic release (initial burst followed by slow release) [17]. |
| Triethyl Citrate (TEC) | A plasticizer used to improve the flexibility and processability of polymeric films, especially in coating formulations [15]. | Added to the granulating solution and coating suspension for Eudragit-based tablets to ensure a stable film structure [15]. |
| Cholesterol | A membrane-stabilizing agent incorporated into liposomal bilayers to increase rigidity and reduce permeability, thereby modulating drug release [16]. | Added to liposome formulations to study its effect on release kinetics under different osmotic stress conditions [16]. |
Nanocarriers have emerged as powerful tools in controlled drug delivery, offering the potential to enhance therapeutic efficacy while reducing systemic side effects. However, their extremely high surface area to volume ratio—a fundamental property at the nanoscale—presents both a significant opportunity and a substantial challenge for controlling drug release profiles. While this property enables greater interaction with biological environments and enhanced functionality, it also creates a strong tendency for rapid drug release due to the short diffusion distance and extensive surface area exposed to the surrounding medium [11] [20]. This technical guide addresses the common challenges researchers face when working with nanocarrier drug release profiles and provides practical methodologies to overcome them.
Technical FAQs: Addressing Research Challenges
Q1: Why do my nanocarriers consistently show high burst release, and how can I mitigate this?
High initial burst release occurs when drug molecules located at or near the nanoparticle surface rapidly dissolve and diffuse into the surrounding medium. This is primarily due to the large surface area and short diffusion path inherent to nanoscale systems [11] [21].
Solutions:
- Implement core-shell structures: Create a physical barrier using polymer membranes to control diffusion rates [11]
- Modify surface properties: PEGylation creates a hydrophilic layer that can slow initial drug release while improving circulation time [11] [20]
- Optimize drug-polymer interactions: Increase hydrophobic interactions or incorporate specific binding motifs to strengthen drug retention
- Adjust manufacturing parameters: Modify solvent removal rates and emulsification conditions to promote more uniform drug distribution
Q2: What are the limitations of dialysis methods for measuring nanocarrier drug release, and what alternatives exist?
Traditional dialysis methods often underestimate burst release and provide inaccurate release kinetics due to several factors [21]:
| Limitation | Impact on Release Data |
|---|---|
| Slow drug permeation through membrane | Masks true burst release kinetics |
| Potential saturation inside dialysis bag | Creates non-sink conditions, altering release rates |
| Lack of internal agitation | Allows drug/particle sedimentation and membrane fouling |
| Continuous concentration gradient disruption | Prevents accurate kinetic measurements |
Superior Alternatives:
- NanoDis System: Uses tangential flow filtration (TFF) with hollow fiber membranes to rapidly separate nanoparticles from dissolved drug, providing more accurate burst release characterization [21]
- Centrifugal ultrafiltration: Faster separation than dialysis but may risk particle damage at high speeds [21]
- In-situ UV measurement with scattering correction: Direct measurement in nanoparticle suspension without separation [21]
Q3: How does nanoparticle size specifically impact drug release kinetics?
The relationship between size and release kinetics involves multiple interacting factors:
Q4: What mathematical models are most appropriate for analyzing nanocarrier release data?
Several mathematical models can describe drug release kinetics from nanocarriers, each with specific applications and limitations [11] [20]:
| Model | Application | Release Mechanism |
|---|---|---|
| Zero-order | Ideal sustained release | Constant release rate independent of drug concentration |
| First-order | Diffusion-dominated systems | Release rate proportional to drug concentration |
| Higuchi | Matrix systems | Drug release by diffusion through the matrix |
| Korsmeyer-Peppas | Polymeric systems | Determines release mechanism (Fickian/non-Fickian) |
| Hixson-Crowell | Erosion-controlled systems | Release via surface erosion and particle dissolution |
The Korsmeyer-Peppas model (Mt/M∞ = ktⁿ) is particularly valuable for identifying the dominant release mechanism through the release exponent 'n' [11].
Experimental Protocols: Key Methodologies
Protocol 1: Controlled Release Nanocarrier Fabrication and Evaluation
Objective: Synthesize PLGA nanocarriers with modified release profiles and characterize their release kinetics using validated methods.
Materials and Reagents:
- PLGA (50:50 lactic:glycolic acid): Biodegradable polymer matrix [21]
- Dichloromethane (DCM): Organic solvent for oil-in-water emulsion
- Polyvinyl alcohol (PVA): Stabilizer and emulsifying agent
- Drug compound: Model compounds (all-trans retinoic acid, doxorubicin)
- Dialysis membrane (MWCO 12-14 kDa): Traditional release assessment [21]
- Phosphate buffered saline (PBS): Release medium simulating physiological conditions
- HPLC system with UV detection: Drug quantification
Procedure:
- Nanoparticle Preparation:
- Dissolve 100 mg PLGA and 10 mg drug in 5 mL DCM
- Emulsify in 20 mL aqueous PVA solution (1% w/v) using probe sonication
- Stir overnight to evaporate organic solvent
- Collect nanoparticles by centrifugation and wash twice with distilled water
Release Study Setup:
- Suspend 10 mg drug-loaded nanoparticles in 50 mL PBS (pH 7.4)
- Maintain at 37°C with constant agitation
- At predetermined intervals, separate nanoparticles via:
- Analyze drug concentration using validated HPLC method
Data Analysis:
- Calculate cumulative drug release (%) vs. time
- Fit data to multiple mathematical models
- Determine release mechanism from best-fit model
Protocol 2: Surface Modification to Modulate Release Profiles
Objective: Implement PEGylation strategy to reduce burst release and prolong circulation time.
Procedure:
- Surface Functionalization:
- Prepare PLGA nanoparticles as above
- Add mPEG-NHS ester (10 mol% relative to polymer) to nanoparticle suspension
- React for 4 hours at room temperature with gentle stirring
- Purify by centrifugation and characterize surface modification
- Release Comparison:
- Conduct parallel release studies with unmodified and PEGylated nanoparticles
- Compare burst release (% released at 1 hour) and overall release profile
- Evaluate the impact on release kinetics
The Scientist's Toolkit: Essential Research Reagents
| Reagent/Category | Function in Nanocarrier Research | Examples & Notes |
|---|---|---|
| Biodegradable Polymers | Form nanoparticle matrix; control degradation rate | PLGA, PLA, PCL; Adjust lactide:glycolide ratio to modify release [11] [21] |
| Surface Modifiers | Reduce burst release; improve stability; enhance targeting | PEG derivatives, polysorbates, poloxamers; PEGylation extends circulation half-life [11] [20] |
| Characterization Tools | Quantify size, surface charge, and drug release | DLS, Zeta Potential, HPLC, TFF systems; NanoDis provides accurate release data [21] |
| Stimuli-Responsive Materials | Enable triggered release at target site | pH-sensitive polymers, thermoresponsive materials, enzyme-cleavable linkers [11] |
| Model Drug Compounds | Benchmark release kinetics under development | All-trans retinoic acid, doxorubicin, fluorescent markers; RA used in neural differentiation studies [21] |
Advanced Troubleshooting: Complex Release Profile Issues
Problem: Inconsistent release profiles between batches
Diagnosis and Solutions:
- Characterize size distribution: Use DLS to ensure consistent nanoparticle size between batches
- Analyze drug loading efficiency: Variations in encapsulation efficiency significantly impact release kinetics
- Standardize purification methods: Incomplete removal of unencapsulated drug causes artificially high burst release
- Control manufacturing parameters: Precisely regulate solvent evaporation rates and mixing conditions
Problem: Achieving zero-order release kinetics from nanocarriers
Implementation Strategies:
- Core-shell architectures: Create reservoir systems with rate-controlling membranes [11]
- Multilayer nanoparticles: Incorporate successive polymer layers with different permeability
- Hybrid particle designs: Combine rapid and slow-release compartments within single systems
- Swelling-controlled systems: Utilize hydrophilic polymers that control release through hydration kinetics [11]
Visualization: Experimental Workflow for Release Study
The high surface area of nanocarriers presents a fundamental challenge in controlled drug delivery that requires multidisciplinary approaches. Through careful design strategies including surface modification, advanced characterization techniques, and appropriate mathematical modeling, researchers can transform this challenge into an opportunity for developing optimized nanocarrier systems with precisely controlled release profiles. The methodologies and troubleshooting approaches outlined in this guide provide a foundation for addressing the complex interplay between nanoscale properties and drug release behavior in pharmaceutical development.
In the field of drug delivery, nanocarriers are submicron-sized (typically 1–1000 nm) colloidal systems designed to transport therapeutic agents. Their primary function within the context of controlled release is to enhance drug bioavailability, provide sustained release kinetics, and enable spatiotemporally precise delivery to target tissues, thereby minimizing systemic side effects [22]. The major platforms—liposomes, polymeric nanoparticles, lipid nanoparticles, and inorganic systems—each offer unique mechanisms for controlling drug release, navigating biological barriers, and responding to specific physiological or external stimuli [23] [24]. This technical support center addresses the key experimental challenges and frequently asked questions researchers encounter when developing and characterizing these advanced drug delivery systems.
Frequently Asked Questions (FAQs) & Troubleshooting
Liposomes
Q1: How can I improve the stability and circulation time of my liposomal formulations?
A: Short circulation half-life is often due to rapid clearance by the Mononuclear Phagocyte System (MPS). To mitigate this:
- PEGylation: Incorporate polyethylene glycol (PEG)-conjugated lipids (e.g., DSPE-PEG) during formulation. PEG creates a steric hydration layer on the liposome surface, reducing opsonization and recognition by immune cells, leading to a longer circulation half-life [20] [24]. Troubleshooting Tip: If your drug encapsulation efficiency drops after PEGylation, consider the post-insertion technique, where PEG-lipids are inserted into pre-formed drug-loaded liposomes.
- Optimize Lipid Composition: Use high-phase-transition-temperature lipids (e.g., DSPC) and include cholesterol (up to 45 mol%) to enhance bilayer rigidity and reduce drug leakage during storage and circulation [23].
Q2: My liposomes are leaking the encapsulated hydrophilic drug too quickly. What could be the cause?
A: Premature leakage can stem from several formulation and handling issues:
- Cause 1: Inadequate Bilayer Rigidity. A fluid lipid bilayer at physiological temperature allows for faster drug diffusion. Solution: Increase the cholesterol content or switch to phospholipids with longer, saturated acyl chains (e.g., replace DOPC with DSPC) to solidify the membrane [23].
- Cause 2: Osmotic Imbalance. A significant difference in osmolarity between the internal and external aqueous phases can cause swelling or shrinkage, stressing the membrane. Solution: Ensure the hydration buffer and the external suspension medium are iso-osmotic.
- Cause 3: Aggregation/Fusion. Liposome aggregation can compromise membrane integrity. Solution: Ensure a sufficient surface charge (high zeta potential, typically |±30| mV) through charged lipids and store formulations at 4°C under an inert gas.
Polymeric Nanoparticles
Q1: What are the key factors controlling drug release kinetics from polymeric nanoparticles?
A: Release kinetics are governed by a combination of diffusion, degradation, and swelling [20].
- Diffusion-Controlled Release: Initially, drug molecules close to the nanoparticle surface diffuse out rapidly (burst release). Sustained release follows as drug from the core diffuses through the polymer matrix. The polymer's porosity and hydrophobicity are critical factors [20].
- Erosion-/Degradation-Controlled Release: For biodegradable polymers like PLGA, the release rate is coupled to the hydrolysis rate of the polymer chains. This rate can be tuned by the lactide:glycolide ratio, molecular weight, and end-group chemistry. Crystalline polymers degrade more slowly than amorphous ones [20].
- Stimuli-Responsive Release: Incorporate monomers that respond to specific triggers (e.g., pH-sensitive linkers for acidic tumor microenvironments, or light-cleavable bonds) for precise spatial and temporal control [25].
Q2: I am observing a high initial burst release from my PLGA nanoparticles. How can I achieve a more linear release profile?
A: A high burst release indicates a large fraction of the drug is adsorbed or loosely associated near the particle surface.
- Optimize Fabrication Method: If using single emulsion, switch to double emulsion (w/o/w) for hydrophilic drugs to better encapsulate them within the core. For nanoprecipitation, try increasing the polymer concentration or adding a co-solvent to slow down diffusion and produce a denser matrix.
- Adjust Polymer Properties: Use a higher molecular weight PLGA or a more hydrophobic variant (higher lactide content) to slow down water penetration and drug diffusion.
- Surface Cross-linking/Washing: A brief, gentle cross-linking step or a more rigorous washing protocol after synthesis can remove the surface-associated drug, mitigating the burst effect.
Lipid Nanoparticles (SLNs & NLCs)
Q1: When should I choose Solid Lipid Nanoparticles (SLNs) over Nanostructured Lipid Carriers (NLCs)?
A: The choice depends on the drug's physicochemical properties and the desired release profile.
- Choose SLNs when a sustained release profile over several weeks is desired. They are composed of a solid lipid matrix that provides a slower, more controlled release. They are generally simpler to formulate and have high biocompatibility [23].
- Choose NLCs when encapsulating a high loading of a poorly soluble drug. By blending solid lipids with liquid lipids (oils), NLCs create a less ordered, imperfect crystal structure that provides more space for drug accommodation and reduces the risk of drug expulsion during storage [23]. They often offer a better compromise between loading capacity and release modulation.
Q2: My Solid Lipid Nanoparticle formulation is expelling the drug during storage. What is happening?
A: Drug expulsion is a classic challenge with SLNs and is typically caused by lipid polymorphism.
- Cause: After production, the lipid matrix often exists in a meta-stable, high-energy α-polymorph. Over time, it recrystallizes into a more stable, perfect β-polymorph with a highly ordered structure. This process squeezes out the encapsulated drug molecules, leading to expulsion and potential crystal growth [23].
- Solution:
- Use NLCs: The inclusion of liquid lipids impedes the formation of a perfect crystal lattice, dramatically improving physical stability and drug retention.
- Lipid Selection: Choose lipids that are less prone to polymorphic transitions (e.g., triglycerides that form stable β' crystals).
- Add Stabilizers: Incorporate certain surfactants (e.g., Poloxamer 188) or oils that can act as crystal inhibitors.
Inorganic Nanoparticles
Q1: What are the primary advantages of using mesoporous silica nanoparticles (MSNs) for drug delivery?
A: MSNs are prized for their unique structural properties that enable precise controlled release:
- High Surface Area and Pore Volume: Allows for exceptionally high drug loading capacities [25].
- Tunable Pore Size: Pore diameter can be precisely controlled during synthesis (typically 2–10 nm), enabling size-based selection of drug molecules and modulation of diffusion rates.
- Easily Functionalizable Surface: The silanol-rich surface allows for simple grafting of "gatekeepers" or "nanovalves" (e.g., azobenzene, cyclodextrins) that can be triggered to open by stimuli like light, pH, or enzymes, providing exquisite control over release timing [25].
Q2: How can I confer biodegradability and reduce the toxicity of my inorganic nanoparticle formulation?
A: The perceived poor biodegradability of inorganic NPs is a major safety concern.
- Surface Coating/Functionalization: Biocompatible coatings like PEG, lipids, or chitosan can reduce non-specific interactions and shield the core from rapid dissolution, mitigating acute toxicity [26] [24].
- Size and Morphology Control: Smaller nanoparticles with high surface area may dissolve more readily. Designing nanoparticles with a specific size and porosity can facilitate their clearance from the body.
- Material Selection: Consider using biodegradable porous silicon or calcium phosphate nanoparticles as alternatives to silica or gold for certain applications, as they can dissolve into benign byproducts.
Essential Characterization Techniques: A Troubleshooting Guide
A systematic characterization protocol is non-negotiable for successful nanocarrier development. The table below summarizes key techniques, their purposes, and common issues encountered.
Table 1: Essential Characterization Techniques for Nanocarriers
| Parameter | Key Technique(s) | Purpose in Controlled Release | Common Issues & Troubleshooting |
|---|---|---|---|
| Particle Size & PDI | Dynamic Light Scattering (DLS) [6] | Predicts biodistribution, cellular uptake, and release kinetics. | Issue: High PDI (>0.3). Solution: Optimize synthesis (e.g., mixing speed, solvent diffusion rate) or use a fractionation step like AF4 [6]. |
| Surface Charge | Zeta Potential [6] | Indicates colloidal stability and predicts interaction with biological membranes. | Issue: Low zeta potential leads to aggregation. Solution: Modify with charged lipids or polymers. Note: Sample dilution for measurement can alter results [6]. |
| Morphology | TEM, SEM [6] | Visualizes core-shell structure, lamellarity (liposomes), and pore structure. Confirms DLS data. | Issue: Sample preparation artifacts (e.g., deformation, aggregation on grid). Solution: Use cryo-TEM for liposomes and soft polymeric NPs. |
| Drug Release | Dialysis Bag, Franz Cell | Quantifies release kinetics (e.g., zero-order, first-order) under sink conditions. | Issue: Sink condition violation. Solution: Ensure sufficient volume and agitation of release medium. Issue: Membrane adsorption. Solution: Include controls and use appropriate membrane molecular weight cutoff. |
| Stability | Size & Zeta Tracking over Time | Assesses physical stability (aggregation, drug leakage) under storage conditions. | Issue: Particle growth over time. Solution: Improve surface charge, add steric stabilizers (PEG), or change storage temperature/buffer. |
Essential Research Reagent Solutions
The following table lists key materials and their functions for developing controlled-release nanocarriers.
Table 2: Key Research Reagents for Nanocarrier Development
| Reagent Category | Specific Examples | Function in Controlled Release |
|---|---|---|
| Lipids (for Liposomes/LNPs) | DSPC, Cholesterol, DSPE-PEG [23] [24] | Forms bilayer structure (DSPC), enhances rigidity and retention (Cholesterol), provides "stealth" properties (DSPE-PEG). |
| Polymers (for Polymeric NPs) | PLGA, PLA, PEG-PLGA block copolymers [20] | Forms biodegradable nanoparticle matrix for sustained release (PLGA/PLA). PEG block creates steric stabilization for long circulation. |
| Stimuli-Responsive Materials | Azobenzene (AZO), Spiropyran (SP) [25] | Acts as a light-responsive "gatekeeper" or trigger for spatiotemporally controlled drug release via photoisomerization. |
| Surface Targeting Ligands | Folate, Transferrin, Peptides, Antibodies [20] [24] | Enables active targeting by binding to receptors overexpressed on specific cell types (e.g., cancer cells), enhancing site-specific delivery. |
| Lipids for mRNA Delivery | Ionizable Cationic Lipids, PEG-lipids [26] | Ionizable lipids encapsulate and protect nucleic acids; PEG-lipids control particle size and stability during formulation. |
Experimental Protocols for Controlled Release Studies
Standard Protocol: In Vitro Drug Release Kinetics
Objective: To quantify the rate and extent of drug release from nanocarriers under simulated physiological conditions.
Materials:
- Drug-loaded nanocarrier dispersion
- Release medium (e.g., PBS, pH 7.4, with 0.1% w/v Tween 80 to maintain sink conditions)
- Dialysis tubing (appropriate MWCO) or a membrane-based dissolution apparatus
- Thermostated water bath/shaker
- HPLC or UV-Vis spectrophotometer for drug quantification
Method:
- Preparation: Place a precise volume of nanocarrier dispersion (with known total drug content) into a dialysis bag and seal it securely.
- Incubation: Immerse the dialysis bag in a large volume (typically 50-100x the sample volume) of pre-warmed release medium (37°C) under constant, gentle agitation.
- Sampling: At predetermined time intervals, withdraw a known aliquot of the external release medium for analysis. Immediately replace with an equal volume of fresh, pre-warmed medium to maintain sink conditions.
- Analysis: Quantify the drug concentration in each sample using a validated analytical method (e.g., HPLC).
- Data Modeling: Calculate the cumulative percentage of drug released and plot it against time. Fit the data to mathematical models (e.g., Korsmeyer-Peppas, Higuchi, zero-order) to elucidate the dominant release mechanism [20].
Advanced Protocol: Light-Triggered Drug Release
Objective: To demonstrate spatiotemporally controlled drug release from photosensitive nanocarriers using light irradiation.
Materials:
- Photosensitive nanocarriers (e.g., AZO-modified liposomes or MSNs) [25]
- Light source (LED or laser) at specific wavelength (e.g., UV ~360 nm for AZO trans-to-cis)
- In vitro release setup (as in Protocol 5.1)
- Power meter
Method:
- Baseline Release: Follow Steps 1-2 from Protocol 5.1. Monitor drug release for a baseline period without light irradiation.
- Light Trigger: After the baseline period, expose the entire dialysis bag or a specific segment to the light source at a controlled power density and for a set duration.
- Post-Irradiation Monitoring: Continue sampling the release medium as before, monitoring for a spike in release rate corresponding to the light trigger.
- Control: Run a parallel experiment with identical nanocarriers kept in the dark throughout the study.
- Analysis: Compare the release profiles of the light-exposed and dark-control samples to quantify the efficiency of the light-triggered release.
Visualization of Key Concepts
Mechanisms of Controlled Drug Release from Nanocarriers
Workflow for Nanocarrier Development & Characterization
Engineering Controlled Release: Advanced Materials, Formulation Techniques, and Targeting Strategies
This technical support center is designed within the context of a broader thesis on controlled drug release in nanocarriers. It addresses common experimental challenges faced by researchers when selecting and working with biodegradable polymers and lipids. The guidance below synthesizes current literature to provide troubleshooting and detailed methodologies to enhance the reproducibility and efficacy of your nanocarrier systems.
Frequently Asked Questions (FAQs) for Researchers
Q1: How does the choice between a natural or synthetic biodegradable polymer influence the drug release profile from my nanocarrier?
The core distinction lies in the degradation mechanism, which directly controls the drug release kinetics.
- Synthetic Polymers (e.g., PLGA, PLA, PCL): These typically degrade via hydrolytic degradation, where water penetrates the matrix and cleaves ester bonds in the polymer backbone [27]. The rate is tunable by adjusting polymer composition (e.g., lactic to glycolic acid ratio in PLGA), molecular weight, and crystallinity. This allows for highly predictable, sustained release profiles over weeks to months.
- Natural Polymers (e.g., Chitosan, Alginate, Gelatin): These primarily degrade through enzymatic degradation by specific enzymes (e.g., proteases, lysozymes) [27]. This process is highly specific but can be less predictable as it depends on the local enzymatic environment at the target site, leading to potential variations in release rates.
Q2: What are the key formulation challenges for lipid nanoparticles (LNPs) in RNA delivery, and how can they be addressed computationally?
LNP optimization is plagued by a vast design space and limited a priori design principles. Key challenges include achieving efficient endosomal escape and maintaining colloidal stability [28].
- Challenge 1: Environment-Dependent Protonation of Ionizable Lipids. The protonation state of ionizable lipids, critical for endosomal escape, is environment-dependent (pH, lipid packing) and difficult to characterize experimentally [28].
- Computational Solution: Use constant pH molecular dynamics (CpHMD) simulations. A scalable CpHMD model has been shown to accurately reproduce the apparent pKa values of different LNP formulations, providing molecular-level insight into charge states under different biological conditions [28].
- Challenge 2: Understanding Self-Assembly and Structure. The complex process of LNP formation and its final nanostructure are difficult to observe.
- Computational Solution: Employ Coarse-Grained Molecular Dynamics (CG-MD) simulations. CG-MD allows for the modeling of larger systems over longer timescales to reveal detailed molecular structures and self-assembly mechanisms of LNPs, which are often difficult to characterize experimentally [28].
Q3: My microsphere formulation has inconsistent drug release profiles between batches. What are the most critical factors to control?
Inconsistent release is often a function of poor control over microsphere architecture and manufacturing.
- Critical Factor 1: Particle Size and Distribution. Drug release kinetics are highly dependent on surface area and diffusion paths. Ensure tight control over emulsification and homogenization processes during synthesis to achieve a uniform particle size distribution [29].
- Critical Factor 2: Drug-Polymer Interactions and Loading Method. The interaction between the drug and the polymer matrix (e.g., hydrophobic/hydrophilic balance) significantly impacts encapsulation efficiency and release. Optimize the drug loading strategy (encapsulation vs. adsorption) and analyze potential chemical interactions [29].
- Critical Factor 3: Polymer Crystallinity and Molecular Weight. These intrinsic polymer properties directly govern the rate of water ingress and polymer chain cleavage, thereby controlling the degradation and release rate. Use polymers with consistent specifications [27] [29].
Troubleshooting Guide: Common Experimental Issues
| Problem | Possible Cause | Suggested Solution | ||
|---|---|---|---|---|
| Rapid, burst release of drug from nanoparticles. | Poor encapsulation; drug adsorbed on the surface rather than trapped within the matrix. | Optimize synthesis (e.g., double emulsion for hydrophilic drugs); increase polymer molecular weight; add a surface wash step to remove unencapsulated drug [27]. | ||
| Incomplete drug release from polymer matrix. | Drug degradation during encapsulation; overly stable polymer matrix; hydrophobic interactions trapping the drug. | Use more gentle encapsulation methods (e.g., avoid high-shear sonication); select a polymer with a faster degradation rate (e.g., PLGA 50:50 over PLA); modify the polymer with hydrophilic segments [27] [29]. | ||
| Low encapsulation efficiency (EE) in LNPs. | Incorrect lipid-to-cargo ratio; poor mixing during formation; cargo properties (size, charge). | Systemically vary the nitrogen-to-phosphate (N/P) ratio for nucleic acids; use microfluidics for highly reproducible mixing; explore helper lipids that improve cargo complexation [28] [30]. | ||
| Poor colloidal stability of nanocarriers (aggregation). | Inadequate surface charge (zeta potential); insufficient steric stabilization; unstable lipid mixture. | Incorporate a small percentage (1-5 mol%) of PEG-lipids or PEG-polymers to provide steric stabilization [31] [30]. Optimize surface charge, as a highly positive or negative zeta potential (typically > | ±30 | mV) improves electrostatic stability [30]. |
| High cytotoxicity of lipid-based carriers. | Cationic lipid components disrupting cell membranes; non-biodegradable polymer accumulation. | Shift to ionizable lipids that are neutral at physiological pH but positively charged in acidic endosomes. Use biodegradable lipids (e.g., containing ester bonds) or polymers (e.g., PLGA) that break down into non-toxic metabolites [31] [27]. |
Detailed Experimental Protocols
Protocol 1: Computational Screening of Ionizable Lipids Using CpHMD
This methodology allows for in silico prediction of a critical performance property (pKa) before synthesis [28].
System Setup:
- Software: Use a molecular dynamics package with CpHMD capabilities (e.g., GROMACS, AMBER, NAMD).
- Model Building: Construct a model membrane patch containing the ionizable lipid, phospholipids (e.g., DOPE), cholesterol, and PEG-lipid at desired molar ratios.
- Parameterization: Employ a force field (e.g., CHARMM, Martini) with parameters for the protonated and deprotonated states of the ionizable lipid's titratable group.
Simulation Execution:
- Solvate the system in a saline buffer box.
- Run CpHMD simulations at a range of pH values (e.g., from 4.5 to 7.4) to model the different environments from bloodstream to endosome.
- Utilize a scalable CpHMD method, such as λ-dynamics, which performs at speeds comparable to standard MD [28].
Data Analysis:
- Calculate the fractional protonation of the ionizable lipid as a function of pH.
- Fit the data to the Henderson-Hasselbalch equation to determine the apparent pKa value of the lipid within the LNP membrane context.
- Validate the model by comparing computed pKa values with experimental measurements for a set of reference lipids (target MAE < 0.5 pKa units) [28].
Protocol 2: Formulating and Characterizing Drug-Loaded PLGA Microspheres
A standard method for creating a classic biodegradable polymer controlled-release system [27] [29].
Formulation (Single Emulsion - O/W Method):
- Dissolve the drug and PLGA polymer in a volatile organic solvent (e.g., dichloromethane).
- Emulsify this organic phase into a large volume of an aqueous surfactant solution (e.g., polyvinyl alcohol, PVA) using a high-speed homogenizer to form an oil-in-water (O/W) emulsion.
- Stir the emulsion continuously for several hours to evaporate the organic solvent, hardening the microspheres.
- Collect the microspheres by centrifugation, wash repeatedly with water to remove residual solvent and surfactant, and lyophilize.
Critical Characterization:
- Particle Size & Distribution: Use Dynamic Light Scattering (DLS). Aim for a low PDI (<0.2) for a narrow distribution.
- Surface Morphology: Analyze by Scanning Electron Microscopy (SEM).
- Drug Encapsulation Efficiency (EE): Dissolve a known amount of microspheres in a suitable solvent and measure drug concentration via HPLC or UV-Vis. EE% = (Actual Drug Load / Theoretical Drug Load) * 100.
- In Vitro Drug Release:
- Place a known amount of drug-loaded microspheres in a phosphate buffer saline (PBS) at 37°C under gentle agitation.
- At predetermined time points, centrifuge the samples and collect the release medium for drug quantification, replacing with fresh buffer to maintain sink conditions.
- Plot the cumulative drug release over time to establish the release profile.
The workflow for this protocol is summarized in the diagram below:
Research Reagent Solutions: Essential Materials
| Category | Item / Reagent | Function / Explanation |
|---|---|---|
| Synthetic Polymers | PLGA (Poly(lactic-co-glycolic acid)) | The most widely used biodegradable polymer; degradation rate and drug release profile can be finely tuned by adjusting the lactide:glycolide ratio [27]. |
| PCL (Polycaprolactone) | A semi-crystalline polyester with a slower degradation rate, suitable for long-term (several months) drug delivery applications [27]. | |
| Natural Polymers | Chitosan | A natural polysaccharide derived from chitin; known for its mucoadhesive properties and ability to enhance penetration across biological barriers [27]. |
| Alginate | A polysaccharide that can form gentle hydrogels in the presence of divalent cations (e.g., Ca²⁺), ideal for encapsulating sensitive biomolecules [27]. | |
| Lipid Components | Ionizable Lipids (e.g., DLin-MC3-DMA) | The functional core of modern LNPs; positively charged at low endosomal pH to facilitate membrane disruption and RNA release, but neutral in the bloodstream to reduce toxicity [28] [31]. |
| Helper Lipids (e.g., DOPE) | Phospholipids that promote non-bilayer structures and facilitate endosomal escape by supporting the transition to a hexagonal phase [30]. | |
| PEG-Lipids | Polyethylene glycol-conjugated lipids used to form the surface corona of LNPs; provide colloidal stability, reduce protein adsorption, and control particle size during formulation [31]. | |
| Cholesterol | A structural lipid that integrates into LNP bilayers to enhance stability and integrity, mimicking its role in natural cell membranes [30]. | |
| Characterization Tools | Constant pH MD (CpHMD) | A computational model to accurately simulate the environment-dependent protonation states of ionizable lipids in LNPs, enabling rational design [28]. |
| Coarse-Grained MD (CG-MD) | A simulation approach that groups atoms into beads, allowing for the study of LNP self-assembly and structure over longer timescales than all-atom MD [28]. |
Visualizing the Degradation Pathways of Biodegradable Polymers
The primary mechanisms by which biodegradable polymers break down to release their drug cargo are illustrated below.
Troubleshooting Guides
Microfluidics Troubleshooting Guide
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Channel Clogging | Particle aggregation, precipitation at interface, too high polymer concentration [32] | Reduce PLGA concentration in organic phase; increase total flow rate (TFR) to enhance shear; use co-solvents to prevent rapid precipitation [32] |
| High Polydispersity Index (PDI) | Inefficient mixing, non-uniform flow profiles, fluctuating flow rates [32] | Use micromixer with chaotic advection (e.g., herringbone); increase TFR to turbulent regime; optimize Flow Rate Ratio (FRR); use 3-inlet design for focused mixing [32] |
| Irreproducible Particle Size Between Batches | Manual pressure control, flow rate instability, chip surface fouling [32] | Use syringe pumps with high precision; implement pulse-dampeners; standardize chip cleaning protocol (e.g., NaOH rinse); use CFD modeling to validate consistent mixing [32] |
| Low Drug Loading Efficiency | Rapid mixing causing drug expulsion, poor drug-polymer compatibility, drug too hydrophilic [20] | Optimize FRR to moderate nucleation kinetics; modify polymer chemistry (e.g., use PLGA with compatible end-groups); use lipophilic drug analogs if possible [20] |
Nanoprecipitation Troubleshooting Guide
| Problem | Possible Causes | Recommended Solutions | ||
|---|---|---|---|---|
| Broad Size Distribution (Batch Method) | Slow or non-uniform mixing, dropwise addition too fast, magnetic stirrer creating vortices [32] | Switch to rapid addition (1-3 sec) with vigorous stirring; use high-speed homogenizer; transition to Flash Nanprecipitation (FNP) with Confined Impinging Jets [33] [32] | ||
| Poor Colloidal Stability (Aggregation) | Inadequate stabilizer concentration, insufficient surface coverage, low zeta potential [20] | Increase PVA concentration (e.g., 2.0-2.5% w/v); ensure stabilizer is present before nucleation; consider alternative stabilizers (e.g., Poloxamer); measure zeta potential (> | 20 | mV) [32] |
| Small Particle Size Not Achieved | Low polymer concentration, high organic-to-aqueous ratio, insufficient supersaturation [32] | Increase polymer concentration in organic phase; reduce aqueous-to-organic volume ratio; ensure rapid solvent diffusion (e.g., use acetone/ACN) [32] | ||
| Organic Solvent Residuals | Inefficient solvent removal, large batch volumes [20] | Extend evaporation time under fume hood; employ reduced pressure evaporation; use dialysis for small volumes; lyophilize final product [32] |
Solvent Injection Troublesaging Guide
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Rapid Particle Aggregation Post-Injection | Too high interfacial tension, stabilizer missing or ineffective, solvent properties incompatible [20] | Inject into aqueous phase containing stabilizer (e.g., PVA); optimize solvent choice (partially water-miscible e.g., ethyl acetate); employ ultrasonic bath during injection [33] |
| Low Yield or Encapsulation Efficiency | Drug leakage to aqueous phase, injection rate too slow, drug-polymer miscibility low [20] | Increase injection rate using syringe pump; match drug lipophilicity with polymer; consider double-emulsion method for hydrophilic drugs [20] |
| Gelation or Bulk Precipitation | Localized high polymer concentration at needle tip, poor dispersion [20] | Use smaller gauge needle (e.g., 25G); increase agitation speed in receiving phase; dilute polymer concentration in organic phase [20] |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between batch and microfluidic nanoprecipitation, and when should I choose one over the other?
A1: The core difference lies in the precision and scalability of mixing. Batch nanoprecipitation involves adding an organic polymer solution to a larger volume of aqueous antisolvent under stirring (e.g., magnetic stirring). It is simple and requires minimal equipment but offers limited control over mixing, often resulting in broader particle size distributions (PDI > 0.1) [32]. Microfluidic nanoprecipitation forces fluids through microscale channels, enabling millisecond mixing times via laminar or chaotic flow. This provides superior control over nucleation and growth, yielding smaller, more monodisperse particles (PDI < 0.1) with high batch-to-batch reproducibility [32]. Choose batch for early-stage, low-throughput feasibility studies. Choose microfluidics when you need high reproducibility, monodisperse particles for in vivo studies, or a path toward scalable, continuous manufacturing.
Q2: How does the "Flow Rate Ratio (FRR)" in microfluidics critically influence nanoparticle characteristics?
A2: The FRR, typically defined as the ratio of the aqueous phase flow rate to the organic phase flow rate (Qaq:Qorg), is a critical process parameter. It directly governs the local supersaturation level at the point of mixing. A higher FRR (e.g., 5:1 to 10:1) creates a more rapid and complete solvent shift, promoting a high nucleation rate and a large number of nuclei. This generally leads to smaller nanoparticle sizes. Conversely, a lower FRR results in a slower solvent displacement, favoring nucleus growth over the formation of new nuclei, which produces larger particles. Furthermore, an optimal FRR ensures complete miscibility and prevents defects, helping to achieve a low PDI [32].
Q3: Our PLGA nanoparticles are unstable and aggregate after one week of storage at 4°C. What are the key formulation factors to check?
A3: Colloidal instability often stems from insufficient steric or electrostatic stabilization. Focus on these factors:
- Stabilizer Type and Concentration: Ensure an adequate concentration of a polymeric stabilizer like Polyvinyl Alcohol (PVA ~2% w/v) is present. The stabilizer must adsorb to the nanoparticle surface during the critical nucleation phase to prevent aggregation [32].
- Zeta Potential: Measure the zeta potential. A value greater than |±20| mV typically indicates good electrostatic stabilization. A low value suggests a need for ionic surfactants or a change in pH [20].
- Lyophilization Protocol: For long-term storage, lyophilization (freeze-drying) is recommended. Always include a cryoprotectant (e.g., trehalose or sucrose at 5-10% w/v) in the formulation before freezing to prevent nanoparticle fusion and ensure easy redispersion [32].
Q4: For pH-responsive drug release in the tumor microenvironment, how can I incorporate this functionality into nanoparticles made by nanoprecipitation?
A4: You can engineer pH-sensitivity through your choice of polymer or by using clever chemical linkages. The acidic tumour microenvironment (pH ~6.5-6.8) can be exploited using polymers with ionizable groups (e.g., tertiary amines) that undergo protonation, leading to nanoparticle swelling or dissolution [4]. Alternatively, you can synthesize a polymer-drug conjugate connected via an acid-labile bond (e.g., hydrazone or acetal). This bond remains stable at blood pH (7.4) but cleaves rapidly in the acidic tumor interstitium or within endosomes/lysosomes (pH 4.5-5.0), triggering drug release [4]. These functional polymers can be directly formulated into nanoparticles using standard nanoprecipitation techniques.
Experimental Protocols
Protocol: Microfluidic Preparation of PLGA Nanoparticles
This protocol details the formulation of monodisperse PLGA nanoparticles using a three-inlet microfluidic mixer, optimized based on recent integrated experimental and Computational Fluid Dynamics (CFD) studies [32].
1. Materials
- Polymer: PLGA (Resomer RG 502 H, 7000–17,000 Da)
- Organic Solvent: Acetonitrile (ACN, 99.95%)
- Stabilizer: Polyvinyl Alcohol (PVA, Mw 9000–10,000, 80% hydrolyzed)
- Aqueous Phase: Deionized Water
- Equipment: Commercial microfluidic platform (e.g., Tamara from Inside Therapeutics) or syringe pumps; Microfluidic chip with herringbone mixer and three-inlet junction; Syringes (1 mL, 10 mL) and tubing; Dynamic Light Scattering (DLS) instrument; Lyophilizer.
2. Method
- Step 1: Solution Preparation.
- Organic Phase: Dissolve 10 mg of PLGA in 1 mL of acetonitrile.
- Aqueous Phase: Dissolve PVA in deionized water to prepare a 2.0% (w/v) solution. Filter both solutions through a 0.45 μm membrane.
- Step 2: Microfluidic System Setup.
- Load the organic phase into a 1 mL syringe.
- Load the aqueous phase into a 10 mL syringe.
- Connect the organic phase syringe to the central inlet of the three-inlet microfluidic chip.
- Connect the aqueous phase syringe to the two flanking inlets via a "Y" connector to ensure equal flow.
- Set the system to the following optimized parameters [32]:
- Total Flow Rate (TFR): 12 mL/min
- Flow Rate Ratio (FRR, Aq:Org): 3:1
- Step 3: Nanoparticle Formation and Collection.
- Start the syringe pumps simultaneously.
- Collect the turbid effluent in a glass vial.
- Step 4: Post-Processing.
- Allow the collected suspension to stand uncovered for 2-4 hours or under a gentle stream of nitrogen to evaporate the organic solvent.
- Centrifuge the nanoparticles at 15,000 rpm for 20 minutes. Discard the supernatant and resuspend the pellet in a minimal volume of deionized water.
- Add a cryoprotectant (e.g., 5% w/v trehalose) and lyophilize for long-term storage.
3. Expected Outcomes Using this protocol, you should obtain PLGA nanoparticles with a mean diameter of approximately 150-200 nm and a polydispersity index (PDI) below 0.1 [32].
Protocol: Batch Nanoprecipitation of PLGA Nanoparticles using DoE
This protocol uses a structured Design of Experiments (DoE) approach to efficiently optimize the batch nanoprecipitation process, accounting for variable interactions [32].
1. Materials (Same as Protocol 3.1)
2. Method
- Step 1: Define DoE Parameters.
- Response Variables: Target Nanoparticle Size = 200 nm, Target PDI = 0.1.
- Input Variables and Ranges:
- PLGA mass: 5 - 15 mg
- ACN volume: 100 - 500 μL
- PVA concentration: 1.5 - 2.5% (w/v)
- Aqueous phase volume: 1 - 3 mL
- Step 2: Execute Experimental Runs.
- Use a DoE software tool (e.g., Stavex) to generate an experimental design, typically 8-12 runs.
- For each run:
- Prepare the aqueous phase by adding the specified volume of PVA solution to a 5 mL glass vial with a magnetic stir bar.
- Begin stirring at a fixed, vigorous speed (e.g., 660 rpm).
- Prepare the organic phase by dissolving the specified mass of PLGA in the specified volume of ACN.
- Add the entire organic phase to the stirring aqueous phase dropwise every 3 seconds.
- Step 3: Characterization and Analysis.
- Characterize the nanoparticle size and PDI for each run using DLS.
- Input the results into the DoE software to build a regression model and identify the optimal parameter combination (e.g., 10 mg PLGA, 200 μL ACN, 2 mL of 2% PVA) that meets your target CQAs [32].
Experimental Workflow and System Diagrams
Microfluidic Nanoprecipitation Workflow
Nanoprecipitation Mixing Regimes
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Role in Formulation | Technical Notes |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer matrix forming the nanoparticle core; encapsulates active ingredient. | The lactic:glycolide ratio (e.g., 50:50) and molecular weight control degradation rate and drug release kinetics. Resomer RG 502 H is a common choice [32]. |
| Polyvinyl Alcohol (PVA) | Steric stabilizer; prevents nanoparticle aggregation by adsorbing to the surface during formation. | Critical for colloidal stability. Use partially hydrolyzed grades (e.g., 80%) for optimal performance. Concentration (1.5-2.5% w/v) is a key DoE variable [32]. |
| Acetonitrile (ACN) | Water-miscible organic solvent for dissolving PLGA and hydrophobic drugs. | Rapid diffusion into the aqueous phase during nanoprecipitation creates the supersaturation needed for nucleation. Preferred for its miscibility and low boiling point [32]. |
| Trehalose | Cryoprotectant; protects nanoparticle structure during lyophilization (freeze-drying). | Prevents fusion and aggregation of nanoparticles during the freezing and water-removal process, ensuring the powder can be easily reconstituted [32]. |
| Microfluidic Chip (Herringbone Mixer) | Provides chaotic advection to achieve rapid, homogeneous mixing of solvent and anti-solvent. | The herringbone grooves induce Dean vortices, thinning diffusion layers and ensuring uniform supersaturation, which is key to low PDI [32]. |
Stimuli-responsive drug delivery systems represent a significant advancement in nanocarrier research, enabling precise spatiotemporal control over drug release [34]. These "smart" systems are engineered to remain stable in circulation but release their therapeutic payload in response to specific pathological cues or external triggers [11] [35]. This targeted approach enhances drug efficacy at disease sites while minimizing systemic side effects, representing a paradigm shift toward personalized and sustainable medical interventions [34]. This technical resource provides comprehensive guidance on the four primary endogenous stimulus mechanisms—pH, enzymes, redox potential, and temperature—for researchers developing controlled release platforms.
Stimulus Mechanisms and Characterization
The following table summarizes the key triggering mechanisms, their operational principles, and relevant characterization techniques.
| Stimulus Type | Trigger Mechanism & Conditions | Common Biomaterials Used | Key Characterization Methods |
|---|---|---|---|
| pH-Responsive | Acidic pH in tumor microenvironment (pH ~6.5-6.8) or endocytic compartments (pH ~5.0-5.5) [35] [36] | Chitosan [34]; Poly(acrylic acid) derivatives; Acetylated dextran [36] | Drug release profiling in buffers at different pHs; Zeta potential measurement; FTIR for chemical bond analysis |
| Enzyme-Responsive | Overexpressed enzymes (e.g., Matrix Metalloproteinases/MMPs, esterases) in disease sites cleaving specific substrates [35] [36] | Peptide-polymer conjugates [35]; Gelatin; Hyaluronic acid [34] | HPLC/MS to detect cleaved linker molecules; Gel electrophoresis for polymer degradation; Fluorescence assays with quenched substrates |
| Redox-Responsive | High intracellular glutathione (GSH) concentration (2-10 mM) vs. extracellular milieu (~2-20 μM) [35] [36] | Disulfide-crosslinked polymers [11]; Lipids with disulfide bonds (e.g., DSPE) | Ellman's assay for thiol quantification; DLS for particle size change upon reduction; TEM imaging of structural disassembly |
| Temperature-Responsive | Mild hyperthermia in tumor environment (~40-42°C) or locally applied heat [35] | Poly(N-isopropylacrylamide)/pNIPAM [35]; Pluronics (Poloxamers) [11] | Dynamic Light Scattering (DLS) for size vs. temperature; Differential Scanning Calorimetry (DSC) for LCST determination |
Experimental Protocols for Trigger Evaluation
Protocol 1: Evaluating pH-Dependent Drug Release Kinetics
This protocol assesses the release profile of a drug from nanocarriers under simulated physiological (pH 7.4) and pathological (acidic) conditions.
- Buffer Preparation: Prepare release media: 0.01 M Phosphate Buffered Saline (PBS) at pH 7.4 and 0.01 M Acetate Buffered Saline at pH 5.0. Filter sterilize (0.22 μm).
- Dialysis Setup: Place a precise volume of drug-loaded nanocarrier dispersion (e.g., equivalent to 1 mg of drug) into a pre-swollen dialysis membrane tube (e.g., MWCO 12-14 kDa).
- Release Study: Immerse each dialysis bag in 200 mL of the respective release medium maintained at 37°C with constant agitation (100 rpm). Ensure sink conditions.
- Sampling and Analysis: At predetermined time intervals, withdraw 1 mL of the external release medium and replace with an equal volume of fresh pre-warmed buffer. Analyze the drug concentration in sampled aliquots using HPLC or UV-Vis spectrophotometry. Plot cumulative drug release (%) versus time to generate release profiles.
Protocol 2: Verifying Enzyme-Responsive Behavior
This method confirms carrier degradation or drug release triggered by a specific enzyme.
- Enzyme Solution: Prepare an activity-confirmed stock solution of the target enzyme (e.g., MMP-2, MMP-9) in an appropriate incubation buffer.
- Incubation Setup: Aliquot a fixed concentration of your enzyme-responsive nanocarrier into three vials:
- Test Group: Add nanocarriers + enzyme solution.
- Enzyme Control: Add enzyme solution + blank buffer (no nanocarriers).
- Nanocarrier Control: Add nanocarriers + incubation buffer (no enzyme).
- Reaction and Analysis: Incubate all vials at 37°C. Monitor the reaction over time. Termination and analysis method depends on the system:
- For drug release: Follow the sampling method from Protocol 1, but with smaller volumes.
- For carrier degradation: Analyze particle size and polydispersity index (PDI) via Dynamic Light Scattering (DLS) at the start and end of incubation. Use Transmission Electron Microscopy (TEM) for visual confirmation of morphological changes.
Troubleshooting FAQs
Q1: My pH-sensitive nanoparticles are releasing the drug too quickly (burst release) at physiological pH (7.4). What could be the cause? A1: Burst release often indicates inadequate carrier stability or non-optimized polymer-drug interactions. Potential solutions include: (1) Increasing the crosslinking density of your polymer matrix to reduce premature diffusion. (2) Incorporating a hydrophobic segment or co-polymer to strengthen the core structure and enhance stability at neutral pH. (3) Re-evaluating your drug loading method; overloading can lead to surface-adsorbed drug, which is prone to rapid release.
Q2: I observe no significant difference in drug release between my redox-responsive system in the presence and absence of the triggering agent (e.g., GSH). What should I check?
A2: This lack of response suggests an issue with the disulfide chemistry or accessibility. Focus on: (1) Verifying the disulfide bond incorporation: Use techniques like 1H-NMR or Raman spectroscopy to confirm the successful integration of disulfide links in your polymer/lipid. (2) Checking bond accessibility: Ensure the disulfide bonds are positioned within the carrier structure where they are accessible to the reducing agent, not buried in a hydrophobic core. (3) Confirming GSH activity: Prepare a fresh GSH solution and verify its reducing activity, as it can oxidize and lose potency over time.
Q3: My enzyme-responsive system shows non-specific release in the control group (without enzyme). How can I improve its specificity? A3: Non-specific release points to hydrolytic instability or non-specific cleavage. To address this: (1) Optimize the linker: Ensure the peptide or chemical linker used is highly specific to the target enzyme and resistant to serum esterases and other common hydrolases. (2) Introduce a shielding layer: Apply a protective coating, such as a thin layer of polyethylene glycol (PEG), to minimize non-specific interactions and hydrolysis in the biological environment. The PEG layer can be designed to be shed upon reaching the target site.
Q4: The phase transition of my thermoresponsive polymer (e.g., pNIPAM) does not occur at the expected Lower Critical Solution Temperature (LCST). Why? A4: The LCST is highly dependent on polymer composition and the external environment. Consider: (1) Polymer composition: The LCST can be tuned by copolymerizing with more hydrophilic monomers (to raise LCST) or more hydrophobic monomers (to lower LCST). Analyze your polymer's actual composition. (2) Environmental factors: The LCST can shift in the presence of salts, solvents, or drugs. Characterize the LCST in the final formulation medium, not just in pure water.
Research Reagent Solutions
The table below lists essential materials and their functions for developing stimuli-responsive nanocarriers.
| Reagent/Material | Function in Stimuli-Responsive Systems | |
|---|---|---|
| Chitosan | A natural polysaccharide used in pH-responsive systems; its amine groups protonate in acidic environments, leading to carrier swelling or dissolution [34]. | |
| Disulfide-Crosslinkers (e.g., Cystamine, DTBP) | Agents containing S-S bonds used to crosslink polymer chains or conjugate drugs; these bonds are cleaved in the high glutathione environment of the cell cytoplasm, triggering release [11]. | |
| Poly(N-isopropylacrylamide) - pNIPAM | A synthetic polymer exhibiting a sharp thermal phase transition (LCST) at ~32°C; used to create thermoresponsive nanocarriers that collapse or aggregate upon mild heating [35]. | |
| Matrix Metalloproteinase (MMP) Substrate Peptides | Short peptide sequences (e.g., GPLG | V) that are specifically cleaved by overexpressed MMPs in the tumor microenvironment; used as linkers in enzyme-responsive systems [35] [36]. |
| DSPE-PEG | A phospholipid-polyethylene glycol conjugate used to stabilize nanocarriers, prolong circulation time, and provide a surface for further functionalization with targeting ligands [11]. |
Experimental Workflow and Mechanism Diagrams
Active targeting methodologies, primarily through the conjugation of specific ligands to nanocarriers, have revolutionized the field of targeted drug delivery. This approach aims to enhance the specificity of therapeutic agents for particular cells, such as cancer cells or immune cells, thereby improving efficacy and reducing off-target effects. The core principle involves attaching biological molecules (e.g., antibodies, peptides, aptamers) to the surface of nanocarriers to facilitate recognition and binding to unique receptors expressed on target cell membranes [37] [38]. Despite the conceptual elegance, the practical implementation of ligand conjugation is fraught with technical challenges that can compromise the performance and clinical translation of these sophisticated delivery systems. This guide addresses the most frequent issues encountered in the lab, providing targeted troubleshooting advice for researchers and drug development professionals.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary factors to consider when selecting a ligand for my nanocarrier system? The choice of ligand is critical and depends on three main factors: the identity and density of the target receptor on the cell of interest, the physicochemical properties of the ligand itself (size, charge, stability), and the conjugation chemistry available. Monoclonal antibodies offer high specificity and affinity but are large and can be immunogenic. Smaller ligands like peptides and aptamers may offer better tumor penetration and lower immunogenicity, though their affinity might be lower. The key is to match the ligand to the application, for instance, using T-cell-specific antibodies for in vivo CAR-T therapy [39] [40].
FAQ 2: Why is controlling ligand density and orientation so crucial, and how can it be achieved? Inconsistent ligand density and random orientation are major causes of batch-to-batch variability and failed experiments. Too few ligands reduce targeting efficiency, while too many can cause particle aggregation, increase immunogenicity, and accelerate clearance from the bloodstream [39]. Random orientation can block the ligand's binding site.
- Solution: Employ site-specific conjugation strategies instead of random chemistries. Techniques such as engineered cysteines, thiol-maleimide linkages, or click chemistry provide superior control over both the density and the orientation of ligands, ensuring the binding domain is available for receptor interaction [39].
FAQ 3: How does the conjugation process itself impact the stability of my nanocarrier? The conjugation process, particularly the chemicals and conditions used, can disrupt the nanocarrier's integrity. This can lead to premature payload leakage, changes in surface charge (zeta potential), and aggregation [39]. For lipid-based systems like LNPs, conjugation can destabilize the lipid bilayer.
- Solution: Consider a post-insertion technique where ligand-PEG-lipid conjugates are incorporated into pre-formed, stable nanocarriers. This method often better preserves encapsulation efficiency and particle integrity compared to adding ligands during the initial formulation step [39].
FAQ 4: What are the best practices for purifying conjugated nanocarriers and analyzing conjugation success? After conjugation, it is essential to remove unbound (free) ligands and aggregates to ensure product quality and accurate experimental results.
- Purification: Techniques like size-exclusion chromatography (SEC) or tangential flow filtration (TFF) are effective for separating free ligand from conjugated nanocarriers [39].
- Analysis: A combination of physicochemical and biological assays is required. Use ELISA or surface plasmon resonance (SPR) to quantify ligand density and confirm binding functionality. Techniques like analytical ultracentrifugation can also be used to quantify free versus bound species [39].
Troubleshooting Guides
Low Targeting Efficiency
This problem manifests as poor cellular uptake in the target cell line despite confirmed receptor expression.
Problem: Nanocarriers show low targeting efficiency and poor cellular uptake. Potential Causes and Solutions:
| Potential Cause | Recommended Solution | Key Experimental Considerations |
|---|---|---|
| Insufficient Ligand Density | Optimize conjugation chemistry to increase ligand density on the particle surface. Use site-specific conjugation. | Use ELISA or SPR to quantify ligand density pre- and post-optimization. Correlate with uptake studies. |
| Improper Ligand Orientation | Switch to site-specific conjugation chemistries that ensure the ligand's binding domain is exposed. | Compare functional binding affinity (via SPR) of randomly-oriented vs. site-specifically conjugated particles. |
| Low Receptor Affinity | Screen ligands with higher binding affinity (lower Kd) or consider multivalent ligand display. | Perform affinity measurements (SPR) for candidate ligands. Test nanocarriers in a panel of cells with varying receptor density. |
| Protein Corona Effect | Modify surface with stealth coatings (e.g., PEG) to minimize non-specific protein adsorption that can shield ligands. | Perform incubation in serum-containing media and re-measure hydrodynamic size and zeta potential to infer corona formation. |
Particle Aggregation and Instability
This issue involves the formation of particle clusters, leading to inconsistent behavior and potential safety concerns.
Problem: Conjugated nanocarriers aggregate or show physical instability. Potential Causes and Solutions:
| Potential Cause | Recommended Solution | Key Experimental Considerations |
|---|---|---|
| Excessive Ligand Density | Titrate the ligand-to-particle ratio to find an optimum that maintains stability while ensuring efficacy. | Use dynamic light scattering (DLS) to monitor particle size and PDI across different ligand loading ratios. |
| Harsh Conjugation Conditions | Shift to milder conjugation chemistries (e.g., click chemistry) or adopt a post-insertion method. | Compare particle size, PDI, and payload leakage before and after conjugation under different conditions. |
| Inadequate Purification | Implement robust purification post-conjugation (e.g., SEC, TFF) to remove aggregates and unreacted species. | Use multi-angle light scattering (MALS) coupled with SEC for high-resolution size distribution analysis. |
| Poor Cryoprotection | Add cryoprotectants (e.g., trehalose, sucrose) prior to freeze-thaw cycles or lyophilization. | Perform stability studies by measuring particle size and encapsulation efficiency after multiple freeze-thaw cycles. |
Inconsistent In Vivo Performance
Here, promising in vitro results fail to translate to animal models.
Problem: Despite good in vitro data, the nanocarrier shows poor target accumulation in vivo. Potential Causes and Solutions:
| Potential Cause | Recommended Solution | Key Experimental Considerations |
|---|---|---|
| Rapid Clearance by RES | Improve stealth properties with PEGylation or use biomimetic coatings (e.g., cell membranes). | Track biodistribution; reduced liver/spleen accumulation indicates successful RES evasion. |
| Off-Target Liver/Spleen Accumulation | This is common. Further optimize ligand density and PEG length to balance targeting and stealth. | Conduct biodistribution studies with radiolabeled or fluorescently labeled nanocarriers. |
| Instability in Bloodstream | Ensure linker stability in blood and integrity of the nanocarrier under physiological conditions. | Perform serum stability assays: incubate particles in serum and monitor size, leakage, and ligand detachment over time. |
| Heterogeneous Target Expression | Confirm target antigen expression and accessibility in the in vivo disease model, not just in cell lines. | Use immunohistochemistry on tissue sections from the animal model to validate target expression. |
Experimental Protocols
Standard Protocol: Post-Insertion Conjugation for Lipid Nanoparticles (LNPs)
This method is widely used to conjugate targeting ligands to pre-formed LNPs while maintaining payload encapsulation and particle integrity [39].
Objective: To attach a targeting ligand (e.g., an antibody fragment) to the surface of a pre-formed LNP via a PEG-lipid anchor.
Materials:
- Pre-formed, payload-loaded LNPs.
- Ligand (e.g., scFv, peptide) functionalized with a reactive group (e.g., maleimide).
- PEG-lipid derivative (e.g., DSPE-PEG-Maleimide).
- Purification equipment: Size-exclusion chromatography (SEC) system or Tangential Flow Filtration (TFF) system.
- Buffer: Purification buffer (e.g., PBS, HEPES), degassed.
Methodology:
- PEG-Lipid Activation: Incubate the PEG-lipid (e.g., DSPE-PEG-Maleimide) with the thiol-functionalized ligand at a predetermined molar ratio. Perform this in degassed buffer for 1-2 hours at room temperature to form the ligand-PEG-lipid conjugate.
- Purification: Purify the ligand-PEG-lipid conjugate from unreacted ligand using a desalting column or dialysis.
- Insertion: Incubate the purified ligand-PEG-lipid conjugate with the pre-formed LNPs. A typical incubation is 1-2 hours at room temperature or 37°C with gentle stirring. The ligand-PEG-lipid will spontaneously insert its hydrophobic tail into the lipid bilayer of the LNP.
- Final Purification: Purify the conjugated LNPs (now CLNPs) using SEC or TFF to remove any uninserted ligand-PEG-lipid conjugates and free ligands.
- Characterization: Analyze the final product for particle size (DLS), polydispersity index (PDI), zeta potential, ligand density (ELISA/SPR), and encapsulation efficiency.
Diagram 1: Post-insertion conjugation workflow.
Advanced Protocol: Site-Specific Conjugation for Controlled Ligand Density
This protocol provides a methodology for achieving uniform ligand orientation and density, which is critical for reproducible performance [39] [41].
Objective: To conjugate ligands to a nanocarrier at a specific site, controlling both density and orientation.
Materials:
- Nanocarrier with engineered conjugation handle (e.g., expressed protein ligand with unique cysteine).
- Ligand with complementary reactive group (e.g., maleimide for thiol chemistry, DBCO for azide click chemistry).
- Click chemistry reagents (if applicable).
- Purification and analysis equipment as in Protocol 4.1.
Methodology:
- Handle Introduction: Engineer a unique reactive amino acid (e.g., a cysteine residue) into the nanocarrier's surface protein or directly into the ligand itself. This provides a specific site for conjugation.
- Ligand Functionalization: If necessary, functionalize the targeting ligand with the complementary reactive group (e.g., maleimide for thiol-based conjugation).
- Controlled Conjugation: React the functionalized ligand with the engineered nanocarrier at a precise molar ratio. For click chemistry (e.g., SPAAC), simply mix the components.
- Quenching and Purification: Quench the reaction (e.g., with excess cysteine for maleimide chemistry) and purify the conjugated product via SEC or TFF.
- Quality Control: Rigorously characterize the product. Key metrics include ligand density (mass spectrometry, ELISA), confirmation of site-specificity (e.g., peptide mapping), and functional binding assays (SPR).
Diagram 2: Site-specific conjugation process.
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagents for Ligand Conjugation Experiments
| Reagent / Material | Function in Conjugation | Key Considerations for Selection |
|---|---|---|
| PEG-Lipids (e.g., DSPE-PEG) | Acts as a spacer and anchor for inserting ligands into lipid nanocarriers; improves solubility and reduces aggregation. | PEG chain length impacts circulation time and ligand accessibility. Functional end-group (e.g., Maleimide, NHS) must match ligand chemistry [39]. |
| Crosslinker Chemistry (e.g., SMCC, Click Chemistry Reagents) | Forms a covalent bond between the nanocarrier and the ligand. SMCC is a common heterobifunctional crosslinker. | Choose between cleavable vs. non-cleavable linkers based on the intended drug release mechanism. Click chemistry (e.g., SPAAC) offers high specificity and efficiency [41]. |
| Targeting Ligands (e.g., scFv, Affibodies, Peptides) | Provides specificity by binding to receptors on the target cell surface. | Balance affinity, size, immunogenicity, and cost. scFv antibodies offer high specificity; peptides are smaller and easier to produce [39] [40]. |
| Size-Exclusion Chromatography (SEC) Columns | Purifies conjugated nanocarriers by separating them from unreacted ligands and small molecule reagents based on hydrodynamic size. | Select a resin with an appropriate separation range for your nanocarrier size. Fast and effective for lab-scale purification [39]. |
| Analytical Tools (e.g., SPR, ELISA Kits) | Characterizes conjugation success by quantifying ligand density and confirming binding affinity and functionality. | SPR provides real-time kinetic data (Ka, Kd); ELISA is a more accessible method for quantitative analysis of ligand attachment [39]. |
Troubleshooting Guide: Common EPR Effect Experimental Challenges
FAQ 1: Why is my nanocarrier accumulation in tumors lower than expected in preclinical models?
Issue: Low tumor accumulation of nanocarriers despite optimization of size and surface properties.
Potential Causes and Solutions:
- Cause: High Interstitial Fluid Pressure (IFP): Solid tumors often exhibit elevated IFP, which can hinder the convection of nanocarriers from vessels into and throughout the tumor interstitium [42] [43].
- Cause: Heterogeneous Vascular Permeability: The EPR effect is not uniform across all tumors or even within different regions of the same tumor. Vascular pore sizes and density can vary significantly [46] [43].
- Cause: Suboptimal Nanocarrier Physicochemical Properties: The size, shape, and surface charge may not be ideal for your specific tumor model.
- Solution: Adhere to the general design principles for EPR-based carriers: a size range of 40-200 nm, a spherical shape, and a neutral or slightly negative surface charge to promote longer circulation and reduce clearance by the reticuloendothelial system (RES) [46] [6]. Surface modification with PEG (PEGylation) is a common strategy to achieve this [20].
FAQ 2: How can I improve the penetration and distribution of nanocarriers within the tumor mass?
Issue: Nanocarriers accumulate around tumor vessels but fail to penetrate deeply into the tissue, limiting their efficacy.
Potential Causes and Solutions:
- Cause: Dense Extracellular Matrix (ECM): A dense network of collagen and other ECM proteins in the tumor stroma can create a significant physical barrier to nanoparticle diffusion [46] [47].
- Cause: Growth-Induced Solid Stress: The rapid proliferation of tumor cells generates mechanical solid stress, which compresses blood and lymphatic vessels, further reducing perfusion and penetration [42].
- Solution: Explore combination therapies with agents that alleviate this solid stress. Some chemotherapeutics that reduce cancer cell density can indirectly improve nanocarrier distribution [42].
FAQ 3: My nanocarrier shows rapid clearance from the bloodstream. How can I extend its circulation time?
Issue: Short plasma half-life of nanocarriers, reducing their opportunity to extravasate into the tumor via the EPR effect.
Potential Causes and Solutions:
- Cause: Opsonization and RES Uptake: Nanocarriers are recognized by the immune system and cleared by the liver and spleen [46] [6].
- Solution:
- PEGylation: Surface coating with polyethylene glycol (PEG) creates a hydrophilic "stealth" layer that reduces protein adsorption and RES uptake [20].
- Size Optimization: Ensure nanoparticles are larger than the renal clearance cutoff (~10 nm) but small enough to avoid rapid RES filtration (typically under 200 nm) [46] [20].
- Surface Charge: Avoid highly positive or negative charges, as they can promote opsonization. Aim for a neutral or slightly negative zeta potential [6].
- Solution:
Quantitative Data for EPR-Based Drug Delivery
The following table summarizes key quantitative parameters and their impact on the EPR effect, crucial for experimental design and troubleshooting.
Table 1: Key Physicochemical Parameters for Optimizing EPR-Based Delivery
| Parameter | Optimal Range | Functional Impact | Characterization Technique |
|---|---|---|---|
| Hydrodynamic Size | 40 - 200 nm [46] | Avoids renal clearance (<10 nm) and excessive RES uptake (>200 nm); ideal for extravasation through leaky vasculature. | Dynamic Light Scattering (DLS) [6] |
| Polydispersity Index (PDI) | < 0.3 [6] | Indicates a uniform particle population, ensuring consistent in vivo behavior. | Dynamic Light Scattering (DLS) [6] |
| Surface Charge (Zeta Potential) | Near Neutral / Slightly Negative [46] [6] | Reduces non-specific interactions with serum proteins and cell membranes, prolonging circulation. | Electrophoretic Light Scattering [6] |
| PEG Density | 5 - 20% (molar ratio) [20] | Creates an effective stealth layer; too low is ineffective, too high can hinder cellular uptake. | Nuclear Magnetic Resonance (NMR), Colorimetric assays [20] |
| Tumor Vasculature Pore Size | 100 - 780 nm [47] [45] | Determines the maximum allowable size of nanocarriers for extravasation; highly variable between tumor models. | Intravital microscopy, Transmission Electron Microscopy [44] |
| Reported Tumor Accumulation (% Injected Dose/g) | 0.7% ID/g (median) [46] | Realistic benchmark from meta-analysis; typically less than 1% of the injected dose reaches the tumor in animal models. | Imaging (e.g., Fluorescence, PET), Radioactive tracing [46] [44] |
Experimental Protocols for Key EPR Characterization
Protocol 1: Characterizing Nanocarrier Physicochemical Properties
Objective: To determine the size, size distribution (PDI), and surface charge (Zeta Potential) of synthesized nanocarriers.
Materials:
- Nanocarrier suspension
- Deionized water or phosphate-buffered saline (PBS)
- Dynamic Light Scattering (DLS) / Zeta Potential Analyzer
Methodology:
- Sample Preparation: Dilute the nanocarrier suspension appropriately using a filtered solvent (water or PBS) to avoid signal saturation from multiple scattering. A general starting point is a dilution to 0.1-1 mg/mL [6].
- Dynamic Light Scattering (DLS):
- Transfer the diluted sample into a disposable sizing cuvette.
- Place the cuvette in the instrument and set the measurement temperature (e.g., 25°C or 37°C).
- Run the measurement. The software will calculate the hydrodynamic diameter (Z-average) and the Polydispersity Index (PDI) based on the intensity of scattered light [6].
- Zeta Potential Measurement:
- Transfer the diluted sample into a dedicated zeta potential cell (folded capillary cell).
- Insert the cell into the instrument.
- Apply an electric field, and the instrument uses Laser Doppler Velocimetry to measure the electrophoretic mobility of the particles, which is then converted to zeta potential [6].
- Data Interpretation: Report the Z-average diameter ± standard deviation, the PDI value, and the zeta potential ± standard deviation from at least three independent measurements.
Protocol 2: Evaluating the EPR Effect via Fluorescence Imaging
Objective: To visually confirm and semi-quantify the tumor accumulation of nanocarriers in a small animal model.
Materials:
- Fluorescently labeled nanocarrier (e.g., with Cy5.5, DiR)
- Animal model with a subcutaneous tumor (e.g., murine xenograft)
- In vivo fluorescence imaging system (IVIS)
- Anesthesia system (e.g., isoflurane)
Methodology:
- Administration: Inject the fluorescently labeled nanocarrier intravenously into the tail vein of the tumor-bearing mouse at a standardized dose (e.g., 5 mg/kg).
- Image Acquisition:
- At predetermined time points post-injection (e.g., 1, 4, 24, 48 hours), anesthetize the mouse.
- Place the mouse in the imaging chamber and acquire fluorescence images using appropriate excitation/emission filters for your fluorophore.
- Maintain consistent imaging parameters (exposure time, binning, f/stop) across all animals and time points [44].
- Data Analysis:
Research Reagent Solutions for EPR Experiments
Table 2: Essential Materials and Reagents for EPR Effect Research
| Reagent / Material | Function in EPR Research | Example & Notes |
|---|---|---|
| PEG-lipids | Stealth coating agent | 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[methoxy(PEG)-2000] (DSPE-PEG2k). Used to create long-circulating liposomes and polymeric micelles [20]. |
| Fluorescent Dyes | In vivo tracking and imaging | DiR, Cy5.5, ICG. Near-infrared dyes are preferred for deep-tissue imaging with low background autofluorescence [44] [48]. |
| PLGA | Biodegradable polymer for nanocarrier matrix | Poly(lactic-co-glycolic acid). Forms the core of nanoparticles for controlled drug release; degradation rate can be tuned by the LA:GA ratio [6] [20]. |
| Clinical Benchmark Formulations | Positive control for EPR studies | Doxil/ Caelyx (PEGylated liposomal doxorubicin) or Abraxane (albumin-bound paclitaxel). Used as reference standards to validate experimental models and methods [46] [49]. |
| Vascular Permeability Modulators | Tool compounds to enhance EPR | Angiotensin II (vasoconstrictor, can enhance tumor blood flow), Nitric Oxide (NO) donors (vasodilators, can increase vascular permeability) [45]. |
| ECM Degrading Enzymes | Tool to overcome penetration barriers | Collagenase, Hyaluronidase. Used in research to study the effect of ECM degradation on nanocarrier penetration and distribution [44] [45]. |
Diagram: The CAPIR Cascade and EPR Enhancement Strategies
The following diagram illustrates the journey of a nanocarrier from injection to its final therapeutic action, known as the CAPIR cascade, and highlights key strategies to enhance each step, particularly for controlled drug release.
Enhancing the EPR Journey for Controlled Release
The CAPIR cascade (Circulation, Accumulation, Penetration, Internalization, Release) outlines the critical steps for successful drug delivery [46]. Each step can be enhanced to improve outcomes:
- Circulation: PEGylation is the primary strategy to achieve long circulation, essential for the EPR effect [20].
- Accumulation: The core EPR effect can be augmented using vascular modulators (e.g., nitric oxide inducers) or physical methods like radiotherapy to increase vessel permeability [44] [45].
- Penetration: ECM disruption (e.g., with collagenase) or using smaller particles can enhance diffusion deep into the tumor [44] [45].
- Internalization: Active targeting with ligands (e.g., antibodies, peptides) can improve cellular uptake, complementing passive EPR accumulation [46] [44].
- Drug Release: This is crucial for the thesis context of controlled release. Stimuli-responsive systems can be designed to release their payload upon encountering specific tumor microenvironment triggers like low pH, specific enzymes, or a redox gradient, or external triggers like ultrasound or light [20] [48]. This ensures the drug is released primarily at the target site, maximizing efficacy and minimizing side effects.
Frequently Asked Questions (FAQs) for Nanocarrier Research
Q1: What are the primary reasons for low drug loading efficiency in polymeric nanoparticles, and how can this be improved?
A1: Low drug loading efficiency often stems from a mismatch between the drug's physicochemical properties and the polymer's characteristics, or from inefficient encapsulation methods.
- Root Causes:
- Drug-Polymer Incompatibility: Hydrophobic drugs in hydrophilic polymers (or vice versa) lead to poor incorporation and rapid leakage [50].
- Inefficient Method: Standard methods like single-emulsion may not adequately trap the drug within the polymer matrix.
- Troubleshooting Guide:
- Optimize Polymer Selection: Use hydrophobic polymers like PLGA for hydrophobic drugs. For hydrophilic drugs, consider polymers that can form ionic complexes or use double-emulsion methods [50] [38].
- Employ Advanced Formulation Techniques: Nano-precipitation or microfluidics can provide better control over particle formation, leading to higher encapsulation efficiency [51].
- Use of Prodrugs: Chemically modify the drug to enhance its affinity for the polymer matrix [50].
Q2: How can I overcome the rapid clearance of nanocarriers by the mononuclear phagocyte system (MPS) to achieve longer circulation half-life?
A2: Rapid MPS clearance is a major barrier, preventing nanocarriers from reaching their target site.
- Root Causes: Opsonins (serum proteins) adsorb onto the nanocarrier surface, marking them for phagocytosis by macrophages in the liver and spleen [52].
- Troubleshooting Guide:
- Surface PEGylation: Grafting polyethylene glycol (PEG) onto the nanocarrier surface creates a hydrophilic "stealth" layer that reduces protein adsorption and MPS recognition [50] [38].
- Biomimetic Coating: A more advanced strategy involves coating nanocarriers with cell membranes (e.g., from red blood cells) to create a "self" surface that evades immune detection [53] [51].
- Optimize Physicochemical Properties: Smaller nanoparticles (size < 100 nm) with a neutral surface charge are less prone to opsonization and MPS clearance [50] [38].
Q3: My actively targeted nanocarriers are not showing improved cellular uptake. What could be going wrong?
A3: Failure of active targeting can occur at several stages, from design to biological barriers.
- Root Causes:
- Ligand Instability or Loss: The targeting ligand (e.g., antibody, peptide) may detach during storage or circulation [38].
- Protein Corona Effect: Serum proteins adsorb onto the nanocarrier surface, masking the targeting ligands and preventing their interaction with the target receptor [50].
- Incorrect Target Selection: The target receptor may not be sufficiently overexpressed on the intended cells, or its expression may vary between patient populations [38].
- Troubleshooting Guide:
- Characterize the Protein Corona: Analyze the nanocarrier's surface after incubation with serum to confirm ligand accessibility.
- Validate Ligand Binding: Perform in vitro binding assays using target cells to ensure the ligand-receptor interaction is functional before moving to complex models.
- Ensure Proper Orientation: Use conjugation chemistries that ensure the ligand is presented in its correct, bioactive orientation [38].
Q4: How can I achieve controlled, sustained drug release at the target site instead of premature burst release?
A4: Premature release is a common issue that reduces efficacy and increases off-target toxicity.
- Root Causes: Weak drug-carrier interactions, diffusion of surface-adsorbed drug, or degradation of the carrier material in circulation [3].
- Troubleshooting Guide:
- Utilize Stimuli-Responsive Materials: Design nanocarriers that release their payload only in response to specific disease-site stimuli, such as:
- Low pH: Use pH-sensitive polymers or linkers that degrade in the acidic tumor microenvironment or within endolysosomes [53] [38].
- Enzymes: Incorporate enzyme-cleavable peptide sequences (e.g., degraded by matrix metalloproteinases in tumors) [53].
- Reactive Oxygen Species (ROS): Use ROS-sensitive materials that degrade in areas of inflammation [53] [54].
- Optimize Carrier Matrix: A denser or more hydrophobic polymer matrix can slow down drug diffusion and provide a more sustained release profile [50] [38].
- Utilize Stimuli-Responsive Materials: Design nanocarriers that release their payload only in response to specific disease-site stimuli, such as:
Q5: What strategies can improve the penetration of nanocarriers across the Blood-Brain Barrier (BBB) for neurodegenerative diseases?
A5: The BBB is a highly selective barrier that severely limits drug delivery to the brain.
- Root Causes: Tight junctions between endothelial cells prevent paracellular transport, and active efflux pumps export foreign substances [53].
- Troubleshooting Guide:
- Surface Functionalization: Graft BBB-transcytosing ligands onto the nanocarrier surface. Examples include:
- Utilize Natural Transport Mechanisms: Employ strategies like adsorptive-mediated transcytosis (AMT) or receptor-mediated transcytosis (RMT) to hijack existing BBB transport pathways [53].
- Consider Alternative Routes: Intranasal administration can bypass the BBB by delivering drugs directly to the brain via the olfactory and trigeminal nerves [55].
Performance Data of Nanocarrier Systems
Table 1: Efficacy of Multi-Drug Cancer Nanotherapy in Preclinical Tumor Growth Inhibition
| Therapy Regimen | Average Tumor Growth (% of Control) | Relative Improvement vs. Single Free Drug |
|---|---|---|
| Single Free Drug | 66.9% | Baseline |
| Free Drug Combination | 53.4% | 20.2% better |
| Single-Drug Nanotherapy | 54.3% | 18.8% better |
| Multi-Drug Nanotherapy | 24.3% | 63.7% better |
Source: Analysis of 273 pre-clinical studies [56].
Table 2: Common Nanocarrier Types and Their Key Characteristics
| Nanocarrier Type | Core Composition | Key Advantages | Common Disease Applications |
|---|---|---|---|
| Liposomes | Phospholipid bilayer [50] | High biocompatibility; co-delivery of hydrophilic/hydrophobic drugs [38] | Cancer (Doxil), Neurodegenerative [50] [53] |
| Polymeric NPs | PLGA, Chitosan, PEG [50] [53] | Controlled release, high stability, tunable degradation [38] | Cancer, Diabetes (oral insulin), MASLD [53] [54] [52] |
| Inorganic NPs | Gold, Iron Oxide, Silica [53] [57] | Unique optical/magnetic properties, large surface area, potential for theranostics [53] [57] | Cancer (imaging + therapy), Neurodegenerative [53] [57] |
| Solid Lipid NPs | Solid lipid matrix [50] | Good biocompatibility, improved drug stability vs. liposomes [50] | Cancer, Neurodegenerative [50] [53] |
Detailed Experimental Protocols
Protocol 1: Formulating FcRn-Targeted PLGA-PEG Nanoparticles for Oral Insulin Delivery
This protocol is based on a strategy to overcome gastrointestinal barriers for biologic delivery [55].
- Nanoparticle Synthesis:
- Dissolve the PLGA-PEG copolymer and insulin in a suitable organic solvent (e.g., dichloromethane).
- Emulsify this solution in an aqueous phase containing a stabilizer (e.g., polyvinyl alcohol) using a probe sonicator or high-pressure homogenizer to form an oil-in-water emulsion.
- Stir the emulsion overnight to evaporate the organic solvent and harden the nanoparticles.
- Collect the nanoparticles by ultracentrifugation and wash to remove residual stabilizer.
- Surface Functionalization:
- Reconstitute the purified nanoparticles in a buffer at a neutral pH.
- Incubate the nanoparticles with the Fc fragment of IgG under gentle stirring. The Fc fragment will conjugate to the terminal PEG groups on the nanoparticle surface, enabling targeting of the neonatal Fc receptor (FcRn) in the intestine.
- Purify the functionalized nanoparticles via centrifugation or filtration.
- In Vivo Evaluation:
- Use a diabetic mouse model (e.g., streptozotocin-induced).
- Administer the FcRn-targeted insulin nanoparticles to fasted mice via oral gavage.
- Monitor blood glucose levels at regular intervals over 12-24 hours. The targeted nanoparticles should show a significant and prolonged hypoglycemic effect compared to non-targeted controls or free insulin.
Protocol 2: Evaluating BBB Penetration of CRT-Modified PLGA Nanoparticles
This protocol details methods to assess nanocarrier delivery to the brain for neurodegenerative disease therapy [53].
- Nanoparticle Preparation and Targeting:
- Prepare PLGA nanoparticles encapsulating a model drug (e.g., curcumin) and a near-infrared dye for imaging using a nano-precipitation or emulsion method.
- Conjugate the brain-targeting CRT peptide to the nanoparticle surface via covalent coupling to surface carboxyl or amine groups.
- In Vitro BBB Model:
- Culture brain microvascular endothelial cells on a porous Transwell insert to create a confluent monolayer, representing the BBB.
- Measure the Transendothelial Electrical Resistance (TEER) to confirm barrier integrity.
- Apply CRT-modified and non-modified (control) nanoparticles to the apical chamber (blood side).
- Collect samples from the basolateral chamber (brain side) over time and quantify nanoparticle concentration (via fluorescence) to calculate the apparent permeability coefficient (Papp).
- In Vivo Validation:
- Administer the fluorescently labeled nanoparticles to mice intravenously.
- After a predetermined circulation time (e.g., 4-24 hours), perfuse the animals transcardially with saline to remove blood from the vasculature.
- Harvest the brains and other major organs.
- Quantify biodistribution using an ex vivo imaging system (IVIS). The CRT-targeted nanoparticles should show higher fluorescence signal in the brain compared to controls.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanocarrier Drug Delivery Research
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| PLGA-PEG Copolymer | Forms biodegradable, stealth nanoparticles; enables sustained release and functionalization [38] [55]. | Used for oral insulin delivery by targeting the FcRn receptor [55]. |
| DSPE-PEG | A phospholipid-PEG conjugate used for PEGylating liposomes and other nanocarriers to prolong circulation [50] [38]. | Key component in Doxil, the first FDA-approved stealth liposome [50]. |
| CRT Peptide | A brain-targeting ligand that facilitates nanoparticle transport across the Blood-Brain Barrier (BBB) via receptor-mediated transcytosis [53]. | Conjugated to PLGA nanoparticles to improve brain delivery of curcumin and Aβ inhibitors in Alzheimer's models [53]. |
| Hyaluronic Acid (HyA) | A naturally occurring glycosaminoglycan used as a targeting ligand for CD44 receptors, often overexpressed on cancer cells and activated macrophages [53]. | Used to coat iron oxide nanoparticles for targeted imaging and therapy in Alzheimer's disease models [53]. |
| pH-Sensitive Lipids | Lipids that undergo structural change in acidic environments (e.g., tumor microenvironment, endosomes), triggering drug release [38]. | Lithocholic acid derivatives used to create liposomes that release anticancer agents in response to low pH [38]. |
Signaling Pathways and Experimental Workflows
Diagram 1: Nanocarrier Journey from Injection to Intracellular Targeting
Diagram 2: Insulin Resistance Pathway and Nano-Intervention in MASLD
Overcoming Hurdles: Addressing Biological Barriers, Toxicity, and Manufacturing Challenges
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My nanocarriers are failing to penetrate the mucus layer and reach the epithelial surface. What could be causing this?
- A: This is typically due to strong adhesive interactions between your nanocarriers and the mucus mesh. The mucus layer acts as a size and biochemical filter, trapping particles that have hydrophobic or charged surfaces [58] [59]. To improve penetration:
- Modify Surface Chemistry: Create a neutral, hydrophilic surface, for example by coating with low molecular weight, dense polyethylene glycol (PEG) to shield adhesive interactions [59].
- Consider Mucus Physiology: Remember that mucus pore size is heterogeneous, ranging from tens of nanometers to over a micron, and varies with health status [58]. Ensure your carrier size is appropriate for your target tissue.
- Utilize Mucus-Penetrating Properties: Design carriers to mimic viruses that have adapted to avoid mucin adhesion, often through balanced hydrophilic and charged residues on their surfaces [58].
Q2: I am observing high variability in nanocarrier transcytosis across epithelial cell models. Which uptake pathway should I target?
- A: Variability often stems from the nanocarrier's unintended engagement of multiple endocytic pathways with different intracellular fates [60] [61]. The optimal pathway depends on your therapeutic goal:
- For Lysosomal Delivery: If your drug (e.g., certain nucleic acids) requires lysosomal activation, target the clathrin-mediated pathway. This pathway reliably delivers its cargo to lysosomes for enzymatic processing [60] [61].
- For Cytosolic or Transcellular Delivery: To avoid lysosomal degradation, aim for the caveolae-mediated or macropinocytosis pathways. These routes can direct nanocarriers to the endoplasmic reticulum or Golgi apparatus, facilitating escape from the degradative pathway and enabling transcytosis across the epithelial layer [61].
Q3: How can I enhance the targeting of nanocarriers to specific endothelial cells, such as those at inflammatory sites?
- A: Precision targeting requires leveraging specific receptor-ligand interactions. A common strategy is to functionalize the nanocarrier surface with ligands that bind to markers upregulated on your target endothelial cells [24].
- Exploit Natural Homing Mechanisms: Inflammation often involves the recruitment of stem cells like EPCs and MSCs. These cells are mobilized and home to damage sites via factors like VEGF and G-CSF [62]. Designing carriers that mimic or interact with these homing signals (e.g., by incorporating specific peptides or antibodies) can enhance targeted delivery to inflamed endothelium [62] [63].
Experimental Protocol: Evaluating Nanoparticle-Mucus Interactions
Objective: To determine the diffusion coefficient and mobility of engineered nanocarriers within native intestinal mucus.
Materials:
- Purified native mucus (e.g., from murine colon) or reconstituted mucin gels (e.g., from MUC2) [64] [59].
- Fluorescently-labeled nanocarriers with varying surface properties (e.g., PEGylated, cationic, anionic).
- Glass-bottom culture dishes or chambered coverslips.
- Confocal microscope or similar imaging system equipped for FRAP (Fluorescence Recovery After Photobleaching).
- Image analysis software (e.g., ImageJ with FRAP plugin).
Methodology:
- Mucus Preparation: Place a 20-50 µL droplet of native or reconstituted mucus into the glass-bottom dish to create a layer approximately 0.5-1 mm thick [59].
- Nanoparticle Incubation: Mix a small volume of your nanocarrier suspension (e.g., 5 µL) with the mucus sample. Allow it to incubate for 15-30 minutes at 37°C to reach equilibrium.
- FRAP Measurement:
- Use the confocal microscope to select a region of interest (ROI) within the mucus sample.
- Photobleach the fluorescence in the ROI with a high-intensity laser pulse.
- Monitor the recovery of fluorescence in the ROI over time as unbleached nanoparticles diffuse back into the area.
- Capture images at regular intervals (e.g., every 5-10 seconds) for 5-15 minutes.
- Data Analysis:
- Normalize the fluorescence intensity in the ROI to the pre-bleach and fully recovered intensities.
- Fit the recovery curve to an appropriate diffusion model to calculate the effective diffusion coefficient (Deff).
- Compare the Deff of your test nanoparticles to that of control particles (e.g., inert PEG-coated beads of similar size) to determine the extent of mucoadhesion. A lower Deff indicates stronger adhesive interactions and poorer mobility [59].
Data Presentation: Nanocarrier Design Parameters
Table 1: Impact of Nanocarrier Physicochemical Properties on Biological Barrier Navigation
| Physicochemical Property | Impact on Mucus Barrier | Impact on Epithelial/Endothelial Barrier | Key Considerations for Drug Release |
|---|---|---|---|
| Size | Optimal size is ~200-500 nm for efficient mucus penetration while avoiding rapid clearance [60] [61]. | Smaller nanoparticles (<100 nm) generally show higher cellular uptake and transcytosis rates [60]. | Smaller particles have larger surface area-to-volume ratio, which can influence drug release kinetics. |
| Surface Charge | Cationic surfaces strongly adhere to negatively charged mucins, trapping carriers. Neutral or slightly anionic surfaces with low binding affinity show best penetration [58] [59]. | Surface charge influences the endocytic pathway; cationic particles often promote endocytosis but may also cause cytotoxicity [61]. | Charge can be used to design responsive release systems (e.g., pH-sensitive coatings that charge-shift in endosomes). |
| Surface Hydrophobicity | Hydrophobic interactions with mucins and other components lead to particle immobilization [59]. | Hydrophobicity can promote non-specific cellular uptake but also increases protein opsonization, which may hinder targeting [60]. | Hydrophobic cores are ideal for encapsulating poorly soluble drugs, with release dependent on polymer degradation. |
| Ligand Functionalization | Can be used to target specific transporters or temporarily reduce mucus viscosity (e.g., with proteolytic enzymes) [61]. | Enables receptor-mediated active targeting to specific cell types (e.g., transferrin receptors on endothelial cells) [24]. | Ligand binding can trigger internalization, directing the carrier to specific intracellular compartments for controlled release. |
Table 2: Key Cellular Internalization Pathways for Nanocarriers
| Internalization Pathway | Carrier Size | Key Machinery | Intracellular Fate | Suitability for Drug Delivery |
|---|---|---|---|---|
| Clathrin-Mediated Endocytosis | ~100-200 nm [61] | Clathrin, dynamin [60] | Traffics to endosomes and lysosomes for degradation [60] [61]. | Ideal for drugs that require lysosomal activation or release. |
| Caveolae-Mediated Endocytosis | ~60-80 nm [60] | Caveolin-1, dynamin [60] | Traffics to caveosomes, avoids lysosomes; can access Golgi and ER [61]. | Excellent for protecting biologic drugs from degradation and promoting transcytosis. |
| Macropinocytosis | Up to 5 µm [60] | Actin, growth factor receptors [61] | Traffics to macropinosomes, which can fuse with lysosomes or recycle contents [61]. | Suitable for larger carriers and delivery of macromolecular complexes. |
Signaling Pathways and Experimental Workflows
MUC2 Synthesis and Secretion Pathway
Nanocarrier Intracellular Trafficking and Fate
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Nanocarrier-Barrier Interaction Studies
| Research Reagent | Function in Experiment | Example Application |
|---|---|---|
| MUC2 Antibodies | Detect and quantify the primary structural mucin in intestinal mucus [64]. | Immunofluorescence staining to assess mucus layer integrity and thickness in vitro or ex vivo. |
| Reconstituted Mucin Gels | Provide a standardized, homogenous model of the mucus barrier for high-throughput screening [59]. | Initial screening of nanocarrier diffusion using FRAP or transwell systems before moving to native mucus. |
| Caco-2/HT-29 Co-cultures | In vitro model of the intestinal epithelium incorporating both absorptive enterocytes and mucus-producing goblet cells [65] [59]. | Studying nanoparticle transcytosis and permeability under physiologically relevant mucus-producing conditions. |
| Fluorescent Dyes (e.g., FITC, Cy5) | Label nanocarriers for visualization and quantification using microscopy or flow cytometry [61]. | Tracking cellular uptake, intracellular trafficking, and transcytosis efficiency of nanocarriers. |
| Chlorpromazine, Genistein, EIPA | Pharmacological inhibitors for specific endocytic pathways (clathrin-mediated, caveolae-mediated, and macropinocytosis, respectively) [61]. | Mechanistic studies to determine the primary internalization pathway of a nanocarrier. |
| PEGylated Lipids/Polymers | Create a hydrophilic, "stealth" corona around nanocarriers to minimize mucoadhesion and protein opsonization [24] [59]. | Formulating mucus-penetrating particles (MPPs) and improving systemic circulation half-life. |
A primary challenge in nanomedicine is engineering the biological identity of nanoparticles to avoid rapid clearance by the body's immune system. Upon injection into the bloodstream, nanoparticles are immediately coated by layers of endogenous proteins, forming a "protein corona" that determines their fate, including evasion of the mononuclear phagocytic system (the body's first line of defense), targeting capability, and cellular uptake [66]. The strategic application of surface coatings, particularly polyethylene glycol (PEG) and emerging alternatives, provides a "stealth" effect that mitigates immune recognition. This technical resource explores the mechanisms, troubleshooting, and experimental protocols central to developing effective stealth nanocarriers for controlled drug release applications.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Core Principles and Mechanisms
What is the fundamental "stealth effect" and how does it work? The stealth effect describes the ability of surface-modified nanoparticles to evade recognition and clearance by the immune system, thereby prolonging their circulation time in the bloodstream. This is achieved primarily by coating nanoparticles with hydrophilic polymers like PEG, which form a hydrated layer that reduces nonspecific adsorption of opsonin proteins. Opsonins tag nanoparticles for phagocytosis by immune cells; preventing their adsorption allows nanoparticles to remain in circulation longer, enhancing their chance of reaching the target site, such as a tumor, via mechanisms like the Enhanced Permeability and Retention (EPR) effect [11] [67].
How does PEGylation confer stealth properties? PEGylation—the covalent attachment of PEG chains to a nanoparticle's surface—imparts stealth through several physicochemical mechanisms:
- Steric Hindrance: The flexible, mobile PEG chains create a dynamic physical barrier that prevents opsonizing proteins from closely approaching and adhering to the nanoparticle surface [68].
- Hydration Layer: The ethylene glycol repeating units bind water molecules via hydrogen bonding, forming a hydrophilic shell that masks the underlying hydrophobic nanoparticle core from immune surveillance [68].
- Reduced Electrostatic Interactions: PEG's non-ionic nature helps shield any charged groups on the nanoparticle surface, minimizing electrostatic interactions with proteins and immune cells [11].
Common Experimental Challenges and Solutions
Why is my PEGylated nanocarrier still being cleared rapidly? The Accelerated Blood Clearance (ABC) phenomenon is a common issue, often linked to the development of anti-PEG antibodies. Upon repeated administration, these antibodies bind to PEGylated nanocarriers, leading to opsonization and rapid uptake by macrophages in the liver and spleen [66] [68]. Key factors influencing ABC are summarized in the table below.
Table: Factors Influencing Accelerated Blood Clearance (ABC) Phenomenon
| Factor | Effect on ABC Phenomenon | Experimental Considerations |
|---|---|---|
| Pre-existing Anti-PEG Antibodies | Found in 20-70% of untreated individuals; cause immediate rapid clearance of the first dose [69] [70]. | Screen animal models or human serum for anti-PEG antibodies before study initiation. |
| Dosing Interval | The ABC effect is most pronounced with repeated doses administered 5-7 days apart [69]. | Optimize dosing schedules; consider longer intervals or alternate polymers for multi-dose regimens. |
| PEG Molecular Weight & Architecture | Lower molecular weight PEG (<20 kDa) and linear structures are more immunogenic [70]. | Use higher MW PEG (>20 kDa) or branched architectures to reduce immunogenicity. |
| Nanoparticle Composition | The core material (lipid, polymer, inorganic) can influence the intensity of the immune response [68]. | The immunogenicity is linked to the conjugated material, not just PEG itself. |
How do I balance stealth properties with active targeting efficiency? A significant challenge is that a dense PEG brush layer can sterically hinder the binding of targeting ligands (e.g., antibodies, peptides) to their receptors on target cells [66]. To achieve an optimal balance:
- Fine-tune the PEG:ligand ratio on the nanoparticle surface.
- Optimize PEG chain length and molecular weight; shorter chains may provide sufficient stealth while reducing interference with ligand binding.
- Engineer ligand orientation and size; use spacer arms to project ligands beyond the PEG corona.
- Consider charge-based interactions or engineering an artificial protein corona to drive organ-specific targeting [66].
Immunogenicity and Safety
Does PEG itself cause an immune response? PEG is a hapten, meaning it is too small to elicit an immune response on its own but can do so when conjugated to a larger carrier (e.g., a protein or nanoparticle) [68]. The immunogenicity reported in the literature is primarily for PEG conjugates, not free PEG. Anti-PEG antibodies, primarily IgM and IgG, are generated following exposure to these conjugates and can lead to reduced drug efficacy and potential hypersensitivity reactions [66] [68] [70].
What are the clinical implications of anti-PEG immunity? The presence of anti-PEG antibodies can have several critical consequences:
- Reduced Efficacy: Accelerated clearance diminishes the therapeutic agent's circulation time and exposure to the disease site, as seen with PEG-asparaginase in leukemia treatment [70].
- Hypersensitivity Reactions: In rare cases, anti-PEG IgE antibodies can trigger anaphylaxis, as observed with some PEGylated lipid nanoparticle COVID-19 vaccines [66] [70].
- Complement Activation-Related Pseudoallergy (CARPA): Antibody-PEG complexes can activate the complement system, leading to the release of anaphylatoxins (C3a, C5a) and causing acute infusion reactions [70].
Advanced Strategies and Alternative Technologies
PEG Alternatives for Next-Generation Stealth
Growing concerns about PEG immunogenicity have spurred the development of alternative stealth polymers. The table below compares key candidates.
Table: Emerging Polymer Alternatives to PEG for Stealth Coating
| Polymer Alternative | Mechanism of Stealth | Reported Advantages over PEG | Development Status |
|---|---|---|---|
| Zwitterionic Polymers (e.g., PCB) | Form a tight hydration layer via electrostatically induced hydration; highly resistant to protein adsorption [71]. | Higher transfection efficiency; mitigates ABC phenomenon; effective endosomal escape [71]. | Preclinical studies show promise for mRNA delivery and gene editing. |
| Poly(2-oxazoline) | Mimics PEG's hydrophilicity and stealth capabilities through a different chemical backbone [70]. | Lower immunogenicity; potential for reduced antibody cross-reactivity [70]. | Phase I trials ongoing; considered a leading "PEG-mimetic." |
| Polysarcosine | A biodegradable polypeptoid with high hydrophilicity and stealth properties [70]. | Non-immunogenic and biodegradable, ideal for repeated dosing [70]. | Preclinical development. |
| Biomimetic Cell Membranes | Coats nanoparticles with natural cell membranes (e.g., erythrocytes, leukocytes) [72]. | Inherits complex biological functions for immune evasion and dynamic targeting [72]. | Extensive preclinical research for cancer, stroke, and inflammatory diseases. |
Experimental Protocols for Assessing Immunogenicity
Protocol 1: Detecting Anti-PEG Antibodies via ELISA Purpose: To quantify anti-PEG IgM and IgG levels in serum samples from animal models or human subjects. Reagents:
- Coating Antigen: PEG-conjugated Bovine Serum Albumin (PEG-BSA) or a similar PEG-carrier protein.
- Blocking Buffer: 1-5% BSA or casein in PBS.
- Test Samples: Serial dilutions of serum or plasma.
- Detection Antibodies: Horseradish peroxidase (HRP)-conjugated anti-species IgM or IgG antibodies.
- Substrate: TMB (3,3',5,5'-Tetramethylbenzidine) or other HRP-compatible chromogenic substrate. Procedure:
- Coat Wells: Immobilize PEG-BSA (e.g., 1-10 µg/mL) on a 96-well ELISA plate overnight at 4°C.
- Block: Add blocking buffer for 1-2 hours at room temperature to prevent nonspecific binding.
- Incubate with Sample: Add serially diluted serum samples and incubate for 1-2 hours.
- Incubate with Detection Antibody: Add HRP-conjugated secondary antibody for 1 hour.
- Develop and Read: Add TMB substrate, stop the reaction with acid, and measure absorbance at 450 nm. Interpretation: Compare sample absorbance to a standard curve or pre-defined cut-off value to determine antibody titer [70].
Protocol 2: Evaluating the ABC Phenomenon in Rodent Models Purpose: To assess the impact of pre-existing or induced anti-PEG antibodies on the pharmacokinetics of a PEGylated nanocarrier. Procedure:
- Sensitization Dose: Administer the PEGylated nanocarrier (the "sensitizing dose") intravenously to the test group of rodents.
- Waiting Period: Allow a 5- to 7-day interval for the immune system to generate anti-PEG IgM antibodies.
- Challenge Dose: Administer a second, identical dose of the PEGylated nanocarrier intravenously.
- Pharmacokinetic Sampling: Collect blood samples at multiple time points post-injection and measure the concentration of the nanocarrier or its payload in plasma.
- Analysis: Compare the clearance half-life and area under the curve (AUC) of the challenge dose in the sensitized group versus a naive control group that received only the challenge dose. Accelerated clearance in the sensitized group confirms the ABC phenomenon [68] [69].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Stealth Nanoparticle Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| mPEG-Lipids (e.g., DMG-PEG2000) | Provides a stealth coating on lipid nanoparticles (LNPs); prevents aggregation and opsonization. | Standard component in mRNA LNP vaccines and therapies [68] [71]. |
| PEG-PLGA Copolymers | Forms the core matrix and stealth shell of biodegradable polymeric nanoparticles. | Used for sustained drug release and studying nanoparticle immunogenicity [69]. |
| Anti-PEG Antibody ELISA Kits | Quantifies anti-PEG IgM and IgG levels in biological samples. | Essential for screening pre-existing immunity in subjects and assessing immune response in preclinical studies [70]. |
| Zwitterionic Lipids (e.g., PCB-Lipids) | Serves as a non-PEG alternative for stabilizing LNPs and conferring stealth. | Formulating LNPs with high transfection efficiency and low immunogenicity for repeated dosing [71]. |
| Complement Assay Kits (e.g., C3a, SC5b-9) | Measures complement activation products in plasma. | Evaluating the potential for CARPA and other complement-mediated infusion reactions [70]. |
Visualizing Key Concepts and Workflows
Mechanisms of Anti-PEG Immune Response and ABC Phenomenon
This diagram illustrates the cellular and molecular mechanisms behind the anti-PEG immune response, which leads to the Accelerated Blood Clearance (ABC) phenomenon.
Strategic Workflow for Mitigating PEG Immunogenicity
This workflow provides a logical decision tree for researchers to navigate and address the challenge of PEG immunogenicity in their nanocarrier designs.
Biocompatibility and Toxicity Profiles of Nanocarrier Components
Frequently Asked Questions (FAQs)
Q1: What are the primary factors that determine the biocompatibility and toxicity of a nanocarrier?
The biocompatibility and toxicity of a nanocarrier are predominantly determined by its physicochemical properties, including [73] [74]:
- Size and Shape: Smaller nanoparticles generally have higher reactivity and potential toxicity. Size also affects biodistribution, cellular uptake, and clearance routes (e.g., particles <10 nm may undergo renal clearance) [11] [6].
- Surface Charge: Cationic (positively charged) surfaces often exhibit higher cytotoxicity as they can disrupt cell membranes. The surface charge, indicated by zeta potential, also influences particle aggregation and interactions with plasma proteins [6] [74].
- Surface Chemistry and Coating: Functionalization with hydrophilic polymers like Polyethylene Glycol (PEG) creates a "stealth" effect, reducing opsonization and recognition by the immune system, thereby increasing circulation time and biocompatibility [73] [11] [20]. The formation of a "protein corona" upon in vivo administration can also alter the nanocarrier's biological identity and toxicity [74].
- Composition and Degradation Products: The intrinsic toxicity of the core material (e.g., certain metals vs. biodegradable polymers) and the safety profile of its metabolic by-products are critical [73] [75].
Q2: How can I assess the cytotoxicity of a newly synthesized nanocarrier in vitro?
A standard in vitro assessment protocol involves the following key methodologies [6] [74]:
- Cytocompatibility Assays: Use cell lines relevant to the intended application (e.g., L929 mouse fibroblasts, human skin fibroblasts) and standard assays like MTT or MTS to measure cell metabolic activity and viability.
- Histopathological Analysis: Although traditionally in vivo, the principles can be mimicked in advanced 3D cell culture models to observe morphological changes and cell death.
- Hemocompatibility Testing: For intravenously administered nanocarriers, it is essential to test for hemolysis (destruction of red blood cells) and platelet activation.
- Oxidative Stress Evaluation: Measure the generation of reactive oxygen species (ROS) using fluorescent probes, as oxidative stress is a common mechanism of nanotoxicity.
Q3: What is the Enhanced Permeability and Retention (EPR) effect, and how does it relate to nanocarrier biocompatibility?
The EPR effect is a passive targeting mechanism in nanomedicine. Solid tumors often develop leaky vasculature and impaired lymphatic drainage. This allows nanocarriers (typically 10-200 nm) to extravasate and accumulate selectively in tumor tissue, while they cannot readily traverse normal endothelium [11] [20]. From a biocompatibility perspective, exploiting the EPR effect enhances spatial control, delivering drugs more selectively to tumors, which translates to reduced toxicity in healthy tissues and higher therapeutic efficacy [11]. Ensuring nanocarriers are designed to be stable in the bloodstream to take advantage of the EPR effect is therefore a key biocompatibility strategy.
Q4: Can you provide examples of nanocarrier components with favorable biocompatibility profiles?
Yes, several materials are well-established for their biocompatibility:
- Lipids and Phospholipids: Used in liposomes and solid lipid nanoparticles, these are often endogenous or biomimetic, leading to high biocompatibility and biodegradability. Examples include Doxil and DaunoXome [76] [75].
- Biodegradable Polymers: PLGA (poly(lactic-co-glycolic acid)) and PLA (polylactic acid) are FDA-approved polymers that degrade into biocompatible metabolites (lactic acid and glycolic acid) [73] [75].
- PEG (Polyethylene Glycol): Widely used for surface functionalization ("PEGylation") to impart stealth properties, reduce immune recognition, and prolong circulation half-life [73] [11] [20].
- Chitosan: A natural polysaccharide known for its biocompatibility, biodegradability, and mucoadhesive properties [73].
- Certain Inorganic Materials: Iron oxide nanoparticles (e.g., in Feraheme) and mesoporous silica, especially when coated with biocompatible shells, are used in clinically approved products [75] [77].
Troubleshooting Guides
Problem 1: Unexpected High Cytotoxicity in vitro
| Symptom | Possible Cause | Solution |
|---|---|---|
| Significant reduction in cell viability in standard assays (e.g., MTT). | Cationic surface charge causing membrane disruption. | Modify surface chemistry by incorporating anionic or neutral coatings (e.g., PEG) to reduce electrostatic interactions with negatively charged cell membranes [6] [74]. |
| Residual toxic solvents or catalysts from synthesis. | Implement more rigorous purification steps such as dialysis or extensive dialysis/ultrafiltration [6]. | |
| High levels of Reactive Oxygen Species (ROS) generation. | Consider using antioxidant coatings or selecting core materials with lower catalytic activity for ROS production [78] [74]. | |
| Very small particle size (<10 nm) leading to high cellular uptake and reactivity. | Optimize formulation to achieve a larger size, typically within the 20-150 nm range for better biocompatibility balance [73] [11]. |
Problem 2: Rapid Clearance from Bloodstream and Low Target Site Accumulation
| Symptom | Possible Cause | Solution | ||
|---|---|---|---|---|
| Short circulation half-life and low efficacy despite good in vitro performance. | Opsonization and uptake by the Reticuloendothelial System (RES). | PEGylate the nanocarrier surface to create a hydrophilic stealth layer that reduces protein opsonization [11] [20] [74]. | ||
| Particle aggregation in physiological salt conditions. | Ensure surface charge (zeta potential) is sufficiently high (typically | >±30 mV | ) to provide electrostatic stabilization, or use steric stabilizers [6]. | |
| Suboptimal particle size. Particles too large may be filtered by the spleen; too small are cleared by kidneys. | Adjust synthesis parameters to achieve a size between 10-200 nm, with 20-100 nm being optimal for many applications [11] [6]. |
Problem 3: Premature Drug Release (Leakage) Before Reaching Target
| Symptom | Possible Cause | Solution |
|---|---|---|
| Drug detected in plasma; side effects similar to free drug; low therapeutic index. | Diffusion-controlled release from matrix-type systems, which often has a high initial burst release. | Switch to a reservoir-type system (e.g., nanocapsules) or incorporate a polymeric membrane to better control diffusion [11] [20]. |
| Instability of the nanocarrier in blood (e.g., liposome disintegration, polymer swelling). | Improve the stability of the carrier by using higher phase transition lipids or cross-linking the polymer shell [11] [75]. | |
| Lack of stimuli-responsive triggers. | Engineer the nanocarrier to be responsive to specific internal (e.g., pH, redox) or external (e.g., light, ultrasound) stimuli at the target site. For example, use disulfide bonds that are cleaved in the high glutathione (GSH) concentration of the tumor microenvironment [77]. |
Quantitative Data on Nanocarrier Biocompatibility and Toxicity
Table 1: Characterization and Toxicity Profiles of Common Nanocarrier Platforms
| Nanocarrier Platform | Typical Size Range | Common Surface Modifications | Key Biocompatibility & Toxicity Considerations | Clinically Approved Examples |
|---|---|---|---|---|
| Liposomes [76] [75] | 20 nm - several μm | PEGylation, ligand attachment (e.g., antibodies). | Generally highly biocompatible due to phospholipid composition. Can cause Complement Activation-Related Pseudoallergy (CARPA) in some patients. | Doxil, DaunoXome, Marqibo |
| Polymeric NPs (e.g., PLGA) [73] [75] | 10 - 200 nm | PEGylation, surface conjugation with targeting moieties. | Excellent biocompatibility; degrades into metabolites (lactic/glycolic acid) processed via natural pathways. Acidic degradation products can cause local inflammation at high doses. | N/A (Used in numerous FDA-approved sustained-release products) |
| Iron Oxide NPs (IONPs) [75] | 5 - 150 nm | Dextran, PEG, or silica coating. | Generally safe; iron is metabolized and incorporated into the body's iron stores. Uncoated or bare IONPs can cause oxidative stress via Fenton reaction. | Feraheme, Feridex |
| Gold NPs [73] | 1 - 200 nm | Coating with citrate, PEG, or polymers. | Considered low toxicity but strongly dependent on surface chemistry and size. Can induce mild inflammatory responses at high concentrations. | N/A (Extensively used in diagnostics and under investigation for therapy) |
| Dendrimers [76] | 1 - 10 nm | PEGylation, surface functionalization. | Cationic dendrimers (e.g., PAMAM) can be cytotoxic by membrane disruption. Toxicity decreases with surface neutralization or acetylation. | N/A |
Table 2: Key In Vitro Assays for Nanotoxicity Assessment
| Assay Category | Specific Assay/Method | Measured Endpoint | Brief Protocol Outline |
|---|---|---|---|
| Cell Viability | MTT/MTS/XTT Assay | Metabolic activity | 1. Seed cells in a 96-well plate. 2. Treat with nanocarrier suspensions at various concentrations. 3. Incubate with tetrazolium dye (e.g., MTT) for 2-4 hours. 4. Solubilize formazan crystals and measure absorbance [74]. |
| LDH (Lactate Dehydrogenase) Release Assay | Membrane integrity / Necrosis | 1. Treat cells with nanocarriers. 2. Collect culture supernatant after incubation. 3. Mix supernatant with LDH assay reagent. 4. Measure absorbance resulting from conversion of tetrazolium salt. | |
| Oxidative Stress | DCFH-DA Assay | Intracellular ROS levels | 1. Pre-load cells with DCFH-DA, a cell-permeable fluorescent probe. 2. Treat with nanocarriers. 3. Measure fluorescence intensity, which is proportional to ROS levels [74]. |
| Hemocompatibility | Hemolysis Assay | Red blood cell lysis | 1. Incubate nanocarriers with fresh whole blood or red blood cell suspension. 2. Centrifuge to separate intact cells. 3. Measure hemoglobin content in the supernatant via absorbance at 540 nm. Low hemolysis (<5%) is desirable for IV administration [6]. |
Key Signaling Pathways in Nanocarrier-Induced Toxicity
The following diagram illustrates the primary molecular mechanisms by which some nanocarriers can induce cellular toxicity, particularly focusing on oxidative stress.
Diagram Title: Key Signaling Pathways in Nanocarrier-Induced Toxicity
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Nanocarrier Evaluation
| Item | Function in Research | Brief Explanation |
|---|---|---|
| Poly(Lactic-co-Glycolic Acid) (PLGA) | Biodegradable polymer for nanoparticle matrix. | An FDA-approved copolymer used to create nanoparticles that degrade into biocompatible metabolites, allowing for controlled drug release [73] [75]. |
| 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC) | Phospholipid for liposome formation. | A saturated, high-phase-transition phospholipid that confers high rigidity and stability to liposomal bilayers, reducing premature drug leakage [75]. |
| DSPE-PEG(2000) | Stealth coating for nanocarriers. | A phospholipid conjugated to polyethylene glycol, used to incorporate PEG onto the surface of liposomes and other nanoparticles to prolong their circulation time [11] [20]. |
| Glutathione (GSH) | Agent to test redox-responsive release. | Used in in vitro experiments to simulate the reductive intracellular environment (e.g., in the cytoplasm or tumor microenvironment) to trigger drug release from disulfide-bond-containing nanocarriers [77]. |
| MTT Reagent | Cell viability and cytotoxicity assay. | A tetrazolium salt that is reduced by metabolically active cells to a purple formazan product, allowing for the quantitative assessment of nanocarrier cytotoxicity [74]. |
| DCFH-DA Probe | Detection of intracellular reactive oxygen species (ROS). | A cell-permeable dye that becomes fluorescent upon oxidation by ROS, used to measure oxidative stress induced by nanocarriers [74]. |
For researchers in controlled drug release, transitioning from a promising nanocarrier formulation in the lab to consistent, large-scale production presents significant hurdles. The very properties that make nanocarriers effective—their size, surface characteristics, and drug release profile—are often difficult to replicate batch after batch. Manufacturing reproducibility and production cost are identified as critical obstacles that block the clinical translation of nanomedicines from the laboratory to the clinic [79] [6]. Inefficient or suboptimal fabrication strategies are a major contributor to this translational gap [79]. This technical support center provides practical solutions to these specific challenges, framed within the context of a broader thesis on controlled drug release.
Frequently Asked Questions (FAQs)
FAQ 1: Why is there so much batch-to-batch variability in my polymeric nanoparticle size, even when following the same protocol?
Answer: Batch variability often stems from inadequate control over mixing dynamics, solvent displacement rates, and energy input during formation. At the laboratory scale, these parameters might be inconsistently applied. To improve reproducibility:
- Implement Process Analytical Technology (PAT): Transition from batch-quality verification to in-line monitoring. Use Dynamic Light Scattering (DLS) probes to track particle size in real-time during synthesis, allowing for immediate adjustment of process parameters [6].
- Adopt Microfluidic Systems: Replace bulk mixing methods with microfluidic devices. These systems offer superior control over mixing kinetics and shear forces, leading to more homogeneous nucleation and growth of nanoparticles, thereby reducing the polydispersity index (PDI) [79].
- Standardize Raw Materials: Ensure strict quality control of starting polymers (e.g., PLGA, PLA) and solvents. Variations in polymer molecular weight, polydispersity, or end-group functionality can significantly impact the final nanoparticle characteristics [6] [51].
FAQ 2: Our nanocarrier formulation works well in vitro, but fails in animal models. Could this be a manufacturing issue?
Answer: Absolutely. This common problem frequently traces back to inadequate physicochemical characterization before moving to in vivo studies. The "success" of a formulation is defined by a precise set of parameters beyond just size.
- Expand Characterization Protocols: Ensure comprehensive pre-clinical characterization. This must include measuring surface charge (zeta potential), which influences stability and cellular interactions; assessing drug release profiles under physiological conditions; and evaluating stability in biological fluids [6] [80].
- Mimic Scale-Up Conditions Early: Laboratory-scale synthesis (e.g., small magnetic stirrers) creates different shear forces than large-scale reactors. If possible, use small-scale equipment that mimics the hydrodynamic environment of larger production equipment to identify stability issues early [79].
FAQ 3: What are the most significant cost drivers in scaling up nanocarrier production for controlled release applications?
Answer: The primary cost drivers shift from research consumables to operational and quality control expenses.
- Raw Materials: High-purity, clinical-grade lipids, polymers, and functionalized PEG-lipids are a major recurring cost [81] [51].
- Purification and Concentration: Tangential flow filtration (TFF) systems required for buffer exchange and concentration represent significant capital investment and operational costs.
- Quality Control (QC) and Analytics: Rigorous, repeated characterization (size, PDI, zeta potential, encapsulation efficiency, sterility, endotoxin) for every batch is mandatory for Good Manufacturing Practice (GMP) and is a substantial, non-negotiable cost [6].
- Low Yield and Process Efficiency: Inefficient synthesis methods that result in low drug encapsulation efficiency or a high percentage of wasted material drastically increase the cost per dose [79].
Troubleshooting Guides
Problem: High Polydispersity Index (PDI > 0.2) in Liposome Formulations
Issue: Your liposome preparation yields a heterogeneous population of vesicles, which can lead to unpredictable drug release rates and biodistribution.
Step-by-Step Resolution:
- Verify Technique: Ensure the organic solvent is completely removed during the thin film hydration step. Use a rotary evaporator with consistent vacuum and temperature control. An incomplete film is a common source of heterogeneity.
- Optimize Energy Input during Size Reduction: The extrusion process is critical.
- Use polycarbonate membranes with a defined, uniform pore size.
- Maintain the extrusion apparatus (e.g., Lipex extruder) at a constant temperature above the phase transition temperature (Tm) of the primary lipid.
- Standardize the protocol: Extrude through a stack of two membranes for a minimum of 21 passes to ensure a narrow, Gaussian size distribution.
- Characterize with Complementary Techniques: DLS can be skewed by a small population of large aggregates. Validate your DLS results with a fractionation method like Asymmetrical Flow Field-Flow Fractionation (AF4) coupled with MALS (Multi-Angle Light Scattering) to resolve sub-populations and confirm homogeneity [6].
Problem: Low and Variable Encapsulation Efficiency of a Hydrophilic Drug
Issue: The active pharmaceutical ingredient (API) is not being efficiently trapped within the nanocarrier, leading to wasted material and insufficient dosing.
Step-by-Step Resolution:
- Select the Appropriate Loading Method:
- For Passive Loading: The drug is incorporated during the nanocarrier formation. Optimize the drug-to-lipid/polymer ratio and the internal aqueous phase volume.
- For Active Loading (Remote Loading): If the API is an ionizable amine, use a pH gradient (e.g., interior: ammonium sulfate, exterior: buffer). The uncharged drug diffuses across the membrane and precipitates as a sulfate salt inside, achieving >90% encapsulation. Ensure the gradient is stable and the incubation time/temperature is optimized.
- Prevent Leaching: After loading, remove unencapsulated drug promptly using gel filtration chromatography or TFF. If the final buffer lacks a stabilizing gradient, drug leakage may occur over time.
- Analyze the Cause: Measure encapsulation efficiency immediately after purification and again after 24-48 hours. A significant drop indicates a stability problem with the bilayer or matrix, requiring formulation re-engineering (e.g., adjusting lipid composition or adding cholesterol to increase rigidity) [82] [51].
Essential Characterization Data for Reproducibility
The following parameters must be rigorously monitored and documented for every batch to ensure consistency and predict in vivo performance.
Table 1: Key Physicochemical Properties for Nanocarrier Characterization
| Property | Target Range | Analytical Technique | Impact on Performance & Reproducibility |
|---|---|---|---|
| Particle Size | 20-200 nm (for IV) | Dynamic Light Scattering (DLS) | Biodistribution, EPR effect, clearance by RES [6] |
| Polydispersity Index (PDI) | < 0.2 (Monodisperse) | Dynamic Light Scattering (DLS) | Indicates batch homogeneity; high PDI leads to variable drug release [6] |
| Zeta Potential | ± >30 mV (high stability) | Electrophoretic Light Scattering | Predicts colloidal stability; prevents aggregation during storage [6] |
| Drug Encapsulation Efficiency (EE%) | > 90% (ideal) | HPLC/UV-Vis after separation | Directly impacts cost and dosing accuracy; low EE wastes API [51] |
| Drug Release Profile | Sustained over days/weeks | Dialysis under sink conditions | Critical for controlled release thesis; must be reproducible batch-to-batch [6] |
Table 2: Primary Cost Drivers in Nanocarrier Manufacturing
| Cost Category | Specific Examples | Strategies for Mitigation |
|---|---|---|
| Raw Materials | Clinical-grade lipids, PEG-lipids, functional polymers, targeting ligands | Dual-sourcing strategies; bulk purchasing at later stages; explore generic alternatives where possible [81] [51] |
| Equipment & Capital | TFF systems, microfluidic homogenizers, GMP-capable reactors | Leverage contract development and manufacturing organizations (CDMOs) for early-phase work to avoid capital outlay [79] |
| Quality Control & Analytics | Repeated DLS, HPLC, sterility/endotoxin testing, stability studies | Invest in robust, transferable assays early; use QC data with statistical process control to reduce failed batches [6] |
| Process Loss & Yield | Low encapsulation efficiency, purification losses, batch failure | Process intensification; continuous manufacturing; implementing PAT to reduce rejects [79] |
Standard Experimental Workflows
The diagrams below outline critical workflows for ensuring reproducible and well-characterized nanocarriers.
Diagram 1: Nanocarrier Characterization Workflow
Diagram 2: Manufacturing Process Improvement Cycle
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanocarrier Research and Development
| Reagent/Material | Function in Controlled Release Research |
|---|---|
| PLGA / PLA Polymers | Biodegradable, biocompatible polymer matrix for sustained drug release over weeks to months [51] |
| DSPC / Cholesterol Lipids | Primary lipid and stabilizer for forming robust, stable liposomal bilayers with controlled permeability [82] |
| PEG-lipids (e.g., DSPE-PEG) | Surface modification to confer "stealth" properties, reduce opsonization, and prolong blood circulation time [51] |
| Microfluidic Mixers | Chip-based devices (e.g., staggered herringbone mixer) to achieve highly reproducible nanoprecipitation [79] |
| Size Exclusion Gels (e.g., Sephadex G-50) | For purification of nanocarriers, separating encapsulated drug from free, unencapsulated drug [6] |
| Ammonium Sulfate | Key reagent for creating a transmembrane pH gradient for active remote loading of weak base drugs [82] |
Optimizing Drug Loading Capacity and Encapsulation Efficiency
Core Concepts and Definitions
What are the fundamental parameters used to assess drug loading in nanocarriers?
Drug Loading Capacity (DLC) and Encapsulation Efficiency (EE) are two critical quality attributes used to evaluate the success of the nanoparticle formulation process. Entrapment Efficiency (EE) is a measure of process effectiveness and drug load, representing the percentage of the initial drug amount that is successfully incorporated into the nanoparticles. Drug Loading Capacity (DLC) indicates the amount of drug weight contained per unit weight of the final nanoparticle formulation [83] [84].
Why is optimizing EE and DLC crucial for controlled drug delivery systems?
High encapsulation efficiency is vital for economic and therapeutic reasons, minimizing drug waste during production and ensuring accurate dosing. For controlled-release systems, sufficient drug loading is a prerequisite to achieve sustained release kinetics that maintain drug concentration within the therapeutic window—between the minimum effective concentration and the minimum toxic concentration—over an extended period [11] [20]. Optimizing these parameters allows for reduced dosing frequency and improved patient compliance [84].
What are the primary mechanisms controlling drug release from nanocarriers?
Drug release from nanocarriers is governed by several mechanisms, which can operate independently or in concert [11] [20]:
- Diffusion-Controlled Release: Drug molecules diffuse through the carrier matrix or a polymeric membrane driven by concentration gradients.
- Solvent-Controlled Release: Includes osmosis-controlled release (water influx into the carrier) and swelling-controlled release (polymer hydration and chain relaxation enabling drug diffusion).
- Degradation-Controlled Release: Drug release occurs as the polymer matrix undergoes hydrolytic or enzymatic degradation.
- Stimuli-Responsive Release: Nanocarriers are engineered to release their payload in response to specific physiological stimuli in the tumor microenvironment, such as low pH, elevated enzymes, or redox conditions [4] [7].
Table 1: Key Formulation Parameters Influencing EE and DLC
| Parameter | Impact on EE/DLC | Optimization Consideration |
|---|---|---|
| Polymer-Drug Ratio (P/D) [84] [85] | Higher polymer content typically increases EE but may reduce DLC percentage. | Optimal P/D balances sufficient EE with therapeutic drug payload. |
| Polymer Properties (MW, composition) [85] | Molecular weight (MW) and lactide/glycolide (LA/GA) ratio affect matrix density and degradation rate. | Adjust based on desired release profile; higher MW and LA content often slow release. |
| Emulsifier HLB [84] | Hydrophilic-Lipophilic Balance affects emulsion stability and droplet size during preparation. | Match HLB to polymer and drug hydrophobicity for stable emulsion formation. |
| Nanoparticle Size [85] | Smaller particles have larger surface area, potentially increasing initial burst release. | Control via process parameters (stirring speed, emulsification method) to modulate release kinetics. |
| Drug-Polymer Interaction | Hydrophobic drugs typically show higher EE in hydrophobic polymers like PLGA. | Drug solubility in polymer solution is a key predictor of successful encapsulation. |
Optimization Strategies and Experimental Design
What advanced statistical approaches can efficiently optimize EE and DLC?
Traditional one-variable-at-a-time optimization is inefficient due to complex factor interactions. Design of Experiments (DoE) is a superior statistical approach that systematically varies all relevant factors simultaneously to build mathematical models, identify optimal conditions, and understand factor interactions with fewer experiments [84] [85].
For instance, a Draper-Lin small composite design has been successfully used to optimize microspheres, evaluating factors like polymer loading, emulsifier HLB, antitacking agent percentage, and dispersed phase volume on responses including EE, particle size, and release profile [84].
Can existing literature data be used for optimization without new experiments?
An emerging evidence-based approach uses meta-analysis of historical data from published literature as input for DoE. This method extracts release data and formulation factors from multiple studies, performs regression modeling to understand relationships, and links this to the drug's therapeutic window for numerical optimization [85]. This approach is particularly valuable for well-researched drug-carrier systems like PLGA-vancomycin capsules [85].
How does continuous manufacturing improve nanoparticle quality attributes?
Continuous manufacturing platforms (e.g., turbulent jet mixers) offer significant advantages over traditional batch processes for nanoparticle production [86]:
- Higher Encapsulation Efficiency: Rapid and efficient mixing ensures better interaction between cargo and lipid/polymer components.
- Narrower Particle Size Distribution: Promotes uniform particle sizes, which contributes to more consistent drug release profiles.
- Enhanced Reproducibility: Real-time monitoring and inline feedback allow precise control of Critical Process Parameters (CPPs), ensuring batch-to-batch consistency of Critical Quality Attributes (CQAs) like size, EE, and drug release [86].
DoE Optimization Workflow
Troubleshooting Common Experimental Challenges
What are the most common causes of low encapsulation efficiency?
- Drug-Polymer Compatibility Mismatch: Hydrophilic drugs often show poor EE in hydrophobic polymers due to partitioning into the external aqueous phase during emulsion-based preparation [84]. Solution: Use polymer-drug combinations with matched hydrophobicity or implement double emulsion methods for hydrophilic drugs.
- Inefficient Emulsification: Unstable emulsion leads to drug diffusion before nanoparticle solidification. Solution: Optimize emulsifier type, concentration, and HLB value; ensure sufficient homogenization energy [84].
- Improper Solvent Removal Rate: Slow solvent evaporation allows more time for drug leakage. Solution: Optimize temperature, pressure, and stirring conditions to achieve rapid solvent extraction [84].
How can initial burst release be minimized?
Initial burst release occurs when drug molecules located on or near the nanoparticle surface rapidly dissolve upon contact with release medium [85].
- Strategy 1: Increase nanoparticle size to reduce surface area-to-volume ratio.
- Strategy 2: Incorporate a polymeric coating or shell to create a diffusion barrier.
- Strategy 3: Optimize polymer molecular weight and crystallinity to reduce matrix porosity.
- Strategy 4: Ensure efficient removal of surface-bound drug through rigorous washing steps post-formulation.
Why do different labs obtain different EE and release profiles with the same formulation?
Variations in EC₅₀ or IC₅₀ values between laboratories are primarily caused by differences in stock solution preparation, particularly at the 1 mM concentration [87]. Minor differences in solvent quality, water purity, weighing accuracy, or solution storage conditions can significantly impact experimental outcomes. Standardization of solution preparation protocols and using qualified reference standards is essential for reproducibility.
Table 2: Troubleshooting Guide for Common Formulation Problems
| Problem | Potential Causes | Corrective Actions |
|---|---|---|
| Low EE | Drug leakage to continuous phase, rapid solvent diffusion, incompatible excipients. | - Increase polymer concentration [84]- Optimize emulsifier HLB [84]- Adjust dispersed phase volume [84] |
| High Initial Burst Release | Drug accumulation on particle surface, high surface area, porous matrix. | - Add surface coating (e.g., PEG) [11] [20]- Increase nanoparticle size [85]- Optimize polymer MW and LA/GA ratio [85] |
| Incomplete Drug Release | Strong drug-polymer interactions, low polymer degradation, insufficient release time. | - Modify polymer composition to enhance degradation [11]- Include porogens in formulation- Use polymer with appropriate LA/GA ratio [85] |
| Broad Size Distribution | Inefficient mixing, non-uniform emulsion droplets, aggregation. | - Implement continuous mixing (e.g., turbulent jet mixers) [86]- Optimize surfactant type and concentration- Improve homogenization method |
| Poor Batch-to-Batch Reproducibility | Uncontrolled process parameters, manual processing steps. | - Adopt continuous manufacturing [86]- Implement Process Analytical Technology (PAT) for real-time monitoring [86] |
Essential Methodologies and Protocols
What are the standard methods for determining encapsulation efficiency?
EE determination requires separation of encapsulated drug from unencapsulated drug, followed by quantification [83]. The general protocol involves:
- Separation Techniques: Ultracentrifugation, gel filtration, dialysis, or ultrafiltration.
- Quantification: HPLC-UV/VIS is most common; fluorescence spectroscopy for fluorescent drugs.
- Calculation: EE% = (Amount of drug in nanoparticles / Total drug added) × 100
Critical Consideration: The separation method must be validated to ensure no nanoparticle disruption during analysis and complete removal of unencapsulated drug [83]. Only 72% of studies in a recent review provided sufficient methodological detail for reproduction—highlighting the need for thorough reporting [83].
How is controlled release kinetics experimentally evaluated and modeled?
In vitro release studies are typically performed in sink conditions using:
- Apparatus: Dialysis method or sample-and-separate techniques.
- Media: Phosphate-buffered saline (PBS) at physiological pH (7.4) or simulated pathological environments (e.g., pH 6.5-5.5 for tumor models) [4].
- Analysis: Drug concentration quantification at predetermined time points via HPLC or UV-Vis spectroscopy.
Release kinetic modeling employs mathematical models to understand release mechanisms [11] [20]:
- Zero-Order Model: Q = k₀t (ideal for controlled release)
- Higuchi Model: Q = kH√t (diffusion-controlled release)
- Korsmeyer-Peppas Model: Mt/M∞ = ktn (determines release mechanism)
Drug Release Mechanisms
Research Reagent Solutions
Table 3: Essential Materials for Nanocarrier Formulation and Characterization
| Reagent/Material | Function/Application | Examples/Notes |
|---|---|---|
| Biodegradable Polymers | Form nanoparticle matrix; control degradation & release kinetics. | PLGA (varying LA/GA ratios, MW) [85], Eudragit RLPO/RSPO [84], Chitosan [7] |
| Surfactants/Emulsifiers | Stabilize emulsions during preparation; control particle size. | Span series, Tween series [84]; PVA; Poloxamers; Optimize HLB value for system [84] |
| Antitacking Agents | Prevent nanoparticle aggregation during preparation. | Talc [84], colloidal silica |
| Organic Solvents | Dissolve polymer and drug for nanoparticle formation. | Dichloromethane (DCM), acetone [84], ethyl acetate |
| Characterization Standards | Validate analytical methods for EE and drug release. | Drug reference standards, polymer characterization standards [83] |
| Continuous Processing Equipment | Advanced nanoparticle manufacturing with improved reproducibility. | Turbulent jet mixers [86], microfluidic systems |
Advanced Applications and Future Perspectives
How do pH-responsive nanocarriers enhance targeted drug delivery?
pH-responsive nanocarriers exploit the acidic tumor microenvironment (pH 6.5-6.8) or endosomal/lysosomal compartments (pH 5.0-5.5) for selective drug release at target sites [4]. These systems utilize materials with ionizable groups or acid-labile linkages that undergo:
- Protonation-induced charge shifts that disrupt nanoparticle structure
- Acid-labile bond cleavage (e.g., hydrazone, acetal) releasing conjugated drugs
- Disruption of hydrophobic interactions causing nanoparticle disassembly
This targeting strategy enhances therapeutic precision while minimizing systemic exposure [4].
What role does surface modification play in optimizing nanocarrier performance?
Surface engineering is critical for controlling nanocarrier behavior in biological systems:
- PEGylation: Grafting polyethylene glycol (PEG) chains creates a hydrophilic protective layer that reduces opsonization, extends circulation half-life, and enhances tumor accumulation via the Enhanced Permeability and Retention (EPR) effect [11] [20].
- Ligand Functionalization: Conjugating targeting moieties (antibodies, peptides, folates) enables active targeting to receptors overexpressed on specific cell types, further improving site-specific delivery [7].
What are the emerging trends in nanocarrier optimization?
- Multi-responsive Systems: Next-generation nanocarriers respond to multiple stimuli (pH, enzymes, redox, temperature) for precise spatiotemporal control [4].
- Continuous Manufacturing: Moving from batch to continuous production using platforms with turbulent jet mixers improves reproducibility, scalability, and quality control [86].
- Computational Workflows: Integration of meta-analysis with DoE enables data-driven formulation optimization without extensive trial-and-error experimentation [85].
- Advanced Characterization: Implementation of Process Analytical Technology (PAT) and inline monitoring during manufacturing provides real-time quality assurance [86].
Troubleshooting Guide: Common Scenarios and Solutions
Problem: Rapid Initial Burst Release of Drug
- Question: Why does my nanocarrier formulation show a high initial burst release in vitro?
- Investigation: This is often observed in matrix-type nanospheres where drug molecules are dispersed throughout the polymer matrix without a diffusion barrier [11]. The large surface area to volume ratio of nanocarriers exacerbates this effect [11].
- Solution: Consider formulating a reservoir system instead, where the drug core is surrounded by a polymeric membrane to better control initial release rates [11] [1]. Alternatively, optimize your matrix composition to strengthen drug-polymer interactions.
Problem: Nanocarrier Aggregation in Physiological Fluid
- Question: My nanocarriers are aggregating in simulated physiological conditions. What could be the cause?
- Investigation: Aggregation is frequently due to an insufficient surface charge (zeta potential) [6]. A zeta potential near neutral (e.g., between -10 mV and +10 mV) may not provide enough electrostatic repulsion to prevent particle attraction [6].
- Solution: Modify the surface chemistry. PEGylation ( coating with polyethylene glycol) creates a hydrated steric barrier that prevents aggregation and opsonization, leading to a longer circulation time [11]. Alternatively, adjust the formulation to achieve a zeta potential of |±30| mV or greater for improved electrostatic stability [6].
Problem: In Vivo Instability and Premature Drug Leakage
- Question: The formulation is stable in buffer but shows significant drug leakage in circulation. How can I improve stability?
- Investigation: The nanocarriers may be destabilized by enzymes or other substances in the blood [88]. Furthermore, nanoparticles that are "too stable" might not release the drug at the target site, while unstable ones cause side effects [88].
- Solution: Incorporate stimuli-responsive "smart" materials. Use linkers or polymers that are stable in circulation but degrade in response to specific internal stimuli at the target site, such as lower pH (e.g., in tumors), higher redox potential (e.g., elevated glutathione), or specific enzymes [88].
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary mechanisms of drug release from nanocarriers? Drug release is primarily governed by three core mechanisms [11] [89]:
- Diffusion-Controlled Release: The drug diffuses through a carrier matrix or a barrier membrane, driven by a concentration gradient. Reservoir systems (capsule-type) often provide more constant release, while matrix systems can exhibit a high initial burst [11].
- Solvent-Controlled Release: This includes osmosis-controlled release (water inflow through a semi-permeable membrane) and swelling-controlled release (water uptake causes the polymer matrix to swell, enabling drug release) [11].
- Degradation-Controlled Release: The drug is released as the biodegradable polymer matrix (e.g., polyesters, polyamides) erodes due to chemical or enzymatic reactions [11].
FAQ 2: Which critical physicochemical properties must I characterize to predict circulation stability? The table below summarizes the key properties, their impact on stability, and characterization methods.
Table 1: Key Characterization for Nanocarrier Stability
| Property | Impact on Stability & Circulation | Recommended Characterization Technique | ||
|---|---|---|---|---|
| Particle Size & PDI [6] | Particles <10 nm are subject to renal clearance. Size affects biodistribution, cellular uptake, and circulation half-life. A high Polydispersity Index (PDI) indicates heterogeneity and can lead to unpredictable behavior. | Dynamic Light Scattering (DLS). Confirm with Electron Microscopy (SEM/TEM) or Atomic Force Microscopy (AFM) for morphology [6]. | ||
| Zeta Potential [6] | Indicates surface charge and colloidal stability. A high value ( | ±30 | mV) prevents aggregation via electrostatic repulsion. Surface charge also influences protein adsorption and clearance by the RES [11] [6]. | Electrophoretic Light Scattering (Laser Doppler Velocimetry) [6]. |
| Surface Hydrophobicity [6] | Hydrophobic surfaces are rapidly opsonized and cleared by the Mononuclear Phagocyte System (MPS). | Hydrophobic Interaction Chromatography, Biphasic Partitioning, or X-ray Photon Correlation Spectroscopy [6]. | ||
| Drug Release Profile | A large initial burst release leads to systemic toxicity and reduces drug delivery to the target site. The goal is minimal release in circulation and controlled release at the target. | In vitro release studies using dialysis or Franz diffusion cells under sink conditions, mimicking physiological pH (7.4) and target site conditions (e.g., pH 6.5-6.8 for tumors) [88]. |
FAQ 3: What formulation strategies can I use to prevent premature release?
- Surface PEGylation: Grafting polyethylene glycol (PEG) onto the nanocarrier surface forms a hydrated steric barrier. This reduces opsonization (protein binding), RES uptake, and premature drug leakage, significantly extending circulation time [11].
- Stimuli-Responsive Formulations: Design nanocarriers that release their payload only upon encountering specific internal or external stimuli at the target site [88].
- Optimized Nano-Encapsulation: Use high-affinity drug-carrier interactions (e.g., ionic, hydrophobic) and a uniform, defect-free polymer matrix or membrane to retard drug diffusion during circulation [11] [90].
Experimental Protocols for Stability Assessment
Protocol 1: Assessing Serum Stability and Drug Retention
- Objective: To evaluate the stability of nanocarriers and their ability to retain the drug in physiologically relevant conditions.
- Materials: Nanocarrier formulation, fetal bovine serum (FBS) or phosphate-buffered saline (PBS), dialysis membrane (if needed), dynamic light scattering (DLS) instrument, HPLC or UV-Vis spectrometer.
- Method:
- Dilute the nanocarrier formulation in PBS (pH 7.4) containing 10-50% FBS.
- Incubate the mixture at 37°C under gentle agitation.
- At predetermined time points (e.g., 0, 1, 2, 4, 8, 24 h), withdraw aliquots.
- For size and PDI: Dilute an aliquot with purified water and measure immediately by DLS to monitor aggregation [6].
- For drug retention: Centrifuge the aliquot using a centrifugal filter (molecular weight cutoff) to separate released drug from encapsulated drug. Quantify the released drug in the filtrate using an analytical method (HPLC/UV-Vis) [90].
Protocol 2: Investigating pH-Triggered Drug Release
- Objective: To validate the functionality of a pH-responsive nanocarrier system.
- Materials: pH-responsive nanocarriers, release media at different pH values (e.g., PBS pH 7.4, acetate buffer pH 5.0 or 6.5), dialysis tubing, Franz diffusion cells.
- Method:
- Place the nanocarrier dispersion inside a dialysis membrane.
- Immerse the membrane in a large volume of release medium at pH 7.4 (simulating blood) to maintain sink conditions.
- Incubate at 37°C. At scheduled intervals, sample the external medium and replace with fresh pre-warmed medium to maintain sink conditions.
- After a set period (e.g., 10 h), carefully replace the external medium with a pre-warmed acidic buffer (pH 5.0 or 6.5) to simulate the tumor microenvironment or lysosomal pH.
- Continue sampling and quantify the drug content to generate two-stage release profile: minimal release at pH 7.4 followed by accelerated release at acidic pH [88].
Research Reagent Solutions
Table 2: Essential Materials for Developing Stable Nanocarriers
| Reagent / Material | Function in Preventing Premature Release |
|---|---|
| Polyethylene Glycol (PEG) [11] | The gold standard for "stealth" coating. Provides a steric hydration layer that minimizes protein adsorption (opsonization) and recognition by the immune system, thereby enhancing circulation time and stability. |
| Poly(Lactic-co-Glycolic Acid) (PLGA) [89] | A biodegradable polyester used as a matrix material. Allows for controlled release kinetics through degradation. Its properties can be tuned based on the LA:GA ratio and molecular weight. |
| pH-Sensitive Polymers (e.g., Eudragit) [1] | Used for delayed release to protect drugs from the stomach acid or for triggered release in slightly acidic environments like tumors (pH ~6.5-6.8) or endosomes (pH ~5.5). |
| Hydrophilic Matrix Formers (e.g., HPMC) [1] | Forms a gel layer upon contact with aqueous media, controlling drug release through a combination of diffusion and erosion. Ideal for creating sustained-release oral formulations. |
| DSPE-PEG [11] | A phospholipid-PEG conjugate widely used to PEGylate the surface of liposomal and lipid-based nanocarriers, providing a stealth property and improving colloidal stability. |
| Crosslinkers (e.g., Disulfide-based) [88] | Used to crosslink the shell of nanocapsules or polymer chains in hydrogels. The crosslinks remain stable in circulation but break under the high redox potential (elevated glutathione) in the cytoplasm of target cells, enabling triggered release. |
Stability Optimization Workflow
The following diagram illustrates a logical workflow for diagnosing and addressing premature drug release in nanocarriers.
Mechanisms of Controlled Drug Release
Understanding the fundamental release mechanisms is crucial for designing nanocarriers that prevent premature release. The following diagram summarizes the primary mechanisms.
From Bench to Bedside: Preclinical Models, Clinical Validation, and Comparative Analysis of Nanocarrier Systems
In Vitro and In Vivo Models for Assessing Release Kinetics and Efficacy
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary limitations of traditional mathematical models (e.g., Korsmeyer-Peppas) for predicting drug release from nanocarriers, and what are the modern alternatives?
Traditional semi-empirical models like Korsmeyer-Peppas and Weibull rely on fixed mathematical forms and a limited number of parameters, which often fail to capture the complex, nonlinear nature of drug release from modern nanocarrier systems, such as those made from PLGA [91]. Their predictability is limited under different drug-carrier combinations as they operate under idealized assumptions, such as homogeneous matrices and constant diffusion coefficients [92].
Modern alternatives leverage machine learning (ML) and data-driven modeling to overcome these limitations. For instance:
- Neural Networks (e.g., DrugNet): A multilayer perceptron (MLP) neural network can use key physicochemical characteristics of the PLGA carrier (molecular weight, PDI, particle size) and the drug itself to predict release profiles with significantly higher accuracy than traditional models [91].
- Gaussian Process Regression (GPR): This non-parametric, probabilistic ML model is effective for handling smaller datasets and capturing highly nonlinear relationships. It has been used to predict key formulation characteristics and optimize liposomal nanocarriers [93] [92].
FAQ 2: How does the pH of the release environment influence drug release kinetics, and how can this be leveraged in therapy?
The pH value of the release matrix or environment is a critical factor affecting drug release profiles, particularly for polymers like PLGA [92]. This is exploited through the design of pH-responsive nanocarriers that take advantage of the acidic tumor microenvironment (TME) [4].
The molecular mechanisms driving pH sensitivity include:
- Protonation-induced charge shifts: Functional groups on the polymer gain a positive charge in acidic environments, causing nanoparticle swelling or disruption.
- Cleavage of acid-labile bonds: Chemical bonds designed into the nanocarrier break specifically at low pH, triggering drug release.
- Disruption of hydrophobic interactions: Changes in polymer solubility at different pH levels can alter the nanocarrier's structure [4].
This allows for site-specific drug release in acidic tumor tissues, enhancing therapeutic precision and reducing off-target effects [4] [94].
FAQ 3: What are the essential parameters to characterize for a PLGA-based nanocarrier to ensure reproducible and predictable drug release?
To reliably model and predict drug release behavior, researchers should comprehensively characterize the following key parameters of PLGA carriers, many of which are used as inputs for advanced ML models [91]:
- Molecular Weight: Affects the degradation rate and, consequently, the drug release rate.
- Polydispersity Index (PDI): Indicates the uniformity of the polymer chains, which influences batch-to-batch consistency and release kinetics.
- Particle Size: Impacts stability, cellular uptake, and the surface-area-to-volume ratio, which governs early-stage release.
- Zeta Potential: Reflects the surface charge and colloidal stability of the nanocarrier suspension.
- Lactide:Glycolide (LA:GA) Monomer Ratio: Determines the degradation profile and hydration rate of the PLGA polymer.
- Encapsulation Efficiency (EE): The percentage of drug successfully loaded; affects the total dose and release profile.
FAQ 4: We are observing an initial burst release in our in vitro drug release assay. Is this a cause for concern?
An initial burst release is a common phenomenon in nanocarrier systems, where a significant portion of the encapsulated drug is released rapidly at the early stage [92]. While sometimes desirable for achieving a quick therapeutic effect, it is often a concern as it can lead to:
- Premature drug depletion before reaching the target site.
- Potential toxicity from a sudden high dose of the drug.
In vitro studies have documented burst releases; for example, a liposomal fentanyl formulation showed an initial burst of approximately 10% before transitioning to a sustained release profile [93]. Investigating the cause is essential. It is often attributed to drug molecules adsorbed on or near the nanoparticle surface. Strategies to mitigate it include optimizing the encapsulation process, modifying the polymer matrix, or applying a surface coating [92].
Troubleshooting Guides
Table 1: Troubleshooting In Vitro Drug Release Testing
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High variability between replicate samples | Inconsistent nanocarrier synthesis (size, PDI), inadequate sink conditions, or unstable temperature/pH. | Standardize synthesis protocol to ensure uniform PDI and particle size [91]; validate that sink conditions are maintained throughout the experiment [95]. |
| Release profile does not match predictive models | Traditional semi-empirical models are too simplistic for complex release mechanisms (e.g., combined diffusion and erosion). | Adopt a data-driven machine learning approach (e.g., ANN, GPR) that can handle nonlinear relationships and multiple input parameters [91] [92]. |
| Lack of in vitro-in vivo correlation (IVIVC) | In vitro conditions fail to mimic the complex physiological environment (e.g., cellular interactions, protein corona, dynamic flow). | Consider using more biorelevant dissolution media and incorporate stimuli-responsive elements (e.g., pH-sensitive polymers) into the nanocarrier design to better simulate the in vivo TME [4] [94]. |
| Unacceptable initial burst release | High surface-associated drug or poor encapsulation efficiency. | Optimize formulation parameters like drug-polymer ratio and consider surface modifications or different fabrication techniques to improve core encapsulation [93] [92]. |
Table 2: Interpreting Discrepancies Between In Vitro and In Vivo Efficacy
| In Vitro Observation | In Vivo Observation | Potential Explanation & Investigation Path |
|---|---|---|
| Sustained release profile over time. | Rapid clearance and low efficacy. | The nanocarrier may be undergoing rapid systemic clearance by the reticuloendothelial system (RES). Investigate surface modification with PEG or other stealth coatings to improve circulation time [96]. |
| High cytotoxicity at target cells. | Low therapeutic efficacy and high systemic toxicity. | Lack of targeting leads to distribution in healthy tissues. Explore active targeting strategies by functionalizing the nanocarrier with ligands specific to markers on target cells (e.g., endothelial cells in diseased tissues) [94] [96]. |
| Good efficacy in cell monolayers. | Poor penetration in solid tumors. | The nanocarrier may have poor penetration in dense tissue. Investigate the Enhanced Permeability and Retention (EPR) effect and consider strategies to enhance it, such as reducing particle size or designing transcytosis-capable carriers [96]. |
Experimental Protocols & Data Presentation
Protocol 1: Standard In Vitro Drug Release Testing via Dialysis
This is a widely used method to evaluate the release kinetics of drug-loaded nanocarriers under controlled, sink conditions [95] [93].
Principle: The nanocarrier formulation is placed in a dialysis membrane tube (molecular weight cutoff selected to retain the nanocarrier but allow free drug diffusion). The tube is immersed in a release medium (e.g., Phosphate-Buffered Saline, pH 7.4, at 37°C) under continuous agitation. The release of the drug from the nanocarrier, through the membrane, and into the medium is quantified over time [93].
Key Steps:
- Preparation: Place a precise volume of the nanocarrier suspension into a pre-hydrated dialysis membrane bag and seal both ends tightly.
- Immersion: Immerse the bag in a known volume of release medium maintained at 37°C with constant stirring.
- Sampling: At predetermined time intervals, withdraw a small aliquot of the release medium from outside the dialysis bag.
- Replenishment: Immediately replace the withdrawn volume with fresh, pre-warmed medium to maintain sink conditions.
- Analysis: Analyze the collected samples using a validated analytical method (e.g., HPLC, UV-Vis spectroscopy) to determine the cumulative percentage of drug released.
- Data Fitting: Plot the cumulative drug release versus time and fit the data to appropriate kinetic models (e.g., traditional Korsmeyer-Peppas or machine learning models) [91] [95] [93].
Protocol 2: AI-Enhanced Formulation Optimization and Characterization
This protocol integrates artificial intelligence to objectively analyze and optimize nanocarrier properties, as demonstrated for liposomal fentanyl [93].
Principle: Use machine learning models to predict optimal formulation parameters and to automate the characterization of nanocarrier morphology, moving beyond subjective manual analysis.
Key Steps:
- Data Collection for Modeling: Prepare multiple batches of nanocarriers with varying formulation parameters (e.g., lipid types, ratios, drug loading). For each batch, record the input parameters and the resulting output characteristics (e.g., particle size, PDI, encapsulation efficiency).
- Predictive Model Training: Use this dataset to train a Gaussian Process Regression (GPR) model. This model can then predict the final nanocarrier characteristics based on new input formulation parameters, enabling data-driven optimization [93].
- Morphological Analysis with AI: Obtain Scanning Electron Microscopy (SEM) images of the optimized nanocarriers. Instead of manual counting, use a Convolutional Neural Network (CNN) implemented in TensorFlow/Keras to automatically classify and quantify liposome morphology (e.g., percentage of spherical, aggregated, or broken particles) [93].
- In Vivo Validation: Evaluate the optimized formulation in a relevant animal model (e.g., rat pain model). Compare the efficacy and safety (e.g., analgesic duration, respiratory effects) of the novel formulation against the standard drug to confirm the in vitro-in vivo correlation [93].
Table 3: Key Input Parameters for Data-Driven Drug Release Models
This table summarizes critical parameters used in advanced models like DrugNet to predict drug release from PLGA nanoparticles [91].
| Parameter Category | Specific Parameter | Role in Release Kinetics |
|---|---|---|
| PLGA Carrier Properties | Molecular Weight, Polydispersity Index (PDI) | Governs polymer degradation rate and release control. |
| Particle Size, Zeta Potential | Influences stability, surface area, and initial burst release. | |
| Lactide:Glycolide Monomer Ratio | Determines degradation profile (hydrophobicity/hydrolysis rate). | |
| Encapsulation Efficiency | Affects total drug payload and release profile shape. | |
| Drug Properties | Molecular Weight, LogP (Hydrophobicity) | Determines diffusion rate through the polymer matrix. |
| Hydrogen Bond Donors/Acceptors, Polar Surface Area | Influences drug-polymer interactions and solubility. | |
| Experimental Conditions | pH of Release Medium | A critical factor, especially for pH-responsive systems [4] [92]. |
| Time Point | The specific time at which release percentage is measured. |
Research Reagent Solutions
Table 4: Essential Materials for Nanocarrier Release and Efficacy Studies
| Item | Function & Application |
|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable, FDA-approved polymer for creating controlled-release nanoparticle cores. Its properties (MW, LA:GA ratio) are key model inputs [91] [92]. |
| Dialysis Membranes | Used in in vitro release studies to physically separate nanocarriers from the release medium while allowing free drug diffusion, enabling kinetic analysis [93]. |
| Phosphate-Buffered Saline (PBS) | A standard isotonic solution (pH 7.4) used as a release medium to simulate physiological conditions for in vitro testing [91]. |
| Machine Learning Libraries (e.g., scikit-learn, TensorFlow/Keras) | Software tools essential for implementing data-driven models like Gaussian Process Regression (GPR) and Convolutional Neural Networks (CNN) for formulation optimization and image analysis [93]. |
| PubChem Database & RDKit Toolset | Resources for obtaining drug structures and calculating molecular descriptors (e.g., LogP, molecular weight) used as features in predictive release models [91]. |
Workflow and Pathway Visualizations
Integrated Drug Release Assessment Workflow
Data-Driven Release Prediction Pathway
Analyzing Clinical Trial Outcomes of Approved Nanomedicines
The application of nanotechnology in medicine has transitioned from a promising research field to a well-integrated component of modern healthcare, particularly in oncology. Nanomedicine is defined as the use of nanoscale materials, typically ranging from 1-100 nm, for the diagnosis, treatment, and prevention of diseases [97] [98]. These sophisticated systems are engineered to improve drug solubility, extend circulation half-life, and enable targeted delivery to specific tissues, thereby enhancing therapeutic efficacy while reducing systemic side effects [11] [98].
The clinical impact of nanomedicine is substantial and growing. As of 2024, the global nanomedicine market was valued at $294.04 billion, with projections estimating growth to $779.19 billion by 2033, reflecting a compound annual growth rate (CAGR) of 10.86% [99]. This growth is fueled by continued innovation and clinical adoption. Currently, there are approximately 100 nanomedicines commercially available, with an additional 563 in various stages of clinical development [97]. The majority of these investigational nanomedicines focus on cancer treatment (53%), followed by infectious diseases (14%) [97].
Table 1: Key Market and Clinical Trial Statistics for Nanomedicines
| Metric | Value | Source/Timeframe |
|---|---|---|
| Global Market Value (2024) | USD 294.04 Billion | [99] |
| Projected Market Value (2033) | USD 779.19 Billion | [99] |
| CAGR (2025-2033) | 10.86% | [99] |
| Commercially Available Nanomedicines | 100 | [97] |
| Nanomedicines in Clinical Development | 563 | [97] |
| Clinical Trials Focused on Cancer | 53% | [97] |
A foundational concept in cancer nanomedicine is the Enhanced Permeability and Retention (EPR) effect. Solid tumors often develop abnormal, leaky vasculature with poor lymphatic drainage, allowing nanocarriers (typically 10-200 nm) to extravasate and accumulate selectively in tumor tissue while sparing healthy cells [11]. This passive targeting is complemented by active strategies where nanocarriers are functionalized with ligands (e.g., antibodies, peptides) that bind receptors overexpressed on target cells [11]. Temporally controlling drug release through mechanisms such as diffusion, degradation, or stimuli-responsiveness is equally critical to maintaining drug concentrations within the therapeutic window and maximizing clinical outcomes [11].
Frequently Asked Questions (FAQs)
Q1: What are some prominent examples of approved nanomedicines and their clinical indications?
Several nanomedicine formulations have become standard of care in various therapeutic areas, especially oncology. The most common carrier systems in approved drugs are liposomes and protein-based nanoparticles [97] [100].
Table 2: Clinically Approved Nanomedicines and Their Applications
| Product Name | Nanoparticle Type | Active Ingredient | Primary Clinical Indication |
|---|---|---|---|
| Doxil/Caelyx | Liposomal | Doxorubicin | Ovarian Cancer, Kaposi's Sarcoma, Multiple Myeloma |
| Abraxane | Protein-based (Albumin) | Paclitaxel | Breast Cancer, Lung Cancer, Pancreatic Cancer |
| Vyxeos | Liposomal | Daunorubicin & Cytarabine | Acute Myeloid Leukemia (AML) |
| Onivyde | Liposomal | Irinotecan | Pancreatic Cancer |
| Onpattro | Lipid Nanoparticle (LNP) | siRNA (transthyretin) | Hereditary Transthyretin-Mediated Amyloidosis |
| Feraheme | Iron Oxide Nanoparticle | Iron | Iron Deficiency Anemia |
| Comirnaty (Pfizer) | Lipid Nanoparticle (LNP) | mRNA | COVID-19 Prevention |
Q2: What are the primary mechanisms controlling drug release from nanocarriers?
Controlled drug release is vital for maintaining therapeutic drug levels and minimizing toxic side effects. The release kinetics from nanocarriers are governed by several core mechanisms [11]:
- Diffusion-Controlled Release: Drug molecules diffuse through a polymer membrane (reservoir system) or a polymer matrix (matrix system) driven by a concentration gradient. Matrix systems often show a high initial "burst release" [11].
- Solvent-Controlled Release: This includes osmosis-controlled release (where water influx through a semi-permeable membrane creates pressure to release the drug) and swelling-controlled release (where water uptake causes the polymer matrix to swell, increasing mesh size and enabling drug diffusion) [11].
- Degradation-Controlled Release: The drug is released as the biodegradable polymer backbone (e.g., polyesters, polyamides) undergoes hydrolysis or enzymatic cleavage. The release rate is directly tied to the degradation rate of the polymer [11].
- Stimuli-Responsive Release: The drug is released in response to specific internal (e.g., pH, enzymes, redox potential) or external (e.g., heat, light, magnetic field) triggers designed to match the pathological environment [11].
Q3: A promising actively targeted nanomedicine failed in our clinical trial despite strong preclinical data. What are common translational challenges?
The disconnect between preclinical success and clinical failure is a significant hurdle. For actively targeted nanomedicines, a major historical challenge has been the lack of validated biomarkers for patient stratification [100]. Unlike with antibody-drug conjugates, biomarkers to identify patients whose tumors overexpress the targeted receptor are not routinely used in nanomedicine trials. Furthermore, scale-up and manufacturing inconsistencies can alter a nanomedicine's critical quality attributes (size, charge, drug loading), leading to a product that differs from the one tested in preclinical models [100]. It is crucial to ensure that the preclinical evidence of safety and efficacy is generated at doses and regimens that match the intended clinical use and that the formulation is compatible with large-scale Good Manufacturing Practice (GMP) production [100].
Troubleshooting Common Experimental Issues
Problem: Poor Tumor Accumulation of Nanocarrier
Potential Cause 1: Rapid Clearance by the Reticuloendothelial System (RES)
- Solution: Modify the nanocarrier surface with hydrophilic polymers like Polyethylene Glycol (PEG) in a process known as PEGylation. This creates a steric barrier that reduces opsonization (protein binding) and recognition by immune cells, leading to a longer circulation half-life and greater opportunity for tumor accumulation via the EPR effect [11].
Potential Cause 2: Incorrect Nanocarrier Size
- Solution: Optimize the particle size. Nanocarriers smaller than 10 nm are rapidly cleared by renal filtration, while very large particles may be sequestered by the spleen or liver. For systemic delivery targeting the EPR effect, a size range of 10-100 nm is generally optimal. Use techniques like dynamic light scattering (DLS) for rigorous size characterization [11].
Problem: Inconsistent or Poorly Controlled Drug Release Kinetics
Potential Cause 1: Inadequate Understanding of Release Mechanism
- Solution: Systematically investigate the primary release mechanism (diffusion, degradation, etc.) in physiologically relevant media (e.g., PBS at pH 7.4 and 5.5). Use mathematical models (e.g., Zero-order, Higuchi, Korsmeyer-Peppas) to analyze in vitro release data and determine the dominant mechanism. This informs rational design changes [11].
Potential Cause 2: Unaccounted For "Burst Release"
- Solution: A large initial burst release is often caused by drug molecules adsorbed on or very near the particle surface. To mitigate this, implement more effective purification steps (e.g., dialysis, gel permeation chromatography) after drug loading to remove unencapsulated drug. Alternatively, consider formulating as a reservoir-type system (core-shell) rather than a matrix system [11].
Problem: Low Drug Loading Capacity
Potential Cause: Weak Drug-Carrier Interaction
- Solution: Employ drug-polymer conjugates (e.g., polymer-drug conjugates are a distinct category of nanomedicine comprising 10% of those in development) [97]. Alternatively, use prodrug strategies where the active pharmaceutical ingredient is modified to be more compatible with the carrier material, or select a carrier matrix with higher affinity for the drug molecule (e.g., using lipid carriers for hydrophobic drugs) [98].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Nanocarrier Development and Testing
| Reagent/Material | Function/Purpose | Key Considerations |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer for constructing matrix-type nanocarriers. | Erosion rate and drug release kinetics can be tuned by adjusting the LA:GA ratio. |
| DSPC/Cholesterol Lipids | Primary components for forming stable liposomal bilayers. | Cholesterol incorporation enhances membrane rigidity and reduces premature drug leakage. |
| mPEG-DSPE Lipid | A PEGylated lipid used for "stealth" functionalization of liposomes or lipid nanoparticles. | The PEG chain length and density critically impact circulation time and RES avoidance. |
| Dialysis Tubing (MWCO) | Used for purifying nanocarriers and for conducting in vitro drug release studies. | The Molecular Weight Cut-Off (MWCO) must be selected to retain the nanocarrier while allowing free drug diffusion. |
| Cell Lines (e.g., HeLa, MCF-7) | In vitro models for assessing nanocarrier cytotoxicity and cellular uptake. | Use relevant models that express the target receptors if testing active targeting. |
| Animal Models (e.g., murine xenografts) | In vivo models for evaluating biodistribution, efficacy, and safety. | Patient-derived xenografts (PDX) may better predict clinical response than standard cell-line-derived models [100]. |
Experimental Protocols for Critical Assays
Protocol: Establishing a RobustIn VitroDrug Release Profile
This protocol is essential for evaluating the controlled release performance of nanocarriers.
- Sample Preparation: Place a known quantity of drug-loaded nanocarriers (e.g., equivalent to 1 mg of drug) into a pre-soaked dialysis tube (select appropriate MWCO).
- Incubation Setup: Immerse the dialysis tube in a release medium (e.g., PBS, with or without surfactants, at pH 7.4). Maintain the system at 37°C under constant, gentle agitation to simulate physiological conditions and avoid stagnant layers.
- Sampling and Analysis: At predetermined time intervals (e.g., 0.5, 1, 2, 4, 8, 24, 48, 72 hours...), withdraw a fixed volume of the external release medium. Replace with an equal volume of fresh, pre-warmed medium to maintain sink conditions.
- Quantification: Analyze the drug concentration in the sampled medium using a validated method (e.g., HPLC, UV-Vis spectroscopy). Plot the cumulative percentage of drug released over time to generate the release profile.
- Modeling: Fit the release data to various mathematical models (e.g., Korsmeyer-Peppas, Higuchi) to elucidate the underlying release mechanism [11].
Protocol: Evaluating Targeting EfficacyIn Vitro
This protocol compares the cellular uptake of targeted versus non-targeted nanocarriers.
- Cell Seeding: Seed relevant cells (e.g., cancer cells expressing a specific receptor) in multi-well plates and culture until ~80% confluent.
- Nanocarrier Treatment: Treat cells with targeted nanocarriers, non-targeted nanocarriers, and free drug controls. Use a fluorescence label (e.g., Cy5, FITC) incorporated into the nanocarrier for detection. Incubate for a set period (e.g., 1-4 hours) at 37°C.
- Inhibition Assay (Optional): Pre-incubate a cell group with an excess of free targeting ligand (e.g., the antibody or peptide) for 30-60 minutes before adding the targeted nanocarriers. This blocks the receptors and serves as a control to confirm receptor-mediated uptake.
- Washing and Analysis: After incubation, wash cells thoroughly with PBS to remove non-internalized nanocarriers.
- Quantification: Analyze using flow cytometry to quantify mean fluorescence intensity (MFI) per cell, or use confocal microscopy to visually confirm internalization and subcellular localization.
Workflow and Pathway Visualizations
Diagram 1: Nanomedicine Translation Path
Diagram 2: Drug Release Mechanisms
The development of methods for controlled drug release is a central pillar of modern therapeutics, aiming to maintain drug concentrations within the therapeutic window, reduce dosing frequency, and minimize side effects [11]. Nanocarriers—submicron-sized drug delivery vehicles—are at the forefront of this research, offering unparalleled control over drug pharmacokinetics and biodistribution [6]. Their small size (typically 1-1000 nm) and high surface-area-to-volume ratio enable enhanced drug solubility, protection of delicate cargoes, and improved tissue targeting [101] [11]. However, the very properties that grant them these advantages also introduce unique challenges in controlling drug release kinetics, as the short diffusion distances can lead to premature drug leakage [11] [20]. This technical support document provides a comparative analysis of major nanocarrier platforms, focusing on their application in controlled release studies, and offers practical troubleshooting guidance for researchers.
Platform Comparison: Structures, Mechanisms, and Characteristics
Nanocarriers for drug delivery can be broadly categorized into synthetic and biomimetic platforms. Their drug release mechanisms are primarily governed by diffusion, carrier erosion/degradation, or responses to specific environmental stimuli [11] [20].
Table 1: Comparison of Major Nanocarrier Platforms for Controlled Drug Release
| Nanocarrier Platform | Core Composition & Structure | Primary Drug Release Mechanism(s) | Key Advantages for Controlled Release | Inherent Limitations & Challenges |
|---|---|---|---|---|
| Liposomes | Phospholipid bilayers forming unilamellar or multilamellar vesicles [101]. | Diffusion through membranes; degradation [11]. | High encapsulation of hydrophilic/hydrophobic drugs; biocompatible [101]. | Premature drug leakage; low stability; batch-to-batch variability [6]. |
| Polymeric Nanoparticles | Biodegradable polymers (e.g., PLGA) forming solid matrix (nanospheres) or reservoir (nanocapsules) [11]. | Diffusion; polymer degradation/erosion [11] [20]. | Tunable degradation rate for predictable release; high encapsulation efficiency [11]. | Risk of burst release; acidic degradation products; complex fabrication [11] [20]. |
| Polymeric Micelles | Amphiphilic block copolymers with hydrophobic core and hydrophilic shell [101]. | Dissociation at critical dilution; diffusion [11]. | Excellent for poorly soluble drugs; small, stable size [101]. | Low stability in blood; potential for premature dissociation [11]. |
| Dendrimers | Highly branched, monodisperse synthetic polymers with defined architecture [6]. | Diffusion from internal cavities; surface group cleavage [20]. | Multivalent surface for functionalization; controllable size [6]. | Potential cytotoxicity at high doses; complex synthesis [6]. |
| Inorganic Nanoparticles | Gold, mesoporous silica, or other inorganic materials [101] [7]. | Diffusion from pores; stimuli-responsive release (e.g., light, heat) [101]. | Tunable porosity; unique stimuli-responsiveness (e.g., photothermal) [101] [7]. | Poor biodegradability; potential long-term toxicity [7]. |
| Biomimetic Nanocarriers | Cell-derived vesicles (e.g., exosomes) or cell membrane-coated nanoparticles [101] [102]. | Membrane fusion; diffusion; often combined with core release mechanisms [101]. | Innate biocompatibility and immune evasion; long circulation half-life [101] [102]. | Complex isolation and characterization; low drug loading capacity [101]. |
Table 2: Key Physicochemical Properties and Their Impact on Controlled Release Performance
| Property | Ideal Range for Controlled Release | Impact on Release Kinetics & Biodistribution | Standard Characterization Method(s) |
|---|---|---|---|
| Particle Size | 10-200 nm for systemic delivery [11] [20]. | Smaller particles: Faster release, potential renal clearance. Larger particles: Slower release, higher RES uptake [6]. | Dynamic Light Scattering (DLS), TEM, AFM [6]. |
| Polydispersity Index (PDI) | < 0.3 (monodisperse) [6]. | High PDI leads to unpredictable, non-uniform drug release profiles from a heterogeneous population [6]. | Dynamic Light Scattering (DLS) [6]. |
| Zeta Potential | > +30 mV or < -30 mV for high electrostatic stability [6]. | Prevents aggregation, ensuring consistent release. Near-neutral charge may improve cellular uptake but risks instability [6]. | Electrophoretic Light Scattering [6]. |
| Drug Loading Capacity | Typically 1-20% (w/w), higher is better [11]. | Higher loading can enable longer sustained release durations and reduce carrier material dose [11]. | HPLC, UV-Vis spectroscopy after separation [11]. |
The following diagram illustrates the primary mechanisms by which drugs are released from nanocarriers, which is fundamental to designing controlled release systems.
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Nanocarrier Development
| Reagent/Material | Function in Nanocarrier Development | Example Application in Controlled Release |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer backbone for matrix-type particles [11] [20]. | Forms nanoparticles with release kinetics tunable by molecular weight and lactide:glycolide ratio [11]. |
| DSPE-PEG | Phospholipid-PEG conjugate for surface functionalization [11]. | Used to PEGylate liposomes and polymeric NPs to reduce RES uptake and prolong circulation half-life [11] [20]. |
| Targeting Ligands (e.g., Folate, RGD peptide) | Molecules attached to nanocarrier surface for active targeting [7]. | Enhances nanocarrier accumulation in specific cells (e.g., folate for cancer cells), enabling localized release [7]. |
| Stimuli-Responsive Lipids/Polymers | Materials that change structure in response to triggers (pH, redox, enzymes) [11] [7]. | Used to create nanocarriers that release drugs specifically in the tumor microenvironment (low pH, high enzymes) [7]. |
| Stabilizing Agents (e.g., BSA, Poloxamers) | Excipients to prevent nanoparticle aggregation [103]. | Added to formulations to maintain colloidal stability during storage, preventing changes in release profile [103] [6]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Why does my nanocarrier formulation exhibit a high initial "burst release" followed by very slow release? A: A high burst release is typically caused by drug molecules adsorbed on or very near the surface of the nanocarrier that diffuse out almost immediately upon contact with the release medium [11] [20]. To mitigate this:
- Optimize the encapsulation process: Ensure the drug is properly encapsulated within the core rather than simply adsorbed on the surface.
- Use a reservoir system: Consider designing a nanocapsule with a polymeric membrane surrounding a drug core, which can provide a more constant, zero-order release profile by acting as a diffusion barrier [11].
- Apply a coating: A thin, rate-controlling polymer coating on the nanocarrier can slow the initial diffusion of surface-bound drug.
Q2: What are the main challenges in using nanocarriers for oral drug delivery, particularly for controlled release? A: Oral delivery presents multiple biological barriers that can disrupt controlled release [80]:
- Mucus Barrier: The intestinal mucus layer can trap and immobilize nanocarriers, preventing them from reaching the epithelial cells.
- Enzymatic Degradation: Harsh pH and digestive enzymes in the GI tract can degrade the nanocarrier itself, causing premature drug release.
- Cellular Uptake Hurdle: Efficient transport across the intestinal epithelium via transcytosis is often low for many nanocarrier types, limiting systemic bioavailability [80]. Strategies to overcome this include designing mucus-penetrating particles (e.g., via PEGylation) and using bioadhesive materials to prolong residence time.
Q3: My nanoparticle conjugates are aggregating during preparation or storage. How can I prevent this? A: Aggregation is often a result of insufficient surface charge or inadequate steric stabilization [103] [6].
- Check Zeta Potential: Ensure your nanocarriers have a sufficiently high zeta potential (typically > |±30| mV) for electrostatic stabilization. Adjust the pH of your suspension medium to optimize surface charge.
- Introduce Steric Stabilizers: Coat particles with steric stabilizers like polyethylene glycol (PEG) or use blocking agents like BSA to create a protective layer that prevents aggregation [103].
- Control Concentration: Avoid using excessively high nanoparticle concentrations. Follow recommended guidelines and use sonication to disperse aggregates before conjugation or use [103].
Experimental Workflow for Characterizing Release Kinetics
A robust characterization of drug release kinetics is non-negotiable for any thesis project on controlled release. The following diagram outlines a standard experimental workflow.
Detailed Protocol for In Vitro Drug Release Study:
Nanocarrier Synthesis & Characterization: Before the release study, fully characterize the batch. Determine particle size, PDI, and zeta potential using Dynamic Light Scattering (DLS). Measure the drug loading capacity and encapsulation efficiency, typically by isolating the nanocarriers from the free drug (via centrifugation or filtration) and analyzing the drug content in the pellet or supernatant using HPLC or UV-Vis spectroscopy [6].
Set Up Release Study: The most common method is the dialysis technique. Place a known volume of the drug-loaded nanocarrier suspension into a dialysis bag (with a molecular weight cut-off that retains the nanocarriers but allows free diffusion of the drug). Immerse the bag in a large volume of release medium (e.g., phosphate-buffered saline, PBS, at pH 7.4) under "sink conditions" (volume at least 5-10 times the volume required for drug saturation). Maintain the system at a constant temperature (e.g., 37°C) with continuous agitation [11].
Sample & Analyze: At predetermined time intervals, withdraw a specific volume of the external release medium for analysis and replace it with an equal volume of fresh, pre-warmed medium to maintain sink conditions. Analyze the drug concentration in the collected samples using a pre-validated analytical method (HPLC is preferred for its specificity) [11].
Model Release Data: Fit the cumulative drug release data versus time to various mathematical models to understand the release kinetics [11] [20]:
- Zero-order Model:
Mt/M∞ = k*t(Ideal for constant release). - Higuchi Model:
Mt/M∞ = k*√t(Describes drug release from a matrix system by Fickian diffusion). - Korsmeyer-Peppas Model:
Mt/M∞ = k*tⁿ(Used to identify the release mechanism; the exponent 'n' is indicative of the transport mechanism).
- Zero-order Model:
The selection of a nanocarrier platform is a critical determinant in the success of a controlled drug release strategy. There is no universally optimal platform; the choice must be dictated by the physicochemical properties of the drug, the desired release profile, the route of administration, and the specific pathological target. Future directions in the field point towards the development of "smart" nanocarriers with multi-stimuli responsiveness and increasingly sophisticated biomimetic designs that more effectively navigate biological barriers. While challenges in scalability, regulatory approval, and long-term toxicity remain, the continued refinement of these platforms holds the key to realizing the full potential of targeted, controlled-release nanomedicines.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary cause of the translational gap between animal studies and human trials? The translational gap stems from a combination of factors. A significant issue is the inherent lack of predictivity of many animal models due to species differences in genetics, metabolism, and immune response [104] [105]. Furthermore, challenges in study design and reporting, such as poor reproducibility and irrelevant endpoints in animal studies, contribute to unreliable data that fails to translate to humans [106]. Operational obstacles like inadequate infrastructure, financial constraints, and prolonged regulatory approvals also hinder successful translation [107].
FAQ 2: What proportion of therapies that succeed in animal studies eventually gain regulatory approval for human use? Recent large-scale analysis has quantified this transition. The table below summarizes the journey of therapeutic interventions from animal studies to human application [105]:
| Development Stage | Proportion of Therapies Advancing | Median Transition Time (Years) |
|---|---|---|
| From Animal Studies to Any Human Study | 50% | 5 |
| From Animal Studies to Randomized Controlled Trial (RCT) | 40% | 7 |
| From Animal Studies to Regulatory Approval | 5% | 10 |
FAQ 3: Are there new technologies that can reduce reliance on animal testing? Yes, momentum is building for human-centric models. Technologies such as perfused human organs (kept viable ex vivo), organs-on-chips, and 3D bioprinting provide human-specific data on drug efficacy and toxicity [104]. These approaches can capture human physiological responses and heterogeneity better than animal models. Regulatory bodies like the FDA have begun to phase out certain animal testing requirements in response to these advances [104].
FAQ 4: How can we improve the selection of animal models to enhance translatability? Frameworks have been developed to objectively evaluate animal models. The Framework to Identify Models of Disease (FIMD) is one such tool, providing a standardized, multi-domain assessment of how well a model replicates human disease [106]. It scores models across eight key domains, including Epidemiology, Symptomatology and Natural History, Genetics, Biochemistry, Aetiology, Histology, Pharmacology, and Endpoints, facilitating the selection of models with the highest potential for predictive success [106].
FAQ 5: What are the major challenges in developing targeted nanocarrier drug delivery systems? The primary challenge is complexity. A targeted nanocarrier is a multi-component system (scaffold, targeting ligand, active drug, and optional stealth components) that is difficult to design, characterize, and manufacture reproducibly at scale [108]. Furthermore, controlling the overall biodistribution remains a hurdle, as a significant portion of an administered nanocarrier dose typically accumulates in the liver and spleen rather than the specific target tissue [108].
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent Sizes and Morphologies in Nanoparticle Synthesis
- Problem: Nanoparticles produced via nanoprecipitation have high polydispersity (PDI), leading to inconsistent experimental results.
- Solution:
- Switch Mixing Method: Replace conventional batch mixing with Flash Nanoprecipitation (FNP) or Microfluidic Nanoprecipitation. These methods ensure rapid and homogeneous mixing, yielding narrower particle size distributions [109].
- Optimize Parameters: Carefully control the organic-to-aqueous phase ratio, polymer concentration, and flow rates in microfluidic systems. These parameters directly influence nucleation and growth kinetics [109].
- Characterize Rigorously: Always use a combination of Dynamic Light Scattering (DLS) for hydrodynamic size and Transmission Electron Microscopy (TEM) for direct visualization of morphology and confirmation of size [6].
Issue 2: Poor Drug Loading or Encapsulation Efficiency in Nanocarriers
- Problem: The amount of active drug encapsulated within the nanocarrier is low, reducing therapeutic potential.
- Solution:
- Match Drug and Polymer Hydrophobicity: For hydrophobic drugs, use hydrophobic polymers (e.g., PLGA, PCL) to improve encapsulation within the nanoparticle core [109].
- Adjust Solvent and Anti-Solvent Selection: The miscibility of the solvent (e.g., acetone, THF) and anti-solvent (water) is critical for inducing rapid supersaturation and efficient drug entrapment [109].
- Consider Drug-Polymer Interactions: Explore polymers that can form ionic or covalent bonds with the drug molecule to enhance loading capacity.
Issue 3: Lack of Correlation Between In-Vivo Animal Results and Human Outcomes
- Problem: A therapy shows promising efficacy and safety in an animal model but fails in human clinical trials.
- Solution:
- Formally Validate Your Animal Model: Use a tool like the FIMD to critically assess how well your animal model recapitulates key aspects of the human disease. Do not rely solely on historical use [106].
- Incorregate Human-Relevant Data Early: Supplement animal data with insights from human-derived systems, such as perfused human organs or patient-derived cells, to better predict human-specific responses [104].
- Ensure Study Rigor: Adhere to the ARRIVE and PREPARE guidelines to improve the internal validity of your animal studies through robust design elements like randomization, blinding, and power calculations [106].
Issue 4: Rapid 'Burst Release' of Drug from Nanocarrier In-Vitro
- Problem: A large fraction of the encapsulated drug is released almost immediately upon placement in release media, rather than in a controlled, sustained manner.
- Solution:
- Optimize Nanoprecipitation Process: Tuning the synthesis parameters can create a denser polymer matrix that acts as a more effective diffusion barrier [109].
- Modify Polymer Composition: Use blends of polymers or co-polymers with different degradation rates (e.g., PLA-PEG) to better control the diffusion and erosion-based release mechanisms [109].
- Adjust Cross-Linking Density: For cross-linked nanocarriers, increasing the cross-linking density can strengthen the network and reduce initial burst release.
Experimental Protocols for Key Characterization assays
Protocol 1: Determining Nanocarrier Size and Surface Charge
- Objective: To measure the hydrodynamic diameter, polydispersity index (PDI), and zeta potential of synthesized nanocarriers.
- Materials: Nanocarrier suspension, deionized water or appropriate buffer (e.g., 1mM KCl), Dynamic Light Scattering (DLS) / Zeta Potential Analyzer.
Method:
- Sample Preparation: Dilute the nanocarrier suspension appropriately with a clean, particle-free solvent (typically deionized water or a low-conductivity buffer) to avoid signal saturation from multiple scattering. A common starting dilution is 1:10 or 1:100 (v:v) [6].
- DLS Measurement:
- Transfer the diluted sample into a clean, disposable sizing cuvette.
- Place the cuvette in the instrument and set the temperature to 25°C (or physiologically relevant temperature).
- Run the measurement. The DLS software will calculate the hydrodynamic diameter (Z-average) and the Polydispersity Index (PDI), which indicates the breadth of the size distribution (values <0.2 are generally considered monodisperse) [6].
- Zeta Potential Measurement:
- Transfer the diluted sample into a dedicated zeta potential cell (e.g., a folded capillary cell).
- Insert the cell into the instrument.
- Set the parameters, including the dielectric constant, viscosity of the dispersant, and the Smoluchowski approximation.
- Run the measurement. The instrument uses Laser Doppler Velocimetry to determine the electrophoretic mobility, which is converted to the zeta potential value in millivolts (mV) [6].
Interpretation: A high absolute zeta potential value (typically > ±30 mV) suggests good physical stability due to electrostatic repulsion preventing aggregation. The size and PDI are critical for predicting biodistribution and cellular uptake.
Protocol 2: Framework to Identify Models of Disease (FIMD) Assessment
- Objective: To systematically evaluate and select an animal model of disease based on its translational relevance to the human condition.
- Materials: FIMD validation sheet, published literature on the candidate animal model and the human disease.
Method:
- Domain Identification: The FIMD framework is based on eight validation domains. For each domain, gather evidence from the literature to answer specific questions [106]:
- Epidemiology: Does the model simulate the disease in relevant sexes and age groups?
- Symptomatology & Natural History: Does it replicate key symptoms, comorbidities, and disease progression?
- Genetics: Are the orthologous genes and mutations involved in the human disease present and similarly expressed?
- Biochemistry: Are relevant pharmacodynamic biomarkers present and do they behave similarly?
- Aetiology: Is the method of disease induction similar to the human context (e.g., genetic, environmental)?
- Histology: Are the tissue and cellular-level pathological changes similar?
- Pharmacology: Does the model respond to known standard-of-care therapies?
- Endpoints: Are the endpoints measured in the model clinically relevant?
- Scoring and Visualization:
- For each domain, assign a score based on the strength of the evidence.
- Input the scores into a radar plot to create a visual profile of the model's strengths and weaknesses across all domains [106].
- Comparison: Use the radar plots and validation sheets to objectively compare different animal models (e.g., mouse vs. rat) and select the one with the highest overall translational potential for your specific research question.
- Domain Identification: The FIMD framework is based on eight validation domains. For each domain, gather evidence from the literature to answer specific questions [106]:
Interpretation: A model that scores highly across multiple domains, particularly those most critical for your disease of interest, is more likely to generate predictive and translatable data.
Research Reagent Solutions
The following table lists key materials and their functions in nanocarrier research for controlled drug release.
| Research Reagent | Primary Function in Nanocarrier Research |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable and FDA-approved polymer used as a matrix for nanoparticle formation, allowing for sustained drug release through controlled degradation [109]. |
| PEG (Polyethylene glycol) | A polymer used for "PEGylation" to create a stealth layer on nanocarriers, which reduces opsonization and clearance by the immune system, thereby extending circulation half-life [108] [6]. |
| DSPE-PEG (1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-PEG) | A phospholipid-PEG conjugate commonly used to functionalize liposomes and polymeric nanoparticles, providing a steric barrier and a terminal group for attaching targeting ligands [108]. |
| Chitosan | A natural polysaccharide polymer used to form cationic nanoparticles, which can promote mucoadhesion and enhance cellular uptake, particularly for oral or nasal drug delivery [109]. |
| Targeting Ligands (e.g., Antibodies, Peptides) | Molecules (e.g., folic acid, RGD peptide) attached to the nanocarrier surface to bind specifically to receptors overexpressed on target cells, enabling active targeting and improved therapeutic efficacy [108]. |
| Solvents (e.g., Acetone, THF) | Water-miscible organic solvents used in nanoprecipitation to dissolve polymers and drugs before mixing with an anti-solvent to induce nanoparticle formation [109]. |
Workflow and Relationship Visualizations
DOT Script for Translational Research Workflow
Title: Drug Development Pipeline
DOT Script for Nanoprecipitation Process
Title: Nanoparticle Formation Steps
DOT Script for FIMD Validation Domains
Title: FIMD's Eight Validation Domains
Regulatory Considerations for Nanocarrier-Based Drug Products
The integration of nanotechnology into drug development has introduced Nanotechnology-Enabled Health Products (NHPs), including nanocarrier-based drug products, which promise revolutionary advancements in medical treatments [110]. These products are designed to provide spatiotemporal control of drug release, thereby enhancing therapeutic efficacy and reducing systemic side effects [11] [20]. However, the unique physicochemical properties of nanocarriers—such as their small size (typically 1-100 nm), large surface area-to-volume ratio, and unique biological behaviors—present complex challenges for regulatory evaluation [110] [6]. The regulatory landscape for these products is multifaceted and varies across different geographical regions, requiring developers to navigate a complex framework of region-specific guidelines [110].
This technical support guide is framed within the broader context of a thesis on methods for controlled drug release in nanocarrier research. It aims to provide researchers, scientists, and drug development professionals with practical troubleshooting guidance and regulatory insights for the development and characterization of nanocarrier-based drug products. Understanding these regulatory considerations is crucial for facilitating the successful translation of nanocarrier research from the laboratory to clinical application.
Fundamental Regulatory Frameworks and Definitions
Globally, regulatory systems for health products are primarily divided into major regions including North America (NoA), Europe, the Middle East, and Africa (EMEA), and Asia-Pacific (APAC) [110]. Among these, the regulatory systems of the European Union (EU) and the United States (US) are particularly influential and often serve as benchmarks for international regulatory standards [110]. In the EU, the European Commission provides the foundational legal framework, while in the US, the Food and Drug Administration (FDA) is the primary enforcing body [110]. The FDA maintains active nanotechnology programs through its participation in the National Nanotechnology Initiative (NNI), focusing on building regulatory science knowledge for products containing nanomaterials [111].
In China, the National Medical Products Administration (NMPA) has also initiated specific regulations for nanomaterials in medical devices, publishing technical guidelines for the evaluation of safety and effectiveness [112]. These guidelines highlight the need for specialized risk assessment approaches, even for devices that may generate nanoparticles through wear and tear, not just those intentionally containing nanomaterials [112].
Regulatory Classification of Nanocarrier Products
A fundamental first step in regulatory navigation is understanding how nanocarrier-based products are classified:
- Medicinal Products: Regulated under Directive 2001/83/EC in the EU, these products achieve their principal intended action through pharmacological, immunological, or metabolic (PIM) mechanisms [110].
- Medical Devices: These products function predominantly through physical or mechanical means, with any PIM action being secondary to their primary mechanism of action [110].
- In Vitro Diagnostic Medical Devices (IVDs): While presenting different technical challenges, some jurisdictions like China's NMPA have issued guidelines that may be relevant when considering the effectiveness of IVD products applying nanomaterials [112].
Table 1: Key Global Regulatory Bodies for Nanocarrier-Based Products
| Region | Regulatory Body | Key Guidelines/Legislation | Focus Areas |
|---|---|---|---|
| United States | Food and Drug Administration (FDA) | National Nanotechnology Initiative programs [111] | Product-specific, science-based approach for safety & efficacy |
| European Union | European Commission | Directive 2001/83/EC [110] | Regulatory framework for medicinal products |
| China | National Medical Products Administration (NMPA) | Technical Guidelines for Evaluation of Safety and Effectiveness of Nanomaterials [112] | Risk assessment of free nanoparticles, biological evaluation |
| Global | Various | Region-specific adaptations | Safety, efficacy, quality of medicinal products & devices |
Technical Requirements and Characterization Methods
Essential Physicochemical Characterization
Regulatory approval of nanocarrier-based products requires comprehensive characterization of their physicochemical properties, which significantly influence their biological behavior, including bioavailability, stability, cellular uptake, and biodistribution [6]. The following parameters are critical for regulatory submissions:
- Particle Size and Distribution: Particle size, shape, and polydispersity index (PDI) affect biodistribution, elimination, circulation half-life, cellular uptake, and endocytosis [6]. Regulatory guidelines typically require multiple complementary techniques for robust size characterization.
- Surface Charge: Zeta (ζ) potential indicates possible electrostatic interactions between nanocarriers, affects their aggregation tendencies, and helps select proper coating materials [6].
- Morphology: The shape of nanocarriers (spherical, disc, cylindrical, etc.) has a profound effect on biological processes including half-life, targeting efficiency, and toxicity [6].
Table 2: Essential Characterization Techniques for Nanocarrier-Based Products
| Parameter | Characterization Technique | Regulatory Significance | Common Issues & Troubleshooting |
|---|---|---|---|
| Particle Size & PDI | Dynamic Light Scattering (DLS) | Determines biodistribution & clearance; particles <10 nm face rapid renal clearance [11] | Sensitive to impurities; unreliable for polydisperse samples; overcome by fractionation (AF4) [6] |
| Surface Charge | Electrophoretic Light Scattering (Zeta Potential) | Predicts electrostatic interactions & aggregation tendencies [6] | Highly sensitive to ionic strength & pH; requires sample dilution [6] |
| Morphology | Atomic Force Microscopy (AFM), SEM, TEM | Shape affects half-life, targeting efficiency & toxicity [6] | AFM requires expertise; sample preparation may alter integrity [6] |
| Drug Release Kinetics | In vitro release studies using various models | Must maintain drug concentration within therapeutic window [11] [20] | Nanocarriers face unique challenges due to large surface area & short diffusion distance [11] |
Diagram 1: Comprehensive characterization workflow for regulatory evaluation of nanocarriers. This integrated approach addresses both physicochemical and biological properties required for regulatory submissions.
Controlled Drug Release Mechanisms and Kinetics
A fundamental aspect of nanocarrier-based products is their ability to control drug release kinetics, which is essential for maintaining drug levels within the therapeutic window—between the minimum effective concentration (MEC) and minimum toxic concentration (MTC) [11] [20]. Understanding and characterizing these release mechanisms is critical for both product development and regulatory approval.
The primary mechanisms controlling drug release from nanocarriers include:
Diffusion-Controlled Release: In capsule-type reservoir systems, the drug diffuses through a polymeric membrane driven by concentration differences [11]. Matrix-type nanospheres, where drug molecules are dispersed throughout the polymer matrix, also show diffusion-controlled release but typically with higher initial release (burst effect) [11].
Solvent-Controlled Release: This includes osmosis-controlled release (where water flows into the drug-loaded core through a semi-permeable membrane) and swelling-controlled release (where water uptake by glassy hydrophilic polymers causes swelling and drug release) [11].
Degradation-Controlled Release: Drug carriers comprising biodegradable polymers such as polyesters, polyamides, and polysaccharides release drugs via degradation of the polymer matrix [11].
Regulatory assessments typically require mathematical modeling of release kinetics using models such as zero-order, first-order, Higuchi, Hixson-Crowell, and Korsmeyer-Peppas models to understand and predict release behavior [11] [20].
Troubleshooting Guides and FAQs
Common Experimental Challenges and Solutions
FAQ: Why does my nanocarrier formulation show premature drug leakage and rapid release?
Answer: This is a common challenge in nanocarrier development due to the large surface area-to-volume ratio and short diffusion distances at the nanoscale [11]. Several factors can contribute to this issue:
- Insufficient barrier properties: The carrier membrane or matrix may not provide adequate diffusion resistance.
- Improper drug-carrier interactions: Weak interactions between the drug and carrier material can lead to rapid release.
- Inadequate stabilization: Lack of proper surface modification can result in instability in biological fluids.
Troubleshooting Guide:
- Modify carrier composition: Increase the density of the polymer matrix or membrane to enhance diffusion barriers.
- Implement core-shell structures: Create reservoir systems where the drug core is surrounded by a rate-controlling polymeric membrane [11].
- Optimize surface modification: Use PEGylation to improve stability and prevent premature release during circulation [11] [20].
- Incorporate stimuli-responsive materials: Utilize materials that release drugs only in response to specific triggers (pH, enzymes, temperature) at the target site [38].
FAQ: How can I prevent nanoparticle aggregation during conjugation and storage?
Answer: Aggregation reduces binding efficiency and affects diagnostic test accuracy, often occurring when nanoparticle concentration is too high [113].
Troubleshooting Guide:
- Optimize concentration: Follow recommended concentration guidelines and use sonication to disperse nanoparticles evenly before conjugation [113].
- Control pH environment: Maintain optimal pH (typically 7-8 for antibody conjugations with gold nanoparticles) using appropriate conjugation buffers [113].
- Use stabilizers: Incorporate stabilizing agents such as BSA or PEG to enhance shelf life and prevent aggregation [113].
- Modify surface charge: Adjust zeta potential through surface chemistry to enhance electrostatic repulsion between particles [6].
FAQ: What are the key considerations for achieving targeted drug delivery to specific tissues or cells?
Answer: Targeted delivery requires overcoming multiple biological barriers and achieving sufficient accumulation at the target site. Current data shows that only about 0.7% of systemically administered nanocarriers successfully accumulate near tumors, with most being taken up by normal tissues [38].
Troubleshooting Guide:
- Optimize size and surface properties: Use particles typically between 10-100 nm with PEGylation to enhance circulation time and reduce RES uptake [11] [20].
- Leverage the EPR effect: Design nanocarriers to exploit the Enhanced Permeability and Retention effect in tumors through appropriate size and surface characteristics [11] [20].
- Implement active targeting: Functionalize nanocarrier surfaces with ligands (antibodies, peptides) that bind to receptors overexpressed in target tissues [11] [38].
- Consider subcellular targeting: For targets within specific organelles (e.g., nucleus), incorporate nuclear localization signals or other targeting moieties [38].
Diagram 2: Drug release mechanisms in nanocarriers and their regulatory implications. Understanding these mechanisms is essential for designing products with controlled release profiles that meet regulatory standards.
Regulatory and Safety Assessment Challenges
FAQ: What are the key safety considerations for nanocarrier-based products from a regulatory perspective?
Answer: Regulatory agencies focus on several unique safety aspects of nanocarriers:
- Potential for free nanoparticle release: Evaluation of the possibility, dosage, duration, and route of exposure of free nanoparticles released from the product [112].
- Biological persistence and distribution: Assessment of particle distribution, persistence in tissues, and potential for bioaccumulation [112].
- Novel toxicological profiles: Comprehensive toxicological evaluation considering the unique properties of nanomaterials, which may differ from bulk counterparts [112] [6].
- Manufacturing consistency: Ensuring batch-to-batch consistency in physicochemical properties that influence safety and efficacy [6].
Troubleshooting Guide:
- Conduct thorough characterization: Implement robust physicochemical characterization protocols as outlined in Table 2.
- Perform specialized toxicity studies: Include studies specifically designed to assess nanomaterial-specific toxicities.
- Evaluate immunogenicity: Assess potential immune responses, especially for surface-modified nanocarriers (e.g., PEGylated systems that may induce anti-PEG antibodies) [38].
- Implement risk control measures: Develop post-market monitoring plans to collect real-world data on benefits and risks [112].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Nanocarrier Development
| Reagent/Material | Function | Regulatory Considerations | Troubleshooting Tips |
|---|---|---|---|
| Polyethylene Glycol (PEG) | Surface modification to enhance circulation time & reduce RES uptake [11] [20] | Potential immunogenicity with repeated dosing; anti-PEG antibodies [38] | Use alternative polymers if immunogenicity observed; optimize PEG chain length & density |
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable polymer for controlled release nanocarriers [38] | Degradation products must be non-toxic; batch consistency critical [6] | Control molecular weight & lactide:glycolide ratio to modulate release kinetics |
| Phospholipids & Cholesterol | Components for liposomal formulations [38] | Quality & sourcing important for reproducibility; stability concerns [6] | Use high-purity grades; include antioxidants if oxidation prone; optimize lipid ratios |
| Cationic Polymers (e.g., CS, PEI) | Gene delivery & complexation with genetic material [38] | Charge-associated toxicity; rigorous safety profiling required [6] | Balance charge density for efficacy vs. toxicity; consider biodegradable cationic polymers |
| Nuclear Localization Signals (NLS) | Peptide sequences for nuclear targeting [38] | Novel targeting approaches require comprehensive safety assessment | Ensure proper conjugation & functionality; validate intracellular trafficking |
| Blocking Agents (BSA, PEG) | Prevent non-specific binding in diagnostic applications [113] | Must not interfere with specific binding or assay performance | Optimize concentration & incubation time; validate after blocking |
The development of nanocarrier-based drug products requires careful integration of scientific innovation with regulatory considerations from the earliest stages of research and development. Success in navigating the complex regulatory landscape depends on:
- Proactive regulatory planning: Engaging with regulatory agencies early and often, understanding region-specific requirements, and anticipating evolving guidelines.
- Comprehensive characterization: Implementing robust, orthogonal methods to fully characterize physicochemical properties and their relationship to biological behavior.
- Strategic product design: Designing nanocarriers with both therapeutic efficacy and regulatory approval in mind, considering factors such as controlled release profiles, targeting efficiency, and safety.
- Thorough safety assessment: Conducting specialized evaluations that address the unique properties of nanomaterials, beyond standard regulatory requirements.
As the field of nanomedicine continues to evolve, regulatory science is steadily advancing to keep pace with innovation. By maintaining a science-based, quality-driven approach to development and leveraging available resources and guidelines, researchers can successfully translate nanocarrier-based products from the laboratory to clinical application, ultimately realizing their potential to improve patient care through advanced drug delivery technologies.
Troubleshooting Guides and FAQs
Nanocarrier Synthesis and Formulation
Q1: My pH-responsive nanocarriers are exhibiting poor drug loading efficiency. What could be the cause and how can I improve it?
- Potential Cause: A mismatch between the hydrophilicity/lipophilicity of the drug and the core environment of the nanocarrier.
- Troubleshooting Steps:
- Analyze Drug Properties: Determine the Biopharmaceutical Classification System (BCS) class of your active pharmaceutical ingredient (API). Low solubility (Class II/IV) drugs require different formulation strategies than high solubility drugs [114].
- Match Material to Drug: For hydrophobic drugs, use lipid-based cores (e.g., nanostructured lipid carriers, solid lipid nanoparticles). For hydrophilic drugs, polymeric nanoparticles with aqueous cores or water-in-oil-in-water double emulsions may be more suitable [4] [114].
- Optimize Synthesis Parameters: Adjust parameters like the aqueous-to-organic phase ratio, surfactant concentration, and energy input (e.g., sonication time) during emulsion formation.
- Experimental Protocol for Optimization:
- Prepare a series of formulations with varying concentrations of the lipid/polymer and surfactant.
- Use a standard method (e.g., dialysis, ultracentrifugation) to separate unencapsulated drug.
- Quantify the drug content in the nanocarrier pellet and the supernatant using HPLC or UV-Vis spectroscopy.
- Calculate Drug Loading (DL) and Encapsulation Efficiency (EE) using the formulas:
DL (%) = (Weight of drug in nanocarrier / Total weight of nanocarrier) × 100EE (%) = (Weight of drug in nanocarrier / Total weight of drug used) × 100
Q2: How can I confirm that my nanocarriers are truly pH-responsive and will release their payload in the tumor microenvironment?
- Potential Cause: The pH-sensitive bond (e.g., acetal, hydrazone) or protonable group (e.g., tertiary amine) may not be functioning as intended, or the release kinetics may be too slow.
- Troubleshooting Steps:
- Validate Responsiveness In Vitro: Conduct a drug release study under simulated physiological conditions.
- Check Material Selection: Ensure the polymer/lipid with pH-sensitive properties (e.g., poly(β-amino ester)) is correctly synthesized and incorporated [4].
- Experimental Protocol for In Vitro Release:
- Use a dialysis method. Place a known volume of nanocarrier dispersion in a dialysis bag (appropriate MWCO).
- Immerse the bag in a release medium (e.g., Phosphate Buffered Saline) at two different pH values: pH 7.4 (simulating blood) and pH 6.5-6.8 (simulating the tumor microenvironment).
- Maintain the system at 37°C with constant agitation.
- At predetermined time intervals, withdraw samples from the external release medium and replace with fresh medium to maintain sink conditions.
- Analyze the drug concentration in the samples to plot a cumulative release profile over time. A significant increase in release rate at the lower pH confirms responsiveness.
AI and Computational Design
Q3: The AI model I am training for virtual screening of nanocarrier materials is performing poorly. What are the key data requirements to improve it?
- Potential Cause: The dataset used for training is likely too small, non-diverse, or lacks high-quality, experimental validation.
- Troubleshooting Steps:
- Data Curation: Use large, publicly available chemical databases (e.g., PubChem, ChemBank, DrugBank) to build a diverse set of molecular structures and properties [115].
- Feature Selection: Ensure the input data includes relevant molecular descriptors (e.g., SMILES strings, 3D atom coordinates, logP, electron density) that influence the desired nanocarrier property (e.g., drug loading, stability, cellular uptake) [115].
- Model Selection: For complex structure-property relationships, move beyond traditional QSAR models to Deep Learning (DL) models like Deep Neural Networks (DNNs) or Convolutional Neural Networks (CNNs), which have shown superior predictivity for ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties [115].
- Experimental Protocol for AI-Driven Material Discovery:
- Objective: To identify a polymer for a pH-responsive nanocarrier with high drug loading and rapid release at pH 6.5.
- Data Collection: Compile a dataset of polymer structures and their experimentally measured properties (e.g., pKa, degradation rate, drug loading capacity) from literature and internal experiments.
- Model Training: Train a DL model (e.g., a Multilayer Perceptron network) to predict the two target properties based on the polymer's molecular features.
- Virtual Screening: Use the trained model to screen a vast virtual library of polymers and select the top 10 candidates for synthesis and experimental validation [116] [115].
Q4: How can I use AI to design a patient-specific nanomedicine dosing regimen?
- Potential Cause: A one-size-fits-all dosing approach does not account for inter-patient variability in genetics, physiology, and tumor biology.
- Troubleshooting Steps:
- Data Integration: Employ AI platforms that can fuse diverse patient data, including clinical parameters, genetic information (genomics, proteomics), and real-world data from clinical trials [116].
- Biomarker Discovery: Use AI-driven deep learning models to analyze complex datasets and discover hidden biomarkers that predict how a patient will respond to a specific nanocarrier formulation [117].
- Predictive Modeling: Develop models that correlate patient-specific factors with nanocarrier pharmacokinetics and pharmacodynamics to optimize drug dosage and release profiles for individual patients [116] [118].
- Workflow Overview: The diagram below illustrates the integrated workflow for developing AI-driven personalized nanomedicine.
Characterization and Quality Assurance
Q5: My nanoparticle batch is showing high polydispersity (PDI). How can I achieve a more uniform size distribution?
- Potential Cause: Unoptimized synthesis conditions leading to uncontrolled nucleation and growth or aggregation of particles.
- Troubleshooting Steps:
- Purification: Use techniques like dialysis, ultrafiltration, or size exclusion chromatography to remove aggregates and unincorporated materials.
- Process Control: Standardize the injection rate of the organic phase into the aqueous phase (or vice versa) during nanoprecipitation. Ensure consistent and adequate energy input during homogenization or sonication.
- Stabilizer Optimization: Increase the concentration of surfactants or stabilizers (e.g., polysorbates, poloxamers) to prevent particle aggregation and coalescence.
- Experimental Protocol for Dynamic Light Scattering (DLS) Measurement:
- Dilute the nanocarrier suspension appropriately in a filtered buffer to avoid scattering artifacts.
- Equilibrate the sample in the DLS instrument at 25°C for 2 minutes.
- Perform a minimum of 3-12 measurements per sample.
- Report the Z-average diameter and the Polydispersity Index (PDI). A PDI value below 0.2 is generally considered acceptable for monodisperse systems [119] [120].
Q6: What are the critical quality attributes (CQAs) for nanomedicine that regulatory agencies focus on?
- Answer: Regulatory agencies like the FDA and EMA emphasize a thorough characterization of nanomedicines due to their unique properties. Key CQAs are summarized in the table below [119] [120] [121].
Table 1: Critical Quality Attributes (CQAs) for Nanomedicine Regulatory Evaluation
| Attribute Category | Specific Parameter | Importance and Rationale |
|---|---|---|
| Particle Properties | Size & Size Distribution (PDI) | Influences biodistribution, targeting via EPR effect, and stability [119]. |
| Surface Charge (Zeta Potential) | Predicts colloidal stability and interaction with biological membranes [119]. | |
| Morphology (Shape) | Affects cellular uptake and blood circulation time [119]. | |
| Structural & Chemical Properties | Drug Loading & Encapsulation Efficiency | Directly impacts efficacy and dosage [114]. |
| Chemical Composition & Purity | Ensures consistency and identifies impurities [120]. | |
| Surface Chemistry & Functionalization | Critical for active targeting and stealth properties [4]. | |
| Performance Attributes | In Vitro Drug Release Profile | Demonstrates controlled and targeted release kinetics [4]. |
| Sterility and Apyrogenicity | Essential for patient safety, especially for injectables. | |
| Stability (Shelflife) | Ensures product quality and performance over time [120]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Nanocarrier Research and Their Functions
| Reagent/Material | Function in Research |
|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable and FDA-approved polymer used to form the core matrix of nanoparticles for sustained drug release [4]. |
| pH-Sensitive Lipids (e.g., DOPE) | Phospholipids that undergo phase transition in acidic environments, facilitating endosomal escape and payload release in pH-responsive systems [4]. |
| Poly(β-amino ester) (PBAE) | A synthetic polymer with tertiary amine groups that protonate in mild acidic pH, causing swelling or disruption for triggered drug release [4]. |
| Poloxamers (e.g., Pluronic F-68) | Non-ionic surfactants used to stabilize nanoemulsions and nanoparticles during formulation and prevent opsonization in vivo [119]. |
| Polyethylene Glycol (PEG) | A polymer conjugated to the surface of nanocarriers ("PEGylation") to impart stealth properties, reduce immune clearance, and prolong circulation time [4] [119]. |
| Targeting Ligands (e.g., Folic Acid, Peptides) | Molecules attached to the nanocarrier surface for active targeting of receptors overexpressed on specific cancer cells [4] [114]. |
| Cremophor EL | A solubilizing agent for highly lipophilic drugs like paclitaxel; however, its use is associated with toxicity, driving the need for alternative nanocarrier systems [114]. |
Conclusion
The field of controlled drug release from nanocarriers has matured significantly, offering sophisticated mechanisms and material systems for precise temporal and spatial delivery. Foundational principles of release kinetics provide the basis for designing advanced stimuli-responsive and targeted nanocarriers. While methodological innovations continue to enhance therapeutic applications, overcoming biological barriers and manufacturing challenges remains critical for clinical translation. The comparative analysis of existing platforms highlights a clear translational bottleneck, underscoring the need for intensified focus on biocompatibility, scalable production, and rigorous clinical validation. Future progress will likely hinge on the development of personalized nanomedicines, intelligent feedback-controlled systems, and interdisciplinary collaboration to fully realize the potential of nanocarriers in improving patient outcomes across a spectrum of diseases.
References
- 1. What Is Controlled Release? How it Works and Common ... [https://www.colorcon.com/education-insights/what-is-controlled-release]
- 2. How Are Controlled-Release Products Administered? [https://vicihealthsciences.com/controlled-release-explained/]
- 3. Controlled Drug Delivery Systems: Current Status and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8512302/]
- 4. Breaking barriers with pH-responsive nanocarriers: a new ... [https://pubmed.ncbi.nlm.nih.gov/40633600/]
- 5. Drug Release Kinetics - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/drug-release-kinetics]
- 6. Nanocarrier Drug Delivery Systems: Characterization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9026217/]
- 7. Recent insights and applications of nanocarriers-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825000344]
- 8. Mathematical Modeling of Release Kinetics from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6471682/]
- 9. Modeling and validation of drug release kinetics using ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2024.1395359/full]
- 10. Controlled Release Society (CRS) [https://www.controlledreleasesociety.org/]
- 11. from Pharmaceutical Nanocarriers - PMC Controlled Drug Release [https://pmc.ncbi.nlm.nih.gov/articles/PMC4322773/]
- 12. Diffusion-Controlled Drug Delivery System - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/diffusion-controlled-drug-delivery-system]
- 13. finals, feb 29, 2012 | PPTX Diffusion [https://www.slideshare.net/slideshow/diffusion-finals-feb-29-2012/11885105]
- 14. Top 10 Troubleshooting Guide Tableting [https://www.biogrund.com/top-10-troubleshooting-guide-tableting/?lang=en]
- 15. Achieving Zero-Order Release Kinetics Using Multi-Step Diffusion-Based Drug Delivery | Pharmaceutical Technology [https://www.pharmtech.com/view/achieving-zero-order-release-kinetics-using-multi-step-diffusion-based-drug-delivery]
- 16. Utilizing Korsmeyer-Peppas model to study drug release ... [https://www.sciencedirect.com/science/article/abs/pii/S0928098719302908]
- 17. Comparative statistical analysis of the release kinetics models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8912140/]
- 18. Understanding the Korsmeyer-Peppas model for drug ... [https://www.linkedin.com/posts/nicholas-peppas-422328144_korsmeyer-peppas-activity-7364115001936146432-Jj0n]
- 19. Drug Release Kinetics and Transport Mechanisms of Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2846103/]
- 20. Controlled drug release from pharmaceutical nanocarriers [https://www.sciencedirect.com/science/article/abs/pii/S0009250914004710]
- 21. Reliable release testing for nanoparticles with the NanoDis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8593552/]
- 22. Nanocarriers - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/nanocarriers]
- 23. A Review on Polymer and Lipid-Based Nanocarriers and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671830/]
- 24. Engineering precision nanoparticles for drug delivery [https://www.nature.com/articles/s41573-020-0090-8]
- 25. Mechanisms of Photoactive Nanocarriers for Imaging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11849580/]
- 26. Experimental Methods for the Biological Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9959606/]
- 27. Biodegradable Polymers in Drug Delivery: A Detailed Review [https://www.asianjpr.com/HTML_Papers/Asian%20Journal%20of%20Pharmaceutical%20Research__PID__2025-15-2-10.html]
- 28. Challenges and opportunities in computational studies for ... [https://www.nature.com/articles/s44386-025-00024-3]
- 29. Advances in drug-loaded microspheres for targeted ... [https://www.sciencedirect.com/science/article/pii/S075333222500438X]
- 30. Drug Nanocarriers for Pharmaceutical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388938/]
- 31. Emerging lipid nanoparticle systems capable of efficient ... [https://pubmed.ncbi.nlm.nih.gov/40901740/]
- 32. Optimization of PLGA Nanoparticle Formulation via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471678/]
- 33. Recent advances in stimulus-assisted nanoprecipitation for ... [https://arxiv.org/html/2511.14627v1]
- 34. Recent advances in stimuli-responsive oral delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S096399692501470X]
- 35. Recent Advancements in Stimuli Responsive Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7914759/]
- 36. Stimuli-Responsive, Cell-Mediated Drug Delivery Systems [https://www.mdpi.com/1999-4923/17/8/1082]
- 37. Multi-epitope ligand-conjugated nanoparticles for tumor ... [https://pubmed.ncbi.nlm.nih.gov/40788329/]
- 38. Nanocarrier‐Based Systems for Targeted Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371215/]
- 39. Overcoming CMC Challenges In The Development Of ... [https://www.advancingrna.com/doc/overcoming-cmc-challenges-in-the-development-of-conjugated-lnp-platforms-for-in-vivo-car-t-therapy-0001]
- 40. The next frontier in antibody-drug conjugates - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366496/]
- 41. Manufacturing Challenges of Therapeutic Antibody–Drug ... [https://www.bioprocessintl.com/emerging-therapeutics-manufacturing/manufacturing-challenges-of-therapeutic-antibody-drug-conjugates]
- 42. Nano-drug delivery: Is the enhanced permeability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7397928/]
- 43. An Updated Review on EPR-Based Solid Tumor Targeting ... [https://www.mdpi.com/2072-6694/14/12/2868]
- 44. The EPR effect and beyond: Strategies to improve tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7359085/]
- 45. Strategies to improve the EPR effect: A mechanistic ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365922001699]
- 46. Recent Advances in Tumor Targeting via EPR Effect for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234032/]
- 47. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 48. Enhanced permeability and retention effect: A key facilitator ... [https://www.sciencedirect.com/science/article/abs/pii/S1572100022002010]
- 49. The Enhanced Permeability and Retention (EPR) Effect [https://pmc.ncbi.nlm.nih.gov/articles/PMC8402171/]
- 50. Biological Nanocarriers in Cancer Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191216/]
- 51. Nanocarrier-Based Delivery Systems for Natural ... [https://www.mdpi.com/1996-1944/18/21/4960]
- 52. Nano-drug delivery systems (NDDS) in metabolic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1419384/full]
- 53. Nanotechnology for Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433253/]
- 54. Nanotechnology applications in the regulation of metabolic ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525003066]
- 55. Drug Delivery Strategies for the Treatment of Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6663576/]
- 56. Analysis of multi-drug cancer nanomedicine [https://www.nature.com/articles/s41565-025-01932-1]
- 57. Controlled drug delivery vehicles for cancer treatment and ... [https://www.nature.com/articles/s41392-017-0004-3]
- 58. The role of mucosal barriers in disease progression and ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X2300323X]
- 59. Engineering the Mucus Barrier - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463277/]
- 60. Nanocarriers' entry into the cell: relevance to drug delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC11115599/]
- 61. Intestinal nanoparticle delivery and cellular response: a ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02930-6]
- 62. 血管内支架植入后的内皮损伤及其修复策略 [https://pmc.ncbi.nlm.nih.gov/articles/PMC9935108/]
- 63. Composite preparation of polypeptide C16 and angiogenin Ang ... [https://patents.google.com/patent/CN115737785A/en]
- 64. Intestinal mucus components and secretion mechanisms [https://www.nature.com/articles/s12276-023-00960-y]
- 65. Advances and future perspectives in epithelial drug delivery [https://www.sciencedirect.com/science/article/abs/pii/S0169409X22001831]
- 66. The benefits and risks of PEGylation in nanomedicine [https://www.nature.com/articles/s41565-025-01951-y]
- 67. The stealth effect from a medicinal chemist perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360436/]
- 68. Considering the immunogenicity of PEG - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413056/]
- 69. The mechanisms of anti-PEG immune response are ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365922008197]
- 70. Immune Response Mechanism of PEG [https://www.creative-diagnostics.com/immune-response-mechanism-of-peg.htm]
- 71. PEG alternatives for RNA therapeutics [https://www.nature.com/articles/s41563-025-02408-2]
- 72. A novel multifunctional nano-drug delivery system based ... [https://pubmed.ncbi.nlm.nih.gov/40528836/]
- 73. Biocompatibility of nanomaterials and their immunological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8357854/]
- 74. Precision Nanotoxicology in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC9697541/]
- 75. Nanotoxicological profiles of clinically approved nanoplatforms [https://bjbas.springeropen.com/articles/10.1186/s43088-023-00458-6]
- 76. Recent advances in the development of biocompatible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9420852/]
- 77. Redox-manipulating nanocarriers for anticancer drug delivery [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02859-w]
- 78. Navigating Neurotoxicity and Safety Assessment of ... [https://www.sciencedirect.com/science/article/pii/S1742706124005439]
- 79. Precise nanoscale fabrication technologies, the “last mile” ... [https://www.sciencedirect.com/science/article/pii/S2211383525001807]
- 80. The challenges of oral drug delivery via nanocarriers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6225504/]
- 81. How Manufacturers Are Rethinking Costs [https://www.bcg.com/publications/2025/how-manufacturers-are-rethinking-costs]
- 82. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 83. Entrapment efficiency methodology for lipid nanoparticles [https://www.sciencedirect.com/science/article/pii/S2352952025000209]
- 84. Maximizing the encapsulation efficiency and the bioavailability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4771436/]
- 85. A new evidence-based design-of-experiments approach ... [https://www.nature.com/articles/s41598-024-82496-3]
- 86. Frequently Asked Questions - Lipid Nanoparticles (LNPs) ... [https://diantpharma.com/?page_id=1308]
- 87. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 88. Delayed Drug Release - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/delayed-drug-release]
- 89. Controlled Drug Release - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/controlled-drug-release]
- 90. Physical and chemical stability of drug nanoparticles [https://www.sciencedirect.com/science/article/abs/pii/S0169409X11000172]
- 91. The Prediction of the In Vitro Release Curves for PLGA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030581/]
- 92. Machine learning integrated with in vitro experiments for ... [https://www.nature.com/articles/s41598-024-82728-6]
- 93. Development and In evaluation of liposomal fentanyl... Vivo [https://pubmed.ncbi.nlm.nih.gov/41087421/]
- 94. Smart on-demand drug release strategies for cancer ... [https://pubmed.ncbi.nlm.nih.gov/40294796/]
- 95. In Vitro Drug Release Testing: Overview, Development and ... [https://www.jove.com/science-education/v/17160/in-vitro-drug-release-testing-overview-development-and-validation]
- 96. for targeted drug delivery in the vascular system: focus... Nanocarriers [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02892-9]
- 97. Nanomedicine Statistics and Facts (2025) [https://media.market.us/nanomedicine-statistics/]
- 98. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 99. Nanomedicine Market Size, Share, Growth, Report 2025-33 [https://www.imarcgroup.com/nanomedicine-market]
- 100. Q&A Translational Cancer Nanomedicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441112/]
- 101. Innovative nanocarriers: Synthetic and biomimetic strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362117/]
- 102. Nanocarrier-Based Delivery Systems for Natural Compounds ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609899/]
- 103. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOor7tbrKK_JWpLiTRbRht4M8ptrDlgfmtbjDSVwSugezTHmd7EWr]
- 104. Beyond animal testing: How human data trials are ... [https://pharmaphorum.com/rd/beyond-animal-testing-how-human-data-trials-are-reshaping-drug-development]
- 105. Analysis of animal-to-human translation shows that only 5% of ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002667]
- 106. Levelling the Translational Gap for Animal to Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7401509/]
- 107. Challenges and opportunities of translating animal research ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02338-8]
- 108. Critical questions in development of targeted nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4817320/]
- 109. Recent Advances in Different Nanoprecipitation Methods ... [https://www.scientificarchives.com/article/recent-advances-in-different-nanoprecipitation-methods-for-efficient-drug-loading-and-controlled-release]
- 110. Regulatory pathways and guidelines for nanotechnology ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 111. Nanotechnology Programs at FDA [https://www.fda.gov/science-research/science-and-research-special-topics/nanotechnology-programs-fda]
- 112. NMPA Initiates Regulation of Nanomaterials in Medical ... [https://cisema.com/en/nmpa-initiates-regulation-of-nanomaterials-in-medical-devices/]
- 113. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOoqCe3L0TTcrSB1U0pkWRheQKXHWVHCbBu1QUw8QC3zb3l_EqAlp]
- 114. Nanocarrier drug delivery systems for gynecological ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006492]
- 115. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 116. Artificial intelligence for personalized nanomedicine [https://pubmed.ncbi.nlm.nih.gov/39645588/]
- 117. The Future of Personalized Care Through AI for Drug ... [https://riverjournalonline.com/around-town/health/the-future-of-personalized-care-through-ai-for-drug-discovery/258971/]
- 118. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 119. Nanomedicine: Principles, Properties, and Regulatory Issues [https://pmc.ncbi.nlm.nih.gov/articles/PMC6109690/]
- 120. Quality Assurance Considerations for Nanoparticles [https://stacks.cdc.gov/view/cdc/210878]
- 121. Quality Assurance and Regulatory Issues of Nanomedicine ... [https://www.cambridge.org/core/books/fundamentals-of-nanomedicine/quality-assurance-and-regulatory-issues-of-nanomedicine-for-the-pharmaceutical-industry/5261262A44572C3A8C76C1307DD44EE0]