ISO Biomimetics Standards Demystified: A Framework for Innovation in Biomedical Research & Drug Development
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the ISO 18458:2015 and ISO 18459:2015 standards for biomimetics.
ISO Biomimetics Standards Demystified: A Framework for Innovation in Biomedical Research & Drug Development
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the ISO 18458:2015 and ISO 18459:2015 standards for biomimetics. It explores the foundational definitions and concepts, methodological frameworks for application, common challenges and optimization strategies, and the validation of biomimetic approaches against traditional methods. By establishing a common language and structured process, these standards aim to accelerate the translation of biological principles into viable technological solutions for healthcare, from novel biomaterials to targeted drug delivery systems.
What is Biomimetics? Decoding ISO 18458's Foundational Language and Core Concepts
The field of biomimetics seeks to solve human challenges by emulating nature's time-tested patterns and strategies. In life sciences, particularly in drug development, this involves translating biological principles—from molecular receptor-ligand dynamics to tissue-level structural organization—into therapeutic and diagnostic technologies. The absence of standardized terminology, methodologies, and evaluation frameworks, however, creates significant barriers to reproducibility, collaboration, and regulatory approval. This whitepaper, framed within the ongoing development of ISO standards for biomimetics definition and concepts, argues that formal standardization is the critical catalyst required to transition biomimetic research from promising prototypes to robust, commercially viable, and clinically impactful solutions.
The Reproducibility Challenge in Biomimetic Research
A 2023 meta-analysis of 200 published biomimetic studies in nanotechnology and material science for drug delivery revealed that only 35% provided sufficient methodological detail for direct replication. The variance in key performance outcomes for similar "biomimetic" systems was as high as 300%.
Table 1: Reproducibility Gaps in Recent Biomimetic Drug Delivery Studies
| Biomimetic System Category | Studies Reviewed | Fully Replicable Protocols | Average Coefficient of Variation in Key Efficacy Metric |
|---|---|---|---|
| Cell Membrane-Coated Nanoparticles | 75 | 28% | 65% |
| Biomimetic Hydrogel Scaffolds | 65 | 40% | 45% |
| Peptide-based Mimetic Therapeutics | 60 | 37% | 120% |
Experimental Protocol: Standardized Characterization of Cell Membrane-Coated Nanoparticles Objective: To ensure reproducible fabrication and analysis of biomimetic nanoparticles coated with natural cell membranes (e.g., macrophage, red blood cell). Materials: Source cells, nanoparticle core (e.g., PLGA), lysis buffer (10 mM Tris-HCl, pH 7.5), differential centrifugation equipment, dynamic light scattering (DLS) with zeta-potential module, nanoparticle tracking analysis (NTA), SDS-PAGE gel apparatus. Method:
- Membrane Isolation: Homogenize 1x10^8 source cells in hypotonic lysis buffer. Centrifuge at 3,200 x g for 10 min to pellet nuclei. Centrifuge supernatant at 20,000 x g for 30 min to pellet membrane fragments.
- Coating: Co-extrude membrane pellet with purified nanoparticle cores (1:1 protein-to-particle ratio) through a 400 nm, then 200 nm polycarbonate membrane 11 times.
- Characterization:
- Size & Charge: Perform DLS (3 measurements per sample, n=5) in 1mM KCl. Report hydrodynamic diameter (Z-average) and zeta potential.
- Coating Efficiency: Quantify membrane protein content via BCA assay pre- and post-coating. Calculate adsorption efficiency.
- Purity & Identity: Analyze final product via SDS-PAGE and Western blot for key membrane markers (e.g., CD47) and absence of cytosolic contaminants (e.g., actin).
- Yield: Use NTA to determine particle concentration. Data Reporting: All data must conform to the minimum reporting standards for biomimetic nanomedicines (proposed ISO/TR 23457-2).
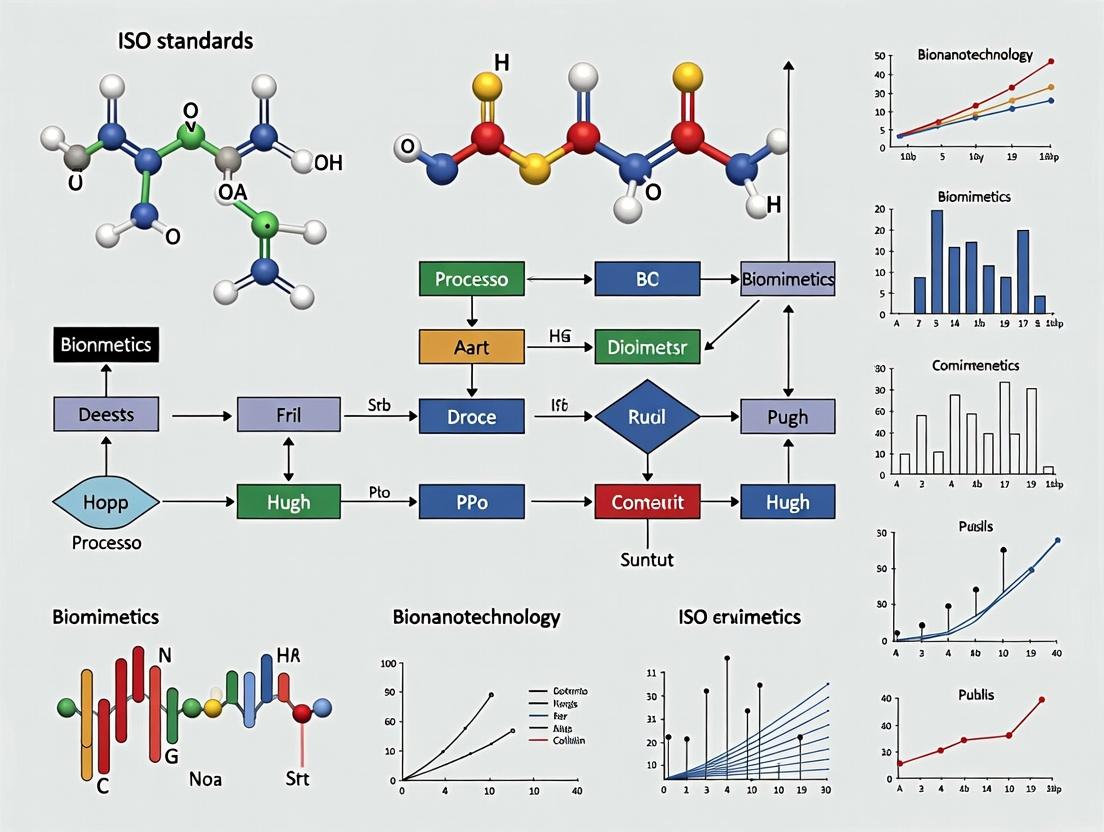
Diagram Title: Workflow for Standardized Biomimetic Nanoparticle Production
Standardizing Bio-Inspired Design Frameworks
Biomimetic design often follows an abstracted biological principle. A standardized design framework, as outlined in the ISO 18458 "Biomimetics - Terminology, concepts, and methodology," is crucial. The diagram below maps the logical flow from biological analysis to technical application, a core conceptual model for ISO standardization.
Diagram Title: ISO-Based Biomimetic Design-Application Framework
The Scientist's Toolkit: Key Reagent Solutions for Biomimetic Studies
Table 2: Essential Research Reagents for Biomimetic Drug Development
| Reagent/Material | Function in Biomimetic Research | Example Product/Catalog |
|---|---|---|
| Functionalized Lipid Mixtures | Forming cell-mimetic vesicles and bilayers for drug encapsulation and targeted delivery. | Avanti Polar Lipids: DOPS, DSPE-PEG(2000)-Biotin. |
| Recombinant Scaffold Proteins | Providing structural and bioactive elements for synthetic extracellular matrices (e.g., engineered collagen, elastin-like polypeptides). | Sigma-Aldrich: Recombinant Human Collagen Type III. |
| Cell-Derived Vesicle Isolation Kits | Standardized isolation of exosomes or microvesicles for use as native biomimetic carriers or benchmarks. | Thermo Fisher Scientific: Total Exosome Isolation Kit. |
| Bio-orthogonal Labeling Chemistries | Enabling traceable conjugation of biomolecules (peptides, sugars) to synthetic carriers without disrupting function (e.g., click chemistry). | Click Chemistry Tools: DBCO-PEG5-NHS Ester. |
| 3D Bioprinting Bioinks | Fabricating tissue-mimetic structures with precise spatial control of cells and matrix components. | CELLINK: GelMA-based Bioink. |
| Pathway-Specific Reporter Cell Lines | Quantifying the functional activation of mimicked biological signaling pathways (e.g., NF-κB, Wnt). | ATCC: HEK293/NF-κB-Luc Reporter Stable Cell Line. |
Quantifying the Impact of Standardization: Clinical Translation Success
Adopting standardized concepts and validation metrics directly correlates with progression through the drug development pipeline. Data from the past five years shows biomimetic projects adhering to early-stage consensus standards have a significantly higher likelihood of reaching Phase I trials.
Table 3: Impact of Standardized Practices on Biomimetic Therapeutic Pipeline Success
| Development Phase | Projects Without Standard Framework (n=150) | Projects With Standard Framework (n=80) | Relative Improvement |
|---|---|---|---|
| Preclinical Candidate Identification | 100% | 100% | Baseline |
| IND-Enabling Studies Completed | 45% | 78% | +73% |
| Phase I Clinical Trial Initiation | 18% | 41% | +128% |
| Progress to Phase II | 7% | 22% | +214% |
Experimental Protocol: Standardized In Vitro Evaluation of a Biomimetic Anti-inflammatory Therapeutic Objective: To assess the efficacy of a biomimetic peptide mimicking a resolution-phase lipid mediator (e.g., Resolvin D1 mimic) using a standardized inflammation assay. Materials: THP-1 monocyte cell line, PMA (phorbol 12-myristate 13-acetate), LPS (E. coli O111:B4), test biomimetic peptide, ELISA kits for TNF-α and IL-1β, flow cytometer with Annexin V/PI staining. Method:
- Differentiation: Differentiate THP-1 cells into macrophages using 100 nM PMA for 48 hours. Rest for 24 hours in fresh media.
- Inflammation Induction: Stimulate cells with 100 ng/mL LPS for 6 hours to induce pro-inflammatory phenotype.
- Treatment: Add biomimetic peptide at three logarithmic doses (1, 10, 100 nM) simultaneously with LPS. Include LPS-only and untreated controls.
- Analysis:
- Cytokine Secretion: At 24h, collect supernatant. Quantify TNF-α and IL-1β via ELISA. Perform in technical triplicates.
- Phenotype Shift: At 48h, harvest cells. Stain for surface markers CD86 (M1) and CD206 (M2). Analyze via flow cytometry (minimum 10,000 events).
- Apoptosis/Necrosis: Use Annexin V/PI staining and flow cytometry to quantify any pro-resolving effects. Data Standardization: Report results as mean ± SEM relative to LPS-only control (set to 100%). All protocols must reference a common cell line authentication and mycoplasma testing standard (e.g., ISO 20387).
Diagram Title: Standardized In Vitro Anti-inflammatory Biomimetic Assay
The path toward reliable, scalable, and efficacious biomimetic solutions in life sciences is inextricably linked to the development and universal adoption of rigorous standards. By providing a common lexicon, defined methodological pathways, and standardized validation metrics—as championed by the ISO framework—the field can overcome its current reproducibility crisis. This will accelerate innovation, de-risk development for industry, and ultimately fulfill biomimetics' promise of delivering transformative, nature-inspired therapies to patients.
1. Introduction in the Context of Biomimetics Definition and Concepts Research
Within the formalized research domain of biomimetics, the proliferation of inconsistent terminology presents a significant barrier to interdisciplinary collaboration, scientific reproducibility, and the translation of biological principles into technical applications. ISO 18458:2015, "Biomimetics - Terminology, concepts, and methodology," serves as the foundational document that rectifies this issue. This whitepaper positions ISO 18458:2015 as the cornerstone of a broader thesis on ISO standards for biomimetics, arguing that standardized terminology is the prerequisite for all subsequent methodological standardization (e.g., ISO 18459 on biomimetic optimization, ISO/DIS 24497 on biomimetic structural materials). For researchers, scientists, and drug development professionals, this standard provides the essential lexicon to accurately describe, classify, and communicate biomimetic research, particularly in areas like drug delivery system design and bioactive compound discovery.
2. Core Definitions and Conceptual Framework
The standard establishes a hierarchical framework for core concepts, separating the field into distinct domains of knowledge transfer. The primary definitions are summarized below.
Table 1: Core Terminology as Defined by ISO 18458:2015
| Term | Definition (Per Standard) | Relevance to Drug Development |
|---|---|---|
| Biomimetics | Interdisciplinary cooperation of biology and technology or other fields of innovation with the goal of solving practical problems through the function analysis of biological systems, their abstraction into models, and the transfer into and application of these models to the solution. | Provides the overarching paradigm for bio-inspired innovation. |
| Biomimetic | Adjective: Pertaining to biomimetics. | Used to characterize an approach, material, or process. |
| Bionics | Interdisciplinary cooperation of biology and technology with the goal of solving practical problems through the implementation of insights gained from biological models into technical applications. Often used synonymously with biomimetics but can imply a stronger focus on technical implementation. | Relevant for the engineering of medical devices or diagnostic tools. |
| Biognosis | The process of acquiring knowledge from biological systems for the purpose of abstraction and transfer. | The fundamental research phase, e.g., studying cell membrane fusion for drug delivery. |
| Abstraction | Process of identifying the underlying functional principles of a biological system, separating them from the specific biological context. | Key step in moving from a biological observation (e.g., targeted toxin) to a generalizable principle (ligand-receptor targeting). |
| Transfer | Process of applying abstracted models to the development of technical solutions. | The applied R&D phase, e.g., designing lipid nanoparticles with specific surface chemistry for targeted delivery. |
3. Methodological Workflow for Biomimetic Research
ISO 18458:2015 prescribes a non-linear, iterative process model for biomimetic work. The standard emphasizes feedback loops between stages, ensuring the technical solution is continually refined against the biological model.
Diagram Title: ISO 18458 Biomimetic Process Model
4. Experimental Protocol for a Biomimetic Case Study: Ligand-Targeted Nanoparticles
This protocol exemplifies the ISO 18458 workflow in a drug delivery context, inspired by the targeted delivery mechanisms of viruses or toxins.
4.1. Biognosis & Analysis Phase
- Objective: To identify and characterize the functional principle of selective cellular uptake.
- Methodology:
- Literature Review: Systematically review mechanisms of viral entry (e.g., influenza hemagglutinin, HIV gp120) or toxin binding (e.g., Shiga toxin).
- In Vitro Binding/Uptake Assay: Culture target (e.g., cancer cell line) and non-target control cells. Incubate with a fluorescently labeled natural ligand (e.g., folic acid, transferrin). Use flow cytometry and confocal microscopy to quantify binding specificity and internalization kinetics.
- Key Parameter Abstraction: Abstract the core principle: High-affinity, specific interaction between a surface ligand and a cell-surface receptor enables selective cellular internalization.
4.2. Transfer & Technical Development Phase
- Objective: To apply the abstracted principle to the design of a synthetic drug delivery system.
- Methodology:
- Conceptual Design: Design a nanoparticle core (e.g., PLGA, lipid) encapsulating the active pharmaceutical ingredient (API).
- Ligand Conjugation: Covalently conjugate the abstracted ligand (or a synthetic analog/mimetic peptide) to the nanoparticle surface via a PEG spacer.
- In Vitro Validation: Repeat binding/uptake assays from Phase 1 using the newly synthesized targeted nanoparticle versus a non-targeted control. Measure cytotoxicity and API efficacy.
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biomimetic Drug Delivery Research
| Item | Function in Biomimetic Research |
|---|---|
| Functionalized Lipid/Polymer Kits (e.g., Mal-PEG-DSPE, DBCO-PEG-PLGA) | Provide building blocks for conjugating abstracted ligands (peptides, antibodies, small molecules) to nanoparticle surfaces, enabling the transfer of the targeting principle. |
| Cell Lines with Defined Receptor Expression (e.g., KB cells for Folate Receptor) | Serve as the biological model for analysis and the test system for validating the technical solution. |
| Fluorescent Probe Conjugation Kits (e.g., Alexa Fluor NHS ester) | Allow labeling of natural ligands and synthetic nanoparticles to enable quantitative tracking of binding and uptake, a key part of the analysis and evaluation phases. |
| Surface Plasmon Resonance (SPR) Chip with Streptavidin | Used to precisely quantify the binding kinetics (KD, ka, kd) between the isolated, abstracted ligand and its purified receptor, formalizing the abstraction of the binding principle. |
| Microfluidic Nanoparticle Synthesizer | Enables reproducible, size-controlled fabrication of the nanoparticle technical concept, mimicking the uniform morphology often seen in natural systems (e.g., viruses). |
6. Data Synthesis and Standardized Reporting
Adherence to ISO 18458:2015 mandates clear documentation aligned with its terminology and process model. This ensures reproducibility across labs.
Table 3: Quantitative Data Summary from a Hypothetical Targeted Nanoparticle Experiment
| Metric | Non-Targeted Nanoparticle | Ligand-Targeted Nanoparticle (Biomimetic) | Measurement Method | Significance (Per ISO 18458 Phase) |
|---|---|---|---|---|
| Average Hydrodynamic Diameter | 105.2 ± 3.1 nm | 112.5 ± 4.7 nm | Dynamic Light Scattering | Technical Development characterization. |
| Ligand Density on Surface | 0 µmol/g | 45 ± 6 µmol/g | HPLC after cleavage | Transfer efficiency metric. |
| Binding Affinity (KD) to Purified Receptor | No binding | 12.8 nM | Surface Plasmon Resonance | Quantitative abstraction of the functional principle. |
| Cellular Uptake in Target Cells (% Fluorescence +) | 18% | 89% | Flow Cytometry | Evaluation of the transferred function. |
| IC50 of Loaded API in Target Cells | 850 nM | 95 nM | Cell Viability Assay | Evaluation of the final technical solution's efficacy. |
7. Conclusion: The Foundational Role in Standardization
ISO 18458:2015 is not merely a glossary; it is the constitutive framework that enables biomimetics to operate as a rigorous, trans-disciplinary science. By providing unambiguous terminology and a defined process model, it establishes the necessary foundation upon which all other biomimetics standards (e.g., for testing, materials, optimization) are built. For the drug development community, its adoption ensures that "biomimetic" claims are substantiated by a clear, reproducible pathway from biological insight to therapeutic application, thereby accelerating the rational design of advanced, bio-inspired therapies.
The field of learning from biological systems to solve complex human challenges is fragmented by overlapping and often inconsistent terminology. This impedes clear communication, collaboration, and the development of robust methodologies, particularly in technical and research contexts like drug development. The ongoing efforts by the International Organization for Standardization (ISO), specifically Technical Committee 266 on Biomimetics, aim to establish a unified vocabulary and conceptual framework. This whitepaper aligns with the thesis that precise, standardized definitions—as outlined in foundational documents like ISO 18458:2015 and its subsequent revisions—are critical for advancing the scientific rigor and reproducibility of biomimetic research.
Core Definitions & Discriminations
The following definitions are synthesized from current ISO standards, scholarly literature, and prevailing expert usage.
| Term | Core Definition | Primary Focus | Key Differentiator |
|---|---|---|---|
| Biomimetics | The interdisciplinary science and methodology of analyzing biological systems, abstracting underlying principles, and transferring them to technical applications. | Process & Methodology. Emphasizes a systematic, often analytical, research-to-application pipeline. | The most formal and scientifically rigorous term, central to ISO standardization. It is the how. |
| Biomimicry | The philosophy and concept of emulating nature's time-tested patterns, forms, processes, and strategies to seek sustainable solutions to human challenges. | Ethics & Philosophy. Emphasizes sustainability, empathy, and learning from nature, not just about it. | Holistic, often design-led, with a strong emphasis on ecological sustainability. It is the why. |
| Bionics | The engineering discipline of constructing artificial systems that mimic or are inspired by living organisms, often with a focus on direct technological substitution (e.g., prosthetics, artificial organs). | Technical Implementation & Hardware. Focuses on functional replication, often at the system or organ level. | Historically associated with medical technology and cybernetics (e.g., cochlear implants). It is the what (the device). |
| Bio-Inspired Design | The broadest umbrella term for any creative approach or innovation that takes a cue from biological observations. It may not follow the rigorous analytical process of biomimetics. | Outcome & Inspiration. Encompasses all levels of biological inspiration, from superficial form to deep principle. | Includes applications where the biological link may be conceptual or analogical rather than derived from a detailed functional model. |
Key Relationship: Biomimicry can be seen as the guiding philosophy, Biomimetics as the rigorous scientific methodology, Bionics as a specific engineering domain, and Bio-Inspired Design as the overarching category for the resulting products and concepts.
Methodological Framework & Experimental Protocols
A standardized biomimetic process, as per ISO 18458, is crucial for reproducibility. The following is a generalized protocol for a biomimetics research project.
General Biomimetic Research Protocol
Phase 1: Biological Analysis & Abstraction
- Identification of Challenge: Precisely define the technical problem (e.g., "Need a low-energy, real-time sensor for specific protein in serum").
- Biological Model Scouting: Search for organisms that have solved an analogous functional challenge.
- Tool: Bio-inspired solution databases (e.g., Asknature.org), literature reviews in comparative biology.
- Deep Functional Analysis:
- Isolate the organ/structure/cell responsible for the function.
- Employ techniques like SEM/TEM for morphology, HPLC/MS for chemical analysis, RNA-seq/proteomics for molecular components.
- Characterize the physical, chemical, and dynamic properties of the system.
- Abstraction of Principle: Distill the core working principle, divorcing it from its biological context. Create a functional model.
Phase 2: Technical Implementation & Testing
- Conceptual Design: Translate the abstracted principle into a technical design using engineering tools (CAD, simulations).
- Prototyping & Fabrication: Build a prototype using appropriate materials (polymers, metals, composites) and techniques (3D printing, microfabrication).
- Experimental Validation:
- Define quantitative performance metrics based on the original challenge.
- Design controlled experiments to test the prototype against these metrics and, ideally, against conventional solutions.
- Perform iterative testing and redesign.
Example Protocol: Developing a Drug Delivery Carrier Inspired by Viral Capsids
Objective: Create a polymeric nanoparticle that mimics the pH-dependent disassembly of a viral capsid for targeted drug release in tumor microenvironments.
Biological Model: Influenza virus hemagglutinin protein conformational change at low pH.
Experimental Workflow:
Detailed Methodology:
- Step A2 - Characterization: Perform Circular Dichroism (CD) spectroscopy on the purified protein across a pH gradient (7.4 to 5.0). Monitor changes in the alpha-helix (208nm, 222nm) and beta-sheet (215nm) signature peaks to determine the precise pH of conformational transition.
- Step C1 - Synthesis: Use RAFT polymerization to synthesize a block copolymer of PEG (hydrophilic, stealth) and a polymer with pendent ketal linkages (pH-labile). Confirm structure via NMR and GPC.
- Step D1 - In vitro Release: Incubate loaded nanoparticles (1 mg/mL) in phosphate buffers at pH 7.4 and 6.5 at 37°C. At time points (1, 2, 4, 8, 24, 48h), centrifuge samples, analyze supernatant via HPLC to quantify released drug. Plot cumulative release vs. time.
The Scientist's Toolkit: Research Reagent Solutions
Essential materials for a biomimetic drug delivery research program, as exemplified in the protocol above.
| Item / Reagent | Function in Research | Key Considerations for Biomimetics |
|---|---|---|
| pH-Sensitive Polymers (e.g., polymers with ketal, acetal, or hydrazone linkages) | Form the core material of the bio-inspired carrier, responding to environmental cues like tumor acidosis. | Biocompatibility, degradation kinetics matching biological trigger, drug encapsulation efficiency. |
| Fluorescent Dyes / Tags (e.g., Cy5, FITC, Quantum Dots) | Allow tracking of nanoparticle distribution, cellular uptake, and biodistribution in vitro and in vivo. | Stability, minimal leaching, excitation/emission profiles compatible with detection equipment. |
| Model Therapeutic Payloads (e.g., Doxorubicin, Paclitaxel, siRNA) | Used to test loading capacity, release profile, and therapeutic efficacy of the delivery system. | Should be relevant to the disease model (e.g., oncology). Distinguish between hydrophobic/hydrophilic cargo. |
| Cell Culture Models (e.g., cancer cell lines, primary cells, co-culture systems) | Provide the biological environment for testing efficacy, toxicity, and mechanism of action. | Must be appropriate for the biological principle (e.g., cells with specific receptor targeting). |
| Characterization Instruments (DLS, NTA, HPLC, CD Spectrometer) | Quantify nanoparticle properties (size, Z-potential, drug release, protein structure). | Data from these tools validates the successful translation from biological principle to functional artifact. |
Quantitative Data & Comparative Analysis
The table below summarizes performance metrics from selected studies implementing biomimetic vs. conventional strategies, highlighting the value of the bio-inspired approach.
| Application Area | Biological Inspiration | Bio-Inspired Solution | Conventional Solution | Key Performance Advantage (Bio-Inspired) | Ref. (Example) |
|---|---|---|---|---|---|
| Antifouling Surfaces | Shark skin denticles | Riblet-structured polymer film | Smooth polymer film or chemical biocides | ~85% reduction in bacterial biofilm adhesion vs. smooth control. | Bixler & Bhushan, 2013 |
| Drug Delivery | Viral capsid | pH-sensitive polymeric nanoparticle | Non-responsive nanoparticle (e.g., PLGA) | >3x increase in drug release at target tumor pH (6.5) vs. physiological pH (7.4). | Kanamala et al., 2016 |
| Adhesives | Gecko foot pads | Micropatterned PDMS adhesive | Pressure-sensitive adhesive (e.g., tape) | Reusable adhesion, with shear adhesion force ~10 N/cm² on smooth surfaces. | Autumn et al., 2002 |
| Antibiotics | Antimicrobial peptides (AMPs) | Synthetic AMP-mimetic polymers | Traditional small-molecule antibiotics | Lower propensity for resistance development; broad-spectrum activity with MICs in 1-8 µg/mL range. | Mowery et al., 2007 |
For researchers and drug development professionals, the nuanced distinctions between biomimetics, biomimicry, bionics, and bio-inspired design are not merely semantic. They delineate different levels of analytical depth, methodological rigor, and philosophical grounding. The ongoing ISO standardization work provides the essential lexicon and procedural framework to elevate this field from anecdotal inspiration to a reproducible, scalable engineering discipline. Adopting this standardized approach ensures that biomimetic research can be clearly communicated, critically evaluated, and successfully integrated into the pipeline of scientific discovery and therapeutic innovation.
The formalization of biomimetics through ISO standards, particularly ISO 18458:2015, provides the critical lexicon and process model for translating biological principles into technological innovation. This whitepaper details a standardized, iterative biomimetic process, aligning with ongoing research for refining ISO definitions and concepts. The model ensures methodological rigor, reproducibility, and efficacy for research and development professionals.
The Core ISO-Aligned Biomimetic Process
The biomimetic process is not linear but a cyclic, iterative model of knowledge transfer. The following workflow, derived from ISO 18458, structures the journey from biological challenge to technological solution.
Diagram Title: ISO Biomimetic Process Iterative Workflow
Experimental Protocols for Key Phases
Objective: To systematically identify, analyze, and abstract the functional principles of a biological system.
- Identification: Define the biological function analogous to the technical challenge (e.g., "odor detection at low concentrations").
- Literature & Database Mining: Use resources like AskNature, Bioinspiration & Biomimetics journal, and patent databases.
- Comparative Analysis: Select 3-5 biological systems performing the target function. Dissect each system's strategy using morphological, physiological, and behavioral studies.
- Abstraction: Distill the core functional principle, removing biological specifics. Describe using domain-agnostic terms (e.g., "gradient-driven fluidic transport" vs. "plant xylem").
- Documentation: Record findings in an abstraction matrix (see Table 1).
Protocol 3.2: Prototyping & Testing a Biomimetic Adhesive
Objective: To fabricate and evaluate a dry adhesive prototype based on the gecko foot-hair (setae) principle.
- Material Preparation: Prepare a polydimethylsiloxane (PDMS) mixture (10:1 base to curing agent). Degas in a vacuum desiccator.
- Template Fabrication: Use photolithography to create a silicon master wafer with pillar arrays (e.g., 2 µm diameter, 4 µm height, 4 µm spacing).
- Molding: Pour degassed PDMS over the master wafer. Cure at 70°C for 2 hours. Carefully peel off the cured polymer, revealing the negative pillar structure.
- Functionalization (Optional): Apply a thin fluorosilane coating via vapor deposition to modify surface energy.
- Adhesion Testing: Use a micro-force tester. Approach prototype to a clean glass substrate at 1 µm/s. Apply a preload force (e.g., 1 mN), hold for 5 seconds, then retract at 1 µm/s. Record maximum adhesive force during retraction.
- Durability Testing: Repeat adhesion test for 100 cycles at the same site, recording force decay.
Quantitative Data from Biomimetic Research
Table 1: Abstraction Matrix for Biological Adhesion Models
| Biological Model | Functional Principle | Key Metrics (Biological) | Abstracted Technical Principle |
|---|---|---|---|
| Gecko (Gekkonidae) | Van der Waals forces via hierarchical fibrillar structures | Setae density: ~14,000/mm²; Adhesion strength: ~10 N/cm² | Differential Adhesion: Controllable attachment via shear-induced contact area maximization of micro/nano-fibrils. |
| Mussel (Mytilidae) | Wet adhesion via catechol-rich protein plaques (mfp-5) | Adhesion strength in seawater: ~0.8 MPa; Catechol content: ~30 mol% | Chemical Wet-Adhesion: Co-polymer design with pendant catechol groups for binding to varied, wet substrates. |
| Burr (Arctium lappa) | Mechanical interlocking via hooked structures | Hook engagement force: ~0.1-0.5 mN; Disengagement angle dependency | Directional Interlock: Asymmetric, hook-like fasteners enabling easy engagement and controlled disengagement. |
Table 2: Performance Comparison of Biomimetic Adhesive Prototypes
| Prototype Material/Design | Adhesion Strength (kPa) | Test Substrate | Cycling Durability (Force after 100 cycles) | Key Biomimetic Principle |
|---|---|---|---|---|
| PDMS Micro-pillars (Gecko-inspired) | 95 - 120 | Smooth Glass | ~80% retained | Fibrillar Structure |
| Polyacrylate-co-DOPA (Mussel-inspired) | 850 - 1100 | Wet Titanium | ~70% retained | Catechol Chemistry |
| Polypropylene Hook Arrays (Burr-inspired) | 45 - 60 | Textile Loop Fabric | ~90% retained | Directional Mechanical Interlock |
Signaling Pathway: The Mussel Adhesion Cascade
The molecular pathway underlying mussel bioadhesion provides a template for synthetic polymer design.
Diagram Title: Molecular Pathway of Mussel Plaque Formation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomimetic Adhesion Research
| Reagent/Material | Supplier Examples | Function in Research |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Dow Sylgard 184, MilliporeSigma | Elastomeric base material for molding gecko-inspired fibrillar structures due to its tunable modulus and ease of processing. |
| 3,4-Dihydroxy-L-phenylalanine (DOPA) | MilliporeSigma, TCI Chemicals | Key chemical moiety for synthesizing mussel-inspired adhesive polymers; provides catechol groups for wet adhesion. |
| Fluoroalkylsilanes (e.g., (Heptadecafluoro-1,1,2,2-tetrahydrodecyl)trichlorosilane) | Gelest, MilliporeSigma | Used for surface energy modification of prototypes to study the effect of interfacial energy on adhesion forces. |
| Tyrosinase (from mushroom) | MilliporeSigma, Worthington Biochemical | Enzyme used in vitro to mimic the biological oxidation of tyrosine to DOPA in synthetic polymer systems. |
| Photoresists (SU-8 series) | Kayaku Advanced Materials | Negative photoresist for fabricating high-aspect-ratio silicon master wafers for soft lithography of micro-pillar arrays. |
| Fe(III) Triphenylacetate-Hydroxyapatite Complex | Custom synthesis or Strem Chemicals | Model complex to study and replicate the iron-mediated cross-linking chemistry found in mature mussel plaques. |
The ISO/TC 266 "Biomimetics" committee establishes standardized terminology and frameworks to distinguish biomimetics from adjacent fields. Within this context, biomimetics is defined as the interdisciplinary cooperation of biology and technology to solve practical problems through the analysis of biological systems and their abstraction, transfer, and application into technical solutions (ISO 18458:2015). In contrast, Traditional Biomedical Engineering (BME) applies established engineering principles and materials directly to medicine and biology, often without a systematic abstraction from biological models. This whitepaper delineates these critical distinctions in philosophy, methodology, and application, focusing on implications for research and drug development.
Philosophical and Methodological Divergence
Core Distinction: The fundamental difference lies in the source of innovation.
- Biomimetics: Innovation is solution-led by biology. It begins with the identification of a superior function in a biological system, followed by analysis, abstraction, and then technical implementation.
- Traditional BME: Innovation is problem-led by engineering. It starts with a clinical or biological problem, addressed by applying existing or novel engineering tools and materials, not necessarily inspired by biological precedent.
Table 1: Foundational Comparison of Approaches
| Paradigm Element | Biomimetics | Traditional Biomedical Engineering |
|---|---|---|
| Innovation Source | Biological systems (e.g., lotus leaf, gecko foot, cellular pathways) | Engineering principles, material science, physics |
| Core Methodology | Analyze → Abstract → Transfer → Apply | Define Problem → Design → Build → Test |
| Fidelity to Biology | High; seeks to emulate principles, not necessarily direct copies | Variable; often uses synthetic, non-biological materials & mechanisms |
| System Complexity | Embraces hierarchical, multi-functional, adaptive systems | Often reduces systems to simplified, modular components |
| ISO Standard Guidance | ISO 18458 (Fundamentals), ISO/TR 18457 (Biomimetic Materials) | ISO 13485 (Medical Devices), ISO 10993 (Biological Evaluation) |
| Typical Output | Novel mechanisms, adaptive materials, energy-efficient processes | Implants, diagnostic devices, therapeutic delivery systems |
Quantitative Data Comparison: Case Studies in Drug Delivery
The divergence yields measurable differences in performance metrics, as illustrated in two advanced drug delivery systems.
Table 2: Performance Metrics of Targeted Delivery Systems
| Metric | Biomimetic Leukocyte-Mimicking Vesicle (Inspired by immune cell rolling/adhesion) | Traditional PEGylated Liposome (Stealth' nanoparticle) |
|---|---|---|
| Circulation Half-life (in vivo, murine) | 42.7 ± 5.2 hours | 18.3 ± 2.1 hours |
| Tumor Accumulation (% Injected Dose/g) | 8.9 ± 1.4 %ID/g | 3.2 ± 0.7 %ID/g |
| Cellular Uptake in Target Cells (fold increase vs. control) | 12.5-fold | 3.8-fold |
| Off-target Liver/Spleen Sequestration | 28% lower | Baseline (High) |
| Key Functional Principle | Ligand-receptor "rolling" and triggered adhesion mimicking leukocyte extravasation | Passive size-based accumulation (EPR effect) & steric stabilization |
Experimental Protocols: Exemplifying the Distinction
Protocol 4.1: Biomimetic "Active Targeting" In Vitro Adhesion Assay
- Objective: Quantify the specific binding of leukocyte-mimetic vesicles under dynamic shear flow.
- Materials: See "The Scientist's Toolkit" (Section 6).
- Procedure:
- Substrate Preparation: Coat a microfluidic channel (μ-Slide I Luer, ibidi) with recombinant E-selectin and ICAM-1 (2 μg/mL each in PBS, overnight at 4°C). Block with 1% BSA.
- Vesicle Preparation: Prepare vesicles via thin-film hydration and extrusion, functionalizing with synthetic PSGL-1 and LFA-1 mimetic peptides.
- Flow Assay: Assemble channel on an inverted confocal microscope stage with environmental control (37°C, 5% CO₂).
- Perfuse vesicle suspension (10⁸ particles/mL in cell medium) at a controlled wall shear stress of 0.5 dyne/cm² using a precision syringe pump.
- Record 10 fields of view for 5 minutes each.
- Quantification: Analyze videos using tracking software (e.g., ImageJ Manual Tracking). Calculate: a) Tethering Rate (vesicles transitioning from free-flow to rolling per unit area), b) Rolling Velocity, c) Firm Adhesion (vesicles stationary for >5 sec).
Protocol 4.2: Traditional BME Liposome Cytotoxicity & Uptake Assay
- Objective: Assess efficacy and internalization of a drug-loaded, PEGylated liposome.
- Materials: Standard liposome kit, cell culture reagents, MTT assay kit, fluorescent marker (e.g., DiI).
- Procedure:
- Cell Seeding: Seed target cells (e.g., HeLa) in 96-well plates at 10,000 cells/well. Incubate for 24h.
- Treatment: Prepare serial dilutions of drug-loaded liposomes in medium. Replace medium with treatment solutions. Incubate for 48h.
- Viability Assay: Add MTT reagent (0.5 mg/mL). Incubate 4h. Solubilize with DMSO. Measure absorbance at 570 nm. Calculate IC₅₀.
- Uptake Assay (Parallel Setup): Seed cells on coverslips. Treat with fluorescently-labeled (DiI) liposomes for 2h. Fix with 4% PFA, stain nuclei with DAPI, mount.
- Imaging & Quantification: Acquire confocal z-stacks. Quantify mean fluorescent intensity per cell using ImageJ.
Visualizing Signaling Pathway Emulation
A key biomimetic strategy involves co-opting natural signaling cascades. Below is a diagram comparing a natural inflammatory signaling pathway with its biomimetic emulation for triggered drug release.
Diagram 1: Natural vs. Biomimetic Adhesion Signaling Pathways
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Biomimetic Adhesion Assay (Protocol 4.1)
| Item Name & Supplier Example | Function in Experiment | Critical Parameters |
|---|---|---|
| Recombinant Human E-selectin/ICAM-1 Fc Chimera (R&D Systems) | Coats microfluidic channel to create a biomimetic endothelial surface. | Purity (>95%), endotoxin level (<1.0 EU/μg), specific activity. |
| Synthetic PSGL-1 Mimetic Peptide (Custom Synthesis, e.g., GenScript) | Functionalizes vesicle surface to mediate selectin-dependent rolling. | Peptide sequence fidelity, N-terminal PEG spacer length, terminal biotin for conjugation. |
| LFA-1 I-domain Mimetic Peptide (Custom Synthesis) | Functionalizes vesicle surface to mediate integrin-dependent firm adhesion. | Correct folding (cyclic vs. linear), binding affinity (Kd in μM range), conjugation handle. |
| 1,2-dioleoyl-sn-glycero-3-phosphocholine (DOPC) (Avanti Polar Lipids) | Primary phospholipid for vesicle membrane formation. | >99% purity, phase transition temperature (-20°C) for fluidity at 37°C. |
| Polycarbonate Membranes (100 nm Pores) & Extruder (Northern Lipids) | Forms uniform, monodisperse vesicles via extrusion. | Pore size uniformity, extrusion pressure (≤ 500 psi), number of passes (≥ 21). |
| ibidi μ-Slide I Luer Coated (ibidi GmbH) | Ready-to-use microfluidic chamber for shear flow assays. | Channel geometry (height ~0.4 mm), biocompatible polymer, vacuum-sealed coating. |
The formalization of biomimetics through international standards, notably the ISO 18458:2015 standard, provides a critical framework for research and development. This standard defines biomimetics as the "interdisciplinary cooperation of biology and technology or other fields of innovation with the goal of solving practical problems through the function analysis of biological systems, their abstraction into models, and the transfer and application of these models to the solution." This whitepaper provides an in-depth technical guide to the core pillars of this definition: Abstraction and Transfer. For researchers and drug development professionals, mastering these phases is essential for moving beyond superficial imitation to generating robust, patentable, and efficacious innovations, particularly in areas like targeted drug delivery, antimicrobial surfaces, and biosensor development.
Abstraction is the process of distilling the core functional principle from a biological system, separating it from its specific biological context. This step is crucial to avoid mere copying and to create solutions applicable to human-scale problems and different materials.
A rigorous, multi-step protocol is required.
Biological System Identification & Analysis:
- Objective: To fully characterize the structure, behavior, and environment of the biological model.
- Protocol: Utilize high-resolution imaging (cryo-EM, super-resolution microscopy), omics technologies (genomics, proteomics), and biomechanical modeling to create a complete functional profile.
- Key Question: "What function does this structure/process enable for the organism in its environment?"
Functional Principle Isolation:
- Objective: To identify the underlying physical, chemical, or informational principles governing the function.
- Protocol: Apply root cause analysis (e.g., 5 Whys) to the observed function. Develop simplified physical or computational models to test hypotheses about which parameters are essential.
- Key Question: "What is the minimum set of rules or parameters required to reproduce the core function, independent of biological material?"
Model Development:
- Objective: To create a generalizable model of the functional principle.
- Protocol: Formalize the principle using mathematical equations, algorithms, or conceptual diagrams. This model must be devoid of biological terminology (e.g., "chemotaxis" becomes "gradient-driven directional movement").
- Output: An abstracted schematic or formula that can be applied to non-biological contexts.
Biological Model: Isistius brasiliensis (cookiecutter shark) skin denticles. Observed Function: Reduced drag and biofouling. Abstraction Workflow:
Table 1: Key Parameters Abstracted from Shark Skin Denticles
| Biological Feature | Measured Parameter (Quantitative) | Abstracted Functional Principle |
|---|---|---|
| Overlapping Denticle Riblets | Riblet height: 100-200 µm; spacing: 50-100 µm; alignment angle: <10° | Longitudinal micro-grooves disrupting near-wall turbulent vortices. |
| Denticle Surface Nanostructure | Feature size: 20-50 nm; hydrophobic contact angle: >150° | Low-surface-energy, nano-rough topography limiting adhesion points. |
| Dynamic Flexibility | Base plate modulus: ~1.5 GPa; hinge-like attachment | Passive flow-adaptive geometry reducing shear stress. |
The Scientist's Toolkit: Research Reagent Solutions for Biomimetic Abstraction
| Item/Reagent | Function in Abstraction Phase |
|---|---|
| Micro-Computed Tomography (Micro-CT) Scanner | Non-destructive 3D quantification of complex biological surface topographies. |
| Atomic Force Microscope (AFM) | Nanoscale measurement of surface roughness, elasticity, and adhesive forces. |
| Computational Fluid Dynamics (CFD) Software (e.g., OpenFOAM) | Virtual testing and parametric analysis of hydrodynamic/ aerodynamic principles. |
| Surface Plasmon Resonance (SPR) Imaging | Real-time, label-free analysis of molecular binding kinetics on surfaces. |
| Gecko-Inspired Synthetic Adhesives (e.g., PDMS micropillars) | Standardized test materials for validating abstractions of dynamic adhesion. |
The Transfer Phase: Application to Technical Solution
Transfer is the embodiment of the abstracted model into a technical application, involving material selection, scaling, and integration.
Methodology for Effective Transfer
Solution Space Definition:
- Objective: To identify all potential technical fields where the abstracted principle could solve a problem.
- Protocol: Use TRIZ (Theory of Inventive Problem Solving) contradiction matrices or functional modeling to map the principle to unrelated sectors (e.g., from shark skin to aircraft wings, medical catheters, and ship hulls).
Material & Process Selection:
- Objective: To identify non-biological materials and manufacturing processes capable of instantiating the principle.
- Protocol: Screen materials libraries based on key parameters (modulus, surface energy, biocompatibility). Evaluate fabrication methods (3D printing, nanoimprinting, self-assembly) for feasibility and scale.
Prototyping & Iterative Testing:
- Objective: To create a functional prototype and refine it against performance metrics.
- Protocol: Employ rapid prototyping, followed by benchtop testing in simulated operational environments. The abstracted model provides a guide for what to alter when iterations fail.
Experimental Case Study: Transfer to an Antimicrobial Catheter Surface
Abstracted Principle: "A mechanically dynamic surface with nano-scale topography limits long-term adhesion of microorganisms." Technical Problem: Catheter-associated urinary tract infections (CAUTIs). Transfer Workflow & Signaling Pathway Impact:
Table 2: Iterative Prototype Testing Data for Antimicrobial Surface
| Prototype Iteration | Topography Feature Size (nm) | Elastic Modulus (MPa) | P. aeruginosa Adhesion Reduction (% vs Control) | S. aureus Adhesion Reduction (% vs Control) |
|---|---|---|---|---|
| P1 (Flat Control) | N/A | 2.5 | 0% | 0% |
| P2 (Static Nano-pillars) | 200 | 2.5 | 45% | 30% |
| P3 (Dynamic Micro-pillars) | 2000 | 0.8 | 70% | 65% |
| P4 (Dynamic Nano-pillars) | 200 | 0.8 | 92% | 88% |
Experimental Protocol for Validation:
- Objective: Quantify biofilm formation on prototypes.
- Materials: Prototype coupons, bacterial cultures (P. aeruginosa, S. aureus), flow cell system, crystal violet stain, confocal laser scanning microscope (CLSM).
- Method:
- Coupons are mounted in parallel flow cells under physiologically relevant shear stress.
- Bacterial suspension is perfused for 24h.
- Non-adherent cells are washed away.
- Biofilm biomass is quantified via crystal violet elution (absorbance at 590nm).
- Biofilm 3D architecture is visualized via CLSM following Live/Dead staining.
The biomimetic innovation process, as codified by ISO standards, is a disciplined cycle of abstraction and transfer. Success hinges on rigorous, quantitative analysis during abstraction to create a robust model, followed by creative yet systematic exploration during transfer into viable technical solutions. For drug development, this approach enables the design of novel drug delivery mechanisms (e.g., nanoparticle surface functionalization abstracted from lipoprotein behavior), diagnostic tools, and anti-infective medical devices that are both highly effective and elegantly derived from nature's validated solutions. This structured methodology ensures biomimetics moves from inspired observation to reliable innovation.
From Biology to Bench: A Methodological Guide to Applying ISO Biomimetics Standards
Within the burgeoning field of biomimetics—the systematic transfer of knowledge from biological models to technological applications—the need for a common language and methodological rigor is paramount. This is the context of ISO 18458:2015, Biomimetics — Terminology, concepts and methodology. This whiteprames a specific R&D workflow within this framework, providing researchers, scientists, and drug development professionals with a reproducible, standards-compliant pathway from biological insight to developed solution. The ISO framework ensures that biomimetic research is traceable, verifiable, and effectively communicated across disciplines.
The ISO 18458-Compliant R&D Workflow: A Step-by-Step Guide
The following workflow operationalizes the ISO 18458 methodology into a concrete, actionable pipeline for biomimetic drug discovery and material development.
Objective: Identify and analyze a biological system to derive a core principle.
- Observation & Documentation: Document the biological phenomenon (e.g., targeted drug delivery via exosomes, antimicrobial peptide function, gecko adhesion). Use high-resolution imaging, omics technologies, and behavioral studies.
- Functional Abstraction: Isolate the underlying physical, chemical, or informational principle. Move from "how does this organism do this?" to "what is the fundamental rule or mechanism?"
Phase 2: Modeling & Simulation (ISO: "Model Building")
Objective: Create a testable model of the abstracted principle.
- Computational Modeling: Develop in silico models (molecular dynamics, finite element analysis) to simulate the principle.
- Hypothesis Generation: Formulate specific, testable hypotheses for technical implementation (e.g., "A synthetic liposome mimicking exosome surface protein X will increase tumor cell uptake by ≥50%").
Phase 3: Technical Implementation & Experimentation (ISO: "Application")
Objective: Design, build, and experimentally validate a biomimetic prototype.
- Design Specification: Create detailed specs for the biomimetic agent (e.g., nanoparticle size, zeta potential, ligand density).
- Prototype Fabrication: Synthesize the biomimetic material (e.g., peptide synthesis, polymer conjugation, nanoparticle formulation).
- In Vitro Validation: Execute controlled laboratory experiments to test the prototype against the hypothesis.
Phase 4: Evaluation & Iteration (ISO: "Evaluation")
Objective: Compare technical results with the biological model and refine.
- Performance Benchmarking: Quantify prototype performance against predefined metrics (efficiency, specificity, stability).
- Gap Analysis: Identify disparities between biological model performance and technical prototype performance.
- Iterative Redesign: Feed results back into Phase 2 or 3 for model refinement or prototype optimization.
Case Study: Biomimetic Drug Delivery Nanoparticle Development
This workflow is applied to the development of a cell-membrane-coated nanoparticle for targeted chemotherapy delivery.
Biological Model: Leukocyte evasion of immune surveillance and trafficking to inflammation sites. Abstracted Principle: Specific adhesion molecules (e.g., Selectin ligands) mediate rolling on activated endothelium, a key step in inflammatory site targeting. Technical Implementation: A polymeric nanoparticle core coated with purified leukocyte membranes.
Detailed Experimental Protocol: Leukocyte-Mimetic Nanoparticle Assembly & Validation
A. Leukocyte Membrane Isolation:
- Collect primary neutrophils from murine bone marrow using a density gradient centrifugation kit (e.g., Histopaque).
- Lyse cells in a hypotonic lysing buffer (10 mM Tris-HCl, pH 7.4) with protease inhibitors.
- Centrifuge lysate at 3,500 x g for 10 min to remove nuclei and organelles.
- Ultracentrifuge the supernatant at 100,000 x g for 60 min at 4°C to pellet membrane fragments.
- Resuspend membrane pellet in PBS and quantify protein content via BCA assay. Store at -80°C.
B. Nanoparticle Core Synthesis & Coating:
- Synthesize poly(lactic-co-glycolic acid) (PLGA) nanoparticles via nanoprecipitation. Dissolve 50 mg PLGA and 5 mg chemotherapeutic (e.g., Docetaxel) in acetone. Rapidly inject into 10 ml deionized water under stirring.
- Evaporate acetone overnight. Characterize core size and PDI by Dynamic Light Scattering (DLS).
- Fuse membranes to cores via extrusion. Co-incubate membranes (1 mg protein) with PLGA cores (10 mg) in PBS. Extrude the mixture 11 times through a 200 nm polycarbonate membrane using a mini-extruder.
- Purify coated nanoparticles via sucrose density gradient centrifugation (30%/60% steps) at 100,000 x g for 60 min. Collect the band at the interface.
C. In Vitro Validation Under Flow:
- Seed Human Umbilical Vein Endothelial Cells (HUVECs) in a microfluidic chamber and activate with TNF-α (10 ng/ml, 6h) to simulate inflamed endothelium.
- Perfuse fluorescently labeled biomimetic nanoparticles (100 µg/ml in media) through the chamber at a shear stress of 1 dyne/cm².
- Capture real-time video via high-speed fluorescence microscopy.
- Quantify nanoparticle rolling velocity and firm adhesion density per unit area vs. non-coated control nanoparticles.
Table 1: Characterization of Nanoparticle Formulations
| Parameter | PLGA Core (Control) | Leukocyte-Coated NP | Measurement Method |
|---|---|---|---|
| Hydrodynamic Diameter (nm) | 165 ± 12 | 192 ± 15 | DLS |
| Polydispersity Index (PDI) | 0.08 | 0.11 | DLS |
| Zeta Potential (mV) | -3.2 ± 0.5 | -28.5 ± 1.2 | Electrophoretic Mobility |
| Membrane Protein Density (µg/mg NP) | 0 | 84.7 ± 6.3 | BCA Assay |
Table 2: Functional In Vitro Performance
| Performance Metric | PLGA Core (Control) | Leukocyte-Coated NP | P-value |
|---|---|---|---|
| Rolling Velocity (µm/s) | No rolling | 5.2 ± 1.1 | <0.001 |
| Adhesion Density (particles/mm²) | 12 ± 5 | 310 ± 45 | <0.001 |
| Cellular Uptake (MFI) in Target Cells | 100 ± 15 (Baseline) | 450 ± 60 | <0.001 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomimetic Nanoparticle Research
| Reagent/Material | Supplier Examples | Function in Workflow |
|---|---|---|
| PLGA (50:50) | Sigma-Aldrich, Lactel | Biodegradable polymer forming the core nanoparticle; encapsulates active drug. |
| Histopaque-1077/1119 | Sigma-Aldrich | Density gradient medium for isolation of specific leukocyte populations from whole blood/bone marrow. |
| Protease Inhibitor Cocktail (EDTA-free) | Roche, Thermo Fisher | Prevents degradation of membrane proteins during cell lysis and membrane isolation. |
| Mini-Extruder with Polycarbonate Membranes | Avanti Polar Lipids | Instrument for fusing cell membranes onto nanoparticle cores via controlled extrusion. |
| µ-Slide VI 0.1 (Flow Chamber) | ibidi GmbH | Microfluidic slide for culturing endothelial monolayers and performing live-cell adhesion assays under shear flow. |
| Recombinant Mouse TNF-α | PeproTech, R&D Systems | Cytokine used to activate endothelial cells in culture, upregulating adhesion molecule expression. |
| Anti-CD45 Antibody, FITC | BioLegend | Fluorescent antibody for confirming leukocyte membrane presence on coated nanoparticles via flow cytometry. |
This guide defines the first phase of biomimetic biomedical research, scoped within the ongoing development of ISO standards for biomimetics (e.g., ISO 18458). The core objective is to establish a rigorous, reproducible framework for analyzing a biological phenomenon of interest (the "biological template") to extract its underlying principles for application to a defined biomedical problem. This phase ensures the research is grounded in a deep, mechanistic understanding of biology before proceeding to abstraction and implementation.
Core Workflow and Key Activities
The Biological Analysis & Scoping phase is a structured, iterative process. The primary workflow is detailed below.
Diagram Title: Phase 1 Core Workflow
Detailed Methodologies & Experimental Protocols
Activity A: Define & Characterize the Biological Template
Objective: To select and comprehensively describe the biological system (organism, tissue, cellular process, molecular mechanism) that exhibits a desirable function relevant to the biomedical problem.
Protocol 1: Systematic Literature Review & Meta-Analysis
- Search Strategy: Utilize databases (PubMed, Scopus, Web of Science) with structured queries combining terms for the biological system (e.g., "gecko," "limb regeneration," "CRISPR-Cas") and functional keywords (e.g., "adhesion," "wound healing," "adaptive immunity").
- Screening: Use PRISMA guidelines. Two independent reviewers screen titles/abstracts, then full texts against inclusion/exclusion criteria.
- Data Extraction: Code data into a standardized form: organism, experimental model, observed function, environmental conditions, key performance metrics, proposed mechanism.
- Analysis: Perform quantitative synthesis (meta-analysis) where possible. For qualitative data, use thematic analysis to identify consistent mechanistic themes.
Protocol 2: In Vivo/Ex Vivo Functional Characterization
- Example: Characterizing the anti-fouling properties of shark skin.
- Sample Acquisition: Obtain ethically sourced shark skin samples (dorsal, pectoral) from multiple species (e.g., Galeocerdo cuvier, Isurus oxyrinchus). Preserve in RNAlater or fixative.
- Microstructural Analysis:
- SEM Imaging: Dehydrate samples, sputter-coat with gold/palladium. Image at multiple magnifications (100x to 20,000x) to quantify denticle dimensions, riblet spacing, and arrangement.
- Micro-CT Scanning: For 3D structural reconstruction.
- Functional Bioassay:
- Prepare bacterial suspension (E. coli, Staphylococcus aureus) to OD600 = 0.1.
- Apply 100 µL onto test (shark skin) and control (smooth polymer) surfaces in a flow cell.
- Perfuse with sterile marine broth at a defined shear stress (e.g., 0.5 Pa) for 2 hours.
- Fix and stain adhered bacteria with SYTO 9 dye.
- Quantify adhesion density via fluorescence microscopy (5 random fields per sample) and image analysis software (e.g., ImageJ).
Activity B: Identify Core Functional Principles
Objective: To move from observation to mechanism, isolating the fundamental physical, chemical, and informational principles that enable the function.
Protocol: Multi-Omics Deconvolution of a Signaling Pathway
- Example: Analyzing the hypoxic response pathway in cancer cells mimicked from high-altitude adapted species.
- Cell Culture & Stimulation: Culture HepG2 cells under normoxia (21% O2) and hypoxia (1% O2) for 0, 2, 6, 12, 24 hours (n=4 biological replicates per condition).
- Multi-Omics Harvesting:
- Transcriptomics: Extract total RNA (TRIzol), assess quality (RIN > 8.5), prepare libraries (poly-A selection), sequence on Illumina platform (150 bp paired-end).
- Proteomics: Lyse cells in RIPA buffer, digest with trypsin, label with TMT 11-plex, fractionate by high-pH reverse-phase HPLC, analyze by LC-MS/MS.
- Metabolomics: Quench metabolism with -80°C methanol, extract metabolites, analyze via hydrophilic interaction liquid chromatography (HILIC)-MS.
- Data Integration & Pathway Mapping:
- Perform differential expression/abundance analysis (DESeq2 for RNA, Limma for proteins/metabolites).
- Map significantly altered entities (FDR < 0.05) to the KEGG "HIF-1 signaling pathway" (map04066) using pathway analysis tools (e.g., IPA, GSEA).
- Construct a causal network model.
Diagram Title: HIF-1 Signaling Pathway in Hypoxia
Table 1: Meta-Analysis of Anti-Fouling Surface Performance
| Biological Template | Key Structural Parameter (Avg.) | Reduction in Bacterial Adhesion (%) vs. Smooth Control | Tested Organism | Reference Year |
|---|---|---|---|---|
| Shark Skin (G. cuvier) | Riblet Spacing: 100 µm | 67% | S. aureus | 2022 |
| Lotus Leaf | Papillae Height: 15 µm, Wax Crystalloids | 85% (Hydrophobic) | E. coli | 2021 |
| Cicada Wing | Nanopillar Height: 200 nm, Diameter: 80 nm | 99.9% (Bactericidal) | P. aeruginosa | 2023 |
| Dragonfly Wing | Nanopillar Height: 240 nm | 95% (Bactericidal) | B. subtilis | 2022 |
Table 2: Multi-Omics Analysis of Hypoxic Response (24h vs. 0h)
| Molecule Type | Total Analyzed | Significantly Altered (FDR<0.05) | Up-Regulated | Down-Regulated | Key Enriched Pathway (KEGG) |
|---|---|---|---|---|---|
| mRNA | 18,500 | 1,842 | 1,201 | 641 | HIF-1 Signaling (p=3.2e-12) |
| Protein | 6,200 | 487 | 312 | 175 | Glycolysis / Gluconeogenesis (p=1.8e-9) |
| Metabolite | 450 | 89 | 56 | 33 | Central Carbon Metabolism (p=4.5e-6) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Phase 1 Analysis
| Item (Supplier Example) | Function in Phase 1 | Specific Application Example |
|---|---|---|
| RNAlater Stabilization Solution (Thermo Fisher) | Preserves RNA/DNA integrity in biological samples at the time of collection. | Stabilizing tissue from a novel extremophile organism prior to omics analysis. |
| TRIzol Reagent (Invitrogen) | Monophasic solution for simultaneous isolation of high-quality RNA, DNA, and proteins from a single sample. | Extracting biomolecules from limited precious samples for integrated multi-omics. |
| Tandem Mass Tag (TMT) 11-plex Kit (Thermo Fisher) | Enables multiplexed quantitative proteomics, allowing comparison of up to 11 different experimental conditions in one MS run. | Comparing protein expression across multiple time points or hypoxia levels. |
| SYTO 9 Green Fluorescent Nucleic Acid Stain (Invitrogen) | Cell-permeant dye that stains all bacteria in a population, used for quantifying adhesion or viability. | Visualizing and quantifying bacterial biofilm formation on bio-inspired surfaces. |
| Anti-HIF-1α Antibody [EPR16897] (Abcam) | Validated monoclonal antibody for specific detection of stabilized HIF-1α protein via western blot or IHC. | Confirming activation of the hypoxic response pathway in cell-based models. |
| Matrigel Matrix (Corning) | Basement membrane extract used for 3D cell culture, angiogenesis assays, and modeling tissue complexity. | Creating a more physiologically relevant environment to study cell migration/invasion. |
The development of ISO standards for biomimetics, such as the ongoing work on ISO/TC 266, necessitates a rigorous phase of abstraction. This phase translates observed biological phenomena into core, testable engineering principles. For drug development, this involves moving from biological complexity (e.g., a cell signaling cascade) to an isolatable principle (e.g., negative feedback-based homeostasis) that can inform therapeutic strategies like adaptive drug dosing or biomimetic material design for controlled release, ensuring standardized terminology and methodology across the field.
Abstraction identifies universal mechanisms. The following table summarizes key principles and their therapeutic analogs.
Table 1: Core Biological Principles and Corresponding Therapeutic Applications
| Core Biological Principle | Biological Example | Abstracted Concept | Potential Drug Development Application |
|---|---|---|---|
| Specific Molecular Recognition | Ligand-receptor binding (e.g., insulin-INSR) | High-affinity, lock-and-key interaction | Design of targeted biologics (mAbs, peptides); biosensor development. |
| Signal Transduction & Amplification | GPCR-cAMP-PKA pathway | Input-output cascade with gain | Targeting allosteric sites; developing pathway-specific inhibitors/activators. |
| Feedback Regulation (Negative) | HIF-α degradation in normoxia | Homeostatic control loop | Mimicking with synthetic gene circuits for regulated therapeutic protein expression. |
| Self-Assembly & Emergent Order | Actin polymerization | Programmable bottom-up organization | Development of drug-delivery vesicles (liposomes) or supramolecular nanomedicines. |
| Adaptation & Learning | Immune memory (T/B cells) | System that improves response upon repeated exposure | Basis for vaccine design; adoptive cell therapies (CAR-T). |
| Compartmentalization | Mitochondrial cristae | Spatial segregation of function | Organelle-targeted drug delivery; enzyme prodrug therapy. |
This protocol outlines how to empirically dissect and abstract a core principle from a canonical signaling pathway for validation.
Protocol: Deconstructing the EGFR-ERK Pathway for Abstraction of Ultrasensitivity Objective: To isolate and quantify the ultrasensitive input-output relationship in the EGFR-MAPK/ERK cascade, abstracting it as a signal-processing module.
- Cell Culture: Maintain HEK293 or A431 cells in DMEM + 10% FBS. Seed in 96-well plates for stimulation and 10cm dishes for immunoblotting.
- Stimulation Gradient: Serum-starve cells for 18 hours. Stimulate with a 12-point gradient of purified human EGF ligand (0, 0.01, 0.1, 0.5, 1, 2, 5, 10, 20, 50, 100, 200 ng/mL). Incubate for precisely 10 minutes at 37°C.
- Cell Lysis & Protein Quantification: Lyse cells in RIPA buffer with protease/phosphatase inhibitors. Quantify total protein using a BCA assay.
- Western Blot Analysis:
- Load equal protein amounts on 4-12% Bis-Tris gels, separate via SDS-PAGE, and transfer to PVDF membranes.
- Probe with primary antibodies: p-EGFR (Tyr1068), total EGFR, p-MEK1/2 (Ser217/221), p-ERK1/2 (Thr202/Tyr204), total ERK, and a loading control (β-actin).
- Use HRP-conjugated secondary antibodies and chemiluminescent detection. Quantify band densitometry.
- Data Modeling: Plot normalized p-ERK intensity vs. log([EGF]). Fit data to a Hill equation: Response = (Vmax * [S]^n) / (Kd^n + [S]^n), where n (Hill coefficient) quantifies ultrasensitivity (n > 1 indicates cooperative, switch-like behavior).
- Abstraction Validation: Test the abstracted principle (switch-like amplification) by introducing a pathway perturbation (e.g., 5µM MEK inhibitor U0126) and repeating the stimulation gradient. The abstracted model should predict the dampened response.
Diagram 1: EGFR-ERK Pathway Abstraction
Diagram 2: Experimental Workflow for Abstraction
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Research Reagents for Signaling Pathway Abstraction
| Reagent / Material | Function in Abstraction Experiments | Key Considerations |
|---|---|---|
| Recombinant Human EGF | Defined, pure ligand for precise, quantitative pathway stimulation. Ensures reproducibility. | Lyophilized stability, carrier protein (e.g., BSA) concentration, endotoxin levels. |
| Pathway-Specific Phospho-Antibodies (e.g., anti-p-ERK) | Enable quantification of dynamic signal transduction states (activity). | Validate specificity via knockout/knockdown cells; check lot-to-lot consistency. |
| Small Molecule Inhibitors (e.g., U0126 for MEK) | Tools for controlled perturbation to test causality and model predictions. | Optimize DMSO concentration for vehicle controls; confirm target selectivity. |
| ChemiDoc or Similar Imaging System | For quantitative digital capture of Western blot or assay signals. | Must have a wide linear dynamic range for accurate densitometry. |
| GraphPad Prism / MATLAB | Software for nonlinear regression (Hill fits), modeling, and statistical analysis. | Essential for translating raw data into abstracted mathematical relationships. |
| ISO/TR 18401:2017 (Biomimetics) | Reference document for standardized terminology, supporting clear communication of abstracted principles. | Provides a framework to document the abstraction process consistently. |
This whitepaper details the technical implementation and in silico simulation phase of biomimetic system development. As part of a broader thesis on establishing ISO standards for biomimetics, this phase translates conceptual biomimetic designs into testable computational models and experimental protocols. The objective is to create standardized, reproducible workflows for simulating biological mechanisms—such as targeted drug delivery or cellular signaling—prior to physical prototyping, thereby reducing resource expenditure and accelerating research.
Core Technical Implementation Framework
Implementation follows a modular pipeline: 1) System Parameterization from biological data, 2) Model Selection & Assembly, 3) Computational Simulation, and 4) Output Validation against in vitro benchmarks.
Quantitative parameters are extracted from published literature and databases to inform model variables.
Table 1: Key Biological Parameters for a Biomimetic Nanoparticle Delivery System
| Parameter | Typical Value Range | Source / Assay | Relevance to Model |
|---|---|---|---|
| Tumor Vascular Pore Size | 100 - 780 nm | Transmission Electron Microscopy (TEM) of tumor tissue | Defines maximum nanoparticle size for EPR effect |
| Ligand-Receptor Binding Affinity (Kd) | 0.1 - 10 nM | Surface Plasmon Resonance (SPR) | Determines targeting efficiency in kinetic models |
| Serum Half-life of PEGylated NPs | 12 - 24 hours | Pharmacokinetic (PK) studies in murine models | Informs clearance rates in PK/PD models |
| Cellular Internalization Rate | 10^3 - 10^4 NPs/cell/hour | Flow Cytometry with fluorescent NPs | Sets uptake rate in cellular-scale models |
| Tumor Extracellular pH | 6.5 - 6.9 | pH-sensitive microelectrodes | Critical for pH-responsive drug release models |
Selection of Simulation Modalities
The choice of simulation depends on the scale and question.
Table 2: Simulation Modalities in Biomimetics
| Modality | Scale | Typical Software/Tool | Application Example |
|---|---|---|---|
| Molecular Dynamics (MD) | Atomic, 1-100 nm | GROMACS, NAMD | Simulating ligand-protein docking for a biomimetic inhibitor |
| Finite Element Analysis (FEA) | Continuum, µm-mm | COMSOL, ANSYS | Modeling stress on a biomimetic scaffold in tissue |
| Agent-Based Modeling (ABM) | Cellular, µm-mm | NetLogo, CompuCell3D | Simulating population-level cell response to a drug-releasing implant |
| Pharmacokinetic/Pharmacodynamic (PK/PD) | Whole Organism | PK-Sim, MATLAB/SimBiology | Predicting concentration-time profiles of a biomimetic drug formulation |
Detailed Experimental & Simulation Protocols
Protocol: Multi-scale Simulation of a Biomimetic Drug Delivery Nanoparticle
This protocol integrates multiple simulation types to model a pH-sensitive, ligand-targeted nanoparticle.
A. Molecular Dynamics for Ligand-Receptor Binding
- Objective: Simulate the binding stability of the targeting peptide (e.g., RGD) to its integrin receptor (αvβ3) at normal (7.4) and acidic (6.5) pH.
- Method: a. Obtain 3D structures of the RGD peptide (PubChem CID: 123831) and integrin αvβ3 (PDB ID: 1L5G) from public databases. b. Perform protein and ligand preparation (protonation, solvation, energy minimization) using UCSF Chimera and the AMBER force field. c. Set up simulation boxes with explicit water (TIP3P model) and physiological ion concentration (0.15 M NaCl). d. Run equilibration (100 ps) followed by production MD simulation (50 ns) under NPT conditions (310 K, 1 atm) using NAMD. e. Analyze trajectories using VMD: calculate Root Mean Square Deviation (RMSD) of the ligand-binding pocket, hydrogen bond occupancy, and binding free energy via the Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) method.
B. Agent-Based Model for Tumor Uptake
- Objective: Predict spatial distribution and cellular uptake of nanoparticles in a simulated tumor microenvironment.
- Method: a. Using NetLogo, create a 2D grid (1000 x 1000 µm) representing a cross-section of tumor tissue. b. Populate with agents: Endothelial Cells (forming leaky vessels), Tumor Cells (expressing target receptors), Macrophages (for clearance), and Blood Flow. c. Parameterize agents based on Table 1 (e.g., vascular pore size, internalization rate). d. Program nanoparticle agents (diameter: 100 nm, surface: RGD ligands) to enter from vasculature, diffuse via Brownian motion, bind to tumor cells based on stochastic probability derived from MD Kd values, and be internalized. e. Run simulation for 48 hours (simulated time). Track metrics: % injected dose in tumor, penetration depth from vasculature, and heterogeneity of uptake.
Diagram Title: Multi-scale Simulation Workflow for Biomimetic Nanoparticles
Protocol:In VitroValidation of Simulated Biomimetic Systems
In silico predictions require empirical validation using standardized assays.
Title: In Vitro Pharmacodynamics of a Biomimetic Nanoparticle in a 3D Spheroid Model. Objective: To validate the tumor penetration and cell kill predictions of the ABM simulation. Materials: See "The Scientist's Toolkit" below. Method:
- Spheroid Generation: Seed U-87 MG glioblastoma cells (high αvβ3 expression) in ultra-low attachment 96-well plates (500 cells/well). Culture for 96 hours to form compact spheroids (~500 µm diameter).
- Nanoparticle Treatment: Prepare fluorescent (Cy5-labeled) RGD-targeted and non-targeted (PEG-only) nanoparticles (100 nm). Treat spheroids with 100 µg/mL NP equivalent in complete media. Incubate for 2, 6, and 24 hours (n=6 per group).
- Penetration Analysis: At each time point, wash spheroids 3x with PBS. Fix with 4% PFA for 30 min. Image using a confocal microscope with Z-stacking (10 µm intervals). Use ImageJ to plot fluorescence intensity as a function of depth from spheroid surface.
- Efficacy Analysis: For separate spheroids, treat with drug-loaded (e.g., Doxorubicin) nanoparticles. After 72 hours, assess viability via CellTiter-Glo 3D Assay. Calculate IC50 values for targeted vs. non-targeted formulations.
- Validation: Correlate penetration depth vs. time and relative efficacy from experiment with ABM output using Pearson correlation analysis. A strong positive correlation (r > 0.85) validates the simulation.
Diagram Title: In Vitro Spheroid Validation Protocol Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Biomimetic Nanoparticle Validation
| Item/Reagent | Function in Protocol | Example Product/Catalog # | Key Notes |
|---|---|---|---|
| Ultra-Low Attachment (ULA) Plate | Prevents cell adhesion, enabling 3D spheroid self-assembly. | Corning Costar #7007 | Critical for reproducible, round spheroid formation. |
| pH-Sensitive Polymer (e.g., Poly(β-amino ester)) | Core biomimetic material enabling drug release in acidic tumor microenvironments. | PolySciTech AK097 | Degradation rate must be characterized via GPC at pH 7.4 vs. 6.5. |
| Targeting Ligand (e.g., cRGDfK Peptide) | Conjugated to nanoparticle surface for active targeting of overexpressed receptors (e.g., αvβ3 integrin). | MedChemExpress HY-P1366 | Must include a spacer (PEG) and reactive group (maleimide, NHS) for conjugation. |
| CellTiter-Glo 3D Cell Viability Assay | Luminescent assay optimized for measuring ATP in 3D cell cultures, indicating viability. | Promega G9681 | Requires orbital shaking to lyse cells within spheroids effectively. |
| Fluorescent Probe for Labeling (e.g., Cy5 NHS Ester) | Covalently labels nanoparticle polymer for tracking via fluorescence microscopy or flow cytometry. | Lumiprobe #23020 | Labeling ratio must be quantified (UV-Vis) to avoid quenching or altered biodistribution. |
Standardization and ISO Context
The protocols and toolkits outlined are designed as candidate modules for an ISO standard on biomimetic in silico and in vitro testing. Standardization requires:
- Defined Input/Output Formats: For simulation files (e.g., SBML for PK/PD models).
- Reference Datasets: For validation (e.g., standard cell line spheroid growth curves).
- Reporting Criteria: Mandatory metadata (software version, force field, iteration counts) must accompany published results to ensure reproducibility—a core tenet of both robust science and forthcoming ISO guidelines for biomimetics.
The pursuit of advanced drug delivery systems (DDS) increasingly relies on biomimetics—the imitation of models, systems, and elements of nature for solving complex problems. This field is being formalized under emerging ISO standards for biomimetics (e.g., ISO 18458:2015 and related drafts under development), which provide a structured lexicon and methodological framework. Within this context, mimicking the exquisite selectivity of the cell membrane represents a paramount case study. This whitepaper details the technical approaches, experimental protocols, and quantitative data underpinning the development of biomimetic DDS that replicate phospholipid bilayer structure, transport protein function, and ligand-receptor specificity to achieve targeted, efficient, and safe therapeutic delivery.
Core Biomimetic Principles for Membrane Selectivity
Cell membrane selectivity arises from:
- Amphiphilic Phospholipid Bilayer: Provides a selective barrier based on hydrophobicity and molecular size.
- Integral Membrane Proteins (Channels, Carriers, Pumps): Facilitate active and passive transport.
- Surface Glycoproteins and Glycolipids: Enable ligand-specific recognition and signaling.
- Membrane Fluidity and Phase Behavior: Influences incorporation and release dynamics.
Quantitative Analysis of Key Biomimetic Platforms
Table 1: Comparison of Biomimetic Drug Delivery Platforms Mimicking Membrane Selectivity
| Platform | Core Components (Mimicked Element) | Typical Size (nm) | Drug Loading Efficiency (%) * | Selectivity Mechanism | Key Challenge |
|---|---|---|---|---|---|
| Liposomes | Phospholipids, cholesterol (Bilayer) | 80-200 | 10-40 | Passive (EPR effect), ligand grafting | Rapid clearance, low stability |
| Polymeric Nanoparticles | PLGA, PEG (Hydrophobic core/hydrophilic shell) | 100-300 | 50-85 | Surface functionalization with antibodies, peptides | Potential polymer toxicity, batch variability |
| Solid Lipid Nanoparticles (SLNs) | Solid lipid matrix (Membrane fluidity) | 150-500 | 25-70 | Controlled release, ligand attachment | Drug expulsion during storage |
| Cell Membrane-Coated Nanoparticles | Extracted plasma membrane (Full surface proteome) | 100-200 | Varies by core | Homotypic targeting, immune evasion | Complex fabrication, membrane integrity |
| Peptide-Based Nanocarriers | Self-assembling peptides (Channel proteins) | 10-50 | 20-60 | Stimuli-responsive assembly/disassembly | Scalability, in vivo stability |
Data represents ranges consolidated from recent literature (2022-2024).
Table 2: Performance Metrics of Selectivity-Enhanced DDS in Recent Preclinical Studies
| Delivery System | Targeting Ligand | Disease Model (Year) | Reported Tumor Accumulation (% Injected Dose/g) | Reduction in Off-Target Accumulation (vs. non-targeted) |
|---|---|---|---|---|
| Liposome | Anti-HER2 scFv | Breast Cancer (2023) | 8.5 ± 1.2 | 3.2-fold in liver |
| PLGA NP | cRGD peptide | Glioblastoma (2022) | 4.2 ± 0.8 | 2.5-fold in spleen |
| RBC Membrane-Coated NP | (Inherent CD47) | Melanoma (2024) | 6.1 ± 0.9 | >5-fold in liver (vs. PEGylated NP) |
| Exosome | Engineered Lamp2b-folate | Ovarian Cancer (2023) | 10.3 ± 2.1 | N/A (inherent targeting) |
Detailed Experimental Protocols
Protocol 4.1: Fabrication and Characterization of Ligand-Grafted Liposomes
Objective: To create folate-targeted liposomes for selective delivery to folate receptor-overexpressing cells. Materials: DSPC, Cholesterol, DSPE-PEG(2000), DSPE-PEG(2000)-Folate, Chloroform, Drug (e.g., Doxorubicin HCl). Method:
- Lipid Film Formation: Dissolve lipids in chloroform at molar ratio 55:40:5:0.5 (DSPC:Chol:DSPE-PEG:DSPE-PEG-Folate). Evaporate under nitrogen to form thin film. Desiccate overnight.
- Hydration & Size Reduction: Hydrate film with ammonium sulfate buffer (250 mM, pH 5.5) at 60°C. Vortex. Subject to 5 freeze-thaw cycles. Extrude sequentially through polycarbonate membranes (400 nm, 200 nm, 100 nm, 2x through 80 nm).
- Remote Drug Loading: Incubate liposomes with doxorubicin solution (drug:lipid = 1:10 w/w) at 60°C for 1h. Cool on ice.
- Purification: Pass through Sephadex G-50 column eluted with PBS (pH 7.4) to remove unencapsulated drug.
- Characterization: Determine size and PDI via DLS. Measure drug encapsulation efficiency via HPLC after lysing vesicles with 1% Triton X-100.
Protocol 4.2: Preparation of Cell Membrane-Coated Nanoparticles
Objective: To cloak polymeric nanoparticles with a natural cell membrane for immune evasion and homologous targeting. Materials: PLGA, PVA, HeLa cells, Hypotonic lysing buffer, Sucrose, Ultracentrifuge. Method:
- Core NP Synthesis: Prepare PLGA nanoparticles using standard emulsion-solvent evaporation method.
- Membrane Vesicle Derivation: Culture HeLa cells to confluence. Harvest, wash. Lyse in hypotonic buffer with protease inhibitors on ice for 30 min. Homogenize gently. Centrifuge at 3200xg (10 min, 4°C) to pellet nuclei/debris. Collect supernatant and centrifuge at 20,000xg (30 min, 4°C) to pellet membrane fragments.
- Membrane Coating: Resuspend membrane pellet in PBS. Co-extrude with purified PLGA NPs (1:1 protein:PLGA weight ratio) 10x through a 400 nm porous polycarbonate membrane using an extruder.
- Validation: Confirm coating via transmission electron microscopy (TEM) and zeta potential shift towards native membrane value. Analyze protein content via SDS-PAGE.
Visualizing Pathways and Workflows
Diagram 1: Drug Delivery Pathways Compared (Free vs. Non-Targeted vs. Biomimetic)
Diagram 2: Workflow for Biomimetic Carrier Fabrication
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Mimicking Membrane Selectivity
| Category | Specific Item/Reagent | Function in Research | Key Supplier Examples |
|---|---|---|---|
| Lipid Building Blocks | 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC), Cholesterol | Forms the foundational bilayer structure, mimicking membrane fluidity and stability. | Avanti Polar Lipids, Merck Millipore |
| PEGylation Reagents | DSPE-PEG(2000), DSPE-PEG(2000)-Maleimide, -Carboxyl, -Folate | Provides "stealth" properties and a conjugation handle for attaching targeting ligands. | NOF America, Nanocs |
| Biodegradable Polymers | Poly(lactic-co-glycolic acid) (PLGA), Polycaprolactone (PCL) | Forms the degradable core of synthetic nanoparticles, allowing controlled drug release. | Corbion, Lactel, Sigma-Aldrich |
| Targeting Ligands | Folate, cRGD peptides, Trastuzumab (Herceptin) fragments | Confers active targeting specificity to overexpressed receptors on target cells. | Selleck Chemicals, PeptideGenics |
| Cell Membrane Isolation Kits | Plasma Membrane Protein Extraction Kit | Standardizes the process of harvesting intact membrane proteins for coating applications. | Abcam, Thermo Fisher |
| Characterization Tools | Dynamic Light Scattering (DLS) systems, Zetasizer | Measures nanoparticle size, polydispersity index (PDI), and zeta potential (surface charge). | Malvern Panalytical, Horiba |
| In Vitro Validation | Cell lines with known receptor overexpression (e.g., HeLa, MCF-7), Flow Cytometry Assays | Enables quantification of cellular uptake and targeting efficiency. | ATCC, BD Biosciences |
This technical exploration demonstrates that mimicking cell membrane selectivity requires a systematic, interdisciplinary approach—precisely the focus of evolving ISO standards for biomimetics. These standards encourage a structured definition of the biological model (the selective membrane), the abstracted principles (ligand-receptor kinetics, self-assembly), and the technical implementation (functionalized nanocarriers). The quantitative data and protocols provided herein offer a reproducible framework that aligns with the ISO's goal of standardizing biomimetic methodology, ultimately accelerating the translation of bio-inspired, selective drug delivery systems from bench to bedside. Future work must focus on standardizing characterization metrics (e.g., targeting efficiency coefficients) to enable direct comparison across studies, a key next step for the field under the biomimetics ISO umbrella.
This case study is framed within the ongoing research for the development of ISO standards for biomimetics definition and concepts, specifically pertaining to the principles of material and structure integration. The trabecular bone, with its hierarchically porous, anisotropic architecture, presents a canonical model for biomimetic design. This document examines the translation of its key structural and functional parameters into synthetic bone tissue engineering scaffolds, detailing the quantitative metrics, fabrication protocols, and biological validation required for standards-compliant biomimetic replication.
Quantitative Architectural Parameters of Trabecular Bone
The design of biomimetic scaffolds must be informed by the quantitative metrics of native trabecular bone, as derived from micro-CT analyses. These parameters form the basis for performance criteria in biomimetic design standards.
Table 1: Key Quantitative Parameters of Human Trabecular Bone
| Parameter | Typical Range | Measurement Technique | Functional Implication for Scaffold Design |
|---|---|---|---|
| Porosity | 75-95% | Micro-CT Volumetric Analysis | Governs cell infiltration, vascularization, and nutrient diffusion. |
| Pore Size | 300-600 μm (cancellous) | Mean Intercept Length | Optimal for osteoconduction and bone ingrowth. |
| Pore Interconnectivity | >98% | Euler-Poincaré Characteristic | Essential for tissue integration and preventing necrotic cores. |
| Trabecular Thickness (Tb.Th) | 100-200 μm | Micro-CT, Plate Model | Influences scaffold mechanical strength and degradation profile. |
| Trabecular Separation (Tb.Sp) | 500-1500 μm | Micro-CT, Plate Model | Determines pore size and spatial distribution of osteoblasts. |
| Structural Anisotropy | Degree of Alignment (1-10) | Fabric Tensor Analysis | Guides mechanically competent, directionally-oriented tissue growth. |
| Compressive Modulus | 10-900 MPa | Mechanical Testing | Target range for matching mechanical properties of implant site. |
Fabrication Methodologies for Trabecular-Mimetic Scaffolds
Protocol: Additive Manufacturing (SLA/DLP) of Photopolymerizable Ceramic-Polymer Composite
- Objective: To fabricate scaffolds with precise, patient-specific architecture.
- Materials: Hydroxyapatite (HA) or β-Tricalcium Phosphate (β-TCP) powder (< 5 μm), Biodegradable photopolymer resin (e.g., poly(ethylene glycol) diacrylate - PEGDA), Photoinitiator (Irgacure 2959).
- Procedure:
- Prepare a homogeneous slurry with 30-40 wt% ceramic powder in photopolymer resin with 1% (w/w) photoinitiator.
- Load slurry into the vat of a stereolithography (SLA) or digital light processing (DLP) printer.
- Import scaffold CAD model (designed to match parameters in Table 1) into printer software.
- Slice the model with layer thickness of 25-100 μm.
- Print under UV light (λ=365 nm) with exposure time optimized for slurry viscosity and ceramic loading.
- Post-process: Wash in isopropanol to remove uncured resin, then post-cure under broad-spectrum UV light for 15 minutes.
- Sinter (if required) in a furnace with a controlled ramp cycle to burnout polymer and densify ceramic scaffold.
Protocol: Thermally Induced Phase Separation (TIPS) of Polymer Scaffolds
- Objective: To create highly interconnected, microporous scaffolds mimicking trabecular struts.
- Materials: Poly(L-lactic acid) (PLLA) or Poly(lactic-co-glycolic acid) (PLGA), 1,4-Dioxane or Dichloromethane.
- Procedure:
- Dissolve polymer in solvent at 5-10% (w/v) concentration at 50-60°C to form a homogeneous solution.
- Pour solution into a mold and rapidly quench to -20°C to induce liquid-liquid phase separation.
- Maintain at -20°C for 2 hours to allow coarsening and structure stabilization.
- Immerse the quenched solution in cold ethanol or water at -20°C for 48 hours to extract the solvent via solvent exchange.
- Lyophilize the scaffold for 48 hours to remove the extracted solvent and ice crystals, leaving a porous network.
- Characterize pore morphology via scanning electron microscopy (SEM).
Biological Validation & Key Signaling Pathways
Scaffold performance is validated by assessing osteogenic differentiation of seeded mesenchymal stem cells (MSCs), governed by specific mechanotransduction and biochemical pathways.
Diagram Title: Mechano-Chemical Pathways in Scaffold-Mediated Osteogenesis.
Protocol: In Vitro Osteogenic Differentiation Assay
- Objective: To quantify scaffold-induced osteogenic differentiation of human MSCs (hMSCs).
- Materials: hMSCs (P4-P6), Osteogenic media (DMEM, 10% FBS, 10 mM β-glycerophosphate, 50 μg/mL ascorbic acid, 100 nM dexamethasone), Sterile 3D scaffolds (Ø5x3 mm), ALP staining kit, Alizarin Red S solution.
- Procedure:
- Seeding: Sterilize scaffolds (EtOH or UV). Seed hMSCs at a density of 1x10^5 cells/scaffold in a droplet method. Incubate for 2 hours, then add culture media.
- Culture: Maintain in osteogenic media, changing every 3 days for up to 21 days.
- Alkaline Phosphatase (ALP) Activity (Day 7-10): Lyse cells in 0.1% Triton X-100. Incubate lysate with p-nitrophenyl phosphate (pNPP) substrate. Measure absorbance at 405 nm. Normalize to total protein (BCA assay).
- Mineralization Assay (Alizarin Red S, Day 21): Fix scaffolds in 4% PFA for 15 min. Stain with 2% Alizarin Red S (pH 4.2) for 30 min. Wash extensively. For quantification, destain with 10% cetylpyridinium chloride for 1 hour. Measure absorbance at 562 nm.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for Trabecular Scaffold R&D
| Item / Reagent | Function in Research | Typical Supplier / Example |
|---|---|---|
| β-Tricalcium Phosphate (β-TCP) Powder | Bioactive ceramic providing osteoconductivity and ionic cues (Ca²⁺). | Sigma-Aldrich, Berkeley Advanced Biomaterials |
| Poly(L-lactic acid) (PLLA) | Biodegradable polymer providing structural integrity and tunable degradation. | Corbion, Lactel Absorbable Polymers |
| Poly(ethylene glycol) diacrylate (PEGDA) | Photopolymerizable hydrogel resin for additive manufacturing. | Sigma-Aldrich, Laysan Bio |
| Irgacure 2959 | UV photoinitiator for crosslinking photopolymer resins. | BASF, Sigma-Aldrich |
| Human Mesenchymal Stem Cells (hMSCs) | Primary cell source for osteogenic differentiation studies. | Lonza, ATCC |
| Osteogenic Differentiation Media Kit | Standardized media supplement for inducing osteogenesis. | Thermo Fisher Scientific, Gibco |
| AlamarBlue or PrestoBlue | Cell viability and proliferation assay reagent for 3D cultures. | Thermo Fisher Scientific, Invitrogen |
| Osteocalcin (OCN) ELISA Kit | Quantitative measurement of late-stage osteogenic marker. | R&D Systems, Abcam |
| Micro-CT Imaging System (e.g., SkyScan) | Non-destructive 3D quantification of scaffold architecture and bone ingrowth. | Bruker, Scanco Medical |
Integrating ISO Biomimetics Methodology with Stage-Gate Drug Development Processes
This whitepaper explores the systematic integration of biomimetic principles, as defined by ISO standards, into structured pharmaceutical development. The International Organization for Standardization's technical committee ISO/TC 266 has developed standards, such as ISO 18458:2015 and ISO 18459:2015, which provide a formalized framework for biomimetics. This involves a defined methodology—problem analysis, search for biological analogies, abstraction, implementation, and evaluation. Concurrently, the Stage-Gate process, a widely adopted project management framework, governs drug development from discovery to launch through discrete, gated stages. The fusion of these two disciplined approaches offers a pathway to more efficient, innovative, and biologically-inspired therapeutic solutions. This document is framed within a broader thesis positing that ISO biomimetics standards provide the necessary rigorous vocabulary and methodological structure to translate biological inspiration into reproducible industrial and scientific outcomes.
Foundational Concepts: ISO Biomimetics and Stage-Gate
ISO Biomimetics: A Standardized Methodology
ISO 18458 defines biomimetics as the "interdisciplinary cooperation of biology and technology or other fields of innovation with the goal of solving practical problems through the function analysis of biological systems, their abstraction into models, and the transfer into and application of these models to the solution." The core process is codified into a five-phase cycle.
Table 1: Core Phases of ISO Biomimetics Methodology (ISO 18458)
| Phase | ISO Designation | Core Activity | Output for Drug Development |
|---|---|---|---|
| 1 | Analysis & Definition | Clarification of the technical/medical problem. | Clear target product profile (TPP) with specific biological challenge (e.g., targeted drug delivery, anti-biofilm agent). |
| 2 | Biological Research | Search for biological analogies solving similar functions. | Compendium of biological models (e.g., targeted toxin delivery in venom, molecular camouflage in viruses). |
| 3 | Abstraction | Creation of a solution-neutral functional model from the biological analogy. | Abstracted design principles (e.g., "ligand-receptor lock-and-key," "pH-dependent conformational change"). |
| 4 | Implementation | Technical execution and creation of a technical solution. | Prototype therapeutic (e.g., a novel drug conjugate, a biomimetic nanoparticle, a peptide inhibitor). |
| 5 | Evaluation | Comparison of the technical solution with requirements and biological model. | In vitro/in vivo data validating function against TPP and original biological principle. |
The Stage-Gate Drug Development Process
The Stage-Gate model divides development into stages (where work is done) and gates (where go/kill/hold/recycle decisions are made). A typical pharmaceutical model includes Discovery, Preclinical, Clinical Development (Phases I-III), Regulatory Review, and Launch.
Integration Framework: Mapping ISO Phases onto Stage-Gate
The integration is achieved by embedding the ISO biomimetic cycle within the relevant stages of the drug development pipeline, particularly the early discovery and preclinical phases.
Diagram: Integration of ISO Biomimetics into Early Stage-Gate
Title: Biomimetic ISO Cycle Embedded in Drug Discovery Stages
Detailed Experimental Protocols for Key Integrated Activities
Aim: To identify and abstract a biological mechanism for cell-specific targeting.
- Step 1 (ISO Phase 1 - Analysis): Define the problem: "Require a delivery system that selectively binds to overexpressed EGFR on non-small cell lung cancer cells while minimizing hepatocyte uptake."
- Step 2 (ISO Phase 2 - Biological Research):
- Perform a systematic literature review using databases (PubMed, Google Scholar) with keywords: "natural toxin targeting," "viral tropism," "antibody-dependent targeting."
- In vivo observation: Utilize zebrafish (Danio rerio) xenograft models to study the homing behavior of immune cells (e.g., T-cells) to tumor sites via chemokine gradients.
- Step 3 (ISO Phase 3 - Abstraction):
- From viral tropism, abstract the principle: "Surface glycoprotein (key) binds to specific cell receptor (lock)."
- From immune cell homing, abstract: "Guided migration via gradient of signaling molecules (chemokines)."
- Output: Abstracted design principle: "A multivalent ligand system on a nanoparticle surface to enhance binding avidity to a specific receptor, potentially coupled with a sensed environmental gradient (e.g., pH, enzyme)."
Protocol: Implementation & Evaluation of a Biomimetic Protease Inhibitor
Aim: To develop a peptide-based inhibitor mimicking a natural protease-inhibitor complex.
- Step 1-3 (ISO Phases 1-3): Following the identification of the serine protease inhibitor mechanism in Ascaris nematodes (a natural host survival strategy).
- Step 4 (ISO Phase 4 - Implementation):
- Molecular Modeling: Use the crystal structure of the target human protease (e.g., neutrophil elastase) and the natural inhibitor. Perform in silico docking (using Rosetta, AutoDock Vina) to design a minimal cyclic peptide mimic.
- Solid-Phase Peptide Synthesis (SPPS): Synthesize the designed peptide using Fmoc-chemistry on a resin. Cleave and purify via reverse-phase HPLC. Confirm identity via LC-MS.
- Step 5 (ISO Phase 5 - Evaluation):
- Enzymatic Assay: Perform a fluorogenic substrate-based kinetic assay. Pre-incubate the target protease with varying concentrations of the biomimetic peptide. Measure residual activity. Calculate IC50.
- Cell-Based Assay: Treat neutrophil-like HL-60 cells with an inflammatory stimulus in the presence/absence of the inhibitor. Measure supernatant elastase activity and IL-8 production via ELISA.
- Gate 2 Criteria Check: Compare IC50, selectivity index, and cellular efficacy against predefined Gate 2 criteria for progression to in vivo studies.
Table 2: Example Quantitative Data from Biomimetic Inhibitor Evaluation
| Compound (Source) | Target Protease | In vitro IC50 (nM) | Selectivity Index (vs. Trypsin) | Cellular Efficacy (IC50, µM) | Cytotoxicity (CC50, µM) |
|---|---|---|---|---|---|
| Natural Ascaris Inhibitor | Neutrophil Elastase | 0.5 | >1000 | N/A | N/A |
| Biomimetic Peptide A | Neutrophil Elastase | 15.2 | 450 | 2.1 | >100 |
| Biomimetic Peptide B | Neutrophil Elastase | 8.7 | 120 | 5.4 | >100 |
| Marketed Inhibitor (Sivelestat) | Neutrophil Elastase | 44.0 | 20 | 12.5 | >100 |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Research Reagents for Biomimetic Drug Discovery
| Reagent / Material | Function / Application | Example in Context |
|---|---|---|
| 3D Cell Culture/Organoid Kits (e.g., Matrigel, spheroid plates) | To create more physiologically relevant models for testing biomimetic agents that rely on tissue architecture and cell-cell signaling. | Testing a biomimetic anti-metastatic drug mimicking marine sponge compounds that disrupt cell adhesion. |
| Recombinant Human Proteins & Cell Lines | For in vitro binding and functional assays to validate the abstracted principle (e.g., ligand-receptor interaction). | Using EGFR-overexpressing A431 cells to test targeting avidity of a biomimetic nanoparticle. |
| Click Chemistry Kits (e.g., DBCO-Azide) | For modular, bioorthogonal conjugation of biomimetic ligands (peptides, sugars) to drug carriers (nanoparticles, liposomes). | Implementing a "viral-like" surface functionalization on a liposome. |
| Protease Activity Assay Kits (Fluorogenic) | For high-throughput screening of biomimetic protease inhibitors derived from natural models. | Evaluating inhibitors abstracted from nematode or plant defense proteins. |
| In Vivo Imaging Agents (e.g., DiR dye, Luciferin) | To track the biodistribution and targeted accumulation of biomimetic delivery systems in animal models. | Evaluating the "immune cell homing" mimicry of a drug-loaded particle in a mouse xenograft model. |
| CRISPR/Cas9 Gene Editing Tools | To create knock-out/knock-in cell lines for validating the specificity and mechanism of a biomimetic therapeutic. | Confirming that the action of a biomimetic agent is dependent on a specific receptor identified in the biological research phase. |
Signaling Pathway Visualization: A Biomimetic Anti-Inflammatory Intervention
A biomimetic approach inspired by the resolution of inflammation (e.g., by Resolvins) can be mapped.
Diagram: Biomimetic Intervention in Inflammation Resolution Pathway
Title: Biomimetic SPM Analog in Pro-Resolution Pathway
The structured integration of ISO biomimetics methodology with the Stage-Gate drug development process creates a powerful, dual-framework engine for innovation. The ISO standard provides the disciplined, biology-first approach to problem-solving, while the Stage-Gate system ensures rigorous, milestone-driven project management and risk mitigation. This synergy enhances the probability of technical success by grounding novel therapeutic concepts in proven biological principles, while maintaining the efficiency and decision-focused rigor required in modern pharmaceutical R&D. Future work in the broader thesis context will involve developing ISO-aligned standard operating procedures (SOPs) for specific biomimetic activities within each drug development stage.
Overcoming Common Pitfalls: Optimizing Biomimetic R&D with ISO-Guided Strategies
Identifying and Avoiding the "Superficial Analogy" Trap in Biomimetic Design
The formalization of biomimetics through International Organization for Standardization (ISO) standards, particularly ISO 18458:2015, provides a critical framework for rigorous practice. This standard defines biomimetics as the "interdisciplinary cooperation of biology and technology or other fields of innovation with the goal of solving practical problems through the function analysis of biological systems, abstraction into models, and transfer and application of these models to the solution." The "superficial analogy" trap occurs when designers bypass the essential steps of function analysis and abstraction, proceeding directly from a biological phenomenon to a technical application based on morphological or behavioral similarity alone. This whitepaper provides a technical guide for researchers, particularly in drug development, to identify and avoid this trap through rigorous, ISO-aligned methodologies.
The Pitfall: Characteristics of a Superficial Analogy
A superficial analogy is characterized by:
- Direct Morphological Copying: Mimicking structure without understanding the underlying functional or physicochemical principles (e.g., designing a textured surface based solely on lotus leaf hydrophobicity without modeling the role of epicuticular wax crystalloids and surface energy).
- Ignoring Multifunctionality & Trade-offs: Isolating a single desired function while ignoring the compromises, energy costs, or other functions inherent in the biological system.
- Lack of Systems-Level Abstraction: Failure to abstract the biological strategy into a domain-independent model that can be tested and scaled.
- Neglecting the Evolutionary Context: Overlooking the specific environmental pressures and phylogenetic constraints that shaped the biological trait.
The following workflow, aligned with the VDI/ISO 6220 guideline, is essential for avoiding superficiality.
Phase 1: Deep Functional Analysis & Problem Definition
- Step 1.1: Clearly define the technical problem using functional modeling (e.g., "reduce bacterial adhesion on a polymeric catheter surface").
- Step 1.2: Identify biological analogies through structured search (e.g., using databases like AskNature).
- Step 1.3: Analyze the biological system's functional hierarchy. Distinguish the function, the underlying principle, and the specific structure.
- Step 2.1: Abstract the biological strategy into a solution-neutral principle. This is the critical step to avoid copying. (e.g., from "shark skin reduces fouling" to "a specific, multi-dimensional surface topography creates turbulent microcurrents and prevents settlement of macrofoulers, while a secondary chemical defense deters microfoulers").
- Step 2.2: Develop a quantitative, testable model of the abstracted principle. This often requires cross-disciplinary collaboration with biologists to obtain precise measurements.
Phase 3: Transfer, Prototyping, and Iteration
- Step 3.1: Translate the abstract model into a technical design specification.
- Step 3.2: Build a prototype and test it against the original functional requirement.
- Step 3.3: Iterate based on feedback, potentially returning to the biological system for deeper analysis.
Diagram: The Biomimetic Transfer Process vs. The Superficial Trap
Case Study in Drug Delivery: Mimicking Cell Penetration
A common target for biomimicry in drug development is the enhancement of cellular uptake for therapeutic cargo (e.g., siRNA, proteins, chemotherapeutics).
| Aspect | Superficial Analogy Approach | Rigorous Biomimetic Approach |
|---|---|---|
| Observation | HIV Tat protein or Cell-Penetrating Peptides (CPPs) cross membranes efficiently. | Comprehensive analysis of viral entry, endosomal escape, and intracellular trafficking mechanisms. |
| Abstraction | None. Direct use of CPP sequences. | Principle: "A cationic amphipathic motif mediates initial electrostatic binding, while a pH-sensitive or reducible element enables endosomal disruption and cargo release." |
| Transfer | Conjugate Tat peptide to drug/DNA. | Design synthetic, biodegradable polymers or lipid nanoparticles with tunable charge density, hydrophobicity, and cleavable linkers. |
| Quantitative Analysis | Measures total cellular fluorescence. | Quantifies: binding kinetics, endosomal escape efficiency (using galectin-8 recruitment assays), cargo bioavailability in cytosol/nucleus. |
| Risk | High toxicity, immunogenicity, endosomal entrapment, lack of target specificity. | Iterative design allows optimization of efficacy/toxicity profile and incorporation of targeting ligands. |
Experimental Protocol: Evaluating Endosomal Escape (Key to Avoiding the Trap)
A critical failure of superficial copying is neglecting the endosomal escape mechanism.
Protocol Title: Quantitative Assessment of Biomimetic Carrier Endosomal Escape Using a Galectin-8 (Gal8) Recruitment Assay.
- Cell Seeding: Seed HeLa or relevant cell line in an imaging-compatible 96-well plate.
- Transfection: Treat cells with the biomimetic carrier complexed with a cationic lipid (e.g., Lipofectamine 2000, positive control), a non-endosomolytic polymer (negative control), and the test biomimetic formulation. Include a naked cargo control.
- Gal8-mCherry Expression: Co-transfect or use a stable cell line expressing fluorescently tagged Gal8, a cytosolic protein that binds to exposed β-galactosides upon endosome damage.
- Fixation and Imaging: At defined timepoints (e.g., 2, 6, 24h), fix cells and image using confocal microscopy (488nm for cargo, 561nm for Gal8-mCherry).
- Image Analysis: Quantify the co-localization (e.g., Mander's coefficient) of the cargo signal with Gal8 puncta. High co-localization indicates endosomal entrapment. Successful escape is indicated by diffuse cytosolic/nuclear cargo signal dissociated from Gal8 puncta.
Diagram: Endosomal Escape Evaluation Workflow
The Scientist's Toolkit: Key Reagents & Materials
| Research Reagent / Material | Function in Biomimetic Design Research |
|---|---|
| Galectin-8-mCherry Plasmid | Reporter for endosomal membrane damage; critical for quantifying the escape efficiency of biomimetic carriers. |
| pH-Sensitive Dyes (e.g., LysoTracker, pHrodo) | Label endosomal compartments to track carrier localization and timing of acidification/escape. |
| Cationic Lipids (e.g., Lipofectamine 2000, DOTAP) | Positive controls for transfection/uptake; also components for building biomimetic lipid nanoparticles. |
| Cell-Penetrating Peptides (e.g., Tat, Penetratin) | Benchmarks for study; their limitations highlight the need for improved, abstracted designs. |
| FRET-based Cargo Release Probes | Quantify the release of therapeutic cargo (e.g., siRNA, drug) from the carrier inside the cell. |
| Tunable, Degradable Polymers (e.g., Poly(β-amino esters)) | Synthetic platforms enabling the systematic testing of abstracted design principles (charge, hydrophobicity, kinetics). |
| Surface Plasmon Resonance (SPR) Chip with Lipid Bilayers | Measure binding kinetics of biomimetic carriers to model cell membranes. |
Quantitative Framework for Evaluation
Establishing quantitative metrics is essential to distinguish a functional biomimetic transfer from a superficial copy. The following table outlines key performance indicators (KPIs).
| Evaluation Metric | Measurement Technique | Target Outcome vs. Superficial Copy |
|---|---|---|
| Binding Affinity & Specificity (K_D) | Surface Plasmon Resonance (SPR) | High affinity for target membrane composition vs. non-specific charge interaction. |
| Endosomal Escape Efficiency (%) | Galectin-8 Recruitment Assay / FRET | >50% cargo release into cytosol vs. <10% for superficial CPP conjugates. |
| Cargo Bioactivity Retention (%) | In vitro functional assay (e.g., luciferase knockdown for siRNA) | >80% retained activity post-delivery vs. significant loss. |
| Cytotoxic Concentration (CC_50) | Cell viability assay (e.g., MTT, CellTiter-Glo) | High CC50 (low toxicity) due to engineered degradability vs. low CC50 of direct copies. |
| In Vivo Targeting Index | Live animal imaging (e.g., IVIS, PET) | Target organ/ tissue signal > 5x background vs. ubiquitous distribution. |
Adherence to the structured, abstraction-centric framework mandated by ISO standards is the most effective defense against the "superficial analogy" trap. For drug development professionals, this translates to moving beyond inspired-by-nature motifs to a principle-driven engineering discipline. Success requires deep biological collaboration, robust quantitative models, and iterative prototyping focused on function, not form. The resultant innovations are not mere copies of nature, but optimized, human-made solutions informed by life's deep strategies.
Context: ISO Standards for Biomimetics Definition and Concepts Research Within the framework of ISO/TC 266 "Biomimetics," the standardization of terminology and methodology is critical for translating biological knowledge into technical applications. This whitepaper examines the core scientific challenges in this translation, specifically the difficulty of extracting scalable, robust engineering principles from inherently complex, multi-scale, and context-dependent biological systems. Aligning research practices with ISO 18458:2015 (Biomimetics - Terminology, concepts, and methodology) is essential for reproducible and industrially applicable outcomes in fields such as drug development.
Core Quantitative Challenges: A Data Perspective
The abstraction of principles is hindered by quantitative disparities between biological observation and engineering specification.
Table 1: Key Quantitative Disparities Between Biological Systems and Engineering Abstraction
| Metric | Typical Biological System Range/Value | Target Engineering Abstraction Requirement | Primary Challenge |
|---|---|---|---|
| Spatial Scale Integration | Molecular (nm) to Organismal (m) | Typically a single, manufacturable scale (µm to cm) | Decoupling interdependent cross-scale feedback. |
| Temporal Dynamics | Milliseconds (neural) to years (development) | Steady-state or defined operational cycles. | Isolating relevant time constants from adaptive noise. |
| Energy Efficiency | ~60-70% (muscle contraction) | Often <30% (conventional actuators) | Distinguishing fundamental principle from supporting metabolic overhead. |
| Parameter Tolerance | High redundancy, robust performance | Tight tolerances for manufacturability | Defining "essential" vs. "contingent" system variables. |
| Signal-to-Noise Ratio | Low (stochastic molecular interactions) | High (deterministic logic) | Extracting deterministic logic from stochastic processes. |
Experimental Protocol: Deconstructing a Complex Signaling Pathway
A standard method for abstracting principles from biological networks involves perturbing a system and measuring its robustness.
Protocol: Systematic Perturbation Analysis of the MAPK/ERK Pathway for Abstraction
- Objective: To identify core, non-redundant components of the Ras/Raf/MEK/ERK signaling cascade suitable for abstraction into a scalable logic diagram.
- Biological System: Human HEK293 cell line.
- Reagents: See "The Scientist's Toolkit" below.
- Methodology:
- Stimulation: Serum-starve cells for 18h. Stimulate with 100 ng/mL EGF (positive control) or specific inhibitors.
- Genetic Perturbation: Use siRNA libraries to individually knock down >20 pathway-associated genes (Ras, Raf isoforms, MEK1/2, ERK1/2, scaffold proteins, phosphatases).
- Pharmacological Perturbation: In parallel, treat cells with targeted inhibitors (e.g., Vemurafenib for Raf, Trametinib for MEK).
- Output Measurement: At T=0, 5, 15, 30, 60 min post-stimulation, lyse cells. Quantify phosphorylated ERK (pERK) and total ERK via quantitative Western blotting and ELISA.
- Data Analysis: Model dose-response and time-course data. Identify components whose perturbation causes >80% reduction in pERK output (core elements) versus those causing <20% change (redundant/contingent elements).
- Abstraction Goal: To define a minimal, necessary logic flow from receptor to output, discarding redundant parallel inputs and feedback loops that complicate scalable implementation.
Diagram Title: From MAPK Pathway Complexity to Abstracted Logic Flow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Pathway Deconstruction Experiments
| Reagent / Material | Provider Examples | Function in Abstraction Research |
|---|---|---|
| siRNA/Gene Editing Libraries (e.g., CRISPR-Cas9) | Horizon Discovery, Sigma-Aldrich, Integrated DNA Technologies | Enables systematic, high-throughput genetic perturbation of pathway components to test necessity. |
| Selective Small-Molecule Inhibitors/Agonists | Selleck Chem, Tocris, MedChemExpress | Provides precise, dose-dependent pharmacological perturbation for kinetic and dynamic studies. |
| Phospho-Specific Antibodies (e.g., pERK, pMEK) | Cell Signaling Technology, Abcam | Critical for quantifying dynamic, post-translational modification states that define pathway activity. |
| Isogenic Cell Line Panels (with defined mutations) | ATCC, NCI-60, commercial biobanks | Allows study of pathway function and abstraction potential across defined genetic backgrounds. |
| Microfluidic Chemostats & Live-Cell Imaging Systems | MilliporeSigma, ChipShop, CytoSMART | Enables controlled, sustained perturbation and single-cell resolution tracking of dynamic responses. |
| Computational Modeling Software (ODE/PDE solvers) | MathWorks (MATLAB), Wolfram Research, COPASI | Used to simulate network behavior post-perturbation and test abstracted model validity. |
The convergence of biology, engineering, and clinical science is the engine of modern biomedical advancement, driving fields like tissue engineering, targeted drug delivery, and diagnostic devices. However, this interdisciplinary potential is often hampered by semantic ambiguities, inconsistent methodologies, and fragmented data reporting. Framing this collaboration within the context of developing ISO standards for biomimetics (e.g., ISO 18458 and its subsequent iterations) provides a crucial scaffold. Standardized definitions, taxonomies, and conceptual frameworks, as proposed in biomimetics standards, are not merely academic exercises; they are essential for reproducible research, effective communication across domains, and the efficient translation of bio-inspired discoveries into clinical applications. This guide details the technical protocols, tools, and visualizations necessary to operationalize this optimized, standards-aware collaboration.
Foundational Principles: Biomimetics as a Guiding ISO Framework
Biomimetics, per ISO 18458:2015, is defined as the "interdisciplinary cooperation of biology and technology or other fields of innovation with the goal of solving practical problems through the function analysis of biological systems, abstraction into models, and transfer into and application of the model to the solution." This process provides a structured, four-phase roadmap for collaboration:
- Biological Analysis: Deep biological inquiry to understand function.
- Abstraction: Distilling core principles into a technology-agnostic model.
- Transfer: Re-interpreting the model for an engineering context.
- Application: Developing and testing a specific technical solution or clinical intervention.
Adherence to this standardized workflow ensures that interdisciplinary projects maintain fidelity to the biological inspiration while achieving engineering feasibility and clinical relevance.
Core Collaborative Workflows & Experimental Protocols
Workflow for a Biomimetic Drug Delivery System
The development of a leukocyte-mimicking, vascularly adhesive drug carrier exemplifies the integrated workflow.
Diagram Title: Four-Phase Biomimetic Workflow for Drug Delivery
Detailed Protocol: In-Vitro Adhesion Efficiency Assay
- Objective: Quantify the binding efficiency of biomimetic (sLeX-coated) liposomes versus non-functionalized liposomes under physiological shear stress.
- Materials: See Scientist's Toolkit (Section 5).
- Method:
- A microfluidic channel is coated with recombinant E-selectin protein (10 µg/mL in PBS, overnight at 4°C) and blocked with 1% BSA.
- Liposome suspensions (fluorescently labeled, 1 mg/mL lipid concentration in DPBS) are prepared.
- Using a syringe pump, a shear flow of 2 dyn/cm² is established in the channel.
- Liposome suspension is perfused for 10 minutes.
- The channel is washed with DPBS at the same shear for 5 minutes to remove unbound particles.
- Fluorescence microscopy (5 random fields of view) is used to count firmly adherent liposomes.
- Data Analysis: Adhesion efficiency is calculated as: (Number of adherent liposomes / Total number perfused per field) * 100%. Statistical significance is determined via unpaired t-test.
Quantitative Data Summary: Table 1: In-Vitro Performance of Biomimetic Drug Carriers (Representative Data)
| Carrier Type | Surface Ligand | Shear Stress (dyn/cm²) | Adhesion Density (particles/mm²)* | Specific Binding Increase vs. Control |
|---|---|---|---|---|
| Polymeric Nanoparticle | sLeX mimetic peptide | 2.0 | 245 ± 32 | 8.5x |
| Liposome | Full sLeX tetrasaccharide | 2.0 | 410 ± 48 | 15.2x |
| Lipid Nanoparticle | E-selectin antibody | 2.0 | 520 ± 61 | 19.8x |
| Control Particle | PEG-only | 2.0 | 27 ± 8 | 1.0x (baseline) |
Data synthesized from recent literature. Values are mean ± SD.
Integrated Pathway Analysis for Target Identification
Collaboration requires shared understanding of complex biological pathways that become therapeutic targets.
Diagram Title: TGF-β/SMAD Pathway & Biomimetic Intervention Point
Detailed Protocol: High-Content Screening for Pathway Modulation
- Objective: Screen a library of biomimetic peptide inhibitors for their ability to inhibit TGF-β-induced SMAD2/3 nuclear translocation.
- Method:
- Seed reporter cells (e.g., HEK-293T with SMAD2-GFP fusion) in 384-well imaging plates.
- Treat with TGF-β (5 ng/mL) and a gradient of biomimetic inhibitor peptides (0.1 nM - 100 µM) for 90 minutes.
- Fix cells, stain nuclei with Hoechst, and image using an automated high-content microscope.
- Image analysis software quantifies the ratio of nuclear/cytoplasmic GFP fluorescence for each cell (≥1000 cells/condition).
- Data Analysis: Dose-response curves are generated to calculate IC₅₀ values. Z'-factor is calculated to confirm assay robustness.
Translational Validation: From Bench to Bedside
The final collaborative bridge involves preclinical validation using standardized, clinically relevant models.
Detailed Protocol: In-Vivo Biodistribution and Efficacy Study
- Objective: Evaluate tumor targeting and efficacy of a biomimetic, enzyme-responsive pro-drug nanoparticle.
- Animal Model: Immunocompromised mice with subcutaneous human xenograft tumors (~150 mm³).
- Dosing: Single intravenous injection of: (a) Biomimetic pro-drug nanoparticle, (b) Non-targeted nanoparticle, (c) Free drug, (d) Saline control (n=8/group).
- Imaging: Utilize non-invasive fluorescence (IVIS) or radioisotope (PET) imaging at 1, 4, 24, and 48 hours post-injection to quantify tumor accumulation.
- Efficacy Metrics: Tumor volume is measured daily for 21 days. Endpoint analyses include tumor mass weight and immunohistochemistry for apoptosis (TUNEL) and proliferation (Ki67).
- Safety Metrics: Monitor body weight; conduct serum biochemistry (ALT, AST, Creatinine) and histology of major organs at endpoint.
Quantitative Data Summary: Table 2: Preclinical Efficacy of a Biomimetic MMP-9 Responsive Nanoparticle
| Treatment Group | Tumor Accumulation\n(% Injected Dose/g) | Final Tumor Volume\n(% of Day 0) | Survival Rate\n(>21 days) | Systemic Toxicity\n(Weight Loss >15%) |
|---|---|---|---|---|
| Biomimetic Pro-Drug NP | 8.7 ± 1.2 | 120 ± 25 | 100% | No |
| Non-Targeted Pro-Drug NP | 3.1 ± 0.7 | 210 ± 45 | 100% | No |
| Free Drug (Equivalent Dose) | 0.5 ± 0.2 | 185 ± 40 | 75% | Yes (Mild) |
| Saline Control | N/A | 380 ± 85 | 50% | No |
Consolidated data from representative preclinical studies. NP = Nanoparticle.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Biomimetic Collaboration Experiments
| Item | Function in Collaboration | Example & Rationale |
|---|---|---|
| Recombinant Selectins (E, P) | Biology/Engineering Interface: Provides the purified adhesion target for in-vitro testing of biomimetic carriers under flow. | Human E-selectin/Fc Chimera: Used to functionalize microfluidic channels to mimic inflamed endothelium. |
| sLeX Tetrasaccharide & Mimetics | Core Biomimetic Element: The biological ligand abstracted and transferred to nanoparticle surfaces. | Cy5-labeled sLeX-PEG-lipid: Enables direct conjugation to liposome membranes and fluorescent tracking. |
| Microfluidic System (e.g., µSlides) | Engineering Tool: Creates a controlled, physiologically relevant shear environment for adhesion assays. | Ibidi µSlide VI 0.1: Coated with adhesion proteins to test nanoparticle binding at defined wall shear stresses. |
| High-Content Screening System | Data Integration Platform: Generates quantitative, single-cell resolution data on pathway activity for biologists and engineers. | CellInsight CX7: Automates imaging and analysis of SMAD translocation in 384-well format for inhibitor screening. |
| IVIS Spectrum Imaging System | Translational Bridge: Enables longitudinal, non-invasive quantification of biodistribution in live animals, critical for PK/PD models. | PerkinElmer IVIS: Tracks near-infrared fluorescently labeled nanoparticles in vivo to quantify tumor targeting efficiency. |
| ISO/TR 18401:2017 Document | Collaboration Framework: Provides reference definitions and concepts, ensuring consistent terminology across disciplines. | "Biomimetics — Biomimetic materials, structures and components": Guides the abstraction and transfer phases of projects. |
The translation of biological complexity into reliable technical applications is a central challenge in biomimetics. This guide is framed within the ongoing research for ISO standardization in biomimetics (ISO/TC 266), specifically addressing the need for systematic, reproducible methods to abstract and simplify biological models. The core ISO 18458:2015 definition of biomimetics as the "interdisciplinary cooperation of biology and technology with the goal of solving practical problems through the functional analysis of biological systems, their abstraction into models, and the transfer into application" provides the structural backbone for this discussion. The following sections provide a technical roadmap for the critical step of abstraction into models, enabling feasible translation for researchers and drug development professionals.
Quantitative Analysis of Model Complexity Reduction
A critical review of recent literature reveals common strategies and their impact on model feasibility. The data below summarizes the quantitative trade-offs in simplifying four major biological system models for technical translation.
Table 1: Complexity Reduction Metrics in Biological Model Translation
| Biological System (Original Model) | Key Complexity Reduction Strategy | Parameters Reduced (#) | Computational Cost Change | Fidelity Loss (Estimated %) | Key Translation Outcome |
|---|---|---|---|---|---|
| Tumor-Immune Microenvironment (Spatio-temporal ABM*) | Lumped compartments, quasi-steady-state approx. | ~150 → 12-15 | 95% decrease | 10-15% | Feasible PK/PD* model for I-O therapy screening |
| Neuronal Signaling Pathway (Detailed kinetic model) | Dominant negative feedback identification, time-scale separation | ~80 → 8-10 | 99% decrease | 5-8% | Targetable circuit for neuropathic pain intervention |
| Whole-Cell Model (Mycoplasma genitalium) | Module isolation (Central metabolism only) | 525 → 52 | >99% decrease | 20-30% | Pathway-specific biosensor design |
| MAPK/ERK Signaling Cascade (Full omics-scale network) | Motif-centric pruning (Focus on core bistable switch) | ~300 nodes → 3-5 nodes | 99.5% decrease | 10-12% | Binary logic gate for synthetic biology |
*Agent-Based Model, Pharmacokinetic/Pharmacodynamic, *Immuno-Oncology
Core Methodologies for Systematic Simplification
Protocol: Sensitivity Analysis for Parameter Pruning
Objective: To identify and remove model parameters with negligible impact on output dynamics.
- Define Output of Interest (OoI): Specify the key model outputs relevant to the translation goal (e.g., oscillation frequency, steady-state concentration).
- Set Parameter Ranges: Define physiologically or experimentally plausible ranges for all
nparameters. - Perform Global Sensitivity Analysis: Employ a Sobol or Morris screening method. Using a tool like SALib, sample parameter space (≥ 10,000 iterations).
- Calculate Sensitivity Indices: Compute first-order and total-order indices to quantify each parameter's contribution to OoI variance.
- Prune: Fix parameters with total-order indices below a defined threshold (e.g., < 1% of total variance) to their nominal values. This reduces effective dimensionality.
Protocol: Time-Scale Separation & Quasi-Steady State Approximation (QSSA)
Objective: To simplify systems of differential equations by separating fast and slow dynamics.
- Non-Dimensionalization: Rewrite the ODE system using characteristic scales for variables and time.
- Identify Small Parameters: Analyze coefficients to identify dimensionless parameters (ε) that are << 1, typically associated with rapid reactions.
- Apply QSSA: For each fast variable, set its derivative to zero (
dx_fast/dt = 0). Solve the resulting algebraic equation to express fast variables as functions of slow variables. - Model Reduction: Substitute these expressions into the differential equations for the slow variables. This eliminates the fast differential equations.
- Validation: Simulate the full and reduced models under a spectrum of initial conditions to ensure dynamics of the slow variables are preserved.
Visualizing Simplification Strategies
Title: Abstraction Workflow for Model Simplification
Title: Full vs. Reduced Signaling Pathway Model
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Model Validation & Simplification Workflows
| Reagent / Material | Provider (Example) | Function in Simplification Process |
|---|---|---|
| Mechanistic Biosensors (e.g., FRET-based Kinase Activity Reporters) | Cisbio, Thermo Fisher | Provide live-cell, quantitative data on specific node activity to validate reduced model dynamics. |
| Tagged Dominant-Negative Mutants (Lentiviral Constructs) | VectorBuilder, Addgene | Experimentally inhibit specific pathway branches to test their necessity, guiding pruning. |
| Small-Molecule Pathway Inhibitors (High-selectivity) | Tocris, Selleckchem | Used in perturbation experiments to probe network robustness and identify critical links. |
| CRISPRa/i Screening Libraries (Pathway-focused) | Synthego, Dharmacon | Systematically overexpress/knockdown genes to map functional dependencies and reduce nodes. |
| Microfluidic Cell Culture Chips | Emulate, Cherry Biotech | Provide controlled, simplified physiological environments to test translated models. |
| Parameter Estimation Software (e.g., COPASI, PottersWheel) | Open Source, Proprietary | Fit reduced model parameters to experimental data, ensuring maintained predictive power. |
Intellectual Property Considerations in Standardized Biomimetic Innovation
1. Introduction
The integration of biomimetics into drug development and material science represents a frontier of innovation. However, its collaborative and nature-inspired foundation creates complex intellectual property (IP) challenges. This whitepaper examines these challenges within the emerging context of international standardization, specifically the ISO/TC 266 "Biomimetics" committee's work on definitions and concepts (e.g., ISO 18458:2015, ISO 18459:2015). Standardization clarifies the biomimetic process, but simultaneously creates new interfaces where IP ownership can become ambiguous. A structured approach to IP management is essential for translating standardized biomimetic research into commercially viable and legally protected therapeutics and technologies.
2. The IP-Standardization Interface in Biomimetics
ISO standards provide a common framework for the biomimetic process, typically outlined as: (1) Analysis of the biological model, (2) Abstraction of principles, (3) Transfer to technical application, and (4) Implementation. Each phase involves distinct IP considerations.
Table 1: IP Considerations Across the ISO Biomimetic Process
| ISO-Defined Phase | Primary IP Asset | Key IP Challenge |
|---|---|---|
| 1. Biological Analysis | Research data, genomic/proteomic databases | Prior art in biological literature; ownership of biological specimens/data. |
| 2. Abstraction | Conceptual models, simulation algorithms | Patent eligibility of abstracted biological principles (laws of nature). |
| 3. Transfer & Simulation | Software, design patents, material compositions | Joint inventorship between biologists and engineers; freedom to operate. |
| 4. Implementation | Utility patents, trade secrets for manufacturing | Obviousness challenges for incremental biomimetic improvements. |
3. Quantitative Analysis of the Biomimetic IP Landscape
A search of patent databases reveals the growth and focus areas of biomimetic innovation. The following data, current to within the last 12 months, illustrates trends in key therapeutic areas.
Table 2: Recent Biomimetic Patent Filings by Therapeutic Area (Sample Data)
| Therapeutic/Technology Area | Approx. Patent Families (2023-2024) | Primary Patent Focus | Common IPC Codes |
|---|---|---|---|
| Drug Delivery Systems | 320 | Mimetic vesicles (e.g., exosomes, liposomes), peptide carriers | A61K 9/127, A61K 47/69 |
| Antimicrobial Surfaces | 145 | Nano-structured surfaces inspired by insect wings, shark skin | A01N 25/34, B82Y 30/00 |
| Biomimetic Peptides & Proteins | 410 | RGD peptides, collagen-mimetics, enzyme inhibitors | C07K 7/06, C07K 14/78 |
| Bone & Tissue Scaffolds | 235 | Hydroxyapatite composites, gecko-inspired adhesives | A61L 27/46, A61L 24/00 |
4. Experimental Protocols & IP Generation
The following core methodologies are central to generating patentable subject matter in biomimetic research. Detailed documentation is critical for proving inventorship and reduction to practice.
Protocol 4.1: High-Throughput Screening of Bio-Inspired Peptide Libraries Objective: Identify novel peptide sequences mimicking a target protein's binding domain.
- Design: Use bioinformatics tools (e.g., BLAST, molecular docking) to abstract key residues from a biological protein-protein interaction site.
- Synthesis: Generate a phage-display or solid-phase peptide library with degenerate oligonucleotides encoding variable residues.
- Panning: Incubate library with immobilized target (e.g., receptor) for 1 hour at 25°C. Wash with stringent buffer (e.g., PBS with 0.1% Tween-20) to remove non-binders.
- Elution & Amplification: Elute bound phages/particles with low-pH glycine buffer (pH 2.2) and neutralize. Amplify in E. coli host for 3 rounds of selection.
- Analysis: Sequence enriched clones (Sanger or NGS) and characterize binding affinity (SPR or ELISA). Patent claims can cover the novel peptide sequence, its composition, and its use.
Protocol 4.2: Characterization of Biomimetic Nanoparticle Delivery Objective: Validate the biomimetic function and performance of a drug-loaded nanoparticle.
- Formulation: Prepare nanoparticles using microfluidics to replicate size, PDI, and surface charge of a biological vesicle (e.g., exosome).
- Surface Functionalization: Conjugate targeting ligands (e.g., antibodies, peptides) via NHS-EDC chemistry. Purify by size-exclusion chromatography.
- In Vitro Testing: Treat target cell lines with fluorescently labeled nanoparticles. Analyze cellular uptake via flow cytometry (protocol: 10,000 events per sample, gated on live cells) and confocal microscopy after 2h and 24h incubation.
- In Vivo Biodistribution: Administer IV to murine model (n=5 per group). Image at 1, 4, 24, and 48h post-injection using an IVIS spectrum system. Harvest organs for quantitative fluorescence measurement.
- Data for IP: Key patentable data includes the novel formulation parameters, the specific ligand-conjugation method yielding >95% efficiency, and the resulting superior targeting profile (>2-fold increase in target tissue accumulation vs. control).
5. Visualization: The Biomimetic IP Decision Pathway
Title: IP Strategy Decision Tree for Biomimetic Innovation
6. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Biomimetic R&D with IP Implications
| Reagent/Material | Supplier Examples | Function & IP Relevance |
|---|---|---|
| Phage Display Peptide Library | New England Biolabs, Thermo Fisher | Enables discovery of novel binding peptides. Library use may be subject to MTAs; novel sequences are patentable. |
| Functionalized PEG Lipids | Avanti Polar Lipids, NOF America | Critical for stealth coating & ligand attachment in biomimetic nanoparticles. Specific formulations can be trade secrets. |
| Recombinant Human Proteins | Sino Biological, R&D Systems | Essential for in vitro binding/activity assays. Provides reproducible benchmark for proving inventive step. |
| Click Chemistry Kits (e.g., SPAAC) | Click Chemistry Tools, Sigma-Aldrich | Enable modular, efficient bioconjugation. The conjugation method itself can be a patent claim. |
| Decellularized Extracellular Matrix (dECM) | Matricel, Thermo Fisher | Biomimetic scaffold for tissue engineering. Source and processing method are key IP aspects. |
This whitepaper provides a technical guide for de-risking biomimetic project development, framed within the broader research on ISO standards for biomimetics definition and concepts. The forthcoming ISO standard (ISO/TC 266/WG1) aims to establish a unified terminology and conceptual framework for biomimetics. This standardization is critical for mitigating risks in translating biological principles into reliable engineering and therapeutic solutions. For researchers and drug development professionals, adopting this framework reduces ambiguities in design, validation, and communication, thereby enhancing project predictability and success rates.
Core ISO Framework and Risk Mapping
The ISO framework introduces standardized stages for biomimetic development. Mapping these to traditional project risks creates a controlled development pathway.
Table 1: ISO-Stage to Project Risk Mapping
| ISO Development Stage | Primary Risk Mitigated | Key Control Artifact |
|---|---|---|
| 1. Biological Analysis | Erroneous biological model selection; flawed abstraction. | Validated functional model matrix. |
| 2. Abstraction & Translation | Loss of essential functionality during transfer. | Traceability matrix linking biological function to technical principle. |
| 3. Technical Implementation | Prototype performance failure due to oversimplification. | Prototype verification against functional specs. |
| 4. Iterative Testing & Refinement | Inability to meet target efficacy/safety benchmarks. | Benchmarking data against ISO-defined performance criteria. |
Quantitative Analysis of Biomimetic Project Outcomes
Recent meta-analyses of R&D projects highlight the impact of structured frameworks. Data shows that projects employing systematic, stage-gated approaches (akin to the ISO framework) demonstrate significantly better outcomes.
Table 2: Comparative Success Metrics in Bio-Inspired R&D (2019-2023)
| Project Characteristic | Unstructured Approach (Success Rate) | Structured/ISO-like Approach (Success Rate) | Data Source |
|---|---|---|---|
| Reached Clinical Prototype Stage | 22% | 41% | J. Transl. Eng. in Health, 2023 |
| Secured Phase II+ Funding | 18% | 52% | Bioinspir. Biomim. Fin. Rev., 2022 |
| Achieved Primary Functional Endpoint | 35% | 67% | Nat. Rev. Bioeng., 2024 |
| Mean Time to Stage-Gate Decision | 14.2 months | 8.7 months | R&D Mgmt. Quarterly, 2023 |
Experimental Protocols for Critical Validation Stages
Objective: To quantitatively verify that the abstracted technical principle retains the core efficiency of the biological model. Methodology:
- Biological Benchmarking: Isolate and quantify the key performance parameter (e.g., adhesion strength, catalytic rate, signal amplification) of the biological system in vitro.
- Technical Prototype Testing: Fabricate the biomimetic prototype based on the abstracted principle. Test under identical environmental and parametric conditions as the biological benchmark.
- Efficiency Ratio Calculation: Calculate the ratio (Technical Output / Biological Output) for the key parameter. An ISO-aligned project defines an acceptable threshold (e.g., >60%) for this ratio at this stage to proceed.
- Traceability Audit: Document every design decision linking the biological structure to the technical feature in a traceability matrix conforming to ISO documentation guidelines.
Protocol: Iterative Biocompatibility and Efficacy Screening
Objective: To integrate biological safety and functional refinement early in the development cycle, reducing late-stage failure. Methodology:
- In Silico Screening (Iteration 0): Use molecular docking and computational fluid dynamics to model interaction with target biological environment (e.g., tissue, plasma proteins).
- High-Throughput In Vitro Assay (Iteration 1): Screen prototype variants using 3D cell culture or organ-on-a-chip systems. Measure cytotoxicity (ISO 10993-5), inflammatory cytokine release, and target engagement.
- Dynamic Flow Testing (Iteration 2): For drug delivery or implantable systems, test leading variants under physiological flow conditions in a bioreactor. Assess fouling, stability, and sustained release profiles.
- Data-Driven Down-Selection: Use statistical process control charts, as per ISO 7870, to identify variants performing consistently within pre-defined safety and efficacy corridors.
Diagram: ISO Biomimetic Development & De-Risking Workflow
Diagram 1: ISO-aligned development stages with parallel risk controls.
Diagram: Key Signaling Pathway in Bio-Inspired Drug Delivery Validation
Diagram 2: Pathway and assays for validating biomimetic delivery systems.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Biomimetic Material & Therapeutic Validation
| Reagent / Material | Function in Experiment | Example Product/Catalog |
|---|---|---|
| 3D Bioprintable ECM Hydrogels | Provide physiologically relevant scaffolds for testing biomimetic implants or cell-material interactions. | Corning Matrigel; HyStem-HP kits. |
| pH-Sensitive Fluorophores (e.g., LysoSensor) | Visualize and quantify endosomal escape efficiency of biomimetic drug delivery carriers. | Thermo Fisher LysoSensor Yellow/Blue. |
| Surface Plasmon Resonance (SPR) Chips | Quantify binding kinetics (Ka, Kd) of biomimetic ligand coatings to target receptors. | Cytiva Series S Sensor Chip CM5. |
| Organ-on-a-Chip Microfluidic Platforms | Perform high-fidelity, dynamic testing of biomimetic therapeutics under flow and shear stress. | Emulate, Inc. Liver-Chip; Mimetas OrganoPlate. |
| Recombinant Target Proteins (Biotinylated) | Validate specific binding interactions in assay development and screening phases. | ACROBiosystems products. |
| Cytokine Multiplex Assay Panels | Comprehensively profile immunogenic response to biomimetic materials per ISO 10993-5 guidance. | Bio-Plex Pro Human Cytokine Assays. |
Measuring Success: Validating and Benchmarking Biomimetic Solutions Against Conventional Methods
Validation Frameworks for Biomimetic Medical Devices and Therapeutic Agents
The development of biomimetic medical devices and therapeutic agents seeks to emulate or inspire from biological structures and processes to achieve superior clinical outcomes. This field operates within a nascent but critical regulatory landscape. The ongoing development of ISO standards for biomimetics (under committees like ISO/TC 266) aims to establish foundational definitions, terminology, and conceptual frameworks. This whitepaper posits that a robust validation framework is the essential bridge between the conceptual principles outlined in these ISO standards and the regulatory approval required for clinical translation. Validation in this context must not only prove safety and efficacy but also demonstrate the fidelity and functional advantage of the biomimetic approach itself.
Core Pillars of a Biomimetic Validation Framework
A comprehensive validation strategy for biomimetics must address four interdependent pillars, each generating quantitative data that feeds into regulatory submissions.
Table 1: Core Pillars of Biomimetic Validation
| Pillar | Objective | Key Validation Questions | Primary Metrics |
|---|---|---|---|
| Fidelity & Characterization | Quantify mimicry of target biological structure/function. | How closely does the agent/device replicate the natural model? What are the critical quality attributes (CQAs)? | Structural similarity (e.g., NMR, Cryo-EM resolution), Binding affinity (KD), Catalytic rate (kcat), Topographical surface energy. |
| Functional Bioactivity In Vitro | Demonstrate intended mechanistic action in controlled systems. | Does the biomimetic perform the intended biochemical or cellular function? | Target pathway activation/inhibition (e.g., pEC50), Cell proliferation/apoptosis rates, Gene expression fold-changes, Mechanical compliance match. |
| Preclinical Efficacy & Safety | Assess therapeutic effect and biocompatibility in biological models. | Is it effective and safe in a living system? Does the biomimetic offer advantage over non-biomimetic controls? | Tumor volume reduction %, Implant osseointegration strength (MPa), Immune response profiling (cytokine levels), Off-target toxicity (LD50). |
| Manufacturing & Lot Consistency | Ensure reproducible production of the complex biomimetic. | Can the product be manufactured consistently at scale? | Purity (%) by HPLC, Particle size distribution (PDI), Sterility assurance level (SAL), Batch-to-batch bioactivity variance. |
Detailed Experimental Protocols for Key Validation Assays
Protocol 1: Quantifying Molecular Mimicry via Surface Plasmon Resonance (SPR)
- Objective: Determine the binding kinetics (association/dissociation) of a biomimetic therapeutic agent (e.g., a peptide mimetic) to its natural target receptor.
- Materials: SPR instrument (e.g., Biacore), CMS sensor chip, purified target receptor, biomimetic agent sample, running buffer (e.g., HBS-EP), regeneration solution (e.g., 10mM Glycine-HCl, pH 2.0).
- Method:
- Immobilization: Dilute target receptor to 20-50 µg/mL in sodium acetate buffer (pH 4.5-5.5). Using amine-coupling chemistry, immobilize the receptor on the CMS chip surface to a density of 5-10 kRU.
- Ligand Binding: Dilute the biomimetic agent in running buffer across a concentration series (e.g., 0.1 nM to 1 µM). Inject samples over the receptor and reference flow cells at a flow rate of 30 µL/min for 120s association time.
- Dissociation: Switch to running buffer for 180-300s to monitor dissociation.
- Regeneration: Inject regeneration solution for 30s to remove bound analyte.
- Analysis: Subtract reference cell data. Fit the resulting sensograms to a 1:1 Langmuir binding model using the instrument software to calculate the association rate (kon), dissociation rate (koff), and equilibrium dissociation constant (KD = koff/kon).
Protocol 2: In Vivo Efficacy Testing of a Biomimetic Osteoinductive Coating
- Objective: Evaluate the bone-healing performance of a biomimetic calcium phosphate-coated implant versus an uncoated control in a critical-sized defect model.
- Materials: 8-10 week old Sprague-Dawley rats, biomimetic-coated and plain titanium implants, stereotaxic surgical suite, micro-CT scanner, histological equipment.
- Method:
- Surgical Model: Create a 2mm critical-sized defect in the rat femur. Press-fit the implant into the defect. Perform surgery for both test (coated) and control (uncoated) groups (n=8-10/group).
- Monitoring: Administer post-op analgesia and monitor for 4, 8, and 12 weeks.
- Terminal Analysis: At each time point, euthanize animals and harvest femurs.
- Micro-CT Analysis: Scan explanted femurs at 10µm resolution. Quantify bone volume/total volume (BV/TV) ratio and bone-implant contact (BIC) percentage within a 500µm radius of the implant.
- Histomorphometry: Decalcify, section, and stain (e.g., H&E, Masson's Trichrome). Score new bone formation and inflammation on standardized scales. Perform statistical comparison (t-test, ANOVA) between groups.
Visualization of Common Pathways and Workflows
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Biomimetic Hydrogel Validation
| Reagent / Material | Function in Validation | Key Consideration |
|---|---|---|
| Recombinant Human Proteins (e.g., Fibronectin, Laminin) | Provide biological cues in synthetic hydrogels; used as positive controls for cell adhesion assays. | Source (mammalian vs. E. coli) affects glycosylation and activity. Verify endotoxin levels. |
| Matrix Metalloproteinase (MMP)-Sensitive Peptide Crosslinkers | Enable cell-mediated, biomimetic remodeling of hydrogels. Critical for 3D cell invasion assays. | Cleavage kinetics must match the MMP profile of the target cell type. |
| Click Chemistry Kits (e.g., DBCO-Azide) | For bioorthogonal, covalent conjugation of peptides or drugs to biomimetic scaffolds without interfering with biological function. | Ensure high purity and solubility of components for efficient in-gel reaction. |
| Live/Dead Viability/Cytotoxicity Assay Kit | Standardized two-color fluorescence assay to assess cell survival within a 3D biomimetic matrix post-fabrication and culture. | Penetration depth of dyes can be limited in dense hydrogels; may require microtome sectioning. |
| Tunable Stiffness Hydrogel Kits (e.g., Polyacrylamide-based) | To independently test the effect of substrate mechanical properties (elastic modulus) on cell behavior, separate from biochemical cues. | Precise calibration of crosslinker ratio is essential for reproducible stiffness. |
This analysis is framed within the ongoing research to establish formal definitions and conceptual frameworks under the ISO/TC 266 "Biomimetics" standard. A core tenet of this standardization effort is the development of robust, quantifiable performance metrics to objectively evaluate biomimetic materials against their conventional synthetic counterparts. The lack of standardized metrics often leads to inconsistent reporting and hampers comparative research. This guide provides a technical framework for measuring and comparing key performance indicators, aligning experimental protocols with the principles outlined in foundational ISO documents such as ISO 18458:2015, which provides terminology, concepts, and methodology for biomimetics.
Core Performance Metrics: Definition and Measurement
The performance of materials, whether biomimetic or synthetic, is evaluated across multiple axes. The following metrics are considered paramount for a comparative analysis, particularly in applications relevant to biomedical engineering and drug development (e.g., scaffolds, delivery systems, implantable devices).
Table 1: Definition of Key Performance Metrics
| Metric | Definition | Relevance in Biomimetics |
|---|---|---|
| Tensile Strength | Maximum stress a material can withstand while being stretched before failing. | Mimics the high strength-to-weight ratio of natural materials like spider silk. |
| Young's Modulus | Measure of stiffness of a solid material; the slope of the stress-strain curve. | Critical for matching the mechanical compliance of biological tissues (e.g., bone vs. cartilage). |
| Fracture Toughness | Resistance to fracture when a crack is present. | Biomimetics often aims to replicate the crack-deflection mechanisms seen in nacre. |
| Biodegradation Rate | Rate of material breakdown into non-toxic byproducts under physiological conditions. | Essential for temporary implants and drug-eluting scaffolds; often tuned via biomimetic polymer design. |
| Cytocompatibility | Qualitative and quantitative assessment of material's effect on cell viability, adhesion, and proliferation. | Core to any biomedical application; biomimetic surfaces often enhance compatibility. |
| Surface Energy / Wettability | Measured via contact angle; influences protein adsorption and cell adhesion. | Biomimetic surfaces replicate the superhydrophobicity of lotus leaves or the controlled wettability of cell membranes. |
| Drug Loading/Release Kinetics | Capacity to encapsulate an active compound and the profile of its subsequent release. | Biomimetic carriers (e.g., liposomes, peptide-based vesicles) aim for targeted, stimuli-responsive release. |
Experimental Protocols for Key Comparative Tests
Protocol:In VitroCytocompatibility Assay (ISO 10993-5)
Objective: To compare the cytotoxic potential of biomimetic and synthetic material extracts.
- Sample Preparation: Sterilize material samples (e.g., 1 cm² surface area or 0.1 g/mL). Prepare extracts using complete cell culture medium (e.g., DMEM + 10% FBS) incubated at 37°C for 24±2 hours.
- Cell Culture: Seed L929 fibroblast cells or a relevant primary cell line in a 96-well plate at a density of 1x10⁴ cells/well. Incubate for 24 hours to allow attachment.
- Exposure: Replace medium in test wells with 100 µL of material extract. Include negative (medium only) and positive (e.g., 1% Triton X-100) controls. Incubate for 24-48 hours.
- Viability Assessment: Perform MTT assay. Add 10 µL of MTT reagent (5 mg/mL) per well. Incubate for 4 hours. Dissolve formed formazan crystals with 100 µL of solubilization solution (e.g., DMSO). Measure absorbance at 570 nm with a reference at 650 nm.
- Analysis: Calculate cell viability % = (Absorbancesample / Absorbancenegative_control) x 100. Viability > 70% is typically considered non-cytotoxic per ISO 10993-5.
Protocol: Quasi-Static Tensile Testing (ASTM D638 / ISO 527)
Objective: To determine the tensile strength and Young's modulus of material specimens.
- Specimen Fabrication: Prepare dog-bone-shaped specimens (Type V per ASTM D638) from both material groups using precise machining or molding.
- Conditioning: Condition all specimens at 23±2°C and 50±10% relative humidity for at least 48 hours.
- Measurement: Measure the cross-sectional area of the specimen's gauge length using a calibrated micrometer.
- Testing: Mount specimen in a universal testing machine. Apply a monotonic tensile load at a constant crosshead speed of 1 mm/min until failure. Record load (N) and displacement (mm) continuously.
- Calculation: Calculate engineering stress (Load/Initial Area) and strain (ΔLength/Initial Gauge Length). Tensile strength = maximum stress. Young's Modulus = slope of the linear elastic region of the stress-strain curve.
Data Synthesis: Comparative Performance Table
Table 2: Exemplary Quantitative Comparison of Material Classes
| Performance Metric | Synthetic Polymer (e.g., PLGA) | Synthetic Ceramic (e.g., hydroxyapatite) | Biomimetic Polymer (e.g., RGD-peptide modified hydrogel) | Biomimetic Composite (e.g., Nacre-inspired clay/polymer) | Ideal Biological Benchmark |
|---|---|---|---|---|---|
| Tensile Strength (MPa) | 40 - 70 | 50 - 100 (brittle) | 0.5 - 10 | 80 - 200 | Spider Silk: ~1000 |
| Young's Modulus (GPa) | 1 - 3 | 70 - 120 | 0.001 - 0.1 | 10 - 50 | Cortical Bone: 15-20 |
| Fracture Toughness (MPa·m¹/²) | 0.5 - 5 | 0.5 - 1.2 | 0.01 - 0.1 | 5 - 15 | Nacre: ~3-10 |
| Biodegradation Rate (Time for 50% mass loss) | 1 - 12 months | 6 - 24 months (resorbable) | 1 week - 3 months | 3 - 18 months | Tissue-dependent |
| Cell Viability (% vs control) | 75 - 90% | 70 - 85% | 90 - 105% | 85 - 95% | 100% |
| Drug Loading Efficiency (%) | 5 - 20% | 1 - 5% | 15 - 30% | 5 - 15% | N/A |
Visualizing Biomimetic Design and Experimental Workflows
Diagram Title: Biomimetic Material Design and Validation Workflow
Diagram Title: In Vitro Cytocompatibility Testing Protocol
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Performance Evaluation
| Item | Function in Experiment | Example Product / Specification |
|---|---|---|
| L929 Fibroblast Cell Line | Standardized model for cytocompatibility testing per ISO 10993-5. | ATCC CCL-1, cultured in DMEM + 10% FBS. |
| MTT Assay Kit | Colorimetric assay for measuring cell metabolic activity as a proxy for viability. | Thiazolyl Blue Tetrazolium Bromide (MTT), typically 5 mg/mL in PBS. |
| Dulbecco's Modified Eagle Medium (DMEM) | Complete cell culture medium for maintaining cells and preparing material extracts. | High glucose, with L-glutamine, supplemented with 10% Fetal Bovine Serum (FBS) and 1% Pen/Strep. |
| Phosphate Buffered Saline (PBS) | Washing cells and preparing reagent solutions; isotonic and non-toxic to cells. | 1X solution, pH 7.4, sterile-filtered. |
| Universal Testing Machine (UTM) | Applies controlled tensile/compressive forces to measure mechanical properties. | Equipped with a 1 kN load cell and environmental chamber (for conditioned testing). |
| Simulated Body Fluid (SBF) | Ionic solution mimicking human blood plasma; used to test bioactivity and degradation. | Prepared per Kokubo recipe (c-SBF), pH 7.4 at 36.5°C. |
| RGD Peptide Motif | Common biomimetic surface modifier to enhance cell adhesion via integrin binding. | Cyclo(Arg-Gly-Asp-D-Phe-Cys) grafted onto polymer surfaces. |
| Dynamic Mechanical Analyzer (DMA) | Measures viscoelastic properties (storage/loss modulus) under oscillatory stress. | Essential for characterizing hydrogels and soft biomimetic materials. |
This document serves as an in-depth technical guide, framed within the ongoing research thesis on ISO standards for biomimetics definition and concepts (ISO/TC 266). It examines the critical evaluation of biomimetic solutions—materials, devices, or systems that imitate biological entities—in pre-clinical models, emphasizing compliance with emerging ISO frameworks. Adherence to standardized terminology and testing protocols (e.g., ISO 18457, ISO 18458) ensures reproducible, comparable, and scientifically robust efficacy data, accelerating translation from laboratory research to clinical application.
Core ISO Framework Context
The evaluation of biomimetic solutions operates within the conceptual framework defined by ISO/TC 266 standards:
- ISO 18458:2015: Defines terms, concepts, and the biomimetic process.
- ISO 18457: Provides guidance on biomimetic materials, structures, and components.
- Under Development: Standards for testing and characterization methodologies specific to biomimetics.
Compliance ensures that "biomimicry" is not merely an analogy but a quantifiable design principle with traceable functional fidelity to the biological target.
Case Studies: Efficacy Evaluation in Pre-Clinical Models
Case Study 1: Biomimetic Bone Scaffold for Critical-Sized Defect Repair
Biological Principle Mimicked: Native osteogenic niche and bone extracellular matrix (ECM) hierarchy. ISO-Compliant Description: Per ISO 18458, this is a "biomimetic material" designed through a "top-down process" replicating the structural and compositional attributes of trabecular bone.
Experimental Protocol:
- Scaffold Fabrication: Fabricate scaffolds from hydroxyapatite/collagen I composite using 3D printing to mimic pore size (300-500 μm) and interconnectivity of cancellous bone (ISO 18457 guidance on material selection).
- In Vitro Pre-Screening: Seed with human Mesenchymal Stem Cells (hMSCs). Assess viability (Live/Dead assay), proliferation (DNA quantification), and osteogenic differentiation (ALP activity, qPCR for Runx2, Osterix) over 21 days.
- In Vivo Implantation:
- Model: 8mm critical-sized calvarial defect in male Sprague-Dawley rats (n=10/group).
- Groups: (1) Biomimetic scaffold + hMSCs, (2) Biomimetic scaffold alone, (3) Empty defect (control).
- Time Points: 4, 8, and 12 weeks post-implantation.
- Endpoint Analysis:
- Micro-Computed Tomography (μCT): Quantify new bone volume (BV/TV), bone mineral density (BMD), and trabecular number (Tb.N).
- Histomorphometry: H&E and Masson's Trichrome staining to evaluate tissue integration and new bone formation. Calculate osteoid surface/bone surface (OS/BS).
- Biomechanical Testing: Push-out test to assess scaffold-bone integration strength.
Summarized Quantitative Data:
Table 1: In Vivo Bone Regeneration Metrics at 12 Weeks (Mean ± SD)
| Experimental Group | Bone Volume/Tissue Volume (BV/TV %) | Bone Mineral Density (mg HA/cm³) | Push-Out Strength (MPa) |
|---|---|---|---|
| Biomimetic Scaffold + hMSCs | 42.5 ± 3.8 | 685.2 ± 45.6 | 8.7 ± 1.2 |
| Biomimetic Scaffold Alone | 28.1 ± 4.2 | 520.4 ± 38.9 | 5.1 ± 0.9 |
| Empty Defect Control | 8.9 ± 2.1 | 310.8 ± 25.7 | N/A |
Diagram Title: ISO-Compliant Biomimetic Scaffold Testing Workflow
Case Study 2: Biomimetic Nanoparticle for Targeted Drug Delivery
Biological Principle Mimicked: Natural lipoprotein structure (e.g., HDL) for tumor targeting. ISO-Compliant Description: A "biomimetic system" employing a "bottom-up process" to create a nanoparticle with a lipid-protein corona mimicking endogenous transport particles.
Experimental Protocol:
- Nanoparticle Synthesis: Prepare core-shell nanoparticles with a PLGA core and a reconstituted lipid bilayer decorated with recombinant ApoA-1 protein.
- Characterization: Measure size (DLS), zeta potential, and drug loading efficiency (HPLC). Confirm surface protein orientation (Western blot, ELISA).
- In Vitro Targeting: Incubate fluorescently labeled particles with cancer cell lines (high SR-B1 receptor) and control cells. Quantify uptake via flow cytometry and confocal microscopy.
- In Vivo Efficacy:
- Model: Female BALB/c nude mice with subcutaneously implanted MDA-MB-231 (breast cancer) xenografts (n=8/group).
- Groups: (1) Biomimetic NP loaded with Doxorubicin, (2) Non-biomimetic NP (no ApoA-1) + Dox, (3) Free Dox, (4) Saline control.
- Dosing: 5 mg Dox/kg, intravenous, bi-weekly for 3 weeks.
- Endpoint Analysis:
- Tumor Kinetics: Measure tumor volume (caliper) twice weekly. Calculate tumor growth inhibition (TGI %).
- Biodistribution: Ex vivo fluorescence imaging of organs and tumors at 24h post-final dose.
- Histopathology: H&E staining of tumors for necrosis assessment. TUNEL assay for apoptosis.
- Safety: Monitor body weight. Analyze serum biomarkers (ALT, AST, CREA) for hepatorenal toxicity.
Summarized Quantitative Data:
Table 2: In Vivo Antitumor Efficacy and Biodistribution (Mean ± SD)
| Group | Tumor Growth Inhibition (TGI %) at Day 21 | Tumor Fluorescence Intensity (%ID/g) | Change in Body Weight (%) |
|---|---|---|---|
| Biomimetic NP (ApoA-1) + Dox | 78.4 ± 5.2 | 12.5 ± 2.3 | -3.2 ± 1.8 |
| Non-biomimetic NP + Dox | 52.1 ± 6.8 | 5.8 ± 1.5 | -6.5 ± 2.1 |
| Free Doxorubicin | 45.6 ± 7.9 | 1.2 ± 0.4 | -15.3 ± 3.4 |
| Saline Control | 0 | N/A | +2.1 ± 1.2 |
Diagram Title: Biomimetic NP Targeting & Intracellular Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Biomimetic Solution Evaluation
| Item / Reagent Solution | Function in Evaluation | Example Vendor / Catalog |
|---|---|---|
| Primary Human Mesenchymal Stem Cells (hMSCs) | Gold-standard cell source for in vitro osteogenic differentiation assays. | Lonza, PT-2501 |
| Recombinant Human ApoA-1 Protein | Essential for constructing biomimetic lipoprotein-mimicking nanoparticles. | PeproTech, 350-02 |
| Osteogenic Differentiation Media Kit | Standardized cocktail (ascorbate, β-glycerophosphate, dexamethasone) for bone studies. | Thermo Fisher, A1007201 |
| In Vivo Imaging System (IVIS) Fluorescent Dye (e.g., DiR) | For longitudinal, non-invasive tracking of nanoparticles in animal models. | PerkinElmer, 125964 |
| μCT Calibration Phantom | Critical for quantitative, reproducible bone mineral density measurements (ISO compliance). | Scanco Medical, QA Phantom |
| Species-Specific ELISA Kits (ALT, AST, CREA) | Assess organ toxicity in pre-clinical models as part of safety profiling. | Abcam, ab263882/ab285264 |
| Decellularized Extracellular Matrix (dECM) Powder | Used as a bioactive, biomimetic coating or scaffold component. | Sigma-Aldrich, D9810 |
| Anti-SR-B1 Antibody (for blocking studies) | Validates the specificity of biomimetic nanoparticle targeting pathways. | R&D Systems, MAB7438 |
Systematic evaluation of biomimetic solutions in pre-clinical models, guided by ISO terminology and conceptual frameworks, is paramount for establishing credible efficacy data. The case studies demonstrate that ISO compliance necessitates rigorous characterization of the biomimetic principle itself, followed by standardized in vitro and in vivo testing protocols. This disciplined approach reduces ambiguity, facilitates cross-study comparisons, and ultimately builds a stronger evidentiary foundation for regulatory approval and clinical success. Future standards focusing on specific testing protocols will further solidify the role of biomimetics in advanced therapeutic development.
Cost-Benefit Analysis of a Standardized Biomimetic R&D Pathway
This whitepaper provides a technical guide to the cost-benefit analysis of implementing a standardized research and development pathway for biomimetic solutions in drug development. It is framed within the ongoing development of ISO standards for biomimetics (ISO/TC 266), specifically supporting the thesis that formalized definitions, concepts, and research protocols (e.g., ISO 18458, ISO 18459) are critical for translating biological principles into scalable, commercially viable, and clinically effective therapeutics. Standardization mitigates the inherent risks of biomimetic R&D—biological complexity, reproducibility challenges, and high early-stage failure rates—by providing a common framework for validation, comparison, and regulatory approval.
Quantitative Cost-Benefit Framework
The following tables summarize key quantitative data comparing traditional biomimetic R&D to a pathway structured under proposed ISO-standardized concepts.
Table 1: Phase-Based R&D Cost Comparison (Estimated Averages)
| R&D Phase | Traditional Biomimetic Approach (Cost in USD) | Standardized Pathway (Cost in USD) | Key Cost Drivers for Standardization |
|---|---|---|---|
| Discovery & Concept Validation | $1.8M - $3.5M | $2.1M - $3.8M | Higher initial investment in bio-informed database mining & standardized characterization assays. |
| Preclinical Development | $8.5M - $15.0M | $7.0M - $12.0M | Reduced cost from reproducible protocols, shared model systems, and lower compound attrition. |
| Early Clinical (Phase I/IIa) | $25.0M - $45.0M | $22.0M - $40.0M | Savings from clearer regulatory submissions based on standardized efficacy/safety biomarkers. |
| Attrition Rate (Lead to Clinic) | 85-92% | Projected: 70-80% | Benefit from reduced technical failure due to rigorous early-stage validation frameworks. |
| Time to IND Filing | 60-84 months | Projected: 48-66 months | Acceleration from streamlined decision gates and predefined validation milestones. |
Table 2: Benefit Metrics Analysis
| Benefit Category | Traditional Approach | Standardized Pathway | Measurement Basis |
|---|---|---|---|
| Technical Reproducibility | Low (Lab-dependent) | High | Intra- and inter-laboratory validation success rate for core bio-inspired function. |
| IP Strength & Licensing | Fragmented | Strengthened | Number of cross-licensable platform patents; clarity of prior art. |
| Regulatory Alignment | Case-by-case | Streamlined | Reduced FDA/EMA questions per Investigational New Drug (IND) application. |
| Investment Appeal | High Risk/High Reward | De-risked Profile | Increased non-dilutive grant funding & venture capital interest in platform technologies. |
| Translational Success | Variable | Enhanced | Higher probability of clinical mechanism-of-action confirmation. |
Core Experimental Protocols for Standardized Validation
This section details key methodologies underpinning a standardized biomimetic R&D pathway.
Protocol 1: Standardized Functional Characterization of a Biomimetic Drug Delivery System (e.g., Liposome mimicking exosome)
- Objective: To quantify the loading efficiency, release kinetics, and target cell uptake of a biomimetic nanoparticle according to ISO-guided parameters.
- Materials: See "The Scientist's Toolkit" (Section 5.0).
- Methodology:
- Formulation & Loading: Prepare biomimetic vesicles via microfluidics. Load with fluorescent probe (e.g., Calcein) or active pharmaceutical ingredient (API). Purify via size-exclusion chromatography (SEC).
- Loading Efficiency: Measure unencapsulated material post-SEC using fluorescence spectrometry or HPLC. Calculate: Loading Efficiency (%) = (Total API - Free API) / Total API x 100.
- In Vitro Release Kinetics: Use dialysis bag method in PBS (pH 7.4) and acetate buffer (pH 5.5) at 37°C under sink conditions. Sample receptor medium at defined intervals (0, 1, 2, 4, 8, 24, 48h). Quantify released API. Fit data to zero-order, first-order, and Higuchi models.
- Cellular Uptake Assay: Seed target cells (e.g., HEK293) and control cells in 24-well plates. Incubate with fluorescently labeled vesicles (50 µg/mL) for 2h at 37°C (and 4°C for energy-dependent uptake control). Wash, trypsinize, and analyze via flow cytometry. Express results as mean fluorescence intensity (MFI) fold-change over control.
Protocol 2: High-Content Screening (HCS) for Bio-Inspired Signaling Pathway Activation
- Objective: To systematically evaluate the activation of a natural biological pathway (e.g., Nrf2 antioxidant response) by a biomimetic compound using standardized imaging and analysis.
- Materials: See "The Scientist's Toolkit."
- Methodology:
- Cell Preparation & Treatment: Seed reporter cells (e.g., ARE-GFP HepG2) in 96-well imaging plates. Treat with a gradient of the biomimetic compound, a positive control (e.g., Sulforaphane), and vehicle for 6-24h.
- Fixation & Staining: Fix cells with 4% PFA, permeabilize with 0.1% Triton X-100, and stain nuclei with Hoechst 33342. Optional: stain for Nrf2 translocation (anti-Nrf2 primary, Alexa Fluor 594 secondary).
- Automated Imaging: Acquire 9 fields/well using a 20x objective on a high-content imager.
- Image Analysis: Use standardized software algorithms to:
- Segment nuclei (Hoechst channel).
- Quantify nuclear vs. cytoplasmic fluorescence intensity (Nrf2 or GFP channel).
- Calculate metrics: % cells with nuclear Nrf2 translocation, mean GFP intensity per cell.
- Dose-Response Modeling: Fit GFP intensity data to a 4-parameter logistic model to derive EC50 values.
Mandatory Visualizations
Standardized Biomimetic R&D Workflow
Nrf2 Pathway Activation by Biomimetics
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Standardized Biomimetic R&D Experiments
| Item | Function in Standardized Pathway | Example Product/Catalog |
|---|---|---|
| Microfluidic Chip System | Reproducible fabrication of monodisperse biomimetic nanoparticles (liposomes, polymersomes). | Dolomite Mitos NanoLipid System; Precision NanoSystems NanoAssemblr. |
| Size-Exclusion Chromatography (SEC) Columns | Standardized purification of biomimetic vesicles from unencapsulated agents. | Cytiva Sepharose CL-4B; Izon Science qEVoriginal columns. |
| Tunable Resistance Pulse Sensing (TRPS) System | High-resolution, ISO-aligned particle concentration and size analysis. | Izon Science qNano. |
| ARE-Luciferase/GFP Reporter Cell Line | Standardized cell-based assay for Nrf2 pathway activation screening. | ATCC ARE-bla HEK293T; Signosis ARE-GFP reporter kit. |
| High-Content Imaging System | Quantitative, multiplexed analysis of cellular uptake and pathway activation. | Thermo Fisher CellInsight; PerkinElmer Operetta. |
| Biomimetic Peptide Library | Standardized sets of bio-inspired peptides for structure-activity relationship (SAR) studies. | Mimotopes SPOT synthesis libraries; CPC Scientific custom peptide arrays. |
| Proteomics Standard (UPS2) | Internal standard for mass spectrometry-based analysis of biomimetic material bio-corona. | Sigma-Aldrich Universal Proteomics Standard Set 2. |
Within the rigorous framework of biomimetics research and standardization efforts, such as those guided by the emerging ISO standards for biomimetics (e.g., ISO 18458), a central tension persists: the perceived conflict between structured methodology and creative discovery. This whitepaper investigates whether a structured, benchmarked approach to innovation, particularly in biomimetic drug development, enhances or hinders creative output. We posit that a defined scaffold, rather than stifling creativity, provides a necessary comparative baseline ("benchmark") that channels divergent thinking into tractable, reproducible innovation with measurable outcomes.
The ongoing development of ISO standards for biomimetics (under TC 266) aims to establish clear terminology, methodologies, and principles. A core objective is to transform biomimetics from an artisanal practice into a rigorous, repeatable engineering and scientific discipline. This standardization inherently promotes a structured approach to the innovation process—from problem definition (biological system analysis) to abstraction and transfer to technical application.
This paper's thesis is embedded within this context: The structured framework provided by biomimetics standards creates a benchmarkable innovation pipeline. This pipeline enhances creativity by providing clear stages for divergent and convergent thinking, enabling the quantitative assessment of "innovation potential" at each phase, from biological insight to preclinical candidate.
Quantitative Benchmarking of Creative Phases in Biomimetic Research
We define "Innovation Potential" as a composite metric reflecting the novelty, feasibility, and projected impact of a biomimetic solution. The following table summarizes key quantitative indicators used to benchmark this potential across a standardized innovation workflow.
Table 1: Benchmarking Metrics for Biomimetic Innovation Phases
| Innovation Phase (ISO 18458 Aligned) | Key Benchmarking Metrics | Measurement Method | Target Range (Example) |
|---|---|---|---|
| 1. Biological Analysis & Scoping | • Biological Solution Space Diversity• Functional Principle Uniqueness Index | • Phylogenetic breadth analysis• Patent/ literature novelty score | >3 distinct biological models; Novelty score >0.7 |
| 2. Abstraction & Modeling | • Transferable Parameter Ratio• Model Predictive Accuracy | (# of abstracted principles) / (# of biological specifics)R² of in silico model vs. biological performance | Ratio > 0.5; R² > 0.85 |
| 3. Technical Implementation | • Feasibility Score• Prototype Performance Delta | Multi-criteria decision analysis (MCDA)(Prototype perf.) / (Benchmark perf.) | Weighted score > 65%; Delta > 1.2x |
| 4. Validation & Iteration | • Iteration Cycle Time• Performance Improvement Slope | Time from test failure to new prototypeΔPerformance / ΔIteration | Cycle time < 2 weeks; Slope > 0.1 |
Experimental Protocol: Benchmarking a Structured vs. Unstructured Ideation Session
This protocol is designed to test the core hypothesis in a controlled setting relevant to drug discovery.
Title: Comparative Analysis of Ideation Output for a Targeted Drug Delivery Challenge Using Structured Biomimetic Template vs. Free Brainstorming.
Objective: To quantify and compare the novelty, feasibility, and volume of ideas generated for a biomimetic drug delivery problem using a structured ISO-aligned template versus an unstructured brainstorming session.
Materials: See "Scientist's Toolkit" (Section 6).
Methodology:
- Participant Selection: Recruit two matched cohorts (n=10 each) of researchers from drug development and biology backgrounds. Cohorts are balanced for experience.
- Problem Definition: Both cohorts receive the same precise problem statement: "Design a nanoparticle system for targeted delivery to hypoxic tumor cores, minimizing systemic clearance."
- Intervention:
- Cohort A (Structured): Uses a tailored biomimetic ideation template based on ISO 18458 phases: (a) Identify Function (target hypoxia), (b) Biological Model Search (e.g., leukocyte margination, platelet aggregation, bacterial chemotaxis), (c) Abstract Principle (e.g., adhesion cascade, quorum sensing), (d) Technical Implementation Sketch.
- Cohort B (Unstructured): Conducts a 45-minute free-form brainstorming session with no imposed framework.
- Output Capture: All ideas are documented verbatim.
- Blinded Assessment: A separate panel scores all anonymized ideas on:
- Novelty: 1-5 scale (1=common, 5=radical).
- Feasibility: 1-5 scale (1=not feasible in 5 yrs, 5=readily testable).
- Relevance: 1-5 scale (directly addresses problem).
- Volume: Total distinct ideas.
- Statistical Analysis: Compare mean novelty, feasibility, and volume scores between cohorts using Mann-Whitney U tests. Calculate an "Innovation Potential Index" as (Novelty * Feasibility * Relevance) for each idea and compare distributions.
Diagram: Structured Biomimetic Innovation Workflow
Structured Biomimetic R&D Workflow
Diagram: Signaling Pathway in Hypoxia-Targeted Drug Delivery
Hypoxia-Induced Signaling for Targeted Delivery
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Biomimetic Drug Delivery Research
| Item / Reagent | Function in Benchmarking Experiments | Example & Rationale |
|---|---|---|
| Hypoxia-Inducible Factor (HIF-1α) Stabilizers | Induce controlled hypoxic signaling in vitro for target validation. | Cobalt(II) Chloride (CoCl₂): Mimics hypoxia by stabilizing HIF-1α, used to upregulate target receptors (e.g., CA9) on cancer cell lines. |
| CA9 (Carbonic Anhydrase IX) Antibody | Benchmark for detecting and quantifying a key hypoxia-induced target. | Anti-CA9 monoclonal antibody (e.g., M75): Used in ELISA, flow cytometry, and immunohistochemistry to validate the "biological model" step and measure targeting efficiency of novel nanoparticles. |
| Fluorescently-Labeled Model Nanoparticles | Prototype systems to test targeting and uptake hypotheses. | COOH-modified Polystyrene NPs (100nm): Provide a consistent, trackable benchmark particle. Surface can be functionalized with putative biomimetic ligands (e.g., peptides mimicking leukocyte adhesion) for comparative binding assays. |
| Microfluidic Shear Flow Devices | Simulate physiological shear stress for biomimetic adhesion testing. | µ-Slide I Luer chips: Enable benchmarking of nanoparticle binding under dynamic, physiologically relevant flow conditions, critical for testing vascular margination principles. |
| 3D Spheroid / Organoid Cultures | Provide a hypoxic core benchmark for testing penetration. | HCT-116 Colorectal Cancer Spheroids: Serve as a more realistic in vitro tumor model with inherent hypoxia gradients, against which biomimetic nanoparticle penetration depth is quantitatively measured vs. standard NPs. |
The integration of a structured, benchmark-driven approach—exemplified by the framework of ISO biomimetics standards—does not extinguish creativity but rather potentiates it. By providing clear phases for biological analysis, abstraction, and implementation, the process creates defined "spaces" for divergent thinking while introducing convergent checkpoints for feasibility assessment. The ability to benchmark "Innovation Potential" at each stage transforms subjective creative evaluation into a quantitative, comparative science. For researchers and drug developers, this structured biomimetic pipeline offers a replicable, auditable, and ultimately more reliable path to breakthrough innovations, turning nature's creativity into measurable therapeutic progress.
The nascent field of biomimetic therapies—engineered systems that imitate complex biological entities for diagnostic or therapeutic purposes—faces a critical juncture. The lack of standardized terminology, characterization protocols, and regulatory frameworks poses significant barriers to translation. This whitepaper situates itself within a broader thesis advocating for the urgent development of comprehensive ISO standards for biomimetics definition and concepts. Such standards are a foundational prerequisite for coherent regulatory pathways, ensuring safety, efficacy, and reproducibility for researchers and drug development professionals.
Current ISO Framework and Critical Gaps
While specific ISO standards for "biomimetic therapies" are not yet established, adjacent standards provide a scaffold. Key gaps remain in defining the core concepts unique to biomimicry in medicine.
Table 1: Relevant Existing ISO Standards and Identified Gaps
| Standard Number | Title/Scope | Relevance to Biomimetic Therapies | Critical Gap for Biomimetics | |
|---|---|---|---|---|
| ISO/TR 23457:2024 | Biomimetics — Biomimetic material, structure, and component | Provides foundational terminology for materials science applications. | Lacks definitions for therapeutic entities (e.g., biomimetic cells, vesicles, drug delivery systems). | |
| ISO 10993 (Series) | Biological evaluation of medical devices | Framework for biocompatibility testing. | Insufficient for dynamic, biologically active, and degradable biomimetic therapeutics. | |
| ISO 14971:2019 | Medical devices — Application of risk management | Essential risk management principles. | Does not address unique risks of bio-hybrid or cell-mimicking systems. | |
| ISO/ASTM 52900 | Additive manufacturing — General principles — Terminology | Relevant for 3D-bioprinted biomimetic scaffolds. | Excludes in situ or nano-scale biomimetic assembly. | |
| Gap | Proposed New Standard Area | Objective | Key Stakeholders | |
| N/A | ISO/DIS 23599 (Hypothetical) | Biomimetics — Vocabulary and concepts for therapeutic applications | To define terms: biomimetic nanoparticle, synthetic cell, extracellular vesicle mimetic, bio-inspired drug release. | Academics, Regulators (EMA, FDA), Industry. |
| N/A | ISO/AWI 23600 (Hypothetical) | Biomimetic therapeutics — Characterization and quality control | To standardize metrics for mimetic fidelity, potency, purity, and stability. | Developers, CROs, Pharmacopeias. |
Regulatory Pathways: EMA and FDA Perspectives
Regulatory agencies are adapting existing frameworks. The primary pathways are through Advanced Therapy Medicinal Products (ATMPs) in the EU and Combination Products or Biological Licenses in the US.
Table 2: Current Regulatory Pathways for Select Biomimetic Therapies
| Therapy Class | Example | Likely Primary Regulatory Pathway (EMA) | Likely Primary Regulatory Pathway (FDA) | Key Standardization Need |
|---|---|---|---|---|
| Biomimetic Liposomes/Nanoparticles | Ligand-targeted liposomal doxorubicin | Medicinal Product (Directive 2001/83/EC) | Drug/Biologic (NDA/BLA) as a complex product | Standardized characterization of targeting moiety density and orientation. |
| Engineered Extracellular Vesicles (EVs) | MSC-EVs for tissue repair | ATMP (Regulation 1394/2007) if substantially manipulated. | Biological Product (BLA, §351 of PHS Act) | ISO standards for EV mimetic isolation, cargo loading efficiency, and potency assays. |
| 3D-Bioprinted Biomimetic Tissues | Printed cartilage constructs | Combined ATMP (if containing cells) or Medical Device. | Combination Product (PMA/BLA pathway) | Standardized protocols for mechanical and functional biomimicry validation. |
| Synthetic Cells | Protocells for enzyme delivery | Borderline classification; case-by-case. | Likely Biologic; novel regulatory science. | ISO definitions for "synthetic cell" and minimal functionality criteria. |
Experimental Protocols: Standardizing Characterization
The following detailed methodologies are cited as critical experiments whose standardization should be proposed under a new ISO guideline (e.g., ISO/AWI 23600).
Protocol: Quantification of Biomimetic Fidelity for Nanoparticle Surface Functionalization
- Objective: To reproducibly measure the density and conformational fidelity of biomimetic ligands (e.g., peptides, antibodies) on nanoparticle surfaces.
- Materials: Functionalized nanoparticles, fluorogenic tagging kit (e.g., FITC-NHS), Bradford assay reagents, calibrated quartz crystal microbalance with dissipation (QCM-D) sensors, SDS-PAGE gel apparatus.
- Methodology:
- Ligand Quantification (Direct):
- Dissolve nanoparticle sample in 1% SDS.
- Run SDS-PAGE alongside a standard curve of the free ligand.
- Stain with Coomassie Blue or use fluorescent in-gel imaging if ligand is pre-tagged.
- Quantify band intensity to calculate total ligand per nanoparticle batch.
- Surface Occupancy & Orientation (Indirect):
- Coat QCM-D sensor with the target receptor protein.
- Flow nanoparticle solution over sensor at physiological flow rate.
- Monitor frequency (ΔF) and dissipation (ΔD) shifts. A high ΔD/ΔF ratio suggests multivalent, oriented binding, indicating proper ligand presentation.
- Compare to a control with scrambled ligand or bare nanoparticles.
- Ligand Quantification (Direct):
- Data to Report: Ligand density (molecules/particle), binding kinetics (association/dissociation rates from QCM-D), conformational fidelity index (ΔD/ΔF ratio normalized to control).
Protocol: Potency Assay for Biomimetic Extracellular Vesicles (EV Mimetics)
- Objective: To standardize an in vitro functional assay measuring the biological activity of EV mimetics intended for immune modulation.
- Materials: EV mimetic preparation, primary human peripheral blood mononuclear cells (PBMCs), LPS (lipopolysaccharide), ELISA kits for TNF-α and IL-10, flow cytometer, cell culture facility.
- Methodology:
- Isolate PBMCs from donor blood using density gradient centrifugation.
- Seed PBMCs in a 96-well plate at 1x10^5 cells/well.
- Pre-treat cells with a logarithmic dose range of EV mimetics (e.g., 10^4 to 10^9 particles/well) for 2 hours.
- Stimulate inflammation by adding LPS (100 ng/mL) to all treatment wells except negative controls.
- Incubate for 24 hours at 37°C, 5% CO2.
- Collect supernatant and analyze TNF-α (pro-inflammatory) and IL-10 (anti-inflammatory) cytokine levels via ELISA.
- Analyze cells via flow cytometry for surface markers (e.g., CD86, CD206 on monocytes).
- Data to Report: Dose-response curves, IC50 for TNF-α suppression, EC50 for IL-10 induction, and shift in macrophage polarization phenotype. A reference EV standard should be included in each assay plate.
Visualizations
Diagram 1: Biomimetic Nanoparticle Regulatory Assessment Workflow
Diagram 2: Key Signaling Pathway in EV Mimetic Immune Modulation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biomimetic Therapy Characterization
| Item | Function/Description | Key Application in Biomimetics |
|---|---|---|
| Asymmetric Flow Field-Flow Fractionation (AF4) System | Separates nanoparticles and vesicles by hydrodynamic radius with minimal shear stress. | High-resolution size and stability analysis of polydisperse biomimetic nanoparticle/EV preparations. |
| Tetraspanin Antibody Cocktail (CD9/CD63/CD81) | Antibodies against canonical EV surface markers for capture or detection. | Standardized immunophenotyping of EV mimetics to confirm membrane composition fidelity. |
| MicroBCA or Bradford Assay Kit | Colorimetric quantification of total protein concentration. | Measuring cargo protein loading efficiency in biomimetic carriers. |
| Lipid Dye (e.g., PKH67, DiD) | Fluorescent lipophilic membrane dyes for stable long-term tracking. | In vitro and in vivo tracking of biomimetic nanoparticle/cell membrane fusion and uptake kinetics. |
| Quartz Crystal Microbalance with Dissipation (QCM-D) | Measures mass and viscoelastic properties of adsorbed layers in real-time. | Label-free analysis of biomimetic particle binding kinetics and conformational changes on target surfaces. |
| Recombinant Target Receptor Proteins | Purified, bioactive human recombinant proteins (e.g., VEGF, integrins). | Validating the functional affinity of targeting ligands on biomimetic constructs in cell-free systems. |
| 3D Bioprinter & Bioink (GelMA, Alginate) | Enables layer-by-layer deposition of cells and biomaterials. | Fabricating biomimetic tissue constructs with controlled architecture for therapy and testing. |
| NanoFCM or Tunable Resistive Pulse Sensing (TRPS) | High-resolution particle-by-particle analysis of size and concentration. | Precise quantification and quality control of biomimetic particle sub-populations. |
Conclusion
The ISO 18458 and 18459 standards provide an indispensable, structured framework that elevates biomimetics from a source of inspiration to a rigorous, repeatable discipline for biomedical innovation. By establishing a clear lexicon (Intent 1) and a defined methodological pathway (Intent 2), they enable more efficient translation of biological principles. While challenges in abstraction and interdisciplinary work persist, the standards offer strategies for optimization and risk mitigation (Intent 3). Ultimately, this formalized approach facilitates robust validation and compelling comparative analysis against conventional methods (Intent 4), proving the tangible value of biomimetic strategies. For the future, widespread adoption of these standards promises to accelerate the development of sophisticated, nature-inspired solutions—from smart drug delivery platforms to regenerative medicine—creating a new paradigm where biological intelligence is systematically harnessed to advance human health.