Nanoscale Biological Interactions: Fundamentals for Advanced Drug Delivery and Biomedical Applications
This comprehensive review explores the fundamental principles governing interactions between nanoscale materials and biological systems, providing crucial insights for researchers and drug development professionals.
Nanoscale Biological Interactions: Fundamentals for Advanced Drug Delivery and Biomedical Applications
Abstract
This comprehensive review explores the fundamental principles governing interactions between nanoscale materials and biological systems, providing crucial insights for researchers and drug development professionals. The article systematically examines how physicochemical properties of nanoparticles—including size, surface charge, and functionalization—dictate their behavior in biological environments. It covers both traditional and emerging biomimetic strategies for optimizing nanoparticle performance, addressing critical challenges such as immune clearance, targeting specificity, and biocompatibility. Through comparative analysis of various nanoplatforms and discussion of advanced characterization techniques, this work establishes a foundation for the rational design of next-generation nanomedicines with enhanced therapeutic efficacy and safety profiles.
The Nano-Bio Interface: Fundamental Interactions Governing Nanomaterial Behavior in Biological Systems
The interaction between nanoparticles (NPs) and biological systems is a cornerstone of modern nanomedicine and nanotoxicology research. The biological fate, efficacy, and safety of nanoparticles are predominantly governed by a triad of fundamental physicochemical properties: size, surface charge, and hydrophobicity. These properties collectively determine the behavior of nanoparticles at the nano-bio interface, influencing their cellular uptake, intracellular trafficking, biodistribution, and potential toxicological outcomes. A systematic understanding of these parameters is essential for the rational design of effective and safe nanomedicines, as well as for accurate risk assessment of incidental nanoparticle exposure. This whitepaper provides an in-depth technical analysis of these key properties, framed within the context of fundamental nanoscale biological interactions research for scientific and drug development professionals.
Fundamental Property Analysis and Quantitative Data
The following section synthesizes experimental and computational data on how specific physicochemical parameters direct biological interactions.
Table 1: Quantitative Effects of Nanoparticle Physicochemical Properties on Biological Interactions
| Property | Typical Measurement Techniques | Key Biological Effects | Representative Quantitative Findings |
|---|---|---|---|
| Size | Dynamic Light Scattering (DLS), Transmission Electron Microscopy (TEM) [1] [2] | Cellular uptake efficiency, biodistribution, clearance pathway [3] [1] | NPs of 10-100 nm show optimal tissue penetration and reduced RES clearance [4]. NPs <10 nm undergo rapid renal clearance [4]. Smaller NPs often show higher tissue distribution and more severe effects than larger ones [3]. |
| Surface Charge | Zeta (ζ) Potential [5] [2] [6] | Cellular membrane interaction, protein corona composition, cytotoxicity [3] [7] [6] | Positive charges enhance attachment to negatively charged cell membranes, often leading to higher cytotoxicity [3] [7]. Cationic NPs with high surface charge density (>2.95 µmol/g) cause significant viability loss, oxidative stress, and inflammation, while those with low density (0.23 µmol/g) do not [6]. |
| Hydrophobicity | Contact angle, Chromatography, Fluorescent probes [8] | Protein adsorption, immune clearance, self-assembly, membrane integration [9] [4] [10] | Hydrophobic surfaces enhance plasma protein adsorption (opsonization), leading to rapid clearance by the Mononuclear Phagocyte System (MPS) [4]. Hydrophobic interactions drive the self-assembly of nucleic acid-based biomaterials and facilitate nanoparticle embedding into lipid membranes [9] [10]. |
Experimental Methodologies for Characterizing Nano-Bio Interactions
Protocol 1: Evaluating Cellular Uptake and Cytotoxicity
This protocol is adapted from studies investigating the role of surface charge density on macrophage and epithelial cell responses [6].
- Objective: To quantify the relationship between nanoparticle surface charge density and cellular toxicity outcomes.
- Materials:
- THP-1-derived macrophages, A549, and Calu-3 airway epithelial cells.
- Cationic carbon nanoparticles (CDs) with a similar ζ-potential (+20 to +27 mV) but varying surface charge density (0.23 to 4.39 µmol/g).
- Cell culture reagents (α-MEM/RPMI-1640, FBS, antibiotics).
- Multiplex cytotoxicity assay kit (e.g., CCK-8 for viability).
- Fluorescence Activated Cell Sorter (FACS) and Confocal Laser Scanning Microscopy (CLSM).
- Assay kits for oxidative stress (DCFH-DA), mitochondrial membrane potential (JC-1), and lysosomal integrity (e.g., Acridine Orange).
- Procedure:
- Cell Exposure: Harvest, wash, and suspend cells in an appropriate buffer. Expose cells to escalating doses (e.g., 3 to 200 µg/mL) of the characterized NPs for 24 hours.
- Viability Assessment: Use a CCK-8 or similar assay to measure cell viability loss. Incubate cells with the reagent for 1-4 hours and measure absorbance at 450 nm.
- Cellular Uptake Analysis:
- FACS: After 4 hours of exposure, harvest cells, wash, and analyze the intrinsic fluorescence of the CDs using FACS to quantify uptake.
- CLSM: Seed cells on glass-bottom dishes, expose to NPs, fix, and image using CLSM to visualize intracellular localization.
- Mechanistic Toxicity Profiling:
- Oxidative Stress: Load cells with DCFH-DA dye, expose to NPs, and measure fluorescence intensity corresponding to ROS generation.
- Mitochondrial Function: Stain NP-exposed cells with JC-1 dye and analyze the shift from red (healthy) to green (depolarized) fluorescence.
- Lysosomal Integrity: Stain with Acridine Orange; a loss of red fluorescence indicates lysosomal membrane permeabilization.
- In Vivo Correlation: Adminerve NPs (e.g., via inhalation) to mouse models and assess bronchoalveolar lavage fluid for inflammatory cell infiltrate and pro-inflammatory cytokines to correlate in vitro findings with in vivo airway inflammation.
- Key Interpretation: This protocol establishes that surface charge density, not just the absolute ζ-potential, is a critical descriptor for predicting NP toxicity. High charge density correlates with significant viability loss, oxidative stress, and inflammation [6].
Protocol 2: Assessing Nanoparticle-Membrane Interactions via Computational Simulation
This protocol outlines a computational approach to systematically study the synergistic effects of NP properties on cellular entry pathways [10].
- Objective: To simulate and categorize the interactions between monolayer-protected nanoparticles and model cell membranes.
- Materials:
- High-performance computing (HPC) cluster.
- Molecular dynamics (MD) simulation software (e.g., GROMACS, NAMD).
- Coarse-grained or all-atom force fields.
- Procedure:
- System Setup:
- Parameter Space: Define a 3D parameter space: NP size (3-15 nm), surface charge/pKa (total charge from 0-140 e), and ligand chemistry (hydrophobic alkyls vs. hydrophilic PEG).
- Membrane Model: Construct a model cell membrane composed of zwitterionic DPPC lipids in a bilayer configuration.
- Simulation Box: Place the NP above the membrane surface in an aqueous solution with an ionic imbalance to create a transmembrane potential.
- Simulation Run:
- Equilibrate the system with the NP's position restrained for 0.2 µs.
- Release the NP and allow it to interact freely with the membrane for 1.2 µs of simulation time.
- Trajectory Analysis: Analyze the simulation output to categorize the final outcome of the interaction into one of four types:
- Outer Wrap: Membrane wraps the NP but no translocation; leads to endocytosis.
- Free Translocate: NP completely translocates across the membrane via a pore into the cytosol.
- Embedment: NP partially translocates and remains stably embedded within the membrane.
- Inner Attach: NP mostly translocates but remains attached to the inner membrane leaflet.
- System Setup:
- Key Interpretation: This simulation reveals that cellular entry pathways are determined synergistically by size, charge, and chemistry. Smaller, highly charged, hydrophilic NPs favor free translocation, while larger, less charged, hydrophobic NPs favor embedding or outer wrapping [10].
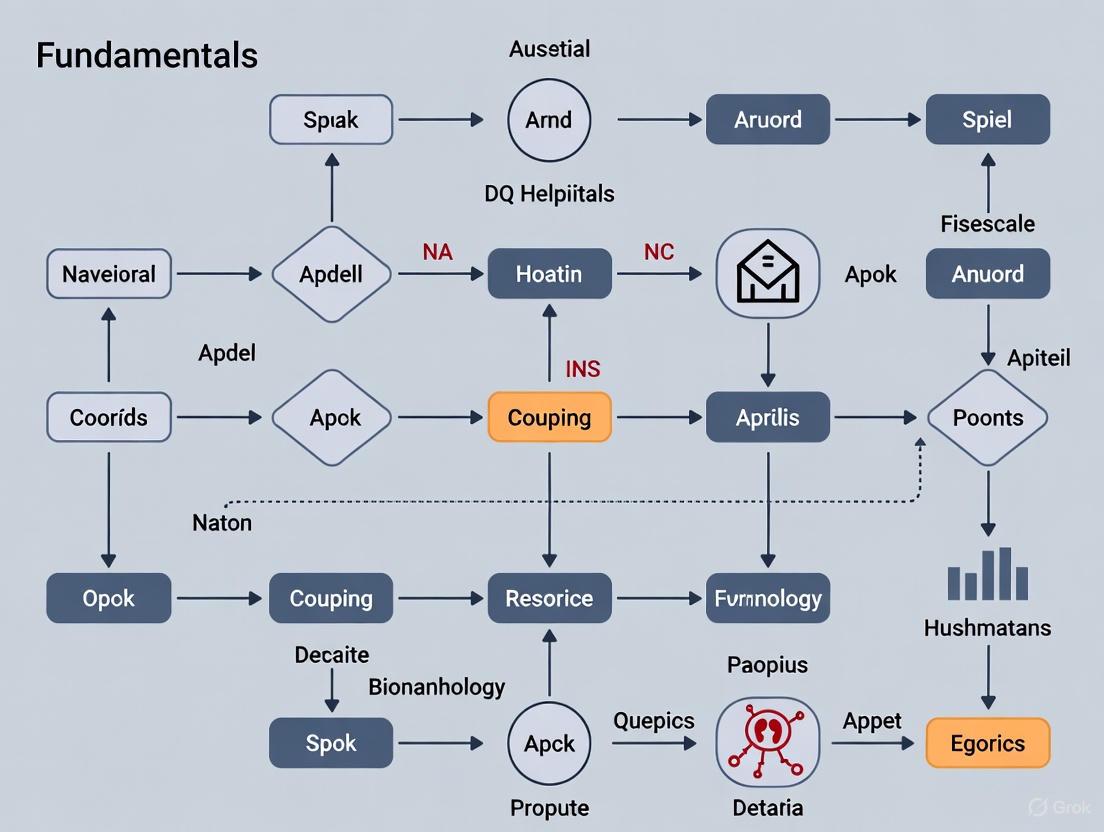
The following diagram illustrates the logical decision process for predicting nanoparticle-membrane interactions based on key physicochemical properties, as revealed by computational studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Nano-Bio Interaction Research
| Item | Function/Application | Specific Examples from Literature |
|---|---|---|
| Cationic Polymers | Functionalizing NPs to impart positive surface charge; nucleic acid condensation for gene delivery. | Branched Polyethylenimine (bPEI) of varying molecular weights (600 Da - 25 kDa) used to create carbon dots with high surface charge density [6]. |
| PEG (Polyethylene Glycol) | Surface coating to provide "stealth" properties, reduce protein adsorption, and prolong circulation half-life. | PEGylated liposomes (e.g., Doxil) show increased bioavailability and prolonged circulation [4]. PEG is a dominant coating in biodistribution studies [1]. |
| Amino Acids & Polyphenols | Acting as reducing and stabilizing agents in the "green" synthesis of bioactive metal nanoparticles. | Tyrosine, Tryptophan, Epigallocatechin Gallate (EGCG), and Curcumin used to synthesize and form a surface corona on gold and silver NPs [2]. |
| Dynamic Light Scattering (DLS) / ZetaSizer | Characterizing hydrodynamic size, size distribution (PDI), and zeta potential of nanoparticles in suspension. | Used to measure hydrodynamic diameter and ζ-potential of NPs in biological buffers [5] [2] [6]. |
| Atomic Force Microscopy (AFM) | High-resolution imaging of nanoparticle morphology, size, and surface roughness; also used to image NP-bacterial cell interactions. | Employed to determine the shape, size, and surface roughness of metal NPs and to visualize Rhodococcus cells after NP exposure [5]. |
The intricate biological interactions of nanoparticles are decisively guided by the triumvirate of size, surface charge, and hydrophobicity. A systematic and quantitative understanding of these properties is non-negotiable for advancing nanomedicine and conducting accurate nanotoxicological assessments. The experimental and computational methodologies outlined herein provide a robust framework for researchers to deconvolute these complex interactions. Future research must continue to embrace a holistic, multi-parameter approach to navigate the bio-nano interface, enabling the rational design of next-generation nanotherapeutics with optimized efficacy and safety profiles.
Upon entering a biological environment, nanoparticles (NPs) are rapidly coated by a dynamic layer of biomolecules, primarily proteins, forming what is known as the protein corona (PC) [11]. This biomolecular coating fundamentally redefines the nanoparticle's biological identity, dictating its subsequent interactions with biological systems [11] [12]. Rather than the pristine nanoparticle surface, it is the protein corona that is "seen" by cells, influencing critical outcomes such as cellular uptake, biodistribution, toxicity, and therapeutic efficacy [11] [13]. Understanding the composition, dynamics, and influence of the protein corona is therefore not merely an academic exercise but a prerequisite for the rational design of effective nanomedicines and the accurate assessment of nanomaterial safety [12] [14]. This guide provides an in-depth technical examination of protein corona formation, its determining factors, analytical methodologies, and its profound impact on nanoparticle fate within the context of nanoscale biological interactions research.
The Fundamentals of Protein Corona Formation and Structure
The formation of the protein corona is a spontaneous and dynamic process initiated the moment a nanoparticle encounters a biological fluid [14]. The structure is typically conceptualized in two distinct layers:
- The Hard Corona: Comprises proteins with high affinity for the nanoparticle surface, forming a stable, tightly bound layer through electrostatic, hydrophobic, and hydrogen-bond interactions [11] [14]. This layer is relatively persistent and can remain attached for extended periods, even under dynamic biological conditions [14].
- The Soft Corona: Consists of proteins that are weakly associated with the hard corona or the nanoparticle surface itself through low-affinity, reversible interactions [12] [14]. This outer layer is highly dynamic, with a composition that fluctuates rapidly in response to changes in the surrounding environment [14].
This division is critical because the hard corona often dictates the long-term biological identity of the nanoparticle, while the soft corona can influence more transient interactions [12]. The entire structure is not static; it undergoes continuous evolution and re-equilibration as the nanoparticle transitions between different biological compartments (e.g., from blood to interstitial fluid), in a process that confers a form of molecular "memory" of the nanoparticle's journey through the body [14].
Table 1: Core Components of the Biomolecular Corona
| Component Type | Example Molecules | Significance & Interaction Mechanism |
|---|---|---|
| Proteins | Albumin, Immunoglobulins, Apolipoproteins (e.g., ApoE, ApoA1), Complement factors [11] [13] | Determine biological response; adsorb via electrostatic/hydrophobic interactions [11] [14]. |
| Lipids | Phospholipids, Cholesterol, Fatty Acids, Triglycerides [14] | Contribute to structural stability and enhance biological mimicry through hydrophobic interactions [14]. |
| Other Biomolecules | Metabolites, Nucleic Acids, Carbohydrates [12] | Form a "complete corona"; can shape signaling and toxicity pathways [12]. |
Factors Governing Corona Composition and Dynamics
The precise composition of the protein corona is not random but is selectively determined by a complex interplay of nanoparticle physicochemical properties and biological environment factors [11] [12].
Nanoparticle Physicochemical Properties
- Size and Surface Curvature: Smaller nanoparticles, with their higher surface curvature and surface-to-volume ratio, exhibit different protein binding affinities and capacities compared to larger particles [11] [12].
- Surface Charge (Zeta Potential): Positively charged nanoparticles often exhibit more abundant protein adsorption due to electrostatic interactions with negatively charged domains of proteins [11]. Surface charge is consistently identified as one of the most significant NP-related predictors in machine learning models of corona composition [15].
- Surface Chemistry and Hydrophobicity: Hydrophobic surfaces tend to adsorb a greater amount of protein and can induce protein unfolding, leading to a more stable and less dynamic corona [14]. Surface functionalization (e.g., with carboxyl or amine groups) directly influences which proteins adsorb [12] [16].
- Core Material and Shape: The core material (e.g., gold, silica, lipid, iron oxide) and the geometric shape of the nanoparticle also contribute to the biological identity of the corona [11] [15].
Biological and Environmental Factors
- Protein Source and Concentration: The composition of the surrounding biological fluid (e.g., blood plasma, fetal bovine serum, interstitial fluid) is a primary determinant. The relative abundance of proteins in the biofluid is the most significant predictor of corona composition, as identified by machine learning models [15].
- Temporal Evolution: The corona is not static. The "Vroman effect" describes the dynamic process where proteins with high concentration and mobility (like albumin) arrive first at the nanoparticle surface but are later displaced by proteins with higher affinity, even if they are less abundant [14].
- pH and Temperature: Local environmental conditions such as pH and temperature can modulate protein structure and binding affinity, thereby influencing corona composition and stability [11].
Figure 1: Dynamics of Protein Corona Formation. The process involves initial adsorption influenced by NP properties, followed by dynamic exchange governed by the Vroman effect and environmental factors, ultimately establishing a stable hard corona, a dynamic soft corona, and a new biological identity.
Analytical Techniques for Protein Corona Characterization
Accurately characterizing the protein corona is methodologically challenging due to its dynamic nature and the risk of introducing artifacts during isolation [13] [14]. The following techniques are commonly employed, often in combination:
Separation and Isolation Techniques:
- Density Gradient Ultracentrifugation (DGU): A gentle method that separates protein-NP complexes from unbound proteins and endogenous biomolecules based on buoyant density. Critical for studying low-density nanoparticles like lipid NPs (LNPs) without inducing aggregation [13].
- Size Exclusion Chromatography (SEC): Separates complexes based on hydrodynamic size, helping to isolate them from free protein [13].
- Magnetic and Affinity-Based Separations: Useful for high-throughput studies but may require NP surface modification, which can alter the corona formation process [13].
Characterization and Identification Techniques:
- Dynamic Light Scattering (DLS) and Zeta Potential Measurement: Used to determine the hydrodynamic size and surface charge of nanoparticles before and after corona formation, providing information on adsorption and stability [11] [16].
- Mass Spectrometry (MS)-Based Proteomics: The gold standard for identifying and quantifying the protein composition of the corona. Liquid Chromatography-MS (LC-MS) enables deep, unbiased profiling of corona proteins [13] [17].
- Isothermal Titration Calorimetry (ITC): Measures the thermodynamics of protein-NP interactions, including binding affinity, stoichiometry, and enthalpy changes [11].
- Circular Dichroism (CD) Spectroscopy: Assesses whether proteins undergo structural changes (e.g., denaturation) upon adsorption to the nanoparticle surface [16].
- Cryogenic Electron Microscopy (Cryo-EM): Allows for direct visualization of the protein corona structure in a near-native state [14].
Table 2: Key Experimental Techniques for Protein Corona Research
| Technique | Key Measurable Parameters | Key Advantages | Common Challenges/Limitations |
|---|---|---|---|
| Density Gradient Ultracentrifugation | Buoyant density of protein-NP complexes [13]. | Gentle; preserves corona integrity; no modification needed [13]. | Time-consuming; requires optimization to separate from endogenous particles [13]. |
| Dynamic Light Scattering (DLS) | Hydrodynamic diameter, polydispersity index (PDI) [11] [16]. | Fast; requires minimal sample preparation [11]. | Assumes spherical particles; sensitive to aggregates and dust [11]. |
| LC-MS Proteomics | Protein identity, relative/absolute abundance [13] [17]. | High-throughput; unbiased; deep coverage [17]. | Can be masked by highly abundant proteins; requires sophisticated data analysis [14]. |
| Isothermal Titration Calorimetry | Binding constants (Kd), enthalpy (ΔH), stoichiometry (n) [11]. | Provides thermodynamic profile of interactions; label-free [11]. | Low throughput; requires significant amounts of sample [11]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Protein Corona Studies
| Reagent/Material | Function in Experimental Workflow | Specific Examples & Notes |
|---|---|---|
| Nanoparticle Cores | Serves as the substrate for corona formation; core material is a key variable [15]. | Gold (Au), iron oxide (magnetic), polystyrene (PS), silica (SiO₂), lipid nanoparticles (LNPs) [15] [13]. |
| Surface Ligands/Functionalizers | Modifies NP surface properties to study its impact on protein adsorption [15]. | Polyethylene glycol (PEG), carboxyl groups (-COOH), amine groups (-NH₂), citrate [15] [18] [16]. |
| Protein Sources | Provides the biological fluid environment for corona formation [15]. | Fetal Bovine Serum (FBS), human plasma, mouse plasma [15] [16]. Critical to note interspecies differences [16]. |
| Stealth Proteins | Used for pre-coating ("engineering") the corona to achieve desired biological outcomes [16]. | Clusterin (ApoJ), Apolipoprotein A1 (ApoA1). Their adsorption confers "stealth" properties [16]. |
| Proteomics Kits & Reagents | For sample preparation, digestion, and analysis in mass spectrometry [17]. | Proteograph Product Suite (uses multiplexed NPs for deep plasma proteomics) [17]. |
Impact on Nanomedicine: Therapeutic Efficacy and Safety
The protein corona directly impacts every aspect of a nanoparticle's performance in biomedical applications, often creating a paradox where it can either hinder or enhance functionality.
Disruption of Targeting and Accelerated Clearance
A primary challenge in nanomedicine is the uncontrolled formation of a protein corona, which can:
- Mask Targeting Ligands: Antibodies or other targeting moieties conjugated to the nanoparticle surface can be obscured by adsorbed proteins, preventing recognition of the intended cell surface receptor [18].
- Induce Opsonization: The adsorption of certain proteins (opsonins) can tag the nanoparticle for rapid recognition and clearance by phagocytic cells of the mononuclear phagocyte system (MPS), primarily in the liver and spleen [11] [18]. This accelerated blood clearance (ABC) drastically reduces circulation half-life and delivery to the target tissue [11].
Strategic Exploitation of the Corona
Conversely, a growing research focus is on strategically exploiting the corona for beneficial outcomes:
- Engineered Stealth Coronas: Pre-coating nanoparticles with specific "dysopsonin" proteins like clusterin or ApoA1 can create a stealth corona that reduces immune recognition and extends circulation time [16]. The stability of this pre-formed corona in full plasma is a critical area of investigation [16].
- Leveraging Natural Targeting: The protein corona can be harnessed for natural targeting. For instance, the adsorption of Apolipoprotein E (ApoE) on lipid nanoparticles facilitates their uptake by hepatocytes via low-density lipoprotein receptors, a phenomenon that underpins the liver tropism of many LNP-based therapies [13].
- Biomimetic Coating Strategies: A powerful approach to control the bio-interface is to coat nanoparticles with natural cell membranes (e.g., from red blood cells, white blood cells, or cancer cells) [18] [19]. This top-down strategy endows the nanoparticle with the complex biological signaling functions of the source cell, enabling long circulation, immune evasion, or specific targeting [18].
Emerging Frontiers: AI Prediction and Advanced Materials
The field is rapidly evolving with the integration of new computational and design tools.
- Artificial Intelligence and Machine Learning: The use of AI/ML to predict corona composition is a transformative approach to overcome the time and cost constraints of experimental methods. Random Forest models have been successfully trained on datasets of NP features (e.g., size, zeta potential), protein features, and experimental conditions to predict protein abundance and enrichment on nanoparticles with high accuracy [11] [15]. These models consistently identify protein abundance in the biofluid, NP zeta potential, and hydrodynamic diameter as the most important predictive features [15].
- Extension to Emerging Materials: The protein corona concept is now being applied to newer material classes like metal-organic frameworks (MOFs), where corona formation can either stabilize or destabilize the framework and modulate its function [12].
- The "Complete Corona": Moving beyond a protein-centric view, the concept of the "complete corona" acknowledges the integral role of metabolites, lipids, and other small molecules in conjunction with proteins to determine a nanoparticle's biological fate [12].
Figure 2: Machine Learning Workflow for Corona Prediction. Random Forest and other ML models integrate features from nanoparticles, proteins, and experimental conditions to predict corona composition, aiding rational NP design.
Detailed Experimental Protocol: Characterizing the LNP Protein Corona
The following protocol, adapted from current research, details a robust method for isolating and characterizing the protein corona on lipid nanoparticles, a clinically critical nanomaterial [13].
Objective: To isolate the hard protein corona from LNPs incubated in human plasma and identify its composition using label-free quantitative mass spectrometry proteomics, while avoiding co-isolation of endogenous plasma particles.
Materials:
- Lipid Nanoparticles (LNPs): Synthesized, e.g., with the ionizable lipidoid 306O10 [13].
- Biological Fluid: Human blood plasma (K2EDTA anticoagulant).
- Density Gradient Medium: OptiPrep or equivalent iodixanol solution.
- Equipment: Ultracentrifuge, swinging-bucket rotor, fractionation system, LC-MS system.
Procedure:
Corona Formation:
- Incurate LNPs (e.g., at a concentration of 1-2 mg/mL lipid) with human plasma (e.g., 90% plasma v/v) for 1 hour at 37°C with gentle agitation [13].
Density Gradient Ultracentrifugation (DGU) - Critical Step:
- Prepare a continuous density gradient (e.g., 0-30% iodixanol) in an ultracentrifuge tube.
- Carefully layer the LNP-plasma incubation mixture on top of the gradient.
- Centrifuge at 200,000 × g for 16-18 hours at 4°C [13]. Note: This extended duration is crucial for effective separation of LNPs from denser endogenous particles like lipoproteins and exosomes.
- After centrifugation, fractionate the gradient from the top. LNP-protein complexes will be found in low-density fractions.
Sample Preparation for Proteomics:
- Recover the LNP-containing fractions.
- Digest the proteins in these fractions using a standard tryptic digestion protocol (e.g., reduction with dithiothreitol, alkylation with iodoacetamide, and overnight trypsin digestion).
- Desalt the resulting peptides using C18 solid-phase extraction tips or columns.
LC-MS Analysis and Data Processing:
- Analyze the peptides by nano-flow Liquid Chromatography coupled to a high-resolution Mass Spectrometer (e.g., Orbitrap Astral or Exploris series) operating in Data-Independent Acquisition (DIA) mode [13] [17].
- Process the raw MS data using specialized software (e.g., DIA-NN) against a human protein sequence database.
- Normalize protein intensities to those found in a control sample of plasma processed without LNPs to distinguish truly enriched "corona proteins" from background [13].
Key Considerations:
- Controls: Always include a "plasma-only" control processed identically to account for endogenous particles.
- Stability: Monitor LNP size and integrity post-DGU via DLS to ensure the isolation process did not cause aggregation or disruption.
- Validation: Functional validation of findings (e.g., via cellular uptake assays with pre-coated LNPs) is essential to link corona composition to biological effect [13].
The protein corona is an inescapable and defining interface in nanomedicine and nanotoxicology. Its composition, governed by the complex interplay of nanoparticle properties and biological environment, ultimately dictates the biological fate of nanomaterials. While the uncontrolled formation of a corona presents a significant barrier to targeted delivery, the strategic engineering of this layer—through pre-coating, biomimetic membrane cloaking, or rational design informed by AI—offers a powerful pathway to overcome these challenges. Future research focused on understanding the "complete corona," its evolution in dynamic physiological systems, and its specific impact on intracellular trafficking will be critical to fully harnessing the potential of nanotechnology in medicine. The ability to predict and control the protein corona represents the key to unlocking the next generation of safe, effective, and precisely targeted nanotherapeutics.
Nanoparticles have transformed contemporary medicine by improving the bioavailability, targeting, and release mechanisms of therapeutic agents [20]. The cellular internalization of nanomaterials is a critical process governing the efficacy of nanomedicines, influencing their distribution, subcellular localization, and eventual biological activity. Understanding these uptake mechanisms is fundamental to designing advanced drug delivery systems that can overcome biological barriers and achieve precise targeting [21]. This review provides a comprehensive technical analysis of the endocytosis pathways and intracellular trafficking behavior of nanomaterials, framed within the broader context of nanoscale biological interactions research for therapeutic applications.
The cellular uptake of nano- and microparticles has been extensively studied in static two-dimensional (2D) in vitro cultures, with thousands of publications exploring these phenomena [22]. However, the relevance of these studies for in vivo applications remains debatable, and the lack of standardized protocols makes comparative analysis challenging. This technical guide aims to synthesize current understanding while emphasizing quantitative parameters and methodologies essential for researchers and drug development professionals working in nanomedicine [22].
Fundamental Mechanisms of Nanoparticle Uptake
Sequential Uptake Process
Nanoparticle internalization by cells follows a multi-step process governed by complex biophysical interactions. In standard in vitro conditions, particles first reach cells through diffusion and sedimentation [22]. Upon contact, particles may adhere to the outer cell membrane through specific receptor-ligand interactions or non-specific forces such as electrostatic attraction [22]. Following a variable dwelling period, particles are typically internalized via endocytosis and subsequently trafficked through endosomal-lysosomal compartments [22]. The intracellular fate involves potential exocytosis, dilution during cell division, or sustained retention depending on particle characteristics and cell type [22].
Key Endocytosis Pathways
Different nanoparticle properties activate distinct endocytic mechanisms, each with unique characteristics and functional implications:
- Clathrin-Mediated Endocytosis (CME): A receptor-mediated pathway utilized by specific ligands, such as the internalization of Fe₂O₃ nanoparticles in the liver via LDLR and TFR1 receptors [23].
- Caveolae-Mediated Endocytosis: Involves flask-shaped membrane invaginations and can bypass lysosomal degradation.
- CLEC4E-Mediated Pathway: A clathrin- and caveolae-independent pathway identified as the primary mechanism for Fe₂O₃ nanoparticle uptake in the intestine [23].
- Macropinocytosis: A receptor-independent process involving actin-driven membrane ruffling that internalizes large volumes of extracellular fluid.
The selective activation of these pathways depends on the unique biomolecular corona that forms on nanoparticle surfaces in different biological milieus [23]. Studies demonstrate that identical nanoparticles can be internalized through distinct tissue-specific mechanisms depending on their corona composition [23].
Quantitative Analysis of Cellular Uptake
Essential Parameters for Quantification
Accurate quantification of nanoparticle uptake requires careful consideration of multiple experimental parameters that significantly influence results [22]. The table below summarizes critical factors that must be documented to enable meaningful cross-study comparisons.
Table 1: Essential Experimental Parameters for Quantitative Uptake Studies
| Parameter Category | Specific Factors | Impact on Uptake Quantification |
|---|---|---|
| Particle Characteristics | Concentration metrics (molar, mass, elemental), colloidal stability, batch-to-batch variation, degradation profile | Different metrics cannot be unequivocally converted; agglomeration enhances sedimentation and artificial uptake [22]. |
| Cell Culture Conditions | Cell density, medium height/volume, medium composition (serum content), proliferation rate, cell surface area/volume | Higher particle concentration in smaller volume increases uptake rate; serum depletion enhances uptake [22]. |
| Exposure Conditions | Incubation time, confluency state, temperature, particle-to-cell ratio | Uptake depends on cell density; incubation must be contextualized with proliferation rate [22]. |
Quantitative Uptake Parameters
Moving beyond qualitative descriptions ("better/faster/more"), rigorous quantification requires specific parameters extracted from uptake kinetics [22]. The "intensity" of particles per cell (I) plotted against incubation time (t) typically follows a saturating exponential curve, characterized by the maximum uptake (Iₘₐₓ) and the rate constant (k) [22]. These parameters allow direct comparison between different particle systems and cell types.
Methodologies for Uptake Quantification
Multiple analytical techniques are employed to quantify nanoparticle internalization, each with distinct advantages, limitations, and appropriate applications.
Table 2: Methodologies for Quantifying Nanoparticle Uptake by Cells
| Methodology | Measured Parameter | Advantages | Limitations |
|---|---|---|---|
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Elemental concentration [22] | High sensitivity, quantitative [22] | Cannot distinguish internalized vs. membrane-adherent particles [22] |
| Fluorescence Spectroscopy/ Microscopy | Fluorescence intensity [22] | Spatial resolution, live-cell capability [22] | pH-dependent quenching, fluorophore bleaching [22] |
| Single Particle Tracking | Individual particle movement [22] | Reveals real-time kinetics [22] | Technically challenging, limited throughput [22] |
| Flow Cytometry | Population-average fluorescence [22] | High-throughput, statistical power [22] | No subcellular localization [22] |
Experimental Protocols
Protocol for Quantitative Uptake Using Elemental Analysis
- Cell Culture: Seed cells at precisely defined density (e.g., 50,000 cells/cm²) in standard multi-well plates and culture until desired confluency [22].
- Particle Exposure: Prepare particle suspensions in relevant culture medium, noting exact volume and height above cells. Apply to cells for predetermined incubation periods [22].
- Removal of Adherent Particles: After incubation, remove extracellular particles through extensive washing. Optional: Use digestive enzymes (trypsin) or chemical etching for extracellular particles when using elemental analysis [22].
- Sample Digestion: Lyse cells using appropriate digesting agents (e.g., nitric acid for metal-based nanoparticles) to completely liberate particulate elements [22].
- Quantification: Analyze digested samples using ICP-MS to determine elemental concentrations. Calculate particles per cell using standard curves and known cell counts [22].
Protocol for Distinguishing Internalized from Surface-Bound Particles
For fluorescence-based studies, these methods can differentiate internalized particles:
- Chemical Quenching: Add non-membrane-permeant quenchers (e.g., metal ions for quantum dots) to extinguish fluorescence from extracellular particles while preserving intracellular signal [22].
- Immunostaining: Colocalize particles with antibodies against endosomal/lysosomal markers (LAMP1, EEA1) to confirm intracellular localization [22].
- pH-Sensing: Use pH-sensitive fluorophores that activate only in acidic endolysosomal compartments [22].
Intestinal Barriers and Nanoparticle Uptake
Targeting the small intestine employing nanotechnology represents a promising approach for oral drug delivery due to its extensive surface area (300-400 m²) and less harsh environment compared to the stomach [21]. However, nanoparticles must overcome significant intestinal barriers to reach systemic circulation.
Mucus Barrier Penetration
The mucus layer, a hydrogel composed primarily of MUC2 mucin glycoproteins secreted by goblet cells, forms the primary physical barrier to oral nanoparticles [21]. This layer varies in thickness from 10-200 μm throughout the intestinal tract and is continuously shed and renewed [21]. Strategies to enhance mucus penetration include:
- Mucus-Penetrating Particles (MPPs): Surface functionalization with low molecular weight polyethylene glycol (PEG) chains creates neutral, hydrophilic surfaces that minimize mucin interactions [21].
- Surface Engineering: Dense charge-bearing neutral hydrophilic surfaces or albumin functionalization reduce mucus binding [21].
- Enzyme Modification: Nanoparticle decoration with proteolytic enzymes (e.g., papain) degrades mucoglycoprotein substructures to enhance penetration [21].
Epithelial Translocation
After penetrating the mucus, nanoparticles must cross the epithelial layer through either paracellular (between cells) or transcellular (through cells) pathways:
- Paracellular Transport: Involves temporary opening of tight junctions using permeation enhancers like chitosan [21].
- Transcellular Transport: Utilizes various endocytic pathways, with M-cells and enterocytes being the primary portals for nanoparticle internalization [21].
Visualizing Uptake Pathways and Experimental Workflows
Endocytosis Pathway Diagram
Quantitative Uptake Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Nanoparticle Uptake Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Endocytic Inhibitors | Chlorpromazine (CME inhibitor), Filipin (caveolae inhibitor), Amiloride (macropinocytosis inhibitor) | Pathway-specific mechanistic studies to determine dominant uptake routes [23] |
| Fluorescent Tags | pH-sensitive dyes (LysoTracker), quantum dots, fluorescent antibodies against endosomal markers | Particle tracking and subcellular localization confirmation [22] |
| Surface Modifiers | Polyethylene glycol (PEG), chitosan, albumin, targeting ligands (RGD peptides, transferrin) | Enhanced stability, mucus penetration, and targeted cellular delivery [21] |
| Analytical Standards | Certified reference materials, standardized particle batches | Method validation and cross-study comparison [22] |
| Cell Culture Supplements | Defined serum concentrations, viability assay kits (MTT, WST-8) | Controlled exposure conditions and cytotoxicity assessment [22] |
The cellular uptake mechanisms of nanomaterials represent a complex interplay between particle physicochemical properties and biological systems. Understanding these processes at quantitative levels enables rational design of nanomedicines with optimized targeting and therapeutic efficacy. Future directions include developing standardized protocols for uptake quantification, advancing real-time imaging methodologies, and creating more sophisticated in vitro models that better recapitulate in vivo conditions. As research progresses, the integration of artificial intelligence and tailored nanomedicine design promises to further enhance our ability to manipulate these fundamental nanoscale biological interactions for improved therapeutic outcomes.
The efficacy of nanodelivery systems is fundamentally constrained by a series of biological barriers that impede the journey of a nanocarrier from the point of administration to its intended site of action within the body. These barriers operate sequentially and in concert, significantly limiting the bioavailability and therapeutic potential of nanomedicines. The first major hurdle is systemic circulation, where nanocarriers must navigate the vascular system while resisting opsonization and clearance by the mononuclear phagocyte system (MPS). The second barrier is immune clearance, primarily mediated by the liver and spleen, which rapidly identify and remove foreign particles from the bloodstream. The final and perhaps most formidable barrier is tissue penetration, where nanocarriers must extravasate from the vasculature and diffuse through dense extracellular matrices to reach target cells. Understanding the mechanisms of these barriers is paramount for the rational design of advanced nanodelivery systems that can overcome these challenges. This guide provides a comprehensive technical overview of these barriers, supported by quantitative data, experimental methodologies, and visualization tools for researchers in nanoscale biological interactions.
Blood Circulation Barrier
Physiological Challenges and Clearance Mechanisms
Upon intravenous administration, nanocarriers enter a dynamic and hostile environment within the bloodstream. The primary challenge in systemic circulation is prolonged retention, as the body's innate defense mechanisms work to clear foreign particles. The mononuclear phagocyte system (MPS), also known as the reticuloendothelial system (RES), plays a pivotal role in this clearance, with macrophages in the liver (Kupffer cells) and spleen rapidly sequestering nanoparticles from circulation. Opsonization—the adsorption of plasma proteins (opsonins) such as immunoglobulins, complement proteins, and fibronectin onto the nanoparticle surface—serves as a biological tag that facilitates recognition and phagocytosis by MPS cells. The rate of clearance is influenced by several physicochemical properties of the nanocarriers, including size, surface charge, and hydrophobicity. For instance, larger particles (>200 nm) are typically cleared faster than smaller ones, and positively charged particles exhibit higher opsonization rates compared to their neutral or negatively charged counterparts.
Table 1: Impact of Nanoparticle Physicochemical Properties on Blood Circulation Half-life
| Property | Impact on Circulation | Optimal Range | Mechanism |
|---|---|---|---|
| Size | Determines MPS uptake and renal clearance | 10-100 nm | Particles <10 nm undergo renal clearance; >200 nm are sequestered by MPS [24] |
| Surface Charge | Affects opsonin protein adsorption | Neutral or Slightly Negative | Cationic surfaces promote opsonization and MPS uptake [24] |
| Hydrophobicity | Increases nonspecific protein adsorption | Hydrophilic | Hydrophobic surfaces attract more opsonins [25] |
| Shape | Influences margination and flow dynamics | Spherical or Ellipsoidal | Rod-shaped particles may exhibit longer circulation times than spherical ones [26] |
Strategic Solutions and Surface Engineering
To circumvent rapid clearance, surface functionalization has emerged as a primary strategy. PEGylation—the covalent attachment of poly(ethylene glycol) (PEG) chains—creates a hydrophilic steric barrier that reduces protein adsorption and MPS recognition, thereby extending circulation half-life. This "stealth" effect is the foundation of several clinically approved nanomedicines. More recently, biomimetic camouflage has shown remarkable promise. This involves coating synthetic nanocarriers with natural cell membranes (e.g., from erythrocytes, leukocytes, or platelets) to confer the nanoparticles with the same biological properties as the source cells. For example, erythrocyte membrane-coated nanoparticles display "self-marker" proteins like CD47, which binds to signal regulatory protein alpha (SIRPα) on macrophages and transmits a "don't eat me" signal, effectively evading immune clearance.
Immune Clearance Barrier
Mechanisms of Immune Recognition
The immune system provides a sophisticated and multi-layered defense against nanocarriers that survive the initial MPS filtration. Immune clearance involves both innate and adaptive components. The complement system can be activated by nanoparticles via the classical, lectin, or alternative pathways, leading to opsonization by C3b and formation of the membrane attack complex (MAC), which can lyse certain lipid-based nanocarriers. Furthermore, nanoparticles can be recognized by pattern recognition receptors (PRRs) on immune cells, triggering inflammatory responses and phagocytosis. A significant challenge in nanodelivery is the accelerated blood clearance (ABC) phenomenon, wherein repeated administration of PEGylated nanoparticles can induce anti-PEG IgM antibodies, leading to rapid clearance of subsequent doses.
Biomimetic Strategies for Immune Evasion
Biomimetic nanoplatforms represent a paradigm shift in overcoming immune clearance. By leveraging the natural biology of cells, these platforms are endowed with complex, biologically derived surfaces that are inherently adept at evading immune surveillance.
Table 2: Cell Membrane-Coated Nanoplatforms for Immune Evasion
| Membrane Source | Key "Self" Markers | Primary Evasion Mechanism | Application Context |
|---|---|---|---|
| Erythrocyte (Red Blood Cell) | CD47 | CD47-SIRPα "don't eat me" signaling [25] | Systemic circulation, prolonged delivery |
| Leukocyte (White Blood Cell) | CD45, CD47 | Mimics "self" leukocyte identity [25] | Targeting inflammatory and tumor sites |
| Platelet | CD47, CD55, CD59 | Evasion of phagocytosis and complement [27] [25] | Targeting damaged vasculature and thrombi |
| Cancer Cell | CD47, MHC-I | Homotypic targeting (homing to source tumor) [25] | Drug delivery to primary tumors and metastases |
The following diagram illustrates the core mechanism of how these biomimetic nanoparticles achieve immune evasion.
Tissue Penetration Barrier
The Tumor Microenvironment as a Model Challenge
The pathophysiological nature of solid tumors exemplifies the extreme challenge of tissue penetration. While the enhanced permeability and retention (EPR) effect allows nanocarriers of a certain size (typically 10-200 nm) to extravasate through the leaky vasculature of tumors, their subsequent penetration into the tumor core is severely limited. The tumor microenvironment (TME) presents multiple obstacles: a dense extracellular matrix (ECM) rich in collagen and hyaluronic acid creates a physical barrier; high interstitial fluid pressure due to poor lymphatic drainage induces an outward convective force that opposes inward diffusion; and the complex architecture of cancer cells and stromal cells further hinders deep penetration. Consequently, nanoparticles often accumulate perivascularly, leading to heterogeneous drug distribution and suboptimal therapeutic outcomes.
Advanced Engineering Strategies for Enhanced Penetration
Innovative nanocarrier designs that can dynamically respond to the TME are critical for overcoming the penetration barrier. Key strategies include:
- Size-Transformable Nanosystems: These carriers are designed to undergo a size shift from large (>100 nm) to small (<50 nm) upon encountering a specific tumor-specific stimulus. The larger size is beneficial for prolonged circulation and initial tumor accumulation via the EPR effect, while the smaller size post-transformation enables deeper penetration into the tumor parenchyma.
- Charge-Reversal Nanoparticles: The surface charge of these nanocarriers is initially negative or neutral during circulation to minimize protein adsorption and MPS uptake. Upon entering the acidic TME (pH ~6.5-6.8), the surface chemistry triggers a switch to a positive charge, which enhances cellular uptake by facilitating interaction with the negatively charged cell membranes.
- Enzyme-Responsive Systems: These are engineered to be degraded or modified by enzymes that are overexpressed in the TME, such as matrix metalloproteinases (MMPs) or hyaluronidases. For instance, a nanocarrier can be decorated with a PEG corona linked via an MMP-cleavable peptide; upon reaching the tumor, MMPs cleave the peptide, shedding the PEG layer and potentially exposing a hidden, cell-penetrating surface.
The following workflow diagram summarizes the multi-stage journey of a nanocarrier and the design strategies employed to overcome each barrier.
Experimental Protocols for Characterization
Protocol: Quantifying Blood Circulation Half-life
Objective: To determine the pharmacokinetic profile and circulation half-life of a novel nanocarrier in a murine model.
Materials:
- Radiolabeled (e.g., 125I) or fluorescently labeled (e.g., DiR) nanocarrier.
- Animal model (e.g., BALB/c mice).
- Microcentrifuge tubes.
- Gamma counter or IVIS imaging system.
- Heparinized capillary tubes or equipment for retro-orbital bleeding.
Procedure:
- Administer the labeled nanocarrier to mice via tail vein injection (dose: e.g., 10 mg/kg).
- At predetermined time points (e.g., 0.08, 0.25, 0.5, 1, 2, 4, 8, 12, 24 hours) post-injection, collect blood samples (e.g., ~20 μL per time point) via retro-orbital bleeding or tail nick into heparinized tubes.
- Lyse the blood cells if necessary and measure the radioactivity or fluorescence intensity in each sample using a gamma counter or plate reader.
- Express the data as the percentage of injected dose per gram of blood (%ID/g) or milliliter (%ID/mL) over time.
- Fit the blood concentration-time data to a two-compartment pharmacokinetic model using software like Phoenix WinNonlin to calculate the alpha half-life (distribution phase, t1/2α) and beta half-life (elimination phase, t1/2β).
Protocol: Assessing Tumor Penetration Depth
Objective: To visualize and quantify the spatial distribution and penetration depth of nanocarriers within a tumor spheroid or ex vivo tumor tissue.
Materials:
- Fluorescently labeled nanocarrier.
- 3D Tumor spheroids (e.g., from U87MG cells) or excised tumor tissue.
- Confocal laser scanning microscope (CLSM).
- Image analysis software (e.g., ImageJ, Imaris).
- Tissue freezing medium (OCT compound) and cryostat (for excised tumors).
Procedure: For Tumor Spheroids:
- Incubate mature spheroids with the fluorescent nanocarrier for a set duration (e.g., 4-24 h).
- Wash the spheroids thoroughly with PBS to remove non-internalized particles.
- Fix the spheroids with 4% paraformaldehyde.
- Transfer a spheroid to a glass-bottom dish and image using CLSM, acquiring Z-stack slices from the top to the bottom of the spheroid.
- Use ImageJ to plot the fluorescence intensity as a function of distance from the spheroid periphery. The penetration depth is defined as the distance at which the fluorescence intensity drops to 50% of its maximum value at the periphery.
For Excised Tumors:
- Administer the nanocarrier to tumor-bearing mice and sacrifice at a predetermined time.
- Excise, embed in OCT, and snap-freeze the tumor.
- Section the tumor into 10-20 μm thick slices using a cryostat.
- Stain for blood vessels (e.g., anti-CD31 antibody) and nuclei (DAPI).
- Image multiple random fields per section using CLSM.
- Quantify the distance from each fluorescent nanoparticle signal to the nearest CD31-positive blood vessel using the distance transform function in ImageJ. Calculate the average and distribution of these distances.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Nanodelivery Barriers
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| DSPE-PEG(2000) | Stealth lipid for liposomes and lipid NPs; extends circulation half-life by reducing opsonization [24]. | Amphiphilic, PEG molecular weight of ~2000 Da. |
| Cell Membrane Extraction Kits | For isolating pure plasma membranes from erythrocytes, leukocytes, etc., to create biomimetic coatings [25]. | Yields membranes with preserved protein function. |
| pH-Sensitive Polymers (e.g., PAA, PDEAEMA) | Backbone for constructing charge-reversal nanocarriers; protonated in acidic TME for enhanced uptake [24]. | pKa values tunable to specific pH thresholds (e.g., pH 6.5-7.0). |
| MMP-Substrate Peptides (e.g., GPLGVRGK) | Linker for enzyme-responsive nanocarriers; cleaved by MMP-2/9 in the TME to trigger payload release or surface transformation [24]. | High specificity and cleavage efficiency. |
| Near-Infrared Dyes (e.g., DiR, Cy7.5) | For non-invasive, real-time tracking of nanocarrier biodistribution and tumor accumulation using fluorescence imaging [28]. | Low background autofluorescence, deep tissue penetration. |
| Dioleoylphosphatidylethanolamine (DOPE) | A helper lipid that promotes endosomal escape via the "proton sponge" effect, enhancing cytosolic delivery of therapeutics [24]. | Fusogenic, conical shape. |
This whitepaper explores the fundamental nanoscale phenomena governing biological interactions, focusing on the intertwined roles of surface area-to-volume (SA/V) ratio and quantum effects. The drastic increase in SA/V ratio at the nanoscale dominates physicochemical behaviors, influencing everything from cellular nutrient uptake to targeted drug delivery. Concurrently, quantum mechanical effects, including tunneling and spin phenomena, become significant in biological processes. This document provides a technical examination of these principles, details experimental methodologies for their investigation, and discusses their critical implications for diagnostic and therapeutic applications in medicine. The content is framed within the broader thesis that a quantitative understanding of these nanoscale fundamentals is essential for advancing biological research and developing next-generation biomedical technologies.
Operating at the scale of 1 to 100 nanometers, the nanoscale is the fundamental dimension of key biological machinery - including proteins, nucleic acids, and cellular organelles. At this scale, the classical physical rules that govern the macroscopic world begin to blend with the distinct laws of quantum mechanics. This confluence gives rise to unique phenomena that are not merely intermediate steps but represent entirely new physical and chemical states that dictate biological interactions.
Two principles are particularly critical: the surface area-to-volume (SA/V) ratio and the emergence of quantum effects. The SA/V ratio, a geometric property, becomes a dominant force at the nanoscale, making surface interactions more significant than bulk properties. This governs reactivity, adsorption, and the integration of nanomaterials with biological systems. Simultaneously, quantum mechanical phenomena such as quantum tunnelling, superposition, and entanglement are now understood to play potential roles in biological processes, from enzyme catalysis to sensory perception. The emerging field of quantum biology seeks to capture and understand these effects, despite the challenges of dissipation and decoherence posed by the warm, wet biological environment [29].
The goal of this whitepaper is to dissect these core principles, provide a framework for their experimental investigation, and contextualize their power in driving innovations across the biomedical landscape, from targeted drug delivery to advanced diagnostic imaging.
Core Principle I: Surface Area to Volume (SA/V) Ratio
Fundamental Impact and Biological Relevance
The surface area-to-volume ratio (SA/V) is a scaling principle that becomes profoundly important at the nanoscale. As a particle or structure decreases in size, its surface area decreases at a slower rate than its volume, resulting in a dramatic increase in the SA/V ratio. This geometric reality means that a vastly larger proportion of the material's atoms or molecules are located on the surface, ready to interact with the environment.
In biological systems, this principle is leveraged for efficiency. For instance, intestinal microvilli and the membrane folds in T-lymphocytes are macroscopic biological structures engineered to maximize surface area, thereby enhancing nutrient uptake and enabling cell deformation for migration, respectively [30]. At the nanoscale, this high SA/V ratio translates to enhanced reactivity, improved solubility, and greater ability to functionalize a material with targeting ligands, drugs, or imaging agents.
Quantitative Analysis of SA/V Scaling
The scaling relationship between surface area (SA) and volume (V) is quantified using the power law: ( SA = aV^b ), where ( b ) is the scaling factor (exponent) and ( a ) is a constant [30]. The value of ( b ) determines the nature of the scaling:
- ( b = 2/3 ) (Allometric/Geometric Scaling): This is the scaling observed in a perfect sphere, where the surface area increases at a slower rate than the volume. This leads to a decreasing SA/V ratio as size increases.
- ( b = 1 ) (Isometric Scaling): This indicates that surface area and volume grow at the same rate, resulting in a constant SA/V ratio across different sizes.
Contrary to the long-held assumption of ( \frac{2}{3} )-geometric scaling, recent single-cell studies on near-spherical mammalian cells (e.g., L1210, THP-1) have revealed that proliferating cells maintain a near-isometric scaling of plasma membrane components [30]. This means that as a cell grows, it maintains a nearly constant SA/V ratio, a feat achieved through increased plasma membrane folding in larger cells. This ensures sufficient plasma membrane area for critical functions like division and nutrient uptake across a wide range of cell sizes.
Table 1: Experimentally Determined Scaling Factors (b) for Surface Area vs. Cell Size
| Cell Line / System | Scaling Factor (b) | Interpretation |
|---|---|---|
| Theoretical Perfect Sphere | 0.667 | SA/V decreases with size |
| Surface-labeled Beads | 0.58 ± 0.01 | SA/V decreases with size [30] |
| L1210 Cells | 0.90 ± 0.02 | Near-isometric scaling (Nearly constant SA/V) [30] |
| THP-1 Cells | 1.01 ± 0.04 | Isometric scaling (Constant SA/V) [30] |
Functional Implications in Drug Delivery
The SA/V ratio is not merely an abstract geometric concept; it has direct, quantifiable impacts on drug delivery and absorption. Research on ketoconazole, a poorly water-soluble drug, has demonstrated that the efficacy of supersaturating drug delivery systems (SDDS) is highly dependent on the SA/V ratio of the experimental or physiological system [31].
The "parachute effect" provided by polymers like HPMC, which maintains drug supersaturation, has a diminishing impact on drug transport as the SA/V ratio increases. This is because at high SA/V ratios, permeation across the membrane becomes so rapid that drug precipitation is less of a limiting factor. This highlights a critical disconnect between in vitro models (with low SA/V ratios) and in vivo conditions.
Table 2: Surface Area to Volume (SA/V) Ratios in Various Experimental and Biological Systems
| System / Model | SA/V Ratio (cm⁻¹) | Context and Significance |
|---|---|---|
| In Vitro Closed System | 0.0 | Lacks absorption sink, overestimates precipitation potential [31] |
| Vertical Franz Diffusion Cell | 1.7 - 17 | Common in vitro permeation model [31] |
| Rat Intestine (in vivo) | 73.32 | Represents actual physiological condition; absorption is very rapid [31] |
Core Principle II: Quantum Effects in Biological Environments
Manifestations of Quantum Biology
At the nanoscale, the frontier of life science intersects with quantum physics. The emerging field of quantum life science investigates how quantum phenomena influence biological processes [29]. While these effects are often masked by decoherence in biological environments, they are increasingly recognized as vital to explaining certain physiological functions.
Key quantum effects with potential biological significance include:
- Quantum Tunneling: This effect allows particles to traverse energy barriers that would be insurmountable according to classical physics. It is crucial in enzyme catalysis, where protons and electrons can tunnel to drive biochemical reactions with high efficiency and specificity.
- Spin Coherence: The quantum property of electron spin is exploited in processes like avian magnetoreception, where it is hypothesized to enable birds to navigate using Earth's magnetic field.
- Entanglement and Superposition: While more speculative in biology, these quintessential quantum states are fundamental to the development of quantum sensors and quantum computing for biological simulation.
Investigation with Advanced Nano-Sensors
Capturing and quantifying these fragile quantum states in living systems is a formidable challenge. The field relies on advanced biological nano quantum sensors and other sophisticated technologies [29]. These tools are designed to measure quantum phenomena with high sensitivity and minimal disruption to the biological system.
Key investigative technologies include:
- Biological Nano Quantum Sensors: Nanoscale sensors, often based on defects in diamonds (NV centers), that can detect minute magnetic and electric fields, temperature, and strain at the quantum level within cells.
- Quantum Technology-Based Hyperpolarized MRI/NMR: This technique dramatically enhances the signal strength in magnetic resonance imaging and spectroscopy, enabling real-time tracking of metabolic processes and improving the detection of diseases like cancer at earlier stages.
- High-Speed 2D Electronic Spectrometers: These devices are used to study energy transfer dynamics, such as those in photosynthetic complexes, to identify signatures of long-lived quantum coherence.
Experimental Protocols and Methodologies
Protocol: Investigating SA/V Scaling in Single Cells
This protocol details the methodology for quantifying the size scaling of plasma membrane components, as described in the preprint on plasma membrane folding [30].
1. Principle: To measure the abundance of cell surface proteins as a proxy for cell surface area and correlate it with single-cell buoyant mass (a proxy for volume) to determine the scaling exponent ( b ).
2. Key Reagent Solutions:
- Suspended Microchannel Resonator (SMR): A cantilever-based instrument for high-precision measurement of single-cell buoyant mass [30].
- Cell Impermeable, Amine Reactive Dye: A fluorophore-coupled dye (e.g., NHS-ester dyes) that labels primary amines on extracellular proteins without crossing the plasma membrane.
- Alternative Labeling Chemistries: Maleimide compounds for labeling thiol groups on cell surface proteins, used for validation.
- Appropriate Cell Culture Media: For maintaining live suspension cell lines (e.g., L1210, BaF3, THP-1) during analysis.
3. Step-by-Step Workflow: 1. Cell Preparation: Harvest near-spherical mammalian suspension cells and keep them on ice to inhibit endocytosis. 2. Surface Labeling: Incubate cells with the amine-reactive fluorescent dye on ice for 10 minutes. Include control samples to validate surface-specificity via microscopy. 3. Exclusion of Dead Cells: Treat cells with a viability dye (e.g., propidium iodide) to exclude dead cells from the final analysis. 4. Coupled Measurement: Pass the labeled cell suspension through the SMR system integrated with a photomultiplier tube (PMT). This setup simultaneously measures the buoyant mass (size) and fluorescence intensity (surface protein content) of thousands of single cells. 5. Data Analysis: Plot fluorescence (proxy for SA) against buoyant mass (proxy for V) on a log-log scale. The slope of the resulting power-law fit is the scaling factor ( b ). A value of ~1 indicates isometric scaling.
Protocol: Functionalization of Nanomaterials for Targeted Delivery
A critical step in applying nanomaterials in medicine is functionalizing their surface to achieve targeted delivery and reduced immunogenicity.
1. Principle: To modify the surface of nanoparticles with functional groups, polymers, or biological ligands to control their interaction with biological systems.
2. Key Reagent Solutions:
- Polyethylene Glycol (PEG): A polymer used to create a "stealth" coating, reducing opsonization and clearance by the immune system [32] [33].
- Targeting Ligands: Antibodies, folic acid, transferrin, or aptamers that bind specifically to receptors overexpressed on target cells (e.g., cancer cells) [34].
- Stimuli-Responsive Linkers: pH-sensitive or enzyme-cleavable bonds that ensure drug release is triggered specifically in the target microenvironment (e.g., tumor tissue) [34].
3. Step-by-Step Workflow: 1. Nanoparticle Synthesis: Synthesize the nanoparticle core (e.g., gold, iron oxide, polymeric) using top-down (e.g., milling) or bottom-up (e.g., chemical vapor deposition) methods [32] [33]. 2. Surface Activation: If necessary, activate the nanoparticle surface to create reactive groups (e.g., carboxyl, amine) for subsequent conjugation. 3. Ligand Conjugation: Covalently link the chosen functional molecules (e.g., PEG, folic acid) to the activated surface using appropriate crosslinker chemistry (e.g., EDC-NHS for carboxyl-amine coupling). 4. Purification and Characterization: Purify the functionalized nanoparticles from unreacted ligands using techniques like dialysis or centrifugation. Characterize the final product for size, surface charge (zeta potential), and conjugation efficiency [32]. 5. Validation: Test the targeting efficiency and stimulus-responsive release in vitro using relevant cell cultures.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Nanoscale Biological Interactions
| Reagent / Material | Function and Application | Key Characteristics |
|---|---|---|
| Amine-Reactive Dyes (NHS-esters) | Labels primary amines on cell surface proteins for quantification of surface area. | Cell-impermeable; allows specific labeling of extracellular proteins [30]. |
| Suspended Microchannel Resonator (SMR) | Measures buoyant mass of single cells with high precision. | Provides a proxy for cell volume/dry mass; enables high-throughput correlation with fluorescence [30]. |
| PEG (Polyethylene Glycol) | Functionalization agent for nanoparticles to reduce immune recognition. | Creates a hydrophilic "cloud"; prolongs circulation half-life in vivo [32] [33]. |
| Targeting Ligands (e.g., Folic Acid) | Functionalization agent for active targeting of nanoparticles to diseased cells. | Binds to receptors overexpressed on target cells (e.g., folate receptor in cancer) [34]. |
| Quantum Dots | Nanoscale semiconductors used as fluorescent probes for bioimaging and biosensing. | Size-tunable emission; high photostability; ideal for tracking and multiplexed assays [32] [34]. |
| Iron Oxide Nanoparticles | Magnetic nanoparticles for use as MRI contrast agents or for magnetic hyperthermia. | Superparamagnetic; can be functionalized for targeting; responsive to external magnetic fields [33] [34]. |
Interrelationship and Biomedical Applications
The synergy between high SA/V ratio and quantum effects is the cornerstone of many modern nanomedical applications. A high SA/V ratio provides the platform for extensive functionalization and interaction, while quantum effects can be exploited for sensitive detection and novel therapeutic mechanisms.
A. Targeted Drug Delivery: Nanoparticles leverage their high SA/V ratio to carry large payloads of therapeutic agents. Their surface is functionalized with targeting ligands (active targeting) and PEG (stealth). The Enhanced Permeability and Retention (EPR) effect facilitates passive accumulation in tumor tissue. Once at the site, the unique tumor microenvironment (e.g., low pH, specific enzymes) can trigger drug release from stimuli-responsive nanocarriers [33] [34].
B. Advanced Diagnostics and Imaging: Quantum dots provide brilliant, stable fluorescence for multiplexed biomarker detection and cellular imaging [32]. Magnetic nanoparticles enhance contrast in MRI, allowing for the detection of previously occult small tumors [34]. The emerging field of quantum technology-based hyperpolarized MRI uses quantum principles to vastly amplify signal, enabling real-time metabolic imaging [29].
The unique phenomena arising at the nanoscale—specifically, the dominating influence of the surface area-to-volume ratio and the emergence of tangible quantum effects—form a fundamental pillar for understanding and innovating within biological environments. The ability to quantitatively measure SA/V scaling in cells and to functionalize nanomaterials based on this principle is now a standard, yet powerful, approach. Concurrently, the burgeoning field of quantum life science, equipped with nano quantum sensors and hyperpolarization techniques, is pushing the boundaries of what is measurable, offering a glimpse into the very quantum mechanical underpinnings of life processes.
Mastering these fundamentals is not an academic exercise; it is a prerequisite for the rational design of next-generation biomedical solutions. From overcoming biological barriers for drug delivery to achieving unprecedented sensitivity in diagnostics, the continued exploration of this unique physical realm promises to redefine the future of medicine and biological research.
Engineering Nano-Bio Interactions: Design Strategies for Targeted Therapeutics and Diagnostics
The systemic administration of nanoparticle-based therapeutics presents a fundamental challenge: the human body has evolved sophisticated mechanisms to recognize and eliminate foreign entities. Upon intravenous injection, nanoparticles are immediately confronted by the mononuclear phagocyte system (MPS), which rapidly clears them from circulation, severely limiting their therapeutic potential [35]. This biological recognition is primarily mediated by the adsorption of blood proteins onto the nanoparticle surface, a process known as opsonization, which tags the particles for phagocytic removal [36]. Furthermore, for nanomedicines to treat diseases like cancer effectively, they must not only evade immune detection but also preferentially accumulate at disease sites and engage with specific cellular targets. Surface engineering addresses this dual challenge through two complementary strategies: PEGylation for stealth properties to prolong circulation, and ligand conjugation for active targeting to enhance specificity [35]. This technical guide examines the fundamental principles, methodologies, and evolving paradigms of these traditional yet critical surface modification techniques, framing them within the broader context of nanoscale biological interactions research.
The Stealth Effect: Fundamentals of PEGylation
Mechanism of Action and Conformational States
Polyethylene glycol (PEG) conjugation, or PEGylation, is a cornerstone technology for conferring "stealth" properties to nanoparticles. The stealth effect operates through two primary mechanisms: immune evasion by reducing protein adsorption and blocking MPS uptake, and reduced receptor-mediated clearance by organs like the liver [35]. PEG achieves this through its physicochemical properties. It is a highly flexible, hydrophilic polymer capable of forming extensive hydrogen bonds with water molecules. For instance, a single PEG2000 polymer can bind approximately 136 water molecules, effectively doubling its molecular weight through hydration [37]. This creates a dense, hydrophilic cloud around the nanoparticle that sterically hinders the approach and adsorption of opsonin proteins.
The protective efficacy of PEG is critically dependent on its surface density, which dictates its physical conformation [37]:
- Mushroom Regime: At low surface density, PEG chains adopt a coiled, mushroom-like conformation due to sufficient space for flexibility. This provides limited steric protection.
- Brush Regime: At high surface density, PEG chains are forced to extend away from the nanoparticle surface, forming a dense, brush-like layer. This conformation offers superior steric shielding and is more effective at minimizing protein adsorption.
Quantitative Impact on Pharmacokinetics
The beneficial effects of PEGylation on nanoparticle pharmacokinetics are well-documented. PEGylated liposomal doxorubicin (Doxil/Caelyx) serves as an iconic clinical example, demonstrating dramatically prolonged circulation time and reduced cardiotoxicity compared to free doxorubicin [38]. The following table summarizes key quantitative data on how PEG properties influence nanoparticle behavior:
Table 1: Impact of PEG Properties on Nanoparticle Behavior and Pharmacokinetics
| PEG Property | Experimental Impact | Reference System |
|---|---|---|
| Molecular Weight | Higher MW PEG (>10,000 Da) more effective at complement activation at high concentrations; ~2,000 Da common for nanocarriers. | [37] |
| Surface Density | Higher density shifts PEG to "brush" regime, enhancing stealth; quantified by equilibrium binding constant (KA) to proteins. | [35] |
| Lipid Anchor Length | DMG-PEG (C14) is "sheddable"; DSPE-PEG (C18) is more stable, enabling targeting. | [39] |
| PEG Ratio in Formulation | Low molar ratios (1.5-3%) improve stability; high ratios (10-20%) cause "PEG dilemma," reducing uptake. | [39] |
Active Targeting: Ligand Conjugation Strategies
While PEGylation provides passive stealth, active targeting involves the functionalization of nanoparticle surfaces with targeting ligands that recognize and bind to specific receptors overexpressed on target cells. This strategy aims to enhance cellular internalization and the specificity of therapeutic delivery.
The process of ligand conjugation often requires PEG derivatives that contain reactive terminal groups. A commonly used strategy involves azide-containing PEG lipids like DSPE-PEG-N3. This group allows for precise, bioorthogonal conjugation to targeting ligands (e.g., peptides, antibodies, or small molecules) that have been modified with a complementary cyclooctyne group (e.g., DBCO) via a copper-free strain-promoted azide-alkyne cycloaddition (SPAAC) "click" reaction [39]. This method is favored for its efficiency and compatibility with biological systems.
The targeting ligands themselves are highly varied. In oncology, common targets include the epidermal growth factor receptor (EGFR), which is overexpressed in many solid tumors. Functionalizing nanoparticles with EGFR-targeting ligands has been shown to restore transfection efficiency in EGFR-positive cell lines in a ligand-specific manner, effectively overcoming the shielding effects of the PEG layer [39]. The success of active targeting is influenced by the density of the ligand and the surface chemistry of the nanoparticle, which must be optimized to ensure the ligand remains accessible and functional despite the presence of the stealth coating [35].
The PEG Dilemma and Emerging Alternatives
Limitations of Conventional PEGylation
Despite its widespread use, traditional PEGylation faces significant drawbacks, collectively known as the "PEG dilemma" [39] [35]. This refers to the trade-off where the PEG corona that provides steric shielding also creates a physical barrier that can hinder cellular uptake and endosomal escape, ultimately reducing the therapeutic efficacy of the encapsulated drug [39]. Furthermore, repeated administration of PEGylated nanoparticles can induce anti-PEG antibodies (IgM and IgG), leading to an Accelerated Blood Clearance (ABC) phenomenon upon subsequent doses and potential hypersensitivity reactions [35] [37]. These immunogenic responses are a growing concern for the long-term viability of PEGylated therapeutics.
Next-Generation Surface Engineering Strategies
To address the limitations of PEG, several advanced surface modulation strategies are being developed:
- Sheddable PEG Coatings: These systems use linkers that are stable in circulation but cleaved in response to specific tumor microenvironment stimuli (e.g., low pH, specific enzymes). This allows the nanoparticle to shed its PEG layer upon reaching the target site, reconciling the conflict between long circulation and efficient cellular uptake [35].
- Alternative Polymer Coatings: Researchers are exploring non-PEG hydrophilic polymers such as poly(2-oxazoline) (pOx) and polysarcosine (pSar). These polymers offer similar stealth properties with a potentially lower risk of inducing immunogenic responses [38].
- Zwitterionic Coatings: Surfaces modified with zwitterionic molecules, which contain both positive and negative charges, can form a super-hydrophilic layer that resists protein fouling through a strong hydration effect, presenting another promising alternative to PEG [38].
Experimental Protocols for Surface Engineering and Characterization
Protocol 1: Formulation of PEGylated mRNA Polyplexes
This protocol details the non-covalent incorporation of PEG-lipids into mRNA complexes based on research by [39].
Materials:
- Cationic Carrier: Lipo-amino fatty acid modified xenopeptide (LAF-XP).
- mRNA: CleanCap FLuc mRNA (5moU).
- PEG Lipids: DMG-PEG (2 kDa) or DSPE-PEG-N3 (2 kDa).
- Buffer: Aqueous buffer (e.g., 10 mM HEPES, pH 7.4).
Procedure:
- Prepare separate solutions of the LAF-XP carrier and PEG lipid in ethanol or a compatible organic solvent.
- Mix the LAF-XP and PEG lipid solutions at the desired molar ratio (e.g., 1.5%, 3%, 10% PEG lipid).
- Dilute the lipid mixture into a rapidly stirring aqueous buffer to form pre-inserted PEG-lipid micelles or bilayers.
- Add the mRNA solution to the lipid mixture at a predetermined nitrogen-to-phosphate (N:P) ratio to complex the RNA and form the final polyplexes.
- Incubate the mixture for 30 minutes at room temperature to allow for complete complexation.
Characterization:
- Colloidal Stability: Assessed by dynamic light scattering (DLS) for particle size and polydispersity index (PDI) before and after incubation in saline or serum-containing media.
- Transfection Efficiency: Quantify luciferase expression in relevant cell lines (e.g., EGFR-positive) 24-48 hours post-transfection.
Protocol 2: Ligand Conjugation via Click Chemistry
This protocol describes the functionalization of pre-formed, azide-containing nanoparticles with a DBCO-modified targeting ligand [39].
Materials:
- Nanoparticles: DSPE-PEG-N3-containing polyplexes or liposomes.
- Ligand: EGFR-targeting peptide or antibody fragment, modified with DBCO.
- Buffer: Phosphate-buffered saline (PBS), pH 7.4.
Procedure:
- Prepare a solution of the DBCO-modified ligand in PBS.
- Add the ligand solution to the nanoparticle suspension at a molar excess of DBCO to azide (e.g., 1.5:1 ratio).
- Allow the reaction to proceed for 2-4 hours at room temperature or overnight at 4°C with gentle agitation.
- Remove unreacted ligand via purification techniques such as size exclusion chromatography (SEC) or dialysis.
Characterization:
- Conjugation Efficiency: Confirm using techniques like HPLC, or spectrophotometric assays to quantify unreacted ligand.
- Targeting Validation: Demonstrate ligand-specific binding and uptake using flow cytometry or confocal microscopy in target receptor-positive vs. receptor-negative cell lines.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for PEGylation and Ligand Conjugation Experiments
| Reagent / Material | Function / Role | Specific Examples |
|---|---|---|
| PEG Lipids | Provide stealth properties and colloidal stability; platform for conjugation. | DMG-PEG 2k (sheddable), DSPE-PEG-N3 2k (for click chemistry) [39]. |
| Cationic Carriers | Complex and condense nucleic acids (mRNA, pDNA) to form polyplexes. | Lipo-amino fatty acid Xenopeptides (LAF-XPs) [39]. |
| Click Chemistry Reagents | Enable bioorthogonal, copper-free conjugation of ligands to nanoparticles. | DBCO-modified ligands, DSPE-PEG-N3 (azide-functionalized) [39]. |
| Targeting Ligands | Mediate specific binding to receptors on target cells. | EGFR-targeting peptides, antibodies, or other receptor-specific molecules [39]. |
| Model Membranes | Study fundamental nanoparticle-lipid interactions in a simplified system. | DPPC, POPC, Cholesterol for Langmuir monolayer studies [40]. |
Visualizing Core Concepts and Workflows
PEG Conformation and the PEG Dilemma
Ligand Conjugation via Click Chemistry Workflow
PEGylation and ligand conjugation represent foundational pillars of nanoparticle surface engineering, directly addressing the critical biological barriers of immune clearance and target recognition. While the "PEG dilemma" underscores the limitations of a purely passive stealth approach, it also drives innovation toward more dynamic, intelligent systems. The future of traditional surface engineering lies in the sophisticated integration of these techniques with stimuli-responsive elements and novel non-PEG polymers [35] [38]. For researchers, a deep understanding of the quantitative relationships between PEG properties, ligand accessibility, and the resulting pharmacokinetics and biodistribution remains paramount. As the field progresses, the principles of PEGylation and targeting will continue to be essential for transforming nanoscale biological interactions into effective clinical therapies.
Cell membrane-coated nanoparticles (CM-NPs) represent a groundbreaking biomimetic strategy in nanoscale biological interactions research. By cloaking synthetic nanocarriers with natural cell membranes, these platforms combine the functionalities of biological systems with the versatility of engineered materials. This whitepaper comprehensively examines the fundamental principles, fabrication methodologies, and multifunctional capabilities of CM-NPs, with particular emphasis on their applications in targeted drug delivery, diagnostic imaging, and therapeutic interventions. The core technological advantage lies in their ability to replicate native cellular behaviors, including immune evasion, homotypic targeting, and extended systemic circulation. This review synthesizes current scientific knowledge into structured data presentations, experimental protocols, and mechanistic visualizations to provide researchers and drug development professionals with a foundational resource for advancing this transformative technology.
Cell membrane-coated nanoparticles constitute a revolutionary class of biomimetic nanoplatforms that bridge the divide between synthetic nanomaterials and biological systems. These sophisticated structures are fabricated by enveloping nanoparticle cores—typically composed of polymeric, metallic, or lipid-based materials—with natural membranes derived from source cells, thereby transferring complex biological functionalities to the resulting composite system [41] [25]. This approach represents a paradigm shift from conventional surface modification techniques, as it preserves the complete repertoire of native membrane proteins, lipids, and carbohydrates in their natural orientation and functionality.
The fundamental premise underlying this technology stems from the observation that natural cells exhibit remarkable capabilities—including immune evasion, tissue-specific homing, and intercellular communication—that are largely mediated by surface membrane components [25]. By harnessing these innate functionalities, CM-NPs overcome significant limitations of traditional nanocarriers, particularly rapid clearance by the mononuclear phagocyte system, insufficient targeting specificity, and suboptimal biocompatibility [42] [25]. The transformative potential of this bioinspired approach has catalyzed extensive research efforts across diverse biomedical applications, establishing CM-NPs as a versatile platform for precision medicine.
Core Concepts and Biological Mechanisms
Membrane Source Diversity and Functional Properties
The biological performance of CM-NPs is fundamentally dictated by the source of the cell membrane, with each type conferring distinct functional advantages tailored to specific therapeutic applications. Table 1 systematically compares the key membrane sources, their inherent advantages, and limitations.
Table 1: Comparative Analysis of Cell Membrane Sources for Nanoparticle Coating
| Membrane Source | Main Advantages | Main Limitations |
|---|---|---|
| Cancer Cell Membrane (CCM) | Enables homotypic targeting through tumor antigen recognition; carries immune evasion proteins (e.g., CD47); improves tumor accumulation and selective uptake [42] | Applicable mainly to cancer settings; potential safety concerns from oncogenic proteins; variability in membrane composition and scalability issues [42] |
| Red Blood Cell (RBC) Membrane | Readily available; well-established isolation methods; strong immune evasion and prolonged circulation time [42] [25] | Does not provide tumor-specific targeting; limited ability to direct nanoparticles to tumor tissues [42] |
| Platelet Membrane | Natural adhesion to damaged vasculature and circulating tumor cells; contributes to immune evasion; useful in metastasis prevention [42] | Limited availability; possible pro-thrombotic activity; less tumor selectivity compared with CCM [42] |
| Immune Cell Membrane | Intrinsic affinity for inflammatory and tumor microenvironments; potential to modulate immune response; can facilitate tissue penetration [42] | Limited cell sources; risk of immunogenicity; functional properties depend on immune cell type [42] |
| Stem Cell Membrane | Tropism toward tumor and injured tissues; possesses immune evasion properties; potential for regenerative applications [42] | Safety concerns related to stemness-associated factors; technical challenges in large-scale preparation [42] |
Key Biological Mechanisms
Immune Evasion and Prolonged Circulation
A paramount advantage of CM-NPs is their ability to circumvent immune surveillance, significantly extending their systemic circulation half-life. This property is largely mediated by the preservation of "self-marker" proteins on the coated membrane, most notably CD47, which interacts with signal-regulatory protein alpha (SIRPα) on macrophages to transmit a "don't eat me" signal that suppresses phagocytic clearance [42] [25]. This biological disguise enables CM-NPs to achieve circulation times substantially longer than those of conventional PEGylated nanoparticles, which often trigger anti-PEG immune responses and eventual clearance [42]. Studies demonstrate that RBC membrane-coated nanoparticles exhibit blood retention rates of approximately 13.1% after 24 hours, significantly outperforming their uncoated counterparts [25].
Homotypic Targeting and Tumor Accumulation
Cancer cell membrane-coated nanoparticles (CCM-NPs) exhibit a remarkable ability to selectively target and accumulate in tumor tissues through homotypic binding mechanisms. This process is mediated by conserved adhesion molecules—including E-cadherin, N-cadherin, galectin-3, integrins, and selectins—that facilitate recognition and binding between source and target cancer cells [42]. This intrinsic tumor-targeting capability enables precision drug delivery while minimizing off-target effects. Research indicates that CCM-NPs can achieve tumor accumulation rates more than two and a half times higher than those of single-membrane-modified particles or conventional nanocarriers [25]. Furthermore, hybrid membrane systems combining cancer cell membranes with RBC membranes synergize homotypic targeting with extended circulation, further enhancing therapeutic efficacy [25].
Tumor Microenvironment Penetration
Beyond preferential accumulation, CM-NPs demonstrate enhanced penetration into the complex tumor microenvironment (TME), which typically presents formidable barriers to drug delivery, including dense extracellular matrix, abnormal vasculature, and elevated interstitial fluid pressure [42]. By retaining the natural machinery for matrix remodeling and migration, CCM-NPs can navigate these obstacles more effectively than uncoated nanoparticles. Experimental evidence from 3D tumor spheroid models confirms significantly improved infiltration depth for cancer cell membrane-coated doxorubicin nanoparticles compared to their uncoated equivalents [42]. This enhanced penetration capability directly translates to improved therapeutic outcomes in solid tumor treatments.
Experimental Protocols and Methodologies
Cell Membrane Extraction and Purification
The isolation of intact, functionally competent cell membranes represents a critical foundational step in CM-NP fabrication. The following protocol outlines a standardized approach for membrane extraction:
Cell Culture and Harvesting: Expand source cells (e.g., cancer cells, erythrocytes, immune cells) under appropriate culture conditions. Harvest cells at 80-90% confluence using gentle detachment methods to preserve membrane integrity [25].
Cell Washing and Suspension: Wash harvested cells three times in ice-cold phosphate-buffered saline (PBS) containing protease inhibitors to prevent protein degradation. Suspend the final cell pellet in hypotonic membrane extraction buffer (typically 10 mM Tris-HCl, 2 mM MgCl₂, 1 mM EDTA, pH 7.4) supplemented with protease inhibitors [25].
Membrane Disruption: Subject cell suspensions to mechanical disruption through multiple freeze-thaw cycles (-80°C to 37°C) or nitrogen cavitation (for more uniform breakage). Alternatively, use gentle sonication (3-5 pulses of 10-15 seconds each on ice) [25].
Differential Centrifugation: Centrifuge the homogenate at 800×g for 10 minutes at 4°C to remove nuclei and unbroken cells. Collect the supernatant and centrifuge at 20,000×g for 30 minutes at 4°C to pellet membrane fragments [25].
Membrane Purification: Resuspend the membrane pellet in sucrose density gradient (typically 30-50% discontinuous gradient) and centrifuge at 100,000×g for 2 hours. Collect the interface band containing purified plasma membranes [25].
Membrane Storage: Resuspend purified membranes in PBS or Tris buffer, aliquot, and store at -80°C until use. Protein concentration should be quantified using BCA or Bradford assay [25].
Advanced extraction techniques, such as styrene-maleic acid (SMA) copolymer technology, enable the formation of stable lipid-protein-polymer complexes (SMALPs) that maintain membrane proteins in their native lipid environment without detergent use [25].
Nanoparticle Core Synthesis and Functionalization
Nanoparticle cores can be fabricated from diverse materials, each offering distinct advantages for specific applications:
Polymeric Nanoparticles (PLGA): Prepare PLGA nanoparticles using single or double emulsion-solvent evaporation methods. Dissolve PLGA polymer in dichloromethane or ethyl acetate, add therapeutic agent, emulsify in aqueous polyvinyl alcohol solution, and evaporate organic solvent to form solid nanoparticles [42].
Silver Nanoparticles (AgNPs): Synthesize using chemical reduction: add 10 mL of 1 mM AgNO₃ dropwise into 30 mL of 2 mM NaBH₄ solution at 0-5°C with vigorous stirring. Add 1-2 mL of PVP solution (10 g·L⁻¹) as a stabilizer. Characterize by UV-Vis spectroscopy (peak at ~400 nm) and TEM (size distribution 10-20 nm) [43].
FePt Metal-Organic Framework Nanoparticles: Develop FePt@ZIF-8 composites by encapsulating FePt nanoclusters within zeolitic imidazolate frameworks. Combine FePt NPs with zinc nitrate and 2-methylimidazole in methanol, then incubate with constant stirring to form core-shell structures [44].
Membrane-Coating Techniques
The successful integration of cell membranes onto nanoparticle cores can be achieved through several approaches:
Co-Extrusion Method: Mix pre-formed nanoparticle cores with cell membrane fragments at appropriate mass ratios (typically 1:1 to 1:3 protein:core mass ratio). Pass the mixture through polycarbonate porous membranes (typically 100-400 nm pores) using an extruder for 10-20 passes [25].
Sonication-Assisted Fusion: Combine nanoparticles and membrane fragments in small volume PBS. Subject the mixture to controlled probe sonication (20-40% amplitude, 30-60 seconds total in pulse mode) on ice. Remove excess membranes by centrifugation or density gradient separation [25].
Microfluidic Electroporation: Utilize microfluidic devices with integrated electrodes to apply precisely controlled electrical fields that facilitate membrane fusion while maintaining structural integrity [25].
Characterization and Quality Assessment
Comprehensive characterization is essential to verify successful membrane coating and functionality:
- Size and Zeta Potential: Dynamic light scattering for hydrodynamic diameter and polydispersity index; laser Doppler electrophoresis for surface charge [25].
- Morphology: Transmission electron microscopy (TEM) and scanning electron microscopy (SEM) for core-shell structure visualization [25].
- Membrane Protein Retention: Western blot, flow cytometry, or immunogold staining to confirm presence of specific membrane markers (e.g., CD47) [42] [25].
- In Vitro Functional Assays: Cellular uptake studies, phagocytosis evasion assays, and tumor spheroid penetration models [42].
Multifunctional Applications
Targeted Drug Delivery Systems
CM-NPs have demonstrated exceptional capabilities in precision drug delivery across multiple therapeutic domains:
Oncology Applications: CCM-NPs exhibit particular promise in cancer therapy. In one representative study, PLGA nanoparticles coated with 4T1 murine mammary cancer cell membranes and loaded with ABT-737 (a Bcl-2 inhibitor) demonstrated enhanced tumor-homing ability and superior therapeutic efficacy against triple-negative breast cancer [42]. Similarly, polymeric nanoparticles carrying doxorubicin and coated with membranes from human acute myeloid leukemia cells induced apoptosis in approximately 80% of target cells, significantly outperforming conventional doxorubicin administration [42].
Traditional Chinese Medicine Delivery: Cell membrane biomimetic platforms have revolutionized the delivery of traditional Chinese medicine (TCM) active ingredients. For instance, biomimetic platelet membrane-coated tetrandrine nanoparticles showed enhanced antitumor efficacy in non-small cell lung cancer, while biomimetic nano-delivery systems significantly improved the ferroptosis-induced anticancer effect of resveratrol in colorectal cancer treatment [45].
Neurological and Inflammatory Diseases: Neutrophil membrane-camouflaged nanosystems achieved targeted delivery to ischemic brain tissue with accumulation rates 15.2 times higher than uncoated nanoparticles, demonstrating exceptional blood-brain barrier penetration capabilities [25]. Similarly, leukocyte-membrane-modified nanocarriers efficiently deliver anti-inflammatory drugs to inflammatory lesions by mimicking natural leukocyte chemotaxis [25].
Diagnostic and Theranostic Platforms
The integration of diagnostic capabilities with therapeutic functions represents a significant advancement in CM-NP technology:
Magnetic Resonance Imaging Enhancement: RBC membrane-coated FePt metal-organic framework nanoparticles (FePt@ZIF-m) have been developed as multifunctional theranostic systems for enhanced MRI and targeted therapy of hepatocellular carcinoma. These platforms leverage the T₁-to-T₂ imaging conversion capability of FePt NPs under different aggregation states, enabling responsive imaging contrast tuned to specific pathological microenvironments [44].
Biosensing and Diagnostic Applications: Silver nanoparticles (AgNPs) functionalized with specific ligands serve as robust platforms for biosensing applications, capitalizing on their pronounced surface plasmon resonance and tunable optical properties. AgNP-based electrochemical and optical biosensors can monitor drug release, oxidative stress, and disease biomarkers with high sensitivity [43].
Immunotherapeutic Applications
CM-NPs present innovative approaches to cancer immunotherapy by serving as versatile platforms for immune modulation:
Cancer Vaccines: CCM-NPs function as effective tumor vaccine platforms by co-delivering tumor-associated antigens and immunostimulatory agents. The inherent antigenic repertoire preserved on cancer cell membranes, combined with loaded adjuvants or immune checkpoint blockers, enables efficient priming of anti-tumor immune responses [42].
Immune Cell Mimicry: Nanoparticles coated with membranes from immune cells (macrophages, T cells, or NK cells) inherit their homing capabilities to inflammatory sites and tumor microenvironments. These platforms can directly modulate immune responses by delivering immunotherapeutic agents to specific immune cell populations [42] [41].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for CM-NP Development
| Reagent/Material | Function/Application | Representative Examples |
|---|---|---|
| PLGA (Poly lactic-co-glycolic acid) | Biodegradable polymer for nanoparticle core; enables controlled drug release [42] | PLGA nanoparticles loaded with ABT-737 for breast cancer therapy [42] |
| Silver Nitrate (AgNO₃) | Precursor for silver nanoparticle synthesis; provides antimicrobial and plasmonic properties [43] | AgNPs for targeted doxorubicin delivery and biosensing applications [43] |
| FePt Alloy Nanoparticles | Magnetic core for MRI contrast and magnetic hyperthermia therapy [44] | FePt@ZIF-m systems for hepatocellular carcinoma diagnosis and treatment [44] |
| ZIF-8 (Zeolitic imidazolate framework-8) | Metal-organic framework for encapsulating imaging agents and drugs; pH-responsive release [44] | ZIF-8 encapsulation of FePt nanoparticles for enhanced MRI contrast [44] |
| Polyvinylpyrrolidone (PVP) | Stabilizing agent for nanoparticle synthesis; prevents aggregation [43] | PVP stabilization of AgNPs during chemical reduction synthesis [43] |
| Doxorubicin (DOX) | Model chemotherapeutic drug for evaluating delivery efficacy [42] [43] | DOX-loaded CCM-NPs for acute myeloid leukemia treatment [42] |
| Protease Inhibitor Cocktails | Preserve membrane protein integrity during extraction and processing [25] | Essential for maintaining CD47 and other signaling proteins during membrane isolation [25] |
Signaling Pathways and Mechanistic Insights
The therapeutic efficacy of CM-NPs is mediated through several critical biological pathways, visualized in the following mechanistic diagram:
Future Perspectives and Challenges
Despite remarkable progress, several challenges must be addressed to advance CM-NP technologies toward clinical translation:
Scalability and Manufacturing: Current membrane extraction and nanoparticle coating techniques face significant hurdles in scalability and reproducibility. Development of standardized, Good Manufacturing Practice (GMP)-compatible processes is essential for clinical translation [25]. Microfluidic-based production systems show promise for scalable manufacturing of homogeneous CM-NPs [25].
Long-term Safety and Biocompatibility: Comprehensive toxicological profiles of CM-NPs, particularly those incorporating synthetic materials or engineered membranes, require thorough investigation. Potential concerns include accelerated blood clearance, complement activation, and organ-specific accumulation [25] [44].
Membrane Engineering and Hybridization: Emerging strategies focus on engineering membrane components to enhance specific functionalities while minimizing undesirable interactions. Hybrid membrane systems—combining membranes from different cell sources—offer opportunities to create nanoparticles with multiplexed capabilities [25] [45].
Regulatory Considerations: The unique biological-synthetic hybrid nature of CM-NPs presents novel regulatory challenges. Establishing appropriate characterization standards, quality control metrics, and safety assessment frameworks will be crucial for regulatory approval [25].
Integration with Emerging Technologies: Convergence of CM-NP platforms with other advanced technologies, including gene editing, artificial intelligence-driven design, and stimuli-responsive materials, will unlock new therapeutic possibilities and application domains [25] [46].
Cell membrane-coated nanoparticles represent a transformative biomimetic platform that effectively bridges nanoscale engineering and biological systems. By preserving the complex surface functionalities of natural cell membranes, these sophisticated nanostructures overcome fundamental limitations of conventional nanocarriers, enabling unprecedented capabilities in targeted drug delivery, diagnostic imaging, and therapeutic intervention. The continued refinement of fabrication methodologies, coupled with deepening understanding of structure-function relationships, promises to accelerate the clinical translation of these innovative platforms. As research advances, CM-NPs are poised to make substantial contributions to precision medicine, particularly in oncology, inflammatory diseases, and regenerative therapies, ultimately fulfilling the promise of biomimicry in nanomedicine.
The strategic delivery of therapeutic agents to tumor sites represents a cornerstone of modern cancer nanomedicine, primarily achieved through two distinct yet complementary mechanisms: passive and active targeting. The Enhanced Permeability and Retention (EPR) effect, first introduced by Maeda and Matsumura in 1986, established the foundational principle for passive targeting by exploiting the unique pathophysiological characteristics of solid tumors [47] [48]. This phenomenon leverages the hyperpermeable vasculature and impaired lymphatic drainage commonly found in tumor tissues to enable selective accumulation of macromolecules and nanocarriers within the tumor interstitium [48]. In contrast, active targeting employs specialized ligands conjugated to nanocarriers to facilitate specific recognition and binding to molecular markers overexpressed on target cell surfaces, thereby enhancing cellular internalization and retention [47] [49]. The efficacy of both strategies is governed by complex nanoscale biological interactions at the interface between engineered nanomaterials and pathological tissue environments, presenting both opportunities and challenges for therapeutic intervention.
Core Mechanisms and Principles
Passive Targeting and the EPR Effect
The EPR effect operates through well-characterized pathological features of solid tumors. Rapid, dysregulated angiogenesis creates blood vessels with structural abnormalities, including large inter-endothelial gaps (100-780 nm) and impaired smooth muscle layers [47] [48]. These anatomical defects permit enhanced extravasation of circulating nanocarriers into tumor tissue, while compromised lymphatic function results in their prolonged retention [48]. The process is further influenced by various inflammatory mediators such as vascular endothelial growth factor (VEGF), bradykinin, prostaglandins, and nitric oxide that sustain vascular hyperpermeability [48].
However, the efficiency of passive targeting is constrained by several physiological barriers. Elevated interstitial fluid pressure (IFP) resulting from vascular leakage and poor drainage creates convective forces that oppose nanoparticle penetration into deeper tumor regions [48] [50]. Additionally, the dense extracellular matrix (ECM) rich in collagen, elastin fibers, and hyaluronic acid presents significant steric and electrostatic hindrances to nanoparticle transport [50]. Tumor perfusion heterogeneity further complicates uniform drug distribution, leaving some regions undertreated [50].
Active Targeting and Ligand-Receptor Interactions
Active targeting strategies employ precise molecular recognition to overcome the limitations of passive accumulation. This approach involves conjugating nanocarriers with targeting moieties that specifically bind receptors overexpressed on tumor cells or vasculature [47] [49]. The primary ligand categories include:
- Antibodies and antibody fragments offering high specificity
- Peptides with selective binding domains
- Aptamers with customizable affinity
- Small molecules (e.g., folic acid, transferrin) with natural receptor affinity [49]
These ligands facilitate receptor-mediated endocytosis after nanocarriers extravasate via the EPR effect, significantly enhancing cellular uptake compared to non-targeted systems [51]. For instance, transferrin-conjugated nanoparticles demonstrate substantially improved retention and deeper tumor penetration through specific engagement with transferrin receptors highly expressed on various cancer cells [51]. The targeting efficacy depends critically on ligand density, orientation, and preservation of bioactivity following nanocarrier functionalization [51].
Table 1: Comparative Analysis of Passive vs. Active Targeting Strategies
| Parameter | Passive Targeting | Active Targeting |
|---|---|---|
| Fundamental Mechanism | Exploitation of pathological tumor vasculature (EPR effect) | Molecular recognition via ligand-receptor interactions |
| Key Determinants | Nanoparticle size (20-200 nm), surface charge, shape, circulation time | Ligand specificity, receptor density, binding affinity, ligand orientation |
| Primary Advantages | Broad applicability across tumors, simpler nanocarrier design | Enhanced cellular internalization, improved tumor retention, potential for biomarker-specific delivery |
| Major Limitations | Heterogeneous efficacy due to tumor variability, limited cellular uptake | Potential immunogenicity, complex manufacturing, prerequisite passive accumulation |
| Clinical Translation | Multiple approved nanomedicines (e.g., Doxil) | Limited clinical success, ongoing investigative trials |
Quantitative Design Parameters for Nanocarriers
Physicochemical Properties Governing Tumor Accumulation
The effectiveness of both targeting strategies depends profoundly on meticulous optimization of nanocarrier physicochemical properties, which dictate their pharmacokinetic profile, biodistribution, and intratumoral fate [50].
Size represents a critical parameter with multidimensional implications. Nanoparticles below 10 nm undergo rapid renal clearance, while those exceeding 400 nm experience splenic filtration and hepatic sequestration [50]. The optimal size range of 20-200 nm balances prolonged circulation against efficient tumor extravasation [49] [50]. Size significantly influences penetration depth within tumor tissue, with smaller particles (<50 nm) demonstrating superior diffusion through the dense extracellular matrix [50].
Surface charge modulates biological interactions through electrostatic forces. Cationic nanoparticles typically exhibit enhanced cellular internalization but accelerated clearance by the mononuclear phagocyte system (MPS) due to opsonin adsorption [50]. Anionic or neutral surfaces, particularly when shielded with hydrophilic polymers like polyethylene glycol (PEG), demonstrate prolonged circulation half-lives by reducing protein adsorption and MPS recognition [49] [50].
Shape affects margination dynamics within blood vessels and vascular adhesion potential. Non-spherical geometries like rods and disks demonstrate enhanced margination toward vessel walls in laminar flow compared to spherical counterparts, increasing extravasation opportunities [50]. Cylindrical micellar architectures show both prolonged systemic circulation (approximately 24h elimination half-life) and superior tumor accumulation (1.4-2.3-fold higher than spherical equivalents) [50].
Table 2: Optimization of Nanocarrier Physicochemical Parameters
| Parameter | Optimal Range | Biological Impact | Design Considerations |
|---|---|---|---|
| Size | 20-200 nm | Prevents renal filtration (<10 nm) and splenic clearance (>400 nm); maximizes EPR effect | Size-shifting systems enable initial circulation stability followed by site-specific size reduction |
| Surface Charge | Slightly negative to neutral | Reduces MPS recognition and protein opsonization; balances circulation time and cellular uptake | PEGylation provides steric stabilization; charge-reversal systems respond to TME stimuli |
| Shape | Rods, disks, high-aspect-ratio structures | Enhances vascular margination and adhesion; improves tumor penetration | Anisotropic structures demonstrate superior pharmacokinetics over spherical equivalents |
| Surface Functionalization | PEG density: 5-20%; Ligand density: 2-10 per particle | Prevents aggregation and immune recognition; optimizes receptor engagement without steric hindrance | Controlled conjugation methods ensure proper ligand orientation and accessibility |
Nanocarrier Platforms and Their Applications
Diverse nanocarrier architectures have been engineered to capitalize on these design principles:
- Lipid-based systems (liposomes, SLNs, NLCs) offer biocompatibility and tunable drug release profiles [48] [49]. Doxil, a PEGylated liposomal doxorubicin formulation, exemplifies successful clinical translation through optimized lipid composition (DSPC, cholesterol, PEG-lipid) that extends circulation to exploit the EPR effect [49].
- Polymeric nanoparticles (PEG, PLGA, PAMAM) provide controlled degradation kinetics and high drug loading capacity [48]. Dendrimers like PAMAM enable precise multivalent ligand display for enhanced targeting avidity [48].
- Inorganic nanoparticles (gold, silver, iron oxide) impart unique optical, magnetic, or catalytic properties for theranostic applications [48]. Sub-5 nm ultrafine iron oxide nanoparticles (uIONPs) demonstrate superior tumor penetration and active targeting efficacy due to their compact dimensions [51].
- Hybrid systems combine material advantages to create multifunctional platforms. AGuIX nanoparticles, based on polysiloxane and measuring ~4 nm, integrate diagnostic imaging and radiosensitizing capabilities while effectively utilizing the EPR effect [48].
Experimentation and Methodology
Experimental Models for Evaluating Targeting Efficacy
Rigorous assessment of targeting strategies employs integrated methodological approaches spanning in vitro validation to in vivo visualization.
In vitro binding specificity assays establish foundational targeting capability. The protocol involves incubating ligand-functionalized nanoparticles with target cells expressing the receptor of interest, followed by extensive washing to remove unbound particles [51]. Quantitative analysis employs flow cytometry or fluorescence microscopy to measure cell-associated signal. Specificity is confirmed through competitive inhibition using free ligand, which should significantly reduce nanoparticle binding [51]. For example, pre-treatment of 4T1 mammary tumor cells with free transferrin effectively blocks subsequent binding of transferrin-conjugated uIONPs, validating receptor-mediated uptake [51].
In vivo biodistribution studies utilize fluorescently labeled nanoparticles (e.g., FITC for active targeting particles, TRITC for non-targeting controls) co-administered to tumor-bearing animal models [51]. Multiphoton or confocal fluorescence imaging at predetermined time points (1, 3, 24 hours) enables spatial and temporal tracking of nanoparticle distribution within tumor tissue [51]. Computational analysis of fluorescence intensities quantifies relative accumulation and penetration depths between targeted and non-targeted formulations [51].
Histological correlation validates targeting specificity at cellular resolution. Following in vivo studies, tumors are excised, sectioned, and stained for receptor expression (immunofluorescence) alongside nanoparticle localization [51]. Colocalization analysis confirms the association between target density and nanoparticle accumulation, providing critical validation of active targeting mechanisms.
Experimental Workflow for Targeting Evaluation
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Targeting Studies
| Reagent/Material | Function and Application | Specific Examples |
|---|---|---|
| Ionizable Lipids | Enable nucleic acid encapsulation; facilitate endosomal escape via pH-dependent charge switching | MC3 (Onpattro); optimized pKa (~6.4) enhances endosomal escape and reduces toxicity [49] |
| PEG-Lipids | Confer steric stabilization; reduce protein opsonization and extend circulation half-life | DMG-PEG, DSG-PEG; molecular weight and density optimization critical for balancing stealth and functionality [49] |
| Targeting Ligands | Mediate specific receptor recognition and cellular internalization | Transferrin (TfR targeting); RGD peptides (integrin targeting); Folate (folate receptor targeting); Antibodies [51] |
| Fluorescent Probes | Enable in vitro and in vivo tracking of nanoparticle distribution | FITC, TRITC, Cy dyes; differential labeling permits simultaneous tracking of multiple formulations [51] |
| Cell Lines | Provide in vitro models with defined receptor expression profiles | 4T1 (murine mammary carcinoma, high TfR expression); HeLa (human cervical cancer, high folate receptor) [51] |
Enhancement Strategies and Combinatorial Approaches
Overcoming the Limitations of Passive Targeting
Significant research focuses on enhancing the EPR effect through pharmacological and physical interventions. Pharmacological priming utilizes vasoactive agents to modify tumor hemodynamics and vascular permeability [52]. Angiogenic factors like erythropoietin can improve tumor perfusion, while corticosteroids remodel vessels and associated extracellular matrix [52]. Nitric oxide donors and enzyme-based strategies employing matrix metalloproteinases (MMPs) facilitate nanoparticle penetration through tumor stroma by modulating physical barriers [47].
Physical methods provide spatiotemporal control over drug delivery. Ultrasound-mediated microbubble oscillation mechanically disrupts vessel walls and adjacent ECM, enhancing nanocarrier extravasation—a strategy under clinical evaluation for brain tumors [52]. Hyperthermia, radiation, and photo-immunotherapy similarly moderate tumor vasculature to improve nanosystem permeation [47] [52]. These approaches address the heterogeneity of the EPR effect between different tumor types and individual patients, a major challenge in clinical translation [47] [48].
Integrated Passive-Active Targeting Systems
The most promising advancements emerge from integrated systems that sequentially overcome delivery barriers. Dual-targeting strategies combine initial passive accumulation via EPR with subsequent active targeting for enhanced cellular internalization [50]. These systems may incorporate stimuli-responsive elements that activate only within the tumor microenvironment, such as size-switching nanoparticles that undergo dimension reduction after tumor entry to enhance penetration depth [50]. Surface charge-reversal systems transition from neutral/negative circulation stability to positive charge at acidic tumor pH to promote cellular uptake [50].
Sequential Biological Barriers in Tumor Targeting
The strategic integration of passive and active targeting mechanisms represents the evolving frontier in cancer nanomedicine. While the EPR effect provides the foundational principle for tumor-selective accumulation, its clinical translation has been hampered by significant heterogeneity across tumor types and individual patients [47] [48]. Active targeting approaches complement passive strategies by enhancing cellular internalization and retention through specific ligand-receptor interactions, yet they remain dependent on initial passive accumulation for tumor access [51].
Future advancements will likely emphasize patient stratification through histological or imaging biomarkers to identify individuals with pronounced EPR effects, thereby improving clinical outcomes [52]. The development of multi-stage drug delivery systems that dynamically respond to environmental cues or external stimuli offers promising approaches to sequentially overcome biological barriers [48] [50]. Furthermore, emerging insights into active transport and retention (ATR) mechanisms involving tumor-associated macrophages and endothelial transcytosis may complement traditional EPR-based paradigms [52].
The rational design of next-generation nanocarriers will require sophisticated optimization of multiple physicochemical parameters in conjunction with combinatorial strategies that physically, pharmacologically, or biologically modulate the tumor microenvironment. As fundamental research continues to unravel the complexities of nanoscale biological interactions, particularly through advanced techniques like single-molecule sensing and superresolution imaging [53], these insights will catalyze the development of increasingly precise and effective targeted therapeutic platforms with enhanced clinical applicability.
The efficacy of any nanoplatform in biomedical applications is fundamentally governed by its interactions with biological systems at the nanoscale. Upon introduction into a biological environment, nanoparticles immediately interface with proteins, cells, and various biomolecules, forming a dynamic "corona" that determines their subsequent biological identity [19] [18]. Protein adsorption onto polymer surfaces, for instance, is a complex, ubiquitous process that impacts essential areas from medical devices to diagnostic tools [54]. The nature of these interactions becomes significantly more complicated with miniaturization, as behavior observed on macroscopic surfaces cannot be effectively extrapolated to the nanoscale, where surface energy and chemical heterogeneity operate on a length scale commensurate with individual biomolecules [54]. A fundamental understanding of these nano-bio interactions is therefore critical for designing nanoplatforms that can navigate biological barriers, evade immune clearance, and deliver their payloads with precision.
This guide provides an in-depth technical overview of three major classes of nanoplatforms—lipid nanoparticles, polymeric carriers, and inorganic nanostructures—framed within the context of nanoscale biological interactions research. It is intended to equip researchers and drug development professionals with the latest advances, methodologies, and design principles driving the field of nanomedicine.
Lipid-Based Nanoplatforms
Lipid nanoparticles represent a groundbreaking platform in drug delivery, renowned for their biocompatibility and versatility in encapsulating diverse cargoes, from small molecules to nucleic acids [55] [56].
Composition and Structure
Lipid-based systems are primarily categorized into liposomes and Lipid Nanoparticles (LNPs). Their distinct compositions dictate their structure, stability, and function.
Table 1: Core Components of Lipid-Based Nanoplatforms
| Component | Category | Key Function | Example Molecules |
|---|---|---|---|
| Ionizable Cationic Lipid | LNP Core | Encapsulates nucleic acids via electrostatic interactions; enables endosomal escape through charge shift at low pH [55] [56] | DLin-MC3-DMA, ALC-0315 |
| Phospholipid | Liposome & LNP Shell | Forms the structural bilayer matrix; influences membrane fluidity and stability [55] | DSPC, DOPE, Phosphatidylcholines |
| Cholesterol | Stabilizer | Modulates membrane fluidity and packing; enhances structural integrity and circulation time [55] [56] | Cholesterol |
| PEGylated Lipid | Stealth Component | Reduces protein adsorption and immune clearance; controls nanoparticle size and stability [55] [56] | DMG-PEG2000, ALC-0159 |
Liposomes are spherical vesicles consisting of one or more amphiphilic phospholipid bilayers enclosing an aqueous core, making them suitable for delivering both hydrophobic (within the bilayer) and hydrophilic (within the core) drugs [55]. In contrast, LNPs, developed primarily for nucleic acid delivery, possess a more complex internal architecture. They feature a lipid shell surrounding an internal core of reverse micelles formed by ionizable lipids, which encapsulate and protect oligonucleotides [56].
Formulation Methods and Experimental Protocols
The method of formulation is a Critical Process Parameter (CPP) that directly impacts Critical Quality Attributes (CQAs) such as size, polydispersity index (PDI), and encapsulation efficiency.
- Microfluidics: This is the gold standard for research and development due to its superior control and repeatability. It is a bottom-up method based on nanoprecipitation.
- Protocol: An ethanolic solution containing the ionizable lipid, phospholipid, cholesterol, and PEG-lipid is rapidly mixed with an aqueous buffer (e.g., citrate buffer at pH 4.0) containing the nucleic acid cargo within a microfluidic chip.
- Mechanism: The rapid mixing at the nanoscale triggers the protonation of ionizable lipids, which electrostatically interact with the anionic nucleic acids, leading to the self-assembly of LNPs with the nucleic acid encapsulated within.
- Typical Performance: Produces LNPs with a size range of 50-200 nm, high homogeneity (PDI <0.2), and encapsulation efficiency often exceeding 90% [56].
- High-Pressure Homogenization: Commonly used for Solid Lipid Nanoparticles (SLNs) and Nanostructured Lipid Carriers (NLCs).
- Hot Homogenization Protocol: The lipid phase is melted and mixed with the drug above its melting point. This melt is dispersed in a hot surfactant solution under high-speed stirring to form a pre-emulsion. This pre-emulsion is then passed through a high-pressure homogenizer (100-2000 bar) for several cycles, and the resulting nanoemulsion is cooled to form solid nanoparticles [57].
- Cold Homogenization Protocol: The drug is incorporated into a melted lipid, which is rapidly solidified using liquid nitrogen or dry ice. The solid mass is then ground into micrometer-sized particles. These particles are dispersed in a cold surfactant solution and homogenized at or below room temperature to form nanoparticles. This method is preferred for hydrophilic or thermolabile drugs [57].
The diagram below illustrates the microfluidic formulation workflow for LNPs.
Polymeric and Biomimetic Nanocarriers
Polymeric carriers offer immense versatility due to the wide range of available polymers and the ability to engineer precise chemical functionalities for controlled interactions.
Surface Patterning and Self-Assembly
A key challenge in diagnostics is creating uniform, high-density protein arrays. Moving beyond top-down lithography, diblock copolymer self-assembly presents a powerful bottom-up method for generating nanoscopic protein patterns [54]. This process relies on the microphase separation of chemically distinct polymer blocks (e.g., polystyrene and poly(methyl methacrylate)) to create periodically arranged, chemically heterogeneous surfaces with a periodicity of tens of nanometers. Proteins then adsorb selectively onto one of the nanoscale domains through self-selective interactions, leading to highly periodic and aligned nanoarrays instantaneously over large areas without the need for pre-patterning the substrate [54]. This method provides a fundamental single-biomolecule-level understanding of protein adsorption on a length scale commensurate with a single protein.
Cell Membrane-Coated Nanoparticles
A premier example of advanced biomimicry is the cell membrane-coated nanoparticle platform. This technology functionalizes synthetic nanoparticulate cores with a naturally derived cell membrane layer, creating particles that leverage the complex biological interactions of source cells [19] [18].
- Experimental Protocol for Coating:
- Source Cell Selection: Choose cells based on the desired targeting capability (e.g., red blood cells for long circulation, cancer cells for homotypic targeting, platelets for binding to damaged vasculature or bacteria).
- Membrane Isolation: Cells are lysed in a hypotonic solution and subjected to differential centrifugation (e.g., low-speed spins to remove nuclei and organelles, followed by ultracentrifugation at 100,000 x g) to collect the purified cell membrane vesicles.
- Membrane Fragmentation: The membrane vesicles are extruded through polycarbonate membranes (e.g., 400 nm, then 200 nm pores) to create small, unilamellar membrane fragments.
- Coating Synthesis: The pre-formed synthetic nanoparticle core (e.g., PLGA) is co-extruded with the cell membrane fragments through a porous membrane (e.g., 100-200 nm). Alternatively, sonication or microfluidic mixing can be used to fuse the membrane onto the core. The resulting core-shell nanoparticles are then purified via density gradient centrifugation [19] [18].
Table 2: Applications of Cell Membrane-Coated Nanoparticles
| Membrane Source | Inherent Biological Function | Nanoplatform Application |
|---|---|---|
| Red Blood Cell (RBC) | Long circulation, immune evasion via CD47 protein | "Stealth" nanocarriers for prolonged systemic drug delivery [18] |
| Cancer Cell | Homotypic adhesion to source cancer cells | Targeted delivery of chemotherapeutics to tumors; cancer vaccines [18] |
| Platelet | Adhesion to damaged vasculature and certain bacteria | Targeted delivery to atherosclerotic plaques or for treatment of bacterial infections [19] [18] |
| White Blood Cell | Inflammation and tumor targeting | Drug delivery to inflammatory sites and tumors [18] |
The following diagram outlines the synthesis workflow and the resulting multi-functional capabilities of these biomimetic nanoparticles.
Inorganic and Bio-Inspired Nanostructures
Inorganic nanoparticles provide unique physical properties (optical, magnetic, electronic) that are exploited for imaging, therapy, and sensing.
Metallic and Magnetic Nanoparticles
Gold nanoparticles (AuNPs) are widely used for their tunable surface plasmon resonance, which enables applications in photothermal therapy and colorimetric sensing. Magnetic nanoparticles (MNPs), typically based on iron oxides like Fe₃O₄ (magnetite), are used for magnetic resonance imaging (MRI) contrast and magnetic hyperthermia. A common method for their synthesis is co-precipitation.
- Protocol: An aqueous solution of Fe²⁺ and Fe³⁺ salts (e.g., in a 1:2 molar ratio) is mixed under an inert atmosphere. A base, such as ammonium hydroxide, is added rapidly under vigorous stirring, leading to the instantaneous formation of a black precipitate of magnetite. The particle size and shape can be controlled by parameters like temperature, pH, and ionic strength of the reaction medium. The nanoparticles are then often coated with a stabilizer like citric acid or polymers to prevent aggregation [57].
Viruses as Natural Nanoparticles
Virus capsids are exemplary biological nanostructures, optimized by evolution to carry, protect, and deliver genetic cargo [58]. These Virus-Like Particles (VLPs) can be repurposed as nanocarriers.
- Structure and Engineering: Viruses come in various precise shapes (icosahedrons, tubes) and sizes. Their structure is encoded in their genome, allowing for high reproducibility. Surface amino acids can be modified via genetic engineering (e.g., site-directed mutagenesis to introduce cysteine residues for thiol chemistry or lysines for amine chemistry) or bioconjugation to attach targeting ligands, drugs, or contrast agents [58].
- Applications: Plant viruses (e.g., Cowpea mosaic virus) and bacteriophages are being engineered as in situ vaccines to stimulate anti-tumor immunity, as targeted drug delivery vectors, and as contrast agents for medical imaging by integrating metal ions into their protein cages [58].
The Scientist's Toolkit: Essential Research Reagents and Materials
This table catalogs key reagents and their functions for researching and developing advanced nanoplatforms.
Table 3: Essential Research Reagent Solutions for Nanoplatform Development
| Reagent / Material | Category | Primary Function in R&D |
|---|---|---|
| Ionizable Cationic Lipids | Lipid Nanoparticles | Enables efficient RNA encapsulation and endosomal escape; a key determinant of LNP performance and toxicity [55] [56] |
| DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | Lipid Nanoparticles | A saturated phospholipid that provides structural integrity to the lipid bilayer in LNPs and liposomes [56] |
| DMG-PEG2000 | Lipid Nanoparticles | A PEG-lipid conjugate used to control LNP size, reduce aggregation, and prolong circulation time by minimizing nonspecific interactions [56] |
| PLGA (Poly(lactic-co-glycolic acid)) | Polymeric Nanoparticles | A biodegradable polymer used as a core material for sustained and controlled drug release; commonly used in cell membrane coating strategies [18] |
| Polydopamine | Bio-Inspired Coating | A versatile mussel-inspired polymer for creating thin, adhesive coatings on nanoparticles, facilitating further functionalization and providing photothermal properties [58] |
| Microfluidic Chips | Formulation Equipment | Enables precise, reproducible, and scalable manufacturing of nanoparticles with controlled properties via rapid mixing [56] |
| Extrusion Assembles | Formulation Equipment | Used for size homogenization of liposomes and for fusing cell membrane coatings onto nanoparticle cores [18] |
The frontier of nanoscale biological interactions research is driving the evolution of advanced nanoplatforms from simple delivery vehicles to sophisticated, multifunctional therapeutics. The future lies in designing intrinsically functional systems—such as LNPs with bioactive lipids, biomimetic cell-membrane coatings, and engineered viral capsids—that minimize complexity while maximizing targeting and efficacy. Key challenges remain in scaling up manufacturing with high reproducibility, thoroughly understanding long-term biocompatibility and potential immunogenicity, and navigating regulatory pathways. As our fundamental knowledge of nano-bio interfaces deepens, the next generation of nanoplatforms will increasingly leverage data-driven design, artificial intelligence, and synthetic biology to create truly intelligent systems for precision medicine.
The manipulation of matter at the nanoscale (1-100 nm) has unlocked unprecedented opportunities in medicine by enabling precise interactions with biological systems [59]. At this scale, materials exhibit unique physicochemical properties that allow them to interface with cellular machinery, cross biological barriers, and modulate immune responses with remarkable specificity [34]. The foundational principle governing these applications is the deliberate engineering of nanoparticles to achieve targeted interactions with specific immune cells, pathogens, or diseased tissues [36]. This whitepaper examines how these fundamental nanoscale interactions are being harnessed across three distinct therapeutic domains: oncology, infectious disease, and autoimmunity, highlighting the shared mechanistic principles while detailing domain-specific applications.
Nanotechnology in Cancer Therapy
Mechanisms of Action and Key Targets
Cancer nanomedicine leverages the unique pathophysiology of tumors, particularly the enhanced permeability and retention (EPR) effect, for passive targeting. Nanoparticles preferentially accumulate in tumor tissues due to their leaky vasculature and impaired lymphatic drainage [34]. Active targeting is achieved through surface functionalization with ligands that bind receptors overexpressed on cancer cells or immune cells within the tumor microenvironment (TME) [60].
Key Pathways and Cellular Targets:
- cGAS-STING Pathway Activation: Certain nanocarriers co-deliver cisplatin and camptothecin to induce DNA damage, stimulating the cGAS-STING pathway and promoting dendritic cell maturation and CD8+ T cell infiltration [60].
- Immune Checkpoint Modulation: Nanoparticles can be engineered to deliver JQ1, which downregulates c-Myc and PD-L1, counteracting therapy-induced immune evasion [60].
- Treg Cell Suppression: tLyp1 peptide-functionalized hybrid nanoparticles target regulatory T cells (Tregs) and inhibit STAT3/STAT5 phosphorylation, reducing immunosuppression in the TME [60].
- CAR-T Cell Engineering: Lipid nanoparticles (LNPs) modified with CD3 antibodies can deliver plasmid DNA encoding chimeric antigen receptors (CARs) and IL-6 shRNA to generate CAR-T cells in vivo while mitigating cytokine release syndrome [60].
Experimental Models and Assessment Methodologies
In vivo efficacy is typically evaluated in murine models of colorectal cancer, pancreatic cancer, or leukemia. Key endpoints include tumor volume measurement, immunohistochemical analysis of immune cell infiltration (CD8+ T cells, NK cells, Tregs), and survival studies [60]. Flow cytometry of dissociated tumors quantifies immune cell populations, while cytokine profiling assesses immunomodulatory effects.
Table 1: Nanoparticle Platforms for Cancer Immunotherapy
| Nanoparticle Platform | Therapeutic Cargo | Target Cell/Pathway | Observed Outcome |
|---|---|---|---|
| CPT-Pt(IV) Prodrug NP | Cisplatin, Camptothecin | cGAS-STING pathway | Increased CD8+ T cell infiltration, tumor suppression [60] |
| Hyaluronic Acid/Adamantane NP | Pyropheophorbide-a, JQ1 | CD44+ pancreatic cancer cells | Enhanced T lymphocyte infiltration, PD-L1 downregulation [60] |
| tLyp1 peptide-improved hybrid NP | Imatinib | Treg cells (STAT3/STAT5) | Reduced Treg suppression, increased CD8+ T cells [60] |
| AntiCD3-LNP/CAR19 + shIL6 | CAR DNA, IL-6 shRNA | T cells | In vivo CAR-T generation, reduced cytokine release [60] |
| Selenopeptide NP | Doxorubicin | NK cells | Synergistic chemo-immunotherapy, NK cell activation [60] |
Signaling Pathway Visualization
Diagram 1: Nanoparticle Modulation of Anti-Tumor Immunity. NPs can activate cytotoxic pathways via cGAS-STING and simultaneously suppress immunosuppressive Treg activity.
Nanotechnology in Infectious Disease Management
Diagnostic and Therapeutic Platforms
Aptasensor Diagnostics: Aptamer-based sensors (aptasensors) offer rapid, sensitive pathogen detection through multiple transduction mechanisms including colorimetry, fluorescence, electrochemistry, surface-enhanced Raman spectroscopy (SERS), and surface plasmon resonance (SPR) [61]. These systems leverage the high specificity of aptamers selected via Systematic Evolution of Ligands by Exponential Enrichment (SELEX) to bind viral proteins, whole pathogens, or toxins.
Engineered Membrane Vesicle Therapies: EMVs derived from red blood cells, platelets, macrophages, or bacteria can be functionalized for targeted anti-infective therapy [62]. Applications include:
- Targeted Drug Delivery: EMVs functionalized with pathogen-targeting ligands enable precise antibiotic delivery.
- Pathogen and Toxin Neutralization: EMVs act as decoys for bacterial toxins, viruses, and inflammatory cytokines.
- Nanovaccines: EMVs displaying antigenic epitopes stimulate robust, specific immune responses [62].
Experimental Protocols for Aptasensor Development
SELEX Protocol for Aptamer Selection:
- Library Preparation: Synthesize a random single-stranded DNA or RNA library (10^14-10^15 sequences).
- Incubation with Target: Expose library to immobilized target (purified pathogen proteins or whole inactivated pathogens).
- Partitioning: Separate bound from unbound sequences through washing.
- Amplification: PCR amplify bound sequences (RT-PCR for RNA libraries).
- Stringency Cycling: Repeat binding under increasingly stringent conditions (8-15 cycles).
- Cloning and Sequencing: Identify enriched sequences through cloning and Sanger sequencing or high-throughput sequencing.
- Characterization: Determine binding affinity (K_d) and specificity of selected aptamers via ELISA or surface plasmon resonance [61].
Aptasensor Fabrication and Validation: For electrochemical aptasensors, immobilize thiolated aptamers on gold electrodes. Measure electrical impedance or voltammetric changes upon target binding. Validate against clinical samples, determining sensitivity, specificity, limit of detection (LOD), and dynamic range [61].
Table 2: Nano-Platforms for Infectious Disease Management
| Platform | Mechanism | Target Pathogen | Key Advantage |
|---|---|---|---|
| Aptasensors | Pathogen recognition via immobilized aptamers | Viruses (SARS-CoV-2, HIV, HBV), Bacteria | Rapid, low-cost, high-sensitivity detection [61] |
| EMVs (Red Blood Cell) | Toxin decoy, Drug delivery | Bacterial toxins, Broad-spectrum | Long circulation time, biocompatibility [62] |
| EMVs (Bacterial OMV) | Natural immunogenicity, Antigen display | Bacterial sources, Viral antigens | Intrinsic adjuvant properties, versatile engineering [62] |
| EMVs (Macrophage) | Inflammatory targeting, Cytokine neutralization | Sepsis, hyperinflammation | Innate tropism to inflamed tissues [62] |
Diagnostic and Therapeutic Action Workflow
Diagram 2: Integrated Diagnostic and Therapeutic Action. Parallel pathways show rapid detection via aptasensors and multi-pronged therapeutic action through EMVs.
Nanotechnology in Autoimmune Disorder Management
Restoring Immune Tolerance
Autoimmune disease management using nanotechnology focuses on achieving immune tolerance without systemic immunosuppression through two primary strategies:
Targeted Immunosuppressant Delivery: Nanoparticles encapsulate immunosuppressive drugs (e.g., methotrexate, prednisolone) and are functionalized to target inflamed tissues or specific immune cells. Hyaluronic acid-based NPs preferentially accumulate in inflamed joints for rheumatoid arthritis treatment, minimizing off-target effects [63].
Active Immune Tolerance Induction: Nanoparticles are engineered to directly modulate autoreactive immune cells:
- Navacims: MHC-peptide complexes displayed on nanoparticles bind autoreactive T cells and reprogram them into regulatory T cells [63].
- Liposomal Autoantigens: Liposomes encapsulating autoantigens promote antigen-specific tolerance in Type 1 diabetes, multiple sclerosis, and rheumatoid arthritis models [63].
- mRNA-LNPs: Lipid nanoparticles deliver mRNA to T cells, generating immunosuppressive cells that dampen pro-inflammatory responses [63].
Key Methodologies and Assessment
Nanoparticle Synthesis and Functionalization:
- Lipid Nanoparticles: Prepare via microfluidic mixing of ionizable lipids, phospholipids, cholesterol, and PEG-lipids with mRNA payload.
- Surface Functionalization: Conjugate targeting ligands (antibodies, peptides, hyaluronic acid) using maleimide-thiol chemistry or carbodiimide crosslinking.
- Characterization: Determine size (dynamic light scattering), zeta potential (laser Doppler electrophoresis), encapsulation efficiency (HPLC), and morphology (transmission electron microscopy).
In Vivo Efficacy Models:
- Collagen-Induced Arthritis: Assess nanoparticle accumulation in joints, clinical arthritis scores, histopathological evaluation, and cytokine profiling.
- Experimental Autoimmune Encephalomyelitis: Monitor disease progression, CNS infiltration, and antigen-specific T cell responses.
- NOD Mouse Model (Type 1 Diabetes): Track blood glucose, insulitis scores, and autoreactive T cell populations.
Table 3: Nanotechnology Approaches for Autoimmune Diseases
| Nanoparticle Platform | Therapeutic Agent | Target Disease | Mechanism of Action |
|---|---|---|---|
| Hyaluronic Acid NP | Methotrexate | Rheumatoid Arthritis | Targeted joint delivery, reduced systemic exposure [63] |
| Liposome | Prednisolone phosphate | Arthritis (Rat Model) | Sustained release in inflamed tissue [63] |
| Navacims | MHC-Peptide Complexes | Multiple Autoimmune Diseases | Autoreactive T cell reprogramming to Tregs [63] |
| mRNA-LNP | mRNA encoding immunomodulators | Autoimmunity (Preclinical) | In vivo generation of immunosuppressive cells [63] |
| Iron Oxide NP | None (Imaging Agent) | Multiple Sclerosis, Type 1 Diabetes | Detection of inflammatory lesions via MRI [63] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Nanotechnology Development
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Ionizable Lipids | LNP core structure, mRNA encapsulation | mRNA-LNP for immune tolerance [63] |
| DSPE-PEG | Nanoparticle stealth coating, functionalization | Prolonged circulation, ligand conjugation [59] [62] |
| Hyaluronic Acid | Targeting ligand, biodegradable polymer | Joint-targeted delivery in arthritis [63] |
| Maleimide-functionalized Lipids | Covalent conjugation of thiolated ligands | Antibody, peptide attachment to NP surface [62] |
| PLGA | Biodegradable polymer for controlled release | Sustained drug delivery platforms [59] [64] |
| Gold Nanoparticles | Plasmonic core for sensing/therapy | Photothermal therapy, diagnostic probes [63] [64] |
| Quantum Dots | Fluorescent imaging agents | Multiplexed biomarker detection [64] |
| Magnetic Nanoparticles | MRI contrast, magnetic targeting | Inflammation detection, targeted delivery [63] [64] |
| Aptamers (ssDNA/RNA) | Target recognition elements | Pathogen detection, targeted therapeutics [61] |
The applications of nanotechnology across cancer therapy, infectious disease, and autoimmune disorders share fundamental principles: leveraging nanoscale properties for targeted delivery, overcoming biological barriers, and achieving specific immunomodulation. While the therapeutic objectives differ—immune activation in cancer, pathogen clearance in infection, and tolerance restoration in autoimmunity—the core approach remains engineering nanoparticles to interact precisely with biological targets. Future progress hinges on addressing translational challenges including biocompatibility, scalable manufacturing, and rigorous safety assessment [36] [34]. The continued elucidation of nanoscale biological interactions will enable increasingly sophisticated therapeutic platforms, ultimately yielding more effective and personalized medical treatments across these diverse disease domains.
Overcoming Biological Challenges: Optimization Strategies for Improved Nano-Bio Performance
The mononuclear phagocyte system (MPS), previously referred to as the reticuloendothelial system (RES), constitutes a primary barrier that nanoparticles encounter following intravenous administration [65]. This sophisticated biological defense network includes resident tissue macrophages in organs such as the liver and spleen, along with blood monocytes, dendritic cells, and their bone marrow progenitors [65]. Upon entering the bloodstream, nanocarriers are rapidly coated by serum proteins in a process known as opsonization, which triggers their recognition and clearance by MPS cells through a variety of receptors [65]. This biological response presents a significant challenge for nanocarrier drug delivery systems (NDDS), as many particles exhibit a blood half-life of less than several minutes, with less than 1% of the injected dose typically reaching the intended target tissue [65] [66].
The imperative to overcome this biological barrier stems from the tremendous potential of nanocarriers in therapeutic applications, particularly in oncology. These systems can improve the pharmacokinetic profiles and bioavailability of carried drugs, enable accurate delivery to tumor or target sites, and enhance therapeutic outcomes [66]. However, the propensity of nanoparticles circulating in the blood to be recognized and opsonized makes them susceptible to phagocytic clearance by the MPS, substantially undermining their targeting efficacy and therapeutic potential [66]. This review comprehensively addresses the strategies being developed to mitigate immune recognition, reduce opsonization, and evade MPS clearance, thereby advancing the clinical application of nanomedicines.
Core Mechanisms of Nanoparticle Clearance
The Mononuclear Phagocyte System
The MPS functions as a pivotal defense mechanism responsible for the degradation and removal of exogenous substances from the blood, including foreign pathogens and therapeutic nanoparticles [66]. The endothelial cells within MPS-related organs are typically fenestrated, which facilitates the filtering of substances in the bloodstream. Nanoparticles of approximately 100 nm in size can pass through the endothelial fenestrations in the liver and spleen, as well as the vascular endothelium in lymph nodes, making them particularly vulnerable to clearance [66]. The orchestrated action of MPS components represents the fundamental pathway through which conventional nanoparticles are eliminated from circulation.
Protein Corona Formation and Opsonization
The process of opsonization begins immediately upon nanoparticle introduction to biological fluids. Serum proteins adsorb to the nanoparticle surface, forming a "protein corona" that determines the biological identity presented to immune cells [65]. This corona typically includes immunoglobulins, complement proteins, and other opsonins that mark the particle for phagocytosis. The composition of this protein layer depends on the nanoparticle's surface chemistry, charge, hydrophobicity, and topography, with certain surface characteristics favoring the adsorption of specific proteins that either promote or mitigate immune recognition [67].
Accelerated Blood Clearance (ABC) Phenomenon
A significant challenge in clinical translation is the accelerated blood clearance (ABC) phenomenon, which occurs upon repeated administration of nanocarriers [67] [66]. This phenomenon is characterized by the rapid clearance of a subsequent dose from the bloodstream and markedly augmented liver accumulation, substantially undermining targeting efficacy and therapeutic effect [66]. The ABC phenomenon was first observed with PEGylated liposomes but has since been documented with various nanocarriers, including solid lipid nanoparticles, nanoemulsions, lipid nanoparticles, and exosomes [66].
The immunological mechanism behind ABC involves anti-PEG IgM antibodies produced in response to initial doses [66]. PEG polymers feature a repetitive structure resembling T cell-independent type 2 antigens, enabling them to activate B-1 and B-2 lymphocytes, leading to anti-PEG IgM production [66]. The spleen plays a vital role in this immune reaction, with splenic marginal zone B cells being dominant IgM-positive B cells tightly associated with inducing anti-PEG IgM [66]. Subsequent doses of PEGylated nanoparticles are then rapidly opsonized by these pre-existing antibodies and cleared by phagocytes.
Table 1: Nanocarrier Types Documented to Induce ABC Phenomenon
| Nanocarrier Type | Key Characteristics | Primary Clearance Organs |
|---|---|---|
| Liposomes (PEGylated and conventional) | Lipid bilayer vesicles, tunable size | Liver, spleen |
| Polymeric nanoparticles | Biodegradable polymers, sustained release | Liver, spleen |
| Micelles | Amphiphilic block copolymers | Liver |
| Nanoemulsions | Oil-in-water droplets, thermodynamically stable | Liver |
| Solid lipid nanoparticles | Solid lipid core, improved stability | Liver, spleen |
| Lipid nanoparticles (LNP) | Ionizable lipids, nucleic acid delivery | Liver |
| Microbubbles | Gas-filled cores, imaging and delivery | Liver, lungs |
| Exosomes | Endogenous vesicles, innate tropism | Liver |
Strategic Approaches to Evade Immune Recognition
Surface Engineering and Stealth Coatings
Surface modification represents the most extensively investigated strategy for mitigating opsonization and MPS clearance. The approach involves engineering nanoparticle surfaces to minimize protein adsorption and subsequent immune recognition.
Polyethylene Glycol (PEG) Coating: PEGylation has been the gold standard for stealth nanocarriers for decades [67]. The hydrophilic PEG chains create a steric hurdle that hinders interactions between nanoparticles and opsonins, as well as phagocytic cells such as Kupffer cells, thereby imparting a "stealth effect" [67]. This is achieved through the formation of a hydration layer around nanoparticles, which reduces recognition and binding of nanoparticles by opsonins via spatial repulsion [66]. However, the limitations of PEGylation, particularly the ABC phenomenon upon repeated administration, have motivated the development of alternative strategies [67] [66].
Biomimetic Surface Modifications: Emerging approaches focus on nature-inspired strategies that replicate the properties of biological entities to evade immune detection [67]. These include:
- Cell Membrane Coating: Nanoparticles cloaked with membranes from red blood cells, leukocytes, or platelets inherit the surface proteins and functions of the source cells [67]. RBC membrane-camouflaged nanoparticles, for instance, display "self" markers like CD47 that inhibit phagocytosis by signaling through the CD47-SIRPα pathway [67].
- Polysaccharide Coatings: Materials such as polysialic acid, hyaluronic acid, and dextran provide hydrophilicity and steric hindrance similar to PEG while potentially exhibiting lower immunogenicity [67].
- "Self" Peptide Display: Surface modification with peptides mimicking "self" markers (e.g., CD47) can directly engage inhibitory receptors on phagocytes [68].
Transient MPS Blockade and Modulation
Rather than engineering individual nanoparticles to evade detection, an alternative approach involves temporarily modulating MPS function to create a therapeutic window for nanoparticle delivery.
Macrophage Saturation: This method involves administering blank nanoparticles or macromolecules to saturate phagocytic capacity before delivering therapeutic nanocarriers [65]. The approach has been rediscovered multiple times under different names including "macrophage priming," "preconditioning," and "inverse targeting" [65]. The saturation of macrophages with blocking agents has been shown to improve MRI imaging of tumors with iron oxide nanoparticles and enhance the therapeutic efficacy of drug-loaded vesicles [65].
Macrophage Depletion: More aggressive approaches utilize cytotoxic compounds to deplete macrophage populations temporarily [65]. Liposomal clodronate and gadolinium chloride have been employed to reduce Kupffer cells in the liver and macrophages in the spleen [65]. While effective in preclinical models, these methods raise concerns about long-term impacts on innate immunity and have relatively low potential for clinical translation [65].
Pharmacologic Inhibition: Several clinically approved drugs that impact endosome formation and trafficking can induce MPS blockade [65]. Esomeprazole, a proton-pump inhibitor, blocks V-ATPase and alters lysosomal trafficking in tissue macrophages, hampering MPS uptake of therapeutic nanoparticles and increasing their tumor delivery by 1.8-fold [65]. Chloroquine, an established antimalarial agent, has also shown potential for MPS blockade [65].
Table 2: MPS Blockade Agents and Their Mechanisms
| Blockade Agent | Mechanism of Action | Efficacy | Clinical Translation Potential |
|---|---|---|---|
| Liposomal clodronate | Induces apoptosis in phagocytes via mitochondrial ADP/ATP translocase inhibition | Up to 150x enhancement in tumor delivery [65] | Low due to long-term effects on innate immunity |
| Gadolinium chloride | Suppresses phagocytosis by inhibiting Ca2+ transport through cell membrane | Improves tumor imaging with quantum dots [65] | Moderate, limited by toxicity concerns |
| Empty liposomes (saturation) | Saturates phagocytic pathways and clearance mechanisms | Demonstrated efficacy in enhancing particle circulation [65] | High, especially with clinically approved lipid formulations |
| Esomeprazole | Blocks V-ATPase, alters lysosomal trafficking | 1.8-fold increase in tumor delivery [65] | High, as it is already clinically approved |
| Chloroquine | Alters lysosomal pH and function | Preclinical evidence of reduced clearance | High, known safety profile |
Experimental Protocols for Evaluating Immune Evasion
Assessing Pharmacokinetics and Biodistribution
Protocol: Quantitative Biodistribution Analysis
- Nanoparticle Labeling: Incorporate radioactive (e.g., 111In, 99mTc) or fluorescent labels (e.g., DiR, Cy5.5) during nanoparticle synthesis. Validate that labeling does not significantly alter surface properties.
- Animal Models: Use appropriate animal models (typically mice or rats) with consideration for species differences in MPS function. For ABC studies, ensure animals are naïve to prior nanoparticle exposure unless specifically testing the phenomenon.
- Administration and Sampling: Administer nanoparticles intravenously via tail vein. Collect blood samples at predetermined time points (e.g., 1, 5, 15, 30, 60, 120, 240 minutes post-injection).
- Organ Harvesting and Analysis: Euthanize animals at designated endpoints. Harvest organs of interest (liver, spleen, kidneys, heart, lungs, tumor). For radioactive labels, measure gamma counts. For fluorescent labels, use near-infrared imaging systems or extract dyes for quantitative measurement.
- Pharmacokinetic Modeling: Calculate key parameters including half-life (t1/2), area under the curve (AUC), clearance (CL), and volume of distribution (Vd) from blood concentration data. Compare biodistribution patterns between experimental groups.
Protocol: Evaluating ABC Phenomenon
- Priming Dose: Administer initial dose of test nanoparticles to experimental animals. Maintain control group without priming dose.
- Waiting Period: Allow specific interval between doses (typically 5-14 days) for immune response development.
- Challenging Dose: Administer second dose of identical nanoparticles.
- Blood Clearance Assessment: Monitor blood clearance rates of challenging dose compared to controls.
- Anti-Nanoparticle Antibody Detection: Collect serum before challenging dose. Measure anti-nanoparticle IgM and IgG levels using ELISA with nanoparticle-coated plates.
Characterizing Protein Corona Composition
Protocol: Protein Corona Isolation and Analysis
- Corona Formation: Incubate nanoparticles with human or mouse plasma (typically 1-2 mg/mL nanoparticle concentration in 50-100% plasma) for 1 hour at 37°C.
- Corona Isolation: Separate nanoparticle-protein complexes from unbound proteins via centrifugation (ultracentrifugation or density gradient centrifugation) or size exclusion chromatography.
- Protein Elution and Digestion: Dissociate proteins from nanoparticle surface using SDS buffer or organic solvents. Digest proteins with trypsin.
- Protein Identification: Analyze digested peptides using liquid chromatography-tandem mass spectrometry (LC-MS/MS). Identify proteins by searching against appropriate databases.
- Quantitative Analysis: Use label-free quantitation or isobaric tagging (TMT, iTRAQ) to compare corona compositions between different nanoparticle formulations.
Cellular Uptake and Phagocytosis Assays
Protocol: In Vitro Phagocytosis Assay
- Cell Culture: Maintain relevant phagocytic cells (e.g., RAW 264.7 macrophage cell line, primary Kupffer cells, or bone marrow-derived macrophages) under standard conditions.
- Nanoparticle Exposure: Incubate cells with fluorescently labeled nanoparticles at physiologically relevant concentrations (typically 10-100 μg/mL) for 1-4 hours.
- Quenching External Fluorescence: Treat cells with trypan blue or similar quenching agent to distinguish internalized from surface-bound nanoparticles.
- Quantification: Analyze using flow cytometry to determine percentage of nanoparticle-positive cells and mean fluorescence intensity. Confirm with confocal microscopy for visual internalization assessment.
- Inhibition Studies: Pre-treat cells with phagocytosis inhibitors (e.g., cytochalasin D for actin polymerization, chlorpromazine for clathrin-mediated endocytosis) to elucidate uptake mechanisms.
Visualization of Key Biological Pathways and Experimental Workflows
Nanoparticle Clearance Pathways and Evasion Strategies
Diagram 1: Nanoparticle Clearance Pathways and Evasion Strategies. This workflow illustrates the primary clearance pathway (red) that nanoparticles follow after administration, and the strategic intervention points (green) to evade immune recognition and achieve target site accumulation (blue).
Accelerated Blood Clearance (ABC) Phenomenon Mechanism
Diagram 2: ABC Phenomenon Mechanism and Prevention. This diagram outlines the immunological cascade leading to accelerated clearance of repeated nanoparticle doses (red/orange) and potential preventive strategies (green) that can interrupt this process at various stages.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Nanoparticle Immune Evasion
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Stealth Polymers | PEG (various MW), Polysialic acid, Poly(2-oxazoline), Poly(glycerol) | Create steric barrier against opsonization | PEG molecular weight, density, conformation; ABC phenomenon potential |
| Biomimetic Materials | Red blood cell membranes, Leukocyte membranes, Platelet membranes | Provide "self" camouflage; inherit source cell functions | Source compatibility, isolation purity, coating efficiency |
| MPS Blockade Agents | Liposomal clodronate, Gadolinium chloride, Empty liposomes, Esomeprazole | Temporarily suppress MPS clearance function | Timing, dosage, toxicity, specificity of effect |
| Phagocytic Cells | RAW 264.7, J774A.1, Primary Kupffer cells, Bone marrow-derived macrophages | In vitro phagocytosis assays | Species matching, polarization state, culture conditions |
| Analytical Tools | Dynamic light scattering, Nanoparticle tracking analysis, Flow cytometry, LC-MS/MS | Characterization of size, charge, protein corona, cellular uptake | Multi-method validation required for comprehensive assessment |
| Animal Models | Mice (various strains), Rats, Transgenic models (e.g., macrophage-depleted) | In vivo biodistribution and pharmacokinetics | Species differences in MPS function, immune competence |
The challenge of mitigating immune recognition and MPS clearance of nanoparticles represents a central problem in nanomedicine that intersects materials science, immunology, and pharmacology. While significant progress has been made in understanding the fundamental mechanisms and developing evasion strategies, the perfect stealth nanoparticle remains elusive. Current approaches each present trade-offs: PEGylation suffers from the ABC phenomenon, biomimetic strategies face manufacturing complexities, and MPS blockade introduces additional pharmacological variables.
The future direction points toward intelligent, multifunctional systems that can dynamically respond to their environment or selectively engage with specific biological components while avoiding immune detection. Advances in our understanding of protein corona formation may lead to precision surface engineering that directs favorable opsonin adsorption. Similarly, deeper insights into the immunological mechanisms of the ABC phenomenon may yield strategies to induce tolerance rather than simply avoid detection.
As nanomedicine progresses toward increasingly sophisticated applications, including combination therapies that pair nanocarriers with immunomodulatory agents, the ability to precisely control nanoparticle pharmacokinetics through managed immune interactions will become ever more critical. The strategies outlined in this review provide both the foundational approaches and emerging frameworks for overcoming the biological barriers that have long constrained the full realization of nanomedicine's potential.
The expansion of nanotechnology in biomedicine necessitates a profound understanding of nanoscale biological interactions to mitigate potential toxicological risks. This whitepaper provides an in-depth analysis of the mechanisms underlying nanoparticle toxicity and explores advanced material selection and surface modification strategies to enhance biocompatibility. Within the broader thesis of nanoscale biological interactions research, we detail how physicochemical properties dictate biological responses and present systematic methodologies for evaluating and engineering safer nanoscale materials. The integration of computational predictions, rigorous experimental protocols, and strategic surface engineering provides a framework for developing next-generation nanomaterials with optimized safety profiles for therapeutic and diagnostic applications.
Nanomaterials possess unique physicochemical properties, such as high surface area-to-volume ratios, tunable optical and electronic behavior, and enhanced reactivity, which underpin their diverse applications in medicine, drug delivery, and diagnostics [69]. However, these same properties can elicit adverse biological effects, including oxidative stress, inflammatory responses, and cellular dysfunction, making the assessment of their biocompatibility a critical research frontier [3] [69]. The journey of nanoparticles within a biological system begins at the exposure point (e.g., respiratory system, digestive tract, or via intravenous injection), followed by translocation across biological barriers and systemic distribution to secondary organs [3]. A profound understanding of these interactions at the cellular, organ, and systemic levels is essential to accurately predict toxicological impacts and design practical approaches to eliminate them [3]. This guide frames these concepts within the fundamental research on nanoscale biological interactions, providing researchers and drug development professionals with actionable strategies for material selection and surface engineering to overcome toxicity challenges.
Fundamental Mechanisms of Nanomaterial Toxicity
The toxicity of nanomaterials is not governed by a single factor but by the complex interplay of multiple structural, chemical, and environmental variables. A systematic understanding of these mechanisms is a cornerstone of nanoscale biological interactions research.
Cellular Perturbations and Organ-Level Effects
After entering cells via endocytosis or other pathways, nanoparticles can escape endosomes and accumulate in critical organelles, initiating a cascade of disruptive events [3].
- Membrane and Cytoskeleton Disruption: Nanoparticles can adhere to and disrupt cell membrane structure and function [3].
- Mitochondrial Dysfunction: Accumulation in mitochondria can perturb their function, leading to disrupted energy production and triggering apoptosis [3].
- Genotoxic Effects: Some nanoparticles can transport into the nucleus, causing DNA damage and nuclear alterations [3].
- Cell Death Induction: These disruptions can lead to various forms of cell death, including necrosis, apoptosis, autophagy, pyroptosis, and ferroptosis [3].
At the organ level, nanoparticles can damage functional cells, leading to inflammatory responses and organ damage. For instance, inhaled particles can cause pulmonary inflammation and fibrosis, while distributed particles can accumulate in the liver and spleen, potentially causing toxicity [3].
Oxidative Stress and Signaling Pathways
A primary mechanism of nanoparticle toxicity is the generation of reactive oxygen species (ROS), which disrupts cellular redox homeostasis [69]. This oxidative stress can damage cellular proteins, lipids, and DNA [69]. The ensuing cascade of molecular events involves the perturbation of key cellular signaling pathways:
- NF-κB Pathway: Activation of this pathway by nanoparticles can lead to the expression of pro-inflammatory cytokines, driving inflammation [3].
- MAPK Pathway: This pathway can be activated by oxidative stress, influencing cell decisions regarding proliferation, differentiation, and apoptosis [3].
- Nrf2 Pathway: In response to oxidative stress, the Nrf2 pathway is activated to upregulate the expression of antioxidant genes [3].
The following diagram illustrates the core signaling pathways implicated in nanoparticle-induced toxicity.
Physicochemical Properties Governing Toxicity and Biocompatibility
The biological fate and toxic potential of nanomaterials are decisively influenced by their intrinsic physicochemical properties. Even slight modifications can result in significant changes to their biodistribution, clearance, and toxicity profiles [69].
Table 1: Key Physicochemical Properties and Their Influence on Biocompatibility
| Property | Biological Influence | Key Findings |
|---|---|---|
| Size | Cellular uptake, biodistribution, clearance mechanism [3] [69]. | Smaller particles (< 5.5 nm) may undergo renal clearance; larger particles accumulate in liver/spleen. Smaller NPs generally show higher tissue distribution and toxicity [3] [69]. |
| Shape | Cellular internalization, flow dynamics, membrane disruption [69]. | Needle- or plate-like particles can physically disrupt cell membranes. Nanorod-shaped ZnO shown more toxic than spherical counterparts [69]. |
| Surface Charge | Interaction with cell membranes, protein adsorption, cytotoxicity [3] [69]. | Positively charged NPs exhibit higher cytotoxicity due to electrostatic attraction to negatively charged cell membranes [3] [69]. |
| Surface Chemistry | Biocompatibility, stealth properties, targeting, solubility [3] [4]. | Hydrophobic NPs tend to aggregate and adsorb proteins, leading to rapid clearance. PEGylation creates a "stealth" effect to prolong circulation [4]. |
| Material Composition | Inherent chemical reactivity, ion release, catalytic (nanozyme) activity [69]. | Metallic composition (e.g., Ag, Cu) can release toxic ions. Many metal/metal oxide NPs exhibit enzyme-like activities that disrupt redox homeostasis [69]. |
Surface Modification Strategies for Enhanced Biocompatibility
Surface modification is a powerful and versatile approach to modulating the physicochemical and biological properties of nanoparticles, thereby achieving desired therapeutic efficacy and safety [4]. The following diagram outlines a strategic workflow for selecting and implementing these surface modifications.
Strategic Approaches and Their Applications
Stealth Coatings: Polyethylene glycol (PEG) creates a hydrophilic protective layer that reduces protein adsorption (opsonization) and recognition by the mononuclear phagocyte system (MPS), significantly prolonging circulation half-life. For example, Doxil (PEGylated liposomal doxorubicin) exhibits a 90-fold increase in bioavailability compared to free drug [4]. Chitosan, a biocompatible polysaccharide, confers a positive surface charge, facilitating electrostatic interaction with negatively charged mucosal layers to enhance residence time and drug absorption at specific sites [4].
Active Targeting Ligands: Conjugating nanoparticles with antibodies, peptides, or small molecules enables active targeting to specific receptors overexpressed on target cells (e.g., cancer cells). This "active coating" enhances cellular uptake at the desired site, improving therapeutic efficacy and reducing off-target effects and systemic toxicity [4].
Safer-by-Design and Functional Modifications: This proactive approach involves engineering nanoparticles to minimize inherent hazards. Surface modification can reduce biotoxicity and increase biocompatibility by altering charge, hydrophobicity, and reactivity [3]. For implantable materials, techniques like laser surface patterning can create specific hydrophilic or hydrophobic microstructures (e.g., 'Line' or 'Grid' patterns) that directly control cell adhesion, migration, and drug release profiles [70].
Advanced Surface Modification Techniques for Implants
In orthopedic and dental applications, titanium (Ti) implants are widely used, but their clinical performance depends critically on surface properties that govern osteointegration and resistance to bacterial infection [71]. Advanced surface modification techniques have been developed to functionalize these implants.
Ion Doping and Composite Coatings
Table 2: Efficacy of Ion-Doped Coatings for Titanium Implants
| Coating Type | Osteogenic Performance | Antibacterial Efficacy |
|---|---|---|
| Zinc (Zn)-doped | Increased osteoblast proliferation by 25%; enhanced cell adhesion by 40% [71]. | 24% inhibition of Staphylococcus aureus [71]. |
| Magnesium (Mg)-doped | 38% increase in alkaline phosphatase (ALP) activity; 4.5-fold increase in cell proliferation [71]. | Data not specified in search results. |
| Copper (Cu)-doped | Data not specified in search results. | 99.45% against S. aureus; 98.65% against Escherichia coli [71]. |
| Zn-substituted Hydroxyapatite (HAp) | Promoted mineralized nodule formation by 4.5-fold [71]. | 16.25% bacterial inhibition against E. coli [71]. |
These ion-doped coatings work by providing a controlled release of bioactive ions at the implant-tissue interface, stimulating desired cellular responses while inhibiting bacterial growth [71]. The trend is moving toward multi-functional coatings that simultaneously incorporate osteogenic, antibacterial, and immunomodulatory properties to enhance clinical performance and patient outcomes [71].
Laser-Based Surface Engineering
High-focus laser scanning (HFLS) systems represent a precision tool for implant surface modification. This technique can easily and rapidly pattern material surfaces into specific hydrophilic (e.g., 'Line') or hydrophobic (e.g., 'Grid') structures [70]. These modified surfaces directly influence biological responses: the hydrophilic 'Line' pattern promotes the spread of cell culture medium and enhances cell adhesion and migration, while the hydrophobic 'Grid' pattern shows minimal spread [70]. Furthermore, HFLS-modified materials demonstrate increased drug (e.g., prednisolone) retention and controlled release, maintaining anti-inflammatory effects by reducing the expression of cytokines associated with M1 macrophages [70].
Experimental Protocols for Assessing Toxicity and Biocompatibility
Rigorous and standardized assessment is fundamental to nanoscale biological interactions research. The following protocols provide a framework for evaluating the potential toxicity and biocompatibility of engineered nanomaterials.
In Vitro Cytocompatibility and Cellular Response Assays
Objective: To evaluate the impact of nanomaterials on cell viability, morphology, and function in a controlled environment.
Detailed Protocol:
- Cell Culture: Select relevant cell lines (e.g., human gingival fibroblasts (HGF) for dental implants [70], A549 lung epithelial cells for inhaled particles [69] [72], or HepG2 for liver toxicity [72]). Culture cells in appropriate media (e.g., Dulbecco’s Modified Eagle's Medium supplemented with 10% fetal bovine serum and 1% penicillin) at 37°C in a 5% CO₂ atmosphere [70].
- Nanomaterial Preparation: Disperse the nanomaterials in a sterile physiological buffer or culture medium. Sonication may be required to break up aggregates. Serial dilutions should be prepared to test a range of concentrations.
- Exposure and Incubation: Seed cells in multi-well plates and allow them to adhere. Introduce the nanomaterial suspensions to the cells at the desired concentrations. Incubate for a predetermined time (e.g., 24, 48, or 72 hours).
- Assessment of Cytotoxicity:
- Metabolic Activity Assays: Perform MTT or MTS assays. These measure the reduction of tetrazolium salts by metabolically active cells, providing an indicator of cell viability.
- Membrane Integrity Assays: Use Lactate Dehydrogenase (LDH) release assays. Damaged cells release LDH into the culture supernatant, which is quantified as a marker of cytotoxicity.
- Analysis of Morphology and Adhesion:
- Fluorescence Microscopy: After exposure, fix cells with 4% paraformaldehyde for 15 minutes, permeabilize with 0.5% Triton X-100, and block with 2% Bovine Serum Albumin (BSA) [70].
- Stain for focal adhesions with anti-vinculin antibodies (1:50 dilution) and for actin cytoskeleton with phalloidin. Mount with DAPI to visualize nuclei [70].
- Image using a fluorescence microscope (e.g., Nikon Eclipse Ni-U) to assess changes in cell spreading, cytoskeletal organization, and focal adhesion points [70].
- Scratch Assay for Migration: Create a uniform "wound" in a confluent cell monolayer using a pipette tip. Wash away debris and add fresh medium containing sub-toxic concentrations of the nanomaterial. Monitor and image cell migration into the scratched area over 24-48 hours to evaluate the impact on cell motility [70].
In Vivo Biodistribution and Systemic Toxicity
Objective: To determine the absorption, distribution, metabolism, and excretion (ADME) of nanomaterials and identify target organs for toxicity in a whole-organism model.
Detailed Protocol:
- Animal Model Selection: Typically, rodents (mice or rats) are used. The choice should consider the intended route of human exposure (e.g., intravenous for systemic delivery, inhalation for respiratory exposure, oral for dietary).
- Dosing and Administration: Administer a single or repeated doses of the nanomaterial at concentrations selected based on in vitro data and anticipated human exposure. Control groups should receive the vehicle alone.
- Tissue Collection and Analysis:
- At predetermined time points post-administration, euthanize animals and collect key organs (e.g., liver, spleen, kidneys, lungs, brain, and blood).
- Quantitative Analysis: Use techniques like Inductively Coupled Plasma Mass Spectrometry (ICP-MS) to precisely quantify the elemental composition of the nanomaterial in each tissue, providing biodistribution data [73].
- Histopathological Examination: Fix tissue samples in formalin, embed in paraffin, section, and stain with Hematoxylin and Eosin (H&E). A pathologist should examine the slides in a blinded manner to score for lesions, inflammation, necrosis, or other signs of toxicity.
- Blood Analysis: Collect blood samples to assess systemic hematological and clinical chemistry parameters (e.g., liver enzymes ALT/AST, markers of kidney function like creatinine) to evaluate overall organ health.
The Scientist's Toolkit: Essential Reagents and Materials
This table catalogues key reagents and technologies central to research in nanomaterial toxicity and surface modification.
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Specific Examples |
|---|---|---|
| Polyethylene Glycol (PEG) | "Stealth" coating to reduce protein adsorption and prolong nanoparticle circulation half-life [4]. | PEGylated liposomes (Doxil) [4]. |
| Targeting Ligands | Active targeting to specific cell types via receptor-ligand interactions, enhancing cellular uptake and reducing off-target effects [4]. | Antibodies, peptides (e.g., RGD), small molecules (e.g., folic acid) [4]. |
| Chitosan | Biocompatible polymer that imparts a positive charge, enhancing mucoadhesion and residence time for drug delivery [4]. | Chitosan-coated nanoparticles for oral or mucosal delivery [4]. |
| Metal Ions for Doping | Impart osteogenic and antibacterial properties to implant surfaces [71]. | Zinc (Zn), Magnesium (Mg), Copper (Cu) ions [71]. |
| High-Focus Laser Scanning (HFLS) | Precision surface patterning of biomaterials to control wettability, cell response, and drug release [70]. | Creating 'Line' (hydrophilic) and 'Grid' (hydrophobic) patterns on polystyrene [70]. |
| Cell Lines for Toxicity Screening | In vitro models for assessing cytotoxicity, genotoxicity, and cellular uptake mechanisms [72]. | A549 (lung epithelial), HepG2 (liver), HeLa (cervical), U251 (glioblastoma) [72]. |
| Antibodies for Cytokine Analysis | Detection of inflammatory responses triggered by nanomaterials via Western Blot or ELISA [70]. | Antibodies against M1 macrophage cytokines (e.g., TNF-α, IL-6) [70]. |
Addressing the dual challenges of toxicity and biocompatibility requires a foundational understanding of nanoscale biological interactions. The physicochemical properties of nanomaterials—size, shape, charge, and surface chemistry—are decisive factors in their biological fate and must be strategically engineered through material selection and surface modification. Techniques ranging from PEGylation and active targeting for drug delivery carriers to ion doping and laser patterning for implants provide a powerful toolkit for enhancing biocompatibility. The integration of robust experimental protocols, including in vitro cytocompatibility assays and in vivo biodistribution studies, is essential for validating the safety of these advanced materials. As the field progresses, future research must focus on multi-functional designs, long-term fate studies, and the development of adaptive regulatory frameworks. By combining scientific innovation with rigorous safety assessment, the nanotechnology community can fully realize the transformative potential of nanomaterials in medicine while safeguarding human health.
The efficacy of a therapeutic agent is fundamentally governed by its journey through the biological system—its pharmacokinetics (PK) and its subsequent distribution (biodistribution). Within the broader thesis on nanoscale biological interactions research, optimizing these parameters is paramount for translating nanomedicine from laboratory innovation to clinical reality. Conventional drug delivery systems are often hampered by rapid clearance, off-target distribution, and uncontrolled release kinetics, leading to suboptimal efficacy and potential toxicity. The advent of nanotechnology has provided unprecedented tools to engineer precision drug delivery systems that navigate the complex biological milieu [74] [75].
Nanoparticle (NP)-mediated drug delivery offers distinct advantages over conventional systems, including enhanced drug solubility, stability, and the potential for targeted delivery. The core challenge lies in engineering these nanocarriers to overcome a series of systemic, microenvironmental, and cellular barriers. This requires a deep, fundamental understanding of the interactions at the interface of nanomaterials and biological systems [76] [77]. By leveraging this knowledge, researchers can design NPs with prolonged circulation times, achieve controlled drug release at the target site, and significantly improve the therapeutic index, thereby laying the groundwork for more effective and personalized medical treatments [75].
Engineering Nanoparticles for Prolonged Circulation
A primary obstacle to effective drug delivery is the rapid clearance of intravenously injected nanoparticles by the body's immune system, particularly the reticuloendothelial system (RES). Overcoming this requires strategic surface and structural engineering.
Stealth Properties via Surface Functionalization
The most established method for conferring "stealth" properties to nanoparticles is the surface functionalization with hydrophilic polymers. Polyethylene glycol (PEG) is the gold standard in this domain. PEGylation creates a hydrated layer on the nanoparticle surface that sterically hinders the adsorption of opsonins—proteins that mark foreign particles for phagocytosis [78] [79]. This process effectively camouflages the nanoparticles, allowing them to evade immune detection.
- Mechanism: The polymer chain's flexibility and hydrophilicity form a protective barrier, reducing protein fouling.
- Impact: PEGylation significantly extends the circulation half-life of nanoparticles from minutes to hours, providing a greater opportunity for the particles to reach their intended target through mechanisms like the Enhanced Permeability and Retention (EPR) effect in tumor tissues [78] [75].
Biomimetic Surface Modifications
Inspired by nature and pathogenic strategies, advanced surface modifications are being explored:
- Self-markers: Engineering nanoparticles to display CD47 "self" markers, which signal "do not eat me" to macrophages.
- Cellular membrane coating: Coating nanoparticles with membranes derived from red blood cells or leukocytes to create a biomimetic surface that the body recognizes as its own, further prolonging circulation time [79].
Size and Surface Charge Optimization
The physicochemical properties of nanoparticles are critical determinants of their biological fate.
- Size: Nanoparticles smaller than 10 nm are rapidly cleared by renal filtration. For systemic delivery, particles larger than 10 nm are preferred. Optimal sizes for leveraging the EPR effect in tumors typically range from 10-100 nm, allowing for extravasation through leaky vasculature while avoiding rapid RES clearance [78].
- Surface Charge: Cationic surfaces tend to promote opsonization and nonspecific cellular uptake. Therefore, neutral or slightly negative surface charges are generally favored for prolonged circulation [75].
Table 1: Key Parameters for Engineering Prolonged Circulation
| Engineering Parameter | Optimal Characteristic | Biological Impact |
|---|---|---|
| Surface Coating | PEGylation or biomimetic membranes | Reduces opsonization, evades RES clearance |
| Hydrodynamic Size | 10 - 100 nm | Avoids renal filtration, enables EPR effect |
| Surface Charge | Neutral or slightly negative | Minimizes non-specific interactions with cells/proteins |
| Shape | Spherical, high curvature | Influences flow dynamics and cell uptake |
Strategies for Controlled Drug Release
Controlled release is essential for maintaining drug concentrations within the therapeutic window and minimizing dosing frequency. The large surface-area-to-volume ratio of nanocarriers presents a unique challenge for controlling release kinetics, which is addressed through various engineered mechanisms [78].
Core Drug Release Mechanisms
Drug release from nanocarriers can be governed by several mechanisms, often working in concert:
- Diffusion-Controlled Release: In reservoir-type systems (a core-shell structure), the drug diffuses through an intact polymeric membrane. In matrix-type systems (drug dispersed in a polymer matrix), the drug diffuses through the polymer network, often characterized by an initial burst release followed by a slower phase [78].
- Solvent-Controlled Release: This includes osmosis-controlled release (where water influx builds osmotic pressure to push drug out) and swelling-controlled release (where water uptake causes the polymer matrix to swell, increasing mesh size and enabling drug diffusion) [78].
- Degradation-Controlled Release: Carriers made from biodegradable polymers (e.g., PLGA, polyesters) release their payload as the polymer backbone undergoes hydrolysis or enzymatic cleavage. The rate of degradation can be tuned by the polymer's crystallinity and molecular weight [78].
Stimuli-Responsive Release Systems
For precision targeting, "smart" nanoparticles are designed to release their payload in response to specific internal or external stimuli:
- pH-Sensitive Systems: Exploit the acidic microenvironment of tumors (pH ~6.5-6.9) or endosomes/lysosomes (pH 4.5-5.5) using polymers that undergo hydrolysis or conformational changes at low pH [75].
- Enzyme-Responsive Systems: Utilize enzymes overexpressed in disease sites (e.g., matrix metalloproteinases in tumors) to cleave a labile linker or degrade the nanocarrier shell [75].
- Redox-Responsive Systems: Leverage the high redox potential difference between the extracellular space and the intracellular environment (high glutathione levels) to trigger drug release via cleavage of disulfide bonds [75].
Table 2: Controlled Drug Release Mechanisms and Their Applications
| Release Mechanism | Description | Common Materials |
|---|---|---|
| Diffusion-Controlled | Drug diffusion through a polymer membrane or matrix. | PLGA, Polycaprolactone (PCL), Lipids |
| Degradation-Controlled | Release coupled to polymer backbone hydrolysis. | PLGA, Polyanhydrides, Poly(amino acids) |
| pH-Responsive | Drug release triggered by a drop in pH. | Poly(methacrylic acid), Poly(histidine), Acetal-based linkers |
| Enzyme-Responsive | Enzyme-cleavable linkers or matrices release the drug. | Peptide-crosslinked hydrogels, MMP-sensitive coatings |
Computational Modeling for Prediction and Optimization
Computational modeling has emerged as a powerful tool to predict and optimize the biodistribution and pharmacokinetics of nanoparticles, reducing reliance on extensive in vivo experimentation [76] [80].
Compartmental Modeling
Compartmental models provide a simplified yet effective framework for simulating NP dynamics in vivo. A typical model for targeted drug delivery may include compartments for the administration site, off-target sites, target cell vicinity, target cell interior, and excreta. The model uses a system of differential equations with rate constants describing the reversible transport between these compartments.
- Application: This approach enables the estimation of delivery efficiency (ratio of NPs reaching the target cell interior to the total administered dose) and identifies kinetic bottlenecks through sensitivity analysis [76].
- Accessibility: Web applications like the CompSafeNano cloud platform provide user-friendly interfaces for researchers to conduct such in silico experiments and optimize delivery strategies [76].
Physiologically Based Pharmacokinetic (PBPK) Modeling
PBPK modeling offers a more detailed, mechanistic framework that describes the absorption, distribution, metabolism, and excretion (ADME) of a drug based on its physicochemical properties and physiological parameters.
- Regulatory Use: PBPK modeling is increasingly used in regulatory submissions to support dose selection, particularly for specific populations like pediatrics, and to provide a mechanistic understanding of a drug's fate [81] [80].
- Case Study: A PBPK model was developed for the hemophilia A drug ALTUVIIIO, a recombinant FVIII fusion protein. The model, which incorporated FcRn recycling pathways, was validated using data from a similar product (ELOCTATE) and accurately predicted PK parameters (C~max~ and AUC) in both adults and children, with prediction errors within ±25%. This supported dose selection for pediatric patients [81].
Experimental Protocols for Characterization
Rigorous characterization is essential to validate the performance of engineered nanoparticles. The following protocols outline key experiments for assessing circulation time and drug release.
Protocol: Microfluidic Spray Deposition for AFM Characterization
This protocol, adapted from studies on protein condensates, is ideal for preparing nanoparticle samples for high-resolution imaging while preserving their solution-state properties [82].
Goal: To deposit nanoparticles onto a surface for Atomic Force Microscopy (AFM) with minimal structural disruption. Materials:
- Microfluidic spray deposition device
- Nanoparticle suspension in appropriate buffer
- Hydrophobic substrate (e.g., zinc selenide crystals)
- Atomic Force Microscope
Method:
- Load Sample: Introduce the nanoparticle suspension into the microfluidic device.
- Generate Droplets: The device precisely generates picolitre-volume droplets.
- Ultra-fast Drying: Direct droplets onto the hydrophobic substrate. The millisecond-timescale drying minimizes time for surface-induced conformational changes or aggregation.
- Image via AFM: Use AFM to obtain nanometre-resolution maps of the morphological and mechanical properties of the deposited nanoparticles.
Importance: Compared to manual deposition (which can cause aggregation and remove the dilute phase), this method preserves the native morphology, heterogeneity, and circularity of nanoparticles, enabling accurate characterization [82].
Protocol: In Vitro Drug Release Kinetics
Goal: To quantify the rate and extent of drug release from nanoparticles under simulated physiological conditions. Materials:
- Dialysis bags or Float-A-Lyzer devices (appropriate MWCO)
- Release medium (e.g., PBS at pH 7.4 and pH 5.5 for pH-sensitivity)
- Thermostated shaking water bath
- HPLC system or other analytical instrumentation for drug quantification
Method:
- Preparation: Place a known volume of nanoparticle suspension into a dialysis device. Ensure the molecular weight cut-off (MWCO) of the membrane is smaller than the nanoparticles but allows free diffusion of the released drug.
- Incubation: Immerse the dialysis device in a large volume of release medium to maintain sink conditions.
- Sampling: At predetermined time intervals, withdraw and replace an aliquot of the release medium.
- Analysis: Quantify the drug concentration in each aliquot using HPLC or UV-Vis spectroscopy.
- Modeling: Fit the cumulative release data to mathematical models (e.g., Zero-order, First-order, Korsmeyer-Peppas) to determine the dominant release mechanism [78].
Visualization of Pathways and Workflows
The following diagrams illustrate the core concepts of nanoparticle journey and drug release mechanisms.
Nanoparticle Journey and Fate In Vivo
Diagram Title: NP Journey from Injection to Action
Controlled Drug Release Mechanisms
Diagram Title: Triggers for Controlled Drug Release
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Nanoparticle PK/BD Research
| Reagent / Material | Function & Application |
|---|---|
| PEGylated Lipids (e.g., DSPE-PEG) | Core component for forming stealth lipid nanoparticles or liposomes; confers prolonged circulation. |
| Biodegradable Polymers (e.g., PLGA) | Forms the matrix or shell of nanoparticles for sustained, degradation-controlled drug release. |
| Targeting Ligands (e.g., Peptides, Antibodies, Transferrin) | Conjugated to nanoparticle surface for active targeting to specific cells or tissues (e.g., receptors overexpressed in tumors). |
| pH-Sensitive Polymers (e.g., Poly(methacrylic acid)) | Enables drug release in response to the acidic microenvironment of endosomes or pathological tissues. |
| Microfluidic Devices | Provides precise control over nanoparticle synthesis, leading to homogeneous size distribution and improved reproducibility. |
| Atomic Force Microscopy (AFM) | Enables high-resolution, nanoscale characterization of nanoparticle morphology and mechanical properties. |
| Compartmental/PBPK Modeling Software (e.g., CompSafeNano, Simcyp) | In silico platforms for predicting and optimizing nanoparticle biodistribution and pharmacokinetics. |
The optimization of biodistribution and pharmacokinetics through nanoparticle engineering represents a cornerstone of modern nanoscale biological interactions research. By systematically designing nanocarriers with stealth surfaces, controlled release mechanisms, and targeting capabilities, researchers can significantly enhance therapeutic efficacy and safety. The integration of advanced computational modeling with rigorous experimental characterization creates a powerful feedback loop for the rational design of next-generation nanomedicines. As this field evolves, the convergence of materials science, computational biology, and a deep understanding of biological interfaces will continue to drive the development of precision therapeutics that can dynamically interact with the complex human body, ultimately fulfilling the promise of personalized medicine.
The successful integration of nanoparticles (NPs) into biomedical applications represents a frontier in diagnostic and therapeutic technologies, yet this potential is critically dependent on controlling interactions at the bio-nano interface. When introduced into biological systems, nanoparticles immediately encounter a complex milieu of proteins, lipids, and other biomolecules that rapidly adsorb to their surfaces, forming a dynamic "protein corona" that defines their biological identity [2]. This corona formation often leads to two fundamental challenges: biofouling, the nonspecific accumulation of biological material on the nanoparticle surface, and aggregation, the clumping of nanoparticles, both of which deteriorate functionality and compromise therapeutic efficacy [18] [2]. Biofouling can mask targeting ligands, alter biodistribution, and trigger immune clearance, while aggregation reduces cellular uptake and uniformity of treatment response. The ensuing biological response—primarily opsonization and subsequent clearance by the mononuclear phagocyte system—results in less than 1% of administered nanoparticles typically reaching their intended target site [18]. This review examines advanced surface chemistry strategies designed to overcome these challenges, focusing on molecular-level interventions that preserve nanoparticle functionality within biological environments, thereby bridging the gap between nanomaterial synthesis and clinical application.
Surface Modification Strategies: Principles and Mechanisms
Biomimetic Surface Engineering
Biomimetic approaches leverage evolutionary-optimized biological structures to create stealth nanoparticles. The most advanced platform in this category utilizes cell membrane-coated nanoparticles, where synthetic nanoparticulate cores are functionalized with naturally derived cell membrane layers [18]. This top-down strategy transfers the complete repertoire of source cell surface proteins, receptors, and lipids to the nanoparticle, enabling complex biological interactions impossible to replicate with synthetic chemistry alone. Red blood cell (RBC) membrane cloaking exploits the presence of CD47 "self-marker" proteins, which inhibit macrophage uptake via interaction with signal-regulatory protein α on phagocytic cells, significantly extending systemic circulation half-life [18]. Similarly, coatings derived from platelets capitalize on their inherent affinity for certain pathogens and injured vasculature, enabling targeted drug delivery to bacterial infections or atherosclerotic lesions [18]. Cancer cell membranes facilitate homotypic targeting, where nanoparticles preferentially bind to their source cell type, a mechanism that persists even in the presence of competing heterologous tumors [18].
Polymer-Based Passivation Layers
Polymer coatings create a physical and energetic barrier against nonspecific biomolecule adsorption. Polyethylene glycol (PEG) remains the gold standard for reducing unwanted biological interactions due to its ability to form a hydrated layer that sterically hinders protein adsorption [18]. The effectiveness of PEG stems from its chain length, surface density, and conformation, which create a dynamic "cloud" of hydrated polymer chains that resist biomolecular approach and binding. Beyond PEG, advanced polymer architectures include highly hydrated hydrogels that provide a physical and free-energy barrier to foulant adhesion, and zwitterionic polymers that create electrostatically neutral surfaces with superior protein resistance compared to PEG [83]. These fouling-resistant coatings work primarily by forming a tightly bound water layer that acts as a physical barrier, preventing direct contact between biomolecules and the nanoparticle surface.
Slippery Liquid-Infused and Solid-Like Coatings
An innovative approach to biofouling prevention involves creating surfaces that are physically difficult for organisms to adhere to. Liquid-infused surfaces (LIS) trap a liquid lubricant within a textured nanoparticle coating, creating an exceptionally smooth interface that minimizes adhesion points for proteins and cells [84]. A recent advancement addresses the lubricant loss problem through nanohesive-based "solid-like" slippery coatings (SSC). These utilize amino-functionalized SiO₂ nanoparticles as adhesives to capture carboxy-terminated silicone oil within an epoxy resin matrix [84]. The collective effects of electrostatic interactions, hydrogen bonds, and van der Waals forces between nanoparticles and silicone oil, combined with epoxy resin encapsulation, ensure remarkable lubricant retention and mechanical stability under physiological flow conditions [84].
Bioactive Nanocoatings
Bioactive approaches employ nanomaterials with inherent antimicrobial properties, primarily metal and metal oxide nanoparticles such as silver (Ag), titanium dioxide (TiO₂), zinc oxide (ZnO), and copper oxide (CuO) [83] [85] [86]. These materials prevent biofouling through multiple mechanisms, including photocatalytic production of reactive oxygen species (ROS), metal ion release, and direct membrane disruption [83]. TiO₂ and ZnO nanoparticles, for instance, upon exposure to light, generate ROS like hydroxyl radicals and superoxides that oxidize and degrade organic foulants [83]. Hybrid nanocomposites combining organic polymers with inorganic nanoparticles merge the characteristics of both materials, creating synergistic antifouling activity while potentially reducing toxicity compared to conventional biocidal coatings [83].
Table 1: Comparison of Surface Modification Strategies for Nanoparticles
| Strategy | Key Materials | Primary Mechanism | Advantages | Limitations |
|---|---|---|---|---|
| Biomimetic Coatings | RBC, platelet, cancer cell membranes | CD47 signaling for immune evasion; Homotypic targeting | Multifunctional; Biologically optimized | Complex preparation; Batch variability |
| Polymer Passivation | PEG, zwitterionic polymers, hydrogels | Steric hindrance; Hydration layer formation | Well-established; Tunable chemistry | Potential immunogenicity with PEG |
| Slippery Coatings | SiO₂ nanoparticles, silicone oils, epoxy resins | Low interfacial energy; Liquid interface | Broad-spectrum against proteins/cells | Potential lubricant depletion over time |
| Bioactive Nanocoatings | Ag, TiO₂, ZnO, CuO nanoparticles | ROS generation; Ion release; Contact killing | Potent antimicrobial activity | Potential cytotoxicity to host cells |
Experimental Protocols and Methodologies
Biomolecule-Mediated Synthesis of Bioactive Nanoparticles
Protocol: Synthesis of Surface-Functionalized Gold and Silver Nanoparticles [2]
This method utilizes biological molecules as reducing and stabilizing agents to create nanoparticles with inherent surface coronas that dictate biological interactions.
Materials:
- Tetrachloroauric acid (HAuCl₄) or silver nitrate (AgNO₃)
- Reducing/Stabilizing agents: Tyrosine (Tyr), Tryptophan (Trp), Isonicotinylhydrazide (INH), Epigallocatechin gallate (EGCG), Curcumin (Cur)
- Potassium hydroxide (KOH)
- Ultrapure water (18.2 MΩ·cm resistivity)
Procedure:
- Prepare 100 mL of aqueous solution containing 1 mM KOH and 0.1 mM of the chosen biomolecule (Tyr, Trp, INH, EGCG, or Cur).
- Heat the solution with constant stirring.
- Add 0.1 mM of [AuCl₄]⁻ or Ag⁺ ions to the heated solution.
- Continue heating until the solution volume reduces to approximately 50 mL, thereby concentrating the nanoparticles.
- Characterize the nanoparticles using UV-Vis spectrophotometry (Surface Plasmon Resonance), FTIR (surface functional groups), TEM (size and morphology), and DLS/Zeta potential (hydrodynamic size and surface charge).
Key Applications: The resulting nanoparticles (denoted as AuTyr, AuTrp, etc., based on the reducing agent) exhibit surface corona with free radical scavenging capacity, enzyme-like activities, and limited cytotoxicity, making them suitable for biomedical applications where controlled biointeractions are critical [2].
Fabrication of Solid-Like Slippery Coatings (SSC)
Protocol: Nanohesive-Based Coating for Ultra-Stable Anti-Biofouling [84]
This method creates a solid-like slippery coating through strong molecular interactions between functionalized nanoparticles and lubricants, providing exceptional resistance to protein adhesion, cell attachment, and thrombus formation under dynamic flow conditions.
Materials:
- Amino-functionalized SiO₂ nanoparticles
- Carboxyl-terminated silicone oil
- Epoxy resin
- Suitable solvent (e.g., ethanol)
- Atomizing spray equipment
Procedure:
- Hydrolyze a silane coupling agent to facilitate functionalization.
- Condense the hydrolyzed agent with SiO₂ nanoparticles to create amino-functionalized surfaces.
- Mix the aminated nanoparticles with carboxyl-terminated silicone oil, leveraging strong electrostatic interactions for stable capture.
- Cross-link the oil-containing nanoparticles with epoxy resin to form a translucent SSC solution.
- Uniformly spray the solution onto the target substrate (e.g., medical catheter).
- Allow the coating to cure spontaneously at room temperature.
Performance Validation: The resulting coating maintains exceptional anti-fouling (>71%) and anti-thrombotic (>67%) capabilities under low shear rate (250 s⁻¹, 30 days) and high shear rate (1750 s⁻¹, 7 days) blood flow conditions, significantly outperforming conventional liquid-infused surfaces [84].
Assessing Antifouling Performance: Radical Scavenging Capacity
Protocol: Modified ABTS Assay for Evaluating Antioxidant Surface Properties [2]
This in vitro assay evaluates the radical scavenging capacity (RSC) of nanoparticles, which correlates with their ability to mitigate oxidative stress and potentially reduce biofouling.
Materials:
- 7.4 mM ABTS (2,2'-azino-bis(3-ethylbenzothiazoline-6-sulphonic acid))
- 2.45 mM potassium persulfate (K₂S₂O₈)
- Ethanol
- Nanoparticle suspensions at varying concentrations (0.1-1.2 ppm)
- UV-Vis spectrophotometer
Procedure:
- Generate ABTS radical cations (ABTS·⁺) by reacting ABTS solution with potassium persulfate.
- Incubate the mixture in the dark for 16 hours to allow complete radical formation.
- Dilute the stock ABTS·⁺ solution with ethanol to achieve an absorbance of 0.67 ± 0.02 at 734 nm.
- React different concentrations of nanoparticles with the diluted ABTS·⁺ solution.
- Measure the decrease in absorbance at 734 nm after a fixed time period.
- Calculate the percentage radical scavenging capacity (%RSC) using the formula:
%RSC = [(A_c - A_s)/A_c] × 100where Ac is the absorbance of the control and As is the absorbance with nanoparticles.
Interpretation: Higher %RSC values indicate stronger antioxidant properties, which may contribute to antifouling performance through neutralization of reactive oxygen species involved in biofilm formation and material degradation [2].
Table 2: Essential Research Reagent Solutions for Antifouling Nanomaterial Development
| Reagent Category | Specific Examples | Function in Research |
|---|---|---|
| Reducing/Stabilizing Agents | Tyrosine, Tryptophan, EGCG, Curcumin | Biomolecule-mediated NP synthesis; Imparts bioactive surface corona |
| Functionalized Nanoparticles | Amino-functionalized SiO₂, CuO NPs | Core coating component; Provides structural matrix and antimicrobial activity |
| Polymer Matrices | Epoxy resin, Polyamide 6, Polyethylene glycol (PEG) | Encapsulates active components; Provides mechanical stability and steric hindrance |
| Lubricants | Carboxyl-terminated silicone oil | Creates slippery interface in SSC; Prevents biological adhesion |
| Characterization Reagents | ABTS, Potassium Persulfate | Evaluates antioxidant and radical scavenging properties of surfaces |
Strategic Framework and Implementation Pathways
The following diagram illustrates the logical decision-making process for selecting appropriate surface chemistry strategies based on the intended application and primary biofouling challenges.
Surface Chemistry Selection Framework
The experimental workflow for developing and validating antifouling surface coatings involves systematic synthesis, characterization, and performance testing, as visualized below.
Antifouling Coating Development Workflow
The prevention of biofouling and aggregation through advanced surface chemistry represents a cornerstone for realizing the full potential of nanomedicine. As research progresses, several emerging trends are shaping the next generation of antifouling strategies. Dual-functional coatings that integrate multiple mechanisms—such as combining physicochemical repulsion with contact-active biocides—offer synergistic protection against diverse fouling challenges [87]. Stimuli-responsive "smart" coatings that activate antimicrobial properties only in response to specific triggers (pH changes, enzymes, or pathogens) minimize off-target effects and enhance biocompatibility [85] [87]. Furthermore, the integration of Safe and Sustainable by Design (SSbD) principles ensures that new nanomaterials are developed with thorough consideration of their environmental impact and biological safety from the earliest stages [86]. As these advanced surface engineering strategies mature, they promise to overcome the critical biointerface challenges that have limited the clinical translation of nanotherapeutics, ultimately enabling more precise, effective, and safe medical interventions through controlled nanoscale biological interactions.
The translation of nanoscale biological research from a laboratory setting to industrial-scale manufacturing presents a critical paradox: the very physicochemical properties that enable novel functionality—such as particle size, surface chemistry, and shape—are often the most challenging to control and reproduce at scale. Engineered nanomaterials (ENMs) are defined as materials with at least one dimension between 1-100 nm, a scale that grants unique properties but introduces significant manufacturing complexities [88]. Within biomedical applications, this challenge is amplified by the stringent requirements for biocompatibility, batch-to-batch consistency, and precise characterization in regulated medical products [59] [88]. The fundamental thesis of modern nanoscale research must therefore extend beyond discovering new biological interactions to encompass the entire product lifecycle, ensuring that revolutionary laboratory findings can be feasibly, safely, and economically scaled for widespread clinical impact. This whitepaper examines the core technical hurdles in nanomanufacturing and provides a framework for balancing performance with production feasibility.
Critical Manufacturing Bottlenecks and Technical Hurdles
The Characterization and Quality Control Challenge
A primary bottleneck in scaling nanomaterial production is the lack of robust, standardized characterization methods. The functionality and safety of nanomaterials are dictated by a complex set of physicochemical properties, yet reliably measuring these properties across different production batches and laboratories remains difficult [88].
Table 1: Key Nanomaterial Properties and Associated Characterization Challenges
| Property | Impact on Performance & Safety | Scalability Challenge |
|---|---|---|
| Particle Size & Distribution | Determines biological distribution, clearance, and targeting efficiency [59] [89]. | Lack of certified reference materials (CRMs) for instrument calibration across labs [88]. |
| Surface Chemistry & Charge | Influences protein corona formation, cellular uptake, and potential cytotoxicity [89]. | Difficulty in achieving consistent surface modification and functionalization at scale [59]. |
| Shape & Morphology | Affects flow properties, immune system recognition, and biological barrier penetration [89]. | Reproducible synthesis often yields heterogeneous shapes; characterization is time-consuming [88]. |
| Agglomeration/Aggregation State | Alters effective particle size, bioavailability, and biological response [90]. | Sensitive to synthesis and storage conditions; difficult to control in large-volume batches [88]. |
The availability of nanoscale reference materials (RMs) and certified reference materials (CRMs) is critical for validating characterization methods and ensuring data comparability. Their limited availability for properties beyond basic particle size, such as surface chemistry or particle number concentration, represents a major gap [88].
The Synthesis and Process Control Hurdle
The transition from gram-scale laboratory synthesis to kilogram-scale industrial production is fraught with difficulties. Synthesis methods are broadly classified as top-down (breaking down larger materials) or bottom-up (assembling from atomic/molecular units), each with scalability limitations [59].
Top-down approaches, such as milling and lithography, can introduce surface defects and impurities, while bottom-up approaches, like chemical vapor deposition and sol-gel processes, require exquisite control over reaction conditions to maintain uniformity [59]. In both cases, minor variations in parameters such as temperature, pressure, or mixing dynamics can lead to significant variances in the critical quality attributes (CQAs) of the final product. For complex nanoparticles like lipid nanoparticles (LNPs) used in mRNA delivery, the preparation process directly influences the particle size and dispersion, which in turn affects the protein corona that forms in biological environments and ultimately the nanoparticle's bio-distribution and targeting efficiency [89]. Implementing Quality-by-Design (QbD) principles and Process Analytical Technologies (PAT) is essential for real-time monitoring and control of these CQAs during manufacturing, but their application in nanomedicine production is not yet widespread [59].
The Nano-Bio Interaction and Regulatory Conundrum
Perhaps the most significant challenge lies in the dynamic interface between the nanomaterial and the biological system, known as nano-bio interactions. Upon introduction to a physiological environment, nanomedicines are immediately coated by proteins, forming a "protein corona" that defines their biological identity [89]. This corona, comprising a "soft" and "hard" layer, is influenced by the nanoparticle's original physicochemical properties (size, shape, surface charge, elasticity) and environmental factors (pH, temperature) [89]. The corona can mask targeting ligands, intended for specific cell recognition, leading to off-target effects and dramatically reduced delivery efficiency—often to less than 1% of the administered dose reaching the intended site [89]. This unpredictable interaction poses a profound challenge for regulatory approval. The global regulatory landscape is further complicated by differing definitions of what constitutes a nanomaterial, varying between jurisdictions like the EU and USA, which creates uncertainty for developers aiming for international markets [88].
Quantitative Frameworks for Hazard and Risk Assessment
The large and growing number of engineered nanomaterials makes it impractical to conduct exhaustive toxicological testing for each one. A promising approach to this challenge is the development of quantitative frameworks for grouping ENMs based on hazard potency. One such framework utilizes benchmark dose (BMD) modeling of dose-response data from rodent studies (e.g., pulmonary inflammation) to estimate the potency of different materials [90]. The deposited particle mass dose per gram of lung is used as a normalized metric. Hierarchical clustering is then applied to group materials with similar potency, while random forest models can identify the key physicochemical properties predictive of the hazard group [90]. This methodology supports the derivation of categorical occupational exposure limits (OELs) or occupational exposure bands (OEBs), providing a more efficient and data-driven path for risk assessment and management during manufacturing, especially for new materials with limited toxicity data [90].
Table 2: Quantitative Data from Nanomaterial Research and Manufacturing
| Material/System | Key Parameter Measured | Quantitative Finding | Implication for Scalability | ||
|---|---|---|---|---|---|
| PEGylated Gold Nanoparticles | Accelerated Blood Clearance (ABC) Phenomenon [33] | Dose concentration <1 mg/kg induced strong ABC; >2 mg/kg suppressed it [33]. | Dosage and dosing intervals must be carefully controlled in production to avoid immune priming. | ||
| Al-Zn-Mg-Cu Alloys (Nanoprecipitates) | Precipitate Size & Volume Fraction [91] | Average long-axis diameter ~5 nm; volume fraction varies from 2.73% to 5.21% with composition [91]. | Demonstrates how nanoscale features dictate macroscopic material properties (strength), requiring precise process control. | ||
| High-Order Lithography Correction | Overlay Error [92] | Model reduced overlay to | \mu | + 3\sigma < 1 nm in simulation [92]. | High-precision nanofabrication requires sophisticated modeling and control, increasing process complexity and cost. |
| mRNA Lipid Nanoparticles (LNPs) | Targeted Delivery Efficiency [89] | Typically <1% of administered dose reaches the target site in vivo [89]. | Highlights a major efficacy barrier; scaling production of a fundamentally inefficient design is economically and clinically challenging. |
Experimental Protocols for Critical Nano-Bio Characterization
Protocol for Analyzing Protein Corona Formation
Understanding the protein corona is essential for predicting nanomedicine behavior in vivo. The following protocol details a method for isolating and analyzing the hard corona.
- Nanoparticle Preparation: Synthesize and characterize the nanoparticles for size, PDI, and zeta potential. Use sterile conditions.
- Incubation with Biological Fluid: Incubate a standardized amount of nanoparticles (e.g., 1 mg/mL) with relevant biological fluid (e.g., human plasma or serum) at a specific ratio (e.g., 1:1 v/v) for 1 hour at 37°C under gentle agitation.
- Isolation of Corona-Coated Particles:
- Ultracentrifugation: Subject the mixture to ultracentrifugation (e.g., 100,000 × g for 1 hour) to pellet the nanoparticles with their hard corona.
- Washing: Carefully remove the supernatant and gently wash the pellet with a neutral buffer (e.g., PBS) to remove loosely associated proteins (soft corona). Repeat centrifugation.
- Size-Exclusion Chromatography (SEC): As an alternative or complementary method, use SEC to separate corona-coated nanoparticles from unbound proteins.
- Protein Elution and Digestion: Re-suspend the hard corona-nanoparticle pellet in a strong denaturing buffer (e.g., SDS-containing buffer) or an organic solvent to dissociate the proteins. Precipitate the nanoparticles via centrifugation. Recover the protein-containing supernatant and digest the proteins using an enzyme like trypsin.
- Analysis:
- Mass Spectrometry (LC-MS/MS): Analyze the digested peptides via liquid chromatography coupled with tandem mass spectrometry to identify the individual protein components of the corona.
- SDS-PAGE: Use sodium dodecyl sulfate–polyacrylamide gel electrophoresis for a quick visual profile of the total protein composition and molecular weights.
This protocol allows researchers to correlate the nanoparticle's original properties with the composition of its biological identity, providing critical data for designing scalable formulations with predictable in vivo behavior [89].
Protocol for Assessing Cytocompatibility and Immunogenic Response
Before scaling production, a rigorous safety profile is necessary.
- Cell Culture: Select relevant cell lines (e.g., hepatocytes, immune cells, or primary cell cultures). Culture cells under standard conditions.
- Nanoparticle Exposure: Expose cells to a concentration range of the nanomaterial (e.g., 0-100 µg/mL) for 24-72 hours. Include negative and positive controls.
- Viability Assay: Perform a standard MTT or CellTiter-Glo assay to measure metabolic activity and quantify cell viability relative to untreated controls.
- Inflammation Response Assay: Using immune cells (e.g., macrophages), measure the secretion of pro-inflammatory cytokines (e.g., IL-1β, TNF-α, IL-6) post-exposure using ELISA or a multiplex bead-based assay.
- Oxidative Stress Detection: Assess the generation of reactive oxygen species (ROS) using a fluorescent probe like DCFH-DA and flow cytometry or fluorescence microscopy.
- Data Analysis: Determine the IC50 value for cytotoxicity and the minimum concentration eliciting a significant immunogenic or oxidative stress response. This data is vital for establishing a safe dosage range during preclinical development [59].
Visualization of Workflows and Interactions
Diagram 1: From Synthesis to Biological Fate
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Nanoscale Biological Interactions Research
| Research Reagent / Material | Core Function | Role in Scalability & Performance |
|---|---|---|
| Certified Reference Materials (CRMs) [88] | Provides benchmark values for instrument calibration and method validation (e.g., for particle size). | Ensures consistency and comparability of characterization data across different production batches and labs, which is foundational for quality control. |
| Ionizable Cationic Lipids [89] | Key component of lipid nanoparticles (LNPs) for complexing and delivering mRNA; enables endosomal escape. | The chemical structure and purity of synthetic lipids are Critical Quality Attributes (CQAs) that must be strictly controlled for scalable GMP production. |
| Polyethylene Glycol (PEG)-Lipids [59] [89] | Used to functionalize nanoparticle surfaces; confers "stealth" properties by reducing opsonization and extending circulation time. | PEGylation is a common process, but batch-to-batch consistency in PEG chain length and conjugation efficiency is a major scalability challenge. |
| Characterization Standards & Kits | Includes standardized kits for measuring cytotoxicity, endotoxin, and cytokine levels. | Provides standardized, reproducible assays for safety and efficacy screening, which is crucial for the regulatory approval process of scaled-up products. |
The path to successfully scaling nanomedicines requires a fundamental shift from a discovery-centric mindset to an integrated product development approach. Future progress hinges on several key developments: the increased availability of certified reference materials for a wider array of physicochemical properties [88]; the adoption of advanced process analytical technologies (PAT) and modeling, potentially enhanced by artificial intelligence (AI), to achieve real-time control over CQAs [93] [59]; and a deeper, mechanistic understanding of nano-bio interactions to design materials with more predictable in vivo behavior [89]. Furthermore, international harmonization of regulatory definitions and requirements will significantly streamline the translation process [88]. By proactively addressing these scalability and manufacturing challenges, the field of nanoscale biological research can fully deliver on its promise of transformative therapeutics, ensuring that groundbreaking laboratory innovations can be reliably manufactured to benefit patients worldwide.
Assessing Nano-Bio Interactions: Analytical Methods and Platform Performance Evaluation
The expanding application of engineered nanoparticles (NPs) in biomedicine, from drug delivery to diagnostic imaging, necessitates a profound understanding of their interactions with biological systems [3]. These interactions dictate NP biodistribution, cellular uptake, potential efficacy, and toxicity. A comprehensive analysis of these events is fundamental to the rational design of safe and effective nanomedicines. This guide provides an in-depth examination of advanced characterization techniques, framing them within the core principles of nanoscale biological interaction research essential for scientists and drug development professionals.
The journey of nanoparticles within a biological system is complex, beginning with administration and culminating in interactions at the cellular and subcellular levels. Regardless of the route of administration, nanoparticles can traverse biological barriers and become systemically available [3]. Their intrinsic physicochemical properties—such as size, shape, charge, surface chemistry, and composition—critically influence their fate, including protein corona formation, cellular internalization pathways, and eventual organ-level accumulation [3]. Advanced characterization techniques are therefore required to quantitatively track, visualize, and analyze these processes across multiple biological scales.
Quantitative Biodistribution of Nanoparticles
A critical first step in understanding nanoparticle behavior in vivo is quantifying their distribution throughout the body. Pharmacokinetic studies provide valuable quantitative data on the percentage of injected dose per gram of tissue (%ID/g), allowing for the comparison of different nanoparticle formulations.
A large-scale analysis of published pharmacokinetics data, encompassing 2018 datasets, derived average Nanoparticle Biodistribution Coefficients (NBC) for various tissues in mice after intravenous administration [94]. The data quantitatively characterize the distribution of graphene oxide, lipid, polymeric, silica, iron oxide, and gold nanoparticles.
Table 1: Quantitative Biodistribution of Nanoparticles in Mouse Tissues
| Tissue / Organ | Nanoparticle Biodistribution Coefficient (NBC) [%ID/g] |
|---|---|
| Liver | 17.56 |
| Spleen | 12.10 |
| Tumor | 3.40 |
| Kidney | 3.10 |
| Lungs | 2.80 |
| Heart | 1.80 |
| Intestine | 1.80 |
| Pancreas | 1.20 |
| Stomach | 1.20 |
| Skin | 1.00 |
| Muscle | 0.60 |
| Brain | 0.30 |
Source: Adapted from [94]. %ID/g represents the percentage of the injected dose per gram of tissue.
The data reveals that the liver and spleen are the primary organs for nanoparticle accumulation, a phenomenon attributed to the mononuclear phagocyte system (MPS) [94]. This distribution presents a significant challenge for targeting other tissues, particularly the brain, which shows minimal nanoparticle accumulation. Furthermore, significant variability was observed in certain organs, which could often be explained by differences in nanoparticle physicochemical properties like size and material [94].
Advanced Techniques for Visualization and Quantification
Electron Microscopy for High-Resolution Imaging
Transmission Electron Microscopy (TEM) is an indispensable tool for the qualitative and quantitative analysis of nanoparticle-lung interactions and, more broadly, nanoparticle-cell interactions [95]. It provides an ideal method for visualizing particle-related structural changes in the respiratory tract, revealing the sub-cellular localization of nanoparticles, and investigating the three-dimensional nature of these interactions [95].
Experimental Protocol: TEM Sample Preparation and Analysis
Sample Fixation: The choice of fixation is crucial and depends on the scientific question.
- Vascular Perfusion Fixation: Recommended for studying nanoparticle interaction with alveolar macrophages or surfactant, as it washes out these components from the airways [95].
- Instillation Fixation: Suitable for investigating the translocation of nanoparticles into the blood circulation, as it preserves blood content in the pulmonary circulation [95].
- Fixative Solution: Typically, a combination of paraformaldehyde (PFA) and glutaraldehyde (GA) in a suitable buffer, often followed by post-fixation with heavy atom-containing molecules like osmium tetroxide to enhance contrast [95].
Embedding and Sectioning: Fixed samples are dehydrated and embedded in a resin (e.g., EPON) to allow for ultra-thin sectioning (50-100 nm thickness) using an ultramicrotome.
Imaging and Analysis:
- Conventional TEM: Provides high-resolution images to assess ultrastructural changes and nanoparticle localization within cellular compartments (e.g., endosomes, mitochondria, nucleus) [95].
- Energy-Filtered TEM (EFTEM): Used when nanoparticles cannot be distinguished from cellular organelles by conventional TEM alone. EFTEM allows for elemental analysis and mapping, confirming the presence of nanoparticles based on their chemical composition [95].
- Electron Tomography: Creates a high-resolution 3D reconstruction from a series of 2D TEM images, allowing for the detailed study of nanoparticle interactions with cellular organelles in three dimensions [95].
- Stereology: An unbiased quantitative method applied to TEM images to analyze the distribution of nanoparticles within tissues and cells, providing data on particle number, volume, and surface area [95].
<75 chars: TEM Workflow for Nanoparticle Visualization
Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
ICP-MS has emerged as a leading technique for the sensitive, elemental-specific, and quantitative analysis of nanoparticles in complex biological matrices [96]. Two main strategies are employed: single-particle ICP-MS and hyphenated techniques.
Experimental Protocol: Single-Particle ICP-MS (spICP-MS)
Sample Preparation: Biological tissues or fluids require extraction and digestion procedures to liberate nanoparticles into a stable suspension. This step is critical to avoid artifacts and ensure accurate representation of the native state [96].
Nebulization and Ionization: The sample suspension is nebulized into a fine aerosol and transported to the argon plasma, where it is desolvated, vaporized, and the constituent atoms are ionized.
Detection and Analysis: Ions are separated by a mass spectrometer based on their mass-to-charge ratio. In spICP-MS, a highly diluted suspension is introduced, resulting in discrete ion plumes for individual nanoparticles. The frequency of these detection events correlates with nanoparticle concentration, while the intensity of the signal is proportional to the nanoparticle's mass and, consequently, its size [96].
Key Applications:
- Direct Determination: spICP-MS allows for the direct measurement of nanoparticle size distribution, particle number concentration, and metal content at environmentally and biologically relevant levels [96].
- Spatially Resolved Analysis: Laser ablation spICP-MS (LA-spICP-MS) enables the direct analysis and imaging of nanoparticle distribution in tissue sections, providing spatial context to biodistribution studies [96].
Hyphenated Techniques: To address limitations of spICP-MS, such as analyzing complex mixtures, separation techniques can be coupled (hyphenated) with ICP-MS [96]. These include:
- Field-Flow Fractionation (FFF-ICP-MS): Separates nanoparticles based on diffusion coefficient.
- Hydrodynamic Chromatography (HDC-ICP-MS): Separates by size as nanoparticles travel through a column.
- Capillary Electrophoresis (CE-ICP-MS): Separates based on charge and size.
These hyphenated methods provide enhanced insight into particle size distributions, aggregation behavior, and interactions with complex sample matrices, and are often complementary to spICP-MS [96].
Investigating Nanoparticle-Induced Signaling Pathways
Upon cellular internalization, nanoparticles can localize in various organelles—escaping endosomes, accumulating in mitochondria and the endoplasmic reticulum, and even translocating to the nucleus [3]. This can initiate a cascade of intracellular signaling events, leading to diverse cellular outcomes.
The internalization of nanoparticles can cause undesirable nano-organelle interactions, triggering downstream signal mechanisms that result in toxic outcomes. These include cell membrane and cytoskeleton disruption, mitochondrial dysfunction, and nuclear DNA damage [3]. There is increasing evidence that nanoparticles can induce ROS generation, DNA damage, and mitochondrial disturbance, which in turn perturb key cellular signaling pathways, ultimately leading to consequences like cell cycle arrest, apoptosis, and inflammatory responses [3].
<75 chars: NP-Induced Signaling Pathway Cascade
Emerging Technologies: Controlling and Observing Interactions
Innovative technologies are continually being developed to provide greater precision in studying nanobio interactions. One such breakthrough is LEVA (Light-induced Extracellular Vesicle and Particle Adsorption), which enables the precise arrangement of biological nanoparticles, such as extracellular vesicles and particles (EVPs), on a surface [97].
Experimental Protocol: LEVA Technology
Surface Patterning: Ultraviolet light is shined onto a tiny array of mirrors and then onto a surface, creating a stencil-like pattern. The exposed areas undergo a chemical change, becoming sticky to EVPs, while unexposed areas remain neutral [97].
Vesicle Adsorption: EVPs isolated from biofluids or cell cultures are introduced to the patterned surface. They naturally attach only to the exposed, sticky regions, forming highly precise patterns such as dots, lines, or gradients [97].
Cell Interaction Studies: Researchers can then introduce cells (e.g., human neutrophils) to these patterned EVPs and observe real-time interactions using live-cell imaging. This allows for the quantitative study of how cells respond to spatially controlled EVP signals, such as swarming behavior in immune cells [97].
This technology allows scientists to move beyond studying EVPs in suspension and instead observe how cells interact with fixed patterns of these messengers, mimicking their distribution in tissues. This is particularly valuable for understanding processes like cancer migration, wound healing, and immune responses [97].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Reagents for Nanoparticle-Bio Interaction Research
| Reagent / Material | Function in Experimental Protocols |
|---|---|
| Paraformaldehyde (PFA) & Glutaraldehyde | Primary chemical fixatives for TEM that cross-link proteins and preserve cellular ultrastructure [95]. |
| Osmium Tetroxide | Post-fixative for TEM that stabilizes lipids and provides electron density (contrast) to membranes [95]. |
| Epoxy Resin (e.g., EPON) | Embedding medium for TEM that allows for ultra-thin sectioning of biological samples [95]. |
| Titanium Dioxide (TiO₂) / Polystyrene NPs | Model nanoparticles with well-defined properties, used as standards in toxicology and method development [95]. |
| Tungsten Oxide Microparticles | Can be used as a precursor for the in-situ synthesis of tungsten nanoparticles within a copper matrix for metallurgy studies [98]. |
| Fluoride Salts & Aluminum Reduction Agent | Precursors and catalyst for the in-situ synthesis of TiB₂ nanoparticles in a copper matrix via casting [98]. |
| Extracellular Vesicles and Particles (EVPs) | Biological nanoparticles released by cells, studied for their role in intercellular communication; the primary target for analysis using LEVA technology [97]. |
| Isolated Human Neutrophils | Primary immune cells used in functional assays (e.g., with LEVA) to study nanoparticle-driven chemotaxis and immune responses [97]. |
In vitro and in vivo models form the foundational framework of modern pharmaceutical development, serving as indispensable tools for evaluating drug efficacy and safety before human trials commence. These models have become deeply entrenched in discovery and preclinical workflows not because they are perfect, but because they represent trusted, practical systems that have consistently supported the development of clinically successful drugs [99]. The journey from drug discovery to approval is long and expensive, typically taking 10-15 years and requiring billions of dollars, with approximately 90% of drugs failing between Phase 1 trials and market approval [100]. Within this high-stakes environment, assessment models provide critical decision-making data that helps eliminate unsuitable candidates early and de-risks the development process.
The emergence of advanced technologies has begun transforming traditional assessment approaches. Model-Informed Drug Development (MIDD) frameworks now provide quantitative, data-driven insights that accelerate hypothesis testing and improve candidate evaluation efficiency [101]. Simultaneously, advanced in vitro systems such as organ-on-a-chip (OOC) platforms and complex microphysiological systems (MPS) offer more human-relevant models that better recapitulate human physiology [99] [100]. These innovations are particularly valuable for nanoscale biological interactions research, where traditional models often fail to accurately predict human responses due to interspecies differences and the unique behaviors of nanomaterials at the biological interface.
Fundamental Model Systems: From Simple to Complex
In Vitro Cellular Models
In vitro models range from simple two-dimensional (2D) cell cultures to advanced three-dimensional (3D) systems that better mimic human tissue architecture. Traditional 2D cell models remain widely utilized in high-throughput formats (such as 384-well plates) for single-readout assays that assess efficacy or safety across large compound libraries [99]. These models typically recapitulate specific disease states (e.g., breast cancer models) or test particular safety attributes (e.g., hERG ion channel safety). While their simplicity and throughput create high barriers to replacing them, their limitations in predicting human responses are well-documented.
Advanced in vitro systems have emerged to address the translational gaps of simple 2D cultures. These include organoids, microphysiological systems (MPS), and organ-on-a-chip (OOC) platforms that incorporate human cells in more physiologically relevant contexts [99] [100]. For nanoparticles and complex drug formulations, these advanced systems offer significant advantages by modeling human-specific transport mechanisms, cellular uptake processes, and metabolic pathways that differ substantially from those in animal models or simple cell cultures. The gut-liver-on-a-chip system represents one such advanced model that effectively mimics the oral administration pathway for drugs, allowing researchers to study first-pass metabolism and organ-specific toxicity in a human-relevant system [100].
In Vivo Animal Models
In vivo models, particularly rodent models, typically enter the development workflow during lead optimization to evaluate drug candidates in physiologically relevant systems [99]. These models are leveraged for multiple experimental readouts from a single animal, including safety, efficacy, and ADME (absorption, distribution, metabolism, and excretion) studies. For example, dose escalation studies in animals simultaneously enable toxicity assessment and pathological evaluation of organs including the liver, kidneys, and heart.
Different animal models offer specific advantages for particular research applications. Mice and rat models remain the most commonly used systems for investigating overall effects of therapeutics, with 'humanized mice' emerging as particularly valuable tools for accurately modeling human immune responses [100]. Non-human primates serve critical roles in areas where their biochemical and phylogenetic similarities to humans are essential, including vaccine development, orthopedic devices, Parkinson's disease research, and studies of diseases like HIV, Zika virus, and tuberculosis that poorly replicate in murine models [100].
Table 1: Characteristics of Fundamental Assessment Models
| Model Type | Key Features | Common Applications | Limitations |
|---|---|---|---|
| 2D Cell Cultures | High-throughput, cost-effective, simple readouts | Initial efficacy screening, target validation | Poor physiological relevance, lack tissue context |
| 3D Organoids | Three-dimensional architecture, patient-derived cells | Disease modeling, personalized medicine | Variable reproducibility, limited throughput |
| Organ-on-a-Chip | Microfluidics, mechanical cues, multi-cellular environments | Toxicity testing, barrier function studies, nanomaterial transport | Technical complexity, specialized equipment needed |
| Rodent Models | Complete mammalian system, genetic tools available | Efficacy in disease models, preliminary toxicity | Species-specific differences in drug metabolism |
| Non-Human Primates | Phylogenetic similarity to humans, comparable immune responses | Vaccine development, complex disease modeling | Ethical concerns, high cost, limited availability |
Advanced and Emerging Modeling Approaches
Model-Informed Drug Development (MIDD)
MIDD represents a paradigm shift in how assessment models are utilized throughout the drug development lifecycle. This approach employs quantitative modeling and simulation to support drug development and regulatory decision-making, with demonstrated potential to significantly shorten development cycle timelines and reduce costs [101]. A recent analysis estimates that MIDD implementation yields "annualized average savings of approximately 10 months of cycle time and $5 million per program" [102]. The MIDD framework encompasses multiple quantitative tools applied across development stages, from early discovery through post-market surveillance.
The "fit-for-purpose" principle guides MIDD implementation, emphasizing that modeling tools must align with specific Questions of Interest (QOI) and Context of Use (COU) at each development stage [101]. This strategic alignment ensures that models address the most critical uncertainties with appropriate methodology and validation rigor. For nanoscale interaction research, MIDD approaches are particularly valuable for integrating data across different model systems and scaling nanoparticle behavior from in vitro systems to predicted human responses.
Table 2: MIDD Tools and Their Applications in Drug Development
| MIDD Tool | Description | Primary Applications |
|---|---|---|
| PBPK (Physiologically Based Pharmacokinetic) | Mechanistic modeling of drug disposition based on physiology | Predicting human pharmacokinetics, drug-drug interactions, first-in-human dosing |
| QSP (Quantitative Systems Pharmacology) | Integrative modeling combining systems biology with pharmacology | Target validation, mechanism-based efficacy and toxicity prediction, biomarker identification |
| Population PK/PD | Modeling variability in drug exposure and response across individuals | Dose optimization, covariate effect identification, special population dosing |
| QSAR (Quantitative Structure-Activity Relationship) | Computational modeling linking chemical structure to biological activity | Compound optimization, toxicity prediction, lead candidate selection |
| AI/ML in MIDD | Machine learning algorithms applied to complex biological datasets | Predictive toxicology, novel compound synthesis, model definition and validation |
Integrated In Vitro-In Vivo Approaches
The most significant advances in assessment methodologies come from integrated approaches that combine in vitro and in vivo data through computational modeling. These integrated strategies help overcome the limitations of individual model systems while providing a more comprehensive understanding of drug behavior. For nanoparticles and complex formulations, this integration is particularly important due to the unique biophysical properties that influence biodistribution, cellular uptake, and clearance mechanisms.
The In Vitro Permeation Test (IVPT) represents one such integrated methodology that combines laboratory testing with computational analysis. IVPT serves as an important performance test for supporting demonstrations of bioequivalence for generic topical drug products when utilizing characterization-based bioequivalence approaches [103]. These tests measure the rate and extent of drug permeation through biological membranes, providing critical data that can reduce the need for certain clinical studies.
Experimental Protocols and Methodologies
Protocol: Advanced Hepatotoxicity Assessment Using Liver-on-a-Chip
Drug-induced liver injury (DILI) remains a leading cause of drug attrition and post-approval withdrawal, creating an urgent need for human-relevant liver models [100]. The following protocol outlines hepatotoxicity assessment using an advanced liver-on-a-chip platform:
Materials and Reagents:
- Primary human hepatocytes or induced pluripotent stem cell (iPSC)-derived hepatocytes
- Non-parenchymal liver cells (Kupffer cells, hepatic stellate cells)
- Organ-on-a-chip device with appropriate membrane materials
- Hepatocyte culture medium (William's E Medium supplemented with growth factors)
- Test compounds and reference controls
- Albumin and urea assay kits
- CYP450 activity assay substrates
- RNA extraction kit for transcriptomic analysis
Methodology:
- Device Preparation: Coat the membrane surfaces of the microfluidic device with appropriate extracellular matrix proteins (collagen I, Matrigel) to promote cell adhesion and polarization.
- Cell Seeding: Seed primary human hepatocytes at high density (≥1×10^6 cells/cm²) in the main chamber of the device. Allow cells to attach for 4-6 hours before initiating flow.
- Co-culture Establishment: Introduce non-parenchymal cells (2:1 ratio of hepatocytes to non-parenchymal cells) to create a more physiologically relevant liver model.
- Medium Perfusion: Initiate continuous medium flow at physiological shear stress levels (0.5-1.0 dyne/cm²) using a programmable syringe pump.
- Model Validation: Confirm model functionality by measuring albumin secretion (≥5 μg/day/10^6 cells), urea production, and CYP450 enzyme activities (CYP3A4, CYP2C9) against established benchmarks.
- Compound Dosing: Introduce test compounds at clinically relevant concentrations through the perfusion system. Include multiple dosing regimens (single dose, repeated dosing) as appropriate.
- Endpoint Assessment: Evaluate hepatotoxicity through multiple parameters including cell viability (ATP content), membrane integrity (LDH release), metabolic competence (albumin, urea), and mechanistic biomarkers (miR-122, HMGB1).
- Data Analysis: Compare results to known hepatotoxicants (e.g., acetaminophen, troglitazone) and non-hepatotoxic controls to establish predictive validity.
This protocol typically requires 14-21 days from cell seeding to final endpoint assessment and provides a more human-relevant prediction of hepatotoxicity compared to traditional 2D hepatocyte cultures.
Protocol: In Vivo Pharmacokinetic and Toxicity Study in Rodents
Comprehensive in vivo assessment remains essential for evaluating whole-body distribution, metabolism, and toxicity of new chemical entities. The following protocol outlines a standardized approach for rodent pharmacokinetic and toxicity studies:
Materials and Reagents:
- Test article (API or formulation)
- Laboratory rodents (mice or rats) of appropriate strain, age, and gender
- Anesthetics and analgesics for humane animal handling
- Blood collection tubes (EDTA-coated for plasma, serum separator tubes)
- Tissue preservation solutions (neutral buffered formalin)
- Clinical chemistry analyzers
- LC-MS/MS system for compound quantification
- Histopathology supplies (embedding media, stains)
Methodology:
- Study Design: Implement appropriate group sizes (typically n=5-8 for PK, n=10-15 for toxicity) with control, vehicle control, and multiple dose-level groups. Include both single-dose and repeat-dose arms as needed.
- Dose Formulation: Prepare test article in appropriate vehicle with confirmation of stability, homogeneity, and concentration.
- Compound Administration: Administer via clinically relevant route (oral gavage, intravenous injection, etc.) at precise volumes based on body weight.
- Blood Collection: Serial blood sampling at predetermined timepoints (e.g., 0.25, 0.5, 1, 2, 4, 8, 12, 24 hours) for pharmacokinetic profiling.
- Tissue Collection: Euthanize animals at designated endpoints for comprehensive tissue collection (liver, kidney, heart, lung, spleen, brain).
- Bioanalysis: Quantify drug concentrations in plasma and tissues using validated analytical methods (typically LC-MS/MS).
- Clinical Pathology: Evaluate hematology parameters (complete blood count), clinical chemistry (liver enzymes, renal function markers), and urinalysis.
- Histopathology: Process tissues for microscopic evaluation by a board-certified veterinary pathologist using standardized grading criteria.
- Data Analysis: Calculate pharmacokinetic parameters (Cmax, Tmax, AUC, half-life) using non-compartmental analysis. Correlate exposure parameters with observed toxicological findings.
This comprehensive protocol generates critical data on a compound's absorption, distribution, metabolism, excretion, and toxicity profile, supporting regulatory submissions and first-in-human trial design.
Visualization of Model Systems and Workflows
Decision Framework for Model Selection
Decision Framework for Model Selection
Integrated Drug Development Workflow
Integrated Drug Development Workflow
The Research Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagent Solutions for Assessment Models
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Primary Human Cells | Provide human-relevant responses for in vitro models | Source from reputable suppliers; consider donor variability in experimental design |
| iPSC-Derived Cells | Offer patient-specific models with renewable source | Require thorough characterization of differentiation efficiency |
| Extracellular Matrix Proteins | Mimic tissue microenvironment for 3D cultures | Select appropriate matrix (Collagen I, Matrigel, fibrin) for specific tissue types |
| Microfluidic Devices | Enable organ-on-a-chip platforms with physiological flow | Choose appropriate membrane materials and pore sizes for specific applications |
| CYP450 Activity Assays | Assess metabolic competence of liver models | Monitor multiple isoforms (3A4, 2D6, 2C9) for comprehensive assessment |
| Multiplex Cytokine Kits | Evaluate immune responses and inflammatory pathways | Essential for immunotoxicity assessment of nanomaterials and biologics |
| LC-MS/MS Systems | Quantify drug concentrations in biological matrices | Require rigorous validation for regulatory submissions |
| Molecular Probes for Viability | Assess multiple cell health parameters | Combine measures (ATP content, membrane integrity, apoptosis markers) for comprehensive assessment |
| Tissue Preservation Solutions | Maintain tissue architecture for histopathology | Standardized fixation protocols essential for comparative analysis |
| Species-Specific Reagents | Enable analysis in animal models | Critical for accurate interpretation of in vivo studies |
Regulatory Considerations and Future Perspectives
The regulatory landscape for assessment models is evolving rapidly, with recent guidance supporting modernization of traditional approaches. The FDA Modernization Act 2.0 has opened significant new pathways by allowing alternatives to animal testing for drug and biological product applications [100] [102]. This legislation recognizes the value of advanced in vitro models (organoids, OOC systems, human iPSCs) and in silico approaches (computer modeling, MIDD) for assessing drug metabolism and toxicity. Similar regulatory shifts are occurring globally, with the European Union implementing a complete ban on cosmetic products developed using animal models, followed by Canada, Brazil, Colombia, and Mexico [100].
Despite these promising developments, significant challenges remain for widespread adoption of advanced models. Validation represents the primary hurdle, as researchers must still conduct legacy experiments alongside new approaches until sufficient validation is achieved, making advanced models a supplemental cost rather than a replacement in the short term [99]. Both retrospective validation (using therapeutics with known toxicity profiles) and prospective validation (successful use supporting drug progression to clinical trials) are required to build regulatory confidence [99]. The FDA's most recent guidance indicates a more active stance on reducing animal usage but maintains a cautious approach, placing the burden of validation and regulatory evidence on pharmaceutical sponsors [99].
Looking forward, the integration of artificial intelligence and machine learning with advanced model systems promises to transform assessment capabilities. AI/ML algorithms can analyze high-dimensional data (transcriptomics, phenotypic screens) to demonstrate that in vitro models align with relevant disease biology and drug response [99]. These technologies are already being applied to reduce animal use across complex and poorly predicted areas such as cardiac toxicity and immune response, supporting the FDA's goal of eventually eliminating animal testing [99]. For nanoscale interactions research, these computational approaches are particularly valuable for predicting nanoparticle behavior and biological interactions that are difficult to measure experimentally.
The future of assessment models lies in integrated systems that combine the best attributes of in vitro, in vivo, and in silico approaches. These systems will leverage human-relevant in vitro models for high-content screening, targeted in vivo models for specific questions that cannot yet be addressed in vitro, and sophisticated computational models to integrate data and extrapolate to human predictions. This holistic approach will be particularly important for nanotechnology applications, where unique physicochemical properties influence biological interactions across multiple scales. As these technologies mature, they promise to create more predictive, efficient, and human-relevant assessment paradigms that accelerate the development of safe and effective therapeutics.
The study of fundamental nanoscale biological interactions is a cornerstone of modern nanomedicine, critical for designing safe and effective therapeutic and diagnostic agents. The interface where engineered nanoparticles (NPs) meet biological systems—the nano-bio interface—governs critical outcomes including biocompatibility, targeting efficiency, and cellular responses [104]. Understanding the interactions of nanomaterials with biological and environmental media is a key research priority, as emphasized by funding initiatives such as the National Science Foundation's Nanoscale Interactions program, which supports fundamental research to advance quantitative understanding in this area [77]. These interactions are particularly complex, influenced by nanomaterial physicochemical properties including size, surface chemistry, charge, and shape, all of which modulate behavior in biological environments.
This review provides a comparative analysis of four major classes of nanoplatforms—lipid-based, polymeric, metallic, and biomimetic systems—evaluating their fundamental properties, interaction mechanisms with biological systems, and performance in therapeutic applications. The content is framed within the context of a broader thesis on nanoscale biological interactions research, providing researchers and drug development professionals with a technical guide to selecting and engineering nanoplatforms based on their intended application and the desired interaction with biological targets.
Comparative Analysis of Nanoplatform Properties
The design and selection of a nanoplatform are predicated on its intended application, which dictates the necessary physicochemical characteristics, loading capacity, release kinetics, and biocompatibility profile. The four major classes of nanoplatforms each possess distinct advantages and limitations rooted in their material composition and structural organization.
Table 1: Core Characteristics and Applications of Major Nanoplatforms
| Nanoplatform | Core Composition | Key Structural Features | Dominant Interaction Mechanisms | Primary Applications |
|---|---|---|---|---|
| Lipid-Based | Phospholipids, cholesterol [105] | Bilayer membranes, aqueous core, often PEGylated | Membrane fusion, endocytosis, lipid exchange [104] | Drug/gene delivery, vaccines [106] |
| Polymeric | PLA, PLGA, PCL, chitosan [105] [107] | Solid matrix or capsule, tunable degradation | Degradation-controlled release, surface receptor binding | Controlled drug release, tissue engineering |
| Metallic | Gold, silver, iron oxide [104] [108] | Inorganic crystal core, surface functionalization | Plasmonic resonance, catalytic activity, hyperthermia [108] | Bioimaging, photothermal therapy, diagnostics |
| Biomimetic | Natural cell membranes (RBC, platelet) on synthetic cores [107] | Core-shell with biologically derived exterior | CD47 "self-marker" signaling, avoidance of immune clearance [107] | Targeted delivery, stealth platforms, theranostics |
Table 2: Quantitative Performance Comparison of Nanoplatforms
| Nanoplatform | Typical Size Range (nm) | Drug Loading Capacity (%EE) | Release Kinetics Profile | Circulation Half-Life | Key Limitation |
|---|---|---|---|---|---|
| Lipid-Based | 50-100 [105] | Variable (hydrophilic/hydrophobic) | Burst release common, stabilized versions offer sustained release [105] | Moderate, enhanced with PEGylation | Stability, premature leakage [105] |
| Polymeric | 20-200 | High (up to ≥75% reported) [109] | Sustained, controlled via polymer degradation [107] | Long for stable, biodegradable polymers | Potential polymer toxicity, biodegradation rate |
| Metallic | 5-100 (tunable) [104] | Low to moderate (surface conjugation) | Stimuli-responsive (e.g., light, pH) | Varies with surface coating | Biopersistance, potential toxicity [108] |
| Biomimetic | 80-150 | Dependent on core (polymeric/inorganic) | Controlled by core material and membrane permeability [107] | Significantly extended (stealth properties) [107] | Complex fabrication, batch variability |
Experimental Protocols for Assessing Nano-Bio Interactions
A rigorous, multi-technique approach is essential to fully characterize nanoplatform behavior and their interactions with biological systems. The following protocols represent key methodologies cited in foundational research.
Protocol: Interaction Studies with Biomimetic Lipid Membranes
This protocol is designed to evaluate non-specific interactions between nanoparticles and model lipid membranes, which serve as simplified biological interfaces [104].
Materials:
- Glycerol monooleate (GMO) & 1,2-dioleoyl-sn-glycero-3-phosphocholine (DOPC): Lipids for constructing cubic phase membranes and lamellar bilayers as biomimetic interfaces [104].
- Citrate-stabilized AuNPs and AgNPs: Prototypical metallic nanoparticles with weakly associated surface ligands that allow direct interaction with lipid interfaces [104].
- Quartz Crystal Microbalance (QCM) Sensor Chips: Solid supports for forming lipid films for real-time adsorption measurements [104].
- Synchrotron Small-Angle X-ray Scattering (SAXS): For characterizing the structural integrity of cubic lipid phases during and after nanoparticle interaction [104].
Methodology:
- Membrane Preparation: Disperse lipids to form cubosomes (dispersed nanoparticles with internal cubic structure) in aqueous solution using preparation protocols that yield stabilizer-free particles. Alternatively, form solid-supported lipid layers of nanometric thickness on QCM sensor chips [104].
- Exposure and Monitoring: Challenge lipid cubic phase membranes with nanoparticle suspensions (e.g., AuNPs, AgNPs).
- Bulk Interaction Analysis: Employ UV-visible spectroscopy to monitor nanoparticle clustering or aggregation in bulk solution. Use SAXS to detect any disruption or phase changes in the cubic membrane architecture induced by nanoparticles [104].
- Surface Interaction Analysis: Use QCM to measure mass changes associated with nanoparticle adsorption onto supported lipid layers in real-time. Complement with Confocal Laser Scanning Microscopy (CLSM) to visualize the spatial distribution and clustering of fluorescently labeled nanoparticles on the membrane [104].
Protocol: In Vitro Cytotoxicity and Genotoxicity Assessment
This standardized protocol evaluates the biocompatibility and safety of novel nanocarriers, essential for preclinical development [109].
Materials:
- HEK293, HCT-116, and MCF-7 Cell Lines: Representative human cell lines for 2D monolayer and 3D spheroidal culture models.
- Caenorhabditis elegans (C. elegans): A simple multicellular animal model for in vivo toxicity screening, offering advantages including low cost, short lifespan, and molecular-level similarities with humans [109].
- Apoptosis Assay Kits: For detecting the upregulation or downregulation of apoptosis-related pathways.
Methodology:
- Cell Culture: Maintain cell lines under standard conditions. For 3D assessments, generate spheroidal conformations.
- Nanoparticle Exposure: Treat 2D cultures and 3D spheroids with a range of concentrations of both empty and drug-loaded nanocarriers.
- Viability and Cytotoxicity Assay: Incubate for a predetermined period (e.g., 24-72 hours) and assess cell viability using standard assays (e.g., MTT, Alamar Blue). Calculate IC₅₀ values.
- Genotoxicity Assessment: Analyze cells post-treatment for markers of apoptosis and genotoxicity (e.g., caspase activation, DNA damage) to determine if cell death is triggered via specific pathways.
- In Vivo Toxicity Screening: Expose C. elegans to the nanoformulations. Evaluate key physiological parameters including developmental stages, egg-laying behavior, and locomotion to assess overall in vivo toxicity and biocompatibility [109].
Protocol: Physicochemical Characterization and Serum Stability
This protocol ensures that nanoformulations meet key criteria for in vivo administration, particularly for intravenous delivery [109].
Materials:
- Dynamic Light Scattering (DLS) Instrument: For measuring hydrodynamic radius (Rh), size distribution, and polydispersity index (PDI).
- Fetal Bovine Serum (FBS): Protein-rich media to simulate physiological conditions.
- UV-Vis Spectroscopy: For determining drug encapsulation efficiency (%EE).
Methodology:
- Initial Characterization: Dilute the nanoformulation in a suitable buffer and analyze using DLS to determine the mean Rh and PDI. A PDI value below 0.3 is generally indicative of a monodisperse population.
- Encapsulation Efficiency: Separate unencapsulated drug via dialysis or centrifugation. Analyze the drug content within the nanoparticles using UV-Vis spectroscopy and calculate the %EE.
- Serum Stability Test: Incubate the nanoformulation with FBS/PBS solution (e.g., 10-50% FBS) for extended periods (e.g., 1-24 hours) at 37°C.
- Stability Assessment: Re-analyize the incubated sample using DLS. Monitor for significant increases in Rh or PDI, which indicate protein adsorption and corona formation, potentially leading to aggregation. A stable system will maintain its original physicochemical characteristics [109].
Signaling Pathways and Experimental Workflows
The interaction between nanoplatforms and biological systems triggers a sequence of events that determines the nanomaterial's fate and efficacy. The following diagram illustrates the primary pathways, from administration to therapeutic action, highlighting key biological barriers and decision points.
Diagram 1: In Vivo Journey of a Nanoplatform
The experimental development of a novel nanoplatform is an iterative process that moves from design and synthesis through a multi-stage evaluation pipeline. The workflow below outlines the key phases and decision points in this development cycle.
Diagram 2: Nanoplatform Development Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogues critical reagents and materials used in the synthesis, characterization, and biological evaluation of nanoplatforms, as derived from the cited experimental protocols.
Table 3: Essential Research Reagents and Materials for Nanoplatform Development
| Reagent/Material | Function/Application | Example from Literature |
|---|---|---|
| Glycerol Monooleate (GMO) | Lipid for constructing non-lamellar (cubic) biomimetic membranes to study nano-bio interactions [104]. | Used to create stabilizer-free cubosomes for interacting with metallic NPs [104]. |
| Pluronic 188 (Poloxamer) | Non-ionic triblock copolymer surfactant; stabilizes nano-formulations, improves biocompatibility and circulation time [109]. | Forms hybrid nanosystems with Tween 80 for methotrexate delivery [109]. |
| DOPC / DOTAP Lipids | Phospholipids for constructing lamellar lipid bilayers (liposomes, supported membranes). DOTAP introduces positive charge. | Standard lipids for model membrane formation [104]. |
| Poly(Lactic-co-Glycolic Acid) (PLGA) | Biodegradable polymer forming the core of polymeric and hybrid nanoparticles; enables controlled drug release [107]. | Common polymer core in Lipid-Polymer Hybrid Nanoparticles (LPHNPs) [107]. |
| Citrate-stabilized Gold NPs (AuNPs) | Prototypical metallic nanoparticles; easily functionalized, used for studying fundamental interactions and photothermal therapy. | Model NPs for interacting with cubic lipid membranes; exhibit extensive membrane-induced clustering [104]. |
| DSPE-PEG(2000) | Phospholipid-PEG conjugate; used for PEGylating nanocarriers to confer "stealth" properties and prolonged circulation [107]. | Component of the outer shell in LPHNPs to reduce immune recognition [107]. |
| Caenorhabditis elegans | Simple in vivo model organism for preliminary toxicity screening of nanoformulations. | Used to evaluate developmental, egg-laying, and locomotion toxicity of a novel Pluronic 188-Tween 80 nanosystem [109]. |
| Fetal Bovine Serum (FBS) | Protein-rich medium for evaluating the stability of nanoformulations and protein corona formation in simulated physiological conditions. | Used to test the stability of hybrid nanosystems by monitoring size and PDI changes post-incubation [109]. |
The comparative analysis of lipid-based, polymeric, metallic, and biomimetic nanoplatforms reveals that no single platform is universally superior. The optimal choice is dictated by the specific application and the desired interaction with the biological target. Lipid-based systems excel in encapsulating diverse cargoes and fusing with biological membranes, polymeric nanoparticles offer superior control over release kinetics, metallic platforms provide unique theranostic capabilities, and biomimetic systems exhibit unparalleled stealth and targeting potential. The future of nanoplatform development lies in the intelligent design of hybrid systems that combine the strengths of individual materials. Furthermore, a deep understanding of the fundamental nano-bio interactions—such as protein corona formation, interaction with complex biological membranes, and avoidance of immune clearance—remains paramount. As this field progresses, standardized experimental protocols and robust characterization, from physicochemical analysis to advanced in vivo models, will be crucial for translating promising nanoplatforms from the laboratory to the clinic, ultimately fulfilling their potential in advanced drug delivery and diagnostic applications.
Understanding the interactions between nano-engineered particles and biological cells is fundamental to advancing precision medicine, targeted drug delivery, and medical diagnostics. These interactions involve a complex interplay of biological, physical, and chemical processes across multiple spatial and temporal scales. Mathematical modeling provides a powerful toolset to disentangle these complex phenomena, transforming qualitative observations into quantitative, predictive frameworks. By developing mechanistic models that capture the essential features of particle-cell interactions, researchers can move beyond descriptive accounts to generate testable hypotheses, optimize experimental designs, and accelerate the rational design of nano-engineered particles for specific biomedical applications. This technical guide examines cutting-edge mathematical approaches for quantifying particle-cell interactions, with particular emphasis on models that account for the inherent biological heterogeneity often overlooked in traditional analyses.
Core Mathematical Models for Particle-Cell Interactions
Homogeneous Population Model
The foundational model for describing particle-cell interactions assumes a homogeneous cell population where all cells exhibit identical interaction characteristics. This ordinary differential equation-based approach describes the temporal evolution of particle association with cells in a well-mixed system [110].
The concentration of particles per cell in the media, u(t), evolves according to:
Where P(t) (particles/cell) represents the number of particles associated with a cell at time t and is governed by conservation of mass:
Table 1: Parameters of the Homogeneous Population Model
| Parameter | Symbol | Units | Description |
|---|---|---|---|
| Particle concentration | u(t) | particles·cell⁻¹·m⁻³ | Time-dependent concentration of particles in media |
| Initial particle concentration | u₀ | particles·cell⁻¹·m⁻³ | Initial concentration of particles in media |
| Fractional surface coverage | C | dimensionless | Fraction of surface area covered by cells |
| Cell surface area | S | m² | Surface area of cell boundary |
| Particle-cell association rate | r | m·s⁻¹ | Rate constant for particle-cell association |
| System volume | V | m³ | Volume of well-mixed media |
| Cell carrying capacity | K | particles·cell⁻¹ | Maximum number of particles associated per cell |
This model provides an analytical solution for P(t) that depends on whether the carrying capacity K equals Vu₀ or not. For most experimental conditions where P(t) ≪ Vu₀ for all t, the solution approaches a saturation curve where P(t) asymptotically approaches K over time [110].
Heterogeneous Population Model
Recent advances have recognized that biological systems exhibit significant cell-to-cell variability. The heterogeneous population model generalizes the homogeneous approach by incorporating variability in key parameters across individual cells [110].
In this extended framework, the particle-cell association rate r and carrying capacity K are treated as lognormally distributed parameters:
This distribution choice reflects the biological reality that these parameters are non-negative and typically exhibit right-skewed distributions across cell populations.
The heterogeneous model captures two crucial aspects of real biological systems:
- Cell-to-cell heterogeneity: Individual cells within a population exhibit different particle association rates and carrying capacities
- Cell-cell competition: Cells compete for available particles in the system, creating interdependent dynamics
This approach enables researchers to quantify not only average population behavior but also the distribution of behaviors across individual cells, providing significantly more biological insight than homogeneous models.
Parameter Estimation and Model Validation Frameworks
Approximate Bayesian Computation (ABC)
Parameter estimation for particle-cell interaction models presents significant challenges due to the complexity of the models and the noise inherent in biological measurements. Approximate Bayesian Computation (ABC) provides a powerful simulation-based inference framework for estimating parameters in these models [110].
The ABC methodology follows this general workflow:
- Prior Specification: Define prior distributions for model parameters based on biological knowledge
- Parameter Proposal: Sample candidate parameter sets from the prior distributions
- Simulation: Generate synthetic datasets using the mathematical model with proposed parameters
- Distance Calculation: Compare simulated data with experimental data using appropriate distance metrics
- Acceptance/Rejection: Accept parameter sets that generate data sufficiently close to experimental observations
This approach is particularly valuable for models where likelihood functions are intractable or computationally expensive to calculate. ABC methods have been successfully applied to interpret flow cytometry data from particle-cell interaction experiments, enabling robust parameter estimation even with significant biological variability [110].
Equation Learning for Model Identification
Machine learning approaches, specifically equation learning methods, offer complementary techniques for identifying particle-cell interaction mechanisms from experimental data. These data-driven modeling approaches augment established biological knowledge to create interpretable models [111].
A key advantage of equation learning frameworks is their ability to:
- Elucidate particle-cell interactions from experimental association data
- Handle diverse particle-cell pairs including both adherent and suspension cell lines
- Accommodate particles with varying physicochemical properties (6 nm to 1032 nm diameter)
- Work with different surface functionalizations (small molecule, monoclonal antibody, peptide)
- Identify consistent interaction models despite experimental diversity
Application of these frameworks to thirty different particle-cell pairs revealed that only four unique models emerged from 2048 potential models, suggesting that nonlinear saturation effects are a fundamental feature governing particle-cell interactions across diverse experimental systems [111].
Experimental Protocols and Methodologies
Standardized Particle-Cell Interaction Assays
Table 2: Key Experimental Protocols for Particle-Cell Interaction Studies
| Protocol Step | Technical Specifications | Purpose & Rationale |
|---|---|---|
| Cell Culture | THP-1 human leukemia monocytic cell line; standard culture conditions | Maintain consistent, biologically relevant cell population for experiments |
| Particle Incubation | Incubation periods: 1, 2, 4, 8, 16, 24 hours; controlled temperature and CO₂ | Measure time-dependent particle association under physiological conditions |
| Flow Cytometry | 20,000 measurements per time point; calibrated to reference voltage | High-throughput quantification of particle association at single-cell resolution |
| Control Measurements | Cell-only control (11,605 measurements); Particle-only control (≥249,344 measurements) | Establish baseline fluorescence and account for autofluorescence |
| Data Replication | Endpoint measurements from two replicates grouped per time point | Account for biological and technical variability while maintaining statistical power |
Data Acquisition and Processing
The experimental workflow generates three primary data types that require different processing approaches [110]:
- Time-course particle-cell association data (
D_exp): Fluorescent signals from individual cells across multiple time points, providing the kinetic profile of particle association - Cell-only control data (
D_cells: Fluorescent measurements of untreated cells, establishing baseline autofluorescence - Particle-only control data (
D_particles): Fluorescent measurements of individual particles, characterizing the particle population distribution
All measurements must be calibrated to a reference voltage to enable quantitative comparisons across experiments and instruments. The snapshot nature of these time-series data (where multiple cells are measured at each time point, but the same cells are not tracked longitudinally) necessitates specific statistical approaches for proper interpretation [110].
Computational Implementation and Workflow
Model Simulation and Analysis Pipeline
The following diagram illustrates the integrated computational workflow for parameter estimation, model selection, and experimental design optimization in particle-cell interaction studies:
Optimal Experimental Design Strategy
A critical application of mathematical modeling is identifying experimental designs that maximize information gain while minimizing resources. Systematic exploration of 3003 different experimental designs revealed that careful selection of measurement time points significantly enhances parameter estimation precision [110].
The optimal design strategy involves:
- Time point selection: Choosing specific time points that maximize information about model parameters
- Rate-specific optimization: Identifying different optimal designs for different particle-cell association rates
- Robust overall design: Establishing a general optimal design when association rates are unknown
- Resource allocation: Balancing the number of time points against measurement density at each time point
This model-guided experimental design approach enables researchers to extract maximum information from particle-cell interaction experiments, accelerating the optimization of nano-engineered particles for specific biomedical applications.
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Particle-Cell Interaction Studies
| Reagent/Material | Specification/Function | Experimental Role |
|---|---|---|
| Nano-engineered Particles | Polymethacrylic acid (PMA) core-shell particles (150 nm, 214 nm, 633 nm) | Primary test particles with controlled physicochemical properties |
| Cell Lines | THP-1 human leukemia monocytic cell line | Model suspension cell system for interaction studies |
| Characterization Instrument | Flow cytometer with calibrated fluorescence detection | High-throughput single-cell measurement of particle association |
| Control Samples | Cell-only and particle-only suspensions | Establish baseline signals and account for background fluorescence |
| Microfluidic Deposition System | Picoliter-volume droplet generation with millisecond drying | Surface deposition while preserving solution-state properties [82] |
| Atomic Force Microscopy | Nanomechanical mapping with nanometer resolution | Characterize mechanical properties and morphology of condensates [82] |
Interpreting Model Outputs and Biological Significance
Key Quantitative Parameters and Their Interpretation
Table 4: Interpretation of Model Parameters in Biological Context
| Parameter | Biological Significance | Implications for Particle Design |
|---|---|---|
| Particle-Cell Association Rate (r) | Efficiency of initial particle-cell contact and internalization | Higher rates suggest better targeting; can be optimized through surface functionalization |
| Carrying Capacity (K) | Maximum number of particles per cell, reflecting saturation effects | Determines maximum payload delivery; influenced by cell surface area and internalization mechanisms |
| Heterogeneity Parameters (sr, sK) | Cell-to-cell variability in particle association | Quantifies population diversity; important for predicting consistent therapeutic effects |
| Association Half-time | Time required for half-maximal particle association | Informs dosing schedules and kinetic optimization for time-sensitive applications |
Relationship to Nanoscale Biological Interactions
The mathematical frameworks described here operate within the broader context of fundamental nanoscale biological interactions research. The National Science Foundation's Nanoscale Interactions program emphasizes the importance of developing "fundamental and quantitative understanding of the interactions of nanomaterials and nanosystems with biological and environmental media" [77]. This research direction includes:
- Characterization of interactions at nanomaterial-bio interfaces
- Development of predictive tools based on fundamental nanostructure behavior
- Examination of transport, interaction, and impact of nanostructures on biological systems
- Simulations of nanoparticle behavior at interfaces with experimental validation
The mathematical models align perfectly with these research priorities by providing quantitative, predictive frameworks that connect nanoparticle properties to biological interactions and outcomes.
Future Directions and Integration with Emerging Techniques
The field of mathematical modeling for particle-cell interactions is rapidly evolving through integration with emerging experimental and computational techniques. Several promising directions merit emphasis:
- Multi-scale modeling frameworks that connect molecular-scale interactions to cellular-level outcomes
- Integration with high-resolution imaging techniques such as atomic force microscopy for nanoscale property mapping [82]
- Machine learning augmentation of traditional mechanistic models for enhanced predictive capability [111]
- Standardized parameter reporting to enable objective comparisons across different particle-cell systems [110]
- Expansion to complex biological environments including 3D tissue models and in vivo systems
These advances will continue to enhance our fundamental understanding of nanoscale biological interactions while accelerating the development of effective nano-engineered particles for biomedical applications.
The translation of nanotechnology from laboratory research to clinical therapeutics represents a multifaceted challenge, requiring meticulous attention to design, characterization, and safety protocols. Nanomedicine operates at a scale of 1–100 nm, exploiting unique physicochemical properties not present in bulk materials to revolutionize drug delivery, diagnostic imaging, and regenerative medicine [59]. The fundamental advantage of nanoscale therapeutic platforms lies in their ability to enhance treatment efficacy while minimizing adverse side effects through targeted delivery mechanisms [58] [59]. This targeted approach enables precise drug delivery to specific cells or tissues, such as cancer cells, while reducing harm to healthy tissues—a paramount consideration in clinical applications [59]. Despite this potential, significant barriers remain in translating promising in vitro results to clinically viable therapies, including complex biological barriers, potential immune responses, and stringent regulatory requirements for clinical approval [59].
Design Principles for Clinical Translation
Nanomaterial Design and Biocompatibility
The clinical translation of nanomedicines necessitates rigorous design principles focused on biological interactions. A critical first step involves selecting materials with established safety profiles and optimizing their size, surface chemistry, and functionalization to enhance targeting capabilities and circulation time [59]. Polyethylene glycol (PEG) conjugation, or PEGylation, serves as a cornerstone strategy for improving biocompatibility by protecting nanomaterials from immune system detection, thereby extending their plasma half-life and improving delivery to target tissues [59]. Surface functionalization must be carefully designed to avoid triggering adverse immune responses while promoting specific interactions with target cells [59].
Synthesis and Manufacturing Control
Reproducible, scalable manufacturing is essential for clinical translation and requires stringent process controls. Nanomaterial production primarily utilizes two approaches: top-down methods that break down larger materials using mechanical or chemical energy, and bottom-up approaches that construct nanomaterials by assembling atomic or molecular components [59]. Quality-by-Design (QbD) principles coupled with Process Analytical Technologies (PAT) enable real-time monitoring and control during manufacturing to maintain consistent quality and performance standards [59]. The critical manufacturing pathway encompasses several vital stages, outlined in Table 1 below.
Table 1: Critical Manufacturing Steps for Nanomedicines
| Manufacturing Stage | Key Activities | Quality Control Considerations |
|---|---|---|
| Raw Material Selection | Sourcing of high-purity materials | Ensure quality and purity of starting materials |
| Synthesis | Employing top-down or bottom-up approaches | Control of particle size, morphology, and structure |
| Functionalization | Surface modification (e.g., PEGylation) | Consistency of surface coating and ligand attachment |
| Characterization | Assessing size, shape, surface area, composition | Comprehensive physicochemical profiling |
| Formulation | Incorporation into drug delivery systems | Stability, sterility, and dosage accuracy |
| Quality Control | PAT implementation for real-time monitoring | Adherence to Critical Quality Attributes (CQAs) |
Characterization and Analysis Protocols
Comprehensive Physicochemical Characterization
Rigorous characterization of nanomaterials is fundamental to ensuring batch-to-batch reproducibility and predicting biological behavior. Characterization must assess critical physicochemical properties including size, shape, surface area, surface charge, and chemical composition [59]. These parameters profoundly influence biodistribution, cellular uptake, and clearance pathways in vivo. Advanced analytical techniques such as electron microscopy, dynamic light scattering, and surface plasmon resonance provide essential data on nanomaterial properties. Complete characterization must be conducted under conditions mimicking physiological environments to predict performance in biological systems accurately.
Experimental Protocol: Nanomaterial Biocompatibility Testing
Objective: To evaluate the biocompatibility and potential cytotoxicity of engineered nanomaterials using in vitro models.
Materials:
- Nanomaterial suspension (sterile)
- Relevant cell lines (e.g., HEK293, HepG2, or primary cells)
- Complete cell culture medium
- 96-well tissue culture plates
- MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide)
- DMSO (Dimethyl sulfoxide)
- Microplate reader
Methodology:
- Seed cells in 96-well plates at a density of 1×10⁴ cells/well and incubate for 24 hours to allow attachment.
- Prepare serial dilutions of the nanomaterial in complete culture medium (typically 0.1-100 μg/mL range).
- Replace culture medium with nanomaterial suspensions and incubate for 24-72 hours.
- Add MTT reagent (0.5 mg/mL final concentration) and incubate for 4 hours.
- Carefully remove medium and dissolve formed formazan crystals in DMSO.
- Measure absorbance at 570 nm using a microplate reader.
- Calculate cell viability relative to untreated controls.
Data Interpretation: Dose-response curves should be generated to determine IC₅₀ values. Additional assays including oxidative stress measurement (ROS detection), apoptosis assays (Annexin V staining), and inflammatory response evaluation (cytokine profiling) provide complementary safety data [59].
Figure 1: Biocompatibility Testing Workflow
Biological Considerations and Barrier Navigation
Overcoming Biological Barriers
Effective nanomedicine design must account for numerous biological barriers that impede therapeutic delivery. The reticuloendothelial system (RES) rapidly clears untargeted nanoparticles from circulation, while specialized barriers like the blood-brain barrier (BBB) present formidable challenges for neurological applications [59]. Strategic surface modifications, including PEGylation and the incorporation of targeting ligands, can mitigate RES clearance and enhance accumulation at disease sites. Understanding protein corona formation—the spontaneous adsorption of proteins onto nanoparticle surfaces—is crucial as this corona defines biological identity and cellular interactions.
Immunological Considerations
Nanomaterial interactions with the immune system present both challenges and opportunities. Unmodified nanomaterials may trigger unintended immune activation, oxidative stress, or inflammatory responses [59]. Conversely, deliberate engineering can harness these interactions for vaccine development or immunotherapy applications. Preclinical assessment must include comprehensive immunotoxicity evaluation using both in vitro (macrophage uptake assays, complement activation) and in vivo models (rodent and non-rodent species where appropriate).
Table 2: Key Research Reagent Solutions for Nanomedicine Translation
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| Surface Modification Agents | Polyethylene glycol (PEG), Poly(sarcosine), Polysorbate 80 | Enhance circulation time, reduce immunoclearance |
| Targeting Ligands | Folate, Transferrin, RGD peptides, Aptamers | Enable specific tissue/cell recognition |
| Characterization Tools | Dynamic Light Scattering (DLS) instruments, Electron Microscopy, HPLC | Physicochemical property analysis |
| Biological Barrier Models | Caco-2 cells (intestinal), MDCK cells (renal), BBB co-culture systems | Predict in vivo behavior and permeability |
| Contrast Agents | Gadolinium chelates, Quantum dots, Gold nanoparticles | Imaging and tracking applications |
Preclinical to Clinical Transition
Animal Model Selection and Efficacy Assessment
The transition from in vitro models to in vivo systems requires careful consideration of animal models that accurately recapitulate human disease pathophysiology. Selection criteria should include biological relevance, immunological compatibility, and practical considerations related to nanomaterial administration and monitoring. Orthotopic tumor models, genetically engineered animals, and humanized mouse models provide valuable platforms for evaluating targeting efficiency, biodistribution, and therapeutic efficacy. Dosage escalation studies should establish both efficacy and initial safety parameters, with particular attention to organ-specific accumulation and potential toxicities.
Regulatory Pathway and Safety Pharmacology
Navigating regulatory requirements demands rigorous safety assessment beyond standard pharmaceutical evaluation. The unique properties of nanomaterials necessitate specialized toxicology studies addressing potential issues not encountered with conventional drugs, including:
- Pharmacokinetics and Biodistribution: Comprehensive ADME (Absorption, Distribution, Metabolism, Excretion) profiling using radiolabeled or fluorescently tagged nanoparticles.
- Toxicological Evaluation: Repeat-dose toxicity studies in relevant species, with extensive histological examination of RES organs (liver, spleen, kidneys) and potential target tissues.
- Immunotoxicity Assessment: Evaluation of complement activation, cytokine release, and hypersensitivity responses.
- Degradation and Clearance: Analysis of biodegradation pathways and potential accumulation in tissues.
Figure 2: Regulatory Pathway for Nanotherapeutics
Clinical Implementation and Monitoring
Scale-up and Good Manufacturing Practice (GMP)
Successful clinical translation requires transitioning from laboratory-scale synthesis to GMP-compliant manufacturing. This scale-up process must maintain critical quality attributes (CQAs) including particle size distribution, surface characteristics, and drug loading efficiency. Process Analytical Technology (PAT) frameworks enable real-time monitoring and control of critical process parameters (CPPs) to ensure product consistency [59]. Manufacturing controls must address nanomaterial-specific challenges such as aggregation, stability during storage, and sterilization validation, as conventional methods like autoclaving may alter nanomaterial properties.
Clinical Trial Design Considerations
Clinical trials for nanomedicines require special considerations beyond conventional drug trial designs:
- Patient Selection: Biomarker-based stratification may be necessary for targeted therapies.
- Dosing Regimens: Altered pharmacokinetics may require modified dosing schedules.
- Imaging and Monitoring: Incorporation of advanced imaging modalities to track distribution and target engagement.
- Safety Endpoints: Extended monitoring for potential nanomaterial-specific adverse events.
Standardized protocols must evolve within regulatory frameworks to ensure nanomedicine safety and effectiveness during approval, with attention to the complex and costly production processes that can act as barriers to large-scale production [59].
The clinical translation of nanomedicine represents a multidisciplinary endeavor requiring seamless integration of material science, biology, and clinical medicine. As the field advances, key areas for continued development include the standardization of characterization methodologies, harmonization of regulatory requirements across jurisdictions, and implementation of quality-by-design principles throughout development. The integration of artificial intelligence in nanomaterial design and patient selection holds promise for accelerating development timelines and personalizing nanotherapeutic approaches. Furthermore, continued dialogue between researchers, clinicians, regulators, and industry partners is essential to overcome translation barriers and fully realize the potential of nanotechnology in medicine.
Conclusion
The systematic understanding of nanoscale biological interactions provides a powerful foundation for revolutionizing biomedical applications, particularly in targeted drug delivery. The integration of fundamental principles with advanced engineering strategies—from traditional surface modifications to innovative biomimetic approaches—enables the rational design of nanoplatforms with enhanced specificity, reduced immunogenicity, and improved therapeutic outcomes. Future directions will focus on developing increasingly sophisticated multifunctional systems that leverage cellular agency through non-genetic engineering, personalized nanomedicines tailored to individual patient profiles, and smart nanoparticles capable of dynamic response to biological cues. As characterization techniques and predictive models continue to advance, the translation of these nano-bio insights into clinical practice will accelerate, ultimately enabling unprecedented precision in disease diagnosis and treatment while addressing critical challenges in biocompatibility, manufacturing scalability, and regulatory approval.
References
- 1. Data-Driven Prediction of Nanoparticle Biodistribution from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312149/]
- 2. Engineering bioactive surfaces on nanoparticles and their ... [https://www.nature.com/articles/s41598-020-75465-z]
- 3. Exploring the complex interactions of nanoparticles within ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389424003790]
- 4. Recent advances in surface decoration of nanoparticles ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2024.1456939/full]
- 5. Exposure to metal nanoparticles changes zeta potentials of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9676555/]
- 6. Density of surface charge is a more predictive factor of the ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-020-00747-7]
- 7. Intermolecular forces at the interface between NPs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547760/]
- 8. The Importance of Hydrophobicity in Directing Biological ... [https://www.sciencedirect.com/org/science/article/pii/S1525779722000526]
- 9. Hydrophobic Interaction: A Promising Driving Force for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7435255/]
- 10. Understanding the synergistic effect of physicochemical ... [https://www.nature.com/articles/s42003-020-0917-1]
- 11. A review on protein corona formation on nanoparticles and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325009317]
- 12. Biomolecular Transformations Shape the Environmental Fate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590469/]
- 13. Protein corona formed on lipid nanoparticles compromises ... [https://www.nature.com/articles/s41467-025-63726-2]
- 14. The Protein Corona Paradox: Challenges in Achieving ... [https://www.mdpi.com/2313-7673/10/5/276]
- 15. Predicting the protein corona on nanoparticles using random ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d5na00425j]
- 16. Engineered protein corona sustains stealth functionality of ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03565-x]
- 17. Multiplexed Nanoparticle Protein Corona Enables Accurate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604036/]
- 18. Engineering biological interactions on the nanoscale - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6494728/]
- 19. Engineering biological interactions on the nanoscale [https://www.sciencedirect.com/science/article/abs/pii/S0958166918301010]
- 20. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 21. Mechanistic Approaches of Internalization, Subcellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7680634/]
- 22. Quantitative Particle Uptake by Cells as Analyzed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7155048/]
- 23. Fe 2 O 3 nanoparticles are absorbed via the CLEC4E ... [https://pubs.rsc.org/en/content/articlehtml/2025/en/d5en00270b]
- 24. Nanocarrier strategies for deep tumour penetration [https://pubs.rsc.org/en/content/articlehtml/2025/lp/d5lp00154d]
- 25. Cell membrane biomimetic nanoplatforms: a new strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506577/]
- 26. Innovative nanocarriers: Synthetic and biomimetic strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362117/]
- 27. Advances in Nano-Drug Delivery for Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298278/]
- 28. Targeted and intelligent nano-drug delivery systems for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1582659/full]
- 29. Quantum life science: biological nano quantum sensors ... [https://pubs.rsc.org/en/content/articlelanding/2025/cs/d4cs00650j]
- 30. Plasma membrane folding enables constant surface area ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11244959/]
- 31. The impact of surface area per volume (SA/V) ratio on drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641123001388]
- 32. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 33. Cutting-Edge Nanoparticle Innovations in Biomedical ... [https://www.scientificarchives.com/article/cutting-edge-nanoparticle-innovations-in-biomedical-science-synthesis-applications-challenges-and-future-prospects]
- 34. Nanotechnology in medicine: a double-edged sword for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00008-2]
- 35. Beyond PEGylation: nanoparticle surface modulation for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00014-4]
- 36. Exploring the intricacies of protein–nanoparticle interaction ... [https://pubs.rsc.org/en/content/articlehtml/2025/nh/d5nh00076a]
- 37. PEGylation technology: addressing concerns, moving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020137/]
- 38. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 39. PEGylation Enhances Colloidal Stability and Promotes ... [https://www.mdpi.com/2073-4360/17/22/2979]
- 40. Interactions between functionalized PEGylated gold ... [https://www.sciencedirect.com/science/article/abs/pii/S0167732225006683]
- 41. Advances in cell membrane-coated nanoparticles [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d5bm00660k]
- 42. Cancer Cell Membrane-Coated NPs as a Biomimetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566714/]
- 43. Silver Nanoparticles for Biosensing and Drug Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110216/]
- 44. Biomimetic red blood cell membrane-coated FePt metal ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr03294f]
- 45. Cell membrane derived biomimetic nanomedicine for ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925004493]
- 46. Target-induced nanoparticle assemblies - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/ay/d5ay00413f]
- 47. Optimizing Cancer Treatment: A Comprehensive Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584355/]
- 48. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 49. Nanoparticle targeting: Review of passive and active ... [https://insidetx.com/resources/reviews/a-comprehensive-review-of-passive-and-active-nanoparticle-targeting-technics/]
- 50. Regulation of oxidative stress and inflammation caused by ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00342-1]
- 51. Probing and Enhancing Ligand-Mediated Active Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7052897/]
- 52. Image-guided strategies to improve drug delivery to tumors ... [https://www.sciencedirect.com/science/article/pii/S0006291X25010617]
- 53. Single Molecule Sensing - MPI for Medical Research [https://www.mr.mpg.de/14599619/single-molecule-sensing]
- 54. Fundamentals of Nanoscale Polymer–Protein Interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4148170/]
- 55. More than a delivery system: the evolving role of lipid-based ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04508d]
- 56. A complete guide to understanding Lipid nanoparticles (LNP) [https://insidetx.com/resources/reviews/complete-guide-to-understanding-lipid-nanoparticles-lnp/]
- 57. Advances in nanocarrier technology for drug encapsulation [https://link.springer.com/article/10.1007/s43939-025-00271-1]
- 58. Biological and evolutionary concepts for nanoscale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6680157/]
- 59. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 60. Nanomedicine revolutionizing cancer immunotherapy [https://pubs.rsc.org/en/content/articlehtml/2025/na/d5na00390c]
- 61. Research advances in the diagnosis of infectious disease by ... [https://pubs.rsc.org/en/content/articlehtml/2025/nh/d5nh00098j]
- 62. Engineered cell membrane-based nano therapies fight ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925005048]
- 63. Nanotechnology Autoimmune Disease Treatment Advances [https://www.autoimmuneinstitute.org/articles/nanotechnology-breakthroughs-in-autoimmune-disease-treatment]
- 64. Nanoscale frontiers in cancer diagnosis and therapy [https://link.springer.com/article/10.1007/s44371-025-00237-5]
- 65. Rediscovery of mononuclear phagocyte system blockade ... [https://www.nature.com/articles/s41467-024-48838-5]
- 66. Emerging strategies against accelerated blood clearance ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03209-0]
- 67. Review Biomimetic approaches against accelerated blood ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325005903]
- 68. Enhancing tumor immunotherapy with smart nanoparticles ... [https://www.sciencedirect.com/science/article/pii/S2590006425003862]
- 69. Nanomaterial toxicity: a comprehensive review of ... [https://link.springer.com/article/10.1007/s44475-025-00003-2]
- 70. Evaluation of biological functionality of biomaterial surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521315/]
- 71. Advanced surface modification techniques for titanium ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1549439/full]
- 72. Integration of Nanotechnology and Nanomaterials in ... [https://scifiniti.com/3105-0387/2/2025.0019]
- 73. A Systematic Review of Toxicity, Biodistribution, and Biosafety ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12099058/]
- 74. Advances in nanomaterials for precision drug delivery [https://pubmed.ncbi.nlm.nih.gov/40256227/]
- 75. Engineering precision nanoparticles for drug delivery [https://www.nature.com/articles/s41573-020-0090-8]
- 76. Optimizing nanoparticle-mediated drug delivery: insights from ... [https://pubs.rsc.org/en/content/articlehtml/2025/su/d4su00686k]
- 77. Nanoscale Interactions [https://www.nsf.gov/funding/opportunities/nanoscale-interactions]
- 78. Controlled Drug Release from Pharmaceutical Nanocarriers [https://pmc.ncbi.nlm.nih.gov/articles/PMC4322773/]
- 79. A brief history of long circulating nanoparticles [https://www.sciencedirect.com/science/article/pii/S0169409X22002861]
- 80. Modeling Approaches for Determination of ... [https://www.biopharminternational.com/view/modeling-approaches-for-determination-of-pharmacokinetics-pharmacodynamics]
- 81. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 82. Nanoscale profiling of evolving intermolecular interactions ... [https://www.nature.com/articles/s42004-025-01659-z]
- 83. Nanocoating Is a New Way for Biofouling Prevention [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2021.771098/full]
- 84. Robust and ultra-stable nanohesive-based solid-like slippery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593591/]
- 85. Use of Nanotechnology to Mitigate Biofouling in Stainless ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8780138/]
- 86. Nano-engineering of a thermoplastic compound with CuO ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra02611c]
- 87. Dual-functional surface coatings integrating antimicrobial and ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d5mh01132a?page=search]
- 88. Nanoscale reference and test materials for the validation of ... [https://link.springer.com/article/10.1007/s00216-024-05719-6]
- 89. Nano-bio interactions in mRNA nanomedicine [https://www.sciencedirect.com/science/article/abs/pii/S0169409X23004313]
- 90. A quantitative framework to group nanoscale and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5875420/]
- 91. Quantitative study of nanoscale precipitates in Al–Zn–Mg– ... [https://www.sciencedirect.com/science/article/abs/pii/S0921509315005213]
- 92. Method of high-order advanced lithography overlay correction ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d5na00682a]
- 93. Nanotechnology in Biomedical Applications: A Perspective [https://irispublishers.com/abeb/fulltext/Nanotechnology-in-Biomedical-Applications-A-Perspective.ID.000681.php]
- 94. Nanoparticle biodistribution coefficients: A quantitative ... [https://www.sciencedirect.com/science/article/pii/S0169409X23000236]
- 95. Visualization and quantitative analysis of nanoparticles in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2211502/]
- 96. Advances in ICP-MS-Based Nanoparticle Characterization [https://pubmed.ncbi.nlm.nih.gov/40931375/]
- 97. New light-based technology arranges cellular messengers ... [https://www.news-medical.net/news/20251118/New-light-based-technology-arranges-cellular-messengers-with-unprecedented-precision.aspx]
- 98. Fundamental Study of Nanoparticles Enabled High ... [https://escholarship.org/uc/item/21t039g3]
- 99. Advanced In Vitro Models: Opportunities and Challenges ... [https://www.lek.com/insights/hea/us/ei/advanced-vitro-models-opportunities-and-challenges-drug-development]
- 100. Advanced In Vitro Models for Preclinical Drug Safety [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763796/]
- 101. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 102. CERTAINTY 2025: The power of Model-Informed Drug ... [https://www.certara.com/blog/certainty-the-power-of-model-informed-drug-development/]
- 103. Implementing FDA's IVPT Guidance Recommendations [https://www.complexgenerics.org/education-training/implementing-fdas-ivpt-guidance-recommendations-a-step-by-step-ilustration/]
- 104. Interaction of Metallic Nanoparticles With Biomimetic Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8964527/]
- 105. Nanoplatforms for Targeted Stimuli-Responsive Drug Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000772/]
- 106. Biomaterials nanoplatform-based tumor vaccines for ... [https://www.sciencedirect.com/science/article/pii/S2452199X25002749]
- 107. Lipid polymer hybrid nanoparticles: a custom-tailored next ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01849-0]
- 108. Current update on nanoplatforms as therapeutic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7878458/]
- 109. Chemotherapeutic Drug Delivery Nanoplatform Development [https://www.mdpi.com/1422-0067/25/21/11520]
- 110. Quantifying biological heterogeneity in nano-engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440624/]
- 111. Equation learning to identify nano-engineered particle–cell ... [https://pubs.rsc.org/en/content/articlelanding/2022/nr/d2nr04668g]