Nanoscale vs. Microscale Medical Devices: A Comparative Analysis for Next-Generation Biomedical Applications
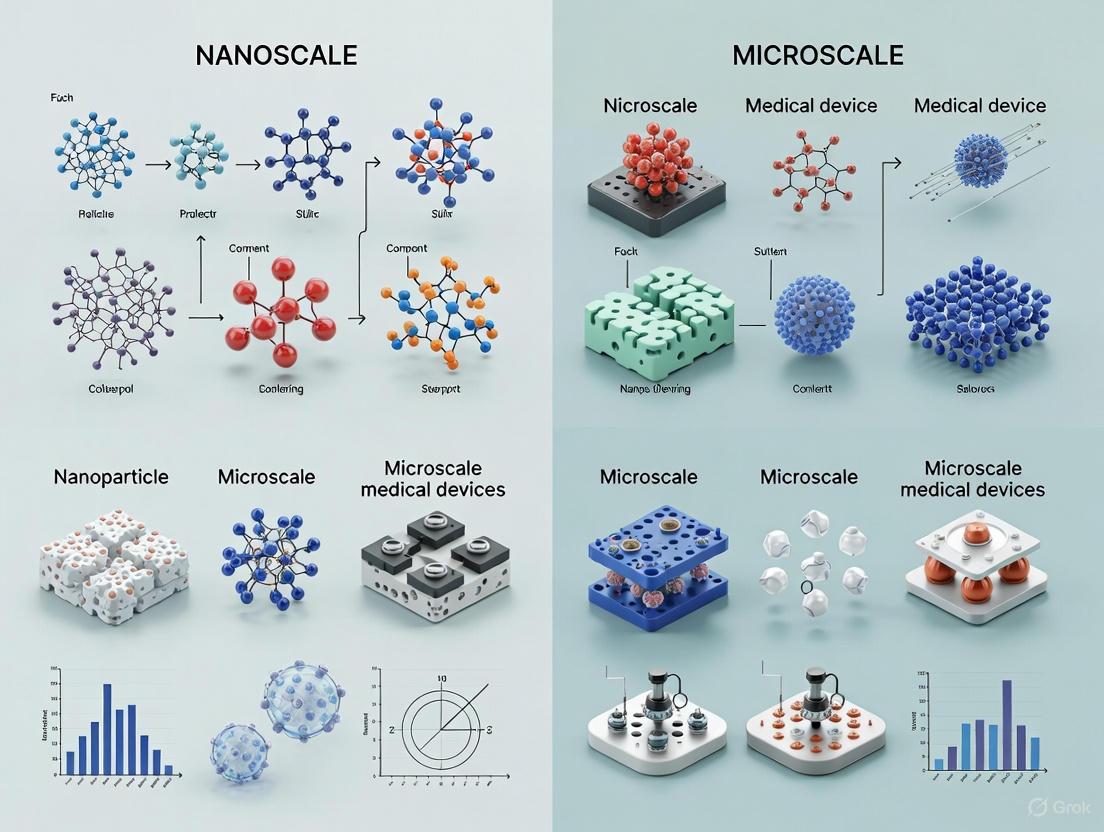
This article provides a comprehensive comparison of nanoscale and microscale medical devices, tailored for researchers, scientists, and drug development professionals.
Nanoscale vs. Microscale Medical Devices: A Comparative Analysis for Next-Generation Biomedical Applications
Abstract
This article provides a comprehensive comparison of nanoscale and microscale medical devices, tailored for researchers, scientists, and drug development professionals. It explores the fundamental principles and unique physicochemical properties that differentiate these device classes. The review details advanced fabrication methodologies, material choices, and their specific applications in targeted drug delivery, advanced diagnostics, and regenerative medicine. It further addresses critical challenges in biocompatibility, manufacturing, and regulatory navigation while offering optimization strategies. Finally, the article presents a rigorous comparative validation of performance characteristics, synthesizing key takeaways to outline future trajectories and clinical implications for the field of precision medicine.
Defining the Scale: Fundamental Principles and Properties of Micro and Nano Medical Devices
The evolution of miniaturized electromechanical systems has catalyzed revolutionary advances across numerous scientific and industrial domains, particularly in medicine and biotechnology. At the heart of this technological revolution lie two interconnected yet distinct fields: Micro-Electromechanical Systems (MEMS) and Nano-Electromechanical Systems (NEMS). These systems represent the integration of mechanical elements, sensors, actuators, and electronics on a common substrate through microfabrication technology, distinguished primarily by their dimensional scale and the physical phenomena they exploit [1]. For researchers, scientists, and drug development professionals, understanding the precise classification boundaries between MEMS and NEMS is not merely academic—it directly influences device design, material selection, fabrication methodologies, and ultimately, functional performance in biomedical applications.
This comparison guide establishes a structured framework for classifying MEMS and NEMS technologies based on dimensional parameters, material properties, transduction mechanisms, and functional capabilities. The ability to accurately categorize these systems enables more informed decisions in developing next-generation medical devices, diagnostic tools, and targeted therapeutic platforms. As the healthcare landscape increasingly embraces precision medicine, the distinction between microscale and nanoscale technologies becomes paramount in designing solutions that can operate effectively within the complex physiological environment of the human body [2] [1].
Dimensional Classification Criteria
Primary Size Parameters
The most fundamental distinction between MEMS and NEMS resides in their characteristic physical dimensions. While a straightforward size threshold provides an initial classification framework, the complete dimensional profile encompasses multiple parameters that collectively determine device categorization and functional potential.
Table 1: Dimensional Parameters for MEMS and NEMS Classification
| Parameter | MEMS Range | NEMS Range | Measurement Methodology |
|---|---|---|---|
| Characteristic Device Size | 1 mm - 100 nm [2] | 100 nm - 1 nm [2] | Scanning Electron Microscopy (SEM) |
| Layer Thickness | 1-100 μm | 1-100 nm | Profilometry, Atomic Force Microscopy (AFM) |
| Feature Resolution | 1-10 μm | 1-100 nm | Optical & Electron Microscopy |
| Surface Area to Volume Ratio | Moderate | Very High | Calculated from dimensional analysis |
The dimensional transition from MEMS to NEMS is not merely a continuation of scaling laws but represents a fundamental shift in operational principles. While MEMS devices typically function with characteristic sizes spanning from 1 millimeter down to 100 nanometers, NEMS devices operate at scales ranging from 100 nanometers down to 1 nanometer [2]. This dimensional crossover approximately at 100 nanometers is significant because it marks the scale where quantum mechanical effects may begin to influence device behavior, and surface area-to-volume ratios increase dramatically, enhancing surface-dominated phenomena crucial for sensing applications [2] [3].
Material Composition Profiles
The selection of materials for MEMS and NEMS fabrication is dictated by both functional requirements and constraints imposed by the dimensional scale. Each material class offers distinct advantages that can be leveraged for specific application domains, particularly in biomedical implementations.
Table 2: Material Composition in MEMS and NEMS
| Material Class | MEMS Applications | NEMS Applications | Key Biomedical Properties |
|---|---|---|---|
| Silicon & Derivatives | Structural components, substrates [2] | Limited due to fabrication complexity | Excellent mechanical properties, CMOS compatibility |
| Polymers (PDMS, Polyimide) | Flexible substrates, microfluidics [2] | Drug delivery carriers, responsive matrices [4] | Biocompatibility, flexibility, cost-effectiveness |
| Metals (Au, Ni, Al) | Electrodes, interconnects, thermal elements [2] | Functional nanoparticles, contrast agents | Electrical conductivity, corrosion resistance |
| Piezoelectrics (PZT, AlN) | Inertial sensors, ultrasonic transducers [2] | High-frequency resonators, energy harvesters | Direct energy conversion, precise actuation |
| 2D Materials (Graphene) | Limited use in conventional MEMS | Membranes, sensors, nanochannels [3] | Atomic thickness, exceptional strength, high sensitivity |
Material diversity increases as systems transition from conventional MEMS to NEMS platforms. Traditional MEMS have extensively utilized silicon due to its excellent mechanical properties and compatibility with complementary metal-oxide-semiconductor (CMOS) processing technology [2]. Polymers such as polydimethylsiloxane (PDMS) and polyimide are widely employed in biomedical MEMS for their biocompatibility and flexibility, making them ideal for wearable devices and lab-on-a-chip applications [2]. In contrast, NEMS increasingly leverage two-dimensional materials like graphene, which at approximately 0.335 nanometers thick represents the ultimate limit of material thickness while offering exceptional mechanical strength, chemical stability, and exceptional electrical conductivity [3]. These material characteristics enable NEMS devices with unprecedented sensitivity for detecting molecular-level interactions, a capability less pronounced in their microscale counterparts.
Fabrication Techniques and Experimental Protocols
MEMS Fabrication Methodologies
The manufacturing paradigm for MEMS predominantly relies on techniques adapted from the semiconductor industry, with modifications to accommodate three-dimensional mechanical structures and diverse material sets. The experimental workflow typically involves sequential additive and subtractive processes performed on substrate wafers.
Protocol: Surface Micromachining for MEMS
Objective: Fabricate a freestanding polysilicon micromirror structure for optical sensing applications.
Materials and Reagents:
- Substrate: Silicon wafer (4-inch diameter, <100> orientation)
- Sacrificial Layer: Phosphosilicate Glass (PSG), 2.0 μm thickness
- Structural Layer: Low-pressure chemical vapor deposition (LPCVD) polysilicon, 2.5 μm thickness
- Etchant: Buffered oxide etch (BOE, 6:1 ratio HF:NH₄F) for release
- Photoresist: AZ-5214E image reversal photoresist
- Etch Mask: Silicon nitride (Si₃N₄, 500 Å) deposited via plasma-enhanced chemical vapor deposition (PECVD)
Experimental Procedure:
- Substrate Preparation: Clean silicon wafer using standard RCA-1 and RCA-2 protocols to remove organic and ionic contaminants.
- Sacrificial Layer Deposition: Deposit PSG layer via PECVD at 350°C to a thickness of 2.0 μm.
- Photolithographic Patterning:
- Dehydrate wafer at 200°C for 30 minutes
- Spin-coat photoresist at 3000 rpm for 30 seconds (resulting thickness ~1.4 μm)
- Soft bake at 95°C for 60 seconds
- Expose through mask #1 (anchor pattern) with UV light at 365 nm, dose 140 mJ/cm²
- Develop in AZ-400K (1:4 dilution) for 60 seconds
- Anchor Etching: Transfer pattern to PSG layer using BOE with etch rate of 100 nm/min, followed by resist stripping in acetone and isopropanol.
- Structural Layer Deposition: Deposit LPCVD polysilicon at 580°C using silane precursor, followed by doping via phosphorus diffusion at 950°C for 30 minutes.
- Structural Layer Patterning:
- Repeat photolithography using mask #2 (mirror pattern)
- Etch polysilicon in SF₆-based plasma etch (rate 300 nm/min)
- Release Etch: Immerse structure in BOE for 45 minutes to remove sacrificial PSG layer, followed by critical point drying with CO₂ to prevent stiction.
Validation Metrics: Measure resonant frequency using laser Doppler vibrometry (expected range: 10-50 kHz); characterize surface flatness via interferometry (<λ/10 deviation).
NEMS Fabrication Methodologies
NEMS fabrication presents significantly greater challenges due to nanoscale feature requirements, often necessitating either advanced lithographic techniques or bottom-up assembly approaches. The experimental protocols frequently combine conventional microfabrication with specialized nanofabrication processes.
Protocol: Graphene NEMS Resonator Fabrication
Objective: Realize a graphene-based nanoelectromechanical resonator for mass sensing applications.
Materials and Reagents:
- Graphene Source: CVD-grown monolayer graphene on copper foil (commercial source)
- Substrate: Silicon wafer with 300 nm thermal oxide
- Transfer Medium: Polymethyl methacrylate (PMMA, 495 kDa molecular weight)
- Etchants: Ammonium persulfate (0.1 M aqueous solution for copper etching), deionized water rinses
- Electrode Materials: Electron-beam evaporated chromium (5 nm adhesion layer) and gold (50 nm)
- Lithography: Hydrogen silsesquioxane (HSQ, XR-1541) negative tone electron-beam resist
Experimental Procedure:
- Graphene Transfer:
- Spin-coat PMMA on graphene/copper at 3000 rpm (thickness ~300 nm)
- Cure at 150°C for 1 minute
- Etch copper backing in ammonium persulfate for 4 hours at room temperature
- Transfer PMMA/graphene stack to target substrate
- Remove PMMA in acetone vapor (60°C) for 2 hours followed by 10-minute immersion in fresh acetone
- Electrode Patterning:
- Pattern alignment marks using electron-beam lithography (EBL) with HSQ resist
- Develop in 25% tetramethylammonium hydroxide (TMAH) for 1 minute
- Evaporate Cr/Au (5 nm/50 nm) and lift-off in Remover 1165 at 80°C
- Graphene Delineation:
- Pattern graphene mesa structures using EBL with HSQ as an etch mask
- Reactive ion etch graphene in O₂/Ar plasma (10 sccm/40 sccm, 100 W, 30 seconds)
- Release Process:
- Create suspension by etching underlying oxide in vapor HF for 3 minutes
- Critical point drying to prevent collapse of suspended structures
Validation Metrics: Confirm monolayer graphene quality via Raman spectroscopy (G/D peak ratio >5, symmetric 2D peak); verify suspension via AFM; measure resonance frequency using laser interferometry (expected range: 10-100 MHz).
Figure 1: NEMS Fabrication Workflow for Graphene Devices
Transduction Mechanisms and Performance Metrics
Comparative Transduction Principles
The fundamental operational principles of MEMS and NEMS devices vary significantly due to scale-dependent physical phenomena. These transduction mechanisms determine how devices interact with their environment, convert signals, and ultimately perform their intended functions in biomedical applications.
Table 3: Transduction Mechanisms in MEMS and NEMS
| Transduction Mechanism | MEMS Implementation | NEMS Implementation | Biomedical Application Examples |
|---|---|---|---|
| Piezoresistive | Silicon strain gauges [1] | Graphene piezoresistors [3] | Pressure sensors, tactile sensing |
| Capacitive | Parallel-plate sensing [1] | Nanogap capacitive sensing | Accelerometers, displacement sensors |
| Piezoelectric | PZT thin films [2] | ZnO nanowires | Energy harvesting, ultrasonic transducers |
| Optical | Micromirrors, interferometry [1] | Photonic crystals, plasmonics | Biosensors, imaging systems |
| Resonant | Silicon cantilevers (kHz-MHz) | Graphene resonators (MHz-GHz) [3] | Mass sensing, molecular detection |
Quantitative Performance Comparison
The scaling effects from micro- to nanoscale manifest as dramatic improvements in key performance metrics, particularly sensitivity, response time, and power consumption. These enhancements enable new capabilities in medical diagnostics and monitoring.
Table 4: Performance Metrics for Biomedical Sensing Applications
| Performance Metric | Typical MEMS Performance | Typical NEMS Performance | Measurement Protocol |
|---|---|---|---|
| Mass Sensitivity | ~10⁻¹² g [2] | ~10⁻²¹ g [3] | Controlled mass loading with calibrated particles |
| Power Consumption | μW-mW range | pW-nW range | Direct current measurement with source meter |
| Resonant Frequency | kHz-MHz range | MHz-GHz range [3] | Laser Doppler vibrometry or electrical readout |
| Scale Factor Stability | 10-100 ppm/°C | 1-10 ppm/°C | Environmental chamber testing (-40°C to +85°C) |
| Quality Factor (Q) in Air | 10-100 | 100-10,000 [3] | Ring-down measurement of resonant peak |
The exceptional properties of two-dimensional materials like graphene substantially enhance NEMS transducer capabilities. Graphene exhibits a pronounced piezoresistive effect with gauge factors typically ranging from 1.9 to 8.8 for chemical vapor deposition (CVD) graphene, enabling highly sensitive strain detection [3]. Furthermore, when configured as resonant structures, graphene NEMS can achieve quality factors (Q) exceeding 10,000 in vacuum conditions, significantly higher than most comparable MEMS resonators [3]. This combination of high sensitivity and exceptional resonance characteristics enables NEMS devices to detect mass changes at the zeptogram (10⁻²¹ grams) scale, sufficient for identifying individual molecules or molecular interactions—a capability with profound implications for molecular diagnostics and drug discovery [2] [3].
Biomedical Applications: Comparative Analysis
Diagnostic and Monitoring Applications
The dimensional and performance characteristics of MEMS and NEMS directly influence their suitability for specific biomedical applications, with each domain offering distinct advantages depending on diagnostic requirements and physiological constraints.
Table 5: Medical Diagnostic and Monitoring Applications
| Application Domain | MEMS Solutions | NEMS Solutions | Key Differentiating Factors |
|---|---|---|---|
| Lab-on-a-Chip Diagnostics | Microfluidic channels, pumps, valves [2] | Nanofluidic channels for single biomolecule analysis | Sample volume requirements, resolution |
| Implantable Sensors | Glucose monitors, intracranial pressure sensors [1] | Cellular-level monitors, neural probes | Size constraints, biocompatibility challenges |
| Medical Imaging | Ultrasound transducers, optical coherence tomography [2] | Enhanced contrast agents, molecular imaging | Resolution limits, penetration depth |
| Point-of-Care Diagnostics | Portable blood analyzers, sweat sensors | Single-molecule detection chips | Sensitivity requirements, cost considerations |
| Wearable Health Monitors | Activity trackers, continuous glucose monitors [1] | Epidermal electronics, smart contact lenses | Form factor, power consumption |
Therapeutic and Surgical Applications
Beyond diagnostics, MEMS and NEMS technologies enable increasingly sophisticated therapeutic interventions, from targeted drug delivery to minimally invasive surgical procedures, each leveraging scale-specific advantages.
Table 6: Therapeutic and Surgical Applications
| Application Domain | MEMS Solutions | NEMS Solutions | Clinical Benefits |
|---|---|---|---|
| Targeted Drug Delivery | Implantable microreservoirs with valves [2] | Nanoparticle-based delivery systems [5] | Specificity of targeting, dosing control |
| Surgical Robotics | Micromechanical instruments, force feedback [4] | Nanoscale end-effectors, cellular manipulation | Precision, minimal tissue damage |
| Tissue Engineering | Scaffolds with micro-scale features | Nanofiber scaffolds with biochemical signaling | Biomimetic architecture, cellular integration |
| Neuromodulation | Microelectrode arrays for neural stimulation | Nanowire-based neural interfaces [4] | Resolution, long-term stability |
| Minimally Invasive Surgery | Endoscopic tools, capsules | Cellular-level surgery, nanoscale manipulation [5] | Recovery time, procedural precision |
The application of hydrogel-based micro/nano-robotic medical devices exemplifies the convergence of MEMS and NEMS principles for therapeutic purposes. These devices feature three-dimensional crosslinked networks integrated with responsive chemical functional groups, enabling them to undergo structural and functional transitions under various external stimuli, including chemical energy, temperature, light, pH, ultrasound, magnetic fields, and ions [4]. Such multi-actuation synergistic strategies combine the physical orientation capability of magnetic nanoparticles with photothermal materials like gold nanoparticles, allowing for precise regulation of hydrogel network structure and drug release kinetics with potential targeting accuracy at the cellular level [4]. This "external navigation combined with internal response" design represents a sophisticated approach that transcends traditional scale boundaries in medical devices.
Figure 2: Multi-Actuation Mechanism in Biomedical Nano/Micro Devices
The Researcher's Toolkit: Essential Materials and Reagents
The experimental protocols for developing and characterizing MEMS and NEMS devices require specialized materials and reagents that enable precise fabrication and functionalization. The following toolkit represents essential resources for researchers working in this interdisciplinary field.
Table 7: Essential Research Reagent Solutions for MEMS/NEMS Fabrication
| Reagent/Material | Function | Key Suppliers | Handling Considerations |
|---|---|---|---|
| SU-8 Photoresist | High-aspect-ratio MEMS structures | Kayaku Advanced Materials | Requires optimized UV exposure and post-bake |
| Polydimethylsiloxane (PDMS) | Microfluidics, flexible substrates | Dow Silicones | Base:curing agent 10:1 ratio, degas before use |
| CVD Graphene | NEMS resonators, sensors | Graphenea, Beijing Graphene Institute | PMMA-assisted transfer, avoid tearing |
| HSQ XR-1541 | Negative tone e-beam resist for NEMS | Dow Silicones | Sensitive to environmental contamination |
| Buffered Oxide Etch (BOE) | Silicon oxide etching for release | Sigma-Aldrich, KMG Chemicals | Teflon containers, precise timing critical |
| Tetramethylammonium Hydroxide (TMAH) | Silicon anisotropic etching | Sigma-Aldrich | 25% concentration, 80°C for <100> Si etch |
| Parylene C | Biocompatible conformal coating | Specialty Coating Systems | CVD deposition, excellent barrier properties |
The classification of micro- and nano-electromechanical systems according to dimensional boundaries reveals a sophisticated technological ecosystem where scale dictates application potential. MEMS devices, with their characteristic dimensions spanning from 1 millimeter down to 100 nanometers, provide robust platforms for medical monitoring, implantable sensors, and microfluidic diagnostic systems [2]. In contrast, NEMS devices, operating at scales from 100 nanometers down to 1 nanometer, offer unprecedented sensitivity for molecular detection, targeted therapeutic delivery, and cellular-level interventions [2] [3].
For researchers and drug development professionals, this dimensional classification provides a strategic framework for technology selection based on application requirements. MEMS technologies offer maturity, reliability, and integration capabilities well-suited for physiological monitoring, diagnostic platforms, and therapeutic delivery systems where microscale interactions are sufficient [1]. Meanwhile, NEMS platforms, though less mature in their development pipeline, enable fundamentally new capabilities in precision medicine through their ability to interact with biological systems at molecular scales, offering potential breakthroughs in early disease detection, highly targeted therapeutic interventions, and fundamental biological research [3] [5].
The ongoing convergence of MEMS and NEMS technologies with advanced materials, artificial intelligence, and wireless connectivity heralds a new era in biomedical devices that will progressively blur these dimensional boundaries [1]. As the field advances, the most impactful innovations will likely emerge from strategic applications of both microscale and nanoscale principles to create integrated systems that leverage the unique advantages of each domain, ultimately enabling more precise, personalized, and effective healthcare solutions.
The evolution of medical devices is intrinsically linked to advancements in materials science, particularly at micro- and nanoscales. Micro-Electro-Mechanical Systems (MEMS) combine mechanical elements, sensors, actuators, and electronics on a common silicon substrate through microfabrication, with characteristic sizes from 1 mm to 100 nm [2]. Scaling down further to Nano-Electro-Mechanical Systems (NEMS), within the 100 nm to 1 nm range, offers greater sensitivity and new functionalities for biomedical applications [2]. The choice of material—silicon, polymers, metals, or piezoelectrics—fundamentally dictates a device's performance, biocompatibility, and integration potential within the human body. This guide objectively compares these material families, providing researchers and drug development professionals with critical data and methodologies to inform the design of next-generation medical devices.
Material Performance Comparison
Critical Properties at a Glance
The selection of a base material is a foundational decision in device design. The following table provides a quantitative comparison of key properties across the four material families.
Table 1: Comparative Properties of Key Materials in Medical Device Fabrication
| Material Family | Example Materials | Young's Modulus (GPa) | Key Strengths | Primary Limitations | Common Fabrication Methods |
|---|---|---|---|---|---|
| Silicon | Single-crystal silicon (SCS), Silicon Carbide (SiC) | ~130-185 (SCS) [2] | Superior mechanical properties, CMOS compatibility, high precision [2] | Brittleness, heat sensitivity [2] | Photolithography, bulk/surface micromachining [2] |
| Polymers | PDMS, Polyimide, SU-8, Parylene C | 0.00057-3 (PDMS) [2] | Biocompatibility, flexibility, low cost, ease of processing [2] | Low thermal stability, challenging dimensional control [2] | Additive manufacturing, soft lithography, deposition [2] |
| Metals | Gold, Nickel, Aluminum, Ni-Cu alloys | ~70 (Au), ~200 (Ni) [2] | Excellent electrical conductivity, durability, corrosion resistance (Au) [2] | Can be heavy, potential cytotoxicity (Ni) | Electrodeposition, sputtering, ICP etching [2] |
| Piezoelectrics | PZT, PVDF, AlN, BaTiO₃ | ~63 (PZT ceramic) [6] | Self-powering (energy harvesting), precise actuation, high sensitivity sensing [2] [6] | Brittleness (ceramics), lower output (polymers), lead toxicity (PZT) [6] [7] | Screen printing, sol-gel, 3D printing, thin-film deposition [6] [7] |
Application-Based Performance Analysis
Material performance must be evaluated in the context of specific applications. The following analysis is based on demonstrated use cases in peer-reviewed literature and commercial reports.
Table 2: Application-Oriented Performance of Material Families
| Application | Superior Material Family | Experimental Performance Data | Comparative Analysis |
|---|---|---|---|
| High-Precision Sensors/Actuators | Silicon & Piezoelectrics | Piezoresistive Si sensors: ΔR/R = πσ (π: piezoresistive coeff.) [1]. Capacitive MEMS: C = εA/d for inertial measurement [1]. | Silicon excels in miniaturized, on-chip integration. Piezoelectrics offer direct energy conversion (sensing/actuation) with high frequency response [2]. |
| Wearable/Flexible Devices | Polymers & Polymer-based Piezoelectrics | PVDF & its copolymers: Flexible, biocompatible, lower piezoelectric coefficient (d₃₃) than PZT but sufficient for wearables [6]. | Polymers (e.g., PDMS) provide substrate flexibility and comfort. PVDF enables mechanical energy harvesting from body movements [1] [6]. |
| Biocompatible Implants | Specific Polymers & Metals | Gold: Corrosion-resistant, biocompatible for biomedical sensors [2]. Polyimide: Biocompatible, used in flexible electronics and lab-on-a-chip [2]. | Gold is ideal for chronic implants requiring stable interfaces. Polymers like polyimide and PLLA offer flexibility and long-term biostability [2] [6]. |
| Energy Harvesting | Piezoelectrics | PZT: High piezoelectric coeff., but rigid [6]. 3D-printed flexible piezoelectrics: Convert multi-directional stress to energy [7]. | Ceramics (PZT) offer high power density. Emerging flexible/organic materials (PVDF, PLLA) enable harvesting from soft, dynamic tissues [6] [7]. |
Experimental Protocols for Material Evaluation
Protocol 1: Piezoresistive Sensing Characterization
Objective: To quantify the sensitivity and linearity of a piezoresistive material (e.g., silicon) by measuring its change in electrical resistance under applied mechanical strain [1].
Materials & Reagents:
- Piezoresistive Cantilever: A silicon-based microfabricated beam with integrated strain gauge.
- Precision Micropositioning System: To apply controlled deflection.
- Source Meter Unit (SMU): To measure electrical resistance (e.g., Keithely 2400).
- Wheatstone Bridge Circuit: For high-sensitivity resistance measurement [1].
- Vibration Isolation Table: To minimize external noise.
Methodology:
- Setup: Mount the piezoresistive cantilever firmly at one end. Connect the strain gauge to the Wheatstone bridge circuit and SMU.
- Calibration: Zero the measurement by balancing the Wheatstone bridge with no applied force.
- Application of Strain: Use the micropositioner to deflect the free end of the cantilever in controlled increments. The induced stress (σ) and strain (ε) cause deformation in the sensing element.
- Data Acquisition: At each deflection step, record the change in electrical resistance (ΔR) via the SMU. The fundamental relationship is ΔR/R = πσ, where π is the piezoresistive coefficient and R is the baseline resistance [1].
- Analysis: Plot the applied strain (ε) against the normalized resistance change (ΔR/R). The slope of the linear region provides the Gauge Factor (GF = (ΔR/R)/ε), a key metric of sensitivity.
Protocol 2: Piezoelectric Energy Harvesting Output Assessment
Objective: To evaluate the voltage and power output of a piezoelectric material in an energy harvesting configuration for powering low-energy devices [6] [7].
Materials & Reagents:
- Piezoelectric Device: A defined sample (e.g., PZT ceramic disc, flexible PVDF film).
- Electrodynamic Shaker: To simulate controlled, cyclic mechanical vibrations.
- Oscilloscope: To measure the open-circuit output voltage (V₀₀).
- Variable Load Resistor Box: To determine power output across different loads.
- Laser Vibrometer: To precisely measure the input mechanical displacement/acceleration.
Methodology:
- Setup: Fix the piezoelectric sample to the shaker. Connect its electrodes to the oscilloscope and the resistor box in parallel.
- Input Calibration: Activate the shaker at a fixed frequency and amplitude. Use the vibrometer to confirm the input mechanical conditions.
- Open-Circuit Measurement: Under steady-state vibration, measure the peak-to-peak open-circuit voltage (V₀₀) on the oscilloscope.
- Power Optimization: Connect the variable load resistor. For a range of resistance values (Rₗₗ), measure the root-mean-square voltage (Vᵣₘₛ) across the resistor. Calculate output power for each point using P = Vᵣₘₛ² / Rₗₗ.
- Analysis: Plot power (P) versus load resistance (Rₗₗ). The peak of this curve indicates the matched load impedance and maximum power output (Pₘₐₓ) of the harvester. The piezoelectric charge coefficient d can be inferred from the relationship between input stress and generated charge [6].
Research Reagent Solutions: The Scientist's Toolkit
Table 3: Essential Materials and Reagents for Device Fabrication and Testing
| Item | Function/Application | Key Characteristics |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Fabrication of flexible substrates, microfluidic channels, and wearable devices [2]. | Biocompatible, elastomeric, transparent, gas-permeable. |
| Lead Zirconate Titanate (PZT) | High-performance actuators, sensors, and ultrasonic transducers [2] [7]. | High piezoelectric coefficient, but contains lead (toxic). |
| Polyvinylidene Fluoride (PVDF) | Flexible piezoelectric sensors and energy harvesters for wearable applications [6]. | Biocompatible polymer, flexible, lower piezoelectric output than PZT. |
| SU-8 Epoxy Resist | Creates high-aspect-ratio microstructures for MEMS and microfluidics [2]. | Negative-tone photoresist, highly cross-linked, chemically resistant. |
| Gold Sputtering Target | Deposition of biocompatible electrodes and conductive traces for implants [2]. | High conductivity, excellent corrosion resistance, and biocompatibility. |
| Silicon-on-Insulator (SOI) Wafers | Base substrate for fabricating high-precision, monolithic MEMS sensors and actuators [2]. | Provides a single-crystal silicon device layer, ideal for complex micromachining. |
Visualizing Material Selection and Experimental Workflows
Decision Pathway for Material Selection
The following diagram outlines a logical workflow for selecting a material family based on primary device requirements, helping researchers navigate the initial design phase.
Diagram 1: A decision pathway for selecting a core material family based on key device requirements.
Piezoresistive Sensor Characterization Workflow
This diagram details the experimental workflow for characterizing a piezoresistive sensor, as described in Protocol 1.
Diagram 2: Step-by-step workflow for the piezoresistive sensor characterization protocol.
In the evolving landscape of medical technology, the distinction between microscale and nanoscale devices is foundational, driving paradigm shifts in diagnostic, therapeutic, and regenerative medicine. Micro-electromechanical systems (MEMS) are typically characterized by dimensions spanning from 1 millimeter down to 100 nanometers, integrating electrical and mechanical components for patient monitoring, diagnosis, and treatment [8]. In contrast, nano-electromechanical systems (NEMS) and nanomaterials operate on a scale of 100 nanometers down to 1 nanometer, a realm where fundamental material properties become dominated by surface and quantum phenomena rather than bulk composition [8] [9]. This comparison guide objectively analyzes how these distinct physicochemical properties—specifically surface area-to-volume ratio, quantum effects, and chemical reactivity—govern the performance, application, and regulatory considerations of medical devices at these different scales, providing researchers with critical data for technology selection and development.
Comparative Analysis of Fundamental Properties
The transition from the micro- to the nanoscale precipitates a fundamental shift in material behavior. These changes are not merely geometric but represent alterations in the very physical laws governing the materials, with direct implications for their performance in medical devices.
Surface Area-to-Volume Ratio
The surface area-to-volume ratio (SA:V) exhibits a non-linear increase as material dimensions decrease, following an inverse power law [10]. This relationship is the primary driver behind many of the unique properties observed at the nanoscale.
- Nanoscale Behavior: At dimensions below 100 nm, the SA:V ratio increases dramatically [11] [10]. This means a significantly larger proportion of the material's atoms or molecules are positioned on the surface rather than in the interior. In biomedical applications, this vast surface area enables more extensive interactions with biological entities, such as proteins, cells, and tissues, which is critical for enhancing drug loading capacity in delivery systems, improving catalytic efficiency in diagnostic assays, and accelerating tissue integration in implants [11].
- Microscale Behavior: MEMS devices, with characteristic dimensions from 100 nm to 1 mm, possess a considerably lower SA:V ratio compared to their nanoscale counterparts [8]. While this reduces their intrinsic chemical reactivity, it provides superior structural integrity for mechanical components such as microgears, cantilevers, and membranes used in sensors and actuators [8].
Table 1: Quantitative Impact of Scale on Surface-Dominated Properties
| Property | Nanoscale Devices & Materials | Microscale Devices (MEMS) |
|---|---|---|
| SA:V Ratio Trend | Very high; increases exponentially with decreasing size [11] [10] | Moderate; scales inversely with size [8] |
| Impact on Drug Loading | High capacity for therapeutic conjugation and encapsulation due to extensive surface [11] | Limited primarily to micro-reservoirs in drug delivery systems [8] |
| Structural Role | Often requires scaffolding or composite integration for macroscopic stability [11] | Provides primary structural components (e.g., silicon cantilevers, gears) [8] |
| Catalytic Efficiency | Exceptional due to high density of active surface sites [10] | Not a primary function; surfaces often serve as passive platforms |
Quantum Confinement and Optical Effects
Quantum mechanical effects become pronounced when material dimensions approach the de Broglie wavelength of electrons, typically in the low nanometer range. This leads to size-tunable properties not found in microscale materials or bulk solids.
- Nanoscale Quantum Phenomena: Semiconductor nanocrystals, known as quantum dots (QDs), exhibit a direct relationship between their physical size and their optoelectronic properties due to the quantum confinement effect [12] [10]. As the size of the QD decreases, the energy band gap increases, resulting in a shift of both absorption and emission spectra to higher energies (a blue shift) [12]. This allows researchers to "fine-tune" the photoluminescence emission of QDs from the UV to the infrared simply by controlling their size during synthesis [12] [10]. For instance, CdSe QDs can emit across the 450-650 nm range, while CdTe QDs can extend into the near-infrared (500-750 nm), which is crucial for deep-tissue imaging [12].
- Microscale Optical Properties: The optical properties of materials used in MEMS, such as silicon, polymers, and metals, are inherently bulk properties. They are determined by the material's composition and crystal structure but cannot be precisely tuned by varying the device's physical dimensions [8]. Their applications in devices are typically structural or electronic (e.g., waveguides, reflectors) rather than active luminescent probes.
Figure 1: Quantum Confinement Mechanism leading to size-tunable optical properties in nanoscale semiconductors, a phenomenon absent in microscale devices and bulk materials.
Table 2: Experimental Optical Data for Size-Tunable Quantum Dots
| Quantum Dot Core | Size Range (nm) | Emission Wavelength Range (nm) | Key Application in Medical Devices |
|---|---|---|---|
| CdSe | 2 - 6 | 450 - 650 [12] | Multiplexed bioimaging and biosensing [12] |
| CdTe | 2.5 - 7 | 500 - 750 [12] | Deep-tissue imaging (NIR-I window) [12] |
| InP/ZnS | ~3 - 6 | 530 - 650 [12] | Heavy-metal-free bioimaging [12] |
| CdSe/ZnS (Core/Shell) | 3 - 7 | 520 - 670 [12] | Enhanced brightness and stability for diagnostics [12] |
Chemical Reactivity and Catalytic Activity
The dramatic increase in surface energy and the presence of coordinatively unsaturated surface atoms make nanomaterials significantly more reactive than microscale materials of the same composition.
- Nanoscale Reactivity: The high density of surface atoms acts as active sites for chemical reactions, dramatically enhancing catalytic efficiency and chemical reactivity [11] [10]. A prime example is silver, where nanoparticles exhibit potent antimicrobial properties not seen in bulk silver due to this increased reactivity [9]. This property is exploited in wound dressings and coatings for medical devices to prevent infection. Furthermore, the melting point of nanocrystals is dramatically lowered, and their solubility is greatly enhanced compared to bulk materials [10].
- Microscale Reactivity: The chemical reactivity of microscale materials is substantially lower and aligns more closely with bulk material behavior [8]. While surface treatments (e.g., plasma activation, chemical etching) can enhance reactivity for specific applications like bonding or adhesion, the intrinsic catalytic potential is minimal compared to nanomaterials. MEMS devices primarily rely on their mechanical and electrical properties rather than their chemical reactivity for function [8].
Experimental Protocols for Property Characterization
Protocol: Quantifying Surface Area via BET Analysis
The Brunauer-Emmett-Teller (BET) method is the gold standard for determining the specific surface area of porous and nanoscale materials.
- Sample Preparation: Pre-treat the nanomaterial (e.g., quantum dots, metal nanoparticles) or microscale powder by degassing under vacuum at an elevated temperature (e.g., 150°C for 2 hours) to remove adsorbed contaminants and moisture [12].
- Gas Adsorption: Cool the sample to cryogenic temperature (typically liquid N₂ at 77 K). Under controlled conditions, expose the sample to incremental doses of an inert adsorbate gas, usually nitrogen (N₂), and measure the quantity of gas adsorbed at each relative pressure (P/P₀) [10].
- Data Analysis: Apply the BET equation to the adsorption data within the relative pressure range of 0.05-0.30 P/P₀. The linearized form of the equation is used to calculate the monolayer volume (V_m) of adsorbed gas.
- Surface Area Calculation: The specific surface area (SBET) is calculated using the formula: ( S{BET} = \frac{Vm N A{cs}}{V0 m} ), where ( N ) is Avogadro's number, ( A{cs} ) is the cross-sectional area of the adsorbate molecule (0.162 nm² for N₂), ( V_0 ) is the molar volume of gas, and ( m ) is the mass of the sample. Expected outcomes show nanomaterials like mesoporous silica nanoparticles can exhibit surface areas >500 m²/g, vastly exceeding those of microscale particles [10].
Protocol: Measuring Quantum Confinement via UV-Vis Spectroscopy
This protocol characterizes the size-dependent optical absorption of semiconductor quantum dots.
- Sample Preparation: Prepare dilute colloidal solutions of the quantum dots (e.g., CdSe, CdTe) in a transparent solvent (e.g., toluene or water, depending on surface functionalization) [12]. For comparison, prepare a suspension of a microscale semiconductor powder (e.g., bulk CdS).
- Instrumentation Setup: Use a UV-Vis spectrophotometer with a wavelength range of at least 300-800 nm. Employ quartz cuvettes for optimal UV transmission.
- Data Acquisition: Record the absorption spectrum of each sample. For quantum dot samples of varying sizes, the absorption onset will show a clear blue shift as the particle size decreases.
- Bandgap Calculation: The Tauc plot method is used to determine the optical bandgap (E_g). Plot (αhν)² versus photon energy (hν), where α is the absorption coefficient. Extrapolate the linear region of the plot to the x-axis; the intercept provides the direct bandgap energy. Experimental data will confirm a direct correlation between decreasing QD size and increasing bandgap energy [12] [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of micro- and nanoscale medical devices rely on specialized materials and reagents.
Table 3: Key Materials and Reagents for Device Research
| Material/Reagent | Core Function | Application Example |
|---|---|---|
| Semiconductor Quantum Dots (CdSe, CdTe, InP) | Fluorescent probes with size-tunable emission and high photostability [12]. | Intracellular tracking, in vivo deep-tissue imaging, and diagnostic assays [12]. |
| Polydimethylsiloxane (PDMS) | A biocompatible, flexible polymer with high gas permeability and easy molding [8]. | Flexible substrates, microfluidic channels, and membranes in biomedical MEMS devices [8]. |
| Gold Nanoparticles & Nanorods | Biocompatible plasmonic materials for enhanced imaging, photothermal therapy, and biosensing [13] [9]. | Contrast agents, LSPR biosensors, and photothermal ablation of tumor cells [13] [9]. |
| Trioctylphosphine Oxide (TOPO) | A coordinating solvent and surface ligand in the high-temperature synthesis of quantum dots [12]. | Prevents aggregation and controls growth during QD synthesis, passivating surface defects [12]. |
| Methyl Viologen | An electrochromic reporter molecule that changes color upon reduction [13]. | Optical readout in closed bipolar electrochemistry (CBE) diagnostic sensors [13]. |
| Lead Zirconate Titanate (PZT) | A piezoelectric material that generates charge under mechanical stress and vice versa [8]. | Precision actuators, energy harvesters, and ultrasonic transducers in MEMS devices [8]. |
Performance Comparison in Medical Applications
The distinct properties of micro- and nanoscale materials dictate their suitability for specific medical applications, with implications for sensitivity, therapeutic efficacy, and regulatory pathways.
- Diagnostic Sensitivity: Nanoscale devices leveraging localized surface plasmon resonance (LSPR) in gold nanoparticles or the intense fluorescence of quantum dots offer exceptional sensitivity for detecting low-abundance biomarkers, enabling early-stage disease diagnosis [13] [12]. For example, LSPR sensors transduce subtle changes in the local dielectric environment (e.g., from biomarker binding) into a measurable shift in resonance wavelength ((\Delta\lambda)) [13]. MEMS-based sensors, while highly precise for measuring physical parameters like pressure or flow, generally lack this molecular-level sensitivity unless integrated with nanoscale recognition elements [8].
- Therapeutic Precision: Nanoscale systems enable targeted drug delivery with superior precision. They exploit the enhanced permeability and retention (EPR) effect of tumor vasculature for passive targeting and can be functionalized with ligands (e.g., antibodies, folic acid) for active targeting to specific cells [14]. This minimizes systemic toxicity and increases therapeutic efficacy. Microscale devices, such as implantable drug pumps, excel at delivering larger, localized volumes of therapeutics but cannot achieve this degree of cellular or sub-cellular targeting [8].
- Regulatory and Safety Considerations: The high reactivity and unique properties of nanomaterials necessitate stringent safety evaluations. The European Medical Device Regulation (MDR) classifies devices containing or consisting of nanomaterials as Class III (highest risk) by default, unless it can be demonstrated that the potential for internal exposure is low or negligible [15]. This is due to concerns about nanoparticle uptake, potential for organ accumulation, and induction of oxidative stress or inflammation [15] [14]. The toxicological assessment of nanostructured medical devices is particularly challenging, as traditional testing methods (e.g., device extracts) may not be representative, requiring evaluation of the nanomaterials themselves [15].
Figure 2: A decision pathway for researchers selecting between nanoscale and microscale platforms based on the primary goal of their medical device project.
The comparative analysis unequivocally demonstrates that the physicochemical properties of materials are fundamentally different at the micro- and nanoscale, leading to distinct and often complementary roles in medical devices. Nanoscale materials offer unparalleled advantages in applications demanding high surface reactivity, quantum-enabled optical tunability, and intimate interaction with biological systems for targeted diagnostics and therapy. Conversely, microscale devices provide the robust, structurally sound platforms necessary for mechanical actuation, fluid handling, and system integration. The future of medical device innovation lies in the convergent integration of these platforms, harnessing the unique strengths of each scale to create next-generation devices that are smarter, more effective, and minimally invasive. Researchers must navigate this landscape with a clear understanding of both the immense potential and the heightened regulatory and safety considerations, particularly for nanoscale constructs.
The fields of nanoscale and microscale devices are driving unprecedented innovation in modern medicine. Micro-electromechanical Systems (MEMS) typically feature components between 1 millimeter and 100 nanometers, integrating mechanical elements, sensors, actuators, and electronics on a single silicon chip. [2] In contrast, nanoscale devices operate at the 1 to 100 nanometer range, exploiting unique quantum and surface area effects that emerge at this scale. [16] This distinction is not merely dimensional; it fundamentally dictates device physics, fabrication methodologies, and ultimate biological applications. Microfluidic systems, which manipulate microliter to picoliter fluid volumes within channels narrower than a millimeter, serve as a crucial bridge between these domains, enabling the precise control necessary for both microscale analysis and nanoscale therapeutic delivery. [17]
The convergence of these technologies is creating a new paradigm in medical science. Miniaturization provides benefits including high precision, quick response times, and low production costs, while nanoscale phenomena enable novel targeting mechanisms and material properties not possible at larger scales. [2] This article provides a comprehensive comparison of these device categories, examining their respective performances, experimental validations, and specialized applications in biomedical research and therapeutic development.
Comparative Performance Analysis of Device Categories
Table 1: Performance comparison of key microfluidic device types
| Device Type | Typical Feature Size | Throughput Capacity | Key Advantages | Primary Limitations | Representative Applications |
|---|---|---|---|---|---|
| Continuous-Flow Microfluidics | 10-500 µm | Moderate | Simple design, established fabrication | Limited parallelization, laminar flow dominance | Chemical synthesis, basic bioassays [17] |
| Droplet Microfluidics | 1-100 µm (droplet diameter) | Very High (<1000 droplets/sec) | Extreme parallelization, isolated microreactors | Complex control systems, potential coalescence | Single-cell analysis, digital PCR, high-throughput screening [17] [18] |
| Digital Microfluidics (DMF) | 100-1000 µm (electrode pitch) | High | Programmable, no pumps required, individual droplet control | Limited volume range, electrode complexity | Point-of-care diagnostics, automated sample preparation [17] [18] |
| Paper-Based Microfluidics | 10-500 µm (channel width) | Low | Ultra-low cost, capillary-driven flow, disposable | Limited fluid control, higher result variability | Low-cost diagnostics, environmental sensing [17] [18] |
Table 2: Performance comparison of nanoscale vs microscale biomedical devices
| Performance Characteristic | Nanoscale Devices | Microscale Devices (MEMS) | Comparative Experimental Findings |
|---|---|---|---|
| Spatial Resolution | 1-100 nm | 100 nm - 1 mm | Nanoscale quantum dots provide superior resolution for intracellular imaging compared to microscale optical sensors [16] |
| Targeting Precision | Subcellular (e.g., nuclear targeting) [19] | Cellular to tissue level [2] | NLS-functionalized nanocarriers achieve 5.8x higher nuclear delivery compared to non-targeted versions [19] |
| Drug Delivery Efficiency | ~0.7% average tumor accumulation [19] | N/A (primarily diagnostic) | Despite targeting, nanocarriers still show low overall accumulation, highlighting delivery challenges [19] |
| Magnetic Field Sensitivity | N/A | 0.83 µT/Hz (MEMS Lorentz force sensor) [20] | MEMS magnetic sensors achieve high sensitivity without magnetic materials, avoiding hysteresis [20] |
| Power Consumption | Minimal for passive targeting | 19.5-43 mW (MEMS sensor/actuator) [20] | Smart MEMS devices can tune power consumption based on operational mode (sensing vs. actuation) [20] |
| Fabrication Complexity | High (molecular assembly) | Moderate (CMOS-compatible processes) [2] | Silicon MEMS leverages established semiconductor manufacturing [2] |
| Therapeutic Payload Capacity | Variable (5-20% loading efficiency for many nanocarriers) [21] | N/A (primarily diagnostic) | Liposomes and polymeric nanoparticles show superior drug loading compared to dendrimers and inorganic nanoparticles [21] |
Experimental Protocols and Methodologies
MEMS Sensor Performance Validation
Objective: Characterize the performance of a bi-axial Lorentz force MEMS magnetometer as both a sensor and actuator. [20]
Materials and Reagents:
- SOIMUMPs fabricated device: Structural layer of single-crystal silicon (2 µm), with patterned electrodes. [20]
- Electrothermal actuation system: DC voltage sources for thermal tuning (electrodes A-G). [20]
- Capacitive sensing setup: AC-DC voltage source (VDC + VAC = 35 V) for resonant drive (electrode H). [20]
- External magnetic field source: Capable of generating fields up to ±400 mT. [20]
- Laser Doppler vibrometer: For non-contact displacement measurement. [20]
Methodology:
- Device Characterization: Measure the native resonance frequency of the clamped-guided curved microbeam using the electrostatic actuator (electrode H) and laser vibrometer. [20]
- Electrothermal Tuning: Apply specific DC voltage combinations (detailed as "tuning cases") to the V-shaped and straight beam actuators to induce controlled axial stress in the microbeam, thereby shifting its resonance frequency. [20]
- Magnetic Sensing Mode: At 19.5 mW input power, expose the device to varying magnetic fields (±400 mT). Measure the resultant resonance frequency shift caused by Lorentz force interaction, calculating sensitivity as ~36.58% T⁻¹. [20]
- Actuator Mode: At 43 mW input power, demonstrate the device's magnetic-field-insensitive operation, achieving ~4 µm displacement with significantly reduced magnetic sensitivity (3.28% T⁻¹). [20]
- Linearity Assessment: Plot resonance frequency shift versus applied magnetic field strength to establish linear response across the measured range. [20]
Nanocarrier Targeting Efficiency Evaluation
Objective: Quantify the nuclear targeting efficiency of ligand-functionalized nanocarriers. [19]
Materials and Reagents:
- Nuclear-targeted nanocarriers: Liposomes or polymeric nanoparticles conjugated with Nuclear Localization Signals (NLS). [19]
- Control nanocarriers: Non-functionalized particles.
- Cell culture model: Appropriate cancer cell lines (e.g., HeLa, MCF-7).
- Fluorescent therapeutic cargo: Doxorubicin or model DNA plasmids tagged with fluorophores (e.g., FITC).
- Confocal microscopy setup: With image analysis software.
- Flow cytometer: For quantitative cellular uptake analysis.
Methodology:
- Nanocarrier Formulation: Prepare NLS-conjugated nanocarriers using standard bioconjugation techniques, encapsulating fluorescent cargo. Prepare identical but non-functionalized control particles. [19]
- Cell Treatment: Incubate cells with targeted and control nanocarriers at equal concentrations (e.g., 100 µg/mL) for predetermined time points (2, 4, 8 hours). [19]
- Subcellular Localization Analysis:
- Fix cells at each time point and stain nuclei with DAPI.
- Image using confocal microscopy, collecting Z-stacks to verify intra-nuclear localization.
- Quantify fluorescence co-localization of the cargo (FITC) with nuclear stains (DAPI) using specialized software.
- Uptake and Efficacy Quantification:
- Analyze cellular uptake via flow cytometry.
- Compare nuclear delivery efficiency by calculating the ratio of nuclear fluorescence in targeted versus control groups.
- Report results as fold-increase (e.g., "NLS-functionalized carriers demonstrated 5.8x higher nuclear delivery"). [19]
Diagram 1: Nuclear targeting assay workflow for evaluating nanocarrier efficiency.
Essential Research Reagents and Materials
Table 3: Key research reagents and materials for device development and evaluation
| Reagent/Material | Category | Primary Function | Research Application Examples |
|---|---|---|---|
| Polydimethylsiloxane (PDMS) | Microscale Material | Flexible substrate for microfluidics, biocompatible encapsulation | Organ-on-chip devices, wearable sensors, flexible MEMS [2] [17] |
| Polyethylene Glycol (PEG) | Nanoscale Material | Surface functionalization to reduce immune clearance ("PEGylation") | Improving nanocarrier circulation time, reducing protein adsorption [19] [21] |
| Nuclear Localization Signals (NLS) | Nanoscale Targeting Ligand | Active targeting to cell nucleus via importin-mediated transport | Nuclear-targeted drug and gene delivery systems [19] |
| Single-Crystal Silicon (SCS) | Microscale Material | Structural component for high-precision MEMS | Sensors, actuators, resonators in biomedical MEMS [2] |
| Lead Zirconate Titanate (PZT) | Microscale Material | Piezoelectric transduction for sensing/actuation | MEMS energy harvesters, ultrasonic transducers, accelerometers [2] |
| Phospholipids & Cholesterol | Nanoscale Material | Liposome formation for drug encapsulation | Biocompatible nanocarriers for therapeutic delivery [19] [21] |
| Poly(lactic-co-glycolic acid) (PLGA) | Nanoscale Material | Biodegradable polymer for controlled drug release | Sustained-release drug delivery systems [19] |
| SU-8 & Polyimide | Microscale Material | Structural polymers for micromachining | MEMS sensors, microfluidic channel fabrication [2] |
Diagram 2: Material selection logic for micro/nano device fabrication.
The comparative analysis presented herein demonstrates that the choice between nanoscale and microscale devices is fundamentally application-dependent. Microscale MEMS devices offer superior performance in physical sensing applications requiring precise mechanical transduction, with proven capabilities in magnetic field detection (0.83 µT/Hz sensitivity) and tunable multi-functionality as both sensors and actuators. [20] Conversely, nanoscale delivery systems provide unprecedented access to subcellular compartments, enabling therapeutic interventions at the molecular level through sophisticated targeting strategies like NLS conjugation. [19]
Emerging hybrid approaches that integrate both technologies show particular promise for future biomedical innovations. Microfluidic platforms naturally serve as integration frameworks, housing both MEMS sensors for environmental monitoring and nanocarriers for targeted therapeutic delivery. [17] [18] The growing integration of artificial intelligence with both nano- and micro-devices is further enhancing their analytical capabilities, enabling real-time data processing and adaptive functionality at the point of use. [22] [18] For researchers and drug development professionals, the strategic selection of device scale must consider the specific biological target, required spatial resolution, and the physical principles best suited to address the scientific question or clinical need at hand.
From Fabrication to Function: Manufacturing Techniques and Breakthrough Applications
Advanced manufacturing technologies are revolutionizing the development of medical devices, enabling new capabilities at both the micro- and nanoscales. This guide provides an objective comparison of three pivotal technologies—additive manufacturing, laser welding, and microfluidic fabrication—within the context of medical research, focusing on their performance characteristics, experimental data, and specific applications for drug development and biomedical science.
The design and manufacturing of devices at micro- and nanoscales offer significant advantages for medical applications, including high precision, rapid response times, and low production costs [2]. Micro-electromechanical Systems (MEMS) and Nano-electromechanical Systems (NEMS) represent the forefront of this miniaturization, with characteristic sizes spanning from 1 millimeter down to 1 nanometer [2].
Table: Fundamental Characteristics and Applications by Scale
| Feature | Microscale Devices | Nanoscale Devices |
|---|---|---|
| Characteristic Size | 1 mm - 100 nm [2] | 100 nm - 1 nm [2] |
| Key Manufacturing Technologies | Additive Manufacturing (FDM, SLS), Laser Welding, Microfluidic Fabrication (Hot Embossing, 3D Printing) [23] [17] | Nanomaterial Synthesis, 2D Material Fabrication, advanced BioMEMS [2] |
| Dominant Materials | Polymers (PDMS, Polyimide), Silicon, Metals (Nickel, Gold), PZT [2] | Two-dimensional materials (Graphene), nanomaterials, advanced composites [2] |
| Primary Medical Applications | Surgical guides, implant prototypes, drug delivery pumps, lab-on-a-chip diagnostics [24] [17] | Targeted drug delivery systems, advanced biosensors, nanoscale actuators [2] |
| Key Advantages | Easier to fabricate and integrate, established regulatory pathways, versatile material options [2] [25] | Enhanced sensitivity, access to unique physical phenomena, superior mechanical properties [2] |
Performance Data and Comparative Analysis
Additive Manufacturing in Medtech
Additive manufacturing (AM), or 3D printing, builds objects layer-by-layer directly from digital models, enabling complex geometries with minimal waste [23]. Its application has significantly expanded from prototyping to creating end-use parts in the medical field [24].
Table: Comparison of Key Additive Manufacturing Technologies
| Technology | Typical Materials | Tensile Strength Range | Dimensional Accuracy | Best-Suited Medical Applications |
|---|---|---|---|---|
| Fused Deposition Modeling (FDM) | Thermoplastics (PLA, ABS, TPU) [23] | 20-60 MPa [23] | ±0.5% (lower limit ±0.5 mm) [23] | Low-cost prototypes, educational models, non-sterile surgical guides [23] |
| Selective Laser Sintering (SLS) | Nylon (PA 12, PA 11), TPU [26] | 40-50 MPa [26] | ±0.3% (lower limit ±0.3 mm) [26] | Biocompatible components, surgical guides, complex ducting [26] |
| Multi-Laser Metal Printing | Titanium alloys, Cobalt-Chrome [27] | 900-1050 MPa (post-HIP) [27] | ±0.1% (lower limit ±0.1 mm) [27] | Fatigue-sensitive orthopedic implants (spine, joints) [27] |
| Electron Beam Melting (EBM) | Titanium alloys [27] | ~900 MPa [27] | ±0.2% (lower limit ±0.2 mm) [27] | Porous bone-integrating structures for implants [27] |
Key Performance Findings:
- Strength Gap: While AM can meet cast and wrought titanium specs, forging remains approximately 20-30% stronger. Advanced Hot Isostatic Pressing (HIP) cycles are being used to close this gap by improving fatigue strength and enhancing mechanical properties [27].
- Production Speed: Multi-laser systems are accelerating build times, dramatically reducing the cost per part and opening the door to new medical applications [27].
- Innovation in Metal AM: GE's Point Melt technology for EBM melts metal powder through small points instead of lines, enabling support-free production of complex geometries like porous structures, which maximizes build chamber utilization [27].
Laser Welding for Medical Devices
Laser welding provides a non-contact, high-precision joining method essential for medical devices that require cleanliness and water tightness, such as endoscopic surgical tools [28].
Table: Laser Welding Performance Specifications
| Performance Metric | Typical Specification/Data | Comparison to Traditional Methods (Adhesives/Mechanical Fasteners) |
|---|---|---|
| Weld Seam Width | < 0.2 mm [28] | Significantly narrower and more controlled. |
| Positioning Accuracy | ±0.005 mm [28] | Far superior, enabled by servo-controlled axes. |
| Water Tightness | Excellent, required for endoscopic devices [28] | Superior, as it eliminates potential leakage points from seals or adhesives. |
| Chemical Contamination | None (no adhesives) [28] | Eliminates risk of chemical contamination from bonding agents. |
| Process Monitoring | Real-time via CCD camera [28] | Enables immediate quality checks and adjustments, unlike most traditional methods. |
Microfluidic Fabrication
Microfluidics manipulates small volumes of fluids in micrometer-scale channels, forming the basis for lab-on-a-chip devices, point-of-care diagnostics, and organ-on-chip research [17]. The global market is projected to grow from USD 22.78 billion in 2024 to between USD 73.85 billion and USD 110.40 billion by the early 2030s [25] [29].
Table: Microfluidic Device Fabrication Methods and Performance
| Fabrication Method | Typical Materials | Feature Resolution | Throughput & Scalability | Primary Application Stage |
|---|---|---|---|---|
| Soft Lithography (PDMS) | Polydimethylsiloxane (PDMS) [17] | ~1 µm [17] | Low to medium; excellent for prototyping [17] | R&D, academic labs, proof-of-concept [17] |
| Hot Embossing | Thermoplastics (PMMA, PC) [25] [17] | ~10 µm [25] | High; suited for mass production [25] | Industrial-scale replication [25] |
| 3D Printing | Photopolymers, Flexdym [17] | ~50 µm [17] | Medium; rapid prototyping, custom geometries [17] | Prototyping, complex custom devices [17] |
| Injection Molding | Polymers (PS, PP) [25] | ~10-25 µm [25] | Very high; cost-effective at large volumes [25] | Mass production of commercial devices [25] |
Key Performance Findings:
- Material Shift: Polymers dominate the market due to lower cost and faster fabrication compared to silicon and glass. PDMS is widely used for prototyping, though its hydrophobic nature and potential for swelling can be limitations [2] [29].
- Market Drivers: The largest application segment is In-Vitro Diagnostics (IVD), accounting for over 50% of the market, driven by the rising demand for point-of-care testing [29].
- Integration Trends: A major trend is the integration of microfluidics with sensors, electronics, and AI to create more functional and automated devices [25] [17].
Experimental Protocols and Methodologies
Protocol: Evaluating Fatigue Strength of 3D-Printed Orthopedic Implants
Objective: To assess and improve the fatigue performance of a titanium spinal implant manufactured via Laser Powder Bed Fusion (LPBF) to meet or exceed wrought titanium specifications [27].
Materials and Reagents:
- Titanium Ti-6Al-4V ELI powder: The raw material for printing, chosen for its high strength-to-weight ratio and biocompatibility.
- Isopropyl Alcohol: Used for post-print cleaning to remove loose powder from the implant's surface and internal channels.
- Inert Gas (Argon): Provides an inert atmosphere during the printing process to prevent oxidation of the molten metal.
- HIP Vessel: The equipment used for post-processing to reduce internal porosity and enhance material density.
Methodology:
- Printing: Manufacture the implant on a multi-laser LPBF system under an argon atmosphere. Key parameters include laser power, scan speed, and layer thickness.
- Post-Processing:
- Stress Relief: Thermally treat the part to relieve internal stresses from the rapid cooling during printing.
- Hot Isostatic Pressing (HIP): Subject the implant to a defined HIP cycle (e.g., 900-1000°C under 1000+ bar argon pressure). The specific time-temperature-pressure profile is fine-tuned to maximize fatigue strength without forming a detrimental "alpha case" surface layer [27].
- Finish Machining: CNC machine critical interfaces to final dimensional tolerances.
- Testing: Subject the finished implant to cyclic loading in a simulated physiological environment (e.g., in saline at 37°C) per ASTM F1800 standards. The number of cycles to failure is recorded and compared to the minimum requirement for wrought titanium spinal implants.
Protocol: Validating Hermetic Seal of a Laser-Welded Implantable Pump
Objective: To verify the watertight integrity of a laser-welded seam on a miniature implantable drug delivery pump [28].
Materials and Reagents:
- Fiber Laser Welding System: Equipped with a high-precision rotary table and CCD visual positioning.
- Test Fluid (DI Water): A safe medium for leak testing; may be substituted with ethanol for dye-penetration tests.
- Pressure Gauge and Regulator: To apply and monitor precise internal pressure to the device.
- CCD Camera System: For real-time monitoring of the weld process and post-weld inspection.
Methodology:
- Fixture Setup: Mount the pump housing and lid in the laser welder's pneumatic chuck, ensuring coaxial alignment accuracy within ±0.005 mm [28].
- Welding: Execute the weld using pre-programmed CNC code. Parameters include a weld seam width of <0.2 mm, with the laser welder head automatically adjusting to the part's contour.
- In-Process Monitoring: The integrated CCD camera monitors the weld pool in real time to detect any instability or defects.
- Hermeticity Testing:
- Pressure Decay Test: Pressurize the welded device with air, submerge it in water, and monitor for bubbles.
- Dye Penetration Test: Apply a colored dye to the weld seam, then wipe clean and examine for any dye that has penetrated through microscopic cracks.
Protocol: Fabricating and Testing a PDMS Organ-on-a-Chip
Objective: To create a microfluidic device for culturing human liver cells under dynamic flow conditions to model drug metabolism [17].
Diagram Title: Organ-on-a-Chip Fabrication and Use Workflow
Materials and Reagents:
- PDMS Sylgard 184: A silicone elastomer kit used to create the transparent, gas-permeable microfluidic chip.
- Silicon Wafer: Serves as the master mold for patterning the microchannels.
- SU-8 Photoresist: A negative photoresist used to create the high-resolution channel patterns on the silicon wafer master.
- Oxygen Plasma Cleaner: Used to activate the PDMS and glass surfaces for irreversible bonding.
- Extracellular Matrix (e.g., Collagen): Coats the internal channels of the chip to promote cell attachment and growth.
- Human Hepatocytes: The primary liver cells used to populate the chip and model liver function.
Methodology:
- Master Fabrication: Create a silicon wafer master with the negative relief of the desired microchannels using standard photolithography with SU-8 photoresist [2] [17].
- PDMS Molding: Mix the PDMS base and curing agent (typically 10:1 ratio), pour over the master, and cure at 65°C for 2-4 hours [17].
- Device Assembly: Peel the cured PDMS off the master, punch inlet/outlet ports, and bond irreversibly to a glass slide using oxygen plasma treatment [17].
- Cell Culture: Sterilize the device, coat the main channel with collagen, and seed human liver cells into the channel. Allow cells to adhere.
- Drug Testing: Connect the chip to a peristaltic pump to create dynamic flow conditions. Introduce the drug candidate into the flow medium and collect outflow for mass spectrometry analysis to measure metabolic products.
Essential Research Reagent Solutions
Table: Key Materials and Reagents for Advanced Medical Device Manufacturing
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| PDMS (Sylgard 184) | Fabrication of microfluidic devices and organ-on-chip models [2] [17] | Biocompatible, transparent, gas-permeable, flexible; enables rapid prototyping. |
| Ti-6Al-4V ELI Powder | Raw material for 3D printing of orthopedic and cranial implants [27] | High strength-to-weight ratio, excellent biocompatibility, corrosion resistance. |
| PA 12 (Nylon 12) Powder | Material for Selective Laser Sintering (SLS) of biocompatible components [26] | Biocompatible, sterilizable, well-documented evidence for regulatory submissions. |
| SU-8 Photoresist | Creating high-aspect-ratio microstructures for MEMS and microfluidic masters [2] | High resolution, chemical resistance; forms the template for PDMS devices. |
| PZT (Lead Zirconate Titanate) | Fabrication of piezoelectric sensors, actuators, and energy harvesters in MEMS [2] | High piezoelectric coefficient, enables conversion of mechanical energy to electrical signals. |
| Medical-Grade PEEK Filament | FDM printing of patient-specific surgical guides and implants [23] | High mechanical strength, radiolucency, excellent chemical and wear resistance. |
| Polyimide | Structural material for flexible electronics and sensors in BioMEMS [2] | High chemical and thermal resilience, excellent mechanical properties. |
The ability to engineer materials at the nanoscale (1-100 nm) has revolutionized numerous scientific fields, particularly medical device research and drug development. The synthesis of nanomaterials is predominantly achieved through two fundamental philosophical approaches: top-down and bottom-up [30] [31]. The choice between these methods is a critical initial decision for researchers, as it directly influences the nanomaterial's physical properties, chemical behavior, and ultimate suitability for specific biomedical applications, such as targeted drug delivery, diagnostic imaging, or implantable devices [30] [32].
In the context of medical device development, this comparison is especially pertinent. Nanoscale devices often exhibit properties vastly different from their microscale counterparts due to increased surface area-to-volume ratios and quantum effects that emerge at the nanoscale [33] [32]. These unique characteristics can lead to enhanced biocompatibility, improved drug loading efficiency, and novel diagnostic capabilities not achievable with microscale materials. This guide provides a detailed, objective comparison of these two synthesis pathways to inform the experimental design of researchers and scientists in the field.
Fundamental Principles and Methodologies
Top-Down Approach: Sculpting from Bulk
The top-down approach involves the mechanical, chemical, or physical breakdown of bulk materials into nanostructures [31] [34]. This method can be likened to a sculptor carving a statue from a large block of marble—it begins with a larger entity and reduces it to the desired nanoscale form. The focus is on creating nanostructures through the reduction of dimensionality.
Key Experimental Protocols for Top-Down Synthesis:
- Mechanical Milling: This technique uses a planetary ball mill where a powder of the bulk material is placed in a chamber with grinding balls. The process relies on the energy transfer from the rotating or vibrating balls to the powder. Key parameters include rotating speed, ball size and quantity, ball-to-powder mass ratio, milling duration, and environment [34]. The shear forces generated during grinding fracture the particles down to the nanoscale.
- Laser Ablation: In this physical method, a high-energy laser beam is focused onto a solid target in a liquid or gas environment. At low laser flux, the absorbed energy heats the material, causing it to evaporate or sublimate. At high flux, the material is instantly converted to a plasma, which upon cooling, condenses into nanoparticles [34].
- Chemical Etching: This multi-step process begins with coating a bulk metal with a masking material (e.g., wax) to protect areas that should not be etched. The masked sample is then submerged in a chemical etchant, which selectively breaks down the molecular bonds in the exposed areas, leading to the formation of nanostructures [34].
- Sputtering: This vacuum-based process involves introducing an inert gas (e.g., Argon) into a chamber, which is then ionized and accelerated by an electric field. The resulting positively charged ions strike a solid target material, dislodging atoms. These vaporized atoms travel and deposit onto a substrate, forming a thin nanoscale film [34].
Bottom-Up Approach: Building from Atoms
In contrast, the bottom-up approach constructs nanomaterials from atomic or molecular precursors via chemical reactions or self-assembly [31] [34]. This philosophy mimics natural processes like DNA replication or protein formation, where complexity emerges from the assembly of simpler building blocks [31]. This approach emphasizes precise control over the fundamental building blocks to create the final nanostructure.
Key Experimental Protocols for Bottom-Up Synthesis:
- Sol-Gel Method: This multi-step chemical process begins with a precursor (often metal alkoxides) dissolved in a solvent to create a colloidal suspension (sol). Hydrolysis and condensation reactions then form a gel-like network. The gel is subsequently dried, often using supercritical drying to prevent collapse of the nanostructure, to produce a solid nanopowder or aerogel [34].
- Chemical Precipitation: This method involves preparing a precursor solution containing metal ions. A precipitating agent (e.g., a reducing agent) is then added, initiating a chemical reaction that causes the metal ions to form solid nanoparticles that precipitate out of the solution. The nanoparticles are separated via centrifugation or filtration and washed to remove impurities [34].
- Microwave-Assisted Synthesis: This technique places the precursor solution in a microwave reactor. The microwaves energize the molecules in the solution, causing rapid and uniform heating. This localized heating initiates and accelerates the nucleation and growth of nanoparticles, allowing for precise control over reaction kinetics [34].
- Self-Assembly: This process relies on the spontaneous organization of nanoparticles into ordered structures or patterns, driven by intermolecular forces such as van der Waals forces, hydrogen bonding, or hydrophobic effects [31] [34]. Nanoparticles are dispersed in a liquid, where they interact and arrange themselves based on their intrinsic properties, much like magnets sticking together.
The following diagram illustrates the fundamental workflows and logical relationships of these two synthesis approaches:
Performance Comparison and Experimental Data
The selection between top-down and bottom-up approaches has profound implications for the characteristics and performance of the resulting nanomaterials. The table below provides a structured, quantitative comparison based on key parameters critical for medical device and drug development applications.
Table 1: Comprehensive Comparison of Top-Down and Bottom-Up Synthesis Approaches
| Comparison Parameter | Top-Down Approach | Bottom-Up Approach |
|---|---|---|
| Fundamental Principle | Breaking down bulk materials into nanostructures [31] [34] | Building nanostructures from atoms or molecules [31] [34] |
| Key Techniques | Mechanical milling, Laser ablation, Chemical etching, Sputtering [34] | Sol-gel, Chemical precipitation, Self-assembly, Microwave-assisted synthesis [34] |
| Scalability & Cost | More suitable for mass production; can be less expensive for large quantities [31] | Can be limited by precursor availability; complex processes may increase cost [31] |
| Structural Defects | Can introduce internal stress and surface defects [30] | Produces structures with fewer defects; more uniform [30] |
| Size & Shape Control | Limited control over monodispersity and complex shapes [30] | Excellent control over size, shape, and composition [30] [31] |
| Sample Crystallinity | Can result in amorphous or polycrystalline structures [30] | Often produces highly crystalline nanostructures [30] |
| Advantages | Simpler for large-scale production; uses existing bulk materials [31] | High precision; complex architectures; better surface chemistry control [30] [31] |
| Disadvantages | Surface imperfections; material waste; limited to simple geometries [30] | Can be time-consuming; expensive precursors; potential stability issues [30] |
The experimental data underlying this comparison is derived from standardized laboratory protocols. For instance, in mechanical milling (top-down), the particle size distribution is typically measured using laser diffraction or dynamic light scattering post-synthesis, revealing a broader dispersion compared to the narrower distribution achieved in bottom-up methods like chemical precipitation, where reaction kinetics and precursor concentration can be tightly controlled [30] [34]. The presence of defects in top-down synthesized nanomaterials is often confirmed through techniques like high-resolution transmission electron microscopy (HR-TEM) and X-ray diffraction (XRD) analysis, which can detect crystallographic imperfections and strain [30].
Applications in Medical Device and Drug Development
The distinct properties of nanomaterials synthesized via these two routes dictate their suitability for specific biomedical applications.
Top-Down Applications
Nanomaterials produced via top-down methods are often employed in applications where high structural integrity and scalability are paramount.
- Implantable Medical Devices: Nanostructured surfaces on orthopedic implants (e.g., spinal implants, joint replacements) are created through techniques like sputtering and chemical etching. These surfaces promote improved osteointegration (bone cell attachment and growth), leading to faster healing and longer implant longevity [35] [36]. For example, Stryker has introduced nanostructured titanium spinal implants that leverage this enhanced integration property [35].
- Antimicrobial Coatings: The high surface area of nanoparticles generated by milling or laser ablation is utilized in wound dressings and device coatings. Silver nanoparticles (AgNPs), known for their antimicrobial properties, can be incorporated to reduce infection risks [32]. Smith & Nephew, for instance, has developed a nanofiber-based wound dressing with time-release antibiotics for chronic wound management [35].
Bottom-Up Applications
Bottom-up synthesized nanomaterials excel in applications requiring high precision, complex functionality, and interaction at the molecular level.
- Targeted Drug Delivery: This is a premier application for bottom-up nanoparticles. Systems can be engineered from polymers, liposomes, or inorganic cores (e.g., iron oxide) using methods like self-assembly and chemical precipitation. Their surface can be functionalized with targeting ligands (e.g., antibodies) to deliver chemotherapeutic agents directly to tumor cells, minimizing systemic side effects [37] [32]. The PEGylated gold nanoparticles (PEG-coated AuNPs) studied for modulating the ABC phenomenon is a key example of precise surface engineering [32].
- Diagnostic Imaging and Biosensors: Quantum dots (nanocrystals of semiconductors) synthesized via bottom-up methods like chemical precipitation offer superior fluorescence properties for bioimaging and biosensing [32]. Companies like Thermo Fisher Scientific provide Qdot nanocrystals for advanced in vivo imaging and cellular tracking [36]. Similarly, iron oxide nanoparticles are used as contrast agents to enhance magnetic resonance imaging (MRI) [32].
- Regenerative Medicine: Nanomaterials play a crucial role in tissue engineering. Injectable hydrogels, such as the nanocellulose hydrogel (FibGel) launched by UPM Biomedicals, are created through bottom-up self-assembly. These gels can act as scaffolds for cell growth or as carriers for precise drug delivery and tissue regeneration [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful synthesis and application of nanomaterials require a suite of specialized reagents and analytical tools. The following table details key solutions and materials essential for research in this field.
Table 2: Key Research Reagent Solutions for Nanomaterial Synthesis and Characterization
| Reagent / Material | Function and Role in Research |
|---|---|
| Metal Salts (Precursors) | Source of metal ions (e.g., Gold chloride, Silver nitrate) for bottom-up synthesis methods like chemical precipitation and sol-gel [34]. |
| Reducing Agents (e.g., Sodium Borohydride, Citrate) | Chemicals that reduce metal ions to their zero-valent atomic state, initiating nucleation and nanoparticle growth in bottom-up synthesis [34]. |
| Stabilizing/Capping Agents (e.g., PEG, PVP) | Polymers or molecules that adsorb onto the surface of nanoparticles to prevent aggregation and control growth, ensuring colloidal stability [32]. |
| Ball Mill and Grinding Media | Equipment and hardened balls (e.g., steel, zirconia) used in top-down mechanical milling to fracture bulk powders into nanoparticles [34]. |
| Single-Particle ICP-MS | Advanced analytical technique for precise measurement of nanoparticle size, size distribution, and concentration in a sample [36]. |
| Electron Microscopy (SEM/TEM) | Essential tools for high-resolution morphological and structural characterization of nanomaterials, providing information on size, shape, and aggregation state [38] [36]. |
| Dynamic Light Scattering (DLS) | Instrumentation for determining the hydrodynamic size distribution and stability of nanoparticles in suspension [38]. |
Both top-down and bottom-up synthesis approaches offer distinct and complementary pathways for nanomaterial production, each with a clear set of advantages and trade-offs. The top-down approach is often favored for applications requiring scalability and the use of robust, bulk-derived materials, such as in nanostructured implants and antimicrobial coatings. The bottom-up approach is indispensable for applications demanding atomic-level precision, complex morphologies, and sophisticated surface functionalization, as seen in targeted drug delivery systems, advanced diagnostics, and regenerative medicine.
For researchers and drug development professionals, the decision between these methods is not a matter of superiority but of strategic alignment with the end application's requirements. Factors such as the desired level of crystallinity, permissible defect density, required scalability, and need for surface functionalization must be carefully weighed. Furthermore, the emergence of hybrid approaches that combine the scalability of top-down methods with the precision of bottom-up techniques represents the cutting edge of nanomaterial synthesis, promising to unlock new possibilities in nanoscale medical device research and beyond.
The advancement of targeted drug delivery represents a paradigm shift in therapeutic interventions, moving from systemic administration to precise, site-specific treatment. At the forefront of this revolution are two distinct technological approaches: nanocarriers and micro/nano-robots. While both operate at the microscopic level, their design principles, operational mechanisms, and therapeutic applications differ significantly. This guide provides an objective comparison for researchers and drug development professionals, framing the analysis within the broader context of nanoscale versus microscale medical device research. Nanocarriers are typically passive or responsive nanoscale systems (1-200 nm) designed to encapsulate and transport therapeutic agents, improving bioavailability and minimizing systemic toxicity [39]. In contrast, micro/nano-robots are autonomous or semi-autonomous devices (1-1000 μm) capable of actively navigating biological environments, performing precise therapeutic functions such as drug delivery, imaging, and tumor ablation [39]. Understanding the performance characteristics, advantages, and limitations of each platform is essential for selecting the appropriate technology for specific therapeutic challenges, particularly in complex disease settings like cancer and neurological disorders where precision is paramount.
Nanocarriers: Engineered Transport Systems
Nanocarriers are colloidal nanoparticles that function as transport systems for therapeutic agents, with a typical size range of 1-200 nm, designed to navigate the body's micro-capillaries [39]. These systems demonstrate superior biocompatibility and offer a sustained release of drugs while overcoming biological barriers like the endosome-lysosome mechanism [39]. The field has been revolutionized by microfluidic technologies that enable precise synthesis of nanocarriers with customizable size, composition, and release profiles [40]. Microfluidic platforms provide unparalleled control over fluid dynamics and nanoparticle synthesis, allowing for the production of lipid nanoparticles (LNPs), liposomes, and other nanocarriers with narrow size distribution and high encapsulation efficiency [40]. These systems have become particularly valuable for overcoming biological barriers in therapeutic delivery, including poor targeting, low bioavailability, and systemic toxicity associated with conventional delivery systems [40].
Table 1: Key Characteristics of Nanocarriers for Drug Delivery
| Parameter | Specifications | Remarks |
|---|---|---|
| Size Range | 1-200 nm [39] | Must be <200 nm to navigate body's micro-capillaries [39] |
| Primary Materials | Lipids, polymers, inorganic nanoparticles (gold, iron oxide) [40] | Lipid-based offer best biocompatibility; polymeric offer controlled release; inorganic have imaging capabilities [40] |
| Drug Encapsulation Efficiency | High (due to rapid self-assembly in microfluidics) [40] | Superior to conventional methods; tunable via flow parameters [40] |
| Targeting Mechanism | Passive targeting (EPR effect) & active targeting (surface ligands) [40] | Surface functionalization enables receptor-mediated targeting [40] |
| Key Advantages | Enhanced biodistribution, improved pharmacokinetics, reduced toxicity, sustained release [39] | Protects payload, overcomes solubility issues, enables controlled release [39] |
| Major Limitations | Limited active propulsion, dependent on biological circulation, potential immune recognition | Batch-to-batch reproducibility challenges with some polymer types [40] |
Micro/Nano-Robots: Active Navigation Systems
Micro/nano-robots represent a more advanced form of nanoscale medical devices, typically ranging from 1-1000 μm, with some designs as small as 1-100 nm [39]. These are autonomous or semi-autonomous devices engineered to perform specific tasks at the nanoscale, capable of active navigation rather than passive circulation [39]. Hydrogel-based micro/nano-robotic medical devices feature unique three-dimensional crosslinked networks integrated with responsive chemical functional groups, enabling them to undergo structural and functional transitions under various external stimuli [4]. These devices can be fabricated using top-down approaches (lithography, etching), bottom-up approaches (self-assembly, DNA origami), or hybrid methods [39]. Unlike passive nanocarriers, micro/nano-robots employ sophisticated actuation mechanisms including magnetic fields, ultrasound, light, and chemical fuels to navigate biological environments [4]. This active propulsion enables capabilities far beyond traditional drug delivery systems, including minimally invasive surgical assistance, biosensing, and in vivo imaging [4].
Table 2: Key Characteristics of Micro/Nano-Robots for Drug Delivery
| Parameter | Specifications | Remarks |
|---|---|---|
| Size Range | 1-1000 μm (typically 0.5-3 μm for medical applications) [39] | Diameter of 0.5-3 μm constructed from 1-100 nm components [39] |
| Primary Materials | Hydrogels, DNA nanostructures, magnetic nanoparticles, polymers [4] [39] | Carbon in diamond/fullerene forms for strength; hydrogels for biocompatibility [39] |
| Drug Loading Capacity | Varies with design; can be engineered for high payload capacity | Modular design facilitates incorporation of various payloads [39] |
| Targeting Mechanism | External guidance (magnetic, acoustic) & internal response (pH, enzymes) [4] | Multi-actuation synergistic strategies combine external fields with internal responses [4] |
| Key Advantages | Active propulsion, precise navigation, multi-modal functionality (drug delivery, imaging, sensing) [4] [39] | Can perform complex tasks beyond drug delivery; cellular-level precision achievable [4] |
| Major Limitations | Complex manufacturing, power source challenges, potential immune response, biocompatibility of components [4] [39] | Magnetic field attenuation in deep tissues; tissue penetration limits for some actuation methods [4] |
Direct Performance Comparison
Table 3: Head-to-Head Performance Comparison of Nanocarriers vs. Micro/Nano-Robots
| Performance Metric | Nanocarriers | Micro/Nano-Robots | Experimental Evidence |
|---|---|---|---|
| Targeting Precision | Tissue-level (enhanced permeability and retention - EPR) to cellular-level (with ligands) [40] | Cellular to subcellular level (with active navigation) [4] | Dual-actuation micro/nano-robots show improved tumor drug enrichment vs. single magnetic field-driven counterparts [4] |
| Drug Release Control | Stimuli-responsive (pH, enzymes) & sustained release profiles [40] | On-demand release via external triggers (light, magnetic, ultrasound) [4] | pH-responsive hydrogels in tumor microacidic environment undergo protonation, leading to polymer chain shrinkage and release [4] |
| Navigation Capability | Passive circulation; limited to biological fluid dynamics | Active propulsion and guidance through biological barriers [4] | Magnetic nanoparticles in hydrogel allow gradient magnetic fields to guide directional movement [4] |
| Manufacturing Scalability | High (with microfluidic systems) [40] | Low to moderate (complex fabrication processes) [39] | Microfluidics enables continuous, one-step production with narrow size distribution [40] |
| Immunogenicity Risk | Low to moderate (depending on surface modification) [40] | Moderate to high (complex materials and structures) [4] | Surface-functionalized nanomaterials show reduced immune recognition; hydrogel matrices generally biocompatible [4] |
| Regulatory Status | More advanced (several FDA-approved formulations) | Mostly preclinical research with some early exceptions [4] | Lipid nanoparticles (LNPs) are clinically leading nanocarrier systems for RNA delivery [40] |
Experimental Protocols and Methodologies
Microfluidic Synthesis of Nanocarriers
The preparation of uniform nanocarriers with precise characteristics requires sophisticated manufacturing approaches. Microfluidic technology has emerged as the gold standard for reproducible and scalable fabrication [40].
Table 4: Key Research Reagents for Microfluidic Nanocarrier Synthesis
| Reagent/Category | Specific Examples | Function in Experiment |
|---|---|---|
| Lipid Materials | Ionizable lipids, phospholipids, cholesterol, PEG-lipids [40] | Structural components of lipid nanoparticles (LNPs); determine stability, fusion with cells |
| Polymeric Materials | PLGA, chitosan, polyesters [40] | Form biodegradable nanoparticle matrix; control drug release kinetics |
| Microfluidic Chips | Glass or PDMS chips with micromixers (herringbone, staggered herringbone) [40] | Create precise mixing environment; control nanoparticle self-assembly |
| Organic Solvents | Ethanol, acetone [40] | Dissolve lipid/polymer components; miscible with aqueous phases |
| Aqueous Buffers | Phosphate buffer saline (PBS), citrate buffers [40] | Form aqueous phase for nanoparticle formation; control pH for stability |
| Characterization Instruments | Dynamic Light Scattering (DLS), Nanoparticle Tracking Analysis (NTA) [40] | Measure particle size, distribution, and concentration |
Protocol: Microfluidic Preparation of Lipid Nanoparticles
- Solution Preparation: Prepare lipid mixture in ethanol (typical concentration 10-50 mg/mL) and aqueous buffer containing therapeutic payload (mRNA, siRNA, or small molecules) [40].
- Microfluidic Setup: Use a pressure- or syringe pump-driven system with appropriate microfluidic chip (flow-focusing or mixing geometry). Maintain temperature control (typically 20-25°C) [40].
- Flow Rate Optimization: Set flow rate ratio (FRR) between aqueous and organic phases between 1:1 and 3:1, with total flow rates (TFR) from 5 to 20 mL/min [40].
- Mixing and Self-Assembly: Rapid mixing in microfluidic channel induces nanoprecipitation and self-assembly through controlled diffusion [40].
- Buffer Exchange: Use tangential flow filtration or dialysis to remove ethanol and exchange into final storage buffer [40].
- Quality Control: Characterize particle size (target 50-150 nm), polydispersity index (PDI <0.2), encapsulation efficiency (>90%), and morphology (spherical, uniform) [40].
Fabrication and Actuation of Micro/Nano-Robots
The creation of functional micro/nano-robots involves sophisticated fabrication techniques and actuation mechanisms that enable their unique capabilities.
Table 5: Key Research Reagents for Micro/Nano-Robot Fabrication
| Reagent/Category | Specific Examples | Function in Experiment |
|---|---|---|
| Hydrogel Polymers | Alginate, chitosan, poly(N-isopropylacrylamide) - PNIPAM [4] | Form 3D network matrix; provide biocompatibility and stimulus responsiveness |
| Magnetic Components | Iron oxide nanoparticles (Fe₃O₄), nickel segments [4] | Enable magnetic actuation and guidance under magnetic fields |
| Photothermal Materials | Gold nanoparticles, gold nanorods, carbon nanotubes [4] | Convert light energy to heat for photothermal actuation and drug release |
| DNA Origami Components | Single-stranded DNA, staples, modified oligonucleotides [39] | Create programmable nanostructures with precise molecular control |
| Crosslinking Agents | Calcium chloride, glutaraldehyde, genipin [4] | Stabilize hydrogel structures through physical or chemical crosslinking |
| Fluorescent Tags | FITC, rhodamine, quantum dots [4] | Enable tracking and visualization in biological environments |
Protocol: Multi-Actuation Hydrogel Micro/Nano-Robot Preparation
- Material Design: Select base polymer (natural or synthetic hydrogel) and incorporate functional components (magnetic nanoparticles, photothermal agents) through physical mixing or chemical conjugation [4].
- Fabrication Approach:
- Crosslinking: Initiate crosslinking through ionic (Ca²⁺ for alginate), chemical (covalent crosslinkers), or physical (temperature-induced) methods [4].
- Surface Functionalization: Modify surface with targeting ligands (peptides, antibodies) or stealth coatings (PEG) to enhance targeting and circulation [4].
- Drug Loading: Incubate with therapeutic payload in swelling state or incorporate during fabrication [4].
- Actuation Testing:
- Magnetic Actuation: Apply rotating or gradient magnetic fields (5-100 mT) for propulsion [4].
- Photo-Actuation: Use NIR laser (650-900 nm) for photothermal response and drug release [4].
- Multi-Modal Actuation: Combine magnetic guidance with photothermal triggering for enhanced targeting and controlled release [4].
Comparative Experimental Data Analysis
Targeting Efficiency and Drug Delivery Performance
Independent studies provide quantitative data on the performance of both platforms in various drug delivery applications. The targeting efficiency and drug delivery capabilities represent critical differentiators between these technologies.
Table 6: Quantitative Comparison of Targeting and Delivery Performance
| Parameter | Nanocarriers | Micro/Nano-Robots | Experimental Context |
|---|---|---|---|
| Tumor Accumulation | 3-10% injected dose/g tissue [40] | 5-15% injected dose/g tissue (with active guidance) [4] | Dual-actuation systems show 1.5-2x improvement over passive accumulation [4] |
| Cellular Uptake | 2-5 fold increase vs. free drug [40] | 5-10 fold increase vs. free drug [39] | Active penetration enhances internalization in 3D tumor models [39] |
| Target/Non-Target Ratio | 3:1 to 5:1 [40] | 5:1 to 15:1 [4] | Magnetic guidance improves specificity in multi-actuation systems [4] |
| Blood Circulation Half-life | 2-24 hours (PEGylated) [40] | 1-8 hours (size-dependent) [4] | Surface modification crucial for both platforms [40] [4] |
| Depth of Tissue Penetration | 50-100 μm from vasculature [40] | 100-500 μm (with active propulsion) [4] | Active motion overcomes diffusion limitations [4] |
| Drug Release Kinetics | Hours to days (sustained) [40] | Minutes to hours (on-demand) [4] | External triggers enable precise temporal control [4] |
Technical and Manufacturing Considerations
The practical implementation of these technologies requires careful consideration of manufacturing complexity, scalability, and regulatory pathways.
Table 7: Technical and Commercialization Comparison
| Consideration | Nanocarriers | Micro/Nano-Robots |
|---|---|---|
| Manufacturing Cost | Moderate (microfluidic systems reduce cost) [40] | High (complex fabrication, specialized materials) [39] |
| Scalability | High (continuous production possible) [40] | Low to moderate (batch processes dominant) [39] |
| Sterilization Methods | Filtration, aseptic processing [40] | Challenge due to heat/radiation sensitivity [4] |
| Storage Stability | 6-24 months (lyophilized) [40] | Weeks to months (condition-specific) [4] |
| Regulatory Pathway | More established (multiple FDA-approved products) [40] | Emerging (case-by-case evaluation) [4] |
| Clinical Translation | Advanced (commercial products in market) [40] | Preclinical/early clinical development [4] |
The comparative analysis presented in this guide demonstrates that both nanocarriers and micro/nano-robots offer distinct advantages for targeted drug delivery applications. Nanocarriers represent a more mature technology with established manufacturing methods, particularly through microfluidic approaches that enable precise control over particle characteristics [40]. Their proven clinical translation and scalability make them suitable for a wide range of therapeutic applications where passive or ligand-mediated targeting is sufficient. In contrast, micro/nano-robots offer unprecedented capabilities for active navigation and multi-modal functionality, enabling cellular-level precision and on-demand drug release [4] [39]. While still primarily in preclinical development, their potential for overcoming complex biological barriers and performing integrated diagnosis and therapy is substantial.
The future evolution of both platforms will likely involve increased convergence, with nanocarriers incorporating more sophisticated targeting mechanisms and micro/nano-robots benefiting from advances in manufacturing scalability. For researchers and drug development professionals, the selection between these technologies should be guided by specific application requirements, with nanocarriers currently offering a more straightforward path to clinical implementation, and micro/nano-robots representing a promising frontier for addressing therapeutic challenges where precision and active navigation are paramount. As both fields advance, they will continue to reshape the landscape of targeted drug delivery, ultimately enabling more effective and personalized therapeutic interventions.
The evolution of medical devices from the micro- to the nanoscale represents a paradigm shift in diagnostic and imaging capabilities. Nanoscale devices leverage unique physicochemical properties that emerge at dimensions below 100 nanometers, enabling unprecedented interaction with biological molecules and pathways. The table below provides a high-level performance comparison of these platforms across key metrics relevant to biomedical research and development.
Table 1: High-Level Performance Comparison: Nanoscale vs. Microscale Medical Devices
| Performance Characteristic | Nanoscale Devices | Microscale Devices |
|---|---|---|
| Spatial Resolution | Atomic/Molecular level (1-100 nm) [41] | Cellular level (>100 nm) |
| Limit of Detection (LOD) | Ultra-high (e.g., biomarker detection at picomolar concentrations) [42] [41] | Lower (e.g., biomarker detection at nanomolar concentrations) |
| Susceptibility to Fouling | Higher, due to close proximity to surface and molecular-scale interactions [43] | Lower, due to larger feature sizes |
| Dependence on Clinical Matrix | High; performance can vary significantly with sample type (e.g., serum vs. buffer) [43] | Moderate; more robust to matrix variations |
| Multiplexing Capability | High (e.g., multicolor quantum dots, multi-analyte sensors) [42] [43] | Limited |
| Therapeutic Integration (Theranostics) | Native capability for combined diagnosis and therapy [42] [41] | Primarily diagnostic or therapeutic, rarely combined |
| Primary Manufacturing Approach | Bottom-up and top-down synthesis [41] | Primarily top-down fabrication |
Quantitative Performance Data in Diagnostics and Imaging
The theoretical advantages of nanoscale devices are borne out in experimental data. The following tables consolidate key performance metrics from recent research, providing a direct comparison for research scientists evaluating these technologies.
Diagnostic Biosensor Performance
Biosensors are a vibrant area of research, with electrochemical and photonic modalities being the two dominant platforms. The performance differences are rooted in their fundamental operational characteristics [43].
Table 2: Comparative Analysis of Biosensor Modalities at the Nanoscale
| Biosensor Modality | Sub-Type | Mechanism | Key Advantage | Reported Limit of Detection (LOD) | Susceptibility to Non-Specific Binding |
|---|---|---|---|---|---|
| Electrochemical | Faradaic | Measures current from redox reactions at an electrode surface [43] | High sensitivity to surface-bound molecules | Varies with target; demonstrated for glucose and other biomarkers [43] | High [43] |
| Electrochemical | Non-Faradaic | Measures capacitance changes in the electrochemical double layer [43] | Label-free detection | Varies with target [43] | High [43] |
| Photonic | Refractive Index (e.g., Microring Resonator) | Tracks resonance shift due to local refractive index change from biomarker binding [43] | Label-free, multiplexing potential | Down to 10⁻⁵ Refractive Index Units (RIU) [43] | Lower than electrochemical [43] |
| Photonic | Fluorescence | Measures intensity of light emitted from labeled biomarkers [43] | High specificity, multicolor operation | Picomolar range for specific biomarkers [43] | Low (due to labeling) |
Advanced Imaging and Contrast Agents
In medical imaging, nanotechnology enhances contrast and specificity, particularly for challenging applications like cancer screening.
Table 3: Performance of Nanoparticle-Based X-Ray Contrast Agents for Breast Cancer Screening
| Contrast Agent Type | Material | Key Imaging Application | Reported Performance Advantage | Research/Clinical Status |
|---|---|---|---|---|
| Conventional | Iodinated small molecules | Contrast-enhanced mammography/tomosynthesis [44] | Baseline | Clinical Standard |
| Nanoparticle | Gold (Au) | Breast CT, Mammography [44] | High X-ray attenuation, potential for targeted imaging [44] | Research Phase |
| Nanoparticle | Bismuth Sulfide (Bi₂S₃) | Mammography [44] | High X-ray attenuation, potentially lower cost than gold [44] | Research Phase |
| Nanoparticle | Silver Sulfide/Telluride (Ag₂S, Ag₂Te) | Mammography, Tomosynthesis [44] | Tunable properties, high contrast-to-noise ratio [44] | Research Phase (Patent Stage) |
Experimental Protocols and Methodologies
To ensure reproducibility and provide a clear framework for comparison, this section outlines standardized experimental protocols for evaluating key device categories.
Protocol: Evaluating a Photonic Microring Resonator Biosensor
This protocol details the process for characterizing a label-free photonic biosensor, as referenced in Figure 2(a) of the search results [43].
1. Sensor Functionalization:
- Surface Activation: Clean the sensor chip (e.g., silicon-based microring resonator) with oxygen plasma.
- Binder Immobilization: Incubate the sensor with a solution containing the capture agent (e.g., antibody, DNA aptamer) specific to the target biomarker. A common method involves using a self-assembled monolayer (SAM) with linker chemistry (e.g., NHS/EDC) to covalently bind the binder molecule to the sensor surface [43].
- Blocking: Treat the surface with a blocking agent (e.g., BSA) to minimize non-specific binding sites.
2. Experimental Setup and Data Acquisition:
- Instrumentation: Mount the sensor chip in a microfluidic flow cell integrated with a tunable laser and photodetector array.
- Baseline Acquisition: Flow a running buffer (e.g., PBS) over the sensor and record the resonance wavelength (λ₀) of each ring to establish a stable baseline.
- Sample Introduction: Introduce the sample (e.g., serum, buffer spiked with target biomarker) at a constant flow rate.
- Real-Time Monitoring: Continuously monitor the resonance wavelength shift (Δλ) as the target biomarker binds to the surface-immobilized capture agent.
3. Data Analysis:
- Binding Curve: Plot Δλ versus time to generate a binding curve.
- Calibration: Construct a calibration curve by plotting steady-state Δλ against known concentrations of the target biomarker.
- LOD Calculation: Determine the Limit of Detection (LOD) as three times the standard deviation of the baseline noise, converted into a concentration using the calibration curve [43].
Diagram 1: Photonic biosensor evaluation workflow.
Protocol: Characterizing Nanoparticle-Based X-Ray Contrast Agents
This protocol summarizes the key steps for evaluating novel nanoparticle contrast agents, as derived from research on breast cancer screening [44].
1. Nanoparticle Synthesis and Functionalization:
- Synthesis: Prepare nanoparticles (e.g., gold, bismuth sulfide) via bottom-up chemical methods (e.g., reduction of gold salts, thermal decomposition) to control size and shape [41].
- Surface Coating: Functionalize the nanoparticle surface with a stabilizing ligand (e.g., PEG) to ensure colloidal stability and biocompatibility [41].
- Targeting (Optional): Conjugate targeting moieties (e.g., peptides, antibodies) to the surface for active targeting of cancer biomarkers.
2. In Vitro Phantom Imaging:
- Phantom Preparation: Create tissue-equivalent phantoms with compartments mimicking healthy and tumorous tissue (varying densities).
- Contrast Administration: Introduce the nanoparticle contrast agent into the "tumorous" compartment, with a standard iodinated agent in a control compartment.
- Image Acquisition: Image the phantoms using clinical X-ray modalities (e.g., mammography, CT scanner).
- Quantitative Analysis: Measure and compare the X-ray attenuation (in Hounsfield Units for CT) or contrast-to-noise ratio (CNR) between the nanoparticle and the standard agent.
3. In Vivo Efficacy and Safety:
- Animal Models: Administer the contrast agent to animal models (e.g., murine models of breast cancer).
- Pharmacokinetics (PK): Analyze blood samples over time to determine key PK parameters: Area Under the Curve (AUC) and peak concentration (Cmax) [4].
- Biodistribution: Quantify nanoparticle accumulation in target tumors and major organs post-imaging.
- Toxicity Assessment: Monitor animals for acute adverse effects and analyze histology of key organs for signs of toxicity.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of nanoscale diagnostic and imaging devices rely on a specific set of materials and reagents. The following table details this core "toolkit" and the function of each component.
Table 4: Essential Research Reagents and Materials for Nanodevice Development
| Toolkit Item | Function | Specific Examples |
|---|---|---|
| Binder Molecules / Capture Agents | Provides specificity by binding the target biomarker of interest. | Antibodies, DNA aptamers, molecularly imprinted polymers [43]. |
| Nanomaterial Cores | Serves as the foundational platform for sensors or contrast agents. | Gold nanoparticles, quantum dots, magnetic nanoparticles, polymeric nanoparticles (PLGA), liposomes [44] [41]. |
| Surface Functionalization Reagents | Modifies the nanomaterial surface to improve stability, biocompatibility, and to conjugate binder molecules. | Polyethylene Glycol (PEG), Silane coupling agents, NHS/EDC chemistry for amine coupling [41]. |
| Clinical Matrix Samples | Used to test device performance in complex, biologically relevant conditions. | Serum, plasma, urine, whole blood [43]. |
| Blocking Agents | Reduces non-specific binding to the sensor or nanoparticle surface, minimizing background signal. | Bovine Serum Albumin (BSA), casein, salmon sperm DNA [43]. |
| Reference/Control Materials | Essential for calibrating sensors and benchmarking new contrast agents. | Iodinated contrast agents (for X-ray), known concentration of purified target analyte [44]. |
The experimental data and protocols presented confirm that nanoscale devices offer transformative advantages in sensitivity, specificity, and functional integration for advanced diagnostics and imaging. However, this enhanced performance comes with increased complexity in manufacturing, characterization, and a greater susceptibility to biofouling and matrix effects.
For researchers and drug development professionals, the choice between micro- and nanoscale platforms is not merely one of superior specs, but of strategic application fit. Microscale devices may offer robustness and simplicity for certain applications, while nanoscale technologies unlock new capabilities in early disease detection, personalized medicine, and theranostics. The future of the field lies in addressing the translational challenges of nanodevices—such as long-term pharmacokinetics and immunogenicity [4]—through interdisciplinary collaboration and robust, standardized experimental frameworks as outlined in this guide.
The convergence of nanotechnology with tissue engineering has ushered in a transformative era for regenerative medicine, fundamentally shifting the focus from micro- to nanoscale architectural control in scaffold design. Nanofibrous scaffolds, particularly those fabricated via electrospinning and thermally-induced phase separation (TIPS), have emerged as superior biomimetic platforms that closely replicate the native extracellular matrix (ECM) [45] [46]. This paradigm shift is driven by the recognition that natural tissues and organs—including bone, skin, tendon, and cartilage—are hierarchically organized into fibrous structures with dimensions down to the nanometer scale [45]. Unlike traditional microscale scaffolds, nanofibrous architectures provide physical and biochemical cues that profoundly influence cellular behaviors, including adhesion, proliferation, migration, and differentiation [47] [46].
The strategic incorporation of bioactive composites further enhances the functionality of these nanoscale constructs. By hybridizing synthetic polymers with natural biopolymers and inorganic components, researchers have developed scaffolds that overcome the limitations of single-component materials, particularly the lack of cell recognition sites and poor hydrophilicity associated with pristine synthetic polymers [45]. This comparative analysis examines the performance of leading nanofibrous scaffold technologies against conventional alternatives, providing researchers and drug development professionals with experimental data and methodologies to inform scaffold selection and development for specific tissue engineering applications.
Table 1: Core Fabrication Techniques for Nanofibrous Scaffolds
| Fabrication Method | Fundamental Principle | Typical Fiber Diameter | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Electrospinning | Uses electric field to draw polymer solution into fibers [45] | 50 nm - several microns [45] | Wide material selection, high surface area-to-volume ratio [47] | Limited 3D thickness control, small pore sizes can restrict cell infiltration [46] |
| Thermally-Induced Phase Separation (TIPS) | Leverages temperature-dependent polymer solution instability to form nanofibrous networks [46] | 50-500 nm [46] | Creates true 3D scaffolds with high porosity, excellent pore interconnection [46] | Longer processing times, limited to thermally stable polymers |
| Molecular Self-Assembly | Spontaneous organization of molecules into ordered structures via non-covalent interactions [46] | 5-20 nm (significantly smaller than other methods) [46] | Achieves finest nanoscale features, biologically relevant fiber dimensions | Complex synthesis, limited mechanical strength, challenging scalability |
Comparative Performance Analysis of Scaffold Architectures
Architectural and Mechanical Performance
The structural integrity and physical properties of scaffolds directly determine their suitability for specific tissue engineering applications. Comparative studies reveal significant differences between nanofibrous composites and conventional alternatives.
Table 2: Mechanical and Physical Properties of Representative Scaffolds
| Scaffold Material Composition | Tensile Strength (MPa) | Young's Modulus (MPa) | Porosity (%) | Degradation Rate | Key Applications |
|---|---|---|---|---|---|
| PCL/Gt-BG Bilayer [48] | ~4x higher than PCL/Gt | Data not specified | Significantly enhanced surface area and total pore volume vs. single layer | Higher than pure PCL | Bone tissue engineering |
| PCL/Chitosan (9.1%) [46] | Maximum Young's modulus in blend series | Optimized balance | Data not specified | Data not specified | Enhanced cell adhesion with mechanical stability |
| PLLA/PCL with IPMs [49] | Suitable for bone regeneration | Matching natural tissue requirements | Interconnected perfusable microchannels (0.4-0.6mm spacing) | Tailorable degradation | Vascularized bone regeneration |
| Pure PCL [48] | Baseline for comparison | Baseline for comparison | Lower than composites | Slow degradation | Control in studies |
| Conventional Microfibrous Scaffolds | Variable | Often higher than nanofibrous | Moderate porosity with limited interconnectivity | Variable | General tissue engineering |
The data demonstrates that composite nanofibrous scaffolds achieve superior mechanical performance compared to single-component systems. The PCL/Gt-BG bilayer scaffold shows a remarkable four-fold increase in tensile strength compared to PCL/Gt alone, highlighting the reinforcing effect of the bioactive glass layer [48]. Similarly, the strategic blending of PCL with chitosan creates an optimal balance where the composite achieves maximum Young's modulus while significantly improving cell adhesion compared to pure PCL [46].
Biological Performance Metrics
The ultimate success of tissue engineering scaffolds is determined by their biological performance, including their ability to support cell growth, promote tissue-specific differentiation, and integrate with host tissue.
Table 3: Biological Performance of Nanofibrous Scaffolds
| Scaffold Type | Cell Response | Osteogenic Potential | Vascularization Capacity | Experimental Evidence |
|---|---|---|---|---|
| PCL/Gelatin Composite [45] | Significant cell proliferation and infiltration (up to 110 μm) | Moderate | Limited data | In vitro cell culture with quantitative measurement via laser scanning microscopy |
| PLLA/PCL with VEGF-loaded IPMs [49] | Enhanced HUVEC migration and neo-blood vessel formation | Strong, with new bone formation | Excellent, with functional vascular networks | Transwell migration, scratch wound, CAM assays, microangiography, rat cranial defects |
| PCL/Gt-BG Bilayer [48] | Biocompatible (non-cytotoxic to MRC-5 cells) | High (HA-like layer formation in SBF) | Limited direct data | Cytotoxicity testing, SBF immersion with HA formation confirmation |
| Collagen-Mimetic PLLA via TIPS [46] | Enhanced cell attachment | Promotes stem cell differentiation | Limited data | In vitro studies with various cell types |
| Conventional Microfibrous Scaffolds | Variable cell adhesion | Limited without biofunctionalization | Often requires additional growth factors | Extensive historical data |
The biological data reveals distinct advantages of composite nanofibrous systems. The incorporation of natural polymers like gelatin significantly improves cellular infiltration compared to synthetic-only scaffolds [45]. Furthermore, scaffolds with engineered architectural features like interconnected perfusable microchannels (IPMs) combined with growth factors (VEGF) demonstrate enhanced capacity for vascularization, which is critical for bone regeneration [49]. The bioactivity of composite scaffolds is further evidenced by the formation of hydroxyapatite-like layers in simulated body fluid, indicating bone-bonding capability [48].
Experimental Protocols for Scaffold Evaluation
Fabrication of PCL/Gelatin/Bioactive Glass Bilayer Scaffold
Objective: To create a biomimetic bilayer scaffold with enhanced mechanical and biological properties for bone tissue engineering [48].
Materials:
- Polycaprolactone (PCL): Synthetic polymer providing mechanical integrity and biodegradability [48]
- Gelatin (Gt): Natural polymer imparting hydrophilicity and cell recognition sites [48]
- Bioactive Glass (BG) Nanoparticles: Ceramic component enabling hydroxyapatite formation and osteoconduction [48]
- Formic Acid: Solvent for polymer dissolution [48]
Methodology:
- Solution Preparation: Prepare 14% (w/v) PCL solution in formic acid with stirring (400 rpm, overnight). For PCL/Gt blend, add 30 w% gelatin (relative to PCL weight) and stir until homogeneous [48].
- BG Incorporation: Disperse 3 w% BG nanoparticles (particle size <10 nm) in PCL/Gt solution using stirring (600 rpm, overnight) followed by ultrasonication (10 minutes) [48].
- Electrospinning Parameters: Use 0.5-1.0 mL/h flow rate, 17-25 kV voltage, and 13 cm needle-to-collector distance [48].
- Bilayer Construction: Electrospin PCL/BG nanofibers directly onto pre-formed PCL/Gt nanofibrous layer using equal volume ratios (50:50) [48].
Key Quality Controls:
- Measure solution viscosity using rotational viscometer (e.g., 5 rpm at 22°C) [48]
- Characterize fiber morphology and diameter using FE-SEM (30 fibers minimum per sample) [48]
- Confirm BG nanoparticle distribution within fibers using TEM [48]
Microchannel-Engineered Scaffold for Vascularized Bone Regeneration
Objective: To create a nanofibrous scaffold with interconnected perfusable microchannels (IPMs) that enhance vascularization and bone regeneration [49].
Materials:
- PLLA/PCL Blend: Base polymer system providing nanofibrous architecture
- Carbamel-Based Sacrificial Template: Creates customizable microchannel networks
- Vascular Endothelial Growth Factor (VEGF): Angiogenic factor promoting blood vessel formation
Methodology:
- Scaffold Fabrication: Combine 3D printing technology with phase separation and sacrificial template methods [49]
- Microchannel Patterning: Create regular IPM networks with adjustable parameters (spacings: 0.4, 0.5, 0.6 mm; diameters: 0.8, 1, 1.2 mm) [49]
- VEGF Loading: Incorporate VEGF into optimized microchannel configuration (0.5/0.8-IPMs) [49]
- In Vivo Evaluation: Implant in rat cranial bone defects to assess bone regeneration [49]
Analytical Methods:
- Transwell Migration Assay: Quantify HUVEC migration toward scaffold [49]
- Scratch Wound Healing Assay: Measure cell migration capacity [49]
- Chorioallantoic Membrane (CAM) Assay: Assess neo-blood vessel formation [49]
- Microangiography: Visualize functional vascular networks in vivo [49]
- Histological Analysis: Evaluate new bone formation in defect models [49]
Diagram Title: Development Workflow for Nanofibrous Composite Scaffolds
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and evaluation of nanofibrous scaffolds require specific materials and characterization tools. The following table details essential components for researchers entering this field.
Table 4: Essential Research Reagents and Materials for Nanofibrous Scaffold Development
| Category/Reagent | Specific Examples | Function/Purpose | Key Considerations |
|---|---|---|---|
| Synthetic Polymers | PCL, PLLA, PLGA, PU [45] [47] | Provide structural integrity, mechanical strength, controlled biodegradation | Molecular weight affects viscosity/spinnability; purity influences cytotoxicity |
| Natural Polymers | Gelatin, Collagen, Chitosan, Silk [45] [46] [48] | Enhance bioactivity, improve cell adhesion, provide biological recognition signals | Potential immunogenicity; batch-to-batch variability; may require crosslinking |
| Bioactive Ceramics | Bioactive Glass (BG), Hydroxyapatite (HA) [46] [48] | Promote mineral formation, enhance osteoconduction, improve mechanical stiffness | Nanoparticle size and distribution affect agglomeration and release profiles |
| Solvents | Formic Acid, Chloroform, Hexafluoroisopropanol (HFIP) [48] | Dissolve polymers for electrospinning or phase separation | Toxicity residues must be removed; affects solution conductivity/viscosity |
| Characterization Tools | FE-SEM, TEM, FTIR, Mercury Intrusion Porosimetry [48] | Analyze fiber morphology, composition, porosity, and mechanical properties | Sample preparation critical for accurate results; multiple techniques recommended |
| Biological Assays | Cell Cytotoxicity (MTT), SBF Immersion, CAM Assay, Animal Defect Models [49] [48] | Evaluate biocompatibility, bioactivity, angiogenesis, and tissue regeneration | Appropriate positive/negative controls essential; follow ethical guidelines |
The comprehensive comparison of nanofibrous scaffolds and bioactive composites reveals a clear trajectory in tissue engineering toward increasingly sophisticated biomimetic designs. The experimental data demonstrates that composite nanofibrous systems consistently outperform single-component and conventional microfiber scaffolds across multiple metrics, including mechanical properties, cellular response, and tissue-forming capacity. The integration of synthetic polymers with natural biopolymers and bioactive inorganic components creates synergistic effects that address the fundamental challenges of regenerative medicine.
Future developments will likely focus on smart scaffolds with enhanced biofunctionality, potentially incorporating controlled release mechanisms, stimulus-responsive elements, and advanced architectural features like interconnected microchannels. As research progresses, the translation of these technologies to clinical applications will require intensified focus on scalability, regulatory compliance, and demonstration of efficacy in complex disease models. For researchers and drug development professionals, the current evidence strongly supports the prioritization of nanoscale composite approaches in developing next-generation solutions for tissue regeneration.
Diagram Title: Multifunctional Scaffold Mechanism of Action
Navigating Challenges: Biocompatibility, Manufacturing, and Regulatory Hurdles
Ensuring Biocompatibility and Assessing Nanotoxicology for Clinical Safety
The integration of nanoscale materials into medical devices represents a paradigm shift in biomedical engineering, offering unprecedented capabilities for diagnostics, targeted drug delivery, and regenerative medicine. These devices, typically with critical dimensions between 1-100 nanometers, exploit unique physicochemical properties that emerge at this scale, including high surface area-to-volume ratios, quantum effects, and tunable optical behavior [41] [50]. However, these same properties that enable enhanced functionality also introduce complex biocompatibility and safety considerations that differ substantially from those of conventional microscale devices. While microscale devices (1-100 micrometers) primarily interact with cells and tissues through their bulk material properties and macroscopic architecture, nanoscale devices engage with biological systems at the molecular level, enabling direct interactions with cellular machinery, protein complexes, and genetic material [2] [41].
This comparison guide objectively evaluates the performance and safety assessment methodologies for nanoscale versus microscale medical devices, with particular emphasis on biocompatibility and nanotoxicology. For researchers and drug development professionals, understanding these distinctions is critical for designing safer biomedical applications and navigating the complex regulatory pathway toward clinical translation. The fundamental challenge lies in balancing the remarkable technological advantages of nanotechnology—including enhanced sensitivity, targeted delivery capabilities, and improved bioavailability—against potential toxicological risks such as oxidative stress induction, inflammatory responses, and altered biodistribution patterns [41] [50].
Comparative Analysis: Nanoscale vs. Microscale Medical Devices
Table 1: Fundamental characteristics and biological interactions of nanoscale versus microscale medical devices.
| Characteristic | Nanoscale Devices (1-100 nm) | Microscale Devices (1-100 μm) |
|---|---|---|
| Size Range | 1-100 nm | 1-100 μm |
| Surface Area to Volume Ratio | Very high | Moderate to low |
| Primary Biological Interaction Level | Molecular/subcellular | Cellular/tissue |
| Dominant Material Properties | Quantum effects, surface plasmon resonance | Bulk material properties |
| Cellular Uptake Mechanisms | Passive diffusion, endocytosis, receptor-mediated uptake | Primarily phagocytosis (for smaller micro-devices) |
| Biodistribution Potential | Can cross biological barriers (e.g., blood-brain barrier), widespread distribution | Typically localized to implantation site or specific organs |
| Clearance Pathways | Renal clearance (<5.5 nm), hepatic accumulation, potential for long-term retention | Biodegradation, encapsulation, surgical removal |
| Key Biocompatibility Concerns | Protein corona formation, oxidative stress, genotoxicity, immunogenicity | Foreign body response, fibrosis, mechanical mismatch |
| Toxicity Assessment Focus | Subcellular effects, reactive oxygen species generation, long-term biodistribution | Cytocompatibility, hemocompatibility, sensitization |
The performance differential between nanoscale and microscale devices stems fundamentally from their dimensional relationship to biological structures. Nanoscale devices approach the size of proteins, DNA, and cellular receptors, enabling intimate interactions that microscale devices cannot achieve [2]. For instance, while a microscale sensor might detect biomarkers through surface binding events, a nanoscale sensor can potentially operate within cells, providing real-time monitoring of metabolic processes. However, this enhanced functionality comes with increased complexity in safety assessment. Where microscale device biocompatibility focuses largely on bulk material properties and macroscopic tissue integration, nanoscale device safety must account for dynamic nano-bio interactions that evolve based on precise physicochemical parameters including size, shape, surface chemistry, and charge [50].
Material Composition and Functionalization Strategies
Table 2: Material options and their biocompatibility profiles for nanoscale and microscale devices.
| Material Category | Specific Examples | Applications | Biocompatibility Advantages | Toxicity Concerns |
|---|---|---|---|---|
| Silicon-Based | Single-crystal silicon, Silicon carbide, Silicon dioxide | MEMS sensors, structural components [2] | Excellent mechanical properties, well-characterized [2] | Brittleness, potential for particle shedding [2] |
| Polymers | PDMS, Polyimide, SU-8, Parylene C, PLA, PLGA | Flexible substrates, microfluidics, drug delivery systems [2] [41] | Tunable biodegradability, biocompatibility, flexibility [2] | Variable degradation rates, potential inflammatory responses |
| Metals | Gold, Nickel, Aluminum, Titanium | Electrodes, conductive components, structural elements [2] | Corrosion resistance (Au), durability (Ni), established safety profiles [2] | Nickel cytotoxicity, metal ion leaching, allergic potential [2] |
| Piezoelectric | PZT, Aluminum Nitride, Zinc Oxide | Energy harvesters, actuators, ultrasonic transducers [2] | Self-powering capability, precise mechanical control [2] | Potential heavy metal toxicity (PZT), unknown long-term effects |
| Carbon-Based | Graphene, Carbon nanotubes, Fullerenes | Biosensors, electrodes, structural reinforcement [2] [50] | Exceptional electrical/thermal conductivity, mechanical strength [2] | Needle-like morphology causing membrane damage, persistent accumulation [50] |
| Two-Dimensional | Graphene, MXenes, Transition metal dichalcogenides | Ultra-sensitive sensors, advanced drug delivery [2] | Ultra-thin structure, high surface area, unique electronic properties [2] | Unknown long-term biodistribution, edge reactivity |
Material selection critically influences both device performance and biological safety. For nanoscale devices, surface functionalization has emerged as a crucial strategy for enhancing biocompatibility and targeting specificity. Polyethylene glycol (PEG) conjugation ("PEGylation") creates a hydrophilic protective layer that reduces opsonization and extends circulatory half-life by minimizing immune system recognition [41]. Additionally, surface modifications with targeting ligands (antibodies, peptides) enable cell-specific interactions, potentially concentrating therapeutic effects while reducing off-target toxicity [41]. For microscale devices, surface modifications typically focus on topographical patterning or bulk coating with bioactive materials like hydroxyapatite to improve tissue integration, representing a fundamentally different approach to biocompatibility enhancement [2].
Nanotoxicology Assessment: Methodologies and Mechanisms
The assessment of nanotoxicology requires specialized methodologies that account for the unique behaviors of nanomaterials in biological systems. Key mechanisms of nanotoxicity include:
Oxidative Stress and Inflammation: Nanoparticles can catalyze the generation of reactive oxygen species (ROS) through their surface reactivity or through disruption of cellular redox balance. This oxidative stress can trigger inflammatory pathways, damage cellular proteins, lipids, and DNA, and potentially lead to chronic inflammation or fibrosis [50]. Assessment methodologies include measuring glutathione depletion, lipid peroxidation, and cytokine release profiles.
Protein Corona Formation: When nanomaterials enter biological fluids, they rapidly adsorb proteins onto their surface, forming a "corona" that fundamentally alters their biological identity and interactions [50]. This dynamic layer influences cellular uptake, biodistribution, and immune recognition. Experimental protocols for characterizing protein corona include incubation with plasma or serum followed by separation techniques (centrifugation, size-exclusion chromatography) and analysis via mass spectrometry or gel electrophoresis.
Cellular Uptake and Intracellular Fate: The high surface area and nanoscale dimensions enable efficient cellular internalization via endocytic pathways. Once internalized, nanoparticles may localize in specific organelles, potentially disrupting lysosomal function, mitochondrial activity, or nuclear integrity [50]. Tracking methodologies include fluorescent labeling combined with confocal microscopy, transmission electron microscopy, and elemental analysis.
Size-Dependent Effects: Size profoundly influences nanomaterial biodistribution, clearance, and toxicity. Particles below 5.5 nm typically undergo renal clearance, while larger particles tend to accumulate in the liver and spleen [50]. Needle- or plate-shaped particles may physically disrupt cell membranes, while spherical particles generally exhibit different uptake patterns [50]. Rigorous nanotoxicology assessment must include comprehensive size characterization using dynamic light scattering, electron microscopy, and analytical ultracentrifugation.
Nanotoxicity Mechanisms Pathway: This diagram illustrates the sequential pathways from nanomaterial exposure through cellular interactions to potential adverse biological outcomes.
Experimental Protocols for Biocompatibility Assessment
In Vitro Cytocompatibility Testing
Protocol 1: Standardized Cytotoxicity Assessment (ISO 10993-5)
- Cell Lines: Use relevant cell types based on intended application (e.g., L929 fibroblasts for general screening, primary human cells for target-specific assessment)
- Extract Preparation: Incubate nanomaterial (0.1-1 mg/mL) in complete cell culture medium for 24±2 hours at 37°C
- Exposure Conditions: Prepare serial dilutions of extracts; include negative (HDPE) and positive (latex) controls
- Endpoint Assessments:
- MTT/XTT assay: Measure mitochondrial activity after 24-72 hours exposure
- Live/Dead staining: Calculate viability ratio using calcein-AM/ethidium homodimer
- LDH release: Quantify membrane integrity after 24 hours exposure
- Acceptance Criteria: >70% viability relative to negative control for non-cytotoxic classification
Protocol 2: Oxidative Stress Measurement
- Cell Preparation: Seed cells at appropriate density and allow attachment for 24 hours
- Nanomaterial Exposure: Treat with sub-cytotoxic concentrations (determined from Protocol 1) for 2-24 hours
- ROS Detection:
- Load cells with 10μM DCFH-DA for 30 minutes
- Wash with PBS and measure fluorescence (Ex/Em: 485/535nm)
- Include positive control (tert-butyl hydroperoxide)
- Antioxidant Depletion: Measure glutathione levels using DTNB assay
- Inflammatory Markers: Quantify IL-6, IL-8, and TNF-α release via ELISA
Hemocompatibility Assessment (ASTM F756-17)
Protocol 3: Hemolysis Testing
- Blood Collection: Draw human blood in heparinized tubes from healthy donors
- Sample Preparation: Incubate nanomaterials (0.1-10 mg/mL) with 1% RBC suspension for 3 hours at 37°C
- Controls: Include negative (PBS) and positive (1% Triton X-100) controls
- Analysis: Centrifuge and measure hemoglobin release at 540nm
- Calculation: % Hemolysis = (Sample OD - Negative OD)/(Positive OD - Negative OD) × 100
- Acceptance Criteria: <5% hemolysis for blood-contacting devices
Table 3: Advanced characterization techniques for nanotoxicology assessment.
| Technique | Application | Key Parameters Measured | Experimental Considerations |
|---|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic size distribution, aggregation state | Size, polydispersity index, stability in physiological media | Must be complemented by microscopy (size overestimation possible) |
| Transmission Electron Microscopy (TEM) | Primary particle size, morphology, internal structure | Actual particle dimensions, shape, aggregation state | Requires sample drying, may not reflect hydrated state |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Elemental composition, biodistribution quantification | Metal content, cellular uptake, distribution in organs | Extremely sensitive, requires appropriate sample digestion |
| Flow Cytometry | Cellular uptake, population-level effects | Internalization efficiency, oxidative stress, viability | Requires fluorescent labeling or light-scatter properties |
| Single-Cell Profiling (SCP) with AI | High-resolution nanocarrier mapping at cellular level [51] | Biodistribution quantification, cell segmentation based on parameters | Utilizes deep learning on 3D imaging data; detects ultra-low doses [51] |
Emerging Technologies and Future Directions
The field of nanotoxicology is rapidly evolving with several emerging technologies enhancing assessment capabilities. Artificial intelligence is revolutionizing nanotoxicology through approaches like Single-Cell Profiling (SCP), which combines high-resolution imaging with deep learning algorithms to precisely map nanocarrier distribution at the cellular level [51]. This method has demonstrated sensitivity 100-1000 times greater than conventional approaches, capable of detecting nanocarriers at ultra-low dosages of 0.0005 mg/kg [51].
Advanced material design strategies are incorporating "safer-by-design" principles that proactively address potential toxicity during the development phase rather than as a post-hoc consideration. These include surface modifications to reduce reactivity, compositional adjustments to enhance biodegradability, and morphological controls to optimize clearance profiles [50]. Functionalization with targeting ligands improves specificity while minimizing off-target effects, and the development of theranostic agents combines diagnostic and therapeutic functions for more controlled application [41] [42].
The regulatory landscape is simultaneously evolving to address the unique challenges posed by nanoscale medical devices. The FDA and other regulatory bodies are developing adaptive frameworks that recognize the dynamic nature of nano-bio interactions, with increased emphasis on real-world performance monitoring and lifecycle management [37] [52]. For AI-enabled nanodevices, the FDA is exploring novel performance metrics and monitoring strategies to address potential performance degradation or data drift in clinical environments [53] [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key research reagents and materials for nanotoxicology and biocompatibility assessment.
| Reagent/Material | Function/Application | Key Characteristics | Experimental Notes |
|---|---|---|---|
| Polydimethylsiloxane (PDMS) | Flexible substrates, microfluidics [2] | Biocompatible, transparent, gas-permeable | Hydrophobic surface may require plasma treatment for cell culture |
| Polyethylene Glycol (PEG) | Surface functionalization, stealth coating [41] | Reduces protein adsorption, extends circulation half-life | PEG density and molecular weight critically impact performance |
| Molecularly Imprinted Polymers (MIPs) | Target-specific recognition in biosensors [51] | Synthetic receptors with precise molecular recognition | Core-shell designs with PBA cores enable electrochemical signaling [51] |
| Prussian Blue Analogs (PBA) | Redox-active core in electrochemical sensors [51] | Facilitates electrochemical signal transduction | Used as core material in printable nanoparticle systems [51] |
| Gold Nanoparticles | Biomedical sensors, conductive components [2] | Biocompatible, surface plasmon resonance properties | Surface charge significantly influences cellular uptake and toxicity |
| Quantum Dots | Imaging agents, diagnostic sensors [42] | Superior optical properties, tunable emission | Potential heavy metal content requires careful toxicity assessment |
| Liposomes | Drug delivery vehicles, membrane models | Biocompatible, customizable surface properties | Surface charge and lipid composition determine biological interactions |
| Carbon Nanolattices | Structural components, tissue engineering [51] | High specific strength, lightweight architectural properties | ML-optimized designs show 118% increased tensile strength [51] |
The comparative analysis of nanoscale and microscale medical devices reveals a complex tradeoff between enhanced functionality and increased safety considerations. While nanoscale devices offer unprecedented capabilities for targeted interactions at the molecular level, they demand more sophisticated toxicological assessment methodologies that account for their dynamic behaviors in biological systems. The emerging toolkit for nanotoxicology—encompassing advanced characterization techniques, AI-enhanced monitoring, safer-by-design principles, and functionalization strategies—provides a robust foundation for addressing these challenges.
For researchers and drug development professionals, successful clinical translation requires integrated assessment strategies that consider the entire lifecycle of nanoscale devices, from initial material synthesis through biological interactions to eventual clearance or degradation. The regulatory landscape continues to evolve in parallel with technological advancements, emphasizing real-world performance monitoring and adaptive safety frameworks. By systematically addressing biocompatibility and nanotoxicology through the comprehensive approaches outlined in this guide, the field can harness the remarkable potential of nanoscale medical devices while ensuring patient safety and therapeutic efficacy.
Overcoming Complex Manufacturing and Scalability Barriers
The advancement of medical science is increasingly dependent on the ability to engineer devices at micro- and nanoscale dimensions. These devices, ranging from advanced biosensors to targeted drug delivery systems, promise revolutionary improvements in diagnostics and therapeutics. However, their transition from laboratory prototypes to commercially viable products is hampered by significant manufacturing and scalability challenges. The core of this issue lies in the fundamental trade-offs between resolution, throughput, material compatibility, and cost that differ dramatically between microscale and nanoscale fabrication processes. This guide provides an objective comparison of these manufacturing paradigms, offering researchers and developers a clear framework for selecting and optimizing fabrication strategies based on empirical data and proven experimental protocols. Understanding these barriers is the first step toward developing robust, scalable manufacturing processes that can bring innovative nanoscale and microscale medical devices from the research bench to clinical application.
Comparative Analysis of Fabrication Techniques
Quantitative Comparison of Direct-Write Fabrication Methods
Direct-write techniques enable computer-controlled deposition and patterning of materials without the need for masks, offering flexibility for prototyping and complex device fabrication. The capabilities of these methods vary significantly, as detailed in Table 1.
Table 1: Comparison of Laser-Based Direct-Write Fabrication Processes [54]
| Technique | Laser Type | Resolution | Compatible Materials | Key Limitations |
|---|---|---|---|---|
| Selective Laser Sintering/Melting (SLS/SLM) | Continuous Wave (CW), Long Pulse (LP) | 50 μm | Ceramics, Polymers, Metals | Requires powder precursor; High temperature; Layered fabrication |
| Micro-laser Sintering | Long Pulse (LP) | 20 μm | Ceramics, Metals | Requires powder precursor; High temperature; Layered fabrication |
| Laser Machining | CW, Excimer (EX), LP, SP, USP | 15 nm | Ceramics, Polymers, Metals | Top-down material removal process |
| Matrix-Assisted Pulsed-Laser Evaporation Direct Write (MAPLE DW) | Excimer (EX) | 10 μm | Polymers, Metals, Ceramics, Biomolecules | Multiple processing parameters; Layered fabrication |
| Stereolithography (SLA) | Continuous Wave (CW) | 1 μm | Polymers, Ceramic Composites, Biomolecule Composites | Requires photopolymerization; Layered fabrication |
| Two-Photon Polymerization (2PP) | Ultra-Short Pulse (USP) | <100 nm | Polymers, Ceramic Composites | Requires photopolymerization |
Emerging Non-Laser Direct-Writing Technologies
Beyond laser-based methods, other advanced techniques are addressing historical bottlenecks in nanoscale fabrication. Capillary-force deposition is one such method, a non-electrochemical approach that uses a glass capillary to form a meniscus of ink for material transfer. This technique offers sub-micrometer resolution (features below 1 µm) and is noted for its controlled deposition without splashes, high repeatability, and compatibility with a broad range of inks including conductive materials, polymers, and quantum dots on flat, flexible, and 3D substrates without requiring vacuum conditions [55].
In contrast, electrophotonic devices represent a different approach by combining electronic and optical modalities for diagnostic applications. Key methodologies in this domain include [13]:
- Closed Bipolar Electrochemistry (CBE): Couples electron transfer reactions in an analytical cell to an optical readout (e.g., colorimetric or fluorescent) in a separate reporter cell, minimizing background interference.
- Localized Surface Plasmon Resonance (LSPR): Utilizes the resonant oscillation of electrons in noble metal nanoparticles to detect changes in the local dielectric environment, which is useful for biomolecular sensing.
- Zero-Mode Waveguides (ZMWs) and Metamaterials: Emerging nanophotonics approaches that enable the study of single molecules and exhibit optical properties not found in nature.
Experimental Characterization and Hazard Assessment Protocols
Dynamic Characterization of MEMS/NEMS Devices
Verifying that microelectromechanical systems (MEMS) and nanoelectromechanical systems (NEMS) perform as designed requires specialized characterization techniques. A standard experimental workflow for dynamic characterization is outlined below.
Dynamic MEMS/NEMS characterization workflow [56]
Detailed Experimental Protocol for MEMS/NEMS Characterization [56]:
Device Actuation: Apply controlled forces to the device using one or more of the following methods:
- Electrostatic Actuation: Apply DC bias with superimposed AC signals to excite resonant structures.
- Piezoelectric Actuation: Use piezoelectric materials to generate strain in response to applied voltages.
- Thermal Actuation: Leverage thermal expansion differences in multilayer structures.
- Photothermal Actuation: Utilize focused laser pulses for parametric excitation of nanomechanical resonators.
Motion Measurement: Quantify device displacement and dynamics using high-sensitivity techniques:
- Laser Doppler Vibrometry (LDV): A non-contact method capable of measuring out-of-plane motions with sub-nanometer resolution and high temporal resolution.
- Stroboscopic Interferometry: Uses phase-shifting interferometry with stroboscopic illumination to create 3D motion maps of periodically moving structures.
- In-Situ SEM Manipulation: Allows for nanomanipulation and real-time observation within a scanning electron microscope.
- Computer Microvision: Tracks in-plane motions by analyzing video microscopy data with nanometer accuracy.
Data Analysis and Parameter Extraction: Process the measured data to extract key device parameters, including resonant frequency, quality factor (Q), damping coefficients, and linear/nonlinear stiffness. This often involves fitting experimental data to analytical models.
Model Verification: Compare extracted parameters with design predictions and finite element simulations. This step often reveals unmodeled effects and drives design refinements, creating an iterative development cycle.
Quantitative Framework for Nanomaterial Hazard Potency Assessment
A critical, often overlooked scalability barrier for medical devices incorporating engineered nanomaterials (ENMs) is the comprehensive assessment of their potential pulmonary toxicity. A quantitative framework has been developed to group ENMs by hazard potency using rodent pulmonary inflammation data, which can inform occupational exposure limits (OELs) during manufacturing [57].
Nanomaterial hazard potency assessment framework [57]
Detailed Experimental Protocol for Hazard Potency Grouping [57]:
Database Construction: Compile a database from in vivo rodent studies (e.g., from sources like NIOSH, CIIT, ENPRA) including data on animal species, strain, sex, material type, exposure route, and dose-response information for pulmonary inflammation. The deposited mass dose of particles in the lungs (µg/g lung) is used as a normalized dose metric.
Benchmark Dose (BMD) Modeling: Model the continuous dose-response relationships for pulmonary inflammation. The BMD is the estimated dose associated with a specific, predetermined level of inflammatory response (Benchmark Response or BMR), which is considered biologically significant and relevant to workers.
Hierarchical Clustering: Use statistical clustering on the BMD estimates to identify groups of materials with similar inflammatory potency. This empirical grouping can result in potency variations by factors of two to 100 between different groups.
Predictive Modeling: Employ a classification random forest model to identify the most important physicochemical properties (e.g., size, surface chemistry) that predict the hazard potency group. This model can then be used to estimate the group assignment for new ENMs based solely on their physicochemical information, facilitating early risk assessment.
Essential Research Reagent Solutions
The experimental protocols and fabrication methods described rely on a suite of specialized materials and reagents. Table 2 details key components essential for research and development in this field.
Table 2: Key Research Reagent Solutions for Micro/Nano Device Fabrication and Characterization
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Photoinitiators | Initiate polymerization in Stereolithography (SLA) and Two-Photon Polymerization (2PP) [54] | Molecules that form radicals upon photon absorption to start chain-growth polymerization. |
| Metallic Nanoparticles (Au, Ag) | Enable Localized Surface Plasmon Resonance (LSPR) sensing [13] | Noble metal nanoparticles with a negative real dielectric constant; electron oscillation creates a localized plasmon resonance. |
| Electrochromic Indicators (e.g., Methyl Viologen) | Provide optical readout in Closed Bipolar Electrochemistry (CBE) [13] | Undergo a colorimetric change upon electron transfer in the reporter cell of a CBE system. |
| Electrofluorigenic Reporters (e.g., Resazurin/Resorufin) | Enable ultrasensitive fluorescence detection in CBE [13] | Redox-sensitive fluorescence; resazurin is converted to highly emissive resorufin electrochemically. |
| Functional Inks | Used in direct-write techniques (e.g., Capillary-force deposition) [55] | Can contain conductive materials, polymers, quantum dots, or biomolecules for deposition. |
| Ceramic & Metal Powders | Precursor materials for Selective Laser Sintering/Melting [54] | Sub-micrometer to 10µm grains that are fused layer-by-layer using a high-power laser. |
The journey to overcome the manufacturing and scalability barriers for micro- and nanoscale medical devices is complex and multifaceted. As the comparative data shows, no single fabrication technique universally excels across all parameters; the choice involves strategic trade-offs between resolution, material compatibility, and scalability. Success in this domain requires an integrated approach that combines advanced fabrication methods, robust experimental characterization, and proactive safety assessment. By leveraging the frameworks and protocols outlined in this guide—from laser-based fabrication and electrophotonic sensing to dynamic MEMS characterization and nanomaterial hazard grouping—researchers and product developers can make more informed decisions. This will ultimately accelerate the development of safe, effective, and commercially viable miniaturized medical devices that push the boundaries of what is possible in patient care.
Functionalization and Surface Modification Strategies for Enhanced Performance
The performance of biomedical devices, whether at the micro or nanoscale, is fundamentally governed by their surface characteristics. Functionalization and surface modification have emerged as critical engineering strategies to enhance biocompatibility, improve targeting precision, extend functional lifespan, and enable novel functionalities that bulk material properties alone cannot provide. Within the broader thesis comparing nanoscale versus microscale medical devices, surface modification approaches present distinct considerations, challenges, and opportunities at each scale. At the nanoscale, surface modifications primarily aim to control biological interactions at the molecular level, enhancing cellular uptake, targeted drug delivery, and evasion of immune responses [41]. In contrast, microscale devices more frequently utilize surface engineering to improve tissue integration, reduce bacterial colonization, and enhance the mechanical durability of implants [2] [58]. This guide systematically compares the surface modification strategies employed for nanoscale and microscale medical devices, providing objective performance comparisons and detailed experimental methodologies to inform research and development across both domains.
Material Platforms and Their Native Surface Properties
The selection of base materials forms the foundation for any surface modification strategy, as intrinsic properties dictate which functionalization approaches are feasible and effective.
Table 1: Fundamental Material Platforms for Medical Devices
| Material Category | Example Materials | Native Surface Properties | Primary Device Applications |
|---|---|---|---|
| Polymers | PEEK, PDMS, Polyimide, PLA, SU-8 | Hydrophobic, chemically inert, low surface energy | Orthopedic implants, microfluidics, flexible substrates, drug delivery systems [2] [59] |
| Metals | Titanium, Nickel, Gold, Nitinol | High surface energy, prone to corrosion, bioactive | Cardiovascular stents, electrodes, surgical tools, implants [2] [60] |
| Semiconductors | Silicon, Silicon Carbide, Graphene | Precise surface chemistry, tunable electronic properties | Biosensors, MEMS/NEMS, diagnostic tools [2] [61] |
| Ceramics & Piezoelectrics | PZT, Aluminum Nitride, Zinc Oxide | Polar surfaces, chemically stable, responsive to stimuli | Energy harvesters, ultrasonic transducers, actuators [2] |
| 2D Materials | Graphene, Transition Metal Dichalcogenides | Ultra-high surface area, quantum confinement effects | Advanced sensors, therapeutic platforms [2] |
For microscale devices, materials like medical-grade PEEK are valued for their biocompatibility and bone-like mechanical modulus but suffer from inherent bio-inertness that limits osseointegration [59]. Similarly, silicon , the workhorse of MEMS technology, offers excellent electronic properties but requires surface passivation and functionalization for stable operation in biological environments [2]. At the nanoscale, materials such as gold nanoparticles and quantum dots provide versatile platforms for functionalization but present challenges regarding potential toxicity and long-term stability in physiological conditions [41].
Surface Modification Techniques: Scale-Dependent Methodologies
Chemical Functionalization Strategies
Chemical modification techniques vary significantly between nanoscale and microscale devices due to differences in surface area-to-volume ratios and penetration depths required.
Nanoscale Devices: PEGylation is a cornerstone technique, wherein polyethylene glycol (PEG) chains are covalently attached to nanoparticle surfaces. This process creates a hydrophilic protective layer that reduces opsonization, prolongs systemic circulation, and enhances accumulation at target sites [41]. Experimental data demonstrates that PEGylated liposomes exhibit circulation half-lives up to 3-5 times longer than their unmodified counterparts [41]. Ligand conjugation represents another critical strategy, involving the attachment of targeting molecules (e.g., antibodies, peptides, aptamers) to nanoparticle surfaces via chemical linkers. For instance, folic acid-functionalized nanoparticles have shown 8-10 times greater cellular uptake in folate receptor-positive cancer cells compared to non-targeted equivalents [41].
Microscale Devices: Plasma treatment is widely employed to modify polymer surfaces like PEEK and PDMS. Exposure to oxygen or ammonia plasma introduces polar functional groups (e.g., hydroxyl, amine, carboxyl) that significantly enhance surface energy and wettability. Quantitative studies report water contact angle reductions from 80° to 30° following oxygen plasma treatment of PEEK, resulting in substantially improved protein adsorption and cell adhesion [59]. Chemical etching techniques utilize strong acids or bases to create micro- and nano-topographies on implant surfaces. Titanium implants treated with acid etching exhibit increased surface roughness (Ra values typically 1-3 μm), which has been correlated with 25-40% greater bone-implant contact strength in mechanical testing [58] [60].
Physical and Coating-Based Approaches
Physical modification techniques alter surface topography or apply functional coatings without necessarily changing chemical composition.
Nanoscale Coatings: Layer-by-layer (LbL) assembly enables precise nanoscale coating thickness through alternating deposition of polyelectrolytes. This technique allows for controlled drug release kinetics, with studies demonstrating near-zero-order release profiles over 30 days for certain antibiotic coatings [58]. Biomimetic coatings replicate natural structures; for example, nacre-inspired coatings on implants have shown a 300% increase in fracture toughness compared to conventional coatings [58].
Microscale Surface Structuring: Additive manufacturing, particularly 3D printing of PEEK, enables the creation of controlled surface porosity. Implants with 60-70% porosity and pore sizes of 300-500 μm demonstrate significantly enhanced bone ingrowth, with histological analysis showing 50% more vascularization after 4 weeks in vivo compared to solid implants [59]. Laser surface texturing creates precise micro-patterns on metal implants that direct cell alignment and growth. Grooved patterns with 10-25 μm width and 5-10 μm depth have demonstrated the ability to increase endothelial cell migration rates by 35%, accelerating vascularization around cardiovascular stents [60].
Table 2: Performance Comparison of Surface Modification Techniques
| Modification Technique | Scale Applicability | Key Performance Metrics | Experimental Outcomes | Limitations |
|---|---|---|---|---|
| PEGylation | Primarily Nanoscale | Circulation half-life, Targeting specificity | 3-5x longer circulation; 8-10x enhanced cellular uptake [41] | Potential immune response to PEG; Limited tissue penetration |
| Plasma Treatment | Primarily Microscale | Water contact angle, Protein adsorption | Contact angle reduction from 80° to 30°; 2x increase in protein adsorption [59] | Temporary effect; Aging of modified surfaces |
| Acid Etching | Microscale | Surface roughness, Bone-implant contact | Ra values of 1-3 μm; 25-40% greater bone contact strength [58] [60] | Potential material degradation; Limited chemical functionality |
| Layer-by-Layer Assembly | Both Scales | Coating thickness, Drug release kinetics | Controlled release over 30 days; 300% increase in fracture toughness [58] | Time-consuming process; Complex quality control |
| 3D Printing | Microscale | Porosity, Pore size, Bone ingrowth | 60-70% porosity; 50% more vascularization [59] | High temperature requirements; Potential warping |
Experimental Protocols for Surface Modification and Characterization
Protocol 1: PEGylation of Nanoparticles for Enhanced Circulation
This protocol details the standard methodology for creating PEGylated liposomal nanoparticles, a common drug delivery platform [41].
Materials and Reagents:
- DSPE-PEG2000: Phospholipid with polyethyleneglycol headgroup (2 kDa), serves as stealth coating material
- Cholesterol: Enhances membrane stability and prevents premature drug release
- Hydrogenated soy phosphatidylcholine (HSPC): Primary structural lipid component
- Chloroform: Organic solvent for lipid dissolution
- Phosphate Buffered Saline (PBS): Hydration medium for liposome formation
- Drug payload: Therapeutic agent (e.g., doxorubicin for cancer applications)
Procedure:
- Dissolve HSPC, cholesterol, and DSPE-PEG2000 at 55:40:5 molar ratio in chloroform
- Evaporate organic solvent using rotary evaporation (40°C, 30 minutes) to form thin lipid film
- Hydrate lipid film with PBS (pH 7.4) at 65°C with vigorous agitation for 1 hour
- Size reduction through sequential extrusion through polycarbonate membranes (400 nm, 200 nm, 100 nm)
- Purify via dialysis or size exclusion chromatography to remove non-encapsulated drug
- Characterize particle size (target: 80-120 nm) using dynamic light scattering and zeta potential
Performance Validation:
- Compare circulation half-life of PEGylated vs. non-PEGylated particles in animal models
- Quantify drug accumulation at target site using fluorescence imaging or HPLC
- Assess macrophage uptake in vitro using flow cytometry
Protocol 2: Plasma Surface Modification of PEEK Implants
This protocol describes oxygen plasma treatment to enhance the bioactivity of PEEK orthopedic implants [59].
Materials and Reagents:
- Medical grade PEEK: Substrate material (sheets, 3D-printed constructs, or machined implants)
- Oxygen gas (high purity): Plasma source gas
- Ethanol (70%): Cleaning solvent
- Deionized water: Rinsing agent
Equipment:
- Plasma cleaner/etcher with RF power source (typically 13.56 MHz)
- Vacuum pump system
- Mass flow controllers for gas regulation
Procedure:
- Clean PEEK substrates with 70% ethanol followed by deionized water rinsing
- Dry samples in nitrogen stream and place in plasma chamber
- Evacuate chamber to base pressure (typically 10-100 mTorr)
- Introduce oxygen gas at controlled flow rate (10-50 sccm)
- Ignite plasma at power density of 0.5-2.0 W/cm²
- Treat samples for 30 seconds to 10 minutes (optimize based on desired effect)
- Vent chamber and remove samples for immediate use or further modification
Performance Validation:
- Measure water contact angle using goniometry (target: <40°)
- Quantify protein adsorption using radiolabeling or colorimetric assays
- Assess cell adhesion and proliferation using osteoblast cell cultures
- Evaluate bone-implant contact in animal models (histomorphometry)
Surface Modification Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Surface Modification Studies
| Reagent/Material | Function | Application Scale | Key Considerations |
|---|---|---|---|
| DSPE-PEG Derivatives | Stealth coating for nanoparticles | Nanoscale | PEG molecular weight (1k-5k Da), end-group functionality [41] |
| Silane Coupling Agents | Surface priming for further modification | Both Scales | Specific reactivity (amino, epoxy, thiol), hydrolysis stability [2] |
| Medical Grade PEEK | High-performance polymer substrate | Microscale | Crystallinity, melt viscosity, impurity profile [59] |
| Oxygen Plasma | Surface activation and functionalization | Microscale | Power density, exposure time, pressure parameters [59] |
| Titanium Dioxide Nanotubes | Nanostructured coating for implants | Both Scales | Tube diameter (30-100 nm), length, crystallinity [58] |
| RGD Peptide Sequences | Cell adhesion promotion | Both Scales | Concentration, spatial presentation, stability [58] |
| Gold Nanoparticles | Versatile platform for functionalization | Nanoscale | Size uniformity, surface chemistry, conjugation efficiency [41] |
Comparative Performance Analysis: Nanoscale vs. Microscale Devices
The functionalization outcomes and performance metrics differ substantially between nanoscale and microscale devices due to their distinct size regimes and primary applications.
Biocompatibility and Immune Response: Nanoscale devices benefit from surface modifications that minimize protein fouling and macrophage recognition. PEGylation creates a hydration barrier that reduces protein adsorption by up to 80% compared to unmodified surfaces [41]. Microscale devices focus on reducing bacterial colonization and foreign body response. Silver nanoparticle coatings on titanium implants have demonstrated 99% reduction in S. aureus and E. coli colonization while maintaining fibroblast viability above 90% [58].
Targeting Efficiency: Nanoscale devices achieve molecular-level targeting through surface-conjugated ligands. Transferrin-functionalized nanoparticles show 15-20 times greater accumulation in brain tumors compared to non-targeted counterparts [41]. Microscale devices utilize topological cues for cellular guidance. Microgrooved surfaces (10-20 μm width) align endothelial cells with 85% directional orientation, significantly accelerating vascular healing around stents [60].
Functional Lifespan: Nanoscale drug carriers employ surface modifications to extend circulation time. PEGylated liposomes maintain therapeutic payloads for 48-72 hours compared to 2-8 hours for unmodified liposomes [41]. Microscale implants use surface treatments to enhance long-term stability. Hydroxyapatite-coated PEEK implants show less than 5% coating degradation after 12 months in simulated body fluid, compared to 25% degradation for uncoated controls [59].
Performance Outcomes by Device Scale
Surface modification strategies for medical devices continue to evolve with emerging trends focusing on multifunctional systems that combine diagnostic and therapeutic capabilities, stimuli-responsive surfaces that adapt to physiological conditions, and biomimetic approaches that precisely replicate natural structures [62]. The integration of artificial intelligence in nanomaterial design is accelerating the development of optimized surface modification protocols, potentially reducing development timelines from years to months [41]. For microscale devices, the convergence of additive manufacturing with surface functionalization enables patient-specific implants with biologically active surfaces [59]. Despite these advances, both nanoscale and microscale devices face shared challenges in standardization, scalability, and regulatory approval that must be addressed through continued interdisciplinary collaboration between materials scientists, engineers, and clinicians.
Addressing Regulatory Science Gaps and Evaluation Frameworks for Novel Devices
The development of medical devices, particularly those leveraging nanotechnology, operates within a complex regulatory framework designed to ensure safety and efficacy. The U.S. Food and Drug Administration's Center for Devices and Radiological Health (CDRH) has identified specific regulatory science priorities to address critical knowledge gaps, including the need to "modernize biocompatibility and biological risk evaluation of device materials" and "develop computational modeling technologies to support regulatory decision-making" [63]. These priorities are particularly relevant for nanoscale devices, which present unique challenges and opportunities compared to their microscale counterparts. The growing importance of this field is evidenced by the steady increase in FDA approvals for AI-enabled medical devices, which reached 139 in 2022 alone [64]. However, significant reporting gaps remain in regulatory submissions, with only 3.6% reporting race/ethnicity data and 81.6% failing to report the age of study subjects, potentially exacerbating algorithmic bias risks in novel devices [64].
The comparison between nanoscale and microscale medical devices represents a critical frontier in medical technology innovation. Nanoscale devices typically feature particles or structures with at least one dimension between 1-100 nanometers, while microscale devices generally range from 1-100 micrometers. This orders-of-magnitude difference in scale translates to fundamental variations in surface area-to-volume ratios, reactivity, and biological interactions that significantly impact device performance, safety profiles, and regulatory evaluation requirements. As the medical device industry increasingly incorporates nanoscale materials, understanding these distinctions becomes essential for researchers, developers, and regulatory professionals working to advance patient care through innovative technologies.
Quantitative Comparison of Nanoscale vs. Microscale Device Performance
A comparative study of poly(3-hydroxybutyrate) composites incorporating either nanoscale (n-BG) or microscale (m-BG) bioactive glass particles revealed significant performance differences across multiple parameters [65]. The systematic evaluation, which examined thermal, mechanical, and biological properties, provides valuable insights into how scale affects device characteristics critical for medical applications, particularly in tissue engineering.
Table 1: Comparative Performance of Nanoscale vs. Microscale Bioactive Glass Composites
| Performance Parameter | Nanoscale (n-BG) Composites | Microscale (m-BG) Composites | Measurement Method |
|---|---|---|---|
| Stiffening Effect | Significant stiffening | Moderate stiffening | modulus measurement |
| Thermal Properties | No significant differences from pure polymer | No significant differences from pure polymer | Thermal analysis |
| Surface Topography | Induced nanostructured topography | Minimal impact on surface structure | Scanning Electron Microscopy (SEM) |
| Protein Adsorption | Considerably improved | Moderate improvement | Total protein adsorption assay |
| In Vitro Bioactivity | High level of bioactivity | Moderate bioactivity | 30-day degradation in SBF |
| Water Absorption | Higher absorption | Lower absorption | Weight change in SBF |
| Cell Biocompatibility | Good biocompatibility with MG-63 cells | Good biocompatibility with MG-63 cells | Cell proliferation study |
The data demonstrates that nanoscale incorporation provides distinct advantages in mechanical reinforcement, surface characteristics, and bioactive properties, while maintaining excellent biocompatibility comparable to microscale composites. The significantly higher protein adsorption on n-BG composites suggests enhanced biointegration potential, which is crucial for tissue engineering applications where device-host interaction determines clinical success [65]. These performance advantages must be balanced against potential regulatory considerations, as novel surface characteristics and enhanced reactivity may require more extensive evaluation to meet CDRH's priority of modernizing biocompatibility assessment methods [63].
Experimental Protocols for Device Evaluation
Composite Fabrication and Material Characterization
The comparative evaluation of nanoscale versus microscale medical devices requires standardized experimental protocols to ensure valid performance comparisons. For composite material systems, the solvent casting technique provides a reproducible fabrication method [65]. The detailed methodology involves:
Material Preparation: Prepare polymer solutions using appropriate solvents (e.g., chloroform for P(3HB)). Disperse precise weight percentages (typically 10, 20, and 30 wt%) of nanoscale and microscale particles separately using ultrasonic homogenization to achieve uniform distribution.
Composite Formation: Cast the particle-polymer suspensions onto level glass plates using a doctor blade to control thickness. Allow controlled solvent evaporation under specified environmental conditions (temperature, humidity, and airflow).
Post-Processing: Vacuum-dry the resulting films to remove residual solvent. Precisely cut samples into standardized dimensions for subsequent testing using laser cutting or precision dies.
Structural Characterization: Analyze surface morphology using Scanning Electron Microscopy (SEM) at appropriate accelerating voltages and magnifications. Perform topological analysis using atomic force microscopy (AFM) for nanoscale surface features. Characterize chemical composition using Fourier-transform infrared spectroscopy (FTIR) and energy-dispersive X-ray spectroscopy (EDS).
Performance Evaluation Methodologies
Comprehensive device evaluation requires multiple standardized assays to assess functional performance:
Table 2: Standardized Testing Protocols for Device Evaluation
| Test Type | Protocol Description | Key Parameters Measured | Standard Reference |
|---|---|---|---|
| Mechanical Testing | Uniaxial tensile testing using universal testing machine | Elastic modulus, tensile strength, elongation at break | ASTM D638 |
| Thermal Analysis | Differential scanning calorimetry (DSC) and thermogravimetric analysis (TGA) | Glass transition temperature, melting temperature, thermal degradation | ASTM E794, E1131 |
| Protein Adsorption | Incubation with fluorescently-tagged protein solutions | Total adsorbed protein, adsorption kinetics | ISO/TR 13014 |
| In Vitro Bioactivity | Immersion in simulated body fluid (SBF) for 30 days | Surface apatite formation, weight change, ion release | ISO 23317 |
| Cytocompatibility | Culture with relevant cell lines (e.g., MG-63 osteoblasts) | Cell proliferation, viability, morphological assessment | ISO 10993-5 |
The in vitro degradation study deserves particular attention for bioactive devices. The protocol involves immersing accurately weighed samples (n≥5 per group) in SBF with controlled pH (7.4) and temperature (37°C) for predetermined intervals (e.g., 7, 14, 21, 30 days). The SBF solution should be refreshed periodically to maintain ion concentration. At each time point, remove samples for mass change measurement, surface characterization, and released ion analysis using inductively coupled plasma (ICP) spectroscopy [65].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful evaluation of nanoscale versus microscale medical devices requires specific research materials and reagents with carefully defined functions:
Table 3: Essential Research Materials for Device Development and Evaluation
| Material/Reagent | Function in Research | Application Example |
|---|---|---|
| Poly(3-hydroxybutyrate) [P(3HB)] | Biodegradable polymer matrix for composite formation | Base material for creating bioactive glass composites [65] |
| Bioactive Glass Particles | Provides bioactivity and enhances mechanical properties | Nanoscale vs. microscale comparison in composite systems [65] |
| Simulated Body Fluid (SBF) | Evaluates bioactivity and degradation in physiological conditions | In vitro testing of apatite formation on device surfaces [65] |
| MTT/XTT Reagents | Measures cell viability and proliferation through metabolic activity | Cytocompatibility testing with relevant cell lines [65] |
| Fluorescently-Tagged Proteins | Quantifies protein adsorption on material surfaces | Evaluation of biointegration potential [65] |
| Methyl Viologen | Electrochromic indicator for sensing platforms | Colorimetric readout in electrophotonic diagnostic devices [13] |
| Resazurin/Resorufin | Redox-sensitive fluorescence indicator | Ultrasensitive detection in electrofluorigenic assays [13] |
| Gold Nanoparticles | Plasmonic material for sensing platforms | LSPR-based detection elements [13] |
The selection of appropriate materials extends beyond basic composition to include critical physical characteristics. For particle-based systems, size distribution, surface chemistry, and crystallinity must be carefully controlled and characterized. Cell culture components should include relevant cell lines matching the intended application (e.g., MG-63 osteoblasts for bone tissue engineering) [65], with culture conditions optimized to maintain phenotype throughout testing. Analytical reagents should be of suitable purity with proper validation of sensitivity and specificity for intended measurements.
Regulatory Evaluation Frameworks and Validation Approaches
The evaluation of novel medical devices requires structured frameworks that address both performance characteristics and regulatory requirements. The CDRH has emphasized the importance of leveraging "Big Data" for regulatory decision-making and employing evidence synthesis across multiple domains [63]. A proposed evaluation framework for wearable devices includes 27 distinct criteria across three domains: 12 for everyday use by users, 6 on device functionality, and 9 on infrastructure for developing research infrastructure [66]. This systematic approach can be adapted for nanoscale versus microscale device comparisons to ensure comprehensive assessment.
The Graphical Evaluation and Review Technique (GERT) provides a valuable approach for modeling complex systems with stochastic characteristics, enabling multi-metric assessment including success probability, operational time, and completion degree [67]. For regulatory evaluation, this methodology can be extended to assess device performance across multiple parameters simultaneously, rather than relying on single outcome measures. This aligns with the CDRH priority to "develop methods and tools to improve and streamline clinical trial design" [63].
A critical consideration in regulatory evaluation is the transparent reporting of demographic and performance data. Current analyses of FDA-approved AI/ML devices reveal significant reporting gaps, with only 22.1% specifying patient demographics in algorithmic testing data [64]. This underscores the importance of comprehensive documentation that includes racial/ethnic composition, socioeconomic diversity, and age distribution of study populations to identify potential algorithmic biases. Furthermore, only 46.1% of devices provided comprehensive detailed results of performance studies, indicating substantial room for improvement in regulatory transparency [64].
The comparative evaluation of nanoscale versus microscale medical devices reveals significant performance advantages at the nanoscale, particularly in mechanical properties, surface characteristics, and bioactive potential. These advantages must be balanced against potential regulatory considerations and the need for more comprehensive characterization. The evolving regulatory landscape, with its emphasis on modernizing biocompatibility assessment, leveraging real-world evidence, and addressing algorithmic bias, presents both challenges and opportunities for device developers.
Future progress in this field will depend on closing critical regulatory science gaps, particularly in standardized evaluation methods for novel nanoscale properties, long-term safety assessment, and computational modeling approaches. Additionally, improved transparency in regulatory submissions, with complete demographic reporting and comprehensive performance data, will be essential for ensuring the equitable deployment of advanced medical devices across diverse patient populations. As the CDRH continues to prioritize regulatory science advancement, researchers and developers have an opportunity to contribute to this evolving framework through rigorous, transparent, and comprehensive device evaluation.
The Role of AI and Smart Manufacturing in Process Optimization and Quality Control
The manufacturing of medical devices, particularly at the micro and nanoscale, demands unprecedented levels of precision, quality, and traceability. Artificial Intelligence (AI) and smart manufacturing paradigms are fundamentally transforming how these devices are designed, produced, and verified. Within the context of a broader thesis comparing nanoscale and microscale medical devices, these technologies provide the essential toolkit for navigating the unique challenges posed by each scale. For nanoscale devices, such as those used for targeted drug delivery, AI enables the precise control and quality verification of features and functions that are beyond human sensory perception [4]. For microscale devices, including many diagnostic tools, AI-driven automation ensures complex assembly with sub-micron accuracy and high-throughput quality control [68]. This guide objectively compares the performance of AI-enabled systems against traditional methods, providing experimental data and protocols relevant to researchers and developers working at the intersection of advanced manufacturing and biomedical innovation.
Smart Manufacturing Technologies: Core Architectures
The foundation of modern medical device manufacturing lies in the integration of several interconnected technologies that create a digital thread from design to delivered product.
The Industrial Internet of Things (IIoT) and Data Acquisition
The IIoT forms the sensory nervous system of a smart factory. A network of interconnected sensors embedded in production equipment collects real-time data on parameters critical to medical device quality, including temperature, vibration, pressure, and machine cycle times [68]. This continuous data stream is the essential feedstock for all subsequent AI and analytics. In nanomaterial synthesis, for example, sensors monitor reaction conditions in real-time, providing the data necessary to ensure batch-to-batch consistency [42].
Digital Twins for Virtual Process Modeling
A digital twin is a dynamic virtual replica of a physical manufacturing asset or process. For medical device manufacturing, digital twins allow engineers to simulate and optimize production lines, test changes, and run "what-if" scenarios without disrupting actual production [68]. This is particularly valuable for scaling up the fabrication of novel micro/nano-devices from laboratory prototypes to industrial production, as it de-risks the process and accelerates time-to-market.
AI and Machine Learning for Predictive Analytics
Machine learning (ML) algorithms analyze the vast datasets generated by IIoT and digital twins to uncover hidden patterns and correlations. ML is the dominant AI technology in manufacturing, with key applications including:
- Predictive Maintenance: Forecasting equipment failures by analyzing vibration and thermal data to minimize unplanned downtime [69] [70].
- Process Optimization: Dynamically adjusting production parameters to maximize yield and minimize waste [68].
- Generative AI: Accelerating the design of novel device components by rapidly generating and evaluating countless design iterations optimized for strength, material usage, and function [68].
Performance Comparison: AI vs. Traditional Methods
The integration of AI and smart technologies yields significant, measurable improvements across key manufacturing performance indicators. The following tables summarize quantitative data comparing AI-driven and traditional manufacturing approaches, with a focus on metrics critical to medical device production.
Table 1: Overall Impact of AI Integration on Manufacturing Efficiency
| AI Integration Level | Production Efficiency Improvement | Downtime Reduction |
|---|---|---|
| Basic AI Integration | 10% | 5% |
| Intermediate AI Integration | 25% | 15% |
| Advanced AI Integration | 40% | 30% |
| Full AI Integration | 60% | 50% |
Source: Research Findings on Smart Factory Performance [70].
Table 2: Comparative Analysis of Manufacturing Approaches for Medical Devices
| Performance Metric | Traditional Manufacturing | AI-Driven Smart Manufacturing | Experimental Data & Context |
|---|---|---|---|
| Defect Detection Rate | Relies on manual sampling and human vision. | Automated, real-time detection using computer vision. | AI-driven quality control can identify microscopic defects and assembly errors in real-time, ensuring stringent quality standards are met consistently [68]. |
| Predictive Maintenance | Reactive or time-based schedules. | Proactive, based on actual equipment condition. | AI-powered predictive maintenance is the leading application in manufacturing, minimizing equipment failures and reducing operational downtime [69]. |
| Production Output | Static or slowly improving. | Dynamically optimized. | Smart factory initiatives report a 10–20% uplift in production output post-implementation [71] [72]. |
| Equipment Downtime | Higher due to unplanned failures. | Significantly reduced. | Advanced AI integration can reduce downtime by up to 30% [70]. |
| Design & Prototyping Cycle | Iterative and physical prototype-dependent. | Rapid, simulation-driven iteration with generative AI. | Generative AI can rapidly assess thousands of design variations, drastically shortening development cycles for complex device components [68]. |
| Scalability for Nano/Micro Fabrication | Challenging; high variability at scale. | High; data-driven process control ensures consistency. | For nanoscale devices, AI integration is crucial for monitoring and controlling processes that are imperceptible to humans, ensuring batch-to-batch consistency [42] [4]. |
Experimental Protocols for Validating AI in Device Manufacturing
For researchers and engineers, validating the efficacy of an AI-driven system against a traditional baseline requires rigorous experimental design. The following protocols outline key methodologies.
Protocol 1: Validating an AI-Based Visual Inspection System
This protocol compares a new AI-powered computer vision system against traditional human inspection for detecting defects in a microfabricated component (e.g., a microfluidic chip).
1. Objective: To determine if the AI system achieves a statistically significant higher detection rate for critical defects while maintaining a false-positive rate below a specified threshold (e.g., <2%).
2. Methodology:
- Sample Preparation: Create a validated set of 1,000 finished components, where a subset (e.g., 100) has known, precisely characterized defects introduced during fabrication.
- Control Group: A team of three experienced quality control technicians will independently inspect the entire sample set using standard microscopy equipment.
- Test Group: The AI system, comprising high-resolution cameras and a trained convolutional neural network (CNN), will inspect the same sample set.
- Blinding: The identity of the samples will be blinded from both the human inspectors and the AI system operators.
- Data Collection: Record for each method: the number of true positives, false positives, true negatives, and false negatives.
3. Data Analysis:
- Calculate the sensitivity (recall), specificity, and precision for both methods.
- Perform a chi-squared test to compare the overall accuracy of the AI system against the aggregate human performance.
- The null hypothesis (that there is no difference in accuracy) is rejected if p < 0.05.
Protocol 2: Evaluating Predictive Maintenance for Nanofabrication Equipment
This protocol assesses the impact of an ML-based predictive maintenance model on the uptime and output quality of a critical piece of equipment, such as an electron beam lithography system used for nanoscale patterning.
1. Objective: To quantify the reduction in unplanned downtime and improvement in process stability after implementing a predictive maintenance system.
2. Methodology:
- Baseline Phase (3 months): Operate the equipment with its existing time-based maintenance schedule. Meticulously log all downtime events, categorizing them as planned (maintenance) or unplanned (failure). Record key process quality metrics (e.g., line width uniformity, defect density) for all production runs.
- Intervention Phase (3 months): Install IoT sensors (vibration, temperature, current) on the equipment. Train an ML model (e.g., a regression model) on the sensor data to predict impending failures. Maintenance is triggered only by ML model alerts.
- Data Collection: In both phases, track: Mean Time Between Failures (MTBF), Mean Time To Repair (MTTR), overall equipment effectiveness (OEE), and key quality metrics.
3. Data Analysis:
- Compare the MTBF and OEE between the two phases using a t-test.
- Analyze the trend of quality metrics to determine if process stability improved during the intervention phase, indicating more consistent device fabrication.
The workflow for implementing and testing such a system is outlined below.
Protocol 3: Generative AI for Optimizing a Micro-Dispenser Nozzle
This protocol uses generative AI to design a more efficient nozzle for a device that dispenses nanoliter volumes of fluid, optimizing for minimal clogging and flow consistency.
1. Objective: To generate a novel nozzle design that maintains structural integrity while achieving a 15% lower flow resistance compared to the baseline design.
2. Methodology:
- Input Constraints: Provide the generative design algorithm with operational constraints: inlet/outlet dimensions, maximum material stress, available build volume for manufacturing, and biocompatibility of the specified material.
- Generative Process: The AI runs a series of iterative simulations (e.g., Computational Fluid Dynamics and Finite Element Analysis) to explore the design space, generating hundreds of potential geometries.
- Validation: The top three AI-generated designs are fabricated using micro-scale additive manufacturing (e.g., micro-stereolithography).
- Testing: The physical prototypes are tested on a calibrated flow bench to measure pressure drop and inspected for manufacturing defects. Performance is compared to the legacy nozzle design.
3. Data Analysis:
- Compare the mean pressure drop of the AI-generated designs against the legacy design using a one-way ANOVA test.
- The generative AI is considered successful if at least one design meets the 15% improvement target with statistical significance (p < 0.05).
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful development and manufacturing of micro and nanoscale medical devices rely on a foundation of specialized materials and software tools.
Table 3: Essential Reagents and Materials for Micro/Nano Device Research and Production
| Item Name | Function / Application | Relevance to Scale |
|---|---|---|
| Stimuli-Responsive Hydrogels | 3D crosslinked networks that undergo structural changes in response to stimuli (pH, temperature, magnetic field) [4]. | Core material for nanoscale drug delivery devices and self-actuating micro-robots. |
| Functionalized Magnetic Nanoparticles | Nanoparticles (e.g., iron oxide) that can be manipulated using external magnetic fields [4]. | Used for guided navigation of nanoscale devices to target sites and for actuation. |
| Biocompatible Polymers (e.g., PLGA, PEG) | Synthetic polymers that degrade in the body with low immunogenicity. | Serve as the structural matrix or coating for both micro and nanoscale devices to ensure biocompatibility and controlled drug release. |
| Quantum Dots | Nanoscale semiconductor particles with unique fluorescent properties. | Used as contrast agents in nanoscale medical imaging and as biosensors in diagnostic devices [42]. |
| Gold Nanoparticles (AuNPs) | Spherical metal nanoparticles with tunable optical and electronic properties. | Used in nanoscale diagnostics (biosensors), as photothermal agents for therapy, and as drug carriers [42]. |
| Convolutional Neural Network (CNN) Software | A class of deep learning algorithms designed for processing pixelated data. | Essential for AI-driven visual inspection of micro-scale device features and nanoscale material morphology. |
| Machine Learning Platform (e.g., Python with scikit-learn) | Software environment for building predictive models. | Used to develop models for predictive maintenance, process optimization, and analyzing complex data from device performance tests. |
The objective data and experimental protocols presented in this guide compellingly demonstrate that AI and smart manufacturing are not merely incremental improvements but foundational shifts in the production of micro and nanoscale medical devices. The transition from traditional, often reactive, methods to data-driven, intelligent systems results in superior product quality, enhanced process reliability, and accelerated innovation cycles. For researchers and drug development professionals, mastering these technologies is no longer optional but essential for advancing the frontiers of nanomedicine and personalized therapeutics. The ability to robustly and consistently manufacture complex devices at these scales will directly translate to more effective, safer, and more accessible medical treatments.
Head-to-Head: Validating Performance, Efficacy, and Commercial Potential
The evolution of medical devices is increasingly propelled by advancements in material science, particularly through the manipulation of material dimensions. The comparison between nanoscale and microscale materials is a central focus in developing next-generation medical implants and devices. This guide provides a direct, data-driven performance comparison of these materials, focusing on three critical properties for biomedical application: bioactivity, mechanical integrity, and degradation behavior. Understanding these properties is essential for selecting appropriate materials for specific clinical applications, from orthopedic implants to targeted drug delivery systems. This analysis synthesizes current research to offer a clear, objective comparison for researchers and product development professionals.
Quantitative Performance Comparison of Select Materials
The following tables summarize key experimental data for representative nanoscale and microscale materials, highlighting their performance across bioactivity, mechanical, and degradation metrics.
Table 1: Performance Comparison of Biomaterials for Orthopedic Applications
| Material | Scale | Yield Strength (MPa) | Ultimate Tensile Strength (MPa) | Corrosion Rate (mm/year) | Cell Viability | ALP Activity (Fold Change) |
|---|---|---|---|---|---|---|
| Mg-0.3Sr-0.4Mn (SM04) Alloy [73] | Micro/Nano (microstructure) | 205 | 242 | 0.39 | >90% | 2.46 |
| Mg-0.3Sr (SM0) Alloy [73] | Micro | ~160 | ~217 | 0.85 | >90% | 1.0 (Baseline) |
| Pure Mg [73] | Macro/Micro | Insufficient | Insufficient | High (Rapid) | N/A | N/A |
| Fe (Iron) [73] | Macro | 200-250 | N/A | Very Slow | N/A | N/A |
| Zn (Zinc) [73] | Macro | 80-120 | N/A | Moderate | N/A | N/A |
Table 2: Characteristic Comparison of Nanoscale vs. Microscale Medical Devices
| Property | Nanoscale Devices | Microscale Devices |
|---|---|---|
| Primary Applications | Targeted drug delivery, advanced imaging, biosensing, tissue engineering [4] [74] | Bone fixation implants, structural supports, conventional drug delivery |
| Key Bioactivity Traits | Enhanced cellular uptake; promotes osteogenesis (e.g., Mg²⁺ ions); can be functionalized for targeted interaction [73] [74] | Good biocompatibility; bioactivity often depends on bulk material composition and surface roughness |
| Typical Mechanical Properties | High strength-to-weight ratios; properties can be highly tunable through nanostructuring [73] | Strength and modulus are more fixed; Mg alloys can approach bone-like modulus (~41-45 GPa) [73] |
| Degradation Profile | Controllable, surface-area-dependent degradation; can be engineered for specific rates and byproducts [73] [4] | Degradation rate is generally slower and less predictable; pure Mg degrades too rapidly [73] |
| Key Challenges | Complex characterization; potential nanotoxicology; regulatory hurdles [38] [74] | Rapid degradation leading to loss of mechanical integrity (Mg); stress shielding (stiffer materials) [73] |
Experimental Protocols for Performance Evaluation
To ensure the comparability and reliability of data, researchers employ standardized experimental protocols. The methodologies used to generate the key data cited in this guide are detailed below.
In Vitro Biodegradation and Biocompatibility Testing
This protocol is used to assess the degradation rate and initial biological response to materials, as performed on Mg-Sr-Mn alloys [73].
- Sample Preparation: Alloy samples are prepared through extrusion and machining. Samples are polished to a specific surface finish to ensure consistency.
- Immersion Test: Samples are immersed in a simulated body fluid (SBF) solution at a controlled temperature (e.g., 37°C) to mimic physiological conditions.
- Corrosion Rate Measurement: The degradation rate is quantified by measuring the hydrogen evolution over time or using mass loss techniques, with results calculated in mm/year.
- Cytocompatibility Assay: Cell viability is evaluated using standard assays (e.g., MTT assay). Extracts from the degraded materials or direct cell culture on the material surface are incubated with osteoblast cell lines (e.g., MC3T3-E1).
- Osteogenic Potential: Alkaline phosphatase (ALP) activity, an early marker of osteoblast differentiation, is measured spectrophotometrically after a defined culture period to assess bioactivity.
Biocompatibility Evaluation of Nanomaterials
For medical devices containing nanomaterials, ISO/TR 10993-22 provides specific guidance for biological evaluation within a risk management framework [38].
- Physical and Chemical Characterization: This critical first step involves a detailed analysis of the nanomaterial, including its chemical composition, particle size and distribution, aggregation state, shape, surface area, and surface chemistry [38].
- Toxicological Testing:
- Cytotoxicity: Assessed using multiple test methods, including both phagocytic and non-phagocytic cell lines, to account for varied nanomaterial uptake [38].
- Hemocompatibility: Evaluation includes testing for complement system activation, as nanomaterials can cause significant inflammatory reactions in blood [38].
- Systemic Toxicity: Studies focus on tissues of the mononuclear phagocyte system (MPS), such as the liver and spleen, and other organs like kidneys and brain, where nano-objects may accumulate. Dose is often measured by particle number or surface area in addition to mass [38].
- Genotoxicity: Bacterial reverse mutation tests (Ames test) are not recommended for free nano-objects; mammalian cell systems (e.g., Mouse Lymphoma Assay) are preferred [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
This table lists key reagents, materials, and instruments essential for conducting research in this field, based on the experimental protocols and technologies discussed.
Table 3: Essential Research Tools for Biomaterial Performance Analysis
| Item | Function/Application |
|---|---|
| Simulated Body Fluid (SBF) | An aqueous solution with ion concentrations similar to human blood plasma, used for in vitro degradation and bioactivity studies [73]. |
| Osteoblast Cell Lines (e.g., MC3T3-E1) | Immature bone-forming cells used in cytocompatibility and bioactivity testing to evaluate a material's effect on bone regeneration [73]. |
| Alkaline Phosphatase (ALP) Assay Kit | A biochemical test to measure ALP activity, serving as a key early marker for osteogenic differentiation and bone-forming bioactivity [73]. |
| Scanning Electron Microscope (SEM) | Used for high-resolution imaging of material surface morphology, degradation features, and cell adhesion on the material surface [73]. |
| Transmission Electron Microscope (TEM) | Provides ultra-high-resolution imaging, capable of visualizing nanoscale precipitates, internal nanostructures, and particle distribution within a matrix [73]. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | An analytical technique for precise measurement of metal ion concentrations released from degrading alloys or present in biological samples [36]. |
| Process Analytical Technologies (PAT) | A system of tools and methodologies (e.g., in-line sensors) for real-time monitoring and control of nanomaterial manufacturing processes to ensure consistent quality [74]. |
| Hydrogel Micro/Nano-Robotic Devices | Responsive platforms used for researching targeted drug delivery and minimally invasive surgery, often actuated by magnetic fields, light, or pH changes [4]. |
Visualization of Research Workflows
The following diagrams illustrate the logical relationships and experimental workflows central to the development and evaluation of biomedical materials.
Biomaterial Development and Testing Pathway
Nanomaterial Biocompatibility Evaluation Workflow
The advent of medical devices at the micro and nanoscale represents a paradigm shift in therapeutic intervention, moving beyond simple drug delivery to encompass complex functionalities like targeted navigation and triggered release. Nanoscale devices, typically between 1-100 nm, exploit unique physicochemical properties that emerge at this scale, while microscale devices (generally 1-1000 μm) often serve as versatile platforms for cell transport or macroscopic tissue engineering [74] [75]. The core distinction in their performance lies in their interaction with biological systems: nanoscale devices can interact with biomolecules and cellular machinery on an intimate level, whereas microscale devices often operate at a cellular or multi-cellular level [75]. Evaluating the pharmacokinetics (PK)—the time course of a device's absorption, distribution, metabolism, and excretion—and the pharmacodynamics (PD)—the relationship between device concentration at the site of action and the resulting therapeutic effect—is critical for comparing their targeting efficiency and therapeutic windows [4]. This guide provides a structured comparison of these two classes of devices, focusing on quantitative performance data and the experimental protocols used to generate them, framed within the broader context of advancing medical device research.
Quantitative Performance Comparison
The following tables synthesize key pharmacokinetic and pharmacodynamic parameters, offering a direct, data-driven comparison between nanoscale and microscale medical devices.
Table 1: Comparative Pharmacokinetic Profiles of Nano- vs. Microscale Devices
| Pharmacokinetic Parameter | Nanoscale Devices | Microscale Devices | Evaluation Method |
|---|---|---|---|
| Primary Targeting Mechanism | Enhanced Permeability and Retention (EPR); Active targeting with ligands [21] [75] | Physical guidance (e.g., magnetic navigation); localized actuation [4] | In vivo fluorescence/radiolabel imaging; MRI tracking [4] |
| Tumor Drug Enrichment Efficiency | Up to 50% higher response rate vs. conventional therapy [76] | Improved efficiency with dual-actuation (e.g., magnetic + light) vs. single actuation [4] | Comparative analysis of drug concentration in target tissue vs. plasma [4] |
| Spatio-temporal Distribution | Can be engineered for long circulation (e.g., PEGylation) [21] | Distribution guided by external fields; retention at site of action can be controlled [4] | Pharmacokinetic modeling (AUC, C~max~) in various tissues [4] |
| Clearance Pathway | Reticuloendothelial System (RES)/Liver & Spleen accumulation for many inorganic NPs; renal for small NPs [21] | Often designed for biodegradation at target site; clearance pathways less defined [4] | Histological examination; mass balance studies [21] |
| Blood Circulation Half-life | Variable; can be extended significantly by surface engineering (e.g., >15 hours for some liposomes) [21] | Typically shorter due to larger size and rapid uptake/sequestration; highly design-dependent [4] | Blood sampling over time to measure particle concentration [4] |
Table 2: Comparative Pharmacodynamic Profiles and Clinical Translation
| Pharmacodynamic & Development Parameter | Nanoscale Devices | Microscale Devices | Implication |
|---|---|---|---|
| Therapeutic Window | Significantly widened by reducing systemic toxicity and increasing local drug concentration [75] | Enhanced via localized action and triggered release, minimizing off-target exposure [4] | Enables higher efficacy with fewer side effects |
| Dose-Response Relationship | Established for many approved nanomedicines (e.g., Abraxane) [21] [76] | Under investigation; complex due to combined effects of device and actuation mechanism [4] | Critical for determining safe and effective dosing regimens |
| Systemic Toxicity Profile | Greatly reduced compared to free drugs; side effects linked to carrier material (e.g., complement activation) [21] [75] | Aims to be minimal; potential for immune response to device materials or mechanical action [4] | Directly impacts patient quality of life and treatment safety |
| Clinical Trial Presence | >2,000 nanomedicine-related trials globally; 53% focused on cancer [76] | Predominantly in preclinical and early-stage clinical research [4] | Indicates level of clinical validation and maturity of the technology |
| Key Clinical Challenge | Potential long-term accumulation and toxicity of non-biodegradable materials [21] | Immunogenicity, ensuring precise control and safety of actuation in vivo [4] | Hurdles that must be overcome for regulatory approval and clinical adoption |
Experimental Protocols for Key Evaluations
Protocol for Assessing Targeting Efficiency and Pharmacokinetics
This protocol is fundamental for quantifying how effectively a device reaches its target and its subsequent journey in the body.
- Device Labeling: The micro/nano device is labeled with a traceable tag. Common labels include:
- Fluorescent dyes (e.g., Cy5.5, FITC): For non-invasive in vivo imaging (e.g., fluorescence reflectance imaging) and ex vivo organ analysis.
- Radionuclides (e.g., ⁹⁹ᵐTc, ⁶⁴Cu): For highly sensitive and quantitative tracking using Single-Photon Emission Computed Tomography (SPECT) or Positron Emission Tomography (PET).
- MRI contrast agents (e.g., Gadolinium chelates, superparamagnetic iron oxide): For anatomical co-localization and tracking using Magnetic Resonance Imaging [21] [76].
- Administration and Biodistribution Study: The labeled device is administered to animal models (e.g., mice, rats) via the intended route (e.g., intravenous injection). At predetermined time points, animals are sacrificed, and key organs (tumor, liver, spleen, kidney, heart, lung, brain) are collected.
- Quantification:
- Ex vivo: Organ homogenization and measurement of fluorescence, radioactivity, or metal content (via Inductively Coupled Plasma Mass Spectrometry, ICP-MS) to determine the percentage of injected dose per gram of tissue (%ID/g) [4].
- In vivo: Real-time imaging to visualize device distribution and accumulation over time.
- Pharmacokinetic Modeling: Blood is serially sampled to measure device concentration in plasma. The data is used to calculate critical PK parameters:
- Area Under the Curve (AUC): Total exposure over time.
- Maximum Concentration (C~max~): Peak plasma concentration.
- Elimination Half-life (t~½~): Time for plasma concentration to reduce by half [4].
Protocol for Evaluating Therapeutic Efficacy and Pharmacodynamics
This protocol establishes the biological effect of the device and defines the therapeutic window.
- Disease Model Establishment: A relevant animal model of the disease (e.g., a subcutaneous or orthotopic tumor model for cancer) is generated.
- Treatment Groups: Animals are randomized into several groups:
- Untreated control group.
- Free drug treatment group (standard of care).
- Nano- or micro-device mediated drug delivery group(s), often at multiple doses.
- Placebo device group (device without active drug) to account for effects of the carrier itself.
- Dosing and Monitoring: Treatment is administered according to a set schedule. Tumor volume (for oncology models) or other relevant disease biomarkers are monitored regularly.
- Endpoint Analysis:
- Efficacy Metrics: Tumor growth inhibition, survival rate, or molecular biomarker levels are measured.
- Toxicity Assessment: Body weight change, blood biochemical analysis (e.g., liver enzymes, kidney function), and histological examination of major organs are performed to assess systemic toxicity [4] [76].
- Dose-Response and Therapeutic Index: By testing multiple doses, a dose-response curve is generated. The Therapeutic Index (TI), often calculated as the ratio of the dose causing toxicity (e.g., TD~50~) to the dose eliciting efficacy (e.g., ED~50~), is determined. A higher TI indicates a wider therapeutic window [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a suite of specialized materials and reagents, each serving a distinct function in the construction and evaluation of micro/nano devices.
Table 3: Essential Reagent Solutions for Device Development and Testing
| Reagent/Material | Function | Specific Examples |
|---|---|---|
| Polyethylene Glycol (PEG) | Surface coating to improve biocompatibility, increase blood circulation time ("stealth" effect), and reduce protein adsorption (opsonization) [21]. | PEG-lipids for liposome coating; PEGylation of polymeric nanoparticles. |
| Targeting Ligands | Molecules attached to the device surface for active targeting of specific cell receptors overexpressed in diseased tissues (e.g., cancer cells) [21] [75]. | Antibodies, peptides (e.g., RGD), folic acid, transferrin. |
| Stimuli-Responsive Polymers | Polymer chains that undergo conformational changes (swelling/collapse) in response to specific triggers, enabling controlled drug release [4]. | poly(N-isopropylacrylamide) (pNIPAM) for temperature response; polymers with acidic groups for pH response. |
| Magnetic Nanoparticles | Incorporated into devices to enable guidance, actuation, and heating (hyperthermia) under an external magnetic field; also used as MRI contrast agents [4] [21]. | Superparamagnetic iron oxide nanoparticles (SPIONs). |
| Fluorescent Probes & Dyes | For labeling devices to enable visualization and tracking in vitro and in vivo using fluorescence microscopy and imaging systems [4] [76]. | Cyanine dyes (Cy5, Cy7), FITC, DiR. |
| Biodegradable Polymer Matrices | Form the structural backbone of many devices; designed to safely break down in the body into non-toxic byproducts after fulfilling their function [4] [21]. | PLGA (poly(lactic-co-glycolic acid)), Chitosan, Gelatin. |
Discussion and Future Perspectives
The comparative data underscores a clear divergence in the operational principles and strengths of nano- and microscale devices. Nanoscale devices primarily excel in systemic administration and leveraging biological pathways (like the EPR effect and receptor-mediated endocytosis) for passive and active targeting, resulting in a well-documented widening of the therapeutic window for many chemotherapeutic agents [21] [75] [76]. In contrast, microscale devices offer a more physically guided approach, where their larger size is an advantage for incorporating complex actuation mechanisms (e.g., magnetic propulsion, photothermal conversion), allowing for potentially superior spatial and temporal control over drug release at the target site [4].
A critical challenge for both platforms is immunogenicity. Nanoscale devices can be opsonized and cleared by the mononuclear phagocyte system, while microscale devices may elicit foreign body responses [4] [21]. Surface engineering, particularly with PEG and other "stealth" polymers, remains a key strategy to mitigate these effects. Furthermore, the clinical translation of these technologies demands a rigorous evaluation of their pharmacokinetic and pharmacodynamic profiles in alignment with regulatory science requirements [37] [4] [77]. This includes detailed studies on absorption, distribution, metabolism, excretion (ADME), potential for long-term accumulation, and comprehensive dose-response relationships.
Future progress will likely hinge on hybrid approaches that combine the best features of both scales. We are already seeing the emergence of multi-actuation micro-robotic devices that incorporate nanoscale components [4]. The integration of artificial intelligence for device design and treatment personalization, along with the development of more sophisticated bioinspired and biodegradable materials, will be pivotal in advancing these innovative therapeutic platforms from laboratory research to clinical reality [74] [75].
The fields of nanoscale and microscale medical devices represent two frontiers of technological innovation that are fundamentally reshaping diagnostic and therapeutic approaches. Nanoscale devices are typically characterized by features or components between 1 and 100 nanometers, leveraging unique physicochemical properties that emerge at this scale, such as enhanced surface area-to-volume ratios and quantum effects [41]. Micro-electromechanical systems (MEMS) and microdevices generally operate at feature sizes spanning from 100 nanometers to 100 micrometers, bridging the gap between the macroscopic world and the nanoscale [2]. This analytical comparison examines the market dynamics, technological capabilities, and research applications of both domains, providing researchers and drug development professionals with a structured framework for evaluating these complementary technologies.
The convergence of nanotechnology, materials science, and biomedical engineering has accelerated development in both sectors [4]. Microscale devices have established a strong foundation in medical applications through silicon-based technologies refined over decades, while nanoscale devices are emerging as transformative tools capable of interacting with biological systems at the molecular level [2] [41]. Understanding the distinct characteristics, advantages, and limitations of each domain is essential for guiding research investment and therapeutic development strategies.
The global market for nanotechnology in medical devices was valued at $3.4 billion in 2024 and is projected to reach $4.7 billion by 2030, growing at a compound annual growth rate (CAGR) of 5.4% [78]. The broader biomedical nanoscale devices market is experiencing robust growth, projected to expand at a CAGR of 5% from 2025 to 2033 [16]. While comprehensive current market data specifically for microscale devices is limited in the provided search results, the established MEMS sector continues to see steady adoption in biomedical applications including sensors, actuators, and microfluidic systems [2].
Table 1: Global Market Overview for Nanoscale and Microscale Medical Devices
| Market Parameter | Nanoscale Devices | Microscale Devices (MEMS) |
|---|---|---|
| 2024 Market Value | $3.4 billion [78] | Established market (specific value not provided in search results) |
| Projected 2030 Value | $4.7 billion [78] | N/A |
| CAGR (2024-2030) | 5.4% [78] | N/A |
| Key Applications | Targeted drug delivery, diagnostic imaging, biosensors [78] [16] | Sensors, actuators, microfluidics, lab-on-a-chip [2] |
| Primary Materials | Graphene, carbon nanotubes, gold nanoparticles, liposomes [78] [16] | Silicon, polymers (SU-8, PDMS, polyimide), metals (nickel, gold) [2] |
Table 2: Market Segmentation Analysis for Biomedical Nanoscale Devices
| Segment | Estimated Annual Market Size | Primary Applications |
|---|---|---|
| Medical Imaging | $400 million [16] | Nanoparticle contrast agents, imaging probes for MRI/CT |
| Nanotools | $300 million [16] | Minimally invasive surgical tools, lab-on-a-chip devices |
| Tumor Cell Amplification | $200 million [16] | Cancer cell detection and targeting technologies |
| Scientific Research | $250 million [16] | Basic research, diagnostic technique development |
Growth Drivers and Market Restraints
Propelling Forces
Multiple synergistic factors are driving adoption and innovation across both nanoscale and microscale medical devices:
Technological Advancements: Breakthroughs in nanomaterials such as graphene, carbon nanotubes, and nanostructured metals have enabled stronger, more flexible, and highly conductive medical tools [78]. In microscale devices, innovations in polymer micromachining and advanced materials like silicon carbide have expanded application possibilities [2].
Rising Chronic Disease Prevalence: The increasing global burden of chronic diseases necessitates more precise, effective, and less invasive diagnostic and therapeutic options, driving demand for both nanoscale and microscale solutions [78] [16].
Shift Toward Minimally Invasive Procedures: Healthcare systems worldwide are increasingly prioritizing minimally invasive treatments that reduce patient recovery times and healthcare costs, accelerating demand for miniaturized medical devices [78].
Increased Research Funding: Significant investments from both government and private sectors are fueling nanotechnology research and development, with growing collaborations between academia and industry accelerating commercialization [78] [16].
Integration with Digital Health: The convergence of medical devices with smart technologies such as the Internet of Things (IoT) and artificial intelligence is creating new functionality for both nanosensors and microsensors in wearable health monitoring and point-of-care diagnostics [78].
Challenges and Restraints
Despite promising growth trajectories, both sectors face significant challenges:
Regulatory Hurdles: Stringent regulatory requirements for medical devices, particularly those involving novel nanomaterials or complex microsystems, present substantial barriers to market entry and can significantly extend development timelines [16]. Regulatory bodies like the FDA and EMA require extensive safety and efficacy data [16].
Technical Complexity: The fabrication of both nanoscale and microscale devices requires specialized expertise and sophisticated manufacturing infrastructure [2] [79]. For microscale devices, technical complexity creates training requirements that can hinder deployment [79].
High Development Costs: The significant capital investment required for research, development, and manufacturing of both nanoscale and microscale medical devices can be prohibitive, particularly for smaller companies and research institutions [79] [16].
Biocompatibility and Safety Concerns: Potential toxicity and long-term effects of nanomaterials require rigorous safety testing [16]. For microscale devices, material selection is crucial for ensuring biocompatibility and durability in biological environments [2].
Technology Obsolescence: The rapid pace of technological innovation in both fields means devices can become outdated quickly, pressuring manufacturers to continually innovate and creating investment risks [79].
Regional Market Analysis
The geographic distribution of the nanoscale and microscale medical device markets reveals distinct regional strengths and growth patterns:
North America: Dominates the market due to significant R&D investments, presence of major industry players, and advanced healthcare infrastructure [16]. The United States life sciences microscopy device market alone is anticipated to reach $19.45 billion by 2033, reflecting strong ecosystem support [79].
Europe: Maintains substantial market share with a strong emphasis on regulatory compliance, advanced technological development, and quality standards [16]. Strategic collaborations between device manufacturers and research institutions foster innovation in the region [79].
Asia-Pacific: Emerging as the fastest-growing region, driven by rapid industrialization, expanding production capabilities, government-driven innovation programs, and rising healthcare expenditure [79] [16]. Countries such as China, Japan, India, and South Korea are particularly active in this sector.
Latin America and Middle East & Africa: Witnessing gradual market progression supported by improving economic conditions, rising urbanization, and growing awareness of advanced medical solutions [79]. These regions represent untapped potential for future market expansion.
Comparative Experimental Analysis: Nanoscale vs. Microscale Devices
Experimental Protocols for Device Evaluation
Robust preclinical evaluation is essential for both nanoscale and microscale medical devices. The following experimental approaches provide comprehensive assessment frameworks:
Table 3: Standardized Experimental Protocols for Device Evaluation
| Experimental Method | Protocol Description | Applications | Key Outcome Measures |
|---|---|---|---|
| In Vitro Biocompatibility Testing | Material samples immersed in cell culture media with human cells; incubation for 24-72 hours [80] | Initial safety screening for both nano and micro devices | Cytotoxicity, inflammatory response, cell viability [80] |
| Vascular Replica Modeling | 3D-printed silicone vascular phantoms perfused with blood-mimicking fluid under physiologic pressure [80] | Testing neurovascular, cardiovascular devices; thrombectomy evaluation | Device navigability, deployment accuracy, particulate generation, recanalization efficacy [80] |
| In Silico Simulation | Computer modeling following ASME V&V 40 framework; finite element analysis with mesh generation [80] | Structural analysis of stents, fatigue testing, flow dynamics | Virtual performance under extreme conditions, projected long-term safety factors [80] |
| In Vivo Animal Studies | Implantation in established models (rabbit elastase aneurysm, swine vascular systems) under GLP standards [80] | Definitive safety and performance evaluation before human trials | Feasibility, acute complications, chronic sequelae, endothelial healing [80] |
Research Reagent Solutions Toolkit
Table 4: Essential Research Reagents for Nano/Micro Device Development
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Flexible polymer for microfluidic devices and vascular replicas [2] | Organ-on-a-chip platforms, aneurysm models [80] |
| Polyethylene Glycol (PEG) | Surface functionalization to enhance biocompatibility and reduce immune recognition [41] | Nanoparticle coating for prolonged circulation, hydrogel modification [41] |
| Fibrin-Rich Clot Analogues | Thrombus-mimicking material for mechanical thrombectomy testing [80] | Evaluating stroke treatment devices in vascular replicas [80] |
| Quantum Dots | Nanoscale semiconductors for imaging and sensing [16] | Biosensors, in vivo imaging, diagnostic agents [16] |
| Magnetic Nanoparticles | Responsive components for actuation and targeting [4] | Targeted drug delivery systems, magnetically guided devices [4] |
| Gold Nanoparticles | Versatile nanomaterials for sensing, imaging, and photothermal therapy [78] | Diagnostic assays, contrast agents, therapeutic applications [78] |
Visualization of Experimental Workflow
The following diagram illustrates a comprehensive integrated preclinical testing workflow for nano- and microscale medical devices, combining multiple evaluation methodologies:
Integrated Preclinical Testing Workflow for Medical Devices
Technological Differentiation and Application Analysis
Material Characteristics and Performance
The fundamental differences between nanoscale and microscale devices begin with their material composition and properties:
Nanoscale Materials: Include graphene, carbon nanotubes, gold nanoparticles, and liposomes that exhibit unique quantum effects, high surface area-to-volume ratios, and enhanced reactivity [78]. These materials enable novel functionality in drug delivery, imaging, and sensing applications that are not possible at larger scales [41].
Microscale Materials: Primarily include silicon, various polymers (SU-8, PDMS, polyimide), and metals (nickel, gold, aluminum) [2]. These materials benefit from well-established fabrication processes and provide robust structural properties for sensors, actuators, and microfluidic systems [2].
Application-Specific Performance
The functional capabilities of nanoscale versus microscale devices diverge significantly across medical applications:
Table 5: Application-Based Performance Comparison
| Medical Application | Nanoscale Device Performance | Microscale Device Performance |
|---|---|---|
| Targeted Drug Delivery | Superior cellular-level targeting via functionalized nanoparticles; demonstrated 2-5x increase in tumor drug concentration [4] [78] | Limited to vascular-level targeting via microfluidic control; suitable for organ-specific delivery |
| Medical Imaging | Enhanced contrast and resolution using quantum dots and nanoparticles; enables molecular-level imaging [16] | Structural and functional imaging with micro-sensors; suitable for tissue-level resolution |
| Biosensing | High sensitivity for biomarker detection; single-molecule detection capability [2] [78] | Multi-parameter sensing platforms; integrated sample processing in lab-on-chip format [2] |
| Minimally Invasive Surgery | Limited current application; potential for nanorobotic systems in development [4] | Established capability with microsurgical tools; sub-millimeter operational precision [4] |
| Tissue Engineering | Nanofibrous scaffolds for enhanced cell adhesion and differentiation [41] | Microstructured scaffolds with vascular networks; 3D tissue constructs [2] |
Emerging Trends and Future Research Directions
The convergence of nanoscale and microscale technologies is creating new opportunities for medical innovation. Key emerging trends include:
Multi-Actuation Synergistic Strategies: Research is shifting toward hybrid actuation systems that combine magnetic navigation with localized photothermal or biochemical responses, enabling more precise control of therapeutic interventions [4]. For example, dual-actuation micro/nano-robotic devices utilizing both magnetic and light fields demonstrate improved tumor drug enrichment efficiency compared to single-mechanism approaches [4].
Advanced Biocompatible Materials: Development of biodegradable and biocompatible nanomaterials is accelerating, with focused attention on minimizing potential toxicity and improving patient safety [16]. Similarly, advances in polymer composites and surface modification techniques are enhancing the biocompatibility of microscale devices [2].
Integration with Artificial Intelligence: AI and machine learning are being incorporated into both nanoscale and microscale device development, enabling more sophisticated data analysis, adaptive functionality, and predictive capabilities [81] [16].
Point-of-Care Diagnostics: The market is seeing increased focus on decentralized testing through both nano-enabled biosensors and microfluidic lab-on-chip devices that allow for rapid, cost-effective diagnostic testing outside traditional laboratory settings [16].
Organ-on-a-Chip Platforms: Microfluidic devices lined with living human cells that simulate organ-level physiology are emerging as valuable tools for drug testing and disease modeling, reducing reliance on animal studies [80]. These systems increasingly incorporate nanoscale sensors for real-time monitoring of cellular responses.
The comparative analysis of nanoscale and microscale medical devices reveals distinct yet complementary growth trajectories, drivers, and application profiles. The nanoscale device market demonstrates robust expansion driven by material innovations and targeted therapeutic applications, while microscale devices maintain steady advancement through refined fabrication processes and system integration. For researchers and drug development professionals, the choice between nanoscale and microscale approaches depends fundamentally on the specific biological targets, required precision, and therapeutic objectives.
Regional analysis indicates continued North American leadership in both sectors, with particularly rapid growth occurring in the Asia-Pacific region. Addressing regulatory challenges and biocompatibility concerns remains critical for both fields, though standardized preclinical testing methodologies are emerging to facilitate technology validation. The increasing convergence of nanoscale and microscale technologies, particularly through multi-actuation systems and integrated sensing platforms, represents the most promising direction for future medical device innovation, potentially enabling unprecedented capabilities in personalized medicine and minimally invasive healthcare interventions.
The evolution of medical technology has been profoundly shaped by the parallel development of microscale and nanoscale devices. While micro-electromechanical systems (MEMS) have established remarkable capabilities in interfacing with tissues and organs, emerging nanoscale devices operate at the molecular level, offering unprecedented access to biological processes. This comparison guide objectively analyzes the comparative advantages of both scales across three critical performance parameters: precision, sensitivity, and minimally invasive capabilities. Understanding these distinctions is crucial for researchers, scientists, and drug development professionals selecting appropriate technological platforms for specific biomedical applications, from targeted drug delivery to real-time physiological monitoring. The convergence of these scales through hybrid approaches is further accelerating innovation in personalized medicine and diagnostic methodologies [1] [82].
Comparative Performance Analysis
The fundamental differences in scale between micro and nano devices directly translate to distinct performance characteristics. The table below provides a quantitative comparison of key parameters based on current experimental data and technological capabilities.
Table 1: Performance Comparison of Microscale vs. Nanoscale Medical Devices
| Performance Parameter | Microscale Devices | Nanoscale Devices |
|---|---|---|
| Spatial Precision | 1 mm to 100 nm [2] | 100 nm to 1 nm [2] |
| Sensitivity (Detection Limit) | Nanomolar (10⁻⁹ M) range for biosensors [1] | Molecular level (single biomarker detection) [42] [82] |
| Minimally Invasive Access | Minimally invasive surgery (e.g., endoscopes, catheters) [83] [1] | Cellular and sub-cellular level access [4] [82] |
| Representative Drug Delivery Payload | Microneedle arrays (≥100 µm channel diameter) [83] | Nanocarriers (e.g., liposomes, dendrimers, polymeric NPs) [82] |
| Key Actuation/Sensing Mechanisms | Piezoresistive, capacitive, optical sensing [1] | Chemical, magnetic, acoustic, pH-responsive, enzymatic [4] [82] |
| Targeting Accuracy | Tissue and organ level [84] | Cellular and sub-cellular level [4] [82] |
Analysis of Comparative Advantages
Nanoscale Precision and Targeting: The defining advantage of nanoscale devices is their ability to operate at the molecular and cellular level. Their size, typically ranging from 1 to 100 nanometers, allows them to interact directly with biomarkers, cell membranes, and intracellular components. This enables applications impossible for larger devices, such as subcellular drug delivery and manipulation of individual proteins or DNA strands. For instance, hydrogel-based micro/nano-robotic medical devices can be designed to undergo structural transitions in response to specific stimuli (e.g., pH, enzymes) found in target micro-environments like tumors, providing exceptional spatial and temporal control [4] [82].
Microscale Precision and Physical Manipulation: Microscale devices (1 mm to 100 nm) excel in applications requiring physical manipulation at the tissue or organ level. Their precision is evidenced in devices like the MISSO Robotic System for joint replacement and robotic systems for endosurgery with a single entry point. The fabrication of intricate geometries via micro-additive manufacturing (Micro-AM), such as microneedles with internal channels as small as 100 µm, allows for precise fluid delivery and sampling at the tissue interface. This scale is ideal for tools used in minimally invasive surgery, including micro-graspers and forceps, which provide surgeons with enhanced control while minimizing trauma [83] [84] [1].
Comparative Sensitivity Analysis
Sensitivity, particularly in diagnostic and sensing applications, is another area where scale imparts distinct advantages. The following table compares sensitivity-related characteristics.
Table 2: Sensitivity and Diagnostic Capabilities Comparison
| Characteristic | Microscale Devices | Nanoscale Devices |
|---|---|---|
| Primary Sensing Modalities | Piezoresistive strain gauges, capacitive plates, optical interferometry [1] | Localized Surface Plasmon Resonance (LSPR), electrofluorigenic sensing, quantum dot fluorescence [82] [13] |
| Key Application Areas | Continuous physiological monitoring (e.g., pressure, acceleration, temperature) [1] | Detection of low-abundance disease biomarkers, viral particles, early-stage cancer cells [42] [82] [13] |
| Signal Amplification Method | Electronic signal conditioning (e.g., Wheatstone bridges, charge amplifiers) [1] | Plasmonic enhancement, catalytic amplification (e.g., nanozymes) [13] |
| Example Detection Limit | Not explicitly quantified in results, but suitable for physiological levels of analytes. | Ultrasensitive detection via electrofluorigenic readout (resazurin to resorufin) [13] |
| Multiplexing Capability | Moderate, through sensor arrays [1] | High, via multi-color quantum dots or LSPR encoding [42] [82] |
Analysis of Sensitivity Advantages
Nanoscale-Enhanced Signal Detection: Nanoscale devices leverage quantum and plasmonic effects to achieve extraordinary sensitivity. Localized Surface Plasmon Resonance (LSPR) sensors utilizing gold or silver nanoparticles can detect shifts in resonant wavelength caused by the adsorption of minute amounts of target molecules, such as disease-specific biomarkers. Furthermore, electrofluorigenic sensing platforms can transform an electrochemical event into a strong fluorescent signal, enabling ultrasensitive detection. These approaches can identify biomarkers at concentrations far below the detection limits of conventional assays, facilitating early disease diagnosis [82] [13].
Robust Sensing at the Microscale: The sensitivity of MEMS-based microscale sensors stems from their ability to transduce physiological signals (pressure, acceleration, chemical concentration) into quantifiable electrical signals with high reliability. For example, capacitive MEMS sensors are highly sensitive to minute changes in distance between electrodes, making them excellent for precision inertial and pressure sensing in implantable and wearable devices. Their integration with on-chip electronics allows for robust, real-time monitoring of physiological parameters, which is crucial for managing chronic conditions in connected health ecosystems like the Internet of Bodies (IoB) [1].
Minimally Invasive Capabilities
The drive toward less invasive procedures is a major trend in medicine, and both micro and nanotechnologies are pivotal in this transition, albeit in different ways.
Levels of Invasiveness and Applications
Microscale Minimally Invasive Technologies: These devices have revolutionized surgery and monitoring by reducing the physical footprint of interventions. Technologies like Transcatheter Aortic Valve Replacement (TAVR) and single-access surgical robotic systems allow for complex procedures to be performed through small incisions or natural orifices, minimizing scarring, pain, and recovery time. BioMEMS devices, fabricated from biocompatible polymers like PDMS and polyimide, can be designed as implantable sensors for continuous monitoring of glucose, cardiac pressure, or neural activity, providing long-term data with minimal tissue disturbance [84] [1].
The Cellular-Level Invasiveness of Nanodevices: Nanoscale devices operate at a fundamentally different level of "invasiveness." They are designed to cross biological barriers—such as the blood-brain barrier or cellular membranes—that are impenetrable to larger devices. For example, nanorobotic medical devices composed of hydrogels can be actuated by external magnetic fields to navigate the vascular system and penetrate deep tissues for targeted drug delivery. Their small size also allows for eventual clearance from the body, with some bioresorbable nanomaterials degrading after fulfilling their function, leaving no permanent implant [4] [82]. This is exemplified by bioresorbable stents with struts as thin as 100 µm, which provide temporary support to arteries and then dissolve [84].
Experimental Protocols for Performance Validation
To objectively compare the capabilities of micro and nanoscale devices, standardized experimental protocols are essential. Below are detailed methodologies for key performance tests.
Protocol for Quantifying Targeting Precision
Objective: To quantify the spatial targeting accuracy of a magnetically guided nano-device versus a microscale device in a simulated vascular network. Materials:
- Microfluidic channel mimicking branched vasculature (20 µm to 200 µm diameter).
- Magnetic nanoparticle-based nano-device (100 nm diameter, e.g., SPION-embedded hydrogel [4]).
- Magnetic micro-device (20 µm diameter, e.g., polymer microbead with ferromagnetic coating).
- External electromagnetic actuation system with real-time microscopy.
- Fluorescent dye for visualization.
Methodology:
- Setup: Prime the microfluidic channel with a buffer solution simulating blood viscosity.
- Navigation: Introduce both device types simultaneously into the channel inlet. Use the magnetic system to navigate them towards a specific, narrow branch (50 µm diameter) at a flow rate of 1 µL/min.
- Actuation Parameters: For the nano-device, use a low-gradient magnetic field (5 mT/m). For the micro-device, a higher gradient (50 mT/m) may be required.
- Measurement: Track the trajectory and final position of each device using time-lapsed fluorescence microscopy. Precision is measured as the deviation (in µm) from the center of the target branch.
- Analysis: The nano-device is expected to demonstrate superior navigation through narrower branches and more precise positioning due to its smaller size and higher responsiveness to subtle field changes in complex flow environments [4].
Protocol for Assessing Diagnostic Sensitivity
Objective: To compare the limit of detection (LOD) of a nanoscale LSPR sensor and a microscale piezoresistive sensor for a model protein biomarker. Materials:
- Gold nanorod LSPR sensor (aspect ratio 3.5, peak resonance ~750 nm) [13].
- MEMS piezoresistive cantilever sensor functionalized with the same antibody.
- Model protein biomarker (e.g., Prostate-Specific Antigen, PSA) in a concentration series from 1 pM to 1 nM.
- Phosphate Buffered Saline (PBS) for dilution.
- UV-Vis spectrometer and electronic readout system.
Methodology:
- Functionalization: Both sensors are functionalized with an identical surface density of anti-PSA antibodies.
- Baseline Measurement: Record the baseline LSPR wavelength for the nanorods and the resonant frequency/resistance for the cantilever in pure PBS.
- Sample Exposure: Expose each sensor to 100 µL of each PSA concentration for 30 minutes.
- Signal Measurement: For the LSPR sensor, measure the redshift in the extinction peak. For the cantilever, measure the change in resonance frequency or resistance due to surface stress.
- LOD Calculation: The LOD is defined as the concentration corresponding to the mean baseline signal plus three times the standard deviation of the noise. The LSPR sensor is anticipated to show a significantly lower LOD, potentially in the femtomolar range, due to the high field confinement and environmental sensitivity of the plasmonic effect [82] [13].
Research Reagent Solutions and Materials
The fabrication and function of micro and nanoscale devices rely on a distinct set of materials and reagents. The table below details key components and their functions.
Table 3: Essential Research Reagents and Materials for Device Fabrication and Application
| Item Name | Function in Research | Relevant Device Scale |
|---|---|---|
| Polydimethylsiloxane (PDMS) | An elastomeric polymer used for flexible substrates, microfluidic channels, and wearable sensors due to its biocompatibility and optical transparency. [2] [1] | Microscale |
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer used to fabricate nanoparticles for controlled drug delivery and as a matrix for thermostic agents. [82] | Nanoscale |
| Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | Magnetic nanoparticles embedded in hydrogels or polymers to enable remote actuation and guidance using external magnetic fields, and as MRI contrast agents. [4] [82] | Nanoscale |
| Gold Nanoparticles (AuNPs) | Used for their tunable Localized Surface Plasmon Resonance (LSPR) in biosensing, as photothermal agents for therapy, and as contrast agents. [82] [13] | Nanoscale |
| Lead Zirconate Titanate (PZT) | A piezoelectric ceramic material used in MEMS actuators, energy harvesters, and ultrasonic transducers for generating and sensing mechanical motion. [2] | Microscale |
| Methyl Viologen | An electrochromic reagent used in closed bipolar electrode (CBE) systems; changes color upon reduction, providing a visual readout for electrochemical events. [13] | Nanoscale |
| Single-Crystal Silicon (SCS) | The foundational material for many MEMS devices, used for high-precision structural components due to its excellent mechanical properties. [2] | Microscale |
Visualizing Experimental Workflows
The following diagrams illustrate core experimental workflows and logical relationships discussed in this guide.
Workflow for Multi-Modal Nanorobot Actuation
Diagram 1: Multi-Modal Actuation of Nanorobots. This workflow shows the sequential use of a magnetic field for deep tissue navigation followed by optical stimulation for precise local action, such as drug release [4].
Sensing Mechanism Decision Pathway
Diagram 2: Device Selection Logic. This decision pathway helps researchers select the appropriate device scale based on the fundamental requirements of their application [2] [4] [82].
The development of medical devices at the micro- and nanoscale represents a pivotal frontier in advancing personalized medicine. Micro-electromechanical systems (MEMS) characteristic sizes spanning from 1 mm to 100 nm, while nano-electromechanical systems (NEMS) operate at 1-100 nm [2]. This divergence in scale dictates fundamental differences in their applications, capabilities, and integration with artificial intelligence (AI) and theranostic platforms. Nanoscale devices leverage unique physicochemical properties that emerge at the molecular level, enabling unprecedented interactions with biological systems [41]. Meanwhile, microscale devices provide the platform for integrating multiple functionalities at a scale compatible with minimally invasive implantation and surgical manipulation [2].
The convergence of AI with these device technologies accelerates their development and application. AI-powered drug development is already revolutionizing how we find and create new medicines, cutting development timelines from decades to years while dramatically reducing costs [85]. Similarly, machine learning algorithms are optimizing the design of nanoscale materials and predicting their behavior in biological systems [51]. This review provides a comparative analysis of nanoscale versus microscale medical devices within the framework of AI integration, theranostic applications, and their collective path toward personalized medicine, supported by experimental data and methodological protocols.
Comparative Analysis: Nanoscale vs. Microscale Medical Devices
Table 1: Fundamental Characteristics of Nanoscale vs. Microscale Medical Devices
| Characteristic | Nanoscale Devices | Microscale Devices |
|---|---|---|
| Size Range | 1-100 nm [2] [41] | 100 nm - 1 mm [2] |
| Key Materials | Liposomes, polymeric nanoparticles, gold nanoparticles, quantum dots, graphene [51] [41] | Silicon, polymers (PDMS, polyimide), metals (nickel, gold), piezoelectric materials (PZT, AlN) [2] |
| Primary Applications | Targeted drug delivery, biosensing, medical imaging contrast agents [4] [41] | Implantable sensors, microfluidics, surgical assistants, energy harvesters [2] |
| Manufacturing Techniques | Bottom-up (self-assembly, chemical vapor deposition) and top-down approaches (lithography) [41] | Surface/bulk micromachining, additive manufacturing, electrodeposition [2] |
| AI Integration Level | High (single-cell profiling, material optimization) [51] | Moderate (device optimization, performance prediction) [2] |
| Theranostic Capability | High (integrated diagnosis and therapy) [41] | Moderate (primarily diagnostic with some therapeutic functions) [2] |
| Regulatory Challenges | Significant (nanotoxicity, long-term effects) [37] [41] | Established frameworks (biocompatibility, mechanical failure) [2] [80] |
AI-Driven Design and Optimization
Computational Design of Nanomaterials
Artificial intelligence has revolutionized the design pipeline for nanoscale medical devices. Machine learning (ML)-driven Bayesian optimization has been successfully applied to enhance the mechanical properties of 3D-printed carbon nanolattices, leading to a 118% increase in tensile strength and a 68% increase in Young's modulus compared to non-optimized structures [51]. The integration of AI in nanomaterial design follows a systematic workflow:
Table 2: AI-Driven Nanomaterial Optimization Protocol
| Step | Method | Application Example |
|---|---|---|
| Data Generation | Finite Element Analysis (FEA) | Structural analysis of nanolattice architectures [51] |
| Model Training | Deep learning on 3D imaging data | Training on high-quality 3D data for cell segmentation [51] |
| Optimization | Bayesian optimization framework | Predicting optimal strut diameters (300-600 nm) for carbon nanolattices [51] |
| Fabrication | Two-photon polymerization (2PP) | Manufacturing nanolattices with specific strength of 2.03 m³ kg⁻¹ at densities of 200 kg m⁻³ [51] |
| Validation | Experimental mechanical testing | Verification of predicted specific strength and Young's modulus [51] |
AI-Enhanced Experimental Planning
Beyond material design, AI tools are now assisting researchers in experimental planning. CRISPR-GPT, developed at Stanford Medicine, demonstrates how large language models can accelerate biomedical research by generating experimental designs, analyzing data, and troubleshooting flaws in gene-editing experiments [86]. The system was trained on 11 years of expert discussions and scientific publications, creating an AI model that "thinks" like a scientist and can guide even novice researchers to successful experimental outcomes on their first attempt [86].
AI-Driven Nanomaterial Design Workflow: This diagram illustrates the iterative process of using artificial intelligence and machine learning to optimize nanomaterial properties, incorporating both computational prediction and experimental validation [51].
Advanced Theranostic Platforms
Hydrogel-Based Micro/Nano-Robotic Devices
Stimuli-responsive hydrogels represent a convergence point for nanoscale and microscale theranostic platforms. These three-dimensional crosslinked networks integrated with responsive chemical functional groups undergo structural and functional transitions under various external stimuli, including chemical energy, temperature, light, pH, ultrasound, magnetic fields, and ions [4]. The multi-drive synergistic strategies employed by these devices enable complex operations at micro- to nanoscales, such as targeted drug delivery, biosensing, minimally invasive surgical assistance, and in vivo imaging [4].
Table 3: Multi-Modal Actuation Mechanisms in Hydrogel Micro/Nano-Robotic Devices
| Actuation Mechanism | Stimulus-Responsive Component | Biomedical Application | Performance Metrics |
|---|---|---|---|
| Magnetic Actuation | Embedded magnetic nanoparticles (e.g., iron oxide) | Physical orientation and navigation across biological barriers [4] | Improved tumor drug enrichment efficiency [4] |
| Photo-Actuation | Gold nanoparticles, carbon nanotubes, azobenzene groups | Triggered drug release through photothermal effects [4] | Cellular-level targeting precision [4] |
| pH-Responsive | Acidic/basic functional groups (protonation/deprotonation) | Drug release in tumor microacidic environment [4] | Polymer chain shrinkage in acidic environments [4] |
| Temperature-Responsive | Poly(N-isopropylacrylamide) - PNIPAM | On-demand deformation through hydrophobic-hydrophilic phase transitions [4] | Controlled drug release kinetics [4] |
Single-Cell Profiling and Targeted Delivery
A significant breakthrough in nanoscale theranostics comes from the development of Single-Cell Profiling (SCP) of nanocarriers, an AI-powered monitoring technology that precisely tracks nanocarrier distribution at the cellular level [51]. This method combines deep learning approaches with high-resolution imaging to quantify nanocarrier biodistribution with exceptional precision and sensitivity.
Experimental Protocol: Single-Cell Profiling of Nanocarriers
- Nanocarrier Administration: Intravenous injection of LNP-based mRNA nanocarriers at ultra-low dosage (0.0005 mg/kg) in mouse models [51]
- Tissue Sampling and Preparation: Collection of target tissues at predetermined time points with fixation and sectioning for imaging [51]
- High-Resolution Imaging: Acquisition of large-scale 3D image datasets using confocal or super-resolution microscopy [51]
- Deep Learning Analysis: Segmentation of cells based on parameters (shape, size) using DL algorithm trained on high-quality 3D data [51]
- Quantification and Mapping: High-resolution mapping of nanocarrier distribution at single-cell level with precise quantification [51]
This approach has demonstrated the ability to quantify mRNA distribution at concentrations 100 to 1,000 times lower than conventional studies, representing a significant advancement in monitoring precision nanomedicine [51].
Experimental Models and Validation Methods
Preclinical Testing Frameworks
The path to clinical translation for micro- and nanoscale devices requires rigorous preclinical validation. A combination of in vitro, in silico, and in vivo models provides complementary insights into device safety and performance [80].
Table 4: Preclinical Testing Modalities for Micro/Nano Medical Devices
| Testing Modality | Methodology | Applications | Limitations |
|---|---|---|---|
| In Vitro Models | Organ-on-a-chip microfluidic devices lined with living human cells [80] | Biocompatibility testing, basic functionality assessment [80] | Lack of full-body complexity, immune system interactions [80] |
| Vascular Replica Models | 3D-printed patient-specific silicone phantoms with blood-mimicking fluid [80] | Device navigation, deployment accuracy, particulate generation assessment [80] | Synthetic materials lack true tissue elasticity and biological responses [80] |
| In Silico Simulation | Finite element analysis following ASME V&V 40 framework [80] | Structural mechanics simulation, fatigue analysis (10-year equivalent cycles) [80] | Cannot capture complex biological responses (clot formation, remodeling) [80] |
| In Vivo Models | Rabbit elastase aneurysm model, swine rete mirabile for liquid embolics [80] | Long-term aneurysm occlusion, endothelial healing, safety evaluation [80] | Anatomical differences from humans, ethical and cost constraints [80] |
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagent Solutions for Micro/Nano Device Development
| Reagent/Material | Function | Application Example |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Flexible substrate for microfluidic devices and replicas [2] [80] | Fabrication of vascular phantom models for device testing [2] [80] |
| Poly(N-isopropylacrylamide) - PNIPAM | Temperature-responsive polymer for controlled drug release [4] | Hydrogel-based micro/nano-robotic devices for targeted therapy [4] |
| Prussian Blue Analog (PBA) | Redox-active core material for electrochemical signal transduction [51] | Printable nanoparticle cores for wearable/implantable biosensors [51] |
| Molecularly Imprinted Polymer (MIP) | Shell material for precise molecular recognition [51] | Target-specific binding in biosensors for biomarker monitoring [51] |
| Polyethylene Glycol (PEG) | Surface functionalization to enhance biocompatibility and targeting [41] | PEGylation of nanomaterials to evade immune detection and extend circulation [41] |
| Lead Zirconate Titanate (PZT) | Piezoelectric material for energy harvesting and sensing [2] | MEMS sensors, actuators, and ultrasonic transducers [2] |
Stimuli-Responsive Material Design Logic: This diagram illustrates the logical relationship between external stimuli, material responses, and resulting theranostic applications in smart hydrogel systems [4].
Regulatory Science and Clinical Translation
The translation of micro- and nanoscale medical devices from research to clinical application faces distinct regulatory challenges. For nanoscale devices, concerns regarding potential toxicity and long-term effects of nanomaterials necessitate rigorous safety testing and regulatory compliance [37] [41]. The pharmacokinetic (PK) and pharmacodynamic (PD) properties of these devices must be thoroughly characterized, including spatio-temporal distribution, retention, degradation, and clearance patterns in complex biological environments [4].
The US FDA and European EMA have developed evolving regulatory frameworks for novel medical devices and nanomedicines [37] [4]. Regulatory science for these technologies must address:
- Safety and Efficiency Evaluation: Comprehensive assessment of biocompatibility and nanotoxicology, including potential for oxidative stress, inflammation, and cytotoxic reactions [37] [41]
- In Vitro Alternatives: Development of New Approach Methodologies (NAMs) to reduce traditional animal testing, such as organ-on-a-chip devices [80]
- Manufacturing Quality Control: Implementation of Quality-by-Design (QbD) principles and Process Analytical Technologies (PAT) to ensure consistent quality and performance of nanomedicines [41]
- Clinical Trial Design: Adaptation of trial methodologies to account for the unique behavior of micro/nano devices in human subjects [4]
The global biomedical nanoscale devices market reflects this evolving regulatory landscape, with projections indicating robust growth reaching an estimated several hundred million dollars by 2025, expanding at a Compound Annual Growth Rate of approximately 5% through 2033 [16].
The convergence of AI, theranostics, and micro/nanoscale device technologies represents a paradigm shift in personalized medicine. Nanoscale devices offer unique capabilities for targeted interactions at the molecular level, while microscale devices provide platforms for integrating multiple functions in clinically deployable formats. The integration of AI across the development pipeline—from design and optimization to experimental planning and data analysis—is dramatically accelerating the translation of these technologies from laboratory concepts to clinical applications.
The future outlook suggests several key trajectories:
- Increased AI Integration: Deep learning will further refine nanocarrier design, device optimization, and experimental planning [51] [86]
- Multi-Modal Functionality: Next-generation devices will combine diagnostic and therapeutic functions with adaptive control mechanisms [4] [41]
- Personalized Formulations: Patient-specific factors will increasingly guide device design and material selection [16] [41]
- Regulatory Evolution: Frameworks will adapt to address the unique challenges and opportunities presented by these convergent technologies [37] [80]
As these trends continue, the distinction between diagnostic and therapeutic medical devices will blur, creating a new generation of intelligent, adaptive systems that can provide personalized medical interventions based on real-time physiological feedback. The successful realization of this future will require ongoing collaboration between materials scientists, engineers, clinicians, computational biologists, and regulatory specialists to ensure that these transformative technologies reach patients safely and effectively.
Conclusion
The comparison between nanoscale and microscale medical devices reveals a complementary yet distinct landscape. While microscale devices (MEMS) excel in miniaturized mechanical functions and integration, nanoscale devices (NEMS) offer unparalleled advantages in bio-interactivity, sensitivity, and precision due to their fundamental physicochemical properties. The future of biomedical devices lies in the synergistic integration of these scales, leveraging micro-architectures for structure and nano-components for targeted function. Key future directions include overcoming translational challenges through advanced material design and standardized regulatory pathways, the deepening convergence with artificial intelligence for intelligent device operation, and the continued push towards multifunctional theranostic platforms. This progression is poised to fundamentally shift treatment paradigms from generalized care to highly personalized, predictive, and preventive medicine, ultimately improving patient outcomes and reshaping the healthcare industry.
References
- 1. Next-Gen Healthcare Devices: Evolution of MEMS and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565985/]
- 2. Prospects and Trends in Biomedical Microelectromechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191261/]
- 3. Graphene MEMS and NEMS [https://www.nature.com/articles/s41378-024-00791-5]
- 4. Micro/nano-robotic medical device: preparation, actuation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509628/]
- 5. Nanobots in the Healthcare - Applications, Benefit, and Key ... [https://www.delveinsight.com/blog/nanobots-in-the-healthcare-sector]
- 6. Next‐Generation Piezoelectric Materials in Wearable and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591194/]
- 7. Piezoelectric Devices Market Size, Share, Industry Report ... [https://www.marketsandmarkets.com/Market-Reports/piezoelectric-devices-market-256019882.html]
- 8. Prospects and Trends in Biomedical ... [https://www.mdpi.com/2218-273X/15/6/898]
- 9. Exploring the World of Nano Medical Devices [https://www.mddionline.com/rd/exploring-the-world-of-nano-medical-devices]
- 10. Surface and Quantum Effects in Nanosized Semiconductor [https://www.sciencepublishinggroup.com/article/10.11648/j.nano.20200803.11]
- 11. Properties and Behavior of Nanoscale Materials [https://www.worldbrainmapping.org/courses/lessons/properties-and-behavior-of-nanoscale-materials/]
- 12. Quantum Dots in Biomedical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6642839/]
- 13. Microscale and Nanoscale Electrophotonic Diagnostic Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC6417966/]
- 14. Nanotechnology in medicine: a double-edged sword for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00008-2]
- 15. Nanostructured Medical Devices: Regulatory Perspective and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11051465/]
- 16. Biomedical Nanoscale Devices Charting Growth Trajectories [https://www.archivemarketresearch.com/reports/biomedical-nanoscale-devices-299713]
- 17. Microfluidics in 2025: Applications, Trends & How It Work [https://eden-microfluidics.com/news-events/microfluidics-overview/]
- 18. Emerging Trends in Microfluidics [https://elveflow.com/microfluidic-reviews/emerging-trends-in-microfluidics/]
- 19. Nanocarrier‐Based Systems for Targeted Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371215/]
- 20. Smart resonant micro-sensor and micro-actuator: high ... [https://www.nature.com/articles/s41378-025-01041-y]
- 21. Review Advantages and limitations of nanostructures for ... [https://advances.umw.edu.pl/en/article/2025/34/3/447/]
- 22. Moving toward Self-Sustained Edge AI Microsystems [https://pubmed.ncbi.nlm.nih.gov/40990448/]
- 23. Recent Advances in Additive Manufacturing: A Review of ... [https://www.mdpi.com/2075-1702/13/9/813]
- 24. Additive Manufacturing Innovation: The Future of 3D Printing [https://www.rapid3devent.com/event/news/additive-manufacturing-innovation/]
- 25. The Microfluidic device industry: Growth outlook 2025 – 2050 [https://www.medicalmicromolding.com/the-microfluidic-device-industry-growth-outlook-2025-2050/]
- 26. Additive Manufacturing in Medtech: The Key Themes of 2025 [https://www.materialise.com/en/inspiration/articles/additive-manufacturing-medtech-themes-2025]
- 27. Exciting New Trends Are Advancing Additive Manufacturing [https://bonezonepub.com/2025/09/14/exciting-new-trends-are-advancing-additive-manufacturing/]
- 28. Laser Welders Deliver Accuracy and Reliability for Medical ... [http://www.hanslaserus.com/knowledge/laser-welders-deliver-accuracy-and-reliability-for-medical-devices/]
- 29. Microfluidic Devices Market Global Forecast 2025-2032 [https://www.businesswire.com/news/home/20250313095991/en/Microfluidic-Technologies-Revolutionizing-Life-Sciences-IVD-Medical-Devices---Microfluidic-Devices-Market-Global-Forecast-2025-2032---ResearchAndMarkets.com]
- 30. Synthesis of nanomaterials using various top - down and bottom - up ... [https://pubmed.ncbi.nlm.nih.gov/34979471/]
- 31. Understanding Bottom-Up and Top-Down Synthesis Methods [https://www.ai-futureschool.com/en/chemistry/bottom-up-and-top-down-synthesis-explained.php]
- 32. Cutting-Edge Nanoparticle Innovations in Biomedical ... [https://www.scientificarchives.com/article/cutting-edge-nanoparticle-innovations-in-biomedical-science-synthesis-applications-challenges-and-future-prospects]
- 33. Sustainable Approaches Towards Nanomaterial Synthesis [https://scifiniti.com/3079-1421/1/2025.0011]
- 34. - Top and down - bottom approach in synthesis of... up [https://www.slideshare.net/slideshow/topdown-and-bottomup-approach-in-synthesis-of-nanoparticlespptx/262873004]
- 35. Global Nanotechnology in Medical Devices Market Size, ... [https://www.maximizemarketresearch.com/market-report/global-nanotechnology-in-medical-devices-market/13145/]
- 36. Top 6 Nanotechnology in Medical Devices Companies 2025 [https://www.expertmarketresearch.com/healthcare-articles/top-nanotechnology-in-medical-devices-companies]
- 37. Advances in medical devices using nanomaterials and ... [https://www.sciencedirect.com/science/article/pii/S2452199X25000659]
- 38. Nanomaterials in Medical Devices [https://namsa.com/resources/blog/nanomaterials-medical-devices-biocompatibility-considerations/]
- 39. Therapeutic applications of nanobots and nanocarriers in cancer... [https://link.springer.com/article/10.1007/s44211-025-00799-5]
- 40. Microfluidic-based nanocarriers for overcoming biological barriers in... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr02322j]
- 41. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 42. Biomedical Nanoscale Devices Strategic Insights: Analysis ... [https://www.archivemarketresearch.com/reports/biomedical-nanoscale-devices-288282]
- 43. Photonic and electrochemical biosensors for near-patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11601118/]
- 44. Emerging nanoparticle-based x-ray imaging contrast ... [https://pubmed.ncbi.nlm.nih.gov/40261216/]
- 45. Biomimetic and bioactive nanofibrous scaffolds from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2676814/]
- 46. Biomimetic nanofibrous scaffolds for bone tissue engineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC3195926/]
- 47. Nanofibrous Scaffolds in Biomedicine [https://www.mdpi.com/2504-477X/8/7/269]
- 48. Electrospun nano-fibrous bilayer scaffold prepared from ... [https://link.springer.com/article/10.1007/s10856-021-06588-6]
- 49. Construction of nanofibrous scaffolds with interconnected ... [https://www.sciencedirect.com/science/article/pii/S2452199X21000931]
- 50. Nanomaterial toxicity: a comprehensive review of ... [https://link.springer.com/article/10.1007/s44475-025-00003-2]
- 51. Top 5 Emerging Trends in Nanotechnology for 2025 [https://www.azonano.com/article.aspx?ArticleID=6865]
- 52. Evaluating AI-enabled Medical Device Performance in ... [https://www.fda.gov/medical-devices/digital-health-center-excellence/request-public-comment-measuring-and-evaluating-artificial-intelligence-enabled-medical-device]
- 53. How to Measure Performance for AI-Enabled Medical ... [https://www.knobbe.com/blog/how-to-measure-performance-for-ai-enabled-medical-devices-fda-seeks-public-input/]
- 54. Laser direct writing of micro- and nano-scale medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC2916174/]
- 55. Microscale and Nanoscale Fabrication: From Traditional ... [https://hummink.com/microscale-and-nanoscale-fabrication-from-traditional-techniques-to-the-hpcap-revolution/]
- 56. Experimental Characterization Techniques for Micro ... [https://link.springer.com/rwe/10.1007/978-3-540-29857-1_51]
- 57. A quantitative framework to group nanoscale and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5875420/]
- 58. Nature-inspired surface modification strategies for ... [https://www.sciencedirect.com/science/article/pii/S2590006425001735]
- 59. Recent Advances in PEEK for Biomedical Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300588/]
- 60. Recent advances in the functionalization of surface ... [https://www.sciencedirect.com/science/article/abs/pii/S2468023025017596]
- 61. Recent Advances and Challenges in Nanoscale ... [https://www.mdpi.com/journal/micromachines/special_issues/I2308JT8R6]
- 62. Editorial: Advances in nanomedicine: revolutionizing ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1736031/full]
- 63. CDRH Regulatory Science Priorities [https://www.fda.gov/medical-devices/science-and-research-medical-devices/cdrh-regulatory-science-priorities]
- 64. A scoping review of reporting gaps in FDA-approved AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11450195/]
- 65. Comparison of nanoscale and microscale bioactive glass ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961207010599]
- 66. Evaluation framework for selecting wearable activity ... [https://pubmed.ncbi.nlm.nih.gov/33634189/]
- 67. A novel equipment contribution evaluation framework for ... [https://www.sciencedirect.com/science/article/pii/S0957417424029099]
- 68. How AI is Revolutionizing Manufacturing [https://www.qad.com/blog/2025/08/ai-in-manufacturing-trends-technologies-benefits]
- 69. Artificial Intelligence in Manufacturing Research Report ... [https://finance.yahoo.com/news/artificial-intelligence-manufacturing-research-report-080200453.html]
- 70. AI Production Optimization: Transforming 2025 ... [https://sparkco.ai/blog/ai-production-optimization-transforming-2025-manufacturing]
- 71. 2025 Smart Manufacturing and Operations Survey [https://www.deloitte.com/us/en/insights/industry/manufacturing/2025-smart-manufacturing-survey.html]
- 72. Smart Manufacturing 2025: Technology's rise - and why it ... [https://www.deloitte.com/dk/en/blogs/cxo-board/blog-tore-s-mart-manufacturing-2025-Technologys-rise-and-why-it-still-comes-down-to-people.html]
- 73. Controllable degradation behavior, mechanical properties ... [https://www.nature.com/articles/s41529-025-00658-8]
- 74. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 75. Nanomedicine: Key Applications, Benefit, and Future ... [https://www.delveinsight.com/blog/nanomedicine-market]
- 76. Nanomedicine Statistics and Facts (2025) [https://media.market.us/nanomedicine-statistics/]
- 77. Nanomaterials for biomedical applications: Addressing ... [https://www.sciencedirect.com/science/article/pii/S266697812500056X]
- 78. Nanotechnology in Medical Devices Market Poised for ... [https://medcloudinsider.com/articles/2025/03/19/nanotechnology-in-medical-devices-market-poised-for-growth.aspx]
- 79. United States Life Sciences Microscopy Devices Market ... [https://www.linkedin.com/pulse/united-states-life-sciences-microscopy-devices-4z3ye/]
- 80. Recent Advances in Preclinical Testing of Novel Devices [https://evtoday.com/articles/2025-june/recent-advances-in-preclinical-testing-of-novel-devices]
- 81. The Top 17 Healthcare Technology Trends 2025 [https://tateeda.com/blog/healthcare-technology-trends]
- 82. Applications of Novel Microscale and Nanoscale Materials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11511338/]
- 83. How micro-AM produces next-gen precision medical devices [https://med-techinsights.com/2024/08/01/how-micro-am-produces-next-gen-precision-medical-devices/]
- 84. MedTech Trends in 2025: Transforming Healthcare [https://www.merillife.com/blogs/med-tech-trends-in-2025-catalyzing-healthcare-through-innovation]
- 85. AI-powered drug development: 2025 Revolution [https://lifebit.ai/blog/ai-powered-drug-development-2025-revolution/]
- 86. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]