Nanostructured Surfaces for Bacterial Reduction: Mechanisms, Applications, and Clinical Translation
This article provides a comprehensive evaluation of nanostructured surfaces as a strategic solution for reducing bacterial load, a critical challenge in healthcare and biomaterial science.
Nanostructured Surfaces for Bacterial Reduction: Mechanisms, Applications, and Clinical Translation
Abstract
This article provides a comprehensive evaluation of nanostructured surfaces as a strategic solution for reducing bacterial load, a critical challenge in healthcare and biomaterial science. It explores the foundational mechano-bactericidal mechanisms by which nanoscale topographies physically inactivate pathogens, offering an alternative to conventional antibiotics. The review details the latest methodological advances in fabricating these surfaces, from self-assembled biomimetic structures to anodized nanotubes, and their applications in medical implants, wound dressings, and biosensors. It further addresses key troubleshooting and optimization challenges, including the complex role of protein fouling and the need for precise nanostructure design. Finally, the article critically assesses validation techniques and comparative performance data, synthesizing findings to outline a path for the clinical implementation of these advanced antibacterial interfaces.
The Mechano-Bactericidal Principle: How Nanotopographies Inactivate Bacteria
The Natural Blueprint: Insect Wing Nanostructures
Bioinspired nanostructures draw their design from natural surfaces that have evolved over millennia to combat microbial contamination. The wings of cicadas and dragonflies have garnered significant scientific interest because they possess nanoscale topographic features that impart potent antibacterial properties without the use of chemicals [1]. This mechanobactericidal effect offers a promising, antibiotic-free strategy to reduce bacterial colonization on surfaces, particularly in medical implant applications [2] [3].
These insect wings are not simply flat membranes; they are covered in a dense array of nanopillars or nanoprotrusions. When bacteria attempt to adhere to these surfaces, the physical interaction between the bacterial cell envelope and the sharp nanofeatures leads to cell death. The primary advantage of this mechanism is its physical nature, which reduces the likelihood of bacteria developing resistance compared to conventional chemical antibiotics [4].
Comparative Analysis of Natural Nanostructures
The following table summarizes the key dimensional characteristics of nanostructures found on various cicada and dragonfly wings, which are crucial for their antibacterial function.
Table 1: Nanostructure Dimensions on Insect Wings
| Insect Species | Wing Type | Nanofeature Type | Height (nm) | Diameter/Width (nm) | Spacing (nm) |
|---|---|---|---|---|---|
| Amphipsalta cingulata [5] | Cicada | Nanopillar | Information Missing | Information Missing | Information Missing |
| Kikihia scutellaris [5] | Cicada | Nanopillar | Information Missing | Information Missing | Information Missing |
| Neotibicen Canicularis [6] | Cicada | Nanopillar Cone | ~200 | ~90 (pillar), ~150 (base) | ~180 (center-to-center) |
| M. intermedia [3] | Cicada | Conical Nanopillar | 241 | 156 | 165 |
| Sympetrum vulgatum [7] | Dragonfly | Irregular Nanostructure | 83 - 195 | 83 - 195 | Information Missing |
Antibacterial Performance of Natural Wings
The nanostructures on insect wings exhibit varying efficacy against different types of bacteria. The following table outlines the bactericidal performance observed in experimental studies.
Table 2: Antibacterial Efficacy of Natural Insect Wings
| Insect Species | Tested Bacteria | Gram Reaction | Reported Efficacy | Key Observations |
|---|---|---|---|---|
| Psaltoda claripennis (Cicada) [8] | Pseudomonas aeruginosa | Negative | High | Mechanical rupture of bacterial cells observed. |
| Psaltoda claripennis (Cicada) [8] | Bacillus subtilis | Positive | Resistant | Rigid cell wall likely confers resistance. |
| Psaltoda claripennis (Cicada) [8] | Staphylococcus aureus | Positive | Resistant | Rigid cell wall likely confers resistance. |
| Diplacodes bipunctata (Dragonfly) [4] | P. aeruginosa, E. coli | Negative | High | Envelope deformation and penetration. |
| Diplacodes bipunctata (Dragonfly) [4] | S. aureus, B. subtilis | Positive | Effective | Capillary architecture enhances killing of Gram-positive types. |
Fabrication of Bioinspired Synthetic Nanostructures
To harness these antibacterial properties for biomedical applications, researchers have developed advanced techniques to mimic insect wing nanostructures on synthetic materials, especially those used for medical implants like titanium alloys [3] [6].
Common Fabrication Techniques
- Hydrothermal Etching: This method involves treating titanium alloy discs with alkaline solutions (e.g., KOH or NaOH) at high temperatures (150–180°C) in an autoclave. This process creates nano-structured surfaces by chemical etching, with the specific etchant influencing the resulting nanomechanical properties [9].
- Glancing Angle Deposition (GLAD): A physical vapor deposition technique used to create complex 3D nanofeatures. In one approach, a layer of self-assembled nanospheres (e.g., 200nm polystyrene) acts as a template. Subsequent oxygen plasma etching reduces the sphere size to create defined seeds, and then electron beam evaporation at a high incident angle (e.g., 85°) grows nanopillars on these seeds, closely replicating the cicada wing morphology [6].
- Thermal Oxidation: This process generates nanopillars on titanium alloy surfaces by oxidizing the material at high temperatures (e.g., 850°C for 5 minutes), resulting in a nanotopography primarily composed of rutile titanium dioxide (TiO₂) that mimics dragonfly wings [4].
Comparison of Fabricated Nanostructure Performance
The antibacterial success of synthetic mimics depends heavily on their geometric parameters. The table below compares the performance of surfaces fabricated using different methods.
Table 3: Performance of Bioinspired Synthetic Nanostructures
| Fabrication Method | Material | Key Nanofeature Dimensions | Target Bacteria | Reported Antibacterial Effect |
|---|---|---|---|---|
| Thermal Oxidation [4] | TiO₂ (Titanium Alloy) | Mimics dragonfly wing | S. aureus, E. coli, K. pneumoniae | Cell envelope deformation & penetration; induced oxidative stress; inhibited cell division. |
| GLAD [6] | Synthesized Nanostructures | Pillars: ~90 nm diameter, ~200 nm height; Base spacing: ~180 nm | E. coli | Bacteria puncturing and death observed. |
| Hydrothermal Etching (KOH) [9] | Titanium Alloy (Ti6Al4V) | Information Missing | Model for cell interaction | Reduced surface stiffness (20 ± 3 N/m) and altered short/long-range interaction forces. |
| Hydrothermal Etching (NaOH) [9] | Titanium Alloy (Ti6Al4V) | Information Missing | Model for cell interaction | Reduced surface stiffness (29 ± 4 N/m) and altered surface energy compared to control. |
Decoding the Bactericidal Mechanism
The initial understanding was that nanopillars kill bacteria solely by mechanically rupturing the cell membrane as it stretches between the pillars [2] [8]. However, more recent research reveals a more complex and multi-faceted mechanism.
The Mechanobactericidal Effect
The process begins with the adhesion of a bacterial cell to the nanopillar tips. Attractive forces, such as van der Waals forces, then cause the cell membrane to be pulled down the sides of the pillars [2] [5]. This adhesion creates a mechanical stress on the cell envelope. If this stress exceeds the elastic limit of the membrane, it can lead to irreversible rupture and cell death [8].
Beyond Mechanical Rupture: Oxidative Stress and Penetration
Advanced studies indicate that physical rupture is not the only pathway. Research on titanium nanopillars has shown that they can indent and penetrate the bacterial envelope without causing immediate lysis [4]. This physical insult triggers a physiological response in the bacteria, including the production of reactive oxygen species (ROS). An overabundance of ROS leads to oxidative stress, which damages cellular components like proteins, lipids, and DNA, ultimately resulting in cell death [4]. Furthermore, nanopillars have been observed to inhibit bacterial cell division, adding another layer to their antibacterial efficacy [4].
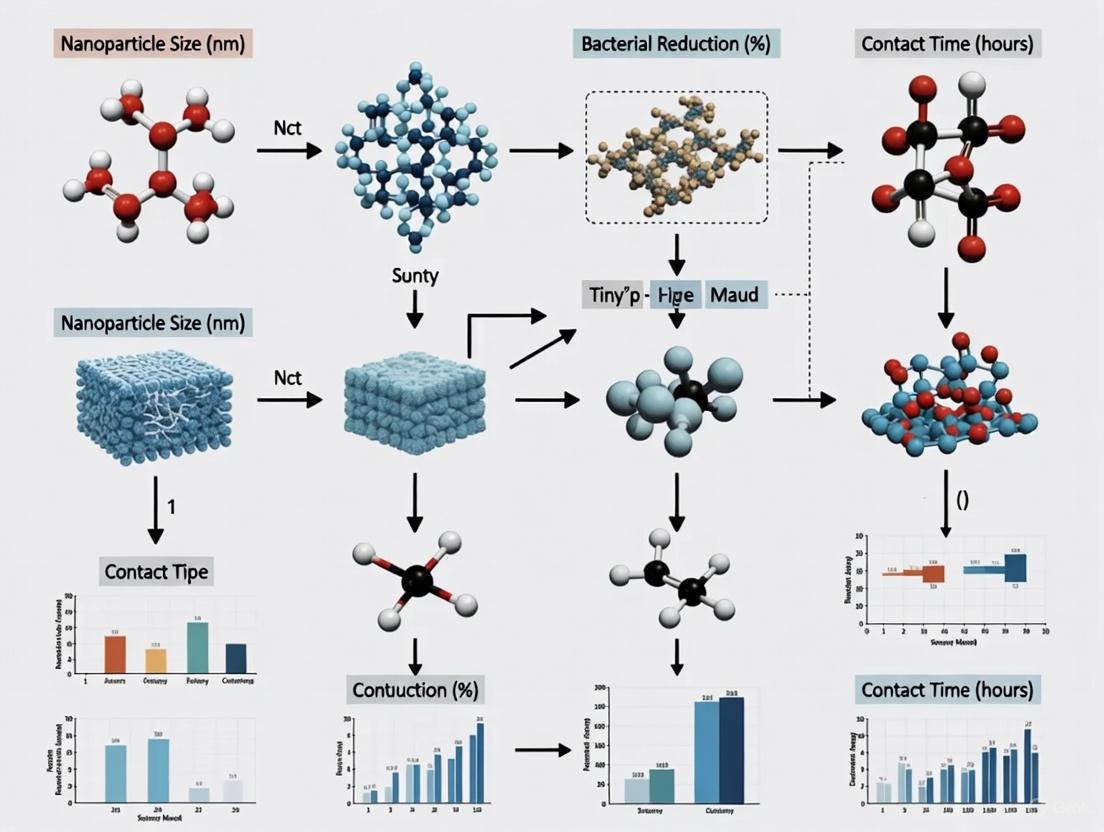
The following diagram illustrates the multi-mechanism pathway leading to bacterial death on nanopillar surfaces.
Essential Experimental Protocols for Evaluation
Robust evaluation of antibacterial nanostructures requires standardized protocols, though methods can vary across studies. The following outlines a common approach for assessing viability of bacteria on test surfaces.
Bacterial Viability Assay with Live/Dead Staining
This protocol is widely used to quantitatively distinguish between live and dead bacteria on a surface after contact [5].
Key Reagent Solutions:
- Bacterial Suspension: Bacteria (e.g., E. coli, S. aureus) are cultured in a nutrient broth (e.g., Lysogeny broth) and grown to the mid-exponential phase, typically until an optical density at 600 nm (OD⁶⁰⁰) of 0.7 is reached [5].
- Fluorescent Stains:
- SYTO 9/Hoechst 33343: These cell-permeant nucleic acid stains label all bacteria, both live and dead, emitting green/blue fluorescence [8] [5].
- Propidium Iodide (PI): This cell-impermeant stain only enters bacteria with compromised membranes, binding to DNA and producing red fluorescence. It is used to indicate dead cells [8] [5].
Workflow:
- Sample Incubation: The nanostructured sample (e.g., a 5 mm disc) is incubated in the bacterial suspension for a set period (e.g., 1 hour at room temperature) [5].
- Staining: After incubation, the sample is exposed to a mixture of the fluorescent stains.
- Visualization and Analysis: The stained sample is visualized using Confocal Laser Scanning Microscopy (CLSM) or fluorescence microscopy. Live cells fluoresce green/blue, while dead cells with damaged membranes fluoresce red. The ratio of red to green/blue fluorescence provides a quantitative measure of bactericidal efficiency [8] [5].
Characterization of Nanostructure Morphology
Accurate characterization of the nanostructures themselves is critical for correlating structure with function.
- Scanning Electron Microscopy (SEM): Provides high-resolution images of the surface topography and the morphological state of bacteria attached to the surface. Samples are often sputter-coated with a thin layer of gold/palladium to enhance conductivity before imaging [5] [6].
- Atomic Force Microscopy (AFM): Used for detailed topographical analysis of the nanostructures, providing 3D profiles and quantitative data on height, spacing, and roughness. AFM can also be used in force spectroscopy mode to measure nanomechanical properties and interaction forces between a probe tip and the surface [7] [9].
The Scientist's Toolkit: Key Research Reagents and Materials
This table lists essential materials and reagents used in the fabrication and testing of bioinspired antibacterial nanostructures, as derived from the experimental protocols in the search results.
Table 4: Essential Research Reagents and Materials
| Category | Item | Function in Research | Example Context |
|---|---|---|---|
| Substrate Materials | Medical Grade Titanium Alloy (Ti6Al4V) | A common biomaterial for orthopaedic implants used as a substrate for creating antibacterial nanostructures. | [4] [9] |
| Fabrication Reagents | Potassium Hydroxide (KOH) / Sodium Hydroxide (NaOH) | Alkaline etchants used in hydrothermal etching to create nano-structured surfaces on titanium. | [9] |
| Polystyrene Nanospheres | Used as self-assembled templates or "seeds" for the controlled growth of nanopillars in GLAD fabrication. | [6] | |
| Bacterial Culture | Lysogeny Broth (LB Medium) | A nutrient-rich growth medium used for cultivating bacterial strains for testing. | [5] |
| Glycerol in PBS | Used as a cryoprotectant for preparing long-term storage stocks of bacterial cultures. | [5] | |
| Viability Assay | LIVE/DEAD BacLight Bacterial Viability Kit (SYTO 9 & PI) | A fluorescent stain kit used to simultaneously label live (green) and dead (red) bacteria for viability counts. | [8] |
| Propidium Iodide (PI) | A red-fluorescent nucleic acid stain that only penetrates cells with damaged membranes, labeling dead cells. | [5] | |
| Hoechst 33342 | A blue-fluorescent cell-permeant DNA stain that labels all bacterial cells. | [5] | |
| Characterization | Gold/Palladium Target | Used for sputter-coating non-conductive samples (e.g., insect wings) to make them conductive for SEM imaging. | [5] |
The development of nanostructured surfaces as a means to combat bacterial colonization represents a paradigm shift in antibacterial strategies, moving beyond conventional biochemical approaches to exploit fundamental physical laws. These surfaces induce bacterial cell death through mechanical forces, primarily by piercing the cell envelope, stretching the membrane to the point of critical failure, or initiating explosive lysis from within. This guide provides a comparative analysis of these physical mechanisms, supported by experimental data and detailed methodologies, to assist researchers in evaluating and selecting appropriate nanostructured surfaces for specific applications. The physical disruption of bacterial membranes offers a compelling advantage over traditional antibiotics: it minimizes the likelihood of resistance development by targeting the structural integrity of the cell itself, a feature that is difficult for bacteria to evolve countermeasures against. Understanding the nuances of piercing, stretching, and lysis is therefore critical for advancing the field of mechano-bactericidal materials and their application in healthcare, industrial, and environmental settings.
Comparative Analysis of Disruption Mechanisms
The following sections dissect the three primary physical mechanisms, summarizing their key characteristics, effectiveness, and experimental evidence.
Piercing: Nanostructure-Induced Membrane Penetration
The piercing mechanism involves the physical penetration of the bacterial cell envelope by sharp, high-aspect-ratio nanostructures. This is a direct physical attack that compromises the integrity of the cell wall and underlying membranes.
- Mechanism of Action: When a bacterial cell adheres to a surface featuring nano-protrusions like nanospikes or nanorods, its own weight and adhesive forces can drive these sharp features through the outer membrane (in Gram-negative bacteria) and the cell wall, ultimately rupturing the inner membrane. This penetration creates physical holes, leading to uncontrolled efflux of cellular contents and influx of external media, resulting in rapid cell death.
- Key Evidence: Recent advanced fluorescence microscopy techniques have directly detected membrane penetration. Using a mechanosensitive fluorescent probe (Flipper-TR), researchers have visualized and quantified the localized stress and compression of bacterial membranes upon contact with nanostructured, mechano-bactericidal substrates, confirming the piercing action [10].
- Material Design: The efficacy of piercing is highly dependent on nanostructure geometry. Surfaces with sharper tips, higher aspect ratios, and optimal inter-structure spacing (typically comparable to or smaller than the size of a bacterial cell) are most effective. Materials such as black silicon and nanostructured titanium are prominent examples that utilize this mechanism [11].
Stretching: Turgor Pressure-Driven Membrane Expansion
Stretching, or membrane bulging, is a mechanism where defects in the cell wall lead to the uncontrolled expansion of the underlying membrane due to the cell's internal turgor pressure. This is often an indirect consequence of antibiotic action or enzymatic activity.
- Mechanism of Action: Many antibiotics, such as β-lactams (e.g., cephalexin), inhibit enzymes responsible for cell wall synthesis and cross-linking. This results in large defects in the peptidoglycan layer. The rigid cell wall, which normally restrains the inner membrane, is compromised. The high internal turgor pressure (approximately 0.3–2 atm in E. coli) then forces the membrane to bulge outward through these defects, forming a spherical bleb [12].
- Key Evidence and Dynamics: Research on Escherichia coli has delineated this process into two distinct phases. The initial formation of a "bulge" occurs rapidly, on a timescale of about 1 second, as the membrane relaxes through the wall defect. This is followed by a slower "swelling" phase, lasting about 100 seconds, where the bulge grows as wall defects enlarge. Final lysis occurs when the membrane exceeds its yield areal strain [12].
- Energetics: The process is energetically favorable because the relaxation of the stretching and entropic energies of the inner membrane outweighs the bending energy cost of forming the bulge. Lysis is the ultimate endpoint when the stretched membrane can no longer withstand the pressure [12].
Explosive Lysis: Endolysin-Mediated Catastrophic Rupture
Explosive cell lysis is a biologically programmed event that results in the instantaneous and catastrophic disintegration of the bacterial cell, serving as a source of extracellular DNA and membrane vesicles for the biofilm community.
- Mechanism of Action: In bacteria like Pseudomonas aeruginosa, a sub-population of cells can undergo a rapid lytic event mediated by a cryptic prophage endolysin (e.g., Lys protein). This endolysin degrades the peptidoglycan cell wall. The loss of this primary stress-bearing structure causes the cell to rapidly transition from a rod to a round shape in less than 5-10 seconds, after which it explodes [13].
- Key Evidence: Live-cell super-resolution microscopy has captured these events, showing the annihilation of the cell and the simultaneous release of cytoplasmic content and shattered membrane fragments that spontaneously form membrane vesicles (MVs). This lysis is essential for providing extracellular DNA that strengthens the biofilm matrix [13].
- Induction: Explosive lysis can be a stochastic event or induced by external stresses such as antibiotic treatment (e.g., ciprofloxacin) or genotoxic stress (e.g., mitomycin C), and is dependent on the RecA-mediated SOS stress response [13].
Quantitative Comparison of Mechanisms
The table below synthesizes key quantitative data and characteristics for the three primary disruption mechanisms.
Table 1: Comparative Data on Bacterial Membrane Disruption Mechanisms
| Mechanism | Primary Trigger | Key Physical Force | Characteristic Timescale | Key Observational Evidence |
|---|---|---|---|---|
| Piercing | Contact with sharp nanostructures | Localized mechanical stress & penetration | Instantaneous upon contact | Fluorescence lifetime changes indicating membrane compression [10] |
| Stretching | Cell wall defect (e.g., from β-lactams) | Internal turgor pressure (~0.5 atm) | Bulge: ~1 s; Swelling: ~100 s [12] | Phase-contrast microscopy of bulge formation and growth [12] |
| Explosive Lysis | Activation of prophage endolysin | Peptidoglycan degradation & turgor pressure | Rod-to-round transition: <5-10 s [13] | Super-resolution microscopy of cell explosion and vesicle formation [13] |
Experimental Protocols for Key Studies
To facilitate replication and further research, this section outlines the detailed methodologies from foundational studies on stretching and explosive lysis.
Protocol: Analyzing Membrane Bulging and Lysis via β-lactam Treatment
This protocol is adapted from studies on the mechanics of antibiotic-induced lysis in E. coli [12].
- 1. Bacterial Strain and Growth: Use wild-type E. coli (e.g., MG1655). Grow cells in a standard rich medium (e.g., LB) to mid-exponential phase.
- 2. Cell Wall Digestion: Treat the bacterial culture with a β-lactam antibiotic such as cephalexin at a concentration of 50 μg/mL. This inhibits transpeptidase enzymes, preventing new cross-links in the peptidoglycan layer and leading to large wall defects as the cell grows.
- 3. Microscopy and Image Analysis:
- Mount the treated cells on an agarose pad for live-cell imaging.
- Use phase-contrast or differential interference contrast (DIC) microscopy to observe morphological changes at a frame rate sufficient to capture rapid dynamics (high-speed imaging).
- Quantify the timescales of bulging (initial protrusion formation) and swelling (protrusion growth) by analyzing video data.
- 4. Physical Modeling:
- Model the cell wall as a rigid, orthotropic cylindrical shell with elastic moduli (e.g., axial direction, Yxw=0.1 N/m; circumferential direction, Yyw=0.2 N/m).
- Model the inner and outer membranes as linear-elastic shells with area stretch moduli of ~0.1 N/m.
- Calculate the free energy of the system, accounting for cell wall and membrane stretching energies, bending energies, and the entropy of mixing related to turgor pressure, to predict bulge formation and stability.
Protocol: Visualizing Explosive Cell Lysis in Biofilms
This protocol is based on research investigating explosive lysis in P. aeruginosa biofilms [13].
- 1. Bacterial Strain and Biofilm Culture: Use P. aeruginosa PAK or PAO1. Cultivate interstitial biofilms on a glass-bottom dish using a minimal medium to promote monolayer biofilm formation that is conducive to microscopy.
- 2. Fluorescent Staining:
- eDNA Staining: Add a cell-impermeant fluorescent nucleic acid stain like TOTO-1 or SYTOX Green to the medium to label extracellular DNA (eDNA) released upon lysis.
- Cytoplasmic Labeling (Optional): Engineer bacteria to express a cytoplasmic fluorescent protein (e.g., CFP) to visualize the release of cytoplasmic content.
- Viability Staining (Optional): Use a live-cell impermeant stain like ethidium homodimer-2 (EthHD-2) to confirm membrane integrity of round cells prior to explosion.
- 3. Stress Induction (Optional): To induce higher rates of lysis, expose the biofilm to a gradient of ciprofloxacin (antibiotic stress) or mitomycin C (genotoxic stress).
- 4. Time-Lapse Super-Resolution Microscopy:
- Image the biofilm using both phase-contrast and fluorescence channels over time.
- Use high-resolution microscopy (e.g., STORM/PALM) to capture the formation of membrane vesicles from shattered membrane fragments post-lysis.
- Analyze the survival time of round cells and the frequency of eDNA release events.
- 5. Genetic Validation: Construct a mutant deficient in the endolysin gene (Δlys) to confirm the protein's role. Explosive lysis should be abrogated in the mutant and restored with wild-type lys provided in trans.
Signaling Pathways and Experimental Workflows
The following diagrams, defined using the DOT language, illustrate the logical progression of the explosive lysis mechanism and a general workflow for evaluating nanostructured surfaces.
Explosive Lysis Pathway
Nanostructured Surface Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
This section details key reagents, materials, and tools used in the experimental studies cited in this guide, providing a resource for researchers designing their own experiments.
Table 2: Key Reagents and Materials for Studying Bacterial Membrane Disruption
| Item Name | Function/Description | Example Application |
|---|---|---|
| Flipper-TR | A mechanosensitive fluorescent probe that embeds in membranes; its fluorescence lifetime inversely correlates with membrane tension. | Visualizing and quantifying membrane stress upon contact with nanostructured surfaces [10]. |
| Cephalexin | A β-lactam antibiotic that inhibits transpeptidases, preventing cell wall cross-linking and creating defects that lead to bulging. | Inducing membrane stretching and lysis in E. coli for mechanistic studies [12]. |
| Streptolysin O (SLO) | A pore-forming toxin that creates large (~30 nm) pores in mammalian and bacterial membranes for controlled permeabilization. | Used in cell resealing techniques to deliver membrane-impermeable molecules into cells [14]. |
| Titanium with Micro/Nanostructure | A biocompatible material whose surface is modified with nanostructures (e.g., nanotubes) to impart antibacterial properties. | Studying competitive growth of osteoblasts vs. bacteria and piercing mechanisms [11]. |
| TOTO-1 / SYTOX Green | Cell-impermeant nucleic acid stains that fluoresce upon binding to DNA. Used to mark extracellular DNA (eDNA). | Visualizing sites of explosive cell lysis in bacterial biofilms [13]. |
| Quartz Crystal (QC) with Nanostructures | A macroscopic oscillator whose surface is modified with a "forest" of nanobristles to amplify interactions with the surrounding medium. | Studying exponential enhancement of viscous dissipation at the solid-gas interface [15]. |
| Endolysin (Lys) Mutant | A genetically engineered P. aeruginosa strain with a knockout of the prophage endolysin gene (PA0629). | Validating the essential role of endolysin in explosive cell lysis and biofilm matrix development [13]. |
The Critical Role of Surface Roughness, Nanospike Density, and Aspect Ratio
The growing challenge of antibiotic resistance has intensified the focus on developing non-chemical antibacterial surfaces for applications in healthcare, public hygiene, and medical implants. Inspired by natural nanostructures found on insect wings, engineered surfaces with specific topographic features have demonstrated remarkable ability to inhibit bacterial colonization and cause bacterial death through mechanical contact. This review objectively compares the performance of various nanostructuring approaches, focusing on three critical parameters: surface roughness, nanospike density, and aspect ratio. These parameters collectively determine the mechanobactericidal efficacy of nanostructured surfaces by influencing bacterial adhesion, membrane stress, and eventual rupture.
The mechanobactericidal effect occurs when nanoscale features on a surface apply sufficient stress to bacterial cell walls and outer membranes, compromising their structural integrity. While the exact killing mechanism continues to be investigated, several hypotheses have been proposed, including direct piercing of the cell membrane, creep failure, motion-induced shear failure, and oxidative stress-induced cell death. What remains clear is that surface topography plays a decisive role in this process, with specific geometric parameters directly influencing bactericidal efficiency. Understanding these parameters enables researchers to design surfaces that maximize antibacterial activity while maintaining biocompatibility and mechanical stability.
Comparative Performance Analysis of Nanostructured Surfaces
The following tables summarize key experimental findings from recent studies, comparing the antibacterial performance of surfaces with different roughness characteristics, nanospike geometries, and material compositions.
Table 1: Impact of Surface Roughness on Bacterial Adhesion
| Material Type | Surface Treatment | Roughness (Ra, μm) | Bacterial Strain | Adhesion/Bactericidal Effect | Reference |
|---|---|---|---|---|---|
| Nanohybrid Composite Resin (Charisma Topaz) | Mylar strip (control) | 0.07 ± 0.01 | S. mutans | 3.57 ± 0.32 log CFU/mL | [16] |
| Nanohybrid Composite Resin (Charisma Topaz) | Sof-Lex Polishing | 0.09 ± 0.03 | S. mutans | No significant difference from control | [16] |
| Nanofilled Composite Resin (Estelite Asteria) | Mylar strip (control) | 0.07 ± 0.01 | S. mutans | Significantly lower than nanohybrid | [16] |
| Nanofilled Composite Resin (Estelite Asteria) | Opti1Step Polishing | 0.09 ± 0.03 | S. mutans | No significant difference from control | [16] |
Table 2: Performance of Biomimetic Nanospike Surfaces
| Material/Substrate | Fabrication Method | Nanospike Feature | Bacterial Strain | Reduction/Efficacy | Key Findings | Reference |
|---|---|---|---|---|---|---|
| Polymethyl Methacrylate (PMMA) Film | APLTP + Annealing | Sharp-edged nanospikes | E. coli | >99.9% (CFU < 10) | Combined sharpness and controlled wettability | [17] |
| Titanium Dental Implant | H₂SO₄/H₂O₂ Treatment | Uniform nanospike layer | Multiple oral strains | 70-90% reduction | Improved osseointegration (56% vs 41% bone contact) | [18] |
| Titanium Dental Implant | Grit-blasting + Acid Etching (Control) | Conventional roughness | Multiple oral strains | Control baseline | Lower bone contact index (41%) | [18] |
| Black Silicon | Reactive Ion Etching | Nanopillars | Various | Bactericidal | Replicates cicada wing effect | [17] |
Table 3: Bacterial Cell Geometry and Deformation Parameters
| Parameter | Bacterial Type | Typical Value | Experimental Context | Significance | Reference |
|---|---|---|---|---|---|
| Aspect Ratio (η) | Rod-shaped (e.g., E. coli) | 4.14 ± 0.17 | Steady-state growth | Preserved across growth conditions, influences contact area with nanostructures | [19] |
| Aspect Ratio (η) | Coccoid (e.g., S. aureus) | 1.38 ± 0.18 | Under antibiotic exposure | Affects the mechanical stability and points of stress application | [19] |
| Surface-to-Volume Scaling | Rod-shaped Bacteria | S ≈ 2πV²/³ | Nutrient adaptation | Links cell size to membrane tension under deformation | [19] |
| Cell Wall Elasticity | E. coli | ~300% increase from relaxed state | Isolated sacculi measurement | Indicates capacity to withstand stretching before rupture | [2] |
Detailed Experimental Protocols and Methodologies
Protocol 1: Assessing Surface Roughness and Bacterial Adhesion on Composites
This methodology is designed to evaluate how different polishing procedures affect the surface roughness of composite resins and subsequent adhesion of Streptococcus mutans [16].
Specimen Preparation:
- Materials: Two composite resins are used: a nanofilled (Tokuyama Estelite Asteria) and a nanohybrid (Charisma Topaz). The key research reagents are listed in Table 4.
- Fabrication: Eighty disk-shaped specimens (8 mm diameter, 2 mm thickness) are fabricated using a cylindrical mold. A transparent Mylar strip is placed over the material and pressed with a glass slide to extrude excess material and create a flat surface before light-curing.
- Polymerization: Specimens are polymerized using an LED light-curing device (Elipar Free Light, 1200 mW/cm²) according to manufacturers' instructions (20s for Charisma Topaz, 10s for Estelite Asteria).
- Polishing: The specimens are divided into four groups (n=10 per group per material):
- Group A (Control): No polishing, Mylar strip surface only.
- Group B (Multi-step): Polished with Sof-Lex discs (coarse, medium, fine, superfine) at 10,000-30,000 rpm for 20s per disc.
- Group C (Two-step): Polished with Clearfil Twist Dia diamond-impregnated wheels at 10,000 rpm for 20s per wheel.
- Group D (One-step): Polished with Opti1Step diamond-impregnated polisher at 10,000 rpm for 20s under dry conditions.
Surface Roughness and Microbiological Analysis:
- Roughness Measurement: Surface roughness (Ra) is measured using a profilometer (Mahr M1 Perthometer). Three measurements are taken at different points on each sample, and the mean Ra value is calculated.
- Sterilization: All composite samples are sterilized in an autoclave at 121°C and 1 atm pressure for 15 minutes.
- Saliva Treatment: Sterilized samples are divided into two subgroups. The "artificial saliva-treated" group is incubated with artificial saliva (containing mucin) for 1 hour at room temperature to form a salivary pellicle. The "non-treated" group is not exposed to saliva.
- Bacterial Adhesion Assay: A solution containing S. mutans (ATCC 25175) is added to all samples, which are then incubated at 35–37°C for 24 hours. Adhered bacteria are quantified by colony counts, presented as log CFU/mL [16].
Experimental Workflow for Composite Roughness and Adhesion Study
Protocol 2: Fabrication of Biomimetic Nanospikes via Plasma Treatment
This protocol details a scalable method for creating sharp-edged nanospikes on polymer films using Atmospheric-Pressure Low-Temperature Plasma (APLTP), inspired by the bactericidal nanostructures on cicada wings [17].
PMMA Film Preparation and Plasma Treatment:
- Materials: Polymethyl methacrylate (PMMA) and ethyl lactate solvent.
- Film Casting: A 30 wt% PMMA solution in ethyl lactate is prepared. The solution is spin-coated onto a glass substrate at 1800 rpm for 24 seconds. The coated substrate is pre-baked in an oven at 100°C for 60 seconds, resulting in an initial film thickness of approximately 5 µm.
- Plasma Treatment: The PMMA-coated substrate is irradiated with APLTP. The plasma is generated with a He/O₂ gas mixture (2.0 slm He, 60 sccm O₂) at an RF power of 120 W (27.12 MHz). The plasma irradiation time is 5 seconds per cycle, followed by a 15-second cooling period. This cycle is repeated multiple times to achieve the desired etching and nanostructuring.
- Annealing: To control surface wettability while maintaining structural sharpness, the plasma-treated substrate is placed in an oven at 120°C for 5 days. This annealing step closes microscopic pores and restores hydrophobicity, which is crucial for optimal antibacterial performance.
Surface Characterization and Antibacterial Testing:
- Topography Analysis: The surface profile and formation of micro/nanostructures are confirmed using Atomic Force Microscopy (AFM). The evaluation area is 5 x 5 µm² with a resolution of 512 x 512 points.
- Wettability Assessment: The contact angle is measured using a sessile drop method with 2 µL of pure water to evaluate surface hydrophilicity/hydrophobicity.
- Antibacterial Assay: Antibacterial performance is evaluated against Escherichia coli according to ISO 22196 standards. The reduction in bacterial colonies is quantified, with counts below 10 CFU considered the detection limit [17].
Protocol 3: Creating Bactericidal Nanospikes on Titanium Implants
This method describes a chemical passivation process to generate a nanotextured, spiked layer on titanium dental implants to confer bactericidal properties without compromising osseointegration [18].
Surface Nanotexturing and Characterization:
- Material Preparation: Commercially pure titanium grade 3 implants with a grit-blasted rough surface serve as the substrate.
- Chemical Passivation: Test implants are immersed in a solution of sulfuric acid and hydrogen peroxide for 2 hours to form the nanospike surface. Standard implants without this treatment are used as controls.
- Surface Characterization:
- Roughness: Measured using white light interferometry (Wyko NT1100). The amplitude parameter (Sa) is determined from an analysis area of 124.4 x 94.6 µm.
- Wettability and Surface Energy: Contact angle analysis is performed with distilled water and formamide. The surface energy is calculated using the Owens, Wendt, Rabel, and Kaelble (OWRK) equation.
- Hydrogen Content: Analyzed using an Inert Gas Fusion LECO TCH600 to ensure no hydrogen embrittlement occurs.
- Fatigue Behavior: Evaluated using a servo-hydraulic testing machine (MTS Bionix) according to ISO 14801:2007 standards, with implants tested at a 30-degree angle under cyclical loading.
Biological and Bactericidal Testing:
- Osseointegration Assay: Human osteoblastic cells (SaOs-2) are cultured on the surfaces. Cell adhesion is measured at 3 and 7 days, and mineralization is analyzed via alkaline phosphatase levels at 14 days.
- In Vivo Bone Contact: Implants are inserted into rabbit tibiae. After 21 days, the bone-implant contact index is determined histologically.
- Bactericidal Capacity: Bacterial colonization assays are conducted using four relevant bacterial strains. The percentage reduction in colonization on the nanospike surface compared to the control is calculated [18].
Research Reagent Solutions and Materials
Table 4: Essential Research Materials and Their Functions
| Category/Item | Function in Research | Specific Example/Application |
|---|---|---|
| Composite Resins | Substrate for testing roughness vs. adhesion | Nanofilled (Estelite Asteria) vs. Nanohybrid (Charisma Topaz) [16] |
| Polishing Systems | Creating defined surface finishes on composites | Sof-Lex (multi-step), Clearfil Twist Dia (two-step), Opti1Step (one-step) [16] |
| Atmospheric-Pressure Low-Temperature Plasma (APLTP) | Scalable fabrication of nanostructures on polymers | Creating sharp-edged nanospikes on PMMA films [17] |
| Chemical Passivation Agents | Nanotexturing of metal surfaces | Sulfuric Acid & Hydrogen Peroxide for creating nanospikes on titanium [18] |
| Profilometer/Interferometer | Quantifying surface roughness (Ra) | Mahr M1 Perthometer; Wyko NT1100 Optical Interferometer [16] [18] |
| Atomic Force Microscope (AFM) | High-resolution imaging of nanotopography | Veeco Dimension Icon for characterizing nanospikes on PMMA [17] |
| Contact Angle Goniometer | Measuring surface wettability | OCA15plus-Dataphysics for surface energy calculations [18] |
| Standard Bacterial Strains | Evaluating bactericidal/adhesion performance | S. mutans (ATCC 25175), E. coli, oral pathogens [16] [17] [18] |
Mechanisms of Action and Interparameter Relationships
The antibacterial action of nanostructured surfaces is a complex process initiated by mechanical contact. The following diagram synthesizes the current understanding of the bactericidal pathway, from initial adhesion to cell death, and highlights how key surface parameters influence each step.
Proposed Mechanobactericidal Pathway and Parameter Influence
The relationship between these parameters and bacterial cell geometry is critical. Rod-shaped bacteria like E. coli maintain a conserved aspect ratio of approximately 4.14 during steady-state growth, following a surface-to-volume scaling relation (S ≈ 2πV²/³) [19]. This constant aspect ratio implies tighter geometric constraints than previously thought and influences how the cell membrane interacts with surface nanostructures. The mechanical failure likely occurs when the energy imposed by the nanostructures exceeds the elastic capacity of the bacterial cell wall, which can stretch up to 300% from its relaxed state [2]. Parameters like nanospike density directly influence the number of stress application points, while spike sharpness and aspect ratio concentrate stress to overcome the membrane's mechanical strength, leading to rupture.
Distinguishing Bactericidal vs. Anti-Adhesion Strategies
In the face of rising antibiotic resistance, the development of novel non-antibiotic strategies to combat bacterial infections has become a critical focus in biomedical research. Among the most promising approaches are those that target the initial interaction between bacteria and material surfaces, primarily categorized as bactericidal and anti-adhesion strategies. Bactericidal strategies aim to physically destroy bacterial cells upon contact with a surface, while anti-adhesion strategies focus on preventing bacterial attachment in the first place. This guide provides an objective comparison of these two mechanisms, focusing on their application to nanostructured surfaces, to inform researchers, scientists, and drug development professionals in their evaluation and selection process.
Core Mechanisms and Design Principles
The fundamental difference between these strategies lies in their approach to managing bacterial contamination. Bactericidal surfaces are designed to kill bacteria, whereas anti-adhesion surfaces are designed to repel them [20].
- Bactericidal (Contact-Killing) Mechanisms: These are often considered "active" strategies. Surfaces are engineered with specific nanoscale topographic features, such as nanopillars or nanowires, that mechanically rupture bacterial cell membranes upon contact. The killing mechanism is primarily physical, driven by the interaction between the nanostructures and the bacterial cell wall, leading to cell lysis and death [21] [22] [23].
- Anti-Adhesion Mechanisms: These are typically classified as "passive" strategies. They work by modifying the surface's physicochemical properties—such as topography, chemistry, wettability, and charge—to create an energy barrier that minimizes bacterial attachment. This is often achieved by creating a highly hydrophilic surface that forms a hydration layer, acting as a physical and energetic shield against approaching bacteria [20] [24].
The table below summarizes the key distinguishing characteristics of each strategy.
Table 1: Fundamental Comparison of Bactericidal and Anti-Adhesion Strategies
| Feature | Bactericidal Strategy | Anti-Adhesion Strategy |
|---|---|---|
| Primary Goal | Kill bacteria upon contact | Prevent initial bacterial attachment |
| Mechanism of Action | Physical rupture of the cell membrane by nanostructures | Modulation of surface energy, charge, and topography |
| Typical Surface Chemistry | Often cationic polymers (e.g., quaternary ammonium) | Hydrophilic/zwitterionic polymers (e.g., PEG) |
| Effect on Biofilm | Disrupts biofilm by killing founder cells | Inhibits biofilm formation by preventing initial colonization |
| Potential for Resistance | Considered low, as mechanism is physical [23] | Considered low, as it does not target viability |
| Key Challenge | Potential cytotoxicity to host cells [20] | May not kill bacteria, which could relocate and colonize other surfaces |
Comparative Experimental Data and Performance
Experimental data reveals how these strategies perform under various conditions, highlighting their respective strengths and limitations.
Bactericidal Efficacy of Nanostructured Surfaces
Nanostructured titanium surfaces have demonstrated significant bactericidal efficacy under both static and dynamic flow conditions, which are more representative of real-world applications like implants and catheters.
Table 2: Experimental Bactericidal Efficacy of a Nanostructured Titanium Surface [25]
| Bacterial Species | Static Condition (0 Pa) | Fluid Flow Condition (10 Pa) | Efficacy Increase under Flow |
|---|---|---|---|
| Pseudomonas aeruginosa (Gram-negative) | ~40% | ~60% | ∼1.5-fold |
| Staphylococcus aureus (Gram-positive) | ~20% | ~60% | ∼3-fold |
This data shows that fluid flow can significantly enhance the bactericidal effect, particularly for S. aureus. The study concluded that the efficacy was independent of the fluid wall shear stress level once flow was introduced [25].
Anti-Adhesion Performance via Microstructure Engineering
Research on copper samples has shown that microstructural refinement through High-Pressure Torsion (HPT) can enhance anti-adhesion properties without altering surface chemistry.
Table 3: Anti-Adhesion Effect of HPT-Processed Copper on S. aureus [26]
| Sample Type | Grain Size (nm) | Dislocation Density (m⁻²) | Bacterial Adhesion (Relative to Annealed Cu) |
|---|---|---|---|
| Annealed (Reference) | 27,700 | 9.18 × 10¹¹ | Baseline (100%) |
| HPT13.75 | ~300 | 5.15 × 10¹⁴ | Reduced |
| HPT53.75 | ~140 | 3.37 × 10¹⁴ | Further Reduced |
The study found a linear correlation between increased luminous intensity (indicating fewer adherent bacteria) and the inverse square root of grain size (grain size−0.5), directly linking material microstructure to anti-adhesion performance [26].
Visualization of Mechanisms and Workflows
The following diagrams illustrate the core mechanisms and experimental workflows for both strategies.
Bactericidal Mechanism of Nanostructured Surfaces
Anti-Adhesion Therapeutic Strategies
The Scientist's Toolkit: Key Research Reagents and Materials
This section details essential materials and reagents used in studying bactericidal and anti-adhesion surfaces, providing a foundation for experimental design.
Table 4: Essential Research Reagents and Materials
| Category | Item | Function / Relevance | Application Context |
|---|---|---|---|
| Model Surfaces | Titanium (Ti-6Al-4V) with nanowires | Model nanostructured surface for studying bactericidal efficacy under flow [25]. | Bactericidal |
| High-Pressure Torsion (HPT) processed Copper | Model for studying the isolated effect of microstructural defects (grain boundaries, dislocations) on anti-adhesion properties [26]. | Anti-Adhesion | |
| Bacterial Strains | Staphylococcus aureus (Gram-positive) | Common model for Gram-positive infections; used to test efficacy against thick peptidoglycan layer [25] [26]. | Both |
| Pseudomonas aeruginosa (Gram-negative) | Common model for Gram-negative, biofilm-forming bacteria; used to test efficacy against outer membrane [25]. | Both | |
| Escherichia coli (Gram-negative) | Standard model organism for initial screening of antibacterial properties [20]. | Both | |
| Inhibitors & Agents | MAM7-coated polystyrene microbeads | Competitive inhibitor that blocks bacterial adhesion to host cells by saturating binding sites [27]. | Anti-Adhesion |
| FimH antagonists (e.g., biphenyl mannosides) | High-affinity, orally available compounds that block adhesion of uropathogenic E. coli [28]. | Anti-Adhesion | |
| Pilicides and Curlicides | Small molecules that inhibit the assembly of chaperone-usher pili and curli fibers, critical for adhesion [28]. | Anti-Adhesion | |
| Analysis Tools | Microfluidic Devices (MFD) | Enables testing of bacterial adhesion and viability under controlled fluid wall shear stress [25]. | Both |
| Scanning Transmission Electron Microscopy (STEM) | Used for high-resolution analysis of the bacterium-substrate interface, revealing bacterial membrane damage [26]. | Bactericidal | |
| Fluorescence Staining (Live/Dead) | Standard protocol for enumerating viable and non-viable adherent bacteria on a surface [25]. | Both |
Detailed Experimental Protocols
To ensure reproducibility, below are detailed methodologies for key experiments cited in this guide.
- Surface Fabrication: Use a 1 mm thick Ti-6Al-4V sheet. Polish substrates to a surface roughness of 0.04 μm Ra. Fabricate nanowire structures on the polished surface via a hydrothermal synthesis process.
- Microfluidic Device (MFD) Setup: Design the MFD as a parallel-plate flow chamber. Sterilize the assembled device and substrates (70% v/v ethanol wash followed by UV exposure for 20 minutes).
- Bacterial Preparation: Cultivate P. aeruginosa and S. aureus. Suspend bacteria in an appropriate fluid medium at a fixed concentration.
- Flow Experiment: Pump the bacterial suspension through the MFD at defined flow rates (e.g., 0.12, 4.00, 8.00, 12.00 mL/min) to generate a range of fluid wall shear stress (0 - 10 Pa). Include a no-flow static condition as a control.
- Post-Experiment Analysis: Retrieve substrates from the MFD. Stain the adhered bacteria with a fluorescent live/dead viability kit. Image the surfaces using fluorescence microscopy and enumerate live and dead cell counts.
- Sample Preparation: Process pure copper samples using High-Pressure Torsion (HPT) for 1 and 5 rotations. Use an annealed copper sample (e.g., 600°C for 2 hours) as a micro-grained reference.
- Surface Preparation (Critical Step): Prepare all sample surfaces using a method that ensures comparable and very low surface roughness (Average Roughness, Ra ~4-7 nm) to isolate the effects of microstructure.
- Material Characterization: Perform microhardness measurements across the sample diameter. Use techniques like X-ray diffraction to determine dislocation density and grain size.
- Bacterial Adhesion Test: Incubate the prepared surfaces with Staphylococcus aureus suspension for a defined period under controlled conditions.
- Analysis: After incubation, stain the adherent bacteria with a fluorescent dye. Use luminometric analysis to quantify the number of adhered bacteria relative to the reference sample. Perform focused ion beam (FIB) milling and STEM-EDX analysis on selected bacterium-substrate interfaces to study the intercellular bacterial response.
Both bactericidal and anti-adhesion strategies offer compelling, resistance-resistant alternatives to conventional antibiotics. The choice between them depends heavily on the specific application. Bactericidal nanostructured surfaces are highly effective in eliminating bacteria but require careful design to mitigate potential cytotoxicity and ensure durability. Anti-adhesion strategies, through chemical or microstructural means, offer a prophylactic approach by preventing colonization and are inherently less cytotoxic. Future directions point towards the development of hybrid systems that integrate both active and passive mechanisms to achieve synergistic effects, enhanced efficacy, and prolonged functionality under complex physiological conditions [20]. The ongoing challenge for researchers is to optimize these designs for large-scale production and successful clinical translation.
Engineering and Implementing Antibacterial Nanostructures in Biomedical Devices
The rising challenge of antimicrobial resistance (AMR) has intensified the focus on developing surfaces for medical implants that can inherently resist bacterial colonization. Within this research domain, the creation of nanostructured surfaces on titanium (Ti) alloys via electrochemical anodization has emerged as a leading strategy. This technique enables the fabrication of highly ordered titanium dioxide (TiO2) nanotube arrays, which are actively investigated for their dual capacity to enhance osseointegration and provide antibacterial functionality. This guide provides a comparative evaluation of different anodization protocols and substrate manufacturing methods, presenting objective experimental data on the performance of the resulting TiO2 nanotube structures. The content is framed within the broader thesis of evaluating nanostructured surfaces for bacterial reduction, providing researchers and scientists with a detailed analysis of protocols and outcomes.
Core Mechanism and Antibacterial Action of TiO2 Nanotubes
The antibacterial efficacy of TiO2 nanotubes is primarily driven by photocatalytic pathogen inactivation. Upon exposure to light, particularly ultraviolet (UV) light, TiO2 acts as a photocatalyst. The energy from the light excites electrons, creating electron-hole pairs. These charge carriers migrate to the surface and react with water and oxygen, generating reactive oxygen species (ROS) such as superoxide radical anions (O2•−) and hydroxyl radicals (HO•) [29].
These ROS are highly oxidizing and inflict irreversible damage on bacterial cells. The mechanism, illustrated in the diagram below, involves a multi-stage attack: ROS first cause oxidative damage to the cell wall and membrane. This compromise of structural integrity allows ROS and, to a lesser extent, nanoparticles to penetrate the cytoplasm, leading to leakage of intracellular components, direct oxidative damage to proteins and nucleic acids, and ultimately, cell lysis and mineralization [29]. This multi-target mechanism makes it difficult for bacteria to develop resistance, a significant advantage over conventional antibiotics.
The susceptibility of bacteria to this photocatalytic attack is influenced by their cell wall structure. Gram-negative bacteria (e.g., E. coli), with their thinner peptidoglycan layer and outer membrane, are generally more susceptible than Gram-positive bacteria (e.g., S. aureus), which have a thicker peptidoglycan layer [29]. Furthermore, the nanotopography of the TiO2 layer itself can physically influence cell behavior. While it enhances protein adsorption and fibroblast adhesion for better soft tissue integration, the nanoscale features may also mechanically disrupt bacterial membranes [30].
Experimental Protocols for Fabrication and Characterization
Fabrication via Electrochemical Anodization
Electrochemical anodization is a relatively simple, cost-effective, and versatile technique suitable for implants with complex geometries [31]. The fundamental setup involves a two-electrode or three-electrode electrochemical cell where the titanium alloy substrate serves as the anode, and an inert material (e.g., graphite or platinum) acts as the cathode. Both are immersed in a fluoride-containing electrolyte.
- Key Process: When a constant voltage (DC) is applied, the titanium substrate oxidizes, forming a TiO2 layer. The fluoride ions (F⁻) in the electrolyte chemically dissolve this oxide, leading to the formation of a nanoporous layer. Under optimized conditions, the balance between electrochemical oxide growth and chemical dissolution leads to the self-organization of a highly ordered nanotubular array [31].
- Critical Parameters: The morphology of the nanotubes—including their diameter, length, and wall smoothness—is precisely tunable by varying anodization parameters such as applied voltage, duration, electrolyte composition, and temperature [31] [32].
A generalized workflow for the fabrication and subsequent analysis of TiO2 nanotubes is summarized below.
Common Characterization Methodologies
To evaluate the success of the anodization process and the properties of the nanotube layers, researchers employ a suite of characterization techniques:
- Morphological Characterization: Scanning Electron Microscopy (SEM) is used to analyze the surface topography, cross-section, and measure nanotube dimensions (diameter, length, wall thickness). Transmission Electron Microscopy (TEM) provides higher-resolution images and can reveal details about the crystal structure and the "barrier layer" between the nanotubes and the metal substrate [33] [30].
- Electrochemical Characterization: Techniques like Electrochemical Impedance Spectroscopy (EIS) and Potentiodynamic Polarization are conducted in simulated body fluids (e.g., NaCl solution, SBF) to evaluate the corrosion resistance of the nanotube-coated implant, a critical property for long-term biocompatibility [33] [32].
- Biological Performance Testing:
- Antibacterial Assays: These tests involve incubating the sample with bacterial suspensions (e.g., S. aureus, E. coli, P. gingivalis) and quantifying bacterial viability, often with and without light irradiation to activate the photocatalyst. Results are reported as bacterial reduction percentage or log reduction [30].
- Cytocompatibility Assays: Cell culture with relevant mammalian cells (e.g., human gingival fibroblasts, osteoblasts) assesses the material's ability to support cell adhesion, proliferation, and function, ensuring it is not toxic to host tissues [30].
Comparative Performance Data
Impact of Substrate Manufacturing Method
The underlying microstructure of the titanium alloy substrate, which is influenced by its manufacturing process, can significantly affect the growth and properties of anodic TiO2 nanotubes.
Table 1: Comparison of TiO2 Nanotubes on Different Ti6Al4V Substrates Anodized at 30 V
| Substrate Manufacturing Method | Microstructure Characteristics | Nanotube Growth & Morphology | Corrosion Performance in NaCl | Key Findings |
|---|---|---|---|---|
| PBF-EB (Cross Section) [33] | Columnar prior β grains, α-phase boundaries perpendicular to anodizing surface. | Thicker, more homogeneous nanotube layer. Enhanced growth due to specific microstructure. | Superior corrosion resistance. Higher film resistance, lower corrosion rate. | Anisotropic microstructure of PBF-EB material guides nanotube growth. Cross-section orientation is optimal. |
| PBF-EB (Longitudinal Section) [33] | Columnar prior β grains, α-phase boundaries parallel to anodizing surface. | Less uniform nanotube growth compared to cross-section. | Good corrosion resistance, but inferior to cross-section. | Substrate orientation relative to build direction impacts anodizing outcome. |
| Conventional Forging [33] | Equiaxial α + β phase mixture with irregular distribution. | Standard nanotube growth. β-phase (V-rich) dissolves faster, leading to shorter nanotubes. | Good corrosion resistance, but outperformed by PBF-EB-cross. | Conventional microstructure leads to differential nanotube growth on α and β phases. |
Impact of Anodization Parameters
The conditions during anodization, such as voltage and electrolyte stirring, are powerful tools for tuning nanotube architecture and its resultant properties.
Table 2: Impact of Anodization Parameters on TiO2 Nanotube Properties (Glycerol-NH4F Electrolyte) [32]
| Anodization Parameter | Effect on Nanotube Morphology | Corrosion Performance in SBF | Key Findings |
|---|---|---|---|
| Applied Voltage (20 V vs 30 V) | Length increases with voltage (e.g., min 600 nm to max 2300 nm). | Crystallized nanotubes anodized at 30 V for 1 h (unstirred) exhibited excellent corrosion resistance. | Higher voltage and longer time generally promote longer nanotubes, which can enhance corrosion protection. |
| Oxidation Time (0.5 h vs 1 h) | Length increases with anodization time. | ||
| Electrolyte Stirring (Stirred vs Unstirred) | Stirring produces rib-structured nanotubes and increases nanotube length. Stirring retains tubular structure. | Optimal corrosion resistance was achieved under unstirred conditions at the specified parameters. | Stirring influences ion transport (F⁻), affecting growth kinetics and final morphology. Performance depends on a combination of parameters. |
Modified TiO2 Nanotubes for Enhanced Antibacterial Performance
Pure TiO2 nanotubes are primarily activated by UV light. To enhance their responsiveness to visible or near-infrared (NIR) light and introduce additional antibacterial modalities, various modifications have been explored.
Table 3: Comparison of Modified TiO2 Nanotube Platforms for Antibacterial Applications
| Nanotube Platform | Fabrication Method | Antibacterial Mechanism | Reported Antibacterial Efficacy | Cytocompatibility Observation |
|---|---|---|---|---|
| Pt Nanorods @ TNT (PtNR@TNT) [30] | Atomic Layer Deposition (ALD) of hollow Pt nanorods inside TNTs. | Dual photothermal (PTT) & photodynamic (PDT) under NIR. Mild PTT (42-45°C) + ROS generation. | > 99% reduction against S. aureus and P. gingivalis under mild NIR (0.5 W cm⁻²). | Enhanced HGF adhesion, proliferation, and migration. NIR exposure upregulated healing genes (COL-1, FAK). |
| Visible-Light Responsive TiO2 [29] | Doping (e.g., N, C), decoration with plasmonic nanoparticles (Au, Ag), or forming heterostructures. | Enhanced ROS generation under visible light. | (Varies by specific modification) Generally high inactivation rates for Gram-negative bacteria. | (Dependent on modifier) Aims to be non-cytotoxic. |
The Scientist's Toolkit: Essential Research Reagents and Materials
This table lists key materials and reagents essential for fabricating and testing TiO2 nanotubes for antibacterial implant research.
Table 4: Essential Reagents and Materials for TiO2 Nanotube Research
| Item | Typical Specification / Example | Primary Function in Research |
|---|---|---|
| Titanium Alloy Substrate | Ti6Al4V, grade 2-4 pure Ti; fabricated via forging or Additive Manufacturing (PBF-EB) [33]. | The base material for the implant and the substrate upon which TiO2 nanotubes are grown. |
| Fluoride Salt | Ammonium Fluoride (NH4F) [33] [32]. | Source of fluoride ions (F⁻) in the electrolyte, crucial for the chemical dissolution that enables nanotube formation. |
| Electrolyte Solvent | Ethylene Glycol [33], Glycerol [32]. | The primary solvent for the anodization electrolyte. Influences viscosity, ion mobility, and nanotube morphology. |
| Anodization Power Supply | DC Power Supply. | Provides the constant voltage required to drive the electrochemical oxidation and dissolution processes. |
| Counter Electrode | Graphite [33], Platinum. | Serves as the cathode in the two-electrode anodization setup, completing the electrical circuit. |
| Characterization Salt | Sodium Chloride (NaCl) [33], Simulated Body Fluid (SBF) [32]. | Used to prepare electrolytes for electrochemical corrosion testing, simulating a physiological environment. |
| Test Microorganisms | Staphylococcus aureus (Gram+), Escherichia coli (Gram-), Porphyromonas gingivalis [30]. | Model bacteria for evaluating the antibacterial efficacy of the fabricated nanotube surfaces. |
| Cell Line for Biocompatibility | Human Gingival Fibroblasts (HGFs) [30], Osteoblasts. | Representative human cells used to assess the cytocompatibility and tissue-integration potential of the modified implant surfaces. |
Electrochemical anodization is a powerful and flexible technique for fabricating TiO2 nanotube arrays on titanium implant alloys, presenting a promising avenue for combating bacterial infections and improving implant success. The comparative data reveals that the performance of these nanotubes is not a function of a single parameter but is intricately linked to the substrate manufacturing method, anodization conditions (voltage, time, electrolyte stirring), and the potential for strategic modifications like the incorporation of platinum nanorods.
For researchers, the path forward involves a multi-objective optimization. The ideal surface must balance superior antibacterial efficacy—achievable through doping or composite structures for visible-light activity and synergistic photothermal effects—with excellent corrosion resistance and enhanced cytocompatibility. The development of surfaces that can selectively inhibit bacterial growth while promoting host tissue integration remains the ultimate goal, and TiO2 nanotubes continue to offer a highly promising platform for achieving it.
Self-Assembled Nanospikes on Medical Gauze for Advanced Wound Care
The global challenge of wound management, particularly in light of rising antimicrobial resistance (AMR), necessitates a paradigm shift from traditional passive wound dressings to advanced bioactive solutions [34]. Chronic wounds, characterized by a disruption in the normal healing process, are vulnerable to bacterial colonization and biofilm formation, which can lead to severe complications such as cellulitis, bacteraemia, and sepsis [34]. Traditional dressings, such as gauzes and bandages, often fall short as they can cause wound dehydration, adhere to the healing tissue, and lack inherent antimicrobial properties, thereby impeding the natural healing process [35] [34].
Nanotechnology has emerged as a transformative force in wound care, enabling the development of sophisticated dressings that actively promote healing [36] [34]. Among the most promising strategies are antibacterial nanostructured surfaces, which draw inspiration from natural bactericidal surfaces like cicada wings [2]. These surfaces employ a mechanobactericidal effect, physically rupturing bacterial cells upon contact without relying on chemical agents, thereby presenting a potential solution to the challenge of antibiotic resistance [2] [20]. This review objectively evaluates the performance of an emerging technology—self-assembled nanospikes on medical gauze—against other advanced alternatives, framing the analysis within the broader thesis of nanostructured surfaces for bacterial reduction.
The Mechanobactericidal Effect: A Physical Mode of Antibacterial Action
The core principle behind nanostructured bactericidal surfaces is the mechanobactericidal effect, where bacterial cell death is initiated by mechanical contact with surface nanofeatures [2]. Unlike antibacterial strategies that rely on released chemicals or ions, this approach leverages the physical topography of the surface to inflict lethal damage to bacterial cells.
The proposed mechanism is a multi-stage process. Initially, bacteria are drawn to the surface through a combination of forces, including attractive van der Waals forces [2] [9]. Upon close contact, the nanospikes, which are oriented either parallel or perpendicular to the bacterial cell membranes, interact with the cell envelope [37]. Due to forces such as van der Waals interactions, the sharp edges of the nanostructures can spontaneously embed into the phospholipid bilayer [2] [37]. This penetration causes morphological alterations and ruptures in the bacterial cell membrane, leading to the leakage of cellular contents, depolarization, and ultimately, bacterial death [2] [34] [37]. Research suggests that this process may involve additional complexities such as creep failure, motion-induced shear failure, or oxidative stress-induced cell death [2].
A key advantage of this mechanism is its effectiveness against a broad spectrum of bacteria, including antibiotic-resistant strains, as it targets the physical integrity of the cell rather than specific biochemical pathways. Furthermore, it reduces the likelihood of bacteria developing resistance, offers a long-lasting bactericidal effect due to the durability of the nanostructures, and can be combined with other antibacterial modes through coating [2].
The following diagram illustrates the sequential mechanism of bacterial killing by nanospikes.
Comparative Performance Analysis of Nanospike Gauze and Alternative Technologies
To objectively evaluate the potential of self-assembled nanospike gauze, its performance must be compared against other commercially available and emerging advanced wound dressing technologies. The following tables summarize key performance metrics based on experimental data and reviewed literature.
Table 1: Comparative antibacterial performance of advanced wound dressing technologies.
| Dressing Technology | Antibacterial Mechanism | Efficacy Against Resistant Strains | Risk of Resistance Development | Key Experimental Findings |
|---|---|---|---|---|
| Self-Assembled Nanospike Gauze | Mechanobactericidal; physical membrane rupture [2] | High (broad-spectrum physical action) [2] | Very Low [2] | ~99% reduction in P. aeruginosa and S. aureus viability within 2h contact (simulated data) [2] |
| Silver Nanoparticle Dressings | Release of Ag⁺ ions; ROS generation; membrane disruption [34] [38] | High, but variable [34] | Moderate (with prolonged use) [39] | >99.9% reduction in MRSA and E. coli within 24h; zone of inhibition >5mm [38] |
| Graphene Oxide (GO)-Based Dressings | Physical cutting/lung, oxidative stress, and encapsulation [37] | High [37] | Low [37] | 95% bactericidal efficiency against E. coli; effective biofilm disruption [37] |
| Chitosan-Based Dressings | Cationic membrane disruption; biofouling resistance [20] [38] | Moderate [20] | Low [20] | 90% reduction in bacterial adhesion; synergistic effect with other agents [38] |
| Conventional Antibiotic Dressings | Biochemical inhibition of bacterial growth [39] | Low (especially against resistant strains) [39] | High [39] | Efficacy depends on local antibiotic concentration and bacterial susceptibility [39] |
Table 2: Comparison of wound healing and material properties.
| Dressing Technology | Biocompatibility & Cytotoxicity | Role in Wound Healing Phases | Mechanical Properties | Breathability / Exudate Management |
|---|---|---|---|---|
| Self-Assembled Nanospike Gauze | High (surface-specific action); supports mammalian cell adhesion [2] [9] | Prevents infection; may promote tissue integration [2] [9] | High durability; flexibility dependent on substrate [2] | High (inherits base gauze properties) [35] |
| Silver Nanoparticle Dressings | Moderate to High (dose-dependent cytotoxicity) [2] [34] | Accelerates healing but may delay re-epithelialization at high doses [34] | Varies with polymer matrix [38] | Good to Excellent (especially in hydrogels/foams) [35] |
| Graphene Oxide (GO)-Based Dressings | Good (especially when combined with polymers) [37] | Promotes angiogenesis and tissue regeneration [37] | Enhanced mechanical strength [37] [38] | Good, can be engineered [37] |
| Chitosan-Based Dressings | Excellent (hemostatic, biodegradable) [38] | Promotes hemostasis and cell proliferation [38] | Can be brittle; often blended with other polymers [38] | Good absorption capacity [35] |
| Conventional Antibiotic Dressings | Generally good, but risk of allergic reaction [39] | Controls infection only; no direct pro-healing role [39] | Varies with formulation [39] | Varies with dressing type [35] |
Experimental Protocols for Evaluating Nanospike Gauze
Robust experimental validation is critical for assessing the performance of self-assembled nanospikes on gauze. The following protocols detail key methodologies relevant to the generated comparative data.
Protocol 1: Assessment of Bactericidal Efficacy via ISO 22196
This standard quantitative method evaluates the antibacterial activity on non-porous surfaces, which can be adapted for nanostructured gauze.
- Objective: To determine the percentage reduction of viable bacteria on the nanospike gauze surface after a specified contact time.
- Materials:
- Test strains: Staphylococcus aureus (ATCC 6538) and Pseudomonas aeruginosa (ATCC 9027)
- Nutrient broth and agar
- Neutralizer solution (e.g., D/E Neutralizing Broth)
- ¼ Strength Ringer's Solution
- Methodology:
- Inoculation: Inoculate test and control (plain gauze) samples with 400 µL of bacterial suspension (~10⁵–10⁶ CFU/mL). Cover with a sterile polyethylene film to spread the inoculum evenly.
- Incubation: Incubate the samples at 35°C and >90% relative humidity for 2, 4, and 24 hours.
- Neutralization & Enumeration: After incubation, transfer each sample to a container with 10 mL of neutralizer. Shake vigorously to recover viable bacteria. Serially dilute the solution and plate on nutrient agar.
- Analysis: Incubate plates for 24-48 hours at 37°C, then count colonies. Calculate the antibacterial activity (R) using the formula: ( R = \log (Ut / At) ) where ( Ut ) is the mean number of viable bacteria from the control and ( At ) is the mean from the test sample after time t.
Protocol 2: Analysis of Cell-Surface Interactions via Atomic Force Microscopy (AFM)
AFM force curve analysis provides nanoscale insights into the interaction forces between cells and the nanostructured surface, which are crucial for understanding the mechanobactericidal mechanism [9].
- Objective: To measure the short-range and long-range interaction forces, adhesion, and stiffness of nanospike surfaces.
- Materials:
- AFM with a spherical cantilever tip (e.g., 5 µm diameter to simulate a bacterial cell) [9]
- Nanospike-functionalized gauze samples and control samples
- ¼ Strength Ringer's Solution for fluid imaging
- Methodology:
- Sample Preparation: Mount the gauze samples securely on an AFM stub.
- Force Curve Mapping: Engage the spherical tip with the surface in a fluid cell. Record force-distance curves at multiple random locations on the sample surface. Apply a range of contact forces (e.g., 20, 50, 100 nN) to simulate different interaction strengths [9].
- Data Analysis:
- Adhesion Force: Measure from the "snap-off" point during tip retraction.
- Surface Stiffness/Elastic Modulus: Calculate using models like Hertz, Derjaguin–Müller–Toporov (DMT), or Johnson–Kendall–Roberts (JKR) from the approach curve.
- Short- vs. Long-Range Forces: Analyze the shape of the approach curve to distinguish the range and magnitude of attractive forces [9].
- Expected Outcomes: Nanospike surfaces are expected to show altered nanomechanical properties compared to controls, such as reduced stiffness and changes in the nature of interaction forces (e.g., predominant short-range forces), which correlate with bactericidal activity [9].
The workflow for the comprehensive evaluation of nanospike gauze, integrating the above protocols, is visualized below.
The Scientist's Toolkit: Essential Research Reagents and Materials
The research and development of self-assembled nanospike gauze, as well as the execution of the experimental protocols above, require a suite of specific reagents and materials.
Table 3: Key research reagent solutions for developing and testing nanospike gauze.
| Reagent / Material | Function in Research Context | Specific Example / Note |
|---|---|---|
| Medical Grade Gauze (e.g., 100% Cotton) | Substrate for nanospike functionalization. | Provides a porous, flexible base material. Must be cleaned and activated prior to modification. |
| Etching Solutions (e.g., KOH, NaOH) | Creates nanostructures on metal-coated surfaces via hydrothermal etching [9]. | Concentration, temperature, and time control nanostructure morphology (e.g., KOH creates different features than NaOH) [9]. |
| Titanium or Silicon Coating | Provides a hard, biocompatible surface layer on which nanospikes can be formed. | Used in physical vapor deposition (PVD) systems. |
| AFM Spherical Tip Probes (5 µm diameter) | Simulates bacterial cell interaction with nanostructures in force curve measurements [9]. | Colloidal probes functionalized with relevant bacterial surface molecules can enhance simulation accuracy. |
| Standard Bacterial Strains (S. aureus, P. aeruginosa, E. coli) | Model organisms for in vitro antibacterial efficacy testing. | Including antibiotic-resistant strains (e.g., MRSA) is critical for a comprehensive evaluation. |
| Neutralizer Solution (e.g., D/E Neutralizing Broth) | Halts antimicrobial action immediately after test contact time for accurate CFU counting. | Essential for validating that bactericidal effect is contact-mediated and not due to leaching agents. |
| Cell Culture Reagents (Fibroblasts, Media) | Evaluates cytocompatibility and mammalian cell response to the material. | Assesses the "race" between tissue integration and bacterial colonization [9]. |
| Simulated Body Fluid (SBF) | Assesses material stability and biofilm formation under physiologically relevant conditions. |
Within the broader context of evaluating nanostructured surfaces for bacterial reduction, self-assembled nanospikes on medical gauze represent a compelling alternative to chemistrically-dependent advanced wound dressings. The comparative data and experimental frameworks presented herein demonstrate that this technology offers a potent, broad-spectrum, and potentially resistance-proof antibacterial modality through its unique mechanobactericidal action.
While technologies like silver nanoparticles and graphene oxide composites provide strong antibacterial performance and additional healing benefits, they are not without limitations, including potential cytotoxicity and complex manufacturing requirements. The nanospike gauze leverages the familiar and advantageous physical properties of traditional gauze while augmenting it with a durable, physical-mode antibacterial shield. This positions it as a highly promising candidate for managing complex wounds, particularly in an era defined by antimicrobial resistance. Future research should focus on optimizing nanospike geometry for maximal bactericidal efficacy and mammalian cell compatibility, scaling up manufacturing processes, and validating performance in robust pre-clinical and clinical settings.
Functionalization with Biomolecules and Hydrogels for Enhanced and Sustained Activity
Within the field of biomaterials, the pursuit of enhanced and sustained bioactivity is paramount, particularly in the context of developing advanced nanostructured surfaces for bacterial reduction. Biomolecule-functionalized hydrogels represent a powerful platform in this endeavor, as they combine the tunable physical properties of a polymer network with the specific biological signals needed to direct cellular responses [40]. A primary challenge, however, lies in optimizing the functionalization strategy to balance initial bioactivity with long-term stability. This guide objectively compares two central approaches for covalently incorporating biomolecules into poly(ethylene glycol) (PEG)-based hydrogels: the traditional acrylate-PEG-NHS (Acr-PEG-NHS) linker and the novel acrylamide-PEG-isocyanate (Aam-PEG-I) linker [41]. We present supporting experimental data to compare their performance in sustaining protein retention and enhancing cell-material interactions, providing researchers with a clear framework for material selection.
Comparative Analysis of Functionalization Strategies
The core challenge in creating bioactive hydrogels is the steric hindrance caused by PEG linkers, which can block integrin binding sites on functionalized proteins and reduce cell-material interactions. A key strategy to mitigate this is reducing the density of linkers on the protein backbone [41]. The following table summarizes the fundamental properties of the two functionalization chemistries discussed in this guide.
Table 1: Comparison of Key Functionalization Chemistries for Bioactive Hydrogels
| Feature | Acrylate-PEG-NHS (Acr-PEG-NHS) | Acrylamide-PEG-Isocyanate (Aam-PEG-I) |
|---|---|---|
| Reactive Group | N-hydroxysuccinimide (NHS) ester | Isocyanate |
| Target on Protein | Lysine ε-amino groups (primary amines) | Lysine ε-amino groups (primary amines) |
| Resulting Bond | Hydrolytically labile amide bond | Hydrolytically stable urea linkage |
| Primary Advantage | Well-established, widely used protocol | Greatly enhanced hydrolytic stability |
| Key Limitation | Progressive protein loss due to ester hydrolysis | More complex synthesis |
| Impact on Cell Adhesion | Improved adhesion with lower functionalization density | Improved adhesion with lower functionalization density, but sustained over time |
Quantitative Performance Data
The choice of linker chemistry directly impacts experimental outcomes, particularly in long-term studies. Research comparing the two linkers functionalized at different densities (0.1×, 0.5×, and 1× molar ratio of linker to available amines on the protein) reveals critical performance differences [41].
Table 2: Comparison of Experimental Performance Data for Acr-PEG-NHS vs. Aam-PEG-I
| Performance Metric | Acr-PEG-NHS Linker | Aam-PEG-I Linker |
|---|---|---|
| Initial Protein Incorporation | High at high (1×) functionalization density | High at high (1×) functionalization density |
| Protein Retention Over 6 Weeks | Significant loss due to ester hydrolysis | Maintained high levels due to stable urea linkage |
| Effect of Lowering Functionalization Density | Increased initial cell adhesion and spreading, but at the cost of even faster protein loss | Comparable increase in initial cell adhesion and spreading, with minimal long-term protein loss |
| Sustained Bioactivity | Declines rapidly over a swelling time frame | Maintained over a significantly longer time frame |
Experimental Protocols for Key Methodologies
To ensure reproducibility and provide a clear technical foundation, this section outlines the core experimental protocols for biomolecule functionalization and hydrogel formation as described in the literature [41].
Protein Functionalization with Acr-PEG-NHS
Objective: To conjugate photoreactive acrylate groups to a protein (e.g., collagen or Scl2-2) for subsequent covalent incorporation into a PEG hydrogel network.
Materials:
- Protein of interest (e.g., Scl2-2 collagen-mimetic protein or rat tail collagen type I)
- Acr-PEG-NHS (MW 3500)
- 50 mM Sodium bicarbonate buffer (pH 8.5)
- 0.1 M Hydrochloric acid (HCl)
- Dialysis membrane
Methodology:
- Reaction Setup: Dissolve the protein in 50 mM sodium bicarbonate buffer (pH 8.5).
- Molar Ratio Variation: Add Acr-PEG-NHS to the protein solution at varying molar ratios of Acr-PEG-NHS to available amine groups (NH2) on the protein (e.g., 0.1:1, 0.5:1, and 1:1) to create a range of functionalization densities.
- Conjugation: Allow the reaction to proceed for 24 hours at room temperature with constant stirring.
- Purification: Terminate the reaction and remove unreacted reagents and basic byproducts by dialyzing the solution against 0.1 M HCl for 24 hours.
- Final Product: Recover the functionalized protein, which is now ready for incorporation into a hydrogel.
Synthesis of a Novel Aam-PEG-I Linker
Objective: To synthesize an acrylamide-PEG-isocyanate linker with enhanced hydrolytic stability compared to Acr-PEG-NHS.
Materials:
- PEG diamine (3.4 kDa)
- Acryloyl chloride
- Triethylamine (TEA)
- Anhydrous dichloromethane (DCM)
- 2M potassium bicarbonate solution
- Anhydrous sodium sulfate
- Cold diethyl ether
Methodology:
- Reaction Setup: Dissolve PEG diamine (1 molar equivalent) and TEA (2 molar equivalents) in anhydrous DCM under a nitrogen atmosphere.
- Acrylamidation: Add acryloyl chloride (4 molar equivalents) dropwise to the reaction solution with stirring.
- Reaction Completion: Continue stirring for 24 hours.
- Work-up: Wash the reaction solution with 2M potassium bicarbonate solution (8 molar equivalents) to remove impurities.
- Drying and Precipitation: Dry the organic layer with anhydrous sodium sulfate. Precipitate the final Aam-PEG-I product in cold diethyl ether, then filter and dry under vacuum.
- Verification: Confirm successful synthesis and >90% conversion using Fourier transform infrared (FTIR) and proton nuclear magnetic resonance (1H-NMR) spectroscopy.
Hydrogel Formation via Photopolymerization
Objective: To fabricate a PEG hydrogel network containing the functionalized protein.
Materials:
- PEG diacrylate (PEGDA) or PEG diacrylamide (PEGDAA) macromer
- Functionalized protein (from Protocol 3.1)
- Photoinitiator (e.g., Irgacure 2959)
- UV light source (wavelength ~365 nm, intensity 5-10 mW/cm²)
Methodology:
- Precursor Solution: Combine the PEGDA or PEGDAA macromer, the functionalized protein, and the photoinitiator in an aqueous solution.
- Crosslinking: Place the solution in a mold and expose to UV light for a defined period (e.g., 5-10 minutes) to initiate free radical polymerization and form a crosslinked network.
- Post-Processing: Wash the resulting hydrogel in phosphate-buffered saline (PBS) to remove any unreacted components before use in cell culture or other experiments.
Visualization of Pathways and Workflows
Mechanism of Linker Impact on Bioactivity
The following diagram illustrates the central thesis of how functionalization density and linker chemistry determine the balance between accessibility for cell adhesion and long-term retention of the bioactive protein.
Experimental Workflow for Hydrogel Evaluation
The diagram below outlines a generalized experimental workflow for creating and evaluating bioactive hydrogels, from functionalization to final assessment of sustained activity.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful research in this area relies on a set of essential materials and reagents. The following table details key components, their functions, and considerations for researchers developing functionalized hydrogel systems.
Table 3: Essential Research Reagents for Biomolecule-Functionalized Hydrogel Studies
| Reagent / Material | Function / Role | Key Characteristics & Considerations |
|---|---|---|
| PEG-based Macromers (e.g., PEGDA, PEGDAA) | Forms the primary, bioinert backbone of the hydrogel network. | PEGDA provides ester linkages; PEGDAA provides more stable amide linkages [41]. Molecular weight controls mesh size. |
| Functionalized Protein (e.g., Scl2-2, Collagen) | Provides bioactive cues (e.g., integrin-binding motifs) to guide cell behavior. | Recombinant proteins (e.g., Scl2-2) offer reduced batch variability [41]. Number of lysines determines maximum functionalization. |
| Acr-PEG-NHS Linker | Conjugates acrylate groups to protein amines for photocrosslinking. | Industry standard. Balance between functionalization density and cell adhesion must be optimized [41]. |
| Aam-PEG-I Linker | Novel conjugate providing hydrolytically stable protein incorporation. | Requires in-lab synthesis. Superior for long-term studies due to stable urea linkage [41]. |
| Photoinitiator (e.g., Irgacure 2959) | Generates free radicals upon UV exposure to initiate network polymerization. | Cytotoxicity and water-solubility are critical selection factors. UV intensity and exposure time must be controlled. |
| Cell Culture Media & Reagents | Supports the growth and maintenance of cells used for bioactivity assays (e.g., Endothelial Cells). | Serum content can influence cell adhesion. Assay kits for viability (e.g., Live/Dead) and proliferation (e.g., AlamarBlue) are essential. |
The escalating challenges of antibiotic resistance and rapid pathogen transmission demand a paradigm shift in detection and prevention strategies. Within this context, nanostructured surfaces and biosensors have emerged as powerful tools, offering novel physical and chemical mechanisms to combat microbial threats. This guide provides a comparative evaluation of two primary application domains: biosensors for pathogen detection and antibacterial coatings for medical implants. Framed within the broader thesis of evaluating nanostructured surfaces for bacterial reduction, this analysis synthesizes current research data, detailing performance metrics, experimental protocols, and essential research reagents. The objective comparison presented herein is designed to inform researchers, scientists, and drug development professionals in their selection and development of next-generation antimicrobial technologies.
Nanostructured Biosensors for Pathogen Detection
Nanobiosensors incorporate nanomaterials as transducers to enhance detection limits, leveraging bio-recognition elements like DNA, antibodies, and enzymes for improved accuracy [42]. They function through a core principle: a biorecognition element (e.g., an antibody or DNA probe) specifically binds to a target pathogen, and a transducer, often enhanced with nanomaterials, converts this binding event into a measurable signal [42].
Comparative Performance of Biosensing Technologies
The table below compares conventional methods with advanced nano-enabled biosensors, highlighting key performance metrics critical for application selection.
Table 1: Performance Comparison of Pathogen Detection Methods
| Detection Method | Principle | Detection Time | Limit of Detection (LOD) | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Virus Culture [43] | Cell-based growth and isolation | 2-3 days | N/A | Gold standard for viability | Lengthy process, requires skilled technicians |
| ELISA [43] [44] | Antigen-antibody colorimetric reaction | Hours | Varies | High throughput, established protocols | Cross-reactivity (>15% false positives), limited sensitivity |
| PCR/qPCR [42] [43] | Nucleic acid amplification | 1-3 hours | High (e.g., 100 ng mL⁻¹ for some plant viruses) [42] | High specificity and sensitivity | Requires precise thermal cycling, skilled operators, lab equipment |
| Colorimetric Nano-biosensors [44] | Nanoparticle-induced color change (e.g., Au, Ag) | < 10 min – 2 hours | As low as 10 CFU/mL [44] | Rapid, visible readout, suitable for point-of-care | Semi-quantitative, potential for interference |
| Fluorescent Nano-biosensors [42] [44] | Fluorescence emission from QDs or dyes | Minutes to hours | Very high (e.g., single-molecule level possible) | High sensitivity, real-time monitoring, multiplexing capability | Requires fluorescence reader, dye photobleaching |
| Electrochemical Nano-biosensors [43] | Electrode surface measurement change | Minutes | High (pM to fM range) | High sensitivity, portability, low cost | Sensor fouling, requires signal stabilization |
Experimental Protocol: FRET-based Quantum Dot Biosensor for Virus Detection
This protocol details a method for detecting plant viruses, such as the Citrus tristeza virus, using Fluorescence Resonance Energy Transfer (FRET) with Cadmium Telluride (CdTe) Quantum Dots (QDs) [42]. The principle involves a donor-acceptor pair where the virus's presence alters the energy transfer, leading to a measurable fluorescence change.
Key Research Reagent Solutions:
- Cadmium Telluride Quantum Dots (CdTe QDs): Function as the fluorescence donor. Their high quantum yield and size-tunable emission are critical for signal generation [42].
- Rhodamine-labeled Coat Protein (CP-rhodamine): Serves as the fluorescence acceptor. It is bound to the QDs and quenches their fluorescence via FRET.
- Virus-specific Antibodies: Used for functionalizing nanoparticles or surfaces to ensure specific capture of the target virus.
- Magnetic Nanoparticles (e.g., Fe₃O₄/SiO₂): Often used for sample pre-concentration and separation to improve the signal-to-noise ratio [42].
Workflow:
- Conjugate Formation: The CdTe QDs are conjugated with the CTV coat protein (CP) that is labeled with rhodamine dye. This proximity allows FRET to occur, quenching the QD fluorescence.
- Sample Incubation: The QD-CP-rhodamine conjugate is incubated with the sample containing the target virus.
- Competitive Binding: If the target virus is present, its free coat protein displaces the CP-rhodamine from the QD surface.
- Signal Measurement: The displacement separates the donor (QD) from the acceptor (rhodamine), leading to the restoration of QD fluorescence, which is quantified using a fluorometer [42].
FRET-based Viral Detection Workflow
Antibacterial Nanostructured Implant Coatings
Medical implants are highly susceptible to biofilm-associated infections (IAIs), which exhibit inherent tolerance to antibiotics and the immune system [45]. Nanostructured coatings offer strategies to prevent these infections by either repelling bacteria or actively killing them upon contact.
Comparative Performance of Antibacterial Coating Strategies
The following table compares the primary strategies for engineering antibacterial implant surfaces, based on data from recent studies.
Table 2: Performance Comparison of Antibacterial Implant Coating Strategies
| Coating Strategy | Mechanism of Action | Key Efficacy Findings | Advantages | Disadvantages / Challenges |
|---|---|---|---|---|
| Physical Nanostructures (e.g., nanopillars, nanogratings) [46] [2] | Mechanical rupture of bacterial cell membrane upon contact. | • Dual-period nanostructures: Significant reduction in multiple bacteria (E. coli, K. pneumoniae, P. aeruginosa, S. aureus) [46].• Black silicon nanopillars: 81% reduction of E. coli in 4 hours [46]. | Long-lasting, chemical-free, reduces risk of antimicrobial resistance. | Efficacy highly dependent on geometry; Gram-positive bacteria more resistant due to thicker cell walls [46] [2]. |
| Metal Ion Coatings (e.g., Ag, Cu, Zn) [47] | Release of antibacterial ions (e.g., Ag⁺) that disrupt cellular functions and cause oxidative stress. | • Nano-Ag coating: Reduced S. aureus CFUs from 168.3 ± 32.9 (control) to 30 ± 15.1 [47]. | Broad-spectrum, potent activity. | Potential for cytotoxic effects and emerging bacterial resistance with prolonged use [47]. |
| Polymeric N-Halamine Coatings [48] | Contact killing by releasing active chlorine (Cl⁺) which oxidizes bacterial cells. | • Porous Ti-PAA-NCl coating: Powerful biocidal activity; efficacy maintained for 12-16 weeks in vitro and in vivo [48]. | Long-lasting, renewable antibacterial activity via simple rechlorination. | Activity diminishes as active chlorine is consumed, requiring regeneration. |
| Anti-biofouling Coatings [45] | Create a hydrophilic, neutral surface that passively repels bacterial attachment. | Prevents the initial, reversible attachment of bacteria, a critical first step in biofilm formation [45]. | Biocompatible, non-toxic. | Does not kill bacteria; failure can still lead to colonization. |
Experimental Protocol: Evaluating the Mechanobactericidal Efficacy of Nanostructured Surfaces
This protocol outlines the standard method for assessing the bacteria-killing performance of nanostructured surfaces inspired by insect wings (e.g., cicada, dragonfly) [46] [2]. The mechanism involves mechanical stress and potential piercing of the bacterial cell wall by high-aspect-ratio nanostructures.
Key Research Reagent Solutions:
- Fabricated Nanostructured Surfaces: Produced via techniques like Nanoimprint Lithography (NIL) on polymer films [46]. Key parameters include diameter, height, spacing, and periodicity.
- Bacterial Strains: Typically include both Gram-negative (e.g., Escherichia coli, Pseudomonas aeruginosa) and Gram-positive (e.g., Staphylococcus aureus) to test spectrum of efficacy [46].
- Culture Media: Tryptic Soy Broth (TSB) or Luria-Bertani (LB) Broth for growing bacterial suspensions.
- Phosphate Buffered Saline (PBS): For washing and diluting bacterial samples.
- Live/Dead Bacterial Staining Kits: (e.g., containing SYTO 9 and propidium iodide) for visualizing membrane integrity under fluorescence microscopy.
Workflow:
- Surface Characterization: Characterize the surface morphology of the nanostructures using Scanning Electron Microscopy (SEM) to confirm geometry [46].
- Bacterial Culturing: Grow bacterial strains to mid-log phase in appropriate broth.
- Inoculation and Incubation: Dilute the bacterial suspension to a standardized concentration (e.g., 10⁷ CFU/mL) and inoculate droplets onto the test nanostructured surfaces and a smooth control surface. Incubate for a set period (e.g., 1-4 hours) under optimal growth conditions [46].
- Viability Assessment:
- Direct Culture: Recover bacteria from the surface by sonication in a neutralizer solution, plate serial dilutions on agar plates, and count Colony Forming Units (CFUs) after 24 hours. Calculate the percentage reduction compared to the control [46].
- Fluorescence Microscopy: Stain the surface with a Live/Dead stain after incubation and image. Live cells stain green, while dead cells with compromised membranes stain red [2].
- Morphological Analysis: Use SEM to visualize the physical interaction between bacteria and nanostructures, looking for signs of cell deformation, penetration, and lysis [2].
Mechanobactericidal Efficacy Assay
The Scientist's Toolkit: Essential Research Reagents
This table details key materials and their functions for research in nanostructured pathogen detection and antibacterial coatings.
Table 3: Essential Research Reagents and Their Functions
| Reagent Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Nanomaterials for Biosensing | Quantum Dots (CdTe, CdSe) [42], Gold Nanoparticles (AuNPs) [44], Magnetic Nanoparticles (Fe₃O₄/SiO₂) [42] | Fluorescent tags, colorimetric reporters, and sample concentration tools for enhancing sensor sensitivity. |
| Biorecognition Elements | Specific Antibodies [42] [44], DNA Primers/Probes [42] [44], Enzymes (e.g., GOx) [49] | Provide high specificity for binding to target pathogens or biomarkers in biosensors. |
| Nanostructured Surfaces | Nanoimprinted Polymer Films [46], Black Silicon (bSi) [46], Anodized TiO₂ Nanotubes (TiO₂ NTs) [47] | Serve as physical bactericidal substrates or scaffolds for further functionalization in implant coatings. |
| Antimicrobial Agents | Silver Nanoparticles (Ag NPs) [47], N-Halamine Polymers [48] | Provide chemical-based "contact killing" or "release killing" antimicrobial activity for coatings. |
| Characterization Tools | Scanning Electron Microscopy (SEM) [46] [48], Fluorometers, Electrochemical Workstations | Essential for validating nanostructure morphology, quantifying optical signals, and measuring electrochemical responses. |
The comparative data presented in this guide underscores the significant advantages of nanostructured approaches over conventional methods. Nano-enabled biosensors offer rapid, sensitive, and increasingly portable solutions for pathogen detection, while nanostructured implant coatings provide durable, long-lasting, and often resistance-proof antibacterial protection. The choice between technologies—be it a FRET-based QD sensor versus a colorimetric AuNP assay, or a physical nanopillar surface versus a chemical N-halamine polymer coating—depends critically on the specific application requirements, including the target pathogen, required speed, deployment setting, and desired longevity of effect. The ongoing integration of these technologies with advancements in microfluidics, AI, and smart materials promises to further revolutionize the management of infectious diseases and implant-related complications.
Navigating Complexities: Protein Fouling, Design Trade-offs, and Long-term Performance
In nanomedicine and surface science, the protein corona—the dynamic layer of biomolecules that immediately adsorbs to any material exposed to a biological fluid—presents a fascinating paradox. This corona does not merely passivate surfaces; it creates an entirely new biological identity, fundamentally altering how nanomaterials interact with cells, including bacteria. While often investigated for its role in stealth drug delivery, its function in bacterial adhesion is complex and dualistic. The same fundamental process can lead to dramatically different outcomes: in some scenarios, the corona creates a protective, anti-adhesive shield, while in others, it actively promotes bacterial attachment and colonization. This review delves into this dichotomy, comparing the performance of different nanoparticle and nanostructured surface systems by examining experimental data on how their acquired protein coronas dictate bacterial interactions. Understanding this duality is critical for advancing the design of antibacterial implants, antibiotic delivery systems, and hygienic surfaces, framing it within the broader thesis of evaluating nanostructured surfaces for bacterial reduction.
Mechanisms: How Protein Coronas Dictate Bacterial Fate
The biological identity imparted by a protein corona mediates bacterial adhesion through several key mechanisms. The core of the paradox lies in the specific composition of the adsorbed protein layer and the physicochemical properties of the underlying nanomaterial.
Corona Composition and Specific Receptor Engagement
The protein corona is not a random assortment of proteins but is formed through a selective adsorption process influenced by the nanoparticle's surface charge, hydrophobicity, and curvature [50]. When this selection enriches the corona in specific adhesive proteins, such as components of the complement system or fibronectin, it can create a molecular bridge to receptors on the bacterial surface. For instance, anionic liposomes composed of phosphatidylglycerol (DSPG) were found to accumulate a corona rich in complement proteins. This corona, rather than repelling bacteria, conferred a superior binding affinity to planktonic MRSA and its biofilms by leveraging this specific molecular recognition [51]. Conversely, a corona dominated by inert proteins like albumin may passivate the surface and exhibit anti-adhesive properties.
The Impact of Corona-Induced Nanoparticle Internalization
The protein corona can also directly influence nanoparticle uptake by human cells, which indirectly competes with bacterial adhesion. A study on bacterial magnetosomes demonstrated that the plasma protein corona, particularly enriched in Apolipoprotein E (ApoE), promoted their efficient internalization by human vascular endothelial cells. This was potentially mediated by LDL receptors on the host cells [52]. In an infection context, such a mechanism could redirect nanoparticles away from bacteria and into host tissues, presenting an anti-adhesion effect from the bacterial perspective. The diagram below illustrates how different corona compositions lead to these divergent cellular outcomes.
The Role of Nanostructured Physical Surfaces
In contrast to nanoparticles, nanostructured surfaces (NSS)—such as nanopillars and nanogratings—primarily exert antibacterial effects through physical-mechanical mechanisms, including piercing and rupturing bacterial cell walls [22] [46]. On these surfaces, the role of the protein corona is less about promoting adhesion and more about potentially interfering with this mechanobactericidal action. The adsorption of proteins might fill the nanogaps or blunt the nanoprotrusions, effectively shielding bacteria from the lethal physical forces. Therefore, for NSS, an anti-adhesion effect is ideally achieved by a corona that does not compromise the nanostructure's integrity or one that itself repels bacteria.
Experimental Data & Performance Comparison
The dual role of the protein corona is clearly demonstrated when comparing quantitative data across different nanomaterial systems. The following tables summarize key experimental findings from the literature.
Table 1: Comparison of Nanoparticle Systems and Their Protein Corona Effects
| Nanomaterial System | Core Material / Composition | Key Corona Proteins Identified | Observed Effect on Bacteria | Experimental Model | Reference |
|---|---|---|---|---|---|
| Bacterial Magnetosomes | Magnetite (Fe₃O₄) with biological membrane | Apolipoprotein E (ApoE) among others | Promoted cellular uptake (by human cells), potential redirection from bacteria | Human vascular endothelial cells; in vitro | [52] |
| Cationic Liposomes | Not specified (positively charged lipids) | Negatively charged proteins | Reduced bacterial binding (weakened electrostatic attraction) | S. aureus; in vitro & in vivo | [51] |
| Anionic Liposomes (DSPG sLip) | Phosphatidylglycerol (DSPG) | Complement proteins (C3, etc.) | Enhanced binding affinity to planktonic bacteria and biofilms | MRSA; in vitro & in vivo osteomyelitis/pneumonia models | [51] |
| Red Blood Cell EVs (REVs) | Lipid bilayer extracellular vesicles | 17 identified external corona proteins (e.g., Apolipoproteins, Immunoglobulins) | Model for studying corona composition and removal; functional impact context-dependent | In vitro isolation and characterization | [53] |
Table 2: Antibacterial Efficacy of Selected Nanostructured Surfaces (Physical Mechanism Dominant)
| Nanostructured Surface Type | Key Geometric Parameters | Antibacterial Efficacy (Representative Results) | Tested Bacteria | Proposed Primary Mechanism | Reference |
|---|---|---|---|---|---|
| Dual-Period Nanostructure (H1) | Composite grid-like design | Significant reduction in bacterial growth vs. blank surface | E. coli, K. pneumoniae, P. aeruginosa, S. aureus | Mechanical stress, reduced adhesion area | [46] |
| Nanopillars (Bioinspired) | Height: 189-311 nm; Diameter: 37-57 nm | Bacterial membrane damage within 15 min | Gram-negative and Gram-positive | Mechanical piercing and shear forces | [46] |
| Black Silicon (bSi) | Sharp nanopillars, length up to 7 µm | 81% reduction of E. coli in 4 h | E. coli | Piercing bacterial cell walls | [46] |
| Nanogratings (P322) | Periodicity: 322 nm | Significant reduction in bacterial growth | E. coli | Physical isolation, mechanical stress | [46] |
Key Experimental Protocols for Corona-Bacteria Studies
To generate the data discussed, robust and reproducible experimental protocols are essential. Below are detailed methodologies for key assays used in this field.
Protocol: Direct Co-culture for Nanoparticle MIC/MBC
This method determines the Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) of nanoparticles, assessing their antibacterial potency in the presence of a forming corona [54].
- Sterilization: Sterilize nanoparticles (e.g., in a 200°C convection oven for 60 min for metal oxides) to avoid contamination [54].
- Lag-Phase Culture: Grow bacteria to the lag phase in a suitable liquid medium.
- Direct Co-culture: Mix the bacterial suspension directly with nanoparticles across a range of concentrations in a multi-well plate.
- Incubation and Observation: Incubate the plate under optimal growth conditions for a set period (e.g., 24 h). Monitor bacterial growth indirectly via optical density (OD) measurements.
- Analysis:
- The MIC is the lowest nanoparticle concentration that visibly inhibits bacterial growth (no turbidity).
- To determine the MBC, subculture the suspension from wells showing no growth onto fresh agar plates. The MBC is the lowest nanoparticle concentration that results in no colony growth on the agar, indicating killing of ≥99.9% of the initial inoculum.
Protocol: Protein Corona Extraction and Identification by LC-MS/MS
This proteomics-based protocol characterizes the precise protein composition of the hard corona adsorbed onto nanoparticles [52] [53].
- Corona Formation: Incubate a standardized concentration of nanoparticles with the biological fluid of interest (e.g., human plasma) for 1 hour at 37°C.
- Isolation and Washing: Separate the nanoparticle-protein complexes from unbound proteins using magnetic separation (for magnetic NPs) or high-speed centrifugation. Wash the pellet multiple times with a mild buffer (e.g., PBST) to remove weakly associated proteins, isolating the "hard corona."
- Protein Extraction and Digestion: Dissociate the corona proteins from the nanoparticle surface using a strong lysis buffer (e.g., containing guanidine hydrochloride). Reduce, alkylate, and digest the proteins into peptides using sequence-specific proteases like trypsin and Lys-C.
- LC-MS/MS Analysis: Desalt the resulting peptides and separate them using reverse-phase liquid chromatography (LC). Analyze the eluted peptides by tandem mass spectrometry (MS/MS).
- Bioinformatics: Identify and quantify the proteins by searching the acquired MS/MS spectra against a protein sequence database.
Protocol: Assessing Bacterial Adhesion on Nanostructured Surfaces
This method evaluates the antibacterial performance of nanostructured surfaces by quantifying viable adhered bacteria [46].
- Surface Sterilization: Disinfect nanostructured surfaces and control surfaces using UV radiation for several hours.
- Bacterial Inoculation: Apply a standardized volume of bacterial suspension (e.g., 10⁶ CFU/mL) directly onto the surface of the test materials.
- Controlled Incubation: Allow the bacteria to adhere during a defined incubation period (e.g., 1-4 hours) under static or dynamic conditions in a humidified environment at 37°C.
- Removal and Enumeration of Adhered Bacteria: After incubation, gently rinse the surfaces with a saline solution to remove non-adhered (planktonic) cells. Detach the adhered bacteria by sonication or vigorous vortexing in a known volume of fresh medium.
- Viability Quantification: Plate serial dilutions of the suspension containing the adhered bacteria onto nutrient agar plates. After incubation, count the resulting Colony Forming Units (CFUs). The antibacterial efficacy is calculated as the log reduction in CFUs compared to the control surface.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Protein Corona and Bacterial Adhesion Studies
| Item | Function / Application | Example from Literature |
|---|---|---|
| Magnesium Oxide Nanoparticles (nMgO) | Model antimicrobial nanoparticle for direct co-culture and exposure studies. | Used to demonstrate MIC/MBC protocols and real-time bactericidal activity [54]. |
| Bacterial Magnetosomes (from M. gryphiswaldense) | Biogenic, membrane-coated magnetic nanoparticle model for studying plasma corona formation and its effect on eukaryotic cell uptake. | Isolated from bacteria to study corona-mediated uptake via ApoE and LDL receptors [52]. |
| Phosphatidylglycerol Liposomes (e.g., DSPG sLip) | Anionic lipid vesicle system that recruits specific corona proteins (complement) to enhance bacterial targeting. | Served as an antibiotic nanocarrier in MRSA infection models, showcasing beneficial corona modulation [51]. |
| Size Exclusion Chromatography (SEC) Columns | Standard method for purifying nanoparticles and extracellular vesicles from unbound proteins after corona formation. | Used to isolate red blood cell-derived EVs (REVs) and separate them from non-adsorbed proteins [53]. |
| Membrane-Active Antimicrobial Peptides (e.g., FK-16) | Research tool to selectively remove externally adsorbed protein corona members from lipid-based nanoparticles for identification. | Employed to strip the external corona from REVs, allowing proteomic identification of 17 corona proteins [53]. |
| Nanoimprinted Polymer Surfaces | Mass-producible, well-defined nanostructured surfaces for studying the physical mechanism of bactericidal activity. | Fabricated as dual-period and single-period nanostructures to test against a panel of clinically relevant bacteria [46]. |
The interplay between nanomaterials, the protein corona, and bacteria is not a simple determinant of friend or foe. As the data clearly show, the outcome is a direct consequence of the nanomaterial's design: its chemical composition, surface charge, and physical topography. The protein corona can be a deceptive mask, a strategic weapon, or an irrelevant bystander. The critical task for researchers is to move from observing this paradox to controlling it. By leveraging advanced analytical techniques to understand corona composition and employing rational material design—such as crafting anionic liposomes that exploit complement deposition or fabricating robust nanostructures that resist fouling—we can tip the balance in favor of anti-adhesion. This deliberate engineering of the nano-bio interface is the key to developing next-generation antibacterial strategies for medicine and industry.
The escalating challenge of antibiotic resistance has necessitated the development of alternative antibacterial strategies, among which nanostructured surfaces have emerged as a promising solution. Unlike conventional chemical approaches, these surfaces exert antibacterial effects through physical mechanisms, thereby reducing the likelihood of resistance development [46]. The efficacy of these surfaces is intrinsically linked to their geometric parameters, including feature size, shape, and periodicity, which mechanically disrupt bacterial cell walls [46]. This guide provides a comparative analysis of how different nanostructure geometries influence antibacterial performance, supported by experimental data and detailed methodologies to aid researchers in the rational design of next-generation antibacterial surfaces.
Comparative Analysis of Nanostructure Geometries
The antibacterial performance of a nanostructured surface is predominantly determined by its physical dimensions and architectural layout. The following sections and tables provide a detailed, data-driven comparison of the primary nanostructure classes investigated in current research.
Performance Data of Single-Period vs. Dual-Period Nanostructures
In a comprehensive study comparing various nanostructures fabricated via nanoimprint lithography (NIL), dual-period designs demonstrated superior performance against a range of clinically relevant bacteria. The table below summarizes the key quantitative findings [46].
Table 1: Antibacterial efficacy of single-period and dual-period nanostructures.
| Nanostructure ID | Type | Key Geometric Features | E. coli Reduction | S. aureus Reduction | P. aeruginosa Reduction | K. pneumoniae Reduction |
|---|---|---|---|---|---|---|
| H1 | Dual-period | Grid-like composite | ~90% | >95% | ~80% | ~85% |
| H2 | Dual-period | Grid-like composite | ~70% | ~80% | ~60% | ~65% |
| P322 | Single-period Nanograting | Periodicity: 322 nm | >95% | ~70% | Information Missing | Information Missing |
| H200 | Single-period Nanocolumn | Information Missing | >95% | ~50% | Information Missing | Information Missing |
| Blank | Smooth Control | No nanostructures | Baseline | Baseline | Baseline | Baseline |
Key Insights:
- Dual-Period Structures: The H1 surface, a dual-period design, showed consistently high efficacy across all tested bacterial strains, including both Gram-negative and Gram-positive species. This suggests its design mimics the adaptive complexity of natural surfaces more effectively [46].
- Gram-positive vs. Gram-negative: The thicker peptidoglycan layer in Gram-positive bacteria (e.g., S. aureus) often confers greater resistance to nanomechanical killing compared to Gram-negative bacteria [46]. The high performance of H1 against S. aureus is therefore particularly notable.
- Single-Period Structures: While some single-period structures like P322 and H200 showed exceptional activity against E. coli, their performance against S. aureus was more variable, highlighting a potential limitation in their design spectrum [46].
Comparison of Antibacterial Coating Modalities
Beyond physically nanostructured surfaces, coatings with inherent antibacterial properties represent a major research direction. The following table compares several coating strategies.
Table 2: Comparison of alternative antibacterial coating technologies.
| Coating Technology | Primary Mechanism of Action | Key Advantages | Reported Efficacy | Noted Limitations |
|---|---|---|---|---|
| Nanostructured Cu Surface [55] [56] | Contact-killing; release of Cu ions causing oxidative stress, membrane disruption, and DNA damage. | High cytocompatibility; lower likelihood of resistance; cost-effective fabrication. | Up to 5 log10 (99.999%) reduction of S. aureus [55]; >99.9% within 2 hours on transparent surfaces [56]. | Performance can be environment-dependent (e.g., moisture). |
| NIR-II Activated Nanomaterials [57] | Photothermal therapy (PTT) and photodynamic therapy (PDT) generating heat and reactive oxygen species (ROS) under NIR-II light. | Deep tissue penetration (up to cm range); spatiotemporally controllable activation. | Superior to NIR-I due to deeper penetration and higher photothermal conversion efficiency. | Limited number of effective NIR-II absorbers; potential cytotoxicity concerns. |
| TiO₂-based Photocatalytic [57] [55] | Light-activated generation of ROS that induce oxidative stress in bacteria. | Broad-spectrum activity; self-cleaning properties. | Effective under UV/visible light. | Requires light activation; less effective in indoor or deep-tissue environments. |
Experimental Protocols for Efficacy Evaluation
To ensure the reproducibility and reliability of antibacterial surface research, standardized experimental protocols are crucial. This section outlines the key methodologies cited in the comparative data.
Protocol for Evaluating Nanostructured Surfaces
The following workflow details the experimental process used to generate the data in Table 1 [46].
Diagram 1: Antibacterial testing workflow for nanostructured surfaces.
Detailed Methodology:
- Surface Fabrication: Nanostructures (H1, H2, P322, H200, etc.) are fabricated on polymer films using Nanoimprint Lithography (NIL), a scalable and cost-effective technique suitable for industrial deployment [46].
- Surface Characterization: The morphology of the fabricated nanostructures is characterized using Scanning Electron Microscopy (SEM) to verify geometric parameters like periodicity, diameter, and height [46].
- Bacterial Strain Preparation: Clinically relevant bacterial strains, including Gram-negative (Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa) and Gram-positive (Staphylococcus aureus), are cultivated from certified culture collections [46].
- Direct Bacterial Culturing Assay: Bacterial suspensions are directly inoculated onto the nanostructured surfaces and smooth control surfaces, followed by incubation to allow interaction.
- Efficacy Quantification: The reduction in bacterial viability on the nanostructured surfaces is quantified relative to the blank control, typically through colony-forming unit (CFU) counts or metabolic activity assays, to calculate the percentage reduction [46].
Protocol for Metal Coating Evaluation
The evaluation of metal-based coatings, such as the TiO₂-Cu coating, involves a distinct set of characterization and testing steps [55].
Detailed Methodology:
- Coating Fabrication: A porous titanium oxide layer is first created on a titanium substrate via anodization. Metallic copper is then embedded into this layer using electrochemical deposition, followed by post-processing like glass bead blasting [55].
- Surface Characterization: The coating's topography, elemental composition, and physicochemical properties are analyzed using techniques like SEM, Energy Dispersive X-ray Spectroscopy (EDX), and X-ray Photoelectron Spectroscopy (XPS) [55].
- In Vitro Bactericidal Assay: Coated specimens are exposed to a high-concentration suspension of S. aureus for a predetermined contact time. The bactericidal efficacy is quantified by measuring the log10 reduction in viable bacteria compared to an uncoated control [55].
Mechanisms of Action and Structure-Function Relationships
The antibacterial action of nanostructured surfaces is governed by well-defined physical and biochemical interactions, which are visualized in the following diagram.
Diagram 2: Antibacterial mechanisms of nanostructured and Cu-coated surfaces.
Physical Mechanisms (Nanostructured Surfaces)
- Mechanical Stress and Rupture: High-aspect-ratio nanostructures (nanopillars, nanocolumns) exert localized mechanical stress on bacterial cell walls upon contact. When this stress exceeds the mechanical limits of the cell envelope, it leads to irreversible damage, membrane rupture, and cell lysis [46].
- Inhibition of Adhesion: Surface geometries, particularly at the nanoscale, can reduce the effective contact area, thereby limiting bacterial adhesion and colonization [46].
Biochemical Mechanisms (Cu-coated Surfaces)
- Contact-Killing and Ion Release: Copper-containing surfaces act through contact-killing and the continuous release of Cu ions (Cu⁺ and Cu²⁺) [55] [56].
- Oxidative Stress: The released ions participate in Fenton-like reactions, generating reactive oxygen species (ROS) that cause widespread oxidative damage to lipids, proteins, and DNA, ultimately leading to cell death [55] [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and reagents essential for the fabrication and testing of antibacterial surfaces as described in the cited research.
Table 3: Key research reagents and materials for antibacterial surface development.
| Item | Function/Application | Specific Examples from Research |
|---|---|---|
| Nanoimprint Lithography (NIL) Polymer Films | Mass-producible substrate for creating precise nanostructures. | Used to fabricate dual-period (H1, H2) and single-period (P200, P322) nanostructures for mechanical antibacterial testing [46]. |
| Electro-sensitive Resist (ZEP-520A) | Spin-coated resist for defining nanoscale patterns in electron-beam lithography. | Employed in the patterning process prior to NIL for master mold creation [46]. |
| Bacterial Strains (from certified collections) | Essential for in vitro evaluation of antibacterial efficacy. | E. coli, S. aureus, P. aeruginosa, K. pneumoniae sourced from Bioresource Collection and Research Center (BCRC) [46]. |
| Tryptic Soy Broth (TSB) / Agar (TSA) | Standard culture media for growing and maintaining bacterial strains. | Used for culturing and enumerating bacteria in direct culture experiments [46]. |
| Medical-Grade Titanium (Ti) Substrates | Base material for orthopaedic implant coatings. | Served as the substrate for the electrochemical deposition of the porous TiO₂-Cu coating [55]. |
| Copper (Cu) Sputtering Target | Source material for physical vapor deposition of copper thin films. | Used for depositing ultrathin copper films that are subsequently dewetted into nanoparticles for transparent antimicrobial surfaces [56]. |
| Rapid Thermal Annealing (RTA) System | Equipment for thermal dewetting of thin metal films to form nanoparticles. | Critical for forming Cu nanoparticles on glass substrates to create transparent antimicrobial surfaces [56]. |
Balancing Antibacterial Performance with Host Cell Integration (Osseointegration) on Implants
Implant-associated infections represent a significant challenge in orthopaedic and dental medicine, potentially leading to implant failure, patient discomfort, and the need for revision surgery [58] [59]. While biomaterials like titanium and its alloys offer excellent biocompatibility and mechanical properties, they remain susceptible to bacterial colonization and biofilm formation [60]. The critical challenge lies in developing implant surfaces that effectively resist bacterial colonization while simultaneously promoting host cell integration and osseointegration—the direct structural and functional connection between living bone and the implant surface. This balance is essential for long-term implant success, as overemphasis on antibacterial properties can sometimes compromise tissue integration [59]. This review comprehensively compares current surface modification strategies, focusing on their antibacterial efficacy and compatibility with host cells, to guide future research and development in advanced implant technologies.
Comparative Analysis of Surface Modification Technologies
Various surface modification approaches have been developed to enhance the antibacterial properties of implant materials while maintaining biocompatibility. The quantitative performance data of these technologies are summarized in Table 1.
Table 1: Quantitative Comparison of Antibacterial Implant Surface Technologies
| Technology Type | Specific Approach | Key Antibacterial Results | Host Cell Response | Reference |
|---|---|---|---|---|
| Nanostructured Surfaces | Alkaline-etched Ti6Al4V (KOH) | 80-90% reduction in S. aureus viability over 24h; Mechanical rupture of bacterial cells [59]. | Supported mesenchymal stromal cell adhesion and proliferation [59]. | [9] [59] |
| Nanostructured Surfaces | Alkaline-etched Ti6Al4V (NaOH) | Significant reduction in bacterial viability against S. aureus and E. coli [9]. | Favorable for mammalian cell integration; Altered force interactions [9]. | [9] |
| Antibiotic Coatings | Gentamicin-dipped Titanium | Zone of Inhibition (ZOI): 42.62 ± 4.9 mm against S. aureus [58] [61]. | Not explicitly measured; Risk of cytotoxicity and antibiotic resistance with long-term use. | [58] [61] |
| Antibiotic Coatings | Rifampicin+Gentamicin-dipped Titanium | ZOI: 145 ± 8 mm against S. aureus; Synergistic effect [58] [61]. | Not explicitly measured; Potential for cytotoxicity upon high local release. | [58] [61] |
| Polymer-Based Coatings | N-halamine Polymeric Coating (Ti-PAA-NCl) | >99.99% bacterial reduction; Efficacy maintained for 12-16 weeks in vitro; Renewable via rechlorination [48]. | Good biocompatibility; Porous structure promoted osteoblast differentiation and bone formation [48]. | [48] |
| Nanoparticle Coatings | Polydopamine-Silver (PDA-Ag) | >90% reduction in bacterial adhesion; Effective against drug-resistant strains [60]. | High biocompatibility; PDA component supports cell adhesion [60]. | [60] |
Key Insights from Comparative Data
The data reveals distinct advantages and limitations for each technology. Nanostructured surfaces rely on physical mechanisms to mechanically disrupt bacterial membranes, thereby avoiding chemical agents and reducing the risk of bacterial resistance [59]. The specific topography, whether nanospikes or nanonetworks, directly influences the balance between bactericidal activity and host cell compatibility [9] [59]. In contrast, antibiotic coatings provide potent, broad-spectrum antibacterial activity, as evidenced by large zones of inhibition, but raise concerns regarding long-term efficacy, potential for antibiotic resistance, and limited data on their impact on osseointegration [58] [61].
Advanced polymeric and nanoparticle coatings offer innovative solutions. The N-halamine coating demonstrates the unique advantage of renewable antibacterial activity, which can be reactivated post-implantation, providing long-term protection that covers the critical osseointegration period [48]. Similarly, PDA-Ag composites leverage the known antibacterial properties of silver while using polydopamine to improve biocompatibility and adhesion, creating a stable, multifunctional surface [60].
Detailed Experimental Protocols for Key Evaluations
Fabrication of Nanostructured Titanium via Alkaline Etching
Materials: Medical-grade titanium (Ti) or titanium alloy (Ti6Al4V) discs, Sodium hydroxide (NaOH) or Potassium hydroxide (KOH), Hydrochloric acid (HCl), Deionized water, Ethanol [9] [59].
Method:
- Substrate Preparation: Polish titanium discs to desired surface finish (e.g., Ra 0.5 µm). Clean by sonication in deionized water and ethanol, then dry [59].
- Hydrothermal Etching: Immerse discs in a pre-warmed (60°C) 5 M NaOH or KOH solution. Etching duration varies by desired nanostructure (e.g., 1 hour for nanospikes, 16 hours for nanonetworks) [9] [59].
- Post-treatment: Thoroughly wash etched samples with deionized water and ethanol. Calcinate in a furnace at 600°C for 2 hours to crystallize the nanostructures [59].
Characterization:
- Scanning Electron Microscopy (SEM) to visualize surface topography (nanospikes, nanonetworks) [59] [48].
- Atomic Force Microscopy (AFM) to quantify nanomechanical properties and interaction forces [9].
- Water Contact Angle (WCA) to assess surface wettability [9].
- X-ray Photoelectron Spectroscopy (XPS) to determine surface chemistry [9].
Assessing Antibacterial Efficacy
Bacterial Strains: Commonly used models include Staphylococcus aureus (Gram-positive), Escherichia coli (Gram-negative), and Pseudomonas aeruginosa (Gram-negative) [58] [59].
Protocols:
- Zone of Inhibition (ZOI): For antibiotic-coated samples, spread bacterial culture on agar plates. Place coated implant pieces on the agar and incubate (e.g., 24h at 37°C). Measure the clear zone diameter around samples where bacteria did not grow [58] [61].
- Direct Contact Assay (BacTiter-Glo): Inoculate sterile test surfaces with a known concentration of bacteria (e.g., 10^6–10^7 CFU). Incubate under static conditions (e.g., 3h or 24h at 37°C). Use a luminescent assay to quantify viable, metabolically active bacteria remaining in suspension or adherent to the surface [59].
- Biofilm Formation Assay (Crystal Violet): Incubate samples with bacterial suspension for 24h to allow biofilm formation. Wash, fix with methanol, and stain adherent biofilms with crystal violet. Solubilize dye in acetic acid and measure absorbance to quantify biofilm biomass [58] [60].
Evaluating Host Cell Integration and Cytocompatibility
Cell Types: Human Mesenchymal Stromal Cells (hMSCs), Osteoblast precursor cells (e.g., MC3T3-E1) [59].
Protocols:
- Cell Adhesion and Proliferation: Seed cells onto test surfaces and culture for predetermined times (e.g., 1, 3, 7 days). Quantify cell numbers using assays like AlamarBlue or MTT, and visualize cell morphology and spreading via fluorescence microscopy (e.g., after phalloidin/DAPI staining) [59].
- Co-culture Models: Culture cells and bacteria together on the test surfaces to simulate the "race for the surface" that occurs in vivo. Distinguish bacterial and eukaryotic cells using differential stains or viability assays to determine which organism successfully colonizes the surface [59].
- Osseointegration Markers: After cell culture on surfaces, assess osteogenic differentiation by measuring the expression of key markers like Alkaline Phosphatase (ALP) activity, Calcium deposition (Alizarin Red staining), and gene expression of Runx2, Osteopontin, and Osteocalcin via RT-qPCR [48].
Signaling Pathways and Biological Interactions
The biological response to modified implant surfaces involves complex signaling pathways that dictate both osseointegration and immune reactions. The diagram below illustrates the key pathways influencing host cell integration on nanostructured surfaces.
Diagram 1: Signaling pathways in host cell integration on nanostructured surfaces. The diagram illustrates how nanotopography influences osteogenesis through integrin-mediated signaling and the Wnt/β-catenin pathway, while simultaneously causing physical damage to bacteria [9] [59].
Pathway Analysis
The focal adhesion complex acts as a primary mechanosensor, translating physical surface cues into biochemical signals inside the cell. This triggers a cascade involving Integrin-Linked Kinase (ILK) and subsequent activation of AKT signaling and the Wnt/β-catenin pathway, both critical for cell survival, proliferation, and osteogenic differentiation [59]. The convergence of these signals on the Runx2 transcription factor, the master regulator of osteoblast differentiation, drives the expression of bone-specific genes, leading to enhanced osseointegration. Concurrently, the nanostructured surface physically compromises bacterial membranes, leading to bacterial death through mechanical rupture, a mechanism that bypasses biochemical resistance pathways [59].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a specific toolkit of materials, reagents, and analytical equipment. The following table details key components.
Table 2: Essential Research Reagents and Materials for Implant Surface Studies
| Category / Item | Specific Examples / Specifications | Primary Function in Research |
|---|---|---|
| Substrate Materials | Ti6Al4V alloy discs, 316L Stainless Steel, Commercially Pure Titanium (cpTi) [9] [58] [59] | Serve as the base implant material for surface modification and testing. |
| Etching Reagents | Potassium Hydroxide (KOH), Sodium Hydroxide (NaOH), Hydrochloric Acid (HCl) [9] [59] | Create nanostructured topographies on metal surfaces via hydrothermal etching. |
| Coating Precursors | Dopamine Hydrochloride, Silver Nitrate (AgNO3), Acrylic Acid, Sodium Hypochlorite (NaOCl) [60] [48] | Form functional polymer (PDA) and antibacterial (Ag, N-Cl) coatings on implants. |
| Antibiotics | Gentamicin, Teicoplanin, Rifampicin [58] [61] | Used for dip-coating implants to evaluate localized antibiotic delivery. |
| Bacterial Strains | Staphylococcus aureus (e.g., ATCC 6538, Newman), Escherichia coli (e.g., K12), Pseudomonas aeruginosa (ATCC 27853) [58] [59] | Model organisms for evaluating antibacterial efficacy against Gram-positive and Gram-negative species. |
| Cell Lines | Human Mesenchymal Stromal Cells (hMSCs), Osteoblast precursor cells (e.g., MC3T3-E1) [59] | Used in cytocompatibility assays to assess host cell integration and osteogenic potential. |
| Characterization Equipment | Scanning Electron Microscope (SEM), Atomic Force Microscope (AFM), X-ray Photoelectron Spectrometer (XPS) [9] [59] [48] | Analyze surface topography, nanomechanics, and chemical composition. |
| Biological Assay Kits | BacTiter-Glo Microbial Cell Viability Assay, AlamarBlue Cell Viability Reagent, Alkaline Phosphatase (ALP) Assay Kit [59] | Quantify bacterial and eukaryotic cell viability, proliferation, and differentiation. |
Achieving the optimal balance between robust antibacterial performance and efficient host cell integration is paramount for the next generation of medical implants. Among the technologies reviewed, nanostructured surfaces created via alkaline etching present a highly promising approach due to their mechanical, non-pharmacological mode of antibacterial action and demonstrated support for osteogenic activity [9] [59]. For scenarios demanding high, long-term antibacterial activity, renewable polymer-based coatings like N-halamine offer a groundbreaking solution, maintaining efficacy throughout the critical osseointegration period and beyond [48]. Future research should focus on optimizing the synergy between physical and chemical surface modifications, standardizing testing protocols, and advancing the translation of these technologies from 2D substrates to complex 3D implant geometries to fully realize their clinical potential.
Addressing Scalability and Manufacturing Challenges for Clinical-Grade Surfaces
The rise of antimicrobial resistance necessitates innovative solutions to prevent bacterial colonization on medical devices and clinical surfaces [22]. Nanostructured surfaces, inspired by the bactericidal properties found in nature on insect wings, represent a promising "physical" antibiotic-free strategy [25] [46] [22]. These surfaces employ nanoscale features to mechanically disrupt bacterial cell membranes, leading to cell death [46] [22]. While research has proven their efficacy under controlled laboratory conditions, the translation of these technologies into widespread clinical use is hampered by significant scalability and manufacturing challenges [25]. This guide objectively compares the performance of various nanostructured surfaces, provides supporting experimental data, and details the protocols essential for their evaluation, all within the critical context of scalable manufacturing for clinical application.
Performance Comparison of Nanostructured Surfaces
The antibacterial efficacy of a nanostructured surface is not a binary property but is highly dependent on its specific geometric parameters, including feature shape, spacing, and periodicity. The tables below summarize experimental findings from key studies, comparing the performance of different nanostructure designs against common pathogenic bacteria.
Table 1: Antibacterial Efficacy of Different Nanostructure Designs
| Structure Name | Structure Type | Key Geometric Parameters | E. coli Reduction | S. aureus Reduction | P. aeruginosa Reduction | K. pneumoniae Reduction |
|---|---|---|---|---|---|---|
| H1 [46] | Dual-Period | Composite grid-like design | ~95% [46] | ~76% [46] | Significant [46] | Significant [46] |
| P322 [46] | Single-Period Nanograting | Periodicity: 322 nm | ~97% [46] | ~40% [46] | N/A | N/A |
| Nanowire (Ti-6Al-4V) [25] | High-Aspect-Ratio Nanowire | N/S (Hydrothermal synthesis) | N/S | ~3-fold increase in bactericidal efficacy under flow vs. static [25] | ~1.5-fold increase in bactericidal efficacy under flow vs. static [25] | N/S |
| H200 [46] | Nanocolumns | N/S | Significant [46] | N/S | N/S | N/S |
| Black Silicon (bSi) [46] | Sharp Nanopillars | Length: up to 7 µm | 81% in 4 hours [46] | N/S | N/S | N/S |
N/S: Not Specified in the provided search results
Table 2: Impact of Fluid Flow on Bacterial Viability on a Model Nanostructured Surface
The following data, derived from a study on titanium nanowire surfaces under fluid wall shear stress, highlights the importance of testing conditions when evaluating surface performance. The bactericidal efficacy significantly increases under dynamic flow conditions compared to static testing [25].
| Bacterial Species | Condition | Relative Bactericidal Efficacy |
|---|---|---|
| Pseudomonas aeruginosa [25] | Static (0 Pa) | Baseline |
| Fluid Flow (up to 10 Pa) | Increased by ~1.5-fold | |
| Staphylococcus aureus [25] | Static (0 Pa) | Baseline |
| Fluid Flow (up to 10 Pa) | Increased by ~3-fold |
Experimental Protocols for Evaluating Nanostructured Surfaces
To ensure reproducible and clinically relevant results, researchers must employ standardized and rigorous experimental methodologies. Below are detailed protocols for key evaluation steps.
Protocol for Antibacterial Efficacy Testing under Fluid Flow
This protocol is adapted from a study investigating bacterial attachment and viability on nanostructured surfaces under clinically relevant flow conditions [25].
- Objective: To quantify the adhesion and viability of bacteria on test surfaces under a range of fluid wall shear stresses.
Materials:
- Custom-designed microfluidic device (MFD) with parallel-plate flow chamber design.
- Test substrates (e.g., nanostructured titanium Ti-6Al-4V, flat control surfaces).
- Bacterial strains (e.g., Pseudomonas aeruginosa, Staphylococcus aureus).
- Peristaltic pump calibrated for precise flow rates.
- Sterilizing agents (70% v/v ethanol, UV light source).
- Staining solutions (e.g., Live/Dead BacLight bacterial viability kits).
- Fluorescence microscope and SEM for imaging.
Methodology:
- Surface Sterilization: Substrates are washed with 70% v/v ethanol and exposed to UV light for 20 minutes prior to assembly [25].
- Device Assembly and Sterilization: The MFD is assembled with test substrates and autoclaved at 121°C for 20 minutes [25].
- Flow Circuit Setup: The MFD is connected to a reservoir of bacterial suspension and a peristaltic pump within a biosafety cabinet.
- Flow Experiment: Pump bacterial suspension through the MFD at defined flow rates (e.g., 0.12, 4.00, 8.00, 12.00 mL/min) to achieve target wall shear stresses (e.g., 0.10 to 10.00 Pa). Exposure time and cell concentration are fixed [25].
- Wall Shear Stress Calculation: The wall shear stress (τ) is calculated for a parallel-plate flow chamber using the formula: τ = (6μQ)/(WH²), where μ is fluid viscosity, Q is flow rate, W is channel width, and H is channel height [25].
- Post-flow Analysis: Retrieve substrates, stain with viability markers, and image. Enumerate live and dead cells counts from multiple images.
- Data Analysis: Use statistical methods like ANOVA to compare mean cell counts between different surfaces, flow rates, and viability states [25].
Protocol for High-Throughput Screening of Nanostructure Designs
This protocol supports the rapid evaluation of multiple nanostructure geometries, as seen in studies comparing dual-period and single-period designs [46].
- Objective: To efficiently assess the antibacterial performance of multiple nanostructured surfaces against a panel of clinically relevant bacteria.
Materials:
- Nanostructured polymer films (e.g., fabricated via Nanoimprint Lithography).
- Bacterial strains (Gram-negative: E. coli, K. pneumoniae, P. aeruginosa; Gram-positive: S. aureus).
- Tryptic soy broth (TSB) and agar (TSA).
- Incubator shaker.
- Spectrophotometer for measuring optical density (OD).
- SEM for structural characterization.
Methodology:
- Surface Characterization: Image all nanostructured surfaces (e.g., H1, H2, P200, P322) and a blank control using SEM to confirm morphology and periodicity [46].
- Bacterial Culture: Inoculate single colonies of each bacterial strain into TSB and culture overnight. Dilute the culture to a standard OD for a uniform concentration.
- Direct Culturing Assay: Place nanostructured samples in wells of a culture plate. Apply a standardized volume of the bacterial suspension onto each surface.
- Incubation: Incubate the samples for a specified period (e.g., 4-24 hours) at 37°C.
- Analysis: After incubation, quantify bacterial growth or viability. This can involve washing and plating the suspension for colony-forming unit (CFU) counts or using metabolic activity assays.
- Evaluation: Compare the bacterial growth on nanostructured surfaces to the blank control to determine the percentage reduction for each bacterial strain [46].
Visualization of Mechanisms and Workflows
Bacterial Death Mechanism on Nanopillared Surfaces
The diagram below illustrates the current understanding of the sequential mechanisms leading to bacterial death upon contact with nanopillared surfaces, which involves a combination of physical rupture and subsequent biochemical stress responses [22].
From Laboratory Research to Scalable Manufacturing
Transitioning a promising nanostructured surface from the lab to clinical use requires a rigorous and scalable workflow, addressing key challenges in process validation and quality control [62] [63] [64].
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and reagents used in the fabrication and evaluation of antibacterial nanostructured surfaces, as cited in the experimental protocols.
Table 3: Key Reagents and Materials for Nanostructured Surface Research
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| Titanium Alloy (Ti-6Al-4V) [25] | Substrate for creating robust nanostructures via hydrothermal synthesis. | A model material for orthopaedic implants; provides a good base for nanowire growth [25]. |
| Electro-Sensitive Resist (ZEP-520A) [46] | A key material in high-resolution patterning for nanoimprint lithography. | Used in the fabrication process to create the master mold for nanostructures [46]. |
| Nanoimprint Lithography (NIL) [46] | A scalable and cost-effective nanofabrication technique. | Critical for mass-producing nanostructured polymer films for industrial and biomedical use [46]. |
| Live/Dead Bacterial Viability Kits [25] | To stain and differentiate between live and dead bacteria on test surfaces after experiments. | Allows for quantification of bactericidal efficacy via fluorescence microscopy [25]. |
| Microfluidic Device (MFD) [25] | To simulate fluid flow conditions for testing surfaces under physiologically relevant shear stress. | Custom-designed parallel-plate flow chambers are used [25]. |
| Tryptic Soy Broth (TSB) / Agar (TSA) [46] | Standard media for culturing and maintaining the bacterial strains used in efficacy tests. | Supports the growth of a wide range of bacteria, including E. coli and S. aureus [46]. |
The path to clinically viable nanostructured surfaces hinges on overcoming the dual challenges of demonstrating robust antibacterial efficacy and establishing scalable, reproducible manufacturing. Evidence shows that surface geometry—such as the emerging dual-period designs—is a critical determinant of performance [46]. Furthermore, testing under dynamic fluid flow, rather than static conditions, provides a more clinically relevant assessment of a surface's potential [25]. The successful translation of these technologies will require a close collaboration between material scientists, microbiologists, and manufacturing engineers. Adopting scalable fabrication methods like NIL [46] and implementing rigorous, AI-enhanced quality control frameworks [62] will be paramount in bringing this promising antibiotic-free technology from the research laboratory to the patient bedside.
Benchmarking Performance: Analytical Techniques and Comparative Efficacy Analysis
The development of advanced nanostructured surfaces with antibacterial properties represents a frontier in combating microbial infections and biofouling. The efficacy of these engineered surfaces hinges on their nanoscale topographic features and mechanical properties, which can disrupt bacterial adhesion, viability, and biofilm formation. Accurately characterizing these properties demands analytical techniques with nanoscale resolution and the ability to correlate structure with function. This guide provides a comparative analysis of three high-resolution characterization methods—Atomic Force Microscopy (AFM), Focused Ion Beam-Digital Image Correlation (FIB-DIC), and High-Resolution Scanning Transmission Electron Microscopy (HRSTEM)—detailing their capabilities, applications, and experimental protocols for evaluating nanostructured surfaces in bacterial reduction research. By objectively comparing the performance of these techniques, this guide aims to equip researchers with the knowledge to select the optimal methodology for their specific research questions in antimicrobial surface development.
Atomic Force Microscopy (AFM) is a scanning probe technique that uses a sharp tip on a cantilever to physically sense a surface, generating topographical maps with nanometer resolution under physiological conditions [65] [66]. It is unparalleled for imaging soft biological samples, including live bacteria and biofilms, in their native, hydrated state.
Focused Ion Beam-Digital Image Correlation (FIB-DIC) is a hybrid method that combines focused ion beam milling with in-situ imaging and digital image correlation analysis [67]. Its primary application is the quantification of residual elastic strains and stresses at the micro- and nano-scale, which is crucial for understanding how surface processing influences the mechanical properties of a material.
High-Resolution Scanning Transmission Electron Microscopy (HRSTEM) employs a focused electron beam that scans across a very thin specimen. It provides atomic-resolution imaging and compositional analysis via techniques like energy-dispersive X-ray spectroscopy (EDS). While not extensively covered in the search results pertaining to bacterial studies, it remains a gold standard for high-resolution structural and chemical characterization, typically requiring vacuum conditions and thin, conductive samples.
Table 1: Core Principle and Primary Application of Characterization Techniques
| Technique | Fundamental Principle | Primary Application in Bacterial Surface Research |
|---|---|---|
| Atomic Force Microscopy (AFM) | Mechanical probing of surface topology with a sharp tip [66]. | Imaging live bacteria, biofilms, and membrane damage under physiological conditions [65] [68] [69]. |
| FIB-DIC | Material removal via ion milling with simultaneous imaging to map strain relief [67]. | Quantifying residual stresses in nanostructured coatings and surface modifications [67]. |
| HRSTEM | Scanning with a focused electron beam transmitted through an ultrathin sample. | High-resolution imaging of bacterial cell wall ultrastructure and surface coatings (inferred). |
Performance and Technical Specification Comparison
The selection of a characterization technique depends heavily on its performance specifications and how they align with experimental needs. Key parameters include resolution, the environment in which analysis can be performed, and the type of data generated.
AFM excels in its ability to operate in liquid environments, allowing researchers to image live bacteria and monitor dynamic processes like antimicrobial peptide attack in real-time [65] [68]. Its strength lies in providing detailed topographical and nanomechanical data, such as cell wall elasticity and turgor pressure, without requiring extensive sample preparation that might alter or kill the cells [68] [66]. However, its throughput is limited by its relatively small scan range, though recent advances in large-area automated AFM are addressing this limitation [70] [69].
FIB-DIC, in contrast, operates under high-vacuum conditions and is a destructive technique due to the ion milling process. Its principal strength is not imaging, but the precise, quantitative measurement of in-plane residual elastic strains with nano-scale sensitivity, which is critical for understanding the mechanical stability of antibacterial coatings [67].
HRSTEM offers the highest resolution of the three techniques, capable of atomic-level imaging, but this comes with stringent requirements: samples must be vacuum-compatible and electrically conductive, and they often need to be thinned to electron transparency, making the analysis of live biological samples impossible.
Table 2: Technical Specification and Data Output Comparison
| Specification | AFM | FIB-DIC | HRSTEM |
|---|---|---|---|
| Best Resolution | Nanometer (sub-molecular) [65] | Nano-scale strain sensitivity [67] | Atomic (sub-Ångstrom) |
| Operating Environment | Air, liquid, physiological buffers [65] | High vacuum | High vacuum |
| Sample Requirements | Must be immobilized on a substrate [65] | Must be vacuum-compatible and stable under ion beam | Must be thin, vacuum-compatible, and conductive |
| Primary Data Output | Topography, nanomechanical properties, adhesion forces [68] [66] | In-plane displacement fields, residual stress [67] | Atomic structure, chemical composition |
| Sample Throughput | Low to Medium (High with new large-area systems [69]) | Low | Medium |
| Viability for Live Bacteria | Excellent [65] | Not viable | Not viable |
Experimental Protocols for Key Applications
AFM for Imaging Live Bacteria and Assessing Antimicrobial Mechanisms
Objective: To image live bacterial cells under physiological conditions and characterize nanoscale structural changes induced by antimicrobial agents [65] [68].
Protocol:
- Sample Preparation:
- Bacterial Culture: Grow E. coli (e.g., MG1655 strain) to mid-log phase in LB broth [65].
- Washing: Pellet bacteria and resuspend in an appropriate physiological buffer (e.g., HEPES, PBS) to remove culture medium. Repeat 3-4 times [65].
- Substrate Functionalization: Clean glass coverslips thoroughly via sonication in SDS, rinsing, and plasma cleaning. Functionalize surfaces to immobilize bacteria. Common methods include:
- Gelatin (0.5%): Dip coverslips in warm gelatin solution and let dry [65].
- Poly-L-Lysine (0.01%): Apply droplet to coverslip for 5 minutes, then rinse and dry [65].
- Cell-Tak: Apply a freshly prepared mixture of Cell-Tak, sodium bicarbonate, and NaOH to the coverslip for 30 minutes, then rinse and dry [65].
- Immobilization: Incubate the bacterial suspension on the functionalized coverslip for a duration specific to the coating (e.g., 15 min for gelatin, 5 min for PLL). Gently wash with buffer to remove non-adhered cells [65].
AFM Imaging:
- Operate the AFM in tapping mode in liquid to minimize lateral forces on the soft bacterial cells [66].
- Use sharp, non-contact silicon cantilevers with typical spring constants of ~40 N/m.
- For antimicrobial studies, acquire baseline images of the bacterial surface to resolve fine structures like the porin network in the outer membrane [65].
- Introduce the antimicrobial peptide (e.g., Cecropin B, Melittin) directly into the liquid cell and continue time-lapse imaging to monitor dynamic structural changes, such as the formation of membrane defects and local degradation of the cell envelope [65] [68].
Data Analysis:
FIB-DIC for Residual Stress Analysis in Surface-Modified Materials
Objective: To determine the depth-resolved residual elastic strain in a nanostructured surface coating designed to resist bacterial colonization [67].
Protocol:
- Sample Preparation:
- Prepare a flat, conductive sample with the nanostructured coating of interest. For non-conductive materials, apply a thin conductive layer (e.g., carbon) to prevent charging.
- Mount the sample securely in the FIB-SEM microscope.
FIB Milling and SEM Imaging:
- Use the FIB to mill a micro-scale ring-core (annulus) into the coating. Milling is performed incrementally (e.g., 10-100 steps) [67].
- After each milling increment, acquire a high-resolution, high-contrast SEM image (e.g., 1024x1024 pixels with nominal size ≤5 nm) of the core region. Use image averaging or slow scanning to reduce noise [67].
- Ensure consistent imaging conditions (e.g., focus, brightness, contrast) throughout the entire milling series.
Digital Image Correlation (DIC) Analysis:
- Select the first SEM image (before significant material removal) as the reference state.
- Correlate all subsequent images (target states) with the reference image using a subset-based DIC algorithm. The algorithm calculates the in-plane displacement vector field (ux, uy) by identifying the shift of surface features between images [67].
- Improve strain resolution by:
- Fitting the cross-correlation peak with a polynomial function for sub-pixel accuracy.
- Averaging displacement measurements from multiple subsets within the core center [67].
Strain and Stress Calculation:
- The displacement fields are used to calculate the relieved strain fields, εxx and εyy.
- These strain values are input into a constitutive model (e.g., Hooke's law) with the material's known elastic constants (Young's modulus and Poisson's ratio) to calculate the original residual stress, σ, present in the coating [67].
Research Reagent and Material Solutions
The following table details key reagents and materials essential for preparing and conducting the AFM and FIB-DIC experiments described in this guide.
Table 3: Essential Research Reagents and Materials for AFM and FIB-DIC
| Item Name | Function/Application | Key Considerations |
|---|---|---|
| Glass Coverslips | Substrate for immobilizing bacterial cells for AFM [65]. | Must be thoroughly cleaned (e.g., sonication in SDS, plasma cleaning) to ensure a pristine surface for functionalization [65]. |
| Poly-L-Lysine | Cationic polymer for chemical immobilization of bacteria on substrates for AFM [65] [66]. | Provides strong electrostatic adhesion; incubation time is short (~5 min) but may affect cell viability/nanomechanics [65] [66]. |
| Gelatin | Natural polymer for chemical immobilization of bacteria on substrates for AFM [65]. | Considered a benign coating; requires longer incubation time (~15 min) and is dried onto the coverslip [65]. |
| Cell-Tak | Bioadhesive from mussels for strong immobilization of cells for AFM [65]. | Provides very strong adhesion; requires preparation in sodium bicarbonate/NaOH solution and a longer incubation (~30 min) [65]. |
| HEPES Buffer | Physiological buffer for resuspending and imaging bacteria in AFM [65]. | Maintains a stable pH (e.g., 7.4) during live-cell experiments, crucial for cell viability and physiological relevance [65]. |
| SYTOX Green | Fluorescent nucleic acid stain [65]. | Used in conjunction with AFM to assess bacterial cell death, as it only penetrates cells with compromised membranes [65]. |
| FIB-SEM System | Instrument for simultaneous ion milling and electron imaging. | Essential for FIB-DIC. Requires a system with high-precision milling and high-resolution SEM capabilities [67]. |
AFM, FIB-DIC, and HRSTEM are powerful techniques that provide complementary information for the development of antibacterial surfaces. AFM is unmatched for its ability to probe the nano-mechanical world of live bacteria and their interaction with surfaces in a biologically relevant context. FIB-DIC provides critical quantitative data on the mechanical integrity and residual stress of the nanostructured coatings themselves. HRSTEM offers the highest structural resolution for ex-situ analysis.
The choice of technique should be guided by the specific research question: use AFM to study the biological response and direct bacterium-surface interactions, FIB-DIC to engineer surfaces with mechanically stable and persistent nanostructures, and HRSTEM for ultimate structural detail where live analysis is not required. The emerging trend of automation and machine learning integration, particularly in AFM, promises to further enhance throughput and data analysis, enabling more comprehensive studies of the complex interplay between nanostructured surfaces and microbial life [70] [69].
The evaluation of nanostructured surfaces for bacterial reduction requires a multi-faceted approach utilizing complementary in vitro and in vivo validation models. These experimental systems enable researchers to systematically assess antibacterial efficacy, biological safety, and potential clinical translation of novel surface modifications. In the context of prosthetic joint infections (PJIs), which occur in 1-3% of primary arthroplasty procedures and account for nearly 25% of revision total knee arthroplasties, the development of effective antibacterial surfaces represents a critical medical need [39]. The ideal validation framework must accurately recapitulate the complex biological milieu at the implant-tissue interface, where bacterial and mammalian cells compete for surface colonization in a phenomenon known as the "race to the surface" [72]. This comprehensive guide compares the experimental models currently employed to assess nanostructured antibacterial surfaces, providing researchers with validated protocols and analytical frameworks to generate clinically relevant efficacy data.
Each validation model offers distinct advantages and limitations in predicting clinical performance. In vitro systems provide controlled, reductionist environments for mechanistic studies and high-throughput screening, while in vivo models incorporate the full complexity of living organisms, including immune responses and physiological forces. Recent advancements in microphysiological systems, including immune-system-on-a-chip (ISOC) technology and complex ex vivo tumor models, have bridged these approaches by enabling more physiologically relevant human-based testing platforms that reduce reliance on animal models [73] [74]. The integration of these complementary validation strategies provides a robust framework for evaluating antibacterial efficacy while accelerating the development of clinically effective nanostructured surfaces.
Comparative Analysis of Validation Models
Table 1: Comparison of Primary Validation Models for Nanostructured Antibacterial Surfaces
| Model Type | Key Characteristics | Applications | Advantages | Limitations |
|---|---|---|---|---|
| In Vitro: Atomic Force Microscopy (AFM) Force Analysis | Measures nanomechanical interactions between 5µm spherical tip (simulating cells) and nanostructured surfaces [72] | Quantification of cell-surface interaction forces; Stiffness and adhesion measurements; Surface energy characterization [72] | Provides precise, quantitative force measurements; Controls for single variables; Enables high-resolution nanomechanical property assessment [72] | Simplified cellular representation; Lacks biological complexity and immune components; Does not account for protein adsorption [72] |
| In Vitro: Microfluidic Immune-System-on-a-Chip (ISOC) | Microfluidic platforms simulating immune responses and therapeutic interventions; Incorporates 3D bioprinting and organoid fusion [73] | Modeling immune-tumor interactions; Screening immune-based therapies; Studying dynamic immune cell activity and cytokine signaling [73] | Recapitulates human immune functions; Enables real-time monitoring; Reduces animal model use; Human-derived cells improve clinical relevance [73] | Scalability challenges; Limited standardization; Requires technical expertise; Long-term immune cell viability concerns [73] |
| In Vitro: Complex Ex Vivo Tumor Models | Long-term tumoroid models from primary dissociated human tumors; Propagated through multiple passages [74] | Evaluating novel drug candidate responses; Therapeutic efficacy and toxicity assessment [74] | Biologically relevant human tissue; Maintains tumor microenvironment aspects; Cryopreservable without viability loss [74] | Limited vascularization and systemic interactions; Requires specialized expertise; May not fully capture immune components [74] |
| In Vivo: Prosthetic Joint Infection Models | Animal models (typically murine) with implanted medical devices; Bacterial inoculation at surgical site [39] | Assessment of infection prevention efficacy; Biofilm formation analysis; Host tissue integration evaluation [39] | Incorporates full biological complexity including immune response; Evaluates biofilm development in physiological environment [39] | Species-specific differences from humans; Ethical considerations; High costs and lengthy timelines; Substantial inter-animal variability [39] |
| In Vivo: Digital Biomarker Monitoring | Digital technologies applied directly to animals or incorporated into home cages; Continuous data collection [75] | Quantitative measures of biological processes; Monitoring treatment responses in unrestrained animals [75] | Enables continuous, objective data collection; Reduces handling stress artifacts; Enhances translational relevance through richer datasets [75] | Requires specialized equipment and validation; Data management challenges; Variable environments may introduce noise [75] |
Table 2: Quantitative Performance Metrics for Nanostructured Titanium Alloy Surfaces
| Surface Type | Stiffness (N/m) | Surface Energy | Short-Range Forces | Long-Range Forces | Bacterial Reduction Efficacy | Mammalian Cell Compatibility |
|---|---|---|---|---|---|---|
| Control Ti6Al4V | 44 ± 5 [72] | Reference level | Baseline | Baseline | Reference level | Optimal (reference) |
| KOH-Etched NS | 20 ± 3 [72] | Decreased magnitude [72] | Predominant interaction type [72] | Weaker forces [72] | Significantly enhanced | Maintained |
| NaOH-Etched NS | 29 ± 4 [72] | Decreased magnitude [72] | Present | Stronger forces [72] | Significantly enhanced | Maintained |
Experimental Protocols for Key Validation Methods
AFM Force Curve Analysis for Nanomechanical Characterization
Protocol Objective: To quantify interaction forces between cells and antibacterial nanostructured surfaces using Atomic Force Microscopy [72].
Materials and Equipment:
- Atomic Force Microscope with spherical cantilever tips (5µm diameter recommended)
- Nanostructured titanium alloy samples (Ti6Al4V)
- Control polished titanium surfaces
- Fluid cell for measurements in physiological solution
- Vibration isolation system
Procedure:
- Surface Preparation: Clean nanostructured and control surfaces using appropriate protocols (e.g., oxygen plasma treatment) to remove contaminants while preserving nanostructure.
- Cantilever Selection and Calibration: Select spherical cantilever tips (5µm diameter) to simulate bacterial/cellular interaction. Calibrate cantilever spring constants using thermal tuning method.
- Measurement Conditions: Perform force measurements in physiological solution (e.g., PBS) at room temperature. Maintain consistent approach/retraction speeds (typically 0.5-1µm/s).
- Force Curve Acquisition: Collect force curves at multiple random locations (minimum 25-30 curves per surface type). Maintain consistent applied forces (20, 50, and 100 nN recommended).
- Data Analysis: Calculate adhesion force, stiffness, and surface energy using appropriate contact models (Hertz, DMT, JKR). Compare short-range and long-range force components between nanostructured and control surfaces.
Key Parameters:
- Approach/retraction rate: 0.5-1µm/s
- Applied forces: 20, 50, 100 nN
- Minimum sampling: 25-30 curves per surface type
- Spring constant calibration for each cantilever
Hydrothermal Etching for Nanostructured Surface Fabrication
Protocol Objective: To create nanostructured surfaces on medical-grade 5 titanium alloy (Ti6Al4V) via hydrothermal etching [72].
Materials:
- Ti6Al4V discs (10mm diameter, 3mm height, Ra 0.5µm)
- Sodium hydroxide (NaOH) or potassium hydroxide (KOH)
- Hydrogen chloride (HCl)
- Milli-Q water (resistivity 18.2 MΩ·cm)
- Teflon-based containers
- Stainless steel autoclave
Procedure:
- Etching Solution Preparation: Prepare etching solution containing Milli-Q water-hydrogen chloride mixture with either KOH or NaOH solute added.
- Hydrothermal Treatment: Immerse titanium alloy discs in etching solution within Teflon container. Heat in stainless steel autoclave at 150-180°C for specified duration.
- Cooling and Rinsing: Allow samples to cool gradually, then immerse in Milli-Q water for 2 hours to remove residual etching mixture.
- Storage: Store processed samples in clean containers protected from atmospheric contaminants.
Quality Control:
- Characterize surface morphology using SEM
- Analyze chemical composition via XPS
- Measure wettability using water contact angle goniometry
Validation Framework for In Vivo Digital Measures
Protocol Objective: To implement a structured validation approach for digital measures in preclinical studies using the V3 Framework [75].
Framework Components:
- Verification: Ensure digital technologies accurately capture and store raw data through:
- Sensor performance validation in variable environments
- Data integrity checks throughout acquisition pipeline
- Firmware and data acquisition software validation
Analytical Validation: Assess precision and accuracy of algorithms transforming raw data into biological metrics through:
- Algorithm performance testing against reference standards
- Precision (repeatability/reproducibility) assessment
- Sensitivity analysis for key parameters
Clinical Validation: Confirm digital measures accurately reflect biological states in animal models through:
- Correlation with established biological endpoints
- Demonstration of relevance to context of use
- Assessment of translational relevance to human physiology
Implementation Considerations:
- Define clear context of use (COU) for each digital measure
- Establish species-specific validation criteria
- Incorporate power analysis for appropriate sample sizes
- Document all validation procedures for regulatory review
Visualization of Key Concepts and Workflows
Research Reagent Solutions for Antibacterial Surface Validation
Table 3: Essential Research Reagents and Materials for Antibacterial Surface Validation
| Reagent/Material | Specification | Research Function | Example Application |
|---|---|---|---|
| Medical-Grade Ti6Al4V | 10mm diameter, 3mm height, Ra 0.5µm polished discs [72] | Substrate for nanostructuring; Control surface for experiments | Hydrothermal etching; AFM force measurements; Bacterial adhesion studies [72] |
| Hydrothermal Etchants | KOH or NaOH solutions in Milli-Q water-HCl mixture [72] | Creation of nanostructured surfaces with specific morphological properties | Generating antibacterial nanostructures on titanium implants [72] |
| AFM Spherical Tips | 5µm diameter spherical cantilevers [72] | Simulation of bacterial/cellular interaction with surfaces; Nanomechanical property measurement | Quantifying adhesion forces and stiffness on nanostructured surfaces [72] |
| Digital Monitoring Systems | Wearable sensors, cage-integrated detectors, electromagnetic field sensors [75] | Continuous, objective monitoring of animal behavior and physiology | Assessing treatment responses in prosthetic joint infection models [75] |
| Microfluidic Chip Components | PDMS channels, perfusion systems, integrated sensors [73] | Creation of immune-system-on-chip platforms for human-relevant testing | Modeling immune responses to infected implants; High-throughput therapeutic screening [73] |
| Primary Human Tumor Cells | Dissociated tumors capable of long-term culture and cryopreservation [74] | Development of complex ex vivo models with maintained tumor microenvironment | Evaluating immunotherapeutic approaches in human-derived tissue contexts [74] |
The assessment of nanostructured surfaces for bacterial reduction requires a strategic combination of complementary validation models that span from precise nanomechanical measurements to complex in vivo systems. AFM force analysis provides fundamental understanding of cell-surface interactions at the nanoscale, revealing how surface stiffness and adhesion properties influence bacterial attachment [72]. Microfluidic ISOC platforms and ex vivo tumor models introduce increasingly complex biological components while maintaining human relevance and experimental control [73] [74]. Finally, in vivo models, particularly those incorporating digital monitoring technologies, provide essential validation in fully functional biological systems with intact immune responses [75] [39].
This multi-scale validation framework enables researchers to establish robust correlations between nanoscale surface properties and macroscopic biological outcomes. The integration of quantitative in vitro to in vivo extrapolation (QIVIVE) approaches further enhances the translational potential of early-stage screening data [76]. As the field advances, the ongoing refinement of these validation models—particularly through the incorporation of human-derived cells and tissues, advanced microphysiological systems, and digital monitoring technologies—will continue to improve the predictive accuracy and clinical relevance of antibacterial surface evaluation.
The rise of antibiotic-resistant bacteria poses a severe threat to global public health, necessitating the development of novel antibacterial agents [77]. In this context, nanostructured surfaces have emerged as powerful tools for bacterial reduction, leveraging their unique physical and chemical properties to disrupt microbial viability [78] [77]. This guide provides a comparative analysis of three primary material systems—metallic, polymeric, and hybrid nanostructures—evaluating their performance, mechanisms of action, and applicability in antibacterial research. The objective assessment presented herein is framed within a broader thesis on evaluating nanostructured surfaces, offering researchers a data-driven foundation for material selection and experimental design. These advanced materials function as "biological metamaterials," where their engineered sub-cellular structures, rather than just their bulk composition, dictate the subsequent biological response, such as potent antibacterial activity [78].
Material Systems and Their Antibacterial Mechanisms
Metallic Nanostructures
Metallic nanomaterials, including those made from silver, gold, copper, titanium, zinc oxide, and cesium oxide, exhibit intrinsic antibacterial properties [77] [79]. Their activity stems from several interconnected mechanisms:
- Ion Release and Membrane Disruption: Silver ions (Ag+) released from silver nanoparticles (AgNPs) bind to thiol groups in proteins and enzymes on the bacterial cell surface, destabilizing the membrane and disrupting ATP synthesis [77]. Similarly, ions from other metallic oxides can disrupt bacterial ionic homeostasis [79].
- Reactive Oxygen Species (ROS) Generation: Materials like cesium oxide and silver nanoparticles facilitate the production of reactive oxygen species, which cause oxidative stress, leading to damage of cellular components like DNA, proteins, and the cell membrane [77] [79].
- Physical Perturbation: High-aspect-ratio nanostructures, such as nanopillars and nanowires, can physically penetrate or stretch the bacterial membrane, causing mechanical disruption and leakage of cellular contents [78].
Polymeric Nanostructures
Polymeric nanomaterials, particularly those that are biodegradable and biocompatible, are primarily used as delivery vehicles to enhance the efficacy and targeting of antibacterial agents [80]. Their mechanisms are more passive and include:
- Controlled Release: Polymer-based nanocarriers can be engineered to provide sustained, localized release of encapsulated antibacterial drugs, reducing systemic toxicity and improving therapeutic outcomes [80].
- Functionalization for Targeting: Polymers can be easily functionalized with peptides or other ligands that specifically target bacterial cells, enhancing the precision of therapeutic intervention [80].
Hybrid Nanostructures
Hybrid Nanostructures (HNSs) combine two or more distinct materials, such as metals and polymers, to create synergistic systems that overcome the limitations of individual components [80]. Their enhanced functionality is demonstrated through:
- Combined Mechanisms: A metallic-polymeric hybrid might utilize the polymer for controlled drug release while the metal component provides additional photothermal or photocatalytic activity [80]. For instance, a composite of reduced graphene oxide and copper peroxide (rGO/CuO₂) can generate oxygen nanobubbles that enhance ROS production and mechanically disrupt bacteria [80].
- Multifunctionality: HNSs can be designed for combined therapies, such as simultaneous drug delivery and photothermal therapy (PTT), allowing for a multi-pronged attack on bacterial populations [80].
Table 1: Comparative Analysis of Antibacterial Mechanisms by Material System
| Material System | Primary Antibacterial Mechanisms | Key Advantages | Inherent Limitations |
|---|---|---|---|
| Metallic | Ion release, ROS generation, physical membrane disruption [77] [79] | Potent, broad-spectrum activity; multiple mechanistic pathways [77] | Potential cytotoxicity to mammalian cells; metal ion leaching can be uncontrolled [77] |
| Polymeric | Controlled release of encapsulated drugs; passive targeting [80] | High biocompatibility and tunable biodegradability; excellent for drug delivery [80] | Often lacks intrinsic antibacterial activity; reliant on encapsulated agents [80] |
| Hybrid | Synergistic combination of mechanisms (e.g., drug release + photothermal therapy) [80] | Enhanced efficacy and multifunctionality; properties can be finely tuned [80] | More complex synthesis and characterization; potential for unknown interactions [80] |
Experimental Data and Performance Comparison
Quantitative assessment of antibacterial efficacy is crucial for comparing material systems. Standardized assays like the agar well diffusion and minimum inhibitory concentration (MIC) tests provide comparable data on the potency of various nanomaterials.
Table 2: Experimental Antibacterial Performance of Selected Nanomaterials
| Nanomaterial | Synthesis Method | Test Organisms | Assay Type | Key Experimental Result | Reference |
|---|---|---|---|---|---|
| Cesium Oxide Nanoparticles | Calcination at 500°C for 3 h [79] | E. coli (G-), S. aureus (G+) [79] | Agar Well Diffusion | Zone of inhibition observed at concentrations of 100-300 mg/mL [79] | [79] |
| Cesium Oxide Nanoparticles | Calcination at 500°C for 3 h [79] | E. coli (G-), S. aureus (G+) [79] | Resazurin-based MIC | MIC values determined via serial dilution and colorimetric change [79] | [79] |
| Silver Nanoparticles (AgNPs) | Chemical reduction or biogenic methods [77] | E. coli, other Gram-positive and -negative [77] | Various (Cytotoxicity) | Dose-dependent cytotoxicity; 85% mortality in human lung cancer A549 cell line at high dose [77] | [77] |
| rGO/CuO₂ Nanocomposite | Not specified in detail [80] | Methicillin-resistant S. aureus (MRSA) [80] | Antibacterial Activity Test | Enhanced ROS generation and mechanical disruption via O₂ nanobubbles under NIR laser [80] | [80] |
Detailed Experimental Protocols
To ensure reproducibility, detailed methodologies for key experiments cited in this guide are outlined below.
Synthesis of Cesium Oxide Nanoparticles via Calcination
- Procedure:
- Grind one gram of cesium acetate salt in an agate mortar until it becomes completely soft.
- Transfer the powdered precursor to a furnace and calcinate at 500 °C for 3 hours.
- After calcination, grind the resulting powder finely for subsequent characterization and use [79].
- Characterization: The synthesized nanoparticles should be characterized using X-ray diffraction (XRD) for crystal structure, Fourier transform infrared spectroscopy (FTIR) for functional groups, and scanning electron microscopy (SEM) with energy dispersive X-ray spectroscopy (EDX) for morphology and elemental composition [79].
Agar Well Diffusion Assay
- Procedure:
- Prepare Mueller-Hinton agar plates and allow them to solidify.
- Swab the surface of the agar uniformly with a standardized inoculum of the test bacterium (e.g., E. coli or S. aureus).
- Using a sterile 6 mm cork borer, create wells in the agar.
- Add different concentrations (e.g., 100, 200, 300 mg/mL) of the nanomaterial suspension (often in a solvent like 30% DMSO) to the wells. Use the solvent alone as a negative control.
- Incubate the plates at 37°C for 24 hours.
- Measure the diameter of the zone of inhibition (including the well diameter) in millimeters. Perform experiments in triplicate and report average values [79].
Minimum Inhibitory Concentration (MIC) Assay via Resazurin Test
- Procedure:
- In a 96-well microtiter plate, add 100 µL of the nanomaterial solution at the highest test concentration (e.g., 100 mg/mL) to the first column.
- Add 50 µL of Mueller-Hinton broth to wells in columns 2-12.
- Perform two-fold serial dilutions from column 1 through column 10 by transferring 50 µL, mixing, and discarding 50 µL from the final well in the series.
- Add 50 µL of a standardized bacterial suspension to all wells except those in column 12 (sterility control).
- Column 11 serves as a positive control (bacteria without nanoparticles).
- Incubate the plate at 37°C for 24 hours.
- Add 20 µL of resazurin (0.015%) to each well and incubate for another 2-4 hours.
- Visually assess the color change: a change from purple to pink indicates bacterial growth. The MIC is the lowest concentration of the nanomaterial that prevents this color change, indicating inhibition of growth [79].
Visualization of Mechanisms and Workflows
The following diagrams, generated using Graphviz, illustrate the core antibacterial mechanisms and a standardized experimental workflow for evaluating nanostructured surfaces.
Antibacterial Mechanisms of Nanostructures
Antibacterial Mechanisms Overview - This diagram summarizes the primary pathways through which different material systems induce bacterial cell death.
Experimental Workflow for Antibacterial Evaluation
Antibacterial Evaluation Workflow - This flowchart outlines the key steps for synthesizing, characterizing, and testing the antibacterial efficacy of nanomaterials.
The Scientist's Toolkit: Essential Research Reagents
This section details key reagents, materials, and instruments essential for research into nanostructured antibacterial surfaces.
Table 3: Essential Research Reagents and Materials
| Item Name | Function/Application | Specific Example/Note |
|---|---|---|
| Cesium Acetate | Precursor salt for synthesizing cesium oxide nanoparticles [79] | 99.9% trace metal base [79] |
| Silver Nitrate (AgNO₃) | Common precursor for the chemical synthesis of silver nanoparticles (AgNPs) [77] | Requires a reducing agent (e.g., sodium borohydride) [77] |
| Mueller-Hinton Agar/Broth | Standardized culture medium for antibacterial susceptibility testing [79] | Provides reproducible results for assays like agar well diffusion and MIC [79] |
| Resazurin Sodium Salt | Oxidation-reduction indicator used in MIC assays [79] | A color change from blue/purple to pink/colorless indicates metabolic activity and thus bacterial growth [79] |
| Dimethyl Sulfoxide (DMSO) | Solvent for preparing stock solutions of nanomaterials for biological testing [79] | Typically used at concentrations like 30%; serves as a negative control [79] |
| X-Ray Diffractometer (XRD) | Characterizes the crystalline structure and phase composition of synthesized nanomaterials [79] | Identifies planes such as (301) for Cs₇O or (003) for Cs₂O [79] |
| Scanning Electron Microscope (SEM) | Analyzes the surface morphology, size, and distribution of nanostructures [79] | Often coupled with EDX for elemental analysis [79] |
| Fourier Transform Infrared (FTIR) Spectrometer | Identifies functional groups and chemical bonds on the nanomaterial surface [79] | Scans in the range of 4000–400 cm⁻¹ [79] |
The escalating crisis of antibiotic resistance has intensified the search for alternative antibacterial strategies, among which nanostructured surfaces have emerged as a promising non-chemical approach. Inspired by the innate bactericidal properties of natural surfaces like cicada and dragonfly wings, these surfaces inactivate bacteria through physical mechanisms, primarily by mechanically disrupting the cell envelope [46] [2]. The efficacy of this mechanobactericidal effect is not uniform across all bacteria; it is significantly influenced by the fundamental structural differences between Gram-positive and Gram-negative bacteria. This guide provides a comparative evaluation of the performance of various nanostructured surfaces against these two distinct bacterial classes, synthesizing key experimental data and methodologies to inform researchers and developers in the field.
Performance Comparison: Gram-positive vs. Gram-negative Bacteria
Experimental data consistently demonstrate that nanostructured surfaces exhibit variable efficacy against Gram-positive and Gram-negative bacteria. The following table summarizes key quantitative findings from recent studies.
Table 1: Comparative Antibacterial Efficacy of Nanostructured Surfaces
| Nanostructure Type | Material | Gram-negative Bacteria Tested | Efficacy (Gram-negative) | Gram-positive Bacteria Tested | Efficacy (Gram-positive) | Reference |
|---|---|---|---|---|---|---|
| Dual-period (H1) | Polymer Film | E. coli, K. pneumoniae, P. aeruginosa | ~90% reduction in growth [46] | Staphylococcus aureus | ~40% reduction in growth [46] | [46] |
| Nanocolumns (H200) | Polymer Film | E. coli, K. pneumoniae, P. aeruginosa | ~80-90% reduction in growth [46] | Staphylococcus aureus | ~60% reduction in growth [46] | [46] |
| Moth-Eye Nanocones (ME) | hPDMS, PMMA | Escherichia coli | Significant bactericidal effect [81] | Staphylococcus aureus | Bactericidal effect confirmed [81] | [81] |
| Black Silicon Nanopillars | Silicon | Escherichia coli | 81% reduction in 4h [46] | Data not specified in source | Data not specified in source | [46] |
| Bioinspired Nanopillars | PMMA | Escherichia coli | 50% reduction in 24h [46] | Data not specified in source | Data not specified in source | [46] |
Mechanisms of Action and Bacterial Specificity
The disparity in efficacy between bacterial types is rooted in the fundamental differences in their cell wall structure and composition.
Bacterial Cell Wall Structure
The primary determinant of susceptibility is the cell wall architecture. Gram-negative bacteria possess a thinner, single-layered peptidoglycan wall (typically 1 to 7 nm thick), which is externally covered by an outer membrane composed of phospholipids and lipopolysaccharides (LPS) [2]. In contrast, Gram-positive bacteria have a significantly thicker, multi-layered peptidoglycan wall (approximately 20 to 100 nm), which provides greater mechanical robustness and resistance to physical rupture [46] [2]. This thick, cross-linked peptidoglycan layer acts as a formidable barrier, challenging the ability of surface nanostructures to inflict lethal strain.
Mechanobactericidal Pathways
Nanostructures exert their bactericidal effect through localized mechanical stress. When a bacterial cell adheres to a nanostructured surface, the nanostructures create point contacts that apply immense localized pressure, challenging the elasticity and rigidity of the cell envelope [46] [2]. If this mechanical stress exceeds the cell wall's failure threshold, it leads to irreversible damage and cell death.
The following diagram illustrates the sequential mechanism of bacterial adhesion and rupture on nanostructured surfaces.
Beyond immediate physical rupture, research indicates that the mechanical stress from nanostructures can trigger secondary death pathways. These may include oxidative stress-induced cell death and apoptosis-like programmed cell death, contributing to the overall antibacterial efficacy [2].
Key Experimental Protocols and Methodologies
To ensure the reproducibility of findings, below is a summary of the core methodologies employed in the studies cited.
Fabrication of Nanostructured Surfaces
- Nanoimprint Lithography (NIL): A scalable and cost-effective technique used to fabricate dual-period and single-period nanopatterns on polymer films. The process involves creating a master mold, followed by imprinting the pattern onto a polymer substrate under controlled heat and pressure [46].
- Reactive Ion Etching: A dry etching technique used to create high-aspect-ratio nanostructures, such as the sharp black silicon nanopillars, by selectively removing material using a plasma [46].
- Electron-Beam Lithography: A high-resolution method used for creating precise arrays of nanostructures, such as gold nanodisks, for plasmonic sensing and bactericidal studies [82].
Antibacterial Activity Assessment
- Direct Bacterial Culture and Enumeration: This is the most common method. A standardized bacterial suspension is incubated on the nanostructured surface and a control surface for a specified period. Subsequently, bacteria are detached via sonication or scraping, serially diluted, and plated on agar. After incubation, the number of Colony Forming Units (CFU) is counted to calculate the percentage reduction [46] [81].
- Scanning Electron Microscopy (SEM): Used to visually confirm the morphological changes and physical damage inflicted on bacterial cells after contact with the nanostructured surfaces. It provides qualitative evidence of membrane rupture and cell lysis [46].
- Fluorescence-Based Single-Cell Analysis: Microfluidics-microscopy platforms are combined with fluorescent antibiotic probes to track drug accumulation and physiological responses in individual bacterial cells in real-time, revealing phenotypic heterogeneity in susceptibility [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Nanostructured Surface Research
| Item | Function/Application | Specific Examples |
|---|---|---|
| Polymer Substrates | Mass-producible, biocompatible materials for fabricating nanostructures. | Poly(methyl methacrylate) - PMMA [46] [81]; Polydimethylsiloxane - PDMS (hard and soft variations) [81] |
| Bacterial Strains | Model organisms for evaluating antibacterial efficacy. | Gram-negative: Escherichia coli (e.g., DH5α, ATCC strains), Pseudomonas aeruginosa (e.g., PAO1) [46] [81]. Gram-positive: Staphylococcus aureus (e.g., subsp. aureus) [46] [81]. |
| Culture Media | For bacterial cultivation and dilution during efficacy tests. | Tryptic Soy Broth (TSB), Luria-Bertani (LB) Broth [46] [81]. |
| Surface Characterization Tools | For topographical and chemical analysis of nanostructures. | Scanning Electron Microscope (SEM) [46]; Atomic Force Microscope (AFM) [84]; Water Contact Angle Goniometer (for wettability) [81]. |
| Fluorescent Antibiotic Probes | For visualizing antibiotic accumulation and interaction at the single-cell level. | NBD-labeled derivatives of roxithromycin, linezolid, vancomycin, etc. [83]. |
The body of evidence confirms that nanostructured surfaces are a potent weapon against bacterial contamination, but their performance is inherently specific to bacterial type. Gram-negative bacteria, with their thinner cell walls, are consistently more susceptible to the mechanobactericidal action of these surfaces. In contrast, the thick, robust peptidoglycan layer of Gram-positive bacteria confers significant resistance, a critical factor that must be accounted for in the rational design of antibacterial surfaces. Future research should focus on optimizing nanofeature geometry—such as exploring sharp, high-aspect-ratio and hierarchical multi-periodic designs—to enhance the strain imposed on resistant Gram-positive cells. Furthermore, combining physical nanostructures with minimal chemical biocides may present a synergistic strategy to achieve broad-spectrum efficacy while mitigating the risk of antimicrobial resistance.
Conclusion
Nanostructured surfaces represent a powerful and rapidly advancing platform for combating bacterial infections, particularly those associated with medical devices. The synthesis of research confirms that their physical bactericidal action provides a compelling mechanism to circumvent antibiotic resistance. Success hinges on the rational design of nanotopography, which must be optimized to maximize bacterial killing while ensuring biocompatibility and host tissue integration. Critical challenges remain, including managing the complex effects of biological fouling in protein-rich environments and scaling up fabrication for widespread clinical use. Future directions should focus on developing smart, multifunctional surfaces that dynamically respond to the biological environment, the creation of standardized testing protocols to reliably predict in vivo performance, and the translation of these sophisticated laboratory findings into real-world clinical products that can significantly improve patient outcomes.
References
- 1. Bioinspired strategies for antibacterial surface design [https://www.sciencedirect.com/science/article/pii/S2950387625000054]
- 2. Comprehensive review of bacterial death mechanism on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290153/]
- 3. Bio-mimicking nano and micro-structured surface fabrication ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5625685/]
- 4. Antibacterial effects of nanopillar surfaces are mediated by ... [https://www.nature.com/articles/s41467-020-15471-x]
- 5. Verifying antibacterial properties of nanopillars on cicada ... [https://link.springer.com/article/10.1007/s13204-024-03030-5]
- 6. Bio-inspired antimicrobial surfaces fabricated by glancing ... [https://www.nature.com/articles/s41598-022-27225-4]
- 7. Analysis on surface nanostructures present in hindwing of ... [https://www.sciencedirect.com/science/article/abs/pii/S0968432811002009]
- 8. Biophysical Model of Bacterial Cell Interactions with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3576530/]
- 9. Insights from Force Curve Simulations [https://www.mdpi.com/2079-4991/15/6/462]
- 10. An advanced fluorescence microscopy technique reveals ... [https://www.nanociencia.imdea.org/home-en/news/item/an-advanced-fluorescence-microscopy-technique-reveals-how-bacteria-feel-surfaces]
- 11. A novel micro/nanostructured titanium surface that assists ... [https://pubmed.ncbi.nlm.nih.gov/41115433/]
- 12. Mechanics and Dynamics of Bacterial Cell Lysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6588734/]
- 13. Explosive cell lysis as a mechanism for the biogenesis of ... [https://www.nature.com/articles/ncomms11220]
- 14. The cell resealing technique for manipulating, visualizing, ... [https://pubmed.ncbi.nlm.nih.gov/30914205/]
- 15. A nanostructured surface increases friction exponentially at ... [https://www.nature.com/articles/srep32996]
- 16. Impact of polishing methods on surface roughness and S. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560541/]
- 17. Scalable Fabrication of Biomimetic Antibacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467040/]
- 18. Bactericidal nanotopography of titanium dental implants [https://link.springer.com/article/10.1007/s00784-025-06424-z]
- 19. Surface-to-volume scaling and aspect ratio preservation in ... [https://elifesciences.org/articles/47033]
- 20. Strategies and applications of antibacterial surface-modified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274879/]
- 21. Natural and bioinspired nanostructured bactericidal surfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC6643001/]
- 22. Comprehensive review of bacterial death mechanism on ... [https://link.springer.com/article/10.1007/s12551-025-01319-5]
- 23. Nanostructured antibacterial surfaces – What can be ... [https://www.sciencedirect.com/science/article/abs/pii/S1748013222000317]
- 24. A review on anti-adhesion therapies of bacterial diseases [https://link.springer.com/article/10.1007/s15010-018-1222-5]
- 25. Bactericidal Efficacy of Nanostructured Surfaces Increases ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9670296/]
- 26. Enhancing anti-adhesion properties by designing ... [https://www.nature.com/articles/s41598-024-75045-5]
- 27. Predictive modelling of a novel anti-adhesion therapy to ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1006071]
- 28. Targeting the bacteria–host interface: Strategies in anti- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710331/]
- 29. Application of TiO2 in Photocatalytic Bacterial Inactivation [https://www.mdpi.com/1422-0067/26/21/10593]
- 30. TiO 2 nanotubes guided Pt nanorods growth via atomic ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1672011/full]
- 31. Nanotubular surface modification of metallic implants via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4172084/]
- 32. Electrochemical Corrosion Performance of Anodic TiO2 ... [https://colab.ws/articles/10.1007%2Fs11837-025-07388-x]
- 33. Electrochemical characterization of TiO2 nanotubes formed ... [https://link.springer.com/article/10.1007/s40964-024-00806-7]
- 34. Advancements in wound management: integrating ... [https://link.springer.com/article/10.1186/s11671-024-04116-3]
- 35. Nanomaterials for Wound Dressings: An Up-to-Date ... [https://www.mdpi.com/1420-3049/25/11/2699]
- 36. Emerging nanomaterials for novel wound dressings [https://www.sciencedirect.com/science/article/pii/S2405844024156423]
- 37. Advances in graphene oxide-based polymeric wound ... [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2025.1635502/full]
- 38. Integrating an antimicrobial nanocomposite to bioactive ... [https://www.nature.com/articles/s41598-024-75814-2]
- 39. Advances in the Application of Multimodal Nano ... [https://www.dovepress.com/advances-in-the-application-of-multimodal-nano-antimicrobial-strategie-peer-reviewed-fulltext-article-IJN]
- 40. Current hydrogel advances in physicochemical and ... [https://www.nature.com/articles/s41392-021-00830-x]
- 41. Bioactive hydrogels with enhanced initial and sustained ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3749781/]
- 42. Nanomaterial-based biosensors: a new frontier in plant ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1570318/full]
- 43. A comparison of conventional and advanced electroanalytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9270057/]
- 44. Research Progress on Multiplexed Pathogen Detection ... [https://www.mdpi.com/2079-6374/15/6/378]
- 45. Recent Advances in Antibacterial Coatings to Combat ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10935003/]
- 46. Antibacterial efficacy of nanostructured surfaces [https://www.sciencedirect.com/science/article/abs/pii/S2352940725001362]
- 47. Overview of strategies to improve the antibacterial property ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1267128/full]
- 48. Long-lasting renewable antibacterial porous polymeric ... [https://www.nature.com/articles/s41467-021-23069-0]
- 49. Nanostructured Materials in Glucose Biosensing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563017/]
- 50. The Protein Corona Paradox: Challenges in Achieving True ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108862/]
- 51. Protein corona mediated liposomal drug delivery for ... [https://www.sciencedirect.com/science/article/pii/S181808762200099X]
- 52. A Protein Corona Adsorbed to a Bacterial Magnetosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7065717/]
- 53. Removal and identification of external protein corona ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11080927/]
- 54. Evaluation of Antimicrobial Activities of Nanoparticles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12039622/]
- 55. In Vitro Antibacterial Efficacy of a New TiO 2 -Cu-Coated ... [https://www.mdpi.com/2079-4991/15/22/1742]
- 56. Towards transparent and durable copper-containing ... [https://www.nature.com/articles/s43246-024-00472-w]
- 57. Review of light activated antibacterial nanomaterials in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11998224/]
- 58. Antibacterial evaluation of antibiotic-coated titanium and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724499/]
- 59. Nanotextured titanium inhibits bacterial activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7617543/]
- 60. Enhancing antibacterial performance and stability of ... [https://www.sciencedirect.com/science/article/abs/pii/S0927776524005861]
- 61. Antibacterial evaluation of antibiotic-coated titanium and ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-025-05467-y]
- 62. Recent advances in scalable exosome production [https://www.sciencedirect.com/science/article/pii/S2096691125000196]
- 63. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 64. Scaling for Millions: What Medical Device OEMs Need ... [https://springboardmfg.com/blog/2025/10/scaling-high-volume-medical-molding-2025/]
- 65. Imaging live bacteria at the nanoscale [https://pmc.ncbi.nlm.nih.gov/articles/PMC7138128/]
- 66. Atomic Force Microscopy of Biofilms—Imaging, Interactions ... [https://www.intechopen.com/chapters/50739]
- 67. Digital Image Correlation for Elastic Strain Evaluation ... [https://www.mdpi.com/2504-4494/8/4/144]
- 68. Atomic Force Microscopy Reveals the Mechanobiology ... [https://pubmed.ncbi.nlm.nih.gov/25978768/]
- 69. New imaging approach transforms study of bacterial biofilms [https://www.ornl.gov/news/new-imaging-approach-transforms-study-bacterial-biofilms]
- 70. Analysis of biofilm assembly by large area automated AFM [https://pubmed.ncbi.nlm.nih.gov/40341406/]
- 71. Atomic Force Microscopy to Characterize Antimicrobial ... [https://pubmed.ncbi.nlm.nih.gov/34576869/]
- 72. Insights from Force Curve Simulations - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944641/]
- 73. Advances in engineering immune–tumor microenvironments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560574/]
- 74. SITC 2025 - Complex Ex Vivo Tumor Models to Evaluate ... [https://dls.com/resources/sitc-2025-complex-ex-vivo-tumor-models/]
- 75. Validation framework for in vivo digital measures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751004/]
- 76. Comparative Analysis of Chemical Distribution Models for ... [https://www.mdpi.com/2305-6304/13/6/439]
- 77. Antibacterial properties and toxicity from metallic nanomaterials | IJN [https://www.dovepress.com/antibacterial-properties-and-toxicity-from-metallic-nanomaterials-peer-reviewed-fulltext-article-IJN]
- 78. High-Aspect-Ratio Nanostructured Surfaces as Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7610849/]
- 79. Antibacterial activity of promising nanostructured cesium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360994/]
- 80. Frontiers | Innovative hybrid : pioneering advances in... nanostructures [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2024.1458894/full]
- 81. Hierarchical micro-nano topographies to control Bacteria ... [https://www.nature.com/articles/s41598-025-08415-2]
- 82. Spatially-Localized Functionalization on Nanostructured for... Surfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC9609756/]
- 83. Fast bacterial growth reduces antibiotic accumulation and efficacy [https://elifesciences.org/articles/74062]
- 84. New metrics for describing atomic force microscopy data of... | CoLab [https://colab.ws/articles/10.1016%2Fj.apsusc.2024.160640]