Navigating the Double-Edged Sword: A Comprehensive Guide to Nanoparticle Cytotoxicity and Immunogenic Response for Advanced Therapeutics
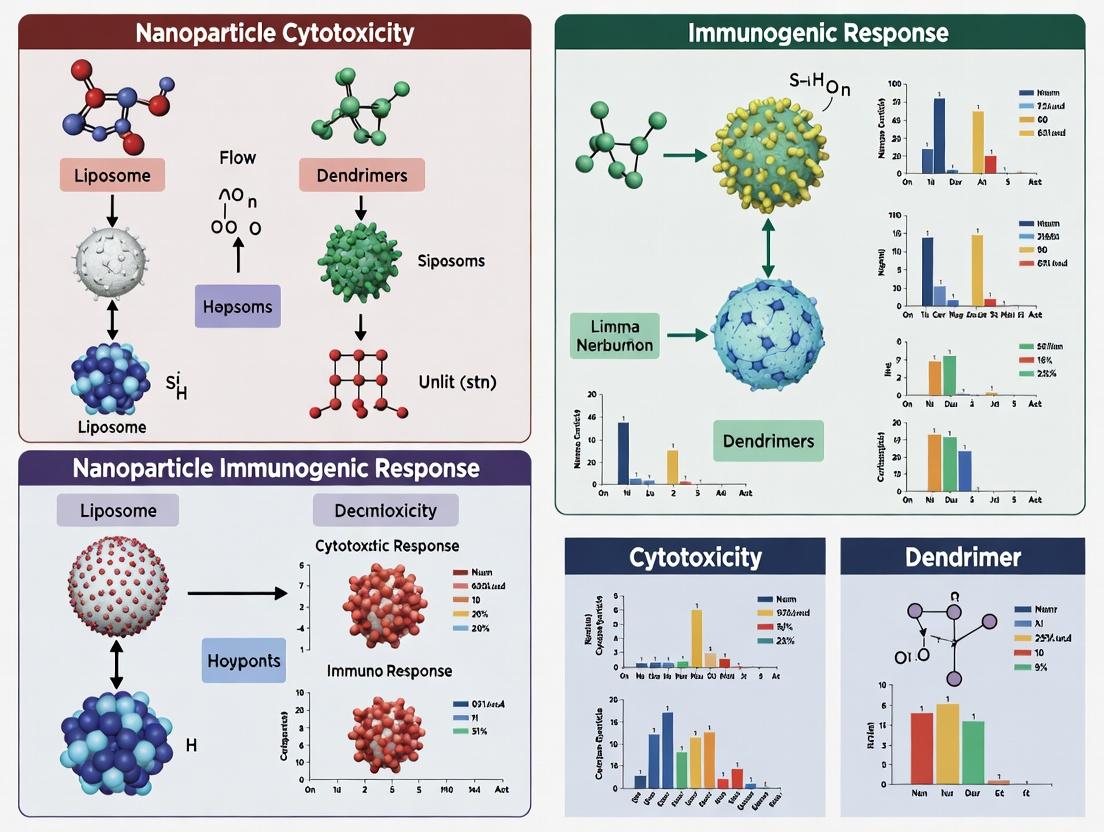
This article provides a detailed scientific and technical analysis of nanoparticle-induced cytotoxicity and immunogenicity, critical challenges in nanomedicine development.
Navigating the Double-Edged Sword: A Comprehensive Guide to Nanoparticle Cytotoxicity and Immunogenic Response for Advanced Therapeutics
Abstract
This article provides a detailed scientific and technical analysis of nanoparticle-induced cytotoxicity and immunogenicity, critical challenges in nanomedicine development. Designed for researchers, scientists, and drug development professionals, the content explores the foundational mechanisms of nanotoxicity, outlines robust in vitro and in vivo assessment methodologies, offers strategies for troubleshooting and optimizing nanoparticle design to mitigate adverse responses, and compares validation frameworks. By synthesizing the latest research, this guide aims to equip professionals with the knowledge to balance therapeutic efficacy with biocompatibility, accelerating the translation of safer nanotherapeutics into clinical applications.
Understanding the Roots of Nanotoxicity: Core Mechanisms Driving Nanoparticle Cytotoxicity and Immunogenicity
Technical Support Center: Troubleshooting Nanoparticle Cytotoxicity Assays
Troubleshooting Guides
Guide 1: Inconsistent ROS Detection Results
- Symptom: High variability in fluorescent signal (e.g., DCFH-DA, DHE) between replicates.
- Common Causes & Solutions:
- Nanoparticle Interference: Some NPs quench fluorescence or auto-oxidize the probe.
- Action: Include a control where dye is incubated with NPs but not cells. Use plate readers with rapid kinetic cycles.
- Uneven Nanoparticle Settling: Leads to varying cellular dose.
- Action: Standardize plate rocking during incubation or use well-characterized dispersion protocols (e.g., with serum albumin).
- Probe Overloading/Photobleaching: Inaccurate measurement.
- Action: Titrate dye concentration; reduce exposure time during imaging.
- Nanoparticle Interference: Some NPs quench fluorescence or auto-oxidize the probe.
Guide 2: Poor Membrane Integrity Assay Reproducibility
- Symptom: High background or low signal in LDH release or PI uptake assays.
- Common Causes & Solutions:
- NP-Enzyme/Assay Interference: NPs can adsorb LDH enzyme or react with assay components.
- Action: Always include an NP-only control with assay reagents. Centrifuge samples thoroughly to pellet NPs before LDH assay.
- Serum Enzyme Contamination: FBS contains endogenous LDH.
- Action: Wash cells thoroughly with PBS before assay initiation. Use low-serum or serum-free media during NP exposure.
- Timing Issues: Membrane damage may be transient or late.
- Action: Perform time-course experiments (e.g., 4, 8, 24h).
- NP-Enzyme/Assay Interference: NPs can adsorb LDH enzyme or react with assay components.
Guide 3: Weak or No Genotoxicity Signal
- Symptom: Low γ-H2AX foci count or comet tail moment despite evidence of oxidative stress.
- Common Causes & Solutions:
- Insufficient Damage or Repair: Damage may be below detection threshold or rapidly repaired.
- Action: Optimize NP dose and exposure time. Consider using repair inhibitors (e.g., PARP inhibitors for base excision repair) as a positive control.
- Fixation/Permeabilization Issues: Antibodies cannot access nuclear antigens.
- Action: Validate protocol with a known genotoxicant (e.g., etoposide, H₂O₂). Titrate Triton X-100 concentration.
- NP-Induced Artifacts in Comet Assay: NPs can cause physical DNA dragging.
- Action: Run an NP-only gel to check for "comet-like" artifacts. Use enzymes (e.g., FPG) to detect specific oxidation.
- Insufficient Damage or Repair: Damage may be below detection threshold or rapidly repaired.
Frequently Asked Questions (FAQs)
Q1: How do I choose the most relevant assay for detecting NP-induced oxidative stress? A: The choice depends on the ROS type and compartment. Use a panel:
- General ROS: DCFH-DA (cytosolic).
- Superoxide: Dihydroethidium (DHE) with HPLC validation for specificity.
- Mitochondrial ROS: MitoSOX Red.
- Glutathione depletion: Monochlorobimane assay.
- Always confirm with a direct antioxidant (e.g., N-acetylcysteine) rescue experiment.
Q2: Our nanoparticles aggregate heavily in cell culture media, skewing dose-response. How can we improve dispersion? A: Standardized dispersion is critical.
- Pre-disperse NPs in sterile 0.1-1% BSA or serum-free media via probe sonication (calibrated energy/time, ice bath).
- Immediately add this stock to complete culture media with serum. Serum proteins act as biocoronas, stabilizing dispersion.
- Characterize the hydrodynamic diameter and PDI in the exact exposure medium using dynamic light scattering (DLS). Report this as the administered dose metric.
Q3: What are the critical controls for proving NP-induced genotoxicity is specific? A: Essential controls include:
- Negative Control: Untreated cells & dispersion media control (e.g., BSA in media).
- Positive Control: Known genotoxicant (e.g., 50 µM Etoposide for 4h for γ-H2AX).
- Nanomaterial Controls: i) Internalized but inert material (e.g., silica-coated non-reactive NPs) to check for physical interference. ii) NP + potent antioxidant (NAC) to link genotoxicity to ROS.
- Sham Control: For magnetic/light-activated NPs, apply the activating field without NPs.
Q4: How can we distinguish between primary (direct) and secondary (inflammation-mediated) genotoxicity? A: Implement a co-culture or conditioned media approach.
- Treat immune cells (e.g., THP-1 macrophages) with NPs.
- After 24h, collect the conditioned media, centrifuge to remove NPs, and apply to target cells (e.g., epithelial cells).
- Compare genotoxicity in target cells from direct NP exposure vs. conditioned media exposure. An effect from conditioned media indicates secondary, inflammation-driven damage.
Table 1: Common Assays for Nanoparticle-Induced Damage Pathways
| Damage Pathway | Key Assays | Readout | Typical Positive Control | Common Pitfalls |
|---|---|---|---|---|
| Oxidative Stress | DCFH-DA fluorescence | General ROS | 100-500 µM tert-Butyl hydroperoxide | Dye auto-oxidation, NP quenching |
| DHE/HPLC | Superoxide (O₂⁻) | Antimycin A (1-10 µM) | Non-specific oxidation to ethidium | |
| GSH/GSSG ratio | Redox state | Diamide (1 mM) | Rapid auto-oxidation of samples | |
| Membrane Disruption | LDH release | Cytotoxicity | 1% Triton X-100 | Serum LDH, NP interference |
| Propidium Iodide uptake | Membrane permeability | 70% Ethanol | NP auto-fluorescence | |
| Annexin V/PI staining | Apoptosis/Necrosis | Staurosporine (1 µM) | Timing-dependent results | |
| Genotoxicity | γ-H2AX foci microscopy | DNA double-strand breaks | Etoposide (50 µM, 4h) | Foci counting subjectivity |
| Alkaline Comet Assay | DNA strand breaks | Methyl methanesulfonate (100 µM) | NP-induced dragging artifacts | |
| Micronucleus (Cytokinesis-block) | Chromosomal damage | Mitomycin C (0.1 µg/mL) | Inadequate cytochalasin B concentration |
Table 2: Example Dose-Response Data for Common Nanomaterials (In Vitro)
| Nanomaterial | Size (nm) | Cell Line | Oxidative Stress (EC₅₀, µg/mL) | Membrane Damage (EC₅₀, µg/mL) | Genotoxicity (Lowest Observed Effect Level, µg/mL) |
|---|---|---|---|---|---|
| Citrate-capped Ag NPs | 20 | A549 | 5-10 (DCF) | 10-15 (LDH) | 2.5 (γ-H2AX) |
| TiO₂ (Anatase) NPs | 30 | BEAS-2B | 50-100 (DHE) | >200 (LDH) | 50 (Comet Assay) |
| Multi-Walled Carbon Nanotubes | 10x5000 | THP-1 | 20-50 (DCF) | 50-100 (LDH) | 10 (Micronucleus) |
| Polymer-coated ZnO NPs | 50 | HepG2 | 5-15 (MitoSOX) | 10-20 (LDH) | 5 (γ-H2AX) |
EC₅₀: Half-maximal effective concentration. Data is representative and highly dependent on surface modification, dispersion, and cell type.
Experimental Protocols
Protocol 1: Standardized Nanoparticle Dispersion for Cell Exposure
- Weigh NP powder in a sterile tube.
- Add sterile 0.1% BSA in PBS (or serum-free medium).
- Sonicate using a probe sonicator (e.g., 30% amplitude, 5 min, pulsed 1s on/1s off) on ice to prevent heating.
- Dilute the stock immediately into complete cell culture medium to the highest treatment concentration.
- Serially dilute in complete medium to create dose range. Vortex each dilution briefly.
- Characterize the primary dose solution (hydrodynamic size, PDI, zeta potential) via DLS.
Protocol 2: Intracellular ROS Measurement using DCFH-DA
- Seed cells in a black-walled, clear-bottom 96-well plate.
- Treat with NPs for desired time.
- Wash cells with PBS.
- Load with 10 µM DCFH-DA in serum-free, phenol-red-free medium for 30 min at 37°C.
- Wash 3x with PBS to remove extracellular dye.
- Add fresh phenol-red-free medium and immediately read fluorescence (Ex/Em: 485/535 nm) on a plate reader, taking kinetic readings every 5-10 min for 1h.
- Normalize fluorescence to protein content (e.g., via Bradford assay).
Protocol 3: Cytokinesis-Block Micronucleus Assay
- Seed cells (e.g., CHO, HepG2) in 6-well plates and allow to attach.
- Treat with NPs for 24h.
- Add Cytochalasin B (final conc. 3-6 µg/mL) to block cytokinesis.
- Continue incubation for an additional 28h (total cytochalasin B exposure: 28h).
- Harvest cells by trypsinization, hypotonic treatment (0.075 M KCl), and fix in 3:1 methanol:acetic acid.
- Drop cells onto slides, air dry, and stain with Giemsa or DNA-specific dye (e.g., DAPI).
- Score micronuclei in binucleated cells only (minimum 1000 BN cells per treatment).
Visualization: Pathways & Workflows
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Supplier Examples | Primary Function in NP Toxicity Studies |
|---|---|---|
| DCFH-DA / CM-H2DCFDA | Thermo Fisher, Sigma-Aldrich | Cell-permeable probe for general intracellular ROS detection. |
| MitoSOX Red | Thermo Fisher | Mitochondria-targeted fluorogenic dye for superoxide detection. |
| CellTox Green Cytotoxicity Assay | Promega | Real-time, fluorescent dye that stains DNA of dead cells (membrane-compromised). |
| Cytokine Profiling ELISA/Multiplex Array | R&D Systems, Bio-Rad | Quantifies secreted inflammatory cytokines (IL-1β, IL-6, TNF-α) indicating immunogenic response. |
| γ-H2AX (phospho-S139) Antibody | MilliporeSigma, Cell Signaling | Gold-standard immunofluorescence marker for DNA double-strand breaks. |
| CometAssay Kit | Trevigen, Abcam | All-in-one kit for standardized single-cell gel electrophoresis (alkaline or neutral conditions). |
| Recombinant Human Albumin (rHA) | Novozymes, Sigma | Protein source for NP dispersion without batch variability of serum-derived BSA. |
| N-Acetylcysteine (NAC) | Sigma-Aldrich | Broad-spectrum antioxidant used in rescue experiments to confirm ROS-mediated effects. |
| Cytochalasin B | Sigma-Aldrich, Tocris | Inhibitor of actin polymerization; essential for cytokinesis-block micronucleus assay. |
| Zeta Potential Reference Standard | Malvern Panalytical | Calibration standard for accurate surface charge measurement of NPs in suspension. |
Technical Support Center
Troubleshooting Guides & FAQs
Category 1: Protein Corona & Characterization Issues
Q1: Our DLS measurements show highly variable hydrodynamic sizes after incubating nanoparticles (NPs) in plasma. What could be causing this inconsistency?
- A: Inconsistent protein corona formation is the likely cause. Ensure the plasma/serum source and concentration are identical across replicates. Pre-incubation temperature and time must be rigorously controlled (e.g., 37°C for 60 min). Filter the biological fluid through a 0.22 µm filter before use to remove aggregates. Always use a consistent vortexing or mixing protocol post-incubation before DLS measurement.
Q2: SDS-PAGE of the hard corona shows smearing instead of distinct bands. How can we improve resolution?
- A: Smearing indicates incomplete elution or protein degradation. Optimize your elution buffer: increase SDS concentration to 4%, add a chaotropic agent (2M urea), and boil samples for 10 minutes, not 5. Ensure you are centrifuging at 100,000 x g for 1 hour at 4°C to firmly pellet NPs with the hard corona before washing. Overloading the gel can also cause smearing; try serial dilutions of your eluate.
Category 2: Inflammasome Activation & Cell Assays
Q3: We cannot detect significant IL-1β release from THP-1 macrophages despite using a known inflammasome activator (e.g., LPS + nigericin) as a positive control.
- A: First, confirm your THP-1 differentiation protocol. Cells must be treated with 100 nM PMA for 48-72 hours, followed by a 24-hour rest period in standard medium for proper maturation into macrophages. For canonical NLRP3 priming, use 10-100 ng/mL Ultrapure LPS for 3-4 hours. The activator (e.g., NPs) must then be added for a sufficient duration (6-24h). Always measure cell viability (LDRAssay) concurrently, as high cytotoxicity can paradoxically reduce IL-1β release.
Q4: Our negative control (PBS) is showing background caspase-1 activity in our FLICA assay.
- A: This is typically due to residual FLICA reagent. Increase the number of post-staining washes from 2 to 4 using the provided apoptosis wash buffer. Ensure you are using a plate reader with appropriate filters (Ex/Em ~492/520 nm for FAM-FLICA). Prepare a "No FLICA" control for each condition to autofluorescence.
Category 3: Complement Activation
Q5: Our ELISA for complement activation fragment C3a shows high background in all samples, including buffer-only controls.
- A: Human serum is rich in pre-formed C3a. You must use serum that has been freshly prepared and aliquoted, never previously freeze-thawed more than twice. Run a "serum-only" control (serum + buffer) and subtract its value from your NP-treated samples to calculate NP-specific activation. Ensure your stop solution is added at the exact time specified in the protocol.
Q6: How do we differentiate between the classical, lectin, and alternative pathway activation by our NPs?
- A: You need pathway-specific functional assays. Use cation depletion (Ca²⁺ chelation with EGTA blocks classical/lectin, leaving alternative) or pathway-specific complement-deficient sera (e.g., C1q-, C2-, or Factor B-deficient). Measure the endpoint (e.g., C5a generation, CH50) in these conditions versus normal human serum. See Table 2 for a summary.
Experimental Protocols
Protocol 1: Isolation and Analysis of the Hard Protein Corona
- Incubation: Incubate 1 mg/mL of NPs in 50% (v/v) human serum in PBS (total vol 1 mL) at 37°C for 1 hour with gentle rotation.
- Separation: Ultracentrifuge the mixture at 100,000 x g for 60 minutes at 4°C.
- Wash: Carefully discard supernatant. Resuspend pellet in 1 mL of ice-cold PBS. Repeat ultracentrifugation step twice.
- Elution: Resuspend final pellet in 100 µL of 2x Laemmli buffer (with 4% SDS and 5% β-mercaptoethanol). Boil for 10 minutes at 95°C.
- Analysis: Centrifuge at 16,000 x g for 5 min. Load supernatant onto a 4-20% gradient SDS-PAGE gel. Perform Coomassie staining or western blot for proteins of interest (e.g., IgG, albumin, fibrinogen, apolipoproteins).
Protocol 2: Assessing NLRP3 Inflammasome Activation in Primed Macrophages
- Cell Preparation: Differentiate THP-1 cells in 96-well plates (10⁵ cells/well) with 100 nM PMA for 48h. Rest for 24h in fresh RPMI-1640 + 10% FBS.
- Priming: Prime cells with 100 ng/mL Ultrapure LPS in serum-free medium for 3 hours.
- Activation: Treat primed cells with NPs (a range of 10-100 µg/mL) or controls (5 µM nigericin for positive, PBS for negative) for 6 hours.
- Analysis: Collect supernatant. Measure IL-1β via ELISA. In parallel, assay for cytotoxicity using LDH release. For intracellular caspase-1, use a FLICA assay according to manufacturer instructions.
Data Presentation
Table 1: Common Protein Corona Components and Their Implications
| Protein Identified | Molecular Weight (kDa) | Abundance Rank (Typical) | Potential Immunogenic Consequence |
|---|---|---|---|
| Human Serum Albumin | 66.5 | 1 (High) | Can mask NP surface, reducing recognition ("stealth effect"). |
| Immunoglobulin G (IgG) | 150 | 2-3 (Medium-High) | Opsonization; can engage Fc receptors on immune cells. |
| Fibrinogen | 340 | Variable (Medium) | Potent activator of macrophages via Mac-1 integrin. |
| Apolipoprotein E (ApoE) | 34 | Variable (Low-Medium) | Influences hepatic clearance and cellular uptake. |
| Complement C3 | 185 | Variable (Low) | Presence indicates complement activation potential. |
Table 2: Key Assays for Immunogenicity Profiling
| Assay Target | Example Assay | Key Readout | Typical Values for "Positive" Control |
|---|---|---|---|
| Protein Corona | SDS-PAGE / LC-MS | Protein band intensity / # of unique IDs | ~30-100 distinct proteins identified. |
| Inflammasome Activation | IL-1β ELISA (cell supernatant) | Concentration (pg/mL) | Nigericin: >500 pg/mL vs. PBS: <20 pg/mL. |
| Complement Activation | C3a Des Arg ELISA (serum) | Concentration (ng/mL) | Zymosan (100 µg/mL): >2000 ng/mL increase over serum baseline. |
| Cell Viability | LDH Release | % Cytotoxicity | Triton X-100 (1%): ~95-100% cytotoxicity. |
Diagrams
Diagram 1: NP Immunogenicity Pathways Overview
Title: Three Key Pathways of Nanoparticle Immunogenicity
Diagram 2: NLRP3 Inflammasome Activation Workflow
Title: Stepwise NLRP3 Inflammasome Activation by NPs
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Immunogenicity Research |
|---|---|
| Ultrapure Lipopolysaccharide (LPS) | Standard agonist for "priming" the NLRP3 inflammasome via TLR4. Ensures activation is specific to Signal 2. |
| Nigericin (or ATP) | Positive control for NLRP3 inflammasome activation (induces K+ efflux). Validates assay functionality. |
| Human AB Serum (Pooled) | Standardized serum source for in vitro protein corona and complement studies, reducing donor variability. |
| EGTA/Mg²⁺ Buffer | Selective chelator (EGTA binds Ca²⁺, not Mg²⁺). Used to inhibit Classical/Lectin complement pathways. |
| Pathway-Specific Complement-Deficient Sera (e.g., C1q-, Factor B-) | Critical for identifying the specific complement activation pathway (Classical vs. Alternative). |
| FLICA Caspase-1 Assay Kit (FAM-YVAD-FMK) | Fluorescent probe for in situ detection of active caspase-1 in live cells. |
| LDH Cytotoxicity Assay Kit | Essential parallel measurement to distinguish specific immune activation from general cell death. |
| Polymeric NPs (e.g., PS, PLGA) | Common benchmark/control particles with well-characterized surface chemistry for comparison. |
Technical Support Center
Troubleshooting Guide & FAQs
Q1: My nanoparticles are aggregating in biological media (e.g., cell culture medium, serum). How can I improve their colloidal stability? A: Aggregation is commonly due to high ionic strength neutralizing surface charge or hydrophobic interactions. To troubleshoot:
- Check Surface Charge (Zeta Potential): Measure the zeta potential in your biological media, not just in water. A value between -30 mV and +30 mV indicates instability. A magnitude > |30| mV suggests good electrostatic stability.
- Assess Hydrophobicity: Use hydrophobic interaction chromatography or dye-binding assays (e.g., Rose Bengal). High hydrophobicity leads to protein corona formation and aggregation.
- Solutions:
- Increase Steric Stabilization: Coat nanoparticles with polyethylene glycol (PEG), polysorbate 80, or other polymers.
- Optimize Surface Charge: For cationic particles causing serum protein aggregation, consider modifying with anionic or neutral coatings.
- Use Freshly Prepared Suspensions: Sonicate particles immediately before use and avoid long incubation times in complex media.
Q2: I am observing unexpectedly high cytotoxicity. Which physicochemical parameter should I investigate first? A: Surface charge is often the primary culprit for acute cytotoxicity, especially cationic charge.
- Primary Investigation: Measure the zeta potential of your nanoparticles in the relevant biological buffer. Strongly cationic surfaces (e.g., > +20 mV) can disrupt cell membranes via electrostatic interactions.
- Secondary Investigation: Evaluate size. Very small nanoparticles (< 5 nm) can cause toxicity by penetrating organelles and generating reactive oxygen species (ROS).
- Protocol: LDH Release Assay for Membrane Damage:
- Seed cells in a 96-well plate.
- Treat with nanoparticle samples and controls for 24h.
- Centrifuge plate, transfer supernatant to a new plate.
- Add LDH assay reagent (containing lactate, INT, diaphorase, NAD+) and incubate for 30 min.
- Measure absorbance at 490 nm and 680 nm (reference). High LDH release correlates with membrane damage from charged or sharp nanoparticles.
Q3: My nanoparticles are not being internalized by the target immune cells (e.g., macrophages). What could be the issue? A: This is likely governed by size, shape, and surface properties.
- Size: For phagocytosis by macrophages, optimal particle size is 1-3 µm. Nanoparticles (< 200 nm) may require opsonization or specific targeting ligands.
- Shape: Macrophages internalize spherical particles more efficiently than high-aspect-ratio rods or fibers.
- Surface Hydrophobicity/Charge: Hydrophobic and charged surfaces are more readily opsonized and recognized by scavenger receptors.
- Experiment to Test: Perform a flow cytometry-based uptake assay using fluorescently labeled nanoparticles. Pre-treat cells with inhibitors for different pathways (e.g., cytochalasin D for phagocytosis, chlorpromazine for clathrin-mediated endocytosis) to determine the entry mechanism.
Q4: How do I systematically test the immunogenic potential (e.g., NLRP3 inflammasome activation) of my nanoparticle library? A: Inflammasome activation is highly sensitive to particle size, shape, and hydrophobicity.
- Key Assay: IL-1β secretion ELISA from primary human macrophages. NLRP3 activation leads to pro-IL-1β cleavage and secretion.
- Required Controls: Use LPS priming (signal 1) alone, ATP (a known NLRP3 activator) as a positive control, and a negative control nanoparticle (e.g., plain PEG-coated).
- Expected Trends: Needle-like shapes, crystalline structures (e.g., silica), and hydrophobic surfaces are potent activators. Small spherical, smooth, hydrophilic particles are typically less activating.
Table 1: Impact of Physicochemical Properties on Biological Responses
| Determinant | Typical Range Tested | Key Biological Response | Experimental Readout |
|---|---|---|---|
| Size | 5 nm - 200 nm (drug delivery) | Cellular uptake efficiency, biodistribution, renal clearance | Flow cytometry (% positive cells), ICP-MS (tissue accumulation) |
| 0.5 µm - 3 µm (vaccines) | Phagocytosis, inflammasome activation | Confocal microscopy, IL-1β ELISA | |
| Shape | Spheres, Rods (AR 1-8), Disks | Cell entry mechanism, circulation time, immunogenicity | Inhibitor studies, IVIS imaging, cytokine array |
| Surface Charge (Zeta Potential) | -50 mV to +50 mV | Serum stability, cytotoxicity, protein corona composition | DLS, LDH/MTS assay, proteomics |
| Hydrophobicity | Log P, Contact Angle | Protein adsorption, clearance by MPS, inflammatory response | HIC, 2D-DIGE, neutrophil recruitment in vivo |
Table 2: Common Characterization Techniques
| Parameter | Primary Technique(s) | Sample Preparation Tip |
|---|---|---|
| Hydrodynamic Size & PDI | Dynamic Light Scattering (DLS) | Always measure in the same medium used for biological tests. Filter samples (0.22 µm). |
| Shape & Morphology | Transmission Electron Microscopy (TEM) | Use compatible grids (e.g., carbon-coated), stain if necessary (uranyl acetate). |
| Surface Charge | Zeta Potential (Laser Doppler Velocimetry) | Use appropriate electrolyte concentration (e.g., 1 mM KCl) and pH adjustment. |
| Surface Hydrophobicity | Hydrophobic Interaction Chromatography (HIC) | Use a phenyl or butyl column with a descending salt gradient. |
Experimental Protocols
Protocol 1: Determining Protein Corona Composition Objective: To identify proteins adsorbed onto nanoparticles from biological fluids. Materials: Nanoparticles, complete cell culture medium with 10% FBS, ultracentrifuge, SDS-PAGE/western blot or LC-MS/MS reagents. Steps:
- Incubate nanoparticles (100 µg/mL) in complete medium at 37°C for 1h.
- Centrifuge at 100,000 x g for 1h at 4°C to pellet nanoparticle-protein corona complexes.
- Carefully remove supernatant and wash pellet gently with cold PBS. Repeat centrifugation.
- Resuspend pellet in Laemmli buffer for SDS-PAGE/western blot analysis of specific proteins (e.g., ApoE, albumin, immunoglobulins) or in urea buffer for trypsin digestion and LC-MS/MS.
Protocol 2: In Vitro Hemolysis Assay for Cytotoxicity Screening Objective: To rapidly assess the membrane-lytic potential of nanoparticles, linked to surface charge and hydrophobicity. Materials: Fresh human or animal red blood cells (RBCs), PBS, Triton X-100 (1% v/v, positive control), nanoparticles. Steps:
- Wash RBCs 3x with PBS and prepare a 5% v/v suspension.
- Incubate 100 µL of RBC suspension with 100 µL of nanoparticle solutions (serial dilutions in PBS) for 1h at 37°C.
- Centrifuge at 500 x g for 5 min.
- Measure absorbance of supernatant at 540 nm (peak for hemoglobin).
- Calculate % hemolysis: [(Abssample - AbsPBS) / (AbsTritonX100 - AbsPBS)] * 100. >5% hemolysis indicates significant membrane disruption.
Diagrams
Title: Biological Fate Dictated by Nanoparticle Size
Title: Nanoparticle-Induced NLRP3 Inflammasome Activation
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Nanotoxicity/Immunogenicity Research |
|---|---|
| Dynabeads (Various Sizes/Coats) | Model particles with controlled size and surface chemistry for comparative uptake and activation studies. |
| CellROX Green/Orange Reagent | Flow cytometry or fluorescence microscopy probe for detecting nanoparticle-induced reactive oxygen species (ROS). |
| Cytochalasin D | Pharmacologic inhibitor of actin polymerization; used to confirm phagocytic uptake pathways. |
| Recombinant Human/Mouse Cytokine ELISA Kits (IL-1β, TNF-α, IL-6) | Gold-standard for quantifying specific inflammatory cytokine release from immune cells. |
| PEG-SH (Thiol-Polyethylene Glycol) | Common reagent for "PEGylating" and shielding gold, iron oxide, or other metallic nanoparticles to reduce protein binding and immunogenicity. |
| Polystyrene Nanoparticles (Fluorescent, Carboxyl/Amine-modified) | Commercially available standards with uniform size for calibrating instruments and as controls in uptake experiments. |
| Pierce LDH Cytotoxicity Assay Kit | Colorimetric assay for quantifying membrane integrity damage, a key endpoint for cationic nanoparticle toxicity. |
| Albumin from Bovine Serum (BSA), Fraction V | Used as a model "corona" protein or as a blocking/passivating agent to reduce non-specific nanoparticle interactions. |
Technical Support Center: Troubleshooting for Integrated Omics and Imaging in Nanotoxicology
Thesis Context: This support content is designed for researchers investigating the mechanistic basis of nanoparticle (NP)-induced cytotoxicity and immunogenic responses, utilizing integrated omics and high-resolution imaging to deconvolute complex biological interactions.
Frequently Asked Questions (FAQs)
Q1: During a multi-omics workflow (transcriptomics & proteomics) on NP-treated macrophages, I find poor correlation between mRNA and protein expression levels for key inflammatory markers. What are potential causes and solutions?
A1: This is a common challenge. Causes and troubleshooting steps are summarized below:
| Potential Cause | Diagnostic Check | Recommended Solution |
|---|---|---|
| Post-Transcriptional Regulation | Check miRNA/siRNA expression data from sequencing. | Integrate miRNA-seq or perform ribosome profiling (Ribo-seq) to assess translation efficiency. |
| Protein Turnover/Degradation Rates | Review proteasome/autophagy pathway activity in proteomics data. | Use pulsed SILAC (Stable Isotope Labeling by Amino acids in Cell culture) to measure protein half-lives. |
| Technical Discrepancy in Sample Timing | Verify harvest times are identical for both analyses. | Standardize: harvest all samples for omics at the exact same post-exposure time point. |
| NP Interference with Assay Kits | Run a spike-in control with known protein/mRNA concentration. | Include an extra purification step (e.g., column-based cleanup) post-lysis to remove NP residues. |
Q2: In live-cell imaging of mitochondrial depolarization (using JC-1 dye) following NP exposure, I observe inconsistent dye aggregation/ratio values. How can I resolve this?
A2: Inconsistencies often stem from NP-dye interactions or imaging protocol issues.
| Issue | Troubleshooting Step | Protocol Adjustment |
|---|---|---|
| NP Adsorption of Dye | Image a dye-only control with NPs. | Pre-incubate NPs with serum-containing media to form a corona before adding dye-loaded cells. |
| Photobleaching/J-aggregate Instability | Check intensity loss over time in control wells. | Reduce illumination intensity/time, use a neutral density filter, and take rapid sequential images. |
| Variable NP Settling | Check focal plane for uneven cell layers. | Use a gentle, continuous agitation system during exposure or plate cells on a confocal dish with a #1.5 coverglass bottom. |
Q3: When integrating single-cell RNA sequencing (scRNA-seq) data with high-resolution immunofluorescence images for spatial context, how do I align the two datasets from the same sample?
A3: Use a computational anchor-based integration workflow.
- Experimental Protocol:
- Sample Preparation: Split your NP-treated cell population (e.g., primary immune cells).
- Portion A: Process for scRNA-seq using a standard 10x Genomics protocol.
- Portion B: Seed onto imaging chamber slides, fix, and stain with a panel of 5-10 antibodies for key markers (e.g., CD45, CD68, MHC-II, TNF-α).
- Imaging: Acquire high-resolution (60x) multi-channel images. Extract cell-specific expression values for the antibody panel (mean fluorescence intensity per cell).
- Computational Integration:
- Create a "pseudo-bulk" reference from the scRNA-seq data for the antibody-target genes.
- Use tools like Seurat's
FindTransferAnchorsor Tangram to map the scRNA-seq data onto the spatial positions of imaged cells based on the shared antibody/transcript features.
The Scientist's Toolkit: Research Reagent Solutions
| Item Name | Function/Application in NP Cytotoxicity Research |
|---|---|
| LIVE/DEAD Viability/Cytotoxicity Kit (Invitrogen) | Distinguishes live (calcein-AM, green) from dead (ethidium homodimer-1, red) cells in real-time after NP exposure. |
| CellROX Deep Red Oxidative Stress Reagent | Fluorogenic probe for measuring reactive oxygen species (ROS) in live cells via high-content imaging or flow cytometry. |
| Olink Target 96 Inflammation Panel | Multiplex, antibody-based proteomics assay for 92 inflammatory proteins from small sample volumes; ideal for supernatant from NP-treated cells. |
| MitoTracker Deep Red FM | Cell-permeant dye that stains mitochondria in live cells; useful for tracking mitochondrial morphology and localization upon NP insult. |
| Nucleofector Technology (Lonza) | Enables high-efficiency transfection of hard-to-transfect primary immune cells (e.g., macrophages) for CRISPR or reporter gene assays. |
| Cytiva Biacore Series S CMS Chip | Surface plasmon resonance (SPR) sensor chip to characterize the kinetics of NP or protein corona binding to immune receptors (e.g., TLRs). |
| Nanoparticle Tracking Analysis (NTA) System (Malvern) | Measures NP size distribution and concentration in complex biological fluids (serum, BALF) prior to cell exposure. |
Table 1: Omics Signatures Associated with High-Cytotoxicity vs. Low-Cytotoxicity Nanoparticles (from Integrated Studies)
| Parameter | High-Cytotoxicity NPs (e.g., Cationic PS, certain metal oxides) | Low-Cytotoxicity NPs (e.g., PEGylated Liposomes, Silica-coated) |
|---|---|---|
| Transcriptomic Hallmark (Pathway Enrichment) | NLRP3 inflammasome activation, p53 pathway, ER stress/UPR | Nrf2-mediated oxidative stress response, xenobiotic metabolism |
| Proteomic Shift (Upregulated Proteins) | IL-1β, Caspase-1, HMGB1, Phospho-eIF2α | HO-1, SOD2, GSTP1, Catalase |
| Metabolomic Profile (LC-MS) | Depleted glutathione, increased succinate, lactate | Stable glutathione levels, normal TCA cycle intermediates |
| Characteristic Imaging Phenotype | Mitochondrial fragmentation, lysosomal membrane permeabilization, plasma membrane blebbing | Intact mitochondrial network, autophagosome formation, stable lysosomes |
Detailed Experimental Protocols
Protocol: Correlative Light and Electron Microscopy (CLEM) for Visualizing NP Intracellular Fate
- Objective: To track the subcellular localization of immunogenic NPs and associate it with organelle damage.
- Steps:
- Labeling: Incubate NPs (e.g., 50 µg/mL) with a fluorescent tag (e.g., Cy5) for 1 hour. Purify via centrifugal filter.
- Cell Treatment: Seed primary dendritic cells on a MatTek grid-bottom dish. Expose to labeled NPs for the desired time (e.g., 4h).
- Live-Cell Imaging: Using a confocal microscope with an environmental chamber, locate a cell of interest and capture a Z-stack of the fluorescence signal.
- Fixation: Immediately fix cells in situ with 2.5% glutaraldehyde/2% PFA in 0.1M cacodylate buffer.
- EM Processing: Post-fix in 1% osmium tetroxide, dehydrate in ethanol, and embed in EPON resin directly on the dish.
- Sectioning & Imaging: Using the fluorescent map, trim the block to the region of interest. Cut 70-nm ultrathin sections. Acquire TEM images.
- Correlation: Use software (e.g., IMOD) to align the light and electron microscopy images.
Signaling Pathways and Workflows
(Diagram Title: NP-Induced Cytotoxicity & Immunogenicity Cascade)
(Diagram Title: Integrated Omics-Imaging Experimental Workflow)
From Bench to Bedside: Standardized Methods for Assessing Nanoparticle Safety and Immune Activation
Essential In Vitro Assays for Cytotoxicity (MTT/XTT, LDH, Apoptosis/Necrosis Markers, ROS Detection)
Welcome to the Technical Support Center. This guide is designed to support researchers working within the critical field of nanoparticle cytotoxicity and immunogenic response, providing troubleshooting and FAQs for key in vitro assays.
Troubleshooting Guides & FAQs
MTT/XTT Assay Section
Q1: My formazan crystals are not dissolving properly after adding the solubilization solution, leading to high background and inconsistent readings. What could be wrong? A: This is a common issue. Potential causes and solutions include:
- Cause 1: Insufficient incubation time with the solubilization solution (typically DMSO or SDS-based).
- Solution: Increase incubation time (e.g., extend to 4-6 hours) on an orbital shaker, protected from light.
- Cause 2: Evaporation of culture medium during the MTT incubation, causing crystal precipitation in dry areas.
- Solution: Ensure plates are sealed with parafilm during the MTT incubation step and humidity is maintained.
- Cause 3: Nanoparticle interference. Some nanoparticles can directly reduce MTT or adsorb the formazan product.
- Solution: Include critical controls: wells with nanoparticles but no cells, and wells with nanoparticles in complete medium. Centrifuge plates before measuring absorbance to pellet insoluble nanoparticles/interfering materials.
Q2: I observe unexpected stimulation of metabolic activity (increased signal) at low nanoparticle concentrations. Is this real or an artifact? A: While low-dose stimulation (hormesis) is possible, nanoparticle interference is more likely.
- Artifact Cause: Certain nanomaterials (e.g., carbon-based, some metal oxides) can catalyze the reduction of MTT/XTT tetrazolium salts independent of cellular enzymes.
- Troubleshooting: Perform the "nanoparticle-only" control as stated above. Consider switching to a different assay (e.g., LDH, ATP) for validation. For XTT, ensure the electron coupling reagent is fresh and properly mixed.
LDH Assay Section
Q3: The LDH release in my positive control (Triton X-100 treated) is lower than expected, indicating poor assay sensitivity. A: This suggests suboptimal cell lysis or reagent issues.
- Solution 1: Verify the concentration and incubation time of the lysis agent. For robust cell lines, increasing Triton X-100 to 1-2% or extending lysis time to 45-60 minutes may be necessary.
- Solution 2: Check reagent stability. The NAD+ substrate and dye mixture are often light and temperature sensitive. Prepare fresh or use a commercially available, validated kit.
- Protocol Reminder: After adding the lysis solution, visually confirm cell detachment under a microscope.
Q4: How do I differentiate between apoptotic and necrotic LDH release in nanoparticle-treated cells? A: Standard LDH measures total plasma membrane damage. To differentiate:
- Experimental Setup: At your assay timepoint, collect two sets of supernatant: 1) Spontaneous LDH (from wells with untreated/media-changed cells). 2) Total LDH (from wells where you add lysis buffer at the end to release all remaining LDH).
- Calculation: Necrotic Release (%) = (Spontaneous LDH from treated wells / Total LDH from treated wells) x 100. Low spontaneous release with high total LDH indicates early apoptosis (intact membrane). High spontaneous release indicates necrosis or late apoptosis.
Apoptosis/Necrosis Markers Section
Q5: My flow cytometry results for Annexin V/PI are showing a high percentage of cells in both early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis, but the negative control also shows a background signal. A: Background can arise from several sources.
- Cause 1: Mechanical stress during cell harvesting (especially if cells are adherent and require trypsinization).
- Solution: Use gentle detachment methods. For nanoparticle-treated cells, consider harvesting supernatant (containing detached apoptotic/necrotic cells) AND adherent cells separately, then combine for analysis.
- Cause 2: Calcium concentration is critical for Annexin V binding.
- Solution: Ensure the binding buffer contains the recommended 2.5 mM Ca2+. Use a commercial buffer for consistency.
- Cause 3: Nanoparticle auto-fluorescence or light scattering interference.
- Solution: Include nanoparticle-only samples to set appropriate gating and compensation. Use a wash step with PBS after staining to reduce background.
Q6: What are the key markers to confirm immunogenic cell death (ICD) induced by nanoparticles, beyond standard apoptosis assays? A: ICD involves the emission of "danger signals" or Damage-Associated Molecular Patterns (DAMPs).
- Key Surface Marker: Calreticulin (CRT) translocation to the plasma membrane (detectable by flow cytometry).
- Key Released Mediators: Extracellular ATP (measured by luciferase-based assays) and High Mobility Group Box 1 (HMGB1) release into supernatant (measured by ELISA).
- Workflow: Treat cells with nanoparticles, collect supernatant for ATP/HMGB1, and analyze adherent cells for surface CRT.
ROS Detection Section
Q7: My ROS probe (e.g., DCFH-DA) shows an instant spike upon adding nanoparticles, even in cell-free conditions. How do I interpret this? A: This indicates probe-nanoparticle interaction, not cellular ROS.
- Artifact Cause: Many nanomaterials (e.g., CeO2, Mn3O4) possess intrinsic catalase- or peroxidase-like activity that can oxidize the dye.
- Solution: Always run a cell-free control with nanoparticles + dye. Consider using multiple, chemically distinct ROS probes (e.g., DHE for superoxide) for confirmation. For intracellular validation, use pre-treatment with a ROS scavenger like N-acetylcysteine (NAC) to see if the signal is quenched.
Q8: How can I determine if ROS generation is a primary cause of cytotoxicity or a secondary consequence of cell death? A: Perform a time-course and inhibitor study.
- Protocol: Measure ROS generation at earlier time points (e.g., 30min, 1h, 3h, 6h) post-nanoparticle exposure, well before significant cell death occurs (as measured by LDH or Annexin V). In parallel, pre-treat cells with an antioxidant (e.g., 5mM NAC) for 1-2h before nanoparticle addition, then measure both ROS and subsequent cell death (e.g., at 24h). If NAC pre-treatment inhibits both early ROS and later cell death, it suggests a causal role.
Table 1: Comparison of Key Cytotoxicity Assays
| Assay | What it Measures | Key Advantages | Key Limitations | Optimal Readout Time Post-NP Exposure |
|---|---|---|---|---|
| MTT/XTT | Cellular metabolic activity (dehydrogenase enzymes) | High-throughput, inexpensive, well-established. | Susceptible to NP interference; measures viability, not direct death. | 24-72 hours |
| LDH Release | Plasma membrane integrity (cytosolic enzyme leak) | Direct measure of cytolysis/necrosis; easy protocol. | Cannot detect early apoptosis; serum can contain LDH. | 4-24 hours |
| Annexin V/PI | Phosphatidylserine exposure (Apoptosis) & membrane integrity (Necrosis) | Distinguishes apoptosis stages & necrosis. | Requires flow cytometry; sensitive to handling. | 6-48 hours (time-course) |
| ROS Detection | Reactive Oxygen Species (e.g., H2O2, superoxide) | Early event indicator; mechanistic insight. | High artifactual potential from NPs; probe specificity issues. | 0.5-6 hours |
Table 2: Common Artifacts & Controls for Nanoparticle Cytotoxicity Testing
| Interference Type | Affected Assay(s) | Recommended Control Experiments |
|---|---|---|
| Catalytic Activity | MTT/XTT, ROS probes | Cell-free control: NPs + assay reagents. |
| Adsorption | MTT/XTT (formazan), LDH, cytokines | Supernatant incubation control: Incubate released product (e.g., LDH) with NPs, then measure. |
| Light Scattering/Absorption | All colorimetric/fluorimetric assays | NP-only background control: NPs in medium + assay reagents. |
| Auto-fluorescence | Flow cytometry, fluorimetric assays | NP-only sample for flow gating/background subtraction. |
Experimental Protocols
Protocol 1: MTT Assay for Nanoparticle-Treated Cells (with NP controls)
- Seed cells in a 96-well plate and incubate for 24h.
- Treat cells with nanoparticle suspensions or controls (media, positive control like 100µM H2O2) for desired time.
- Prepare NP-Control Plate: In a separate plate, add NPs to cell-free medium.
- Add MTT: To both plates, add MTT reagent (0.5 mg/mL final concentration). Incubate 2-4h at 37°C.
- Solubilize: Carefully remove medium, add DMSO (or specified solubilizer). Shake gently for 15 min.
- Measure: Read absorbance at 570 nm, with a reference at 650 nm. Correct treated cell values with NP-control plate values.
Protocol 2: Annexin V-FITC/PI Staining for Flow Cytometry
- Harvest Cells: Collect supernatant (contains detached cells) and gently trypsinize adherent cells. Pool, wash twice with cold PBS.
- Stain: Resuspend ~1x10^5 cells in 100µL 1X Annexin V Binding Buffer. Add 5µL Annexin V-FITC and 5µL Propidium Iodide (PI). Incubate for 15 min at RT in the dark.
- Analyze: Add 400µL binding buffer and analyze within 1 hour on a flow cytometer. Use unstained, Annexin V-only, and PI-only controls for compensation.
Protocol 3: Intracellular ROS Detection using DCFH-DA
- Load Probe: After NP treatment, replace medium with serum-free medium containing 10-20µM DCFH-DA. Incubate 30 min at 37°C.
- Wash: Wash cells 2-3 times with PBS to remove extracellular dye.
- Measure: For fluorescence plate readers: Add fresh PBS and measure fluorescence (Ex/Em ~485/535 nm). For microscopy, image immediately. Include controls: Untreated cells (basal ROS), NPs + dye in cell-free wells, and a positive control (e.g., 100µM tert-Butyl hydroperoxide, 30 min).
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for NP Cytotoxicity Testing
| Reagent/Kit | Primary Function | Critical Notes for Nanoparticle Research |
|---|---|---|
| Tetrazolium Salts (MTT, XTT) | Indicator of cellular metabolic activity. | Use with interference controls. XTT requires an electron coupling reagent. |
| LDH Detection Kit | Quantifies lactate dehydrogenase release from cytosol. | Ideal for measuring necrotic damage. Ensure kit components are fresh. |
| Annexin V-FITC/PI Apoptosis Kit | Differentiates live, early apoptotic, late apoptotic, and necrotic cells. | Calcium-dependent binding; handle cells gently to avoid false positives. |
| Cell-permeable ROS Probes (DCFH-DA, DHE) | Detect intracellular reactive oxygen species. | Highly prone to artifact; cell-free nanoparticle-probe controls are mandatory. |
| N-acetylcysteine (NAC) | Broad-spectrum antioxidant. | Used (5-10mM pre-treatment) to test causal role of ROS in NP toxicity. |
| Triton X-100 (1-2% in PBS) | Positive control for LDH assay (causes complete cell lysis). | Verify complete lysis under microscope for your cell type. |
| Calreticulin (CRT) Antibody | Detect surface CRT exposure for Immunogenic Cell Death (ICD). | Use non-permeabilized cells for flow cytometry to confirm surface localization. |
Diagrams
Title: NP Cytotoxicity & Assay Interference Pathways
Title: MTT Assay Workflow with NP Control
FAQs & Troubleshooting Guides
Q1: In our DC maturation assay using nanoparticle (NP)-treated monocyte-derived DCs, we are seeing high variability in CD86 and HLA-DR surface expression between donors. What could be the cause and how can we mitigate this? A: High donor-to-donor variability in DC maturation markers is a common challenge, often linked to the donor's immune status and monocyte isolation efficiency.
- Troubleshooting Steps:
- Standardize Monocyte Isolation: Use positive selection (CD14+ microbeads) instead of plastic adherence for higher purity and consistency.
- Include Reference Controls: In every experiment, include a well-characterized positive control (e.g., 100 ng/mL LPS + 20 ng/mL IFN-γ) and an inert negative control (e.g., PBS-treated). This normalizes donor responses.
- Increase Replicates: Use cells from at least 3 different donors in triplicate for statistical power.
- Check NP Sterility: Perform an endotoxin/LAL test on your NP stock. Contaminating endotoxin is a potent, variable DC activator.
Q2: Our cytokine release assay (Luminex/ELISA) from PBMCs exposed to NPs shows unexpectedly low or undetectable levels of key cytokines like IL-6, TNF-α, and IL-1β. What are potential reasons? A: Low cytokine detection can stem from assay sensitivity, cell health, or NP interference.
- Troubleshooting Steps:
- Confirm Cell Viability: Use a live/dead stain (e.g., propidium iodide) to ensure NP cytotoxicity isn't reducing the responding cell population. Frame data within your thesis's cytotoxicity findings.
- Optimize Incubation Time: Kinetic profiles differ. Sample supernatants at multiple time points (e.g., 6, 24, 48 hours).
- Check for Assay Interference: Some NPs can adsorb cytokines or interfere with detection antibodies. Perform a spike-and-recovery experiment by adding a known cytokine concentration to NP-treated supernatant.
- Increase Cell Concentration: Use 1-2 x 10^6 PBMCs/mL to ensure sufficient secretor cells.
Q3: During leukocyte activation profiling by flow cytometry, we observe high background fluorescence in channels detecting FITC and PE after NP treatment. How do we address this? A: This indicates NP autofluorescence or non-specific antibody binding, which confounds activation marker detection.
- Troubleshooting Steps:
- Include NP-Only Controls: Always stain cells treated with NPs without antibodies to establish autofluorescence levels. Use this to set compensation and gating thresholds.
- Titrate Antibodies: Perform antibody titration on NP-treated cells to find the optimal signal-to-noise ratio.
- Use a Viability Dye: Distinguish live cells, as dead cells exhibit high non-specific binding. Use a near-IR fixable viability dye to avoid spectral overlap.
- Implement a Blocking Step: Incubate cells with Fc receptor blocking reagent (human TruStain FcX) for 10 minutes prior to surface antibody staining.
Experimental Protocols
Protocol 1: Standardized DC Maturation Assay Objective: To assess the impact of nanoparticles on dendritic cell maturation.
- Isolate CD14+ Monocytes from human PBMCs using magnetic-activated cell sorting (MACS).
- Differentiate into Immature DCs (iDCs): Culture 1x10^6 cells/mL in RPMI-1640 with 10% FBS, 100 ng/mL GM-CSF, and 50 ng/mL IL-4 for 6 days. Refresh cytokines on day 3.
- NP Exposure: On day 6, harvest iDCs and seed at 5x10^5 cells/mL. Treat with a range of NP concentrations (based on your cytotoxicity thesis data), positive control (LPS+IFN-γ), and negative control (vehicle). Incubate for 24h.
- Flow Cytometry Analysis: Harvest cells, wash, and stain with fluorochrome-conjugated antibodies against CD83, CD86, HLA-DR, and CD11c. Include a viability dye. Analyze on a flow cytometer. Gate on live, CD11c+ cells to calculate MFI and % positive for maturation markers.
Protocol 2: Multiplex Cytokine Release Assay from PBMCs Objective: To quantitatively profile a broad panel of cytokines released upon NP exposure.
- PBMC Preparation: Isfresh PBMCs from healthy donor blood via density gradient centrifugation.
- Stimulation: Seed PBMCs at 1x10^6 cells/well in a 96-well plate. Treat with NPs, positive control (e.g., 1 µg/mL PHA-L), and negative control. Incubate at 37°C, 5% CO2 for 24 hours.
- Supernatant Collection: Centrifuge plate at 300 x g for 5 min. Carefully collect supernatant into a fresh tube. Centrifuge again at 500 x g for 10 min to remove residual cells/debris. Store at -80°C.
- Luminex Assay: Thaw samples on ice. Use a commercially available human cytokine 25-plex panel (e.g., Invitrogen) following manufacturer instructions. Briefly, mix samples with antibody-coated magnetic beads, incubate, wash, add detection antibody, then streptavidin-PE. Analyze on a Luminex analyzer. Generate standard curves for each cytokine for quantification.
Data Summary Tables
Table 1: Expected DC Maturation Marker Expression (Mean Fluorescence Intensity Range)
| Stimulus | CD83 MFI | CD86 MFI | HLA-DR MFI |
|---|---|---|---|
| Immature DCs | 200 - 500 | 1,000 - 3,000 | 10,000 - 30,000 |
| LPS + IFN-γ | 8,000 - 15,000 | 20,000 - 50,000 | 80,000 - 150,000 |
| "Low-Reactogenic" NP | 500 - 2,000 | 5,000 - 15,000 | 30,000 - 70,000 |
| "High-Reactogenic" NP | 5,000 - 12,000 | 15,000 - 40,000 | 60,000 - 120,000 |
Table 2: Typical Cytokine Release Ranges from PBMCs (pg/mL)
| Cytokine | Unstimulated | PHA-L Stimulated | Threshold for Positive Response |
|---|---|---|---|
| IL-6 | 5 - 50 | 1,000 - 10,000 | > 100 |
| TNF-α | 10 - 100 | 2,000 - 8,000 | > 200 |
| IL-1β | < 20 | 500 - 4,000 | > 50 |
| IFN-γ | < 10 | 5,000 - 20,000 | > 100 |
| IL-10 | < 20 | 200 - 1,500 | > 50 |
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Function & Rationale |
|---|---|
| Ficoll-Paque Premium | Density gradient medium for high-viability PBMC isolation from whole blood. |
| CD14 MicroBeads, human | For positive selection of monocytes with high purity for consistent DC differentiation. |
| Recombinant GM-CSF & IL-4 | Essential cytokines to drive monocyte differentiation into immature dendritic cells. |
| LPS (Ultra-Pure, from E. coli) | Standard positive control for robust TLR4-mediated DC maturation and cytokine induction. |
| LIVE/DEAD Fixable Viability Dyes | Critical for excluding dead cells in flow cytometry, which bind antibodies non-specifically. |
| Human TruStain FcX (Fc Receptor Block) | Reduces background in flow cytometry by blocking non-specific antibody binding. |
| LEGENDplex Human Inflammation Panel | Pre-configured multiplex bead array for simultaneous, precise quantification of 13+ cytokines. |
| Cell Counting Kit-8 (CCK-8) | For parallel assessment of NP cytotoxicity (cell viability) via WST-8 reduction. |
Visualization: Signaling Pathways & Workflows
Diagram 1: NP Immune Recognition & Signaling Pathways
Diagram 2: Comprehensive Immunogenicity Profiling Workflow
Technical Support Center: Troubleshooting & FAQs
Frequently Asked Questions
Q1: Our nanoparticle formulation shows unexpected acute toxicity in mice at a dose deemed safe in vitro. What are the primary systemic factors to investigate? A1: Unexpected in vivo acute toxicity often stems from factors not captured in cell cultures. Prioritize investigating: 1) Complement Activation-Related Pseudoallergy (CARPA): A common hypersensitivity reaction to nanocarriers. Monitor for transient hypotension, leukopenia, or thrombocytopenia immediately post-injection. 2) Liver/Kidney Sequestration: High accumulation can cause organ-specific toxicity. Check for elevated serum ALT, AST, and BUN/creatinine. 3) Nanoparticle Aggregation in Blood: Size aggregation can cause capillary blockade. Examine blood smears or use dynamic light scattering on blood samples post-administration. 4) Impurity Leaching: Metal ions or organic solvents from synthesis can cause systemic effects. Perform ICP-MS on blood samples.
Q2: During a chronic toxicity study (28-day repeat dose), we observe gradual weight loss and reduced activity in the treatment group. How should we differentiate between immunogenic response and general toxicity? A2: This requires a multi-parameter approach. Follow this diagnostic workflow:
- Clinical Pathology: Run CBC with differential (look for sustained neutrophilia/lymphopenia) and serum cytokine panels (IL-6, TNF-α, IFN-γ) at multiple time points.
- Histopathology with Specific Staining: Beyond H&E, perform immunohistochemistry on key organs (spleen, liver, injection site) for CD68+ (macrophage infiltration), CD3+ (T-cell infiltration), and signs of germinal center formation.
- Anti-Nanoparticle Antibody Assay: Collect serum pre-dose and at termination. Use an ELISA where plates are coated with your nanoparticle. Detect IgM/IgG to confirm an adaptive immune response.
- Control Comparison: Ensure you have a "vehicle control" group (receiving all excipients without the active nanoparticle) to rule out excipient-related chronic inflammation.
Q3: Biodistribution data from IVIS or radioactive labeling shows inconsistent organ accumulation between animals. What are the top technical sources of this variability? A3: High variability in biodistribution often originates from administration technique and nanoparticle preparation.
- Injection Technique: For intravenous (IV) tail vein injections, inconsistent rate, bolus leakage, or partial intra-arterial administration drastically alters first-pass distribution. Standardize injection volume, rate (use syringe pumps), and needle size. Always use warm cages for tail vein dilation.
- Nanoparticle Stability: Aggregation post-resuspension or in storage leads to non-uniform dosing. Always characterize hydrodynamic size and PDI via DLS immediately before animal dosing. Filter samples through a 0.22 µm filter if compatible.
- Animal Physiology: Fasting state, circadian rhythm, and age/sex can influence mononuclear phagocytic system (MPS) activity. Strictly control animal husbandry conditions and randomize adequately.
- Imaging Artifacts: For IVIS, ensure animals are shaved uniformly and positioned identically. Account for autofluorescence in organs like the gut.
Q4: We suspect a Type I (IgE-mediated) or Type IV (T-cell mediated) hypersensitivity reaction to our nano-formulation. What are the definitive rodent models and readouts? A4:
- For Type I Hypersensitivity (Anaphylaxis):
- Model: Passive Cutaneous Anaphylaxis (PCA) in rats or mice. Pre-sensitize with nanoparticle + adjuvant, then later challenge with nanoparticle IV along with Evans blue dye.
- Definitive Readout: Extravasation of Evans blue at the sensitization site, measured by dye extraction and spectrophotometry. Also measure serum mast cell protease (MMCP-1 in mice) immediately after challenge.
- For Type IV Hypersensitivity (Delayed-Type):
- Model: Local Lymph Node Assay (LLNA) or Guinea Pig Maximization Test (for stronger prediction).
- Definitive Readout (LLNA): Apply nanoparticle to ear dorsum for 3 consecutive days. On day 5, inject ³H-thymidine. Isolate auricular lymph nodes and measure proliferation via ³H-thymidine incorporation. A Stimulation Index >3 indicates sensitization potential.
Troubleshooting Guides
Issue: High Mortality During Acute Toxicity (LD50) Study.
- Step 1 (Immediate): If mortality occurs within minutes, suspect CARPA or acute embolism. Necropsy immediately, focusing on lungs for signs of edema and hemorrhage. Collect blood for complement factor analysis (C3a, SC5b-9).
- Step 2 (Dose Preparation): Re-audit dose calculation and preparation. Verify nanoparticle concentration (via absorbance, elemental analysis), sterility (perform rapid endotoxin test), and absence of large aggregates (use DLS/NTA).
- Step 3 (Administration): Review injection records. Consider step-wise dosing starting at << expected toxic dose to establish a response curve. Implement ECG/respiratory monitoring for next cohort.
Issue: Poor Signal-to-Noise in Quantitative Biodistribution via ICP-MS.
- Problem: Background elemental levels too high or nanoparticle signal too low.
- Solution Checklist:
- Digestion: Use trace metal-grade nitric acid and peroxides in a closed-vessel microwave digester for complete tissue digestion.
- Background Control: Analyze tissues from naive animals (no injection) to establish precise baseline element levels. Subtract this background.
- Washing: Perfuse animals thoroughly with saline-EDTA via cardiac puncture post-euthanasia to remove blood pool signal.
- Signal Enhancement: If using gold or other elemental tags, consider signal amplification techniques. Ensure your nanoparticle has a sufficiently high payload of the detectable element.
Issue: Failure to Elicit Immune Response in Adjuvant Studies for Immunogenicity Assessment.
- Problem: Nanoparticle intended as a vaccine carrier shows no antibody titer.
- Solution Flow:
- Validate Antigen Integrity: Confirm the antigen is properly conjugated/adsorbed and not degraded. Run an SDS-PAGE or HPLC.
- Optimize Adjuvant/Route: Switch from subcutaneous to intramuscular. Consider adding a known adjuvant (e.g., Alum, CpG) to your formulation in a prime-boost regimen.
- Timing: Ensure an appropriate boost schedule (typically 2-3 weeks post-prime). Collect serum 10-14 days post-boost for peak antibody titer.
- Readout Sensitivity: Use a more sensitive assay than standard ELISA (e.g., electrochemiluminescence). Ensure your coating strategy efficiently captures the nanoparticle-antigen complex.
Data Presentation
Table 1: Standard Parameters for Acute & Chronic Rodent Toxicity Studies of Nanomaterials
| Parameter | Acute Study (Single Dose) | Chronic Study (Repeated Dose, e.g., 28-day) | Key Methodologies |
|---|---|---|---|
| Observation Duration | 14 days | Daily, for study duration + recovery period | Clinical scoring sheets, video monitoring. |
| Clinical Signs | Twice daily for first 4 hrs, then daily. | At least once daily. | Detailed check for piloerection, respiration, secretions, motility. |
| Body Weight | Recorded daily. | Recorded 1-3 times per week. | Statistical analysis of trends. |
| Food/Water Consum. | Optional, but recommended. | Measured weekly. | Per-cage or individual metabolic caging. |
| Hematology | Terminal only (Day 14). | Interim (Day 14) and Terminal (Day 28+). | CBC, differential, coagulation panel. |
| Clinical Chemistry | Terminal only (Day 14). | Interim and Terminal. | Liver (ALT, AST, ALP), Kidney (BUN, Creatinine), Inflammation (CRP). |
| Gross Necropsy | All animals, at death or terminal. | All animals. | Standardized organ weight protocol (heart, liver, spleen, etc.). |
| Histopathology | Target organs from all dose groups. | Full tissue list from control and high-dose, target organs from all. | H&E staining; IHC if indicated (e.g., CD68, Caspase-3). |
Table 2: Common Biodistribution Measurement Techniques & Their Characteristics
| Technique | Detection Limit | Spatial Resolution | Quantitative? | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Radioactive Labeling (γ-counter) | ~ng | Organ level | Excellent | Gold standard, highly quantitative, deep tissue. | Radiation safety, label detachment. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | pg-ng | Organ level | Excellent | Ultra-sensitive, multi-element, absolute quantitation. | Destructive, no real-time data. |
| Fluorescence Imaging (IVIS) | ~µg | ~1-3 mm (2D) | Semi-quantitative | Real-time, longitudinal, easy. | Limited depth, autofluorescence, quenching. |
| X-ray Computed Tomography (CT) | mg (for heavy elements) | ~50-100 µm | Good for high-Z materials | Anatomical context, high resolution. | Low sensitivity for most nanomaterials. |
Experimental Protocols
Protocol 1: Standard Acute Systemic Toxicity Test (OECD Guideline 425 Adapted for Nanomaterials) Objective: To estimate the LD50 or identify signs of acute toxicity after a single intravenous bolus. Materials: Test nanoparticle suspension, vehicle control, sterile syringes (1 mL), 27G needles, rodent restrainer, warm cage or lamp, healthy mice/rats (6-12 weeks, n=5/group minimum). Procedure:
- Dose Preparation: Sonicate nanoparticle suspension (e.g., water bath, 5 min) and filter (0.22 µm) immediately before dosing. Confirm concentration.
- Animal Preparation: Place animals in a warm cage (∼30°C) for 5-10 minutes to dilate tail veins.
- Administration: Using a syringe pump, administer a single bolus IV via the lateral tail vein at a constant rate (e.g., 100 µL/10 sec for a 200 µL volume). Record exact time.
- Immediate Observation: Observe animals individually for the first 30 minutes, then at 1, 2, 4, 8, and 24 hours post-dose. Record clinical signs (lethargy, dyspnea, tremor, piloerection).
- Follow-up: Weigh animals daily for 14 days. Note any mortality or moribund state.
- Terminal Analysis: On day 14, euthanize survivors. Collect blood for hematology/serum chemistry. Perform gross necropsy and weigh key organs. Preserve organs in 10% NBF for histopathology. Key Adaptation for Nano: Include a group injected with a known complement activator (e.g., liposomal doxorubicin) as a positive control for hypersensitivity.
Protocol 2: Quantitative Biodistribution via Radioisotope Labeling Objective: To determine the percentage of injected dose (%ID) per gram of tissue over time. Materials: Nanoparticle labeled with a gamma-emitting radionuclide (e.g., ¹¹¹In, ⁹⁹mTc, ⁶⁴Cu), dose calibrator, gamma counter, perfusion pump, pre-weighed tissue vials. Procedure:
- Dose Calibration: Precisely measure the radioactivity (µCi) of the prepared dose in a dose calibrator. Prepare a standard dilution for subsequent counting efficiency.
- Administration: Inject a known volume/activity IV via tail vein (as in Protocol 1).
- Time Points: Euthanize animals (n=5/time point) at pre-determined times (e.g., 5 min, 1h, 4h, 24h, 7d).
- Perfusion: To clear blood-pool radioactivity, perform transcardial perfusion with 20-30 mL of heparinized saline (10 U/mL) at a steady rate.
- Tissue Collection: Dissect and weigh all organs of interest (blood sample, heart, lungs, liver, spleen, kidneys, brain, muscle, bone, tail at injection site).
- Gamma Counting: Place each tissue in a vial and count in a gamma counter alongside the dose standard and background. Correct for decay and isotope half-life.
- Calculation: %ID/g = (Tissue counts / Counting efficiency) / (Injected dose counts) / (Tissue weight in grams) * 100%. Critical Step: Validate label stability >95% in serum incubation studies prior to in vivo use.
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Application in Rodent Nano-Studies |
|---|---|
| Lipopolysaccharide (LPS) | Positive control for acute inflammatory response and cytokine storm. Used to validate assay sensitivity in toxicity studies. |
| Poloxamer 407 or Tween 80 | Common surfactants used to stabilize nanoparticle suspensions for injection, preventing aggregation in biological fluids. |
| Evans Blue Dye | Used in vascular permeability assays, such as the Passive Cutaneous Anaphylaxis (PCA) test, to quantify extravasation due to hypersensitivity. |
| Heparinized Saline | Used for systemic perfusion prior to tissue collection in biodistribution studies to clear the blood-pool signal, improving organ-specific data. |
| Rodent Serum/Plasma | Used for in vitro stability studies (DLS in serum) and to pre-coat nanoparticles to study protein corona formation before in vivo experiments. |
| Alum (Aluminum Hydroxide) | A common vaccine adjuvant used as a positive control in studies investigating nanoparticle immunogenicity and adaptive immune response. |
| Commercial ELISA Kits (MMCP-1, Cytokines) | For quantifying specific biomarkers: Mouse Mast Cell Protease-1 (MMCP-1) for anaphylaxis; IL-6, TNF-α, IFN-γ for systemic inflammation. |
| ³H-thymidine or BrdU | Used in the Local Lymph Node Assay (LLNA) to measure T-cell proliferation as a definitive readout for Type IV hypersensitivity potential. |
| ICP-MS Multi-Element Standards | Certified reference materials for calibrating ICP-MS instruments, essential for accurate quantitative biodistribution of metal-based nanomaterials. |
| Tissue Digestion Tubes (MTE) | Microwave-assisted, closed-vessel tubes made of Teflon for complete, contamination-free digestion of tissue samples prior to elemental analysis. |
Technical Support Center: Troubleshooting Nanoparticle Cytotoxicity & Immunogenicity Experiments
FAQs & Troubleshooting Guides
Q1: My negative control wells show significant cell death. What could be the cause? A: This indicates a fundamental contaminant or experimental condition error.
- Troubleshooting Steps:
- Check Solvent Cytotoxicity: Ensure the vehicle (e.g., DMSO, PBS) used to suspend nanoparticles is at a non-toxic concentration (e.g., DMSO <0.1% v/v for most cell lines). Run a vehicle-only control.
- Assay Interference: Nanoparticles can interfere with common assays (e.g., MTT, LDH). They may catalyze redox reactions or adsorb assay components. Solution: Include a nanoparticle-only control (no cells) in your assay plate to check for signal interference. Consider switching to an interference-resistant assay (e.g., resazurin-based for metabolic activity, or a luminescent ATP assay).
- Check Sterility: Use sterile-filtered (0.22 µm) nanoparticle suspensions and media. Bacterial or endotoxin contamination can cause immune activation and death.
Q2: How do I choose the right dosage metric (e.g., mass concentration, particle number, surface area) for in vitro studies? A: The optimal metric depends on the hypothesized mechanism of action. Inconsistent metrics are a major source of irreproducibility in nanotoxicology.
- Guidance: Follow the recommendations from recent consensus papers.
- Troubleshooting: If your dose-response is erratic, test multiple metrics. For surface-area-driven toxicity (common with reactive metal oxides), calculate and dose based on specific surface area (m²/mL). For particle-number-dependent effects (e.g., cellular uptake saturation), use concentration derived from particle size analysis (# particles/mL). Always report all three: mass concentration (µg/mL), surface area, and particle number.
Q3: My nanoparticles aggregate heavily in biological media, skewing dosing and uptake. How can I stabilize them? A: Aggregation alters effective dose, hydrodynamic size, and cellular interaction.
- Protocol for Dispersion:
- Sonication: Sonicate the stock nanoparticle suspension in a water bath or with a probe sonicator (e.g., 30% amplitude, 10 min on ice to prevent overheating) immediately before dosing.
- Serum Pre-coating: Pre-incubate nanoparticles with 10-50% FBS or human serum in media for 30 min at 37°C to form a stabilizing "protein corona."
- Characterization: Critical: Measure the hydrodynamic diameter and polydispersity index (PDI) via Dynamic Light Scattering (DLS) after dispersion in the complete cell culture medium to be used in the experiment. This is your relevant dosing size.
Q4: My chosen immortalized cell line shows no immunogenic response to nanoparticles reported to be inflammatory in vivo. What biological model should I use? A: Immortalized lines often have dampened immune pathways.
- Solution:
- Primary Cells: Use primary human peripheral blood mononuclear cells (PBMCs), monocyte-derived macrophages, or dendritic cells. Protocol: Isolate PBMCs via density gradient centrifugation (Ficoll-Paque). Differentiate monocytes with GM-CSF (M1-like) or M-CSF (M2-like).
- Co-culture Models: Establish a transwell co-culture of epithelial cells and macrophages to study crosstalk.
- Reporter Cell Lines: Use THP-1 monocytic cells with an NF-κB or IRF reporter gene to quantitatively measure pathway activation.
Q5: How do I differentiate between caspase-dependent apoptosis and pyroptosis (immunogenic cell death) in my assay? A: Both cause DNA fragmentation and positive Annexin V staining, but pyroptosis is gasdermin-mediated and highly inflammatory.
- Diagnostic Protocol:
- Inhibitor Assay: Pre-treat cells with Z-VAD-FMK (pan-caspase inhibitor, 20 µM) and VX-765 (caspase-1 inhibitor, 10 µM). If cell death is inhibited only by VX-765, it suggests pyroptosis.
- Western Blot Markers:
- Apoptosis: Cleaved caspase-3, cleaved PARP.
- Pyroptosis: Cleaved caspase-1, mature IL-1β, cleaved gasdermin D (GSDMD-N terminal).
- Morphology: Image cells using high-content imaging. Pyroptotic cells exhibit large balloon-like protrusions (pyroptotic bodies), distinct from apoptotic blebbing.
Table 1: Common Dosage Metrics for Spherical Nanoparticles
| Metric | Calculation Formula | When to Use | Key Challenge |
|---|---|---|---|
| Mass Concentration | Weighed mass / Volume (µg/mL) | Standard dosing, pharmaco-kinetic scaling | Ignores size and surface properties. |
| Particle Number | (Mass / (Density * Particle Volume)) / Volume (#/mL) | Uptake saturation studies, single-particle effects | Requires precise core size and monodispersity. |
| Total Surface Area | (Particle Surface Area) * (Particle Number) (m²/mL) | Surface-reactivity-driven toxicity (ROS, dissolution) | Requires accurate size and assumes spherical geometry. |
| Molar Concentration | (Mass / Molar Mass) / Volume (nmol/mL) | For molecularly defined nanoparticles (e.g., drug conjugates). | Not applicable for polydisperse inorganic materials. |
Table 2: Advantages and Limitations of Biological Models for Immunogenicity
| Model System | Key Advantages | Major Limitations | Best For Screening |
|---|---|---|---|
| Immortalized Cell Line (e.g., THP-1) | Reproducible, easy, scalable, amenable to genetic modification. | Often have altered TLR/cytokine pathways; may not reflect primary cell physiology. | High-throughput toxicity ranking. |
| Primary Human PBMCs/Macrophages | Physiologically relevant, donor variability reflects human population. | Donor variability, finite lifespan, more expensive, requires ethical approval. | Mechanistic immunogenic response. |
| Murine Models (in vivo) | Full systemic response, ADME, organ-level pathology. | Species-specific immune differences, high cost, complex ethics. | Final pre-clinical validation. |
| Organ-on-a-Chip (Co-culture) | Captures tissue-tissue interfaces and fluid flow. | Technically complex, low-throughput, nascent validation. | Investigating nanoparticle translocation and secondary effects. |
Detailed Experimental Protocols
Protocol 1: Assessing NLRP3 Inflammasome Activation by Nanoparticles Objective: To determine if nanoparticles activate the NLRP3 inflammasome, leading to caspase-1 activation and IL-1β release. Materials: THP-1 cells (or primary human macrophages), PMA, LPS, ATP, nanoparticle suspension, IL-1β ELISA kit, caspase-1 activity assay kit, cell culture reagents. Procedure:
- Differentiation: Seed THP-1 cells at 2x10⁵ cells/well in a 24-well plate with 100 nM PMA for 48h. Rest in fresh media for 24h.
- Priming (Signal 1): Stimulate cells with ultrapure LPS (100 ng/mL) for 3h to induce pro-IL-1β transcription via NF-κB.
- Nanoparticle Challenge (Signal 2): Replace media with nanoparticle suspension in serum-free media (pre-dispersed). Incubate for 6h. Positive Control: Add ATP (5 mM) for the final 30 min.
- Analysis:
- Extracellular IL-1β: Collect supernatant, centrifuge (500xg, 5 min) to remove debris. Measure IL-1β via ELISA.
- Caspase-1 Activity: Lyse cells, measure activity using a fluorescent substrate (e.g., YVAD-AFC) per kit instructions.
- Cell Viability: Run a parallel plate with identical treatments and assay via ATP-based luminescence.
Protocol 2: Characterizing Nanoparticle-Hydrodynamic Size in Biological Media Objective: To measure the effective hydrodynamic diameter and stability of nanoparticles under experimental conditions. Materials: Nanoparticle stock, complete cell culture media (with serum), DLS instrument, 0.22 µm syringe filter, sonicator. Procedure:
- Preparation: Sonicate nanoparticle stock (as per Q3 protocol). Dilute to the highest test concentration (e.g., 100 µg/mL) in complete media. Do not filter after adding nanoparticles.
- Incubation: Incubate the suspension at 37°C for 0h, 1h, and 24h to mimic exposure times.
- Measurement: For each time point, transfer suspension to a clean, disposable DLS cuvette. Run DLS measurement at 37°C.
- Data Acquisition: Record the Z-average hydrodynamic diameter, polydispersity index (PDI), and intensity size distribution. A PDI >0.3 indicates a polydisperse/aggregated sample.
- Interpretation: Report the size at the time of dosing (0h in media). The 24h measurement indicates stability over the experiment's duration.
Visualizations
Diagram Title: Nanoparticle Cytotoxicity Experiment Workflow
Diagram Title: Key Immunogenic vs. Apoptotic Signaling Pathways
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Purpose | Example Vendor/Product |
|---|---|---|
| Ultrapure LPS | Toll-like receptor 4 (TLR4) agonist; provides precise "Signal 1" for inflammasome priming studies. | InvivoGen (tlrl-3pelps) |
| ATP (disodium salt) | NLRP3 inflammasome activator; used as a positive control for "Signal 2" in macrophage assays. | Sigma Aldrich (A6419) |
| Z-VAD-FMK | Broad-spectrum, cell-permeable caspase inhibitor. Used to distinguish caspase-dependent from -independent cell death. | Cayman Chemical (14463) |
| VX-765 (Belnacasan) | Specific caspase-1 inhibitor. Critical tool to confirm inflammasome-mediated pyroptosis. | Selleckchem (S2228) |
| Poly(I:C) HMW | TLR3 agonist; positive control for testing nanoparticle-induced antiviral/interferon responses. | InvivoGen (tlrl-pic) |
| Recombinant Human M-CSF | For differentiating human monocytes into M2-like macrophages in vitro. | PeproTech (300-25) |
| Recombinant Human GM-CSF | For differentiating human monocytes into M1-like macrophages or dendritic cells. | PeproTech (300-03) |
| Dihydroethidium (DHE) | Cell-permeable fluorescent probe for detecting intracellular superoxide production (ROS). | Thermo Fisher (D11347) |
| Annexin V-FITC / PI Kit | Standard flow cytometry kit to discriminate apoptotic (Annexin V+/PI-) and necrotic/late apoptotic (Annexin V+/PI+) cells. | BioLegend (640914) |
| 0.22 µm PES Syringe Filter | For sterile filtration of nanoparticle suspensions and media. Essential for preventing microbial contamination. | Millex-GP (SLGP033RS) |
Engineering for Safety: Proactive Strategies to Mitigate Cytotoxicity and Unwanted Immune Responses
Technical Support Center: Troubleshooting & FAQs
FAQs & Troubleshooting for PEGylation
Q1: After PEGylation, my nanoparticles show increased aggregation instead of improved stability. What could be the cause? A: This is often due to insufficient surface coverage or incorrect PEG chain density. Below a critical grafting density, PEG chains cannot form the necessary "mushroom" or "brush" conformation to provide steric stabilization, leading to bridging flocculation.
- Solution: Increase the molar ratio of PEG reagent to nanoparticle surface functional groups. Optimize reaction time and pH. Purify post-reaction to remove unreacted PEG that might cause depletion aggregation. Characterize final product with DLS and zeta potential.
Q2: I observe a significant drop in nanoparticle targeting ligand activity post-PEGylation. How can I mitigate this? A: This is a classic "shielding" issue. Nonspecific conjugation chemistry can modify the targeting ligand.
- Solution: Use site-specific conjugation strategies (e.g., click chemistry after orthogonal functionalization). Employ heterobifunctional PEG linkers with a reactive group (e.g., maleimide) for the ligand and another (e.g., NHS ester) for the nanoparticle. Consider a "post-insertion" method where ligand-PEG conjugates are inserted into pre-formed nanoparticle coatings.
FAQs & Troubleshooting for Biomimetic Coatings
Q3: My cell membrane coating efficiency on synthetic nanoparticles is consistently low (<20%). How can I improve this? A: Low efficiency often stems from mismatched surface charge or improper vesicle preparation.
- Solution:
- Surface Charge: Temporarily adjust the core nanoparticle's zeta potential (slightly negative often works best) via pretreatment to facilitate fusion with membrane vesicles.
- Membrane Vesicle Preparation: Ensure membrane-derived vesicles are the correct size (extrude through 100-400 nm pores) and are unilamellar. Use a gentle process like sonication or extrusion for fusion, not vigorous vortexing.
- Verify with a membrane-specific dye (e.g., PKH26) and quantify by flow cytometry of particles.
Q4: My biomimetic nanoparticles are still being opsonized and cleared rapidly in in vivo models. What are the key checkpoints? A: This indicates the coating may be incomplete or unstable.
- Solution Checklist:
- Characterization: Use TEM with negative staining to visualize the core-shell structure. Perform SDS-PAGE to confirm the full membrane protein profile is present.
- Stability Test: Incubate in 100% serum at 37°C for 1 hour and re-analyze size. A significant increase indicates coating desorption.
- Protein Corona Analysis: Isolate particles from plasma via centrifugation and analyze adsorbed proteins by LC-MS/MS to identify residual opsonins.
FAQs & Troubleshooting for Stealth Technologies
Q5: How do I quantitatively evaluate the "stealth" property of my engineered nanoparticles? A: The primary metric is the rate of macrophage uptake in vitro and blood half-life in vivo. Use the following standardized protocol:
Protocol: Macrophage Uptake Assay (J774A.1 or RAW 264.7 cells)
- Cell Seeding: Seed macrophages in 24-well plates at 2.5 x 10^5 cells/well and culture overnight.
- NP Treatment: Incubate cells with fluorescently-labeled nanoparticles at a standard concentration (e.g., 50 µg/mL) in serum-containing medium for 2-4 hours at 37°C.
- Washing: Wash cells 3x with cold PBS to remove non-internalized NPs.
- Analysis: Analyze using flow cytometry. Report Mean Fluorescence Intensity (MFI) and the percentage of NP-positive cells. Always include uncoated NP controls.
Q6: My PEGylated nanoparticle formulation shows good initial stealth but loses it upon storage. What is happening? A: This is likely due to the "PEG dilemma" – hydrolysis or oxidation of PEG chains or their anchor points over time.
- Solution:
- Storage: Store lyophilized under inert gas (argon/nitrogen) at -20°C, not in aqueous solution at 4°C.
- Stabilizers: Add antioxidants (e.g., 0.02% ascorbic acid) to the formulation buffer.
- Chemistry: Consider using more stable linkers (e.g., amide bonds instead of esters) for PEG conjugation.
Table 1: Impact of Surface Engineering on Key Nanoparticle Parameters
| Surface Coating | Avg. Hydrodynamic Size Increase (nm) | Zeta Potential Shift (mV) | Macrophage Uptake Reduction (% vs. Uncoated) | In Vivo Circulation Half-life (t1/2, h) |
|---|---|---|---|---|
| PEG (Low Density) | +5 to +15 | -5 to -10 | 40-60% | ~2-4 |
| PEG (High Density) | +20 to +30 | -10 to -20 | 70-90% | ~12-24 |
| Biomimetic (RBC) | +8 to +12 | -15 to -25 | 80-95% | ~20-40 |
| Biomimetic (Platelet) | +10 to +20 | -10 to -15 | 60-80% | ~8-15 |
Table 2: Common Characterization Techniques for Coating Validation
| Technique | Parameter Measured | Target Outcome for Successful Coating |
|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic Diameter, PDI | Monomodal size distribution, increased size post-coating. |
| Zeta Potential | Surface Charge | Shift consistent with coating material (e.g., more negative for PEG). |
| X-ray Photoelectron Spectroscopy (XPS) | Surface Atomic Composition | Appearance of coating-specific elements (e.g., N for proteins, Si for silica). |
| FTIR / NMR | Chemical Bonds | Signature peaks for coating polymers (e.g., C-O-C for PEG). |
| Cryo-Electron Microscopy | Core-Shell Structure | Visual confirmation of a uniform coating layer. |
Experimental Protocols
Protocol: Standard NHS-PEG-NHS Conjugation to Amine-Mesoporous Silica Nanoparticles (MSNs) Objective: To covalently attach PEG chains to amine-functionalized MSNs to reduce cytotoxicity and immunogenic clearance. Reagents: Amine-MSNs (100 nm, 1 mg/mL in MES buffer), NHS-PEG-NHS (5 kDa, 100 mM in DMSO), MES Buffer (0.1 M, pH 6.0), Quenching Buffer (1M Tris-HCl, pH 7.4), PBS (pH 7.4). Procedure:
- Activation: Dilute 1 mL of Amine-MSNs in 9 mL MES buffer. Add NHS-PEG-NHS solution dropwise to achieve a 10:1 molar ratio (PEG:estimated surface amines) under gentle stirring.
- Reaction: React for 2 hours at room temperature under constant stirring.
- Quenching: Add 1 mL of Quenching Buffer and stir for 15 minutes to deactivate unreacted NHS esters.
- Purification: Centrifuge at 20,000 x g for 15 minutes. Wash pellet 3x with PBS to remove excess PEG and byproducts.
- Resuspension: Resuspend final PEG-MSNs in 1 mL sterile PBS. Characterize size and zeta potential immediately.
Visualizations
PEGylation Chemical Conjugation Workflow
Stealth Nanoparticle Evaluation Pipeline
MPS Clearance vs. Stealth Coating Action
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Primary Function | Key Consideration for Cytotoxicity/Immunogenicity Research |
|---|---|---|
| Heterobifunctional PEG Linkers (e.g., MAL-PEG-NHS) | Enables controlled, sequential conjugation of targeting ligands to nanoparticles. | Reduces nonspecific binding and preserves bioactivity, minimizing off-target immune reactions. |
| Membrane Protein Extraction Kits | Isulates intact plasma membrane proteins from cells (e.g., RBCs, leukocytes) for biomimetic coating. | Maintains native protein function and orientation critical for self-recognition. |
| Dynamic Light Scattering (DLS) & Zeta Potential Analyzer | Measures nanoparticle size, polydispersity, and surface charge in physiological buffers. | Essential for monitoring coating stability and predicting opsonization potential. |
| Pre-formed Lipid Vesicles (e.g., DOPC, DSPE-PEG) | Used for hybrid coating formation or as a model membrane for fusion studies. | PEG-lipids (DSPE-PEG) allow for simple integration of stealth properties. |
| Fluorescent Dyes (e.g., Cy5, DiD, PKH26) | Labels nanoparticles or coating components for tracking uptake and biodistribution. | Choose dyes with minimal cellular toxicity and that do not alter surface properties. |
| Macrophage Cell Lines (RAW 264.7, J774A.1) | Standardized in vitro model for testing nanoparticle uptake by the Mononuclear Phagocyte System (MPS). | Provides quantitative, high-throughput data on stealth performance before animal studies. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: During in vitro cytotoxicity screening, my biodegradable polymeric nanoparticles show high toxicity even at low doses, contradicting literature claims of biocompatibility. What could be wrong? A: This is a common issue often linked to residual reactants or solvents from synthesis. Biodegradable polymers like PLGA or polycaprolactone require rigorous purification.
- Protocol for Purification & Assessment:
- Purification: Post-synthesis, subject nanoparticles to 3 cycles of centrifugation (e.g., 20,000 x g, 30 min, 4°C) with copious amounts of sterile, deionized water or PBS. Consider using tangential flow filtration for larger batches.
- Residual Solvent Test: Perform Gas Chromatography-Mass Spectrometry (GC-MS) on a lyophilized sample of your nanoparticle suspension to detect traces of dichloromethane, chloroform, or ethyl acetate.
- pH Check: Re-suspend purified nanoparticles in cell culture media and incubate at 37°C for 24h. Measure the media pH. Acidic degradation products can leach and cause cytotoxicity.
- Control: Include an inert gold nanoparticle control of similar size and surface charge.
Q2: My inert gold nanoparticles (AuNPs) intended for imaging are unexpectedly triggering an inflammatory cytokine response in macrophage assays. How do I diagnose the surface contamination? A: Inert cores can become immunogenic due to adsorbed biomolecules or synthesis by-products.
- Diagnostic Protocol:
- Endotoxin Testing: Use the Limulus Amebocyte Lysate (LAL) chromogenic assay. Endotoxin levels must be <0.25 EU/mL for in vitro immunology studies.
- Protein Corona Analysis: Incubate AuNPs in 10% FBS for 1h at 37°C, isolate via centrifugation, and elute adsorbed proteins using SDS-PAGE loading buffer. Analyze via gel electrophoresis or mass spectrometry.
- Surface Charge & Ligand Integrity: Measure zeta potential. A significant shift from expected values may indicate ligand displacement or contamination. Confirm ligand density via NMR or a colorimetric assay specific to your ligand chemistry (e.g., Ellman's test for thiols).
Q3: When switching from an inert silica to a biodegradable chitosan core for drug delivery, my encapsulation efficiency plummets. How can I troubleshoot this? A: This stems from fundamental differences in material chemistry and drug-material interactions.
- Troubleshooting Workflow:
- Analyze Drug Properties: Log P (hydrophobicity) and pKa of your drug are critical. Hydrophobic drugs poorly encapsulate in hydrophilic chitosan without modification.
- Modify Core or Protocol:
- Option A: Chemically modify chitosan with hydrophobic moieties (e.g., acetyl groups).
- Option B: Change the encapsulation method. For chitosan, ionotropic gelation is standard for hydrophilic drugs. For hydrophobic drugs, consider a double emulsion (W/O/W) method or switch to a more compatible polymer like PLGA.
- Quantify Efficiency: Use the formula: EE% = (Mass of drug in nanoparticles / Initial mass of drug) x 100. Measure via HPLC of the supernatant post-encapsulation and purification.
Q4: How do I systematically choose between inert and biodegradable materials for a new therapeutic nanoparticle design aimed at minimizing immunogenicity? A: Base your selection on the application's Required Performance Attributes (RPAs), as summarized in the table below.
Table 1: Performance Comparison of Inert vs. Biodegradable Core Materials
| Performance Attribute | Inert Materials (e.g., Gold, Silica, Iron Oxide) | Biodegradable Materials (e.g., PLGA, Chitosan, Lipids) | Key Consideration for Immunogenicity |
|---|---|---|---|
| Long-term Cytotoxicity | Low, if surface-passivated | Variable; can increase as degradation accelerates | Inert: Persistent body burden risk. Biodegradable: Risk from acidic/byproduct accumulation. |
| Clearance Pathway | Often slow, renal/hepatic depending on size | Metabolic clearance, hydrolysis to natural metabolites | Inert: Long-term exposure may trigger adaptive response. Biodegradable: Degradation products may act as haptens. |
| Surface Modification Ease | Typically excellent (e.g., Au-S chemistry) | Can be challenging; may require copolymer synthesis | Both: Pegylation is crucial for both to reduce opsonization and subsequent immune recognition. |
| Drug Release Profile | Burst release from surface, difficult sustained release | Tunable, sustained release via degradation control | Sustained release (biodegradable) may reduce peak immunostimulant concentration vs. burst release (inert). |
| Encapsulation Efficiency | Generally low for hydrophilic drugs | Can be very high, especially for hydrophobic drugs | Improper encapsulation can lead to surface-associated drug, increasing immune cell activation. |
| Typical In Vivo Half-life | Can be very long (days to months) | Usually shorter (hours to days), tunable | Longer circulation increases chance of immune cell interaction. |
Experimental Protocols
Protocol 1: Assessing Nanoparticle Degradation & Byproduct Cytotoxicity Objective: Quantify degradation and link to cell viability for biodegradable nanoparticles. Method:
- Incubation: Place 5 mg of sterile nanoparticles in 10 mL of simulated biological fluids (e.g., PBS pH 7.4, and endolysosomal mimic pH 5.0). Incubate at 37°C with gentle agitation.
- Sampling: At scheduled intervals (e.g., 1, 3, 7, 14 days), centrifuge samples. Collect supernatant.
- Analysis:
- Degradation: Measure dry mass of pelleted nanoparticles.
- Byproducts: Analyze supernatant via HPLC/GC-MS for degradation products (e.g., lactic/glycolic acid for PLGA).
- Cytotoxicity: Apply collected supernatants (pH-adjusted) to cultured cells (e.g., THP-1 macrophages). Perform MTT/LDH assay after 24h.
Protocol 2: Profiling Immunogenic Response via Cytokine Array Objective: Compare innate immune activation by inert vs. biodegradable nanoparticles. Method:
- Cell Preparation: Differentiate THP-1 monocytes into macrophages using 100 ng/mL PMA for 48h.
- Exposure: Treat macrophages with nanoparticles (10-100 µg/mL) and controls (LPS for positive, media for negative) for 18-24h.
- Collection: Centrifuge culture media to remove cells/debris.
- Quantification: Use a multiplex bead-based cytokine assay (e.g., Luminex) or ELISA to quantify key pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) and anti-inflammatory markers (IL-10).
Visualizations
Decision Workflow for Core Material Selection
Nanoparticle Core Properties Modulate Immunogenic Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Cytotoxicity & Immunogenicity Assessment
| Item | Function in Experiments | Example Product/Catalog |
|---|---|---|
| Differentiated THP-1 Cells | Human monocyte model for standardized macrophage response studies. | ATCC TIB-202, differentiated with PMA. |
| LAL Endotoxin Assay Kit | Quantifies bacterial endotoxin contamination on nanoparticles. | Pierce Chromogenic Endotoxin Quant Kit. |
| Multiplex Cytokine Assay Panel | Simultaneously measures multiple inflammatory cytokines from a small sample volume. | Bio-Plex Pro Human Inflammation Panel 37-plex. |
| MTT Cell Viability Assay | Colorimetric measurement of metabolic activity as a proxy for cytotoxicity. | Thiazolyl Blue Tetrazolium Bromide (Sigma M2128). |
| Density Gradient Medium | Purifies nanoparticles and separates them from unencapsulated drug/ligands. | OptiPrep (Iodixanol) for gentle separation. |
| PEGylated Lipid / Polymer | For surface functionalization to create a stealth coating and reduce opsonization. | DSPE-mPEG(2000) or PLGA-PEG copolymers. |
| Zeta Potential Analyzer | Measures surface charge, critical for predicting colloidal stability and protein adsorption. | Instruments: Malvern Zetasizer series. |
| Simulated Biological Buffers | For in vitro degradation studies under physiologically relevant conditions. | PBS (pH 7.4), Acetate Buffer (pH 5.0). |
Technical Support Center
Troubleshooting Guide & FAQs
Q1: During in vitro cytotoxicity assays with ligand-conjugated nanoparticles, we observe higher-than-expected cell death in non-target cell lines. What could be the cause? A: This off-target cytotoxicity is often due to non-specific cellular uptake or ligand-independent interactions. First, verify the integrity of the ligand conjugation via HPLC or MALDI-TOF. A common issue is incomplete purification leading to free, unbound ligand in the solution, which can saturate receptors and cause unpredictable effects. Run a control with the free ligand at the estimated concentration of any unconjugated material. Second, check the nanoparticle's surface charge; a highly positive zeta potential (>+15 mV) can cause non-specific membrane disruption. Aim for a slightly negative or neutral charge for reduced non-specific uptake. Third, confirm receptor expression levels on your non-target cell line using flow cytometry; some "non-target" lines may have low but sufficient receptor density for uptake.
Q2: Our stimuli-responsive nanoparticles show premature payload release in serum before reaching the target site. How can we improve serum stability? A: Premature release is a critical failure mode. This typically indicates an instability in the linker or the nanoparticle core under physiological conditions.
- For pH-sensitive systems: Test the trigger pH threshold. The linker may be too sensitive, reacting at plasma pH (7.4) instead of the intended endosomal pH (5.5-6.0). Consider using a more stable linker like an acetal instead of some hydrazone bonds.
- For enzyme-sensitive systems: Serum contains a multitude of esterases and proteases. Incorporate a poly(ethylene glycol) (PEG) shield or a protective stealth layer to sterically hinder enzyme access. Use a cleavable peptide sequence that is specific to the intracellular enzyme (e.g., cathepsin B) and not abundant in serum.
- General Solution: Perform a stability assay: incubate nanoparticles in 100% FBS at 37°C. Sample at time points (0, 1, 2, 4, 8, 24h) and measure payload content via fluorescence or HPLC. <10% release over 24h is a good benchmark for in vivo applications.
Q3: Our active targeting strategy fails to show a significant improvement in cellular uptake compared to non-targeted (PEGylated) particles in flow cytometry. What steps should we take? A: This points to a failure in the targeting moiety's function.
- Validate Ligand Activity: Test the binding affinity of your conjugated ligand vs. free ligand in a receptor-binding assay (e.g., SPR, ELISA). Conjugation chemistry can damage the ligand's binding epitope.
- Check "PEG Dilemma": The PEG corona, while reducing non-specific uptake, can also sterically shield the targeting ligand. Use a heterobifunctional PEG spacer with the ligand at the distal end. Optimize PEG density; a common range is 5-15 ligand molecules per nanoparticle.
- Confirm Internalization Pathway: Some ligand-receptor complexes are internalized more efficiently than others. Use a pharmacological inhibitor (e.g., chlorpromazine for clathrin-mediated endocytosis) to confirm the expected uptake mechanism is active.
Q4: We observe significant nanoparticle aggregation and increased immunogenic response in murine models, despite in vitro stability. How can we mitigate this? A: In vivo aggregation is often driven by opsonization and protein corona formation, leading to rapid clearance by the MPS and immunogenic reactions.
- Immediate Check: Measure the hydrodynamic diameter and PDI via DLS immediately after reconstitution in PBS and after incubation in mouse plasma for 30 minutes. An increase >20 nm suggests problematic corona-induced aggregation.
- Surface Optimization: Increase PEG surface density and use longer PEG chains (e.g., PEG5000 over PEG2000). Consider "brush" over "mushroom" PEG conformation.
- "Self" Marker: Incorporate a minimal "self" peptide such as CD47 (or its mimetic) to suppress phagocytic uptake by macrophages.
Q5: How do we quantitatively distinguish between specific (ligand-mediated) and non-specific uptake of nanoparticles? A: A standard competitive inhibition protocol is required.
- Pre-incubate target cells with a large excess (10-100x molar concentration) of free targeting ligand for 30 minutes.
- Add fluorescently labeled targeted nanoparticles.
- Incubate, wash, and analyze via flow cytometry or confocal microscopy.
- Calculate: % Specific Uptake = (MFIno inhibitor - MFIwith inhibitor) / MFI_no inhibitor * 100%. MFI = Mean Fluorescence Intensity. A value below 50% indicates a suboptimal targeting system.
Table 1: Comparison of Common Stimuli-Responsive Linkers and Their Properties
| Linker Type | Stimulus | Typical Trigger Point | Payload Release Kinetics (Half-life at trigger point) | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Hydrazone | Acidic pH | pH 5.0-6.0 | 10-60 minutes | Simple chemistry, fast release | Can be unstable in blood (premature release) |
| Acetal | Acidic pH | pH 4.5-5.5 | 30-120 minutes | More stable in plasma than hydrazone | Slower release kinetics, synthesis complexity |
| Disulfide | Reductive (GSH) | 10 mM GSH (vs. 2-20 µM in blood) | 5-30 minutes | High specificity for intracellular environment | Serum stability depends on PEG shielding |
| Valine-Citrulline (vc) | Proteolytic (Cathepsin B) | Enzyme-specific | 1-4 hours | High specificity, used in ADCs | Can be substrate for some serum esterases |
| Tetrazine / TCO | Bioorthogonal (IEDDA) | Presence of partner molecule | Seconds to minutes | Extremely fast, exogenous control | Requires two components, complexity for in vivo |
Table 2: Benchmarking Common Targeting Ligands and Their Parameters
| Ligand | Target Receptor | Typical Conjugation Method | Approx. Ligands/NP Used in Literature | Reported Increase in Cellular Uptake (vs. Non-targeted) | Notes on Immunogenicity |
|---|---|---|---|---|---|
| Folic Acid | Folate Receptor (FR-α) | NHS-PEG-Nanoparticle | 50-200 | 3-8 fold (in FR+ cells) | Generally low immunogenicity |
| Anti-HER2 scFv | HER2/ErbB2 | Maleimide-thiol (from reduced Ab) | 10-30 | 5-15 fold (in HER2+ cells) | Risk of HAMA response (human anti-mouse antibody) |
| RGD Peptide | αvβ3 Integrin | Click Chemistry or Maleimide | 100-500 | 2-5 fold | Can induce pro-inflammatory signaling in some contexts |
| Transferrin | Transferrin Receptor (TfR) | Amine-carboxyl coupling | 20-80 | 4-10 fold | High endogenous levels can cause competition |
| Aptamer (e.g., AS1411) | Nucleolin | Thiol-gold or Carbodiimide | 30-100 | 3-7 fold | Can activate complement system; nuclease sensitivity |
Detailed Experimental Protocols
Protocol 1: Conjugation of Thiol-Terminated Ligands to Maleimide-Functionalized Nanoparticles Objective: To attach a targeting ligand (e.g., an RGD peptide with a terminal cysteine) to a nanoparticle surface via a stable thioether bond. Materials: Maleimide-PEG-Nanoparticles, Thiol-ligand, Nitrogen/Argon gas, PD-10 Desalting Column, Ellman's Reagent. Procedure:
- Purify thiol-ligand via HPLC and confirm concentration. Reduce any disulfide bonds with TCEP (if necessary) and remove TCEP via desalting.
- Flush nanoparticle solution with inert gas (N2/Ar) for 5 minutes to prevent disulfide formation.
- Add a 1.5-2x molar excess of thiol-ligand (relative to maleimide groups on NPs) to the nanoparticle solution. React for 2-4 hours at room temperature under gentle agitation, protected from light.
- Quench the reaction by adding a 10x molar excess of L-cysteine (relative to maleimide) for 1 hour.
- Purify the conjugate via size-exclusion chromatography (PD-10 column equilibrated with PBS) to remove free ligand and quenching agents.
- Verify conjugation using:
- Ellman's Assay: To confirm consumption of free thiols.
- UV-Vis Spectroscopy: If ligand has a distinct absorbance peak.
- DLS/Zeta Potential: To confirm changes in hydrodynamic size and surface charge.
Protocol 2: Assessing pH-Triggered Release Using Dialysis Objective: To quantify the release profile of a payload (e.g., doxorubicin) from pH-sensitive nanoparticles under simulated physiological and acidic conditions. Materials: Dialysis cassettes (10kDa MWCO), PBS (pH 7.4), Acetate buffer (pH 5.0), Fluorescence plate reader. Procedure:
- Prepare nanoparticle samples loaded with a fluorescent payload. Place 1 mL of sample into a dialysis cassette.
- Immerse cassettes in 200 mL of release medium (PBS pH 7.4 or acetate buffer pH 5.0) at 37°C with gentle stirring. Use separate vessels for each pH condition and time point in triplicate.
- At predetermined time points (e.g., 0.5, 1, 2, 4, 8, 12, 24, 48h), withdraw 100 µL from the external release medium for analysis.
- Replace the external medium with fresh, pre-warmed buffer to maintain sink conditions.
- Quantify the payload concentration in the samples using a fluorescence calibration curve.
- Calculate cumulative release as a percentage of the total loaded payload (determined by lysing a separate nanoparticle sample with 1% Triton X-100).
Diagrams
Diagram 1: Key Signaling Pathways in Nanoparticle Immunogenicity & Targeting
Diagram 2: Workflow for Developing & Testing Targeted Stimuli-Responsive NPs
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Heterobifunctional PEG Linkers (e.g., MAL-PEG-NHS, DBCO-PEG-NHS) | Provide controlled spacer between NP and ligand, enabling specific conjugation chemistry while modulating distance and presentation of the ligand. |
| Thiol-Reactive Crosslinkers (e.g., Traut's Reagent, SPDP) | Introduce sulfhydryl groups onto proteins or peptides for subsequent site-specific conjugation to maleimide-functionalized surfaces. |
| TCEP Hydrochloride | A strong, water-soluble reducing agent used to cleave disulfide bonds in antibodies or peptides without affecting other functional groups, preparing them for thiol conjugation. |
| Size-Exclusion Chromatography Columns (e.g., PD-10, Sephadex G-25) | Critical for rapid purification of nanoparticle conjugates from excess free ligands, quenching agents, and organic solvents after reaction. |
| Dynamic Light Scattering (DLS) & Zeta Potential Analyzer | Essential for routine characterization of nanoparticle hydrodynamic diameter, polydispersity index (PDI), and surface charge before and after surface modification. |
| Fluorescent Payload Probes (e.g., Coumarin 6, DiD/DiR, Doxorubicin) | Allow tracking of nanoparticle uptake (flow cytometry/confocal) and payload release kinetics (fluorescence spectrometry) without requiring complex assays. |
| Competitive Ligands/Receptor Blockers (e.g., free folic acid, RGD peptide, anti-receptor antibodies) | Used in inhibition controls to confirm the specificity of active targeting mediated uptake in cellular experiments. |
| Protein Corona Analysis Kits (e.g., for SDS-PAGE, LC-MS sample prep) | Facilitate the isolation and identification of proteins adsorbed onto nanoparticles, key for understanding in vivo behavior and immunogenicity. |
Technical Support Center: Troubleshooting Nanoparticle Immunogenicity & Cytotoxicity Assays
FAQ 1: My in vitro cell viability assay (e.g., MTT, LDH) shows low cytotoxicity, but in vivo I observe significant inflammatory cell infiltration. What could cause this discrepancy?
- Answer: This is a common issue indicating that standard cytotoxicity assays may not capture immunogenic cell death (ICD) or subtle pro-inflammatory signaling. In vitro assays measure primary necrosis/apoptosis, while in vivo infiltration is driven by immune recognition. Key checks:
- Assay Scope: Confirm your viability assay measures only metabolic activity or membrane integrity, not damage-associated molecular patterns (DAMPs) release.
- Cell Type: Were assays performed only on the target cell line (e.g., HeLa) or also on relevant immune cells (e.g., macrophages, dendritic cells)? Use co-culture systems.
- NP Persistence: In vivo, NPs may accumulate in organs (liver, spleen) and be processed by phagocytes not present in your in vitro model.
- Protein Corona: The in vivo corona formation can drastically alter NP-cell interactions.
- Recommended Protocol: In Vitro Immunogenic Potential Screen
- Seed THP-1 derived macrophages or primary murine bone-marrow-derived dendritic cells (BMDCs) in 24-well plates.
- Treat cells with a titration of your NPs (e.g., 10, 50, 100 µg/mL) for 6-24 hours.
- Collect supernatant for ELISA analysis of IL-1β, IL-6, TNF-α.
- Analyze cell surface markers (e.g., CD80, CD86, MHC-II) via flow cytometry.
- Correlate low-level cytokine release (e.g., 2-5 fold increase over control) with your in vivo findings.
FAQ 2: How do I quantitatively distinguish a "low-level" desirable immune response from a detrimental one?
- Answer: This requires multi-parameter profiling. A "low-level desirable" response is typically transient, enhances specific adaptive immunity (e.g., for vaccines), and does not cause immunopathology. Use the following comparative table to guide interpretation.
Table 1: Quantitative Parameters for Classifying Low-Level Immune Responses
| Parameter | "Desirable" Low Response (e.g., Vaccine Adjuvant) | "Detrimental" Low Response (e.g., Chronic Inflammation) |
|---|---|---|
| Cytokine Peak (e.g., IL-6) | 2-10 fold increase, returns to baseline in 24-48h. | Sustained >2-fold increase lasting >72h. |
| Immune Cell Infiltration | Localized, antigen-presenting cell (APC) rich (e.g., DCs, M1 macrophages). | Widespread, neutrophil/lymphocyte dominant, progressing to fibrosis. |
| Antigen-Specific T-cells | Significant increase in IFN-γ+ CD8+ T-cells upon rechallenge. | Minimal or absent antigen-specific memory. |
| Systemic Biomarkers | No significant change in serum acute phase proteins (e.g., CRP). | Elevated serum CRP/SAA over time. |
| Histopathology Score | Mild, transient inflammation (Score 1-2). | Progressive, granulomatous or lymphoid aggregate formation (Score ≥3). |
FAQ 3: My nanoparticle is intended for a vaccine. What specific assays confirm a beneficial low-level response?
- Answer: Beyond cytokine profiling, you must demonstrate functional antigen-specific immunity.
- Experimental Protocol: Antigen-Specific T-cell Priming Assay (ELISpot)
- Immunize mice (n=5/group) with (a) NP-antigen conjugate, (b) Antigen alone, (c) Adjuvant (e.g., Alum) + Antigen.
- After 10-14 days, isolate splenocytes.
- Perform IFN-γ ELISpot: Plate splenocytes (2x10^5/well) with antigen peptides (10 µg/mL).
- Develop spots per manufacturer's protocol.
- Quantify: A "desirable low response" from your NP may show spot counts significantly higher than antigen alone but comparable to or slightly less than a strong adjuvant like Alum, indicating sufficient priming without excessive reactogenicity.
- Experimental Protocol: Antigen-Specific T-cell Priming Assay (ELISpot)
Signaling Pathways in Nanoparticle Immunogenicity
Experimental Workflow for Immunogenicity Risk Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Nanoparticle Immunogenicity Research
| Reagent / Material | Function / Purpose | Example Vendor(s) |
|---|---|---|
| THP-1 Cell Line | Human monocytic line; can be differentiated into macrophage-like cells for consistent in vitro immunogenicity screening. | ATCC, Sigma-Aldrich |
| LAL Endotoxin Assay Kit | Quantifies bacterial endotoxin contamination on NPs, a major confounder in immune activation studies. | Lonza, Thermo Fisher |
| Luminex/Multiplex Cytokine Panel | Allows simultaneous quantification of 20+ cytokines/chemokines from small sample volumes for comprehensive profiling. | Bio-Rad, R&D Systems |
| NLRP3 Inflammasome Inhibitor (MCC950) | Specific inhibitor to determine the contribution of the NLRP3 pathway to IL-1β release. | Cayman Chemical, Sigma-Aldrich |
| Recombinant Human/Mouse Serum Albumin | Used to form a controlled "protein corona" in vitro to mimic in vivo conditions more accurately. | Sigma-Aldrich, Millipore |
| Fluorescently-Labeled Nanoparticles | Allows tracking of cellular uptake and biodistribution in both in vitro and in vivo models. | Custom synthesis from companies like NanoComposix |
| Annexin V / Propidium Iodide Kit | Distinguishes between apoptotic and necrotic cell death; necrosis is more immunogenic. | Thermo Fisher, BioLegend |
| ELISpot Kit (IFN-γ, IL-4) | Gold standard for quantifying low-frequency, antigen-specific T-cell responses in immunized animals. | Mabtech, BD Biosciences |
Benchmarking and Validation: Comparative Frameworks for Nanoparticle Safety Assessment
Technical Support Center: Troubleshooting Cytotoxicity & Immunogenic Response Assays
FAQs & Troubleshooting Guides
Q1: Our liposomal (DSPC/Cholesterol) formulation shows high batch-to-batch variability in hemolysis assays. What could be the cause? A: Primary causes are often inconsistencies in lipid film hydration, extrusion parameters, or residual solvent. Ensure complete chloroform evaporation under vacuum (>2 hrs), consistent buffer (e.g., PBS, pH 7.4) temperature during hydration (60°C for DSPC), and use a calibrated thermobaric extruder with defined polycarbonate membrane pore size (e.g., 100 nm, 21 passes). Measure Polydispersity Index (PDI) via DLS; target PDI <0.1.
Q2: Poly(lactic-co-glycolic acid) (PLGA) nanoparticles precipitate during PEGylation. How can this be prevented? A: Precipitation indicates colloidal instability during surface modification. Use a slower, dropwise addition (e.g., 0.1 mL/min) of the activated PEG (e.g., mPEG-NHS) solution into the stirring NP suspension under mild conditions (4°C, pH 8.5 borate buffer). Pre-purify NPs via gel filtration to remove unreacted polymers before PEGylation. Increase ionic strength slightly (0.15 M NaCl) to shield charges.
Q3: Gold nanoparticles (AuNPs) give inconsistent results in the MTT assay for cytotoxicity. What is the interference, and how do we mitigate it? A: AuNPs can catalytically degrade MTT formazan or adsorb the dye, leading to false signals. Solution: Use interference-free assays like CellTiter-Glo (luminescence-based ATP quantitation) or Alamar Blue (resazurin reduction). If using MTT, include a nanoparticle-only control (no cells) and perform thorough washing steps (3x with PBS) before formazan solubilization. Validate with a lactate dehydrogenase (LDH) release assay.
Q4: Our multi-walled carbon nanotubes (MWCNTs) trigger high IL-1β secretion in THP-1 macrophages, suggesting NLRP3 inflammasome activation. How do we confirm this specifically? A: Follow this confirmatory protocol: 1) Pre-treat cells with a specific NLRP3 inhibitor (e.g., MCC950, 10 µM) for 1 hr prior to MWCNT exposure. 2) Measure caspase-1 activation via a FLICA assay or Western blot. 3) Perform siRNA knockdown of ASC or NLRP3 and re-measure IL-1β (ELISA). A positive control (e.g., nigericin) and negative control (LPS-priming alone) are mandatory.
Q5: Silica nanoparticles show unexpected high complement (C3a) activation in human serum. Which surface property is likely responsible? A: Positively charged (aminosilane-modified) surfaces or highly hydrophobic patches strongly activate the complement system via the alternative pathway. Troubleshooting: Consider coating with dense PEG brushes (MW >5k Da) or functionalizing with complement inhibitor molecules (e.g., Factor H mimetics). Characterize surface ζ-potential in serum-containing media (target near-neutral).
Table 1: Typical Physicochemical Properties & In Vitro Cytotoxicity Ranges
| Nanomaterial Class | Common Size Range (nm) | Typical PDI | Common ζ-Potential (mV) | Typical IC50 (Cell Viability) | Common Immunogenic Readout (Level) |
|---|---|---|---|---|---|
| Liposomes (PEGylated) | 80 - 120 | 0.05 - 0.10 | -5 to -15 | >1000 µg/mL (often non-toxic) | Complement activation (Low-Medium) |
| PLGA NPs | 150 - 200 | 0.10 - 0.20 | -20 to -30 | 200 - 500 µg/mL | IL-6, TNF-α secretion (Low) |
| Gold NPs (Citrate) | 10 - 30 | 0.15 - 0.25 | -30 to -40 | 50 - 200 µg/mL | ROS generation (High) |
| Mesoporous Silica NPs | 60 - 100 | 0.10 - 0.15 | -20 to -25 | 100 - 300 µg/mL | Inflammasome activation (Medium) |
| Carbon Nanotubes (MWCNT) | Diameter: 10-20, Length: 500-2000 | N/A | +10 to -10 | 10 - 50 µg/mL | IL-1β, TGF-β secretion (High) |
Table 2: Standard Assay Suitability & Known Interferences
| Assay | Best For | Avoid For (Interference) | Recommended Alternative Assay |
|---|---|---|---|
| MTT Formazan | Polymeric NPs, Liposomes | Inorganic NPs (Catalytic), Carbon-based (Adsorption) | CellTiter-Glo, Alamar Blue |
| LDH Release | All classes | NPs causing membrane damage at high dose | Use in tandem with viability assay |
| ELISA (Cytokines) | All classes | NPs that adsorb proteins/cytokines | Include particle-only controls |
| Hemolysis (RBCs) | IV-administrable formulations | NPs that aggregate in saline | Use fresh blood, isotonic conditions |
| Oxidative Stress (DCFH-DA) | All classes | NPs that fluoresce in same channel | DHE for superoxide, specific probes |
Experimental Protocol: Comprehensive In Vitro Immunogenicity Assessment
Title: Protocol for NLRP3 Inflammasome Activation & Cytokine Storm Profiling
Objective: To systematically evaluate nanoparticle-triggered innate immune responses in human macrophages.
Materials:
- THP-1 cells (human monocytic line)
- Phorbol 12-myristate 13-acetate (PMA)
- Ultrapure LPS (for priming)
- Test nanoparticles (sterile, in PBS)
- NLRP3 inhibitor (MCC950)
- Caspase-1 FLICA kit
- ELISA kits for human IL-1β, IL-6, TNF-α
- Cell culture reagents
Methodology:
- Differentiation: Seed THP-1 cells at 1x10^5 cells/well in a 96-well plate. Treat with 100 nM PMA for 48 hours to differentiate into adherent macrophages.
- Priming: Wash cells. Prime with 100 ng/mL LPS in serum-free media for 3 hours.
- Inhibition Control: Add MCC950 (10 µM) to designated wells 1 hour before nanoparticle exposure.
- Nanoparticle Exposure: Add a concentration series of nanoparticles (e.g., 10, 50, 100 µg/mL) in fresh, serum-free media. Incubate for 6 hours (acute cytokine release) or 24 hours (sustained response).
- Sample Collection: Centrifuge supernatant at 300 x g for 5 min. Collect for ELISA analysis.
- Caspase-1 Activity: For adherent cells, add FLICA probe per kit instructions and quantify via fluorescence microscopy or flow cytometry.
- ELISA: Perform cytokine ELISAs on supernatants following manufacturer protocols. Include standard curves.
- Viability: Perform parallel CellTiter-Glo assay on replicate wells to normalize cytokine data to viable cell count.
Visualizations
Diagram 1: NLRP3 Inflammasome Activation Pathway by NPs
Diagram 2: Experimental Workflow for NP Immunogenicity Screening
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Cytotoxicity & Immunogenicity Studies
| Reagent/Solution | Function & Rationale | Example Product/Catalog |
|---|---|---|
| CellTiter-Glo Luminescent Assay | ATP quantitation for viability; minimal interference from most nanomaterials. | Promega, G7570 |
| Pierce LDH Cytotoxicity Assay | Measures membrane integrity via lactate dehydrogenase release. | Thermo Fisher, 88953 |
| Ultra-Pure LPS (E. coli) | Reliable TLR4 priming agent for inflammasome studies; avoids unwanted TLR2 activation. | InvivoGen, tlrl-3pelps |
| MCC950 (CP-456773) | Specific, potent small-molecule inhibitor of NLRP3 inflammasome. Critical for mechanistic confirmation. | Cayman Chemical, 24645 |
| Caspase-1 FLICA Assay (FAM-YVAD-FMK) | Fluorescent probe for in situ detection of active caspase-1. | ImmunoChemistry, 98 |
| Human Cytokine ELISA DuoSet | High-sensitivity, matched antibody pairs for accurate IL-1β, IL-6, TNF-α quantification. | R&D Systems, DY201, DY206, DY210 |
| Sterile, Endotoxin-Free PBS | Critical for NP dispersion/dosing to avoid false immunogenicity from endotoxin. | Corning, 21-040-CV |
| Dispersion Media (0.1% BSA/PBS) | Prevents NP aggregation in biological buffers, improving exposure consistency. | Prepare in-house (Sigma A7906) |
Technical Support Center
Troubleshooting Guide & FAQs
FAQ 1: My MTT assay for nanoparticle (NP) cytotoxicity shows high background absorbance or inconsistent formazan crystal formation. How do I troubleshoot this?
- A: This is often due to NP-interference. Follow this protocol:
- Confirm Interference: Run an "NP-only" control (nanoparticles + MTT + media, no cells). High absorbance indicates MTT reduction or light scattering by NPs.
- Mitigation Protocol: If interference is confirmed, use an ISO 19007:2018-guided washing step. After NP incubation, aspirate media, wash cells 2x with pre-warmed PBS or serum-free medium, then add fresh MTT solution. This removes extracellular NPs.
- Alternative Assay: Switch to a resazurin-based (Alamar Blue) assay (ISO 10993-5), which typically has less NP interference, or a membrane integrity assay like lactate dehydrogenase (LDH) release (OECD TG 487).
FAQ 2: When testing for NP-induced immunogenic cell death (ICD), my ATP release (a key Damage-Associated Molecular Pattern - DAMP) measurements are erratic. What could be wrong?
- A: Erratic ATP release data usually stems from rapid ATP degradation or cell handling issues.
- Protocol Standardization: Adopt the Nanomedicine Consortium's pre-analytical checklist:
- Use a validated, luciferase-based ATP detection kit.
- Pre-warm all reagents to 37°C.
- Critical Step: Immediately post-incubation, place the culture plate on ice and add the ATP detection reagent directly to the well without collecting supernatant. Perform a cell lysis-based measurement to capture total released ATP before degradation.
- Centrifuge samples at 4°C if supernatant measurement is required.
- Control: Include a positive control (e.g., cells treated with 1-10µM mitoxantrone, a known ICD inducer) and a negative control (vehicle-only) in every experiment.
- Protocol Standardization: Adopt the Nanomedicine Consortium's pre-analytical checklist:
FAQ 3: How do I choose the right endotoxin detection method for my nanomedicine formulation, as per guidelines?
- A: Endotoxin testing is critical for immunogenic response research (FDA/ICH). The choice depends on your NP.
| Method | Principle | NP Interference Risk | Recommended Guideline |
|---|---|---|---|
| Limulus Amebocyte Lysate (LAL) Gel-Clot | Gel formation | High (NPs can adsorb enzymes) | FDA Guideline on LAL, ISO 29701 |
| Chromogenic LAL | Colorimetric readout | Moderate-High (color quenching/scattering) | ISO 29701 |
| Recombinant Factor C (rFC) | Fluorescence readout | Lower (simpler cascade) | Preferential per newer consortia (e.g., EUNCL) |
- Troubleshooting Protocol: If you suspect interference (low spike recovery), perform a validated sample dilution as per ISO 29701. Use endotoxin-free water or buffer to dilute the sample 1:10, 1:100, etc., and re-test. A proportional increase in detected endotoxin confirms interference was present in the concentrated sample.
FAQ 4: My flow cytometry results for NP uptake show high autofluorescence, masking specific signals. How can I resolve this?
- A: Autofluorescence is common with certain NPs (e.g., carbon-based, some metal oxides).
- Experimental Controls: Always include an unstained NP-treated sample to set compensation and gating thresholds.
- Protocol Adjustment: Use far-red or infrared fluorescent probes (e.g., Alexa Fluor 647, 750) instead of FITC or PE, as cellular autofluorescence is lower in these channels.
- Validated Washing: Implement a stringent washing protocol from OECD GD 317: Wash cells 3x with cold PBS containing 0.1% BSA and 2mM EDTA. Analyze cells immediately or fix with 1% PFA (if compatible with downstream assays).
- Alternative Validation: Correlate flow data with a quantitative, non-optical method like inductively coupled plasma mass spectrometry (ICP-MS) for metal-based NPs.
Key Experimental Protocols
Protocol 1: ISO 19007-Compliant In Vitro Cytotoxicity Assessment with Interference Checks
- Objective: Reliably assess NP cytotoxicity using MTT.
- Materials: NP suspension, cell line, complete medium, MTT reagent, DMSO, multi-well plate reader.
- Procedure:
- Seed cells in 96-well plate. Incubate 24h.
- Treat with NP serial dilutions. Include cell-only (negative control), vehicle control, and a positive control (e.g., 1% Triton X-100).
- Crucial Step: After treatment, wash all wells 2x with pre-warmed PBS to remove extracellular NPs.
- Add fresh, serum-free medium containing MTT (0.5 mg/mL final). Incubate 2-4h.
- Carefully aspirate MTT medium, add DMSO to solubilize formazan.
- Measure absorbance at 570 nm, reference 650 nm.
- Validation: Run parallel "NP-only" wells (no cells) at all concentrations to subtract any background signal.
Protocol 2: Assessing Immunogenic Cell Death (ICD) Markers (ATP & HMGB1)
- Objective: Quantify release of key DAMPs indicating NP-induced ICD.
- Materials: NP, ICD-positive control (eoxantrone), ATP assay kit, HMGB1 ELISA kit, cell culture materials.
- Procedure for ATP (Extracellular):
- Treat cells in a white-walled 96-well plate for desired time.
- On ice, collect 50µL supernatant into a separate tube.
- Add 50µL of ATP detection reagent (lysing type) directly to the original well to measure total cellular ATP (optional internal control).
- To the supernatant tube, add 50µL of ATP detection reagent. Measure luminescence immediately.
- Procedure for HMGB1 (Extracellular):
- Treat cells in a 12-well plate.
- Collect supernatant, centrifuge at 500xg for 5 min to remove debris.
- Analyze supernatant immediately or store at -80°C.
- Perform HMGB1 ELISA according to manufacturer's protocol, using undiluted or minimally diluted sample to preserve low-concentration signals.
Visualization
Diagram 1: NP Cytotoxicity & Immunogenicity Assessment Workflow
Diagram 2: Key Signaling in NP-Induced Immunogenic Cell Death
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Purpose | Guideline Reference |
|---|---|---|
| Standard Reference Nanomaterials (e.g., Au Citrate, SiO₂, PS nanoparticles) | Positive/Negative controls for assay validation and inter-laboratory comparison. | OECD TG 318, ISO/TS 21362 |
| Recombinant Factor C (rFC) Endotoxin Assay Kit | Detects endotoxin with minimal nanoparticle interference compared to traditional LAL. | ISO 29701, EUNCL-PCC guidelines |
| Resazurin Sodium Salt | Viability indicator dye; often less prone to NP interference than MTT. | ISO 10993-5 |
| ATP Bioluminescence Assay Kit (Cell Lysis Format) | Quantifies ATP release as a key DAMP for Immunogenic Cell Death assessment. | N/A (Consortium Best Practice) |
| HMGB1 ELISA Kit | Quantifies extracellular HMGB1, a late-stage DAMP signaling immunogenicity. | N/A (Consortium Best Practice) |
| Fluorescent Probes (e.g., Alexa Fluor 647-conjugated antibodies) | For flow cytometry; minimizes interference from NP autofluorescence. | N/A (Experimental Optimization) |
| Endotoxin-Free Water & Buffers | Critical for all sample preparation and dilution to avoid false positive immunogenic signals. | FDA Guideline on LAL |
| Serum Albumin (BSA) | Used in washing buffers (PBS + 0.1% BSA) to prevent non-specific NP binding in flow cytometry. | OECD GD 317 |
This technical support center provides guidance for troubleshooting common experimental challenges in nanoparticle immunogenicity and cytotoxicity research, framed within the thesis of advancing safe nanotherapeutic development.
Troubleshooting Guides & FAQs
Q1: In our in vitro cytotoxicity assay (e.g., MTT), we observe high background cell death even in negative controls with "blank" nanoparticles. What could be the cause? A: This is often due to residual synthesis reagents (e.g., solvents, initiators, catalysts) or endotoxin contamination.
- Troubleshooting Steps:
- Purification: Implement stringent purification post-synthesis: dialysis (≥ 72h with frequent buffer changes), tangential flow filtration, or size-exclusion chromatography.
- Endotoxin Testing: Use a Limulus Amebocyte Lysate (LAL) assay. Work under sterile, pyrogen-free conditions.
- Control: Include a "vehicle-only" control (the purified suspension buffer) to isolate particle effects from medium effects.
Q2: Our PEGylated nanoparticle shows unexpected accelerated blood clearance (ABC) and anti-PEG immunogenicity in in vivo models. How can we investigate this? A: The ABC phenomenon is often driven by anti-PEG IgM antibodies.
- Investigation Protocol:
- Serum Analysis: Collect serum pre- and post-injection. Use an ELISA to detect anti-PEG IgM/IgG.
- PEG Conformation: Analyze PEG density and surface conformation (e.g., using X-ray photoelectron spectroscopy). Low-density or unstable PEG coating ("mushroom" vs. "brush" conformation) increases immunogenicity.
- Alternative Stealth Polymers: Test nanoparticles coated with poly(N-vinylpyrrolidone) (PVP) or poloxamers as comparators.
Q3: Nanoparticles intended for passive tumor targeting are accumulating in the liver and spleen, indicating high clearance by the mononuclear phagocyte system (MPS). How can we reduce this? A: This indicates insufficient "stealth" properties.
- Optimization Guide:
- Surface Charge: Ensure a near-neutral zeta potential (between -10 mV and +10 mV). Highly positive or negative surfaces promote opsonization.
- Hydrophilicity: Increase surface hydrophilicity via optimal PEGylation or other hydrophilic polymer coatings.
- "Self" Marker: Explore functionalization with "self" peptides (e.g., derived from CD47) to inhibit phagocytic signaling.
Summarized Data from Key Case Studies
Table 1: Clinical Trial Challenges from Nanoparticle Immunogenicity/Toxicity
| Nanoparticle Platform | Indication | Phase | Key Challenge (Immunogenicity/Toxicity) | Root Cause Identified | Outcome/Resolution |
|---|---|---|---|---|---|
| PEGylated Liposomal Doxorubicin | Various Cancers | Marketed | Complement Activation-Related Pseudoallergy (CARPA) | PEG and/or liposome surface triggering immune cascade in sensitive patients. | Pre-medication with antihistamines/steroids; slow infusion rate. |
| LNPs for siRNA (patisiran) | hATTR Amyloidosis | Marketed | Mild to moderate infusion-related reactions | Reactogenicity potentially linked to ionizable lipid or PEG-lipid component. | Managed with pre-treatment corticosteroids, antihistamines, and slower infusion. |
| Poly(lactic-co-glycolic acid) (PLGA) NPs | Oncology (Trials) | Preclinical/Phase I | Inflammatory response & unintended dendritic cell activation | Degradation products (acidic monomers) and residual PVA surfactant. | Focus on rigorous purification and co-encapsulation of anti-inflammatory agents. |
| Carbon Nanotubes (Therapeutic) | Various | Preclinical | Persistent granulomatous inflammation & fibrosis | High aspect ratio, biopersistence, and metal catalyst impurities. | Shift towards highly purified, shortened, and functionally coated nanotubes. |
Detailed Experimental Protocols
Protocol 1: Assessing Nanoparticle-Induced Complement Activation (In Vitro)
Aim: To evaluate the potential of nanoparticles to activate the complement cascade, a key immunogenicity and toxicity pathway.
- Incubation: Mix 100 µL of human serum (pooled healthy donor) with 100 µL of nanoparticle suspension (at relevant in vivo concentrations) in a low-binding tube.
- Control: Include zymosan (positive control) and PBS (negative control).
- Condition: Incubate at 37°C for 1 hour with gentle agitation.
- Termination: Place samples on ice to stop complement activity.
- Detection (ELISA): Use commercial ELISA kits to quantify key activation products (e.g., C3a, C5a, SC5b-9) in the supernatant according to manufacturer instructions.
- Analysis: Express data as fold-increase over the PBS negative control.
Protocol 2: ComprehensiveIn VitroImmunogenicity Profiling (Dendritic Cell Assay)
Aim: To profile the innate and adaptive immunogenic potential of nanoparticles by assessing dendritic cell (DC) maturation.
- DC Culture: Differentiate human monocyte-derived DCs from CD14+ monocytes using IL-4 and GM-CSF over 5-7 days.
- Nanoparticle Exposure: Harvest immature DCs and expose them to nanoparticles at a range of sub-cytotoxic concentrations (determined via MTT/LDH assay). Use LPS as a positive control for maturation.
- Incubation: Culture for 24-48 hours.
- Analysis:
- Surface Markers: Analyze via flow cytometry for upregulated maturation markers (CD83, CD86, HLA-DR).
- Cytokine Secretion: Measure pro-inflammatory cytokines (IL-6, IL-12p70, TNF-α) in supernatant via ELISA or multiplex assay.
- Interpretation: A significant increase in maturation markers and cytokine secretion indicates an adjuvant-like immunogenic risk.
Visualizations
Diagram 1: CARPA Signaling Pathway
Title: Complement Cascade Leading to CARPA
Diagram 2: Nanoparticle Immunogenicity Assessment Workflow
Title: Immunogenicity Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Nanoparticle Immuno/Toxicity Research
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| LAL Endotoxin Assay Kit | Quantifies endotoxin contamination, a major confounder in immunogenicity studies. | Choose a high-sensitivity format (e.g., chromogenic). Use pyrogen-free labware. |
| Human/Animal Serum | Source of opsonins and complement proteins for in vitro hemolysis, protein corona, and activation studies. | Use pooled donors to account for variability. Heat-inactivate for specific controls. |
| ELISA Kits (C3a, C5a, SC5b-9, Cytokines) | Quantifies specific immune activation biomarkers from in vitro or ex vivo samples. | Validate kit compatibility with nanoparticle-containing samples (may require dilution). |
| Differentiation Kits for Human DCs & Macrophages | Generates consistent, primary innate immune cells for functional assays. | Crucial for standardized immunogenicity profiling between different NP batches. |
| PEG Detection ELISA | Measures anti-PEG antibody titers in serum to investigate the ABC phenomenon. | Distinguish between IgM and IgG isotypes for mechanistic insight. |
| High-Resolution Flow Cytometer | Analyzes immune cell surface marker expression (activation/maturation) and phagocytosis. | Use of pHrodo-labeled NPs allows for quantitative phagocytosis assays. |
| DLS/Zeta Potential Analyzer | Measures hydrodynamic size, PDI, and surface charge—critical for understanding MPS clearance. | Always measure in physiologically relevant buffers (e.g., PBS, cell culture medium). |
Predictive Computational Models and High-Throughput Screening Approaches for Early-Stage De-Risking
Technical Support Center: Troubleshooting & FAQs for Nanoparticle Cytotoxicity & Immunogenicity Research
Q1: Our in vitro cytotoxicity assay (e.g., MTT, LDH) shows inconsistent results between replicates when testing polymeric nanoparticles. What are the primary causes?
A1: Inconsistency often stems from nanoparticle interference with assay reagents or improper dispersion. Key troubleshooting steps:
- Assay Interference: Some nanoparticles can adsorb assay dyes/formazan crystals or catalyze redox reactions. Run an interference control (nanoparticles + assay reagents without cells).
- Dispersion & Stability: Ensure nanoparticles are freshly and uniformly dispersed in cell culture medium using a standardized protocol (e.g., bath sonication for 30 seconds before each treatment). Aggregation causes variable cell exposure.
- Serum Effects: The protein corona formed in serum-containing media alters nanoparticle-cell interaction. Maintain consistent serum concentration (e.g., 10% FBS) across all wells and pre-incubate nanoparticles in medium for 30 min before adding to cells.
Detailed Protocol: Standardized Nanoparticle Dispersion for In Vitro Assays
- Suspend nanoparticles in sterile PBS or culture medium at 2x the desired final concentration.
- Sonicate using a bath sonicator (e.g., 40 kHz) for 10 minutes at room temperature.
- Vortex the suspension for 30 seconds immediately before adding it to an equal volume of 2x concentrated cell culture medium containing serum.
- Mix by gentle pipetting and incubate at 37°C for 30 minutes to allow corona formation.
- Apply the suspension directly to cells. Always include a vehicle control treated with the same protocol.
Q2: Our predictive model, trained on in vitro hemolysis data, fails to correlate with in vivo immunogenic response (e.g., complement activation). What's missing from our feature set?
A2: In vitro hemolysis primarily reflects membrane disruption, while in vivo immunogenicity involves complex protein interactions. Essential missing features likely include:
- Surface Adsorption Descriptors: Quantify nanoparticle propensity to adsorb key plasma proteins (e.g., fibrinogen, immunoglobulins, complement C3) using computational models like molecular dynamics or QSAR descriptors for protein binding.
- Surface Topography & Hydrophobicity: Features describing nanoscale roughness and patch hydrophobicity that drive protein adsorption conformation, leading to "corona" that dictates immune recognition.
- Complement Activation Potential: Incorporate in silico docking scores or quantitative structure-activity relationship (QSAR) models predicting binding affinity to complement pathway components (e.g., C1q, Factor B).
Table 1: Key Feature Categories for Predicting Immunogenic Response
| Feature Category | Specific Descriptors (Examples) | Predictive Goal | Recommended In Vitro Validation Assay |
|---|---|---|---|
| Physicochemical | Hydrodynamic diameter (nm), Zeta potential (mV), Polydispersity Index | Colloidal stability & cellular uptake | DLS, NTA, TEM |
| Surface Chemistry | Hydrogen bond donor/acceptor count, Topological polar surface area, Hydrophobicity index | Protein corona composition | LC-MS/MS of isolated corona |
| Biological Interaction | Molecular docking score with C1q, Albumin binding free energy (ΔG), Fibrinogen adsorption score | Innate immune activation | CH50 assay, ELISA for SC5b-9 |
Q3: During high-throughput screening (HTS) of nanoparticle libraries for cytotoxicity, our automated imaging shows high well-to-well cross-talk in fluorescent readouts (e.g., Calcein AM for viability). How can we mitigate this?
A3: This is common with nanoparticles that scatter/absorb light or quench fluorescence.
- Solution 1: Optimize Wavelengths. Use far-red or near-infrared dyes (e.g., DRAQ7 for dead cell staining) instead of GFP/FITC channels, as nanoparticles have lower interference at longer wavelengths.
- Solution 2: Implement Washed Assays. Change protocol from "add-and-read" to include a wash step (automated) after staining to remove uninternalized nanoparticles that cause interference. Use centrifugation-compatible plates.
- Solution 3: Utilize Label-Free HTS. Switch to impedance-based (e.g., RTCA) or brightfield image-based (cell confluence/morphology) assays to avoid optical artifacts entirely.
Diagram: High-Throughput Screening Workflow with Mitigation Steps
Q4: We want to establish a predictive model for nanoparticle-induced pyroptosis. Which key in vitro readouts should we feed into the computational model?
A4: Focus on causal, quantitative markers of pyroptosis pathway activation beyond general cytotoxicity.
- Primary High-Content Features: Caspase-1 activation (FLICA assay), plasma membrane porosity (propidium iodide influx kinetics), and release of mature IL-1β (ELISA).
- Secondary Confirmation Features: GSDMD cleavage (western blot) and extracellular ATP release (luminescence assay).
- Morphological Features: From live-cell imaging, quantify cell swelling (increased diameter) and rapid propidium iodide uptake dynamics.
Detailed Protocol: High-Content Analysis of Pyroptosis In Vitro
- Seed THP-1 macrophages (differentiated with PMA) in a 96-well imaging plate.
- Treat with nanoparticles +/- LPS priming (100 ng/mL, 3 hours) and Nigericin control.
- Load with Caspase-1 FLICA 660 probe and Propidium Iodide (PI) for the final 30 minutes of treatment.
- Image using a high-content imager with 20x objective. Acquire in FITC (cell mask), Cy5 (FLICA), and TRITC (PI) channels every 15 minutes for 3-6 hours.
- Analysis: Use image analysis software to quantify:
- % FLICA-positive cells (activated Caspase-1).
- Kinetics of PI uptake (slope of intensity increase).
- Correlation between FLICA positivity and early PI entry.
Diagram: Key Signaling in Nanoparticle-Induced Pyroptosis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for De-Risking Cytotoxicity & Immunogenicity
| Reagent / Material | Function in Experimental Context | Key Consideration for Nanoparticles |
|---|---|---|
| AlamarBlue / Resazurin | Fluorescent redox indicator for cell viability. | Less prone to nanoparticle interference than MTT formazan. Validate for interference. |
| Lactate Dehydrogenase (LDH) | Enzyme released upon membrane damage. | Use washed protocols; nanoparticles can cause false-positive LDH inhibition. |
| Propidium Iodide (PI) | DNA intercalating dye for dead cells/membrane pores. | Use kinetic reads for pyroptosis; static endpoint can be misleading. |
| Caspase-1 FLICA Probe | Fluorochrome-labeled inhibitor probe binds active caspase-1. | Gold standard for inflammasome activation. Requires live-cell imaging/flow cytometry. |
| PolySorbate 80 (Tween 80) | Non-ionic surfactant for nanoparticle dispersion. | Use at low, consistent concentrations (e.g., 0.01%) to prevent colloidal instability. |
| Human Plasma-Derived Serum | Serum for corona formation studies. | Prefer over FBS for immunogenicity assays for human-relevant protein corona. |
| CH50 Complement Assay Kit | Measures total classical complement pathway activity. | Use to validate in silico predictions of complement activation. |
| 96-well Impedance Plates (e.g., ACEA xCelligence) | Label-free, real-time cell monitoring. | Ideal for HTS; unaffected by optical interference from nanoparticles. |
| Molecular Dynamics Software (e.g., GROMACS) | Simulates nanoparticle-protein interactions at atomic scale. | Generates binding energy data for predictive model features. |
Conclusion
The journey to clinically successful nanotherapeutics necessitates a rigorous and holistic approach to understanding and managing cytotoxicity and immunogenicity. As explored through the foundational mechanisms, methodological assessments, optimization strategies, and validation frameworks, these responses are not mere obstacles but integral design parameters. The key takeaway is that safety is not an afterthought but must be engineered into nanoparticles from their inception through deliberate material choice, surface modification, and targeted design. Future directions point toward more predictive in silico and organ-on-a-chip models, personalized approaches considering patient-specific immune status, and the strategic harnessing of immunogenicity for vaccine and immunotherapy applications. By mastering this double-edged sword, researchers can unlock the full, safe potential of nanomedicine for transformative patient care.