Optimizing Nanoparticle Drug Delivery: Bridging the Translational Gap from Bench to Bedside
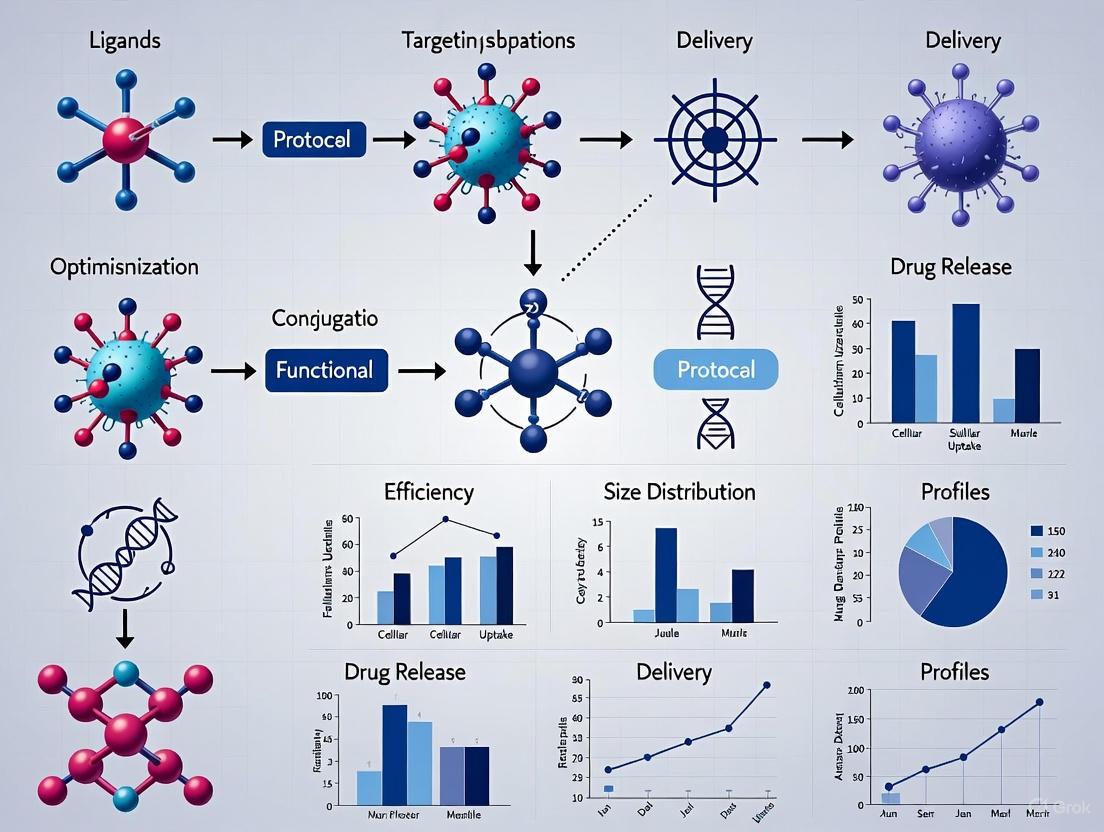
This article provides a comprehensive guide for researchers and drug development professionals on optimizing nanoparticle-based drug delivery protocols.
Optimizing Nanoparticle Drug Delivery: Bridging the Translational Gap from Bench to Bedside
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on optimizing nanoparticle-based drug delivery protocols. It addresses the critical translational gap in nanomedicine, where despite extensive preclinical research, fewer than 0.1% of nanomedicines achieve clinical approval. The content explores foundational principles of nanoparticle design, advanced formulation methodologies including lipid and polymer-based platforms, and innovative troubleshooting strategies leveraging artificial intelligence and machine learning. It further covers critical validation and comparative analysis techniques essential for ensuring safety, efficacy, and manufacturability. By integrating recent advances in computational modeling, AI-driven design, and novel formulation technologies, this resource aims to equip scientists with practical strategies to enhance nanoparticle delivery efficiency, overcome biological barriers, and accelerate the development of clinically viable nanotherapeutics.
Understanding the Nanomedicine Landscape and Translational Challenges
The field of nanomedicine represents a revolutionary approach to drug delivery, offering unprecedented potential for enhancing therapeutic efficacy while minimizing systemic toxicity. Nanoparticle-based systems enable precise drug targeting, improved solubility of hydrophobic compounds, and controlled release profiles that are unattainable with conventional formulations. Despite extensive research investment and promising preclinical results, a significant translational gap persists, with only a minute fraction of laboratory developments progressing to clinical application. Quantitative analysis reveals that while over 100,000 scientific articles on nanomedicines were published in the past decade, only approximately 90 nanomedicine products had obtained global marketing approval by 2023, representing less than 0.1% of research output reaching patients [1]. This discrepancy highlights fundamental challenges in translating nanomedical innovations from laboratory research to clinically viable therapies.
The translational gap in nanomedicine stems from interconnected scientific, manufacturing, and regulatory barriers. Scientifically, the over-reliance on enhanced permeability and retention (EPR) effects observed in murine models has proven problematic, as this phenomenon demonstrates significant heterogeneity and limited occurrence in human tumors [1]. From a manufacturing perspective, complexities in scaling up production while maintaining batch-to-batch consistency present substantial hurdles [2]. Regulatory challenges further complicate translation, as evolving guidelines from the FDA and EMA struggle to keep pace with the unique characteristics of nanopharmaceuticals [3]. This application note provides a comprehensive analysis of these barriers and offers detailed protocols to bridge the translational gap through optimized nanoparticle design, characterization, and manufacturing processes.
Quantitative Analysis of the Translational Landscape
Clinical Translation Metrics for Nanomedicines
Table 1: Clinical Translation Metrics in Nanomedicine (2000-2025)
| Metric | Value | Contextual Reference |
|---|---|---|
| Global nanomedicine approvals | ~90 products | As of 2023, from >100,000 publications [1] |
| Estimated clinical translation rate | <0.1% | Percentage of research output reaching clinic [1] |
| Dominant approved platform types | Liposomes, nanocrystals, lipid nanoparticles (LNPs) | >60% market share [1] |
| Nanomedicines in clinical trials | ~500 candidates | As of 2023 [1] |
| Overall drug development success rate | 7-20% | Varies by study methodology [4] |
| Global nanomedicine market projection | >US $570 billion | By 2032 [1] |
The disproportionately low conversion rate from preclinical research to clinical approval reflects fundamental disconnect between laboratory innovation and clinical practicality. The nanomedicine portfolio remains dominated by first-generation platforms, particularly liposomes, with more complex nanocarriers struggling to achieve regulatory endorsement [1]. This translational bottleneck is exacerbated by the inherent challenges of drug development, where costs can exceed $2.5 billion per approved compound, with nanomedicines facing additional complexities in quality control, manufacturing, and regulatory standardization [1].
Analysis of Success and Failure Cases
Table 2: Comparative Analysis of Approved and Failed Nanomedicines
| Nanomedicine | Platform Type | Indication | Outcome | Key Limiting Factors |
|---|---|---|---|---|
| Doxil/Caelyx | PEGylated liposome | Ovarian cancer, breast cancer | Approved | Reduced cardiotoxicity vs. free doxorubicin; limited by hand-foot syndrome [1] |
| Abraxane | Albumin-bound paclitaxel | Breast cancer, pancreatic cancer | Approved | Improved drug solubility; relies on EPR effect [1] |
| COVID-19 mRNA Vaccines | Lipid nanoparticles (LNPs) | COVID-19 prophylaxis | Approved | Efficient nucleic acid delivery; proven scalability [5] |
| BIND-014 | Targeted docetaxel nanoparticles | Prostate cancer, lung cancer | Phase II failure (terminated) | Failed primary efficacy endpoints despite promising early activity [1] |
The failure of advanced platforms like BIND-014 despite robust preclinical evidence underscores the critical gap between molecular targeting demonstrated in animal models and actual impact on human clinical outcomes [1]. This case illustrates that sophisticated targeting mechanisms alone are insufficient without addressing the complexities of intratumor distribution and patient selection biomarkers.
Root Causes of the Translational Gap
Biological Challenges
The biological challenges in nanomedicine translation primarily center on the limited predictive value of animal models for human pathophysiology. The EPR effect, while robust and reproducible in murine tumor models, demonstrates significant heterogeneity in human patients due to factors including vascular heterogeneity, elevated interstitial pressure, and diverse non-EPR entry routes [1]. This discrepancy frequently results in overestimated efficacy predictions during preclinical development. Additionally, nanomedicine behavior is further complicated by complex interactions with biological barriers that impact pharmacokinetics and pharmacodynamics, causing efficacy signals observed in animals to diminish in clinical trials [1].
Nanoparticle transport faces additional challenges in specific therapeutic contexts, particularly neurological disorders. The blood-brain barrier (BBB) represents a formidable obstacle, with its tight junctions and efflux transporters severely restricting drug delivery to the brain [6]. While BBB integrity may be partially compromised in late-stage Alzheimer's disease, early-stage interventions require sophisticated targeting strategies to achieve therapeutic drug levels in the brain [6]. Similar challenges exist in glioblastoma treatment, where the BBB and tumor heterogeneity limit effective drug accumulation despite the urgent need for improved therapies [7].
Manufacturing and Scalability Hurdles
The transition from laboratory-scale synthesis to industrial production represents a critical bottleneck in nanomedicine development. Polymeric nanoparticles, exemplified by PLGA systems, demonstrate exceptional versatility in controlled release applications but present significant challenges in batch-to-batch reproducibility during scale-up [1] [2]. Conventional small-scale production methods are characterized by substantial variability, complicating the maintenance of critical quality attributes (CQAs) when increasing production volume [2]. This manufacturing inconsistency directly impacts nanoparticle performance, including drug release profiles, stability, and in vivo behavior.
The complexity of nanomedicine manufacturing extends beyond particle synthesis to comprehensive quality control systems. Critical process parameters (CPPs) and critical material attributes (CMAs) must be rigorously controlled throughout scale-up to ensure final product quality [8]. Advanced manufacturing technologies, including microfluidics and supercritical fluid processes, offer improved reproducibility but require specialized expertise and infrastructure not routinely available in conventional pharmaceutical production facilities [8].
Regulatory and Characterization Challenges
The regulatory landscape for nanomedicines remains complex and evolving, with harmonized standards still under development. Regulatory agencies including the FDA and EMA provide guidance on nanopharmaceuticals, but the absence of universally accepted characterization standards complicates the approval pathway [3]. Key challenges include standardized assessment of nanotoxicology, immunogenicity, and long-term biocompatibility, particularly for novel nanomaterial platforms without established regulatory precedent.
Comprehensive characterization presents additional hurdles, as nanomedicines require multifaceted analysis of physicochemical properties, surface characteristics, drug release kinetics, and stability under physiological conditions. The dynamic nature of nanoparticles in biological environments further complicates characterization, as properties may change significantly upon interaction with plasma proteins and cellular components [1]. These challenges collectively contribute to the protracted development timelines and high attrition rates observed in nanomedicine translation.
Experimental Protocols for Translation-Ready Nanomedicine Development
Protocol: Computational Modeling for Lipid Nanoparticle Optimization
Objective: Employ multiscale computational modeling to predict LNP behavior and optimize formulation prior to experimental validation, reducing development cycles and resource utilization.
Materials:
- Hardware: High-performance computing cluster (minimum 64 cores, 256 GB RAM)
- Software: GROMACS, CHARMM, or AMBER for molecular dynamics; Martini Coarse-Grained force field; Python with scikit-learn for machine learning analysis
- Experimental validation: Microfluidic mixer for LNP formation; dynamic light scattering for size and PDI; transfection efficiency assays
Procedure:
System Preparation (Week 1)
- Obtain or generate molecular structures of ionizable lipids, helper lipids, cholesterol, and PEG-lipids
- Parameterize novel lipids using quantum chemistry calculations (DFT) when necessary
- Build initial simulation boxes with varying lipid ratios and protonation states
Molecular Dynamics Simulation (Weeks 2-4)
- Run all-atom MD simulations (50-100 ns) to study lipid-RNA interactions and internal structure
- Perform coarse-grained MD simulations (1-10 μs) to capture self-assembly过程和endosomal escape mechanisms
- Implement constant pH molecular dynamics (CpHMD) to model environment-dependent protonation states [5]
- Apply enhanced sampling techniques (metadynamics, umbrella sampling) for rare events like endosomal fusion
Data Analysis and Machine Learning (Week 5)
- Extract key parameters: membrane curvature, lipid diffusion coefficients, nucleic acid encapsulation efficiency
- Train random forest or neural network models using experimental data and simulation descriptors
- Identify critical formulation parameters predicting encapsulation and transfection efficiency
Experimental Validation (Weeks 6-8)
- Prepare LNP formulations with compositions predicted by computational models
- Characterize physicochemical properties (size, PDI, encapsulation efficiency)
- Evaluate in vitro performance using relevant cell lines
Troubleshooting:
- If simulations show poor agreement with experimental data, verify force field parameters and consider longer equilibration times
- For unstable simulations, increase constraint algorithms and reduce timestep
- If ML models show poor predictive power, expand feature set and increase training data diversity
Protocol: Advanced In Vitro BBB Penetration Assessment
Objective: Establish a predictive in vitro blood-brain barrier model to evaluate nanoparticle penetration capabilities for neurological applications.
Materials:
- Cell lines: Primary human brain microvascular endothelial cells (HBMECs), astrocytes, pericytes
- Transwell systems: 12-well plate, 3.0μm pore size, 1.12 cm² growth area
- Nanoparticles: Fluorescently labeled nanoparticles with various surface modifications
- Characterization equipment: TEER measurement system, confocal microscopy, HPLC-MS
Procedure:
BBB Model Establishment (Days 1-7)
- Culture HBMECs on collagen-coated Transwell apical chambers
- Seed astrocytes and pericytes in basolateral chambers to establish tri-culture system
- Monitor transendothelial electrical resistance (TEER) daily until >150 Ω·cm²
- Validate barrier integrity with sodium fluorescein permeability (Papp < 1.0 × 10⁻⁶ cm/s)
Transport Studies (Day 8)
- Apply nanoparticles (100 μg/mL) in serum-free medium to apical chamber
- Collect basolateral samples at 0, 15, 30, 60, 120, and 240 minutes
- Analyze nanoparticle concentration using appropriate methods (fluorescence, HPLC)
- Calculate apparent permeability coefficients (Papp)
Mechanistic Investigations (Day 9)
- Pre-treat with various inhibitors: chlorpromazine (clathrin-mediated endocytosis), amiloride (macropinocytosis), nystatin (caveolae-mediated endocytosis)
- Evaluate energy dependence by performing transport at 4°C
- Assess specific receptor-mediated pathways using receptor-blocking antibodies
Intracellular Trafficking (Day 10)
- Fix cells at designated time points
- Immunostain for endosomal/lysosomal markers (EEA1, LAMP1)
- Image using confocal microscopy with z-stack acquisition
- Analyze colocalization coefficients using ImageJ software
Data Analysis:
- Calculate Papp = (dQ/dt) × (1/(A × C₀)), where dQ/dt is transport rate, A is membrane area, C₀ is initial concentration
- Compare transport efficiency across different nanoparticle formulations
- Determine primary transport mechanisms through inhibitor studies
Diagram 1: Experimental workflow for assessing nanoparticle transport across in vitro blood-brain barrier models.
Protocol: Quality-by-Design (QbD) Approach for Nanoparticle Manufacturing
Objective: Implement systematic QbD methodology to identify critical process parameters and establish design space for reproducible nanomedicine manufacturing.
Materials:
- Equipment: Microfluidic mixer (e.g., staggered herringbone, multi-inlet vortex mixers)
- Analytical instruments: DLS, NTA, HPLC, DSC, XPS
- QbD software: MODDE, Design-Expert, or JMP for experimental design and analysis
Procedure:
Define Quality Target Product Profile (QTPP) (Week 1)
- Identify critical quality attributes (CQAs): particle size, PDI, encapsulation efficiency, drug loading, zeta potential, release profile
- Establish target ranges for each CQA based on therapeutic requirements
- Document QTPP in structured format with justification for each parameter
Risk Assessment (Week 2)
- Conduct failure mode and effects analysis (FMEA) for materials and process parameters
- Identify potential critical material attributes (CMAs) and critical process parameters (CPPs)
- Prioritize high-risk factors for experimental evaluation
Experimental Design (DoE) (Week 3)
- Design screening experiments (fractional factorial or Plackett-Burman) to identify significant factors
- Develop response surface methodology (RSM) designs (central composite or Box-Behnken) for optimization
- Define factor ranges based on preliminary experiments and risk assessment
Process Optimization (Weeks 4-6)
- Execute DoE experiments using automated microfluidic systems
- Characterize CQAs for each experimental run
- Build mathematical models relating CPPs to CQAs
- Establish design space with proven acceptable ranges for CPPs
Control Strategy (Week 7)
- Define normal operating ranges and proven acceptable ranges for CPPs
- Implement process analytical technology (PAT) for real-time monitoring
- Establish control strategy for raw materials and in-process testing
Data Analysis:
- Perform multiple linear regression to build predictive models
- Calculate model adequacy metrics (R², Q², model validity)
- Generate contour plots to visualize design space
- Validate models with confirmation experiments
Visualization of Key Biological Pathways and Workflows
Nanoparticle Transport Across the Blood-Brain Barrier
Diagram 2: Primary mechanisms for nanoparticle transport across the blood-brain barrier.
Quality-by-Design Implementation Workflow
Diagram 3: Systematic Quality-by-Design workflow for nanomedicine development.
Research Reagent Solutions for Translational Nanomedicine
Table 3: Essential Research Reagents and Materials for Nanoparticle Translation Studies
| Reagent/Material | Function/Application | Key Considerations | Representative Examples |
|---|---|---|---|
| Ionizable Lipids | LNP core component for nucleic acid encapsulation | pKa optimization (6.2-6.5), biodegradability, fusogenicity | DLin-MC3-DMA, SM-102, ALC-0315 [5] |
| PEG-Lipids | Surface stabilization, reduction of protein adsorption | Chain length, concentration-dependent immunogenicity | DMG-PEG2000, DSG-PEG2000 [1] |
| Targeting Ligands | Active targeting to specific cells/tissues | Conjugation chemistry, density, orientation, binding affinity | Transferrin, folate, RGD peptides, monoclonal antibodies [6] |
| Biodegradable Polymers | Controlled release, structural matrix | Degradation rate, mechanical properties, byproducts | PLGA, PLA, chitosan, poly(β-amino esters) [1] [7] |
| BBB Models | Assessment of brain penetration | TEER values, transporter expression, paracellular permeability | Primary HBMECs, iPSC-derived endothelial cells, triple-culture systems [6] |
| Microfluidic Devices | Reproducible nanoparticle production | Mixing efficiency, Reynolds number, throughput | Staggered herringbone mixer, multi-inlet vortex mixer [8] |
| Characterization Instruments | Comprehensive nanoparticle analysis | Resolution, sensitivity, standardization | DLS, NTA, HPLC, TEM, SPR [1] |
Bridging the translational gap in nanomedicine requires a fundamental shift from isolated nanoparticle optimization to integrated formulation strategies that address biological, manufacturing, and regulatory challenges simultaneously. The protocols and methodologies outlined in this application note provide a framework for developing translation-ready nanomedicines with enhanced potential for clinical success. Key advancements in computational modeling, predictive in vitro systems, and QbD manufacturing represent critical enablers for accelerating nanomedicine translation.
Future progress will depend on continued collaboration between computational scientists, formulation experts, biologists, and clinical researchers to establish robust predictive models and standardized characterization approaches. The integration of artificial intelligence and machine learning throughout the development pipeline offers particular promise for identifying optimal formulation parameters and predicting in vivo performance. Additionally, increased emphasis on patient stratification biomarkers and disease-specific targeting strategies will be essential for demonstrating clear clinical benefit in well-defined patient populations. By adopting these comprehensive approaches, the nanomedicine field can systematically address the translational gap and fulfill its potential to revolutionize therapeutic interventions for complex diseases.
The selection of an appropriate nanoparticle platform is a critical determinant of success in drug development, impacting therapeutic efficacy, stability, and clinical translatability. This application note provides a systematic comparison of three core nanoparticle platforms: lipid-based, polymeric, and lipid-polymer hybrid systems. Within the context of optimizing nanoparticle-based drug delivery protocols, we present standardized experimental methodologies, quantitative performance data, and characterization workflows to guide researchers in selecting and implementing these technologies. By integrating detailed protocols with comparative analysis of pharmaceutical attributes, this document serves as a practical framework for rational nanocarrier design and development in preclinical research.
Nanoparticle-based delivery systems have revolutionized pharmaceutical development by addressing fundamental challenges associated with conventional drug administration, including poor solubility, limited bioavailability, and off-target toxicity [1]. Among the diverse array of nanocarriers, three platforms have emerged as particularly significant for therapeutic delivery: lipid nanoparticles, polymeric nanoparticles, and lipid-polymer hybrid nanoparticles.
Lipid-based systems, notably liposomes and lipid nanoparticles (LNPs), offer superior biocompatibility and have gained validation through clinical success in mRNA vaccine delivery [9] [1]. Polymeric nanoparticles (PNPs) provide exceptional structural stability and controlled release profiles through their tunable polymer matrices [10] [11]. Hybrid systems strategically combine material classes to leverage the advantages of both components while mitigating their individual limitations [12] [13].
The global nanoparticle technology market, valued at an estimated USD 10.8 billion in 2025 and projected to reach USD 18.4 billion by 2035, reflects the growing importance of these platforms across pharmaceutical applications [14]. This document establishes standardized protocols and comparative metrics to support researchers in navigating the selection, formulation, and characterization of these core platforms within integrated drug development workflows.
Comparative Analysis of Nanoparticle Platforms
A systematic understanding of the fundamental attributes of each nanoparticle platform enables informed selection based on therapeutic requirements. The following analysis compares the core characteristics, advantages, and limitations of lipid, polymeric, and hybrid systems.
Table 1: Fundamental Characteristics of Core Nanoparticle Platforms
| Parameter | Lipid Nanoparticles | Polymeric Nanoparticles | Lipid-Polymer Hybrids |
|---|---|---|---|
| Core Composition | Ionizable lipids, phospholipids, cholesterol, PEG-lipids [9] | PLGA, PLA, chitosan, PEG-b-PLA [10] [13] | Polymer core with lipid shell [12] [13] |
| Structural Model | Amorphous or non-bilayer structure [9] | Solid polymer matrix [11] | Core-shell architecture [13] |
| Key Advantage | Excellent biocompatibility; Efficient nucleic acid delivery [9] [1] | Superior stability; Controlled release kinetics [10] [13] | Combines stability of polymers with biocompatibility of lipids [12] |
| Primary Limitation | Poor structural stability; Drug leakage [12] [13] | Potential biocompatibility concerns; Use of toxic solvents [10] [13] | Complex fabrication process [13] |
Table 2: Pharmaceutical Performance and Application Scope
| Parameter | Lipid Nanoparticles | Polymeric Nanoparticles | Lipid-Polymer Hybrids |
|---|---|---|---|
| Drug Loading | Moderate for hydrophobic drugs; Poor for hydrophilic macromolecules [13] | High for hydrophobic drugs [13] | High for both hydrophobic and hydrophilic drugs [12] |
| Encapsulation Efficiency | Low for macromolecular peptides/proteins [12] | High for hydrophobic drugs [13] | High for peptides and proteins [12] |
| Release Profile | Burst release potential [13] | Sustained, controlled release [10] [13] | Controlled release with reduced burst effect [12] |
| Ideal Cargo | Nucleic acids (siRNA, mRNA), small molecules [9] | Small molecules, hydrophobic drugs [11] | Peptides, proteins, sensitive biologics [12] [13] |
The selection of a nanoparticle platform represents a critical risk-benefit analysis. Lipid nanoparticles (LNPs) provide a clinically validated platform for nucleic acid delivery but face challenges with structural stability and encapsulation of macromolecules [9] [13]. Polymeric nanoparticles (PNPs) offer superior control over drug release profiles but raise potential biocompatibility concerns and often require organic solvents in preparation [10] [13]. Lipid-polymer hybrid nanoparticles (LPHNs) represent an advanced solution that combines the structural stability of polymers with the biocompatibility and surface functionalities of lipids, making them particularly suitable for delivering sensitive biomolecules like peptides and proteins [12] [13].
Experimental Protocols
Standardized preparation methods are essential for generating reproducible, high-quality nanoparticles with predetermined characteristics. Below are detailed protocols for the fabrication of each platform.
Lipid Nanoparticle Preparation via Microfluidic Mixing
This protocol describes the preparation of LNPs using microfluidic mixing, a method that ensures excellent control over particle size and uniformity [9] [15].
Materials:
- Lipid Mixture: Ionizable lipid (e.g., DLin-MC3-DMA), phospholipid (e.g., DSPC), cholesterol, PEG-lipid (e.g., DMG-PEG 2000) [9]
- Aqueous Phase: Tris-EDTA buffer (pH 7.4) or citrate buffer (pH 4.0)
- Therapeutic Payload: mRNA, siRNA, or small molecule drug
- Equipment: Microfluidic mixer (e.g., NanoAssemblr, Precigenome system), syringe pumps, thermomixer [15]
Procedure:
- Lipid Phase Preparation: Dissolve ionizable lipid, phospholipid, cholesterol, and PEG-lipid in ethanol at a defined molar ratio (e.g., 50:10:38.5:1.5). Total lipid concentration should be 5-10 mM.
- Aqueous Phase Preparation: Dissolve the therapeutic payload (e.g., mRNA) in an acidified aqueous buffer (pH 4.0) at a concentration of 0.1-0.2 mg/mL.
- Microfluidic Mixing:
- Load the lipid and aqueous phases into separate syringes.
- Set the total flow rate (TFR) to 10-15 mL/min and the flow rate ratio (FRR, aqueous:organic) to 3:1.
- Initiate simultaneous pumping through the microfluidic mixer.
- Collect the resulting LNP suspension in a sterile vessel.
- Buffer Exchange and Purification:
- Dialyze the formed LNPs against PBS (pH 7.4) for 2 hours at 4°C to remove ethanol.
- Alternatively, use tangential flow filtration (TFF) to concentrate and diafilter the LNPs.
- Sterile Filtration: Filter the final formulation through a 0.22 µm sterile filter.
- Storage: Store LNPs in single-use bags at 2-8°C for short-term storage [15].
Critical Parameters:
- Lipid composition and molar ratios directly impact encapsulation efficiency and endosomal escape [9].
- Flow rates during microfluidic mixing determine particle size and polydispersity [13].
Polymeric Nanoparticle Preparation via Nanoprecipitation
This protocol describes the formation of PNPs using nanoprecipitation, a simple and versatile method ideal for encapsulating hydrophobic drugs [11] [2].
Materials:
- Polymer: PLGA, PLA, or PEG-b-PLA
- Organic Solvent: Acetone or acetonitrile
- Aqueous Phase: Deionized water with or without stabilizer (e.g., Poloxamer 188)
- Drug: Hydrophobic active compound (e.g., paclitaxel)
Procedure:
- Organic Phase Preparation: Dissolve the polymer and drug in a water-miscible organic solvent (e.g., acetone) at a typical polymer concentration of 5-10 mg/mL.
- Aqueous Phase Preparation: Fill a beaker with deionized water (typically 10-20 mL) containing a stabilizer (e.g., 0.1-0.5% w/v Poloxamer 188).
- Nanoprecipitation:
- Under moderate magnetic stirring (500-700 rpm), rapidly inject the organic phase (1-2 mL) into the aqueous phase using a syringe.
- Continue stirring for 2-4 hours to allow complete solvent evaporation.
- Concentration and Purification:
- Concentrate the PNP suspension using rotary evaporation or ultrafiltration.
- Purify by centrifugation or dialysis to remove free drug and solvent residues.
- Storage: Store the final PNP suspension at 4°C or lyophilize for long-term storage.
Critical Parameters:
- Polymer molecular weight and drug-to-polymer ratio control drug loading and release kinetics [10].
- The injection speed and stirring rate significantly influence particle size distribution [2].
Lipid-Polymer Hybrid Nanoparticle Preparation
This two-step protocol forms LPHNs with a polymeric core and lipid shell, combining the advantages of both systems for peptide/protein delivery [12] [13].
Materials:
- Polymer: PLGA or PEG-b-PLA
- Lipids: Lecithin, cholesterol, DSPE-PEG
- Aqueous Phase: Deionized water or PBS
- Drug: Peptide or protein (e.g., insulin)
Procedure:
- Polymeric Core Formation:
- Prepare PNPs encapsulating the peptide/protein drug using the nanoprecipitation or single-emulsion method described in Section 3.2.
- Characterize the resulting PNPs for size and PDI before proceeding.
- Lipid Film Hydration:
- Dissolve lipids (lecithin, cholesterol, DSPE-PEG) in chloroform in a round-bottom flask.
- Remove solvent via rotary evaporation to form a thin, uniform lipid film.
- Hydrate the lipid film with an aqueous buffer to form liposomes.
- Down-size the liposomes by extrusion through polycarbonate membranes (100 nm pore size).
- Hybridization:
- Combine the prepared PNPs and liposomes in a 1:1 weight ratio.
- Sonicate the mixture using a probe sonicator (5-10 cycles of 30 seconds pulse, 45 seconds rest) at 4°C.
- Alternatively, use co-extrusion through membranes to facilitate fusion.
- Purification: Purify the resulting LPHNs by ultracentrifugation (100,000 × g for 45 minutes) to remove unincorporated lipids and polymers.
- Storage: Store the LPHN dispersion at 4°C or lyophilize with cryoprotectants.
Critical Parameters:
- The lipid-to-polymer ratio determines final hybrid architecture and surface properties [13].
- Sonication energy and time must be optimized to ensure complete fusion without damaging the payload [12].
Characterization Workflows and Techniques
Comprehensive characterization is imperative for correlating nanoparticle physicochemical properties with biological performance. The following workflow outlines critical quality attributes (CQAs) and corresponding analytical techniques.
Diagram: Comprehensive characterization workflow for nanoparticle analysis, linking physicochemical properties to functional performance.
Size and Morphology Analysis
Nanoparticle Tracking Analysis (NTA):
- Principle: NTA utilizes light scattering and Brownian motion to determine particle size distribution and concentration in liquid suspensions [14] [16].
- Protocol:
- Dilute nanoparticle samples in purified water or PBS to achieve 20-100 particles per frame.
- Inject sample into the measurement chamber using a sterile syringe.
- Capture 60-second videos using camera level 12-16.
- Analyze at least three recordings per sample with detection threshold optimized for minimal background.
- Application: Particularly valuable for analyzing extracellular vesicles and heterogeneous LNP samples [16].
Electron Microscopy:
- Scanning Electron Microscopy (SEM):
- Protocol: Deposit nanoparticle suspension on silicon wafer, air-dry, and sputter-coat with gold/palladium before imaging.
- Output: High-resolution surface morphology and size verification [14].
- Transmission Electron Microscopy (TEM):
- Protocol: Apply sample to carbon-coated grid, stain with uranyl acetate, and image under appropriate magnification.
- Output: Internal structure visualization and core-shell confirmation in hybrid systems [12].
Drug Loading and Release Kinetics
Encapsulation Efficiency (EE) and Drug Loading (DL):
- Protocol:
- Separate unencapsulated drug using size exclusion chromatography or ultracentrifugation.
- Lyse nanoparticles using organic solvent (for lipid systems) or surfactant (for polymeric systems).
- Quantify drug content using validated UV-Vis, HPLC, or fluorescence spectroscopy methods.
- Calculations:
- EE (%) = (Amount of encapsulated drug / Total drug input) × 100
- DL (%) = (Weight of encapsulated drug / Total nanoparticle weight) × 100
In Vitro Release Kinetics:
- Protocol:
- Place nanoparticle suspension in a dialysis membrane (appropriate MWCO).
- Immerse in release medium (PBS, pH 7.4 with 0.1-0.5% surfactant to maintain sink conditions).
- Maintain at 37°C with constant agitation.
- Withdraw aliquots at predetermined time points and replace with fresh medium.
- Analyze drug content using appropriate analytical methods.
- Plot cumulative release versus time to determine release profile.
Advanced Characterization Techniques
Nuclear Magnetic Resonance (NMR) Spectroscopy:
- Application: Confirms polymer structure, monitors polymerization conversion, and quantifies drug-polymer conjugation efficiency [11].
- Protocol:
- Dissolve nanoparticles in deuterated solvent (e.g., CDCl₃, D₂O).
- Acquire ¹H NMR spectrum with sufficient scans for signal-to-noise ratio.
- Analyze characteristic peaks to verify successful conjugation and quantify loading.
Fluorescence-Based Single Particle Analysis:
- Application: Quantitative analysis of marker abundance on individual nanoparticles using fluorescent nanoparticle tracking analysis (fNTA) or nano-flow cytometry (nFCM) [16].
- Protocol:
- Label nanoparticles with fluorescent antibodies or dyes.
- Use reference fluorospheres with assigned equivalent reference fluorophore (ERF) values for calibration.
- Express fluorescent signal in ERF units to determine bound antibodies per particle.
- Combine with bulk measurements for comprehensive heterogeneity assessment.
The Scientist's Toolkit: Research Reagent Solutions
Successful nanoparticle development requires specialized materials and reagents with defined functions. The following table catalogs essential components for formulating advanced nanocarriers.
Table 3: Essential Research Reagents for Nanoparticle Formulation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, ALC-0315 | pH-responsive endosomal escape [9] | Critical for nucleic acid delivery; Optimize pKa for specific applications |
| Structural Lipids | DSPC, DOPE | Form nanoparticle structure and bilayer | Influence membrane fluidity and stability |
| Sterol Stabilizers | Cholesterol | Enhance membrane integrity and packing | Modulates stability and cellular uptake [9] |
| PEGylated Lipids | DMG-PEG2000, DSPE-PEG | Reduce opsonization, prolong circulation | Potential immunogenicity with repeated dosing [1] |
| Biodegradable Polymers | PLGA, PLA, PCL | Form stable nanoparticle matrix | Degradation rate controls drug release kinetics [10] [13] |
| Functional Polymers | PEG-b-PLA, Chitosan | Enhance stability, mucoadhesion | PEG provides stealth properties; Chitosan for mucosal delivery [10] |
| Stimuli-Responsive Polymers | PBAEs, pH-sensitive polymers | Enable triggered drug release | Activate in response to tumor microenvironment [10] |
| Characterization Standards | Fluorescent beads, ERF standards | Instrument calibration and quantification | Enable cross-platform data comparison [16] |
The strategic selection and optimization of nanoparticle platforms require careful consideration of therapeutic objectives, cargo characteristics, and administration routes. Lipid nanoparticles excel in nucleic acid delivery with proven clinical success, polymeric nanoparticles offer superior control for sustained small molecule delivery, while hybrid systems represent a promising approach for complex biologics like peptides and proteins.
Standardized protocols for preparation, characterization, and analysis are fundamental for generating reproducible, clinically translatable nanomedicines. The experimental frameworks and comparative data presented in this application note provide a foundational resource for researchers developing nanoparticle-based therapeutics. As the field advances, integration of machine learning for formulation design [15], development of novel non-PEG stealth alternatives [1], and implementation of scalable manufacturing processes [2] will be critical for bridging the translational gap between preclinical promise and clinical reality.
The efficacy of nanoparticle-based drug delivery systems is critically dependent on their ability to navigate a series of biological barriers. This application note details the primary hurdles—clearance by the reticuloendothelial system (RES), also known as the mononuclear phagocyte system (MPS); endosomal entrapment following cellular uptake; and the heterogeneous Enhanced Permeability and Retention (EPR) effect in solid tumors. We provide validated, quantitative data on these barriers and practical protocols to overcome them, framing this within the context of optimizing drug delivery protocols for clinical translation. The following table summarizes the impact and primary strategies for each barrier.
Table 1: Summary of Key Biological Barriers in Nanoparticle Drug Delivery
| Biological Barrier | Impact on Delivery | Primary Overcoming Strategies |
|---|---|---|
| RES/MPS Clearance | Rapid removal from blood (t½ < several minutes); <1% of injected dose typically reaches target site [17] | Surface PEGylation; MPS Blockade; Biomimetic camouflage [18] [17] [19] |
| Endosomal Entrapment | Traps >95% of internalized cargo, leading to lysosomal degradation [20] | Proton-sponge polymers; Fusogenic lipids; Cell-penetrating peptides (CPPs) [20] [19] |
| Heterogeneous EPR Effect | Highly variable nanoparticle accumulation in human tumors, limiting therapy predictability [21] [22] | Tumor vasculature modulation; Pharmacological priming; Physical methods (e.g., ultrasound) [23] [22] |
Protocol: Overcoming RES/MPS Clearance
Background and Principle
The Mononuclear Phagocyte System (MPS), historically termed the RES, is the primary system responsible for clearing particulate matter from the circulation. Resident macrophages in the liver (Kupffer cells) and spleen rapidly recognize, take up, and remove intravenously administered nanoparticles, often resulting in a blood half-life of only several minutes and leaving less than 1% of the injected dose to reach the intended target [17]. The principle of evasion involves engineering a "stealth" nanoparticle surface that minimizes opsonization (binding of serum proteins) and subsequent phagocytosis.
Detailed Methodology: Formulation of PEGylated LPD Nanoparticles
This protocol describes the synthesis of stable, PEGylated Liposome-Polycation-DNA (LPD) nanoparticles, which have demonstrated significantly reduced liver uptake and enhanced tumor delivery [18].
Materials
- Cationic Liposomes: Composed of DOTAP (or multivalent DSGLA) and Cholesterol at a 1:1 molar ratio.
- Nucleic Acids: siRNA (e.g., anti-luciferase GL3) and calf thymus DNA.
- Polycation: Protamine sulfate.
- PEG-lipid: DSPE-PEG2000.
- Buffers: Nuclease-free water, Phosphate Buffered Saline (PBS).
- Equipment: Dynamic Light Scattering (DLS) instrument, Zeta potential analyzer, Size Exclusion Chromatography (SEC) column (Sepharose CL 2B), Transmission Electron Microscope (TEM).
Step-by-Step Procedure
Prepare Core Complex:
- Mix 150 µl of suspension A (8.3 mM cationic liposomes + 0.2 mg/ml protamine) with 150 µl of solution B (0.16 mg/ml siRNA + 0.16 mg/ml calf thymus DNA) quickly.
- Incubate the mixture at room temperature for 10 minutes. The protamine and nucleic acids condense to form a compact, negatively charged core.
Form LPD Nanoparticles:
- The cationic liposomes from the core complex collapse onto the core via charge-charge interaction, subsequently fusing and reorganizing to form a nanoparticle coated with two lipid bilayers. The inner bilayer is stabilized ("supported") by the core [18].
PEGylate via Post-Insertion:
- Incubate the freshly prepared LPD suspension (300 µl) with 37.8 µl of a DSPE-PEG2000 micelle solution (10 mg/ml) at 50°C for 10 minutes.
- Allow the PEGylated LPD to cool and stabilize at room temperature for 10 minutes.
Purification and Characterization:
- Purify: Use size exclusion chromatography (Sepharose CL 2B) with PBS as the eluent to remove unincorporated lipids and free PEG.
- Characterize:
- Size & Distribution: Analyze by Dynamic Light Scattering (DLS). The expected diameter is 100-150 nm.
- Surface Charge: Measure zeta potential in 1 mM KCl. Successful PEGylation should result in a near-neutral zeta potential, indicating complete charge shielding.
- Structure: Confirm the distinct multilamellar structure using Transmission Electron Microscopy (TEM) with negative staining.
Alternative Strategy: MPS Blockade
An alternative/complementary strategy is the temporal blockade of the MPS to saturate clearance mechanisms.
- Procedure: Pre-administer a "blocking" dose of empty nanoparticles (e.g., non-therapeutic liposomes) 1-24 hours before injecting the therapeutic nanoparticle dose [17]. The blocking dose saturates phagocytic cells, temporarily reducing their capacity to clear the second dose.
- Example: Intravenous administration of blank liposomes can enhance the tumor delivery of a subsequent dose of paclitaxel-loaded nanoparticles by up to 150% [17].
- Considerations: The size, composition, and dose of the blocking agent are critical. Clinically relevant, biodegradable particles (e.g., empty liposomes) are preferred.
Table 2: Research Reagent Solutions for RES Evasion
| Research Reagent | Function/Application | Key Considerations |
|---|---|---|
| DSPE-PEG2000 | PEG-lipid for stealth coating; reduces opsonization and RES uptake [18] | Post-insertion method allows high surface density (~10 mol%) without disrupting nanoparticle integrity [18] |
| Ionizable Cationic Lipids (e.g., DSGLA) | Forms stable supported bilayer in LPD; enhances encapsulation of nucleic acids [18] | Multivalent lipids confer higher stability against PEG disruption compared to monovalent lipids like DOTAP [18] |
| Liposomal Clodronate | Macrophage depletion agent for MPS blockade; induces apoptosis in phagocytic cells [17] | Provides long-term blockade but has low clinical translation potential due to toxicity and prolonged immune suppression [17] |
| Gadolinium Chloride (GdCl3) | MPS function inhibitor; blocks Ca2+ channels in Kupffer cells [17] | Effective for preconditioning but associated with toxicity issues, including proinflammatory cytokine release [17] |
Protocol: Enhancing Endosomal Escape
Background and Principle
Most non-viral delivery vectors enter cells via endocytosis, resulting in their entrapment within endosomes. These endosomes mature into lysosomes, where the acidic environment and enzymes degrade the therapeutic cargo. It is estimated that the endosomal escape process is highly inefficient, with only a few percent of the internalized cargo successfully reaching the cytosol [20]. Strategies to overcome this barrier are designed to disrupt the endosomal membrane in a controlled manner, facilitating the cytosolic release of the payload.
Detailed Methodology: Employing pH-Sensitive LNPs for siRNA Delivery
Lipid Nanoparticles (LNPs) containing ionizable cationic lipids are a leading platform for nucleic acid delivery, leveraging the proton sponge effect and membrane fusion for escape [19].
Materials
- Lipids: Ionizable cationic lipid (e.g., DLin-MC3-DMA), Phospholipid (e.g., DSPC), Cholesterol, PEGylated lipid (e.g., DMG-PEG2000).
- Aqueous Buffer: Citrate buffer (pH 4.0).
- Therapeutic Payload: siRNA.
- Equipment: Microfluidic mixer or tube vortexer, DLS instrument.
Step-by-Step Procedure
- Prepare Lipid Mixture: Dissolve the ionizable cationic lipid, phospholipid, cholesterol, and PEG-lipid in ethanol at a specific molar ratio (e.g., 50:10:38.5:1.5 mol%).
- Prepare Aqueous Phase: Dissolve the siRNA in a citrate buffer (pH 4.0).
- Rapid Mixing:
- Microfluidic Method: Simultaneously pump the ethanolic lipid solution and the aqueous siRNA solution into a microfluidic chip at a controlled flow rate and ratio (typically 1:3 to 1:5, aqueous-to-ethanol) to form LNPs.
- Vortexing Method: Rapidly inject the ethanolic lipid solution into the aqueous siRNA solution under vigorous vortexing.
- Buffer Exchange and Dialysis: Dialyze the formed LNP suspension against a large volume of PBS (pH 7.4) for several hours to remove ethanol and raise the pH.
- Characterization: Determine particle size (expected 80-100 nm), polydispersity index (PDI < 0.2), and siRNA encapsulation efficiency (using a Ribogreen assay).
Mechanism of Action
The ionizable cationic lipids are neutral at physiological pH (7.4) but acquire a positive charge in the acidic environment of the endosome (pH ~5.5-6.5). This leads to:
- Proton Sponge Effect: The lipids buffer the endosomal pH, causing continued proton influx and chloride ion entry, leading to osmotic swelling and endosomal rupture [20].
- Membrane Fusion/Destabilization: The positively charged lipids interact with and destabilize the anionic endosomal membrane, promoting fusion or pore formation and releasing the cargo into the cytosol [19].
Protocol: Addressing Heterogeneity of the EPR Effect
Background and Principle
The Enhanced Permeability and Retention (EPR) effect is the cornerstone of passive targeting in solid tumors. However, its effectiveness in humans is highly heterogeneous, influenced by factors such as tumor type, size, stage, and blood flow [21] [22]. Advanced large tumors often have compromised blood flow due to thrombus formation and high interstitial pressure, leading to a poor EPR effect [21] [22]. The principle of enhancement involves using pharmacological or physical interventions to modulate the tumor vasculature and microenvironment, thereby improving nanoparticle perfusion and accumulation.
Detailed Methodology: Pharmacological Priming with Vasoactive Agents
This protocol uses angiotensin II (AT-II) to transiently elevate systemic blood pressure, enhancing tumor blood flow and nanoparticle extravasation [22].
Materials
- Vasoactive Agent: Angiotensin II (AT-II), sterile solution.
- Nanoparticles: Therapeutic nanoparticles (e.g., Doxil, polymeric micelles).
- Animal Model: Mice with established solid tumors (e.g., subcutaneous xenografts).
- Equipment: IV injection setup, physiological monitoring equipment.
Step-by-Step Procedure
- Tumor Model Preparation: Establish solid tumors in mice (e.g., 100-300 mm³ in volume).
- Administer Priming Agent:
- Inject AT-II intravenously at a low dose (e.g., 50-100 µg/kg) dissolved in saline.
- The injection induces a transient hypertensive episode that lasts approximately 10-15 minutes.
- Administer Nanoparticles:
- Inject the therapeutic nanoparticles intravenously precisely 1-2 minutes after the AT-II administration.
- The increased systemic blood pressure during the hypertensive window preferentially augments blood flow to the tumor due to its poorly regulated vasculature, thereby enhancing nanoparticle accumulation.
- Monitoring: Monitor animal blood pressure to confirm the hypertensive effect and ensure animal welfare.
Alternative Strategy: Vascular Normalization Therapy
An alternative strategy involves "normalizing" the disorganized tumor vasculature to improve perfusion and reduce hypoxia.
- Procedure: Administer an anti-angiogenic agent, such as an anti-VEGF receptor antibody (e.g., DC101) or a tyrosine kinase inhibitor (e.g., erlotinib), over several days (e.g., 100 µg/mouse, every other day for 6 days) prior to nanoparticle injection [22].
- Mechanism: This treatment prunes immature, leaky vessels and matures others, resulting in a more organized vascular network. This can lead to a more uniform distribution of nanoparticles, particularly those of smaller size (~12 nm), with studies showing up to a 3-fold increase in tumor accumulation [22].
Table 3: Strategies to Modulate the EPR Effect for Improved Drug Delivery
| Modulation Strategy | Example Agent | Mechanism of Action | Reported Outcome |
|---|---|---|---|
| Pharmacological Priming | Angiotensin II (AT-II) [22] | Induces transient hypertension, increasing tumor blood flow and nanoparticle extravasation. | Selective increase in tumor accumulation due to defective vascular regulation in tumors [22]. |
| Vascular Normalization | Anti-VEGFR2 Antibody (DC101) [22] | Prunes immature vessels and normalizes the tumor vasculature, improving perfusion. | Up to 3-fold increase in tumor accumulation of smaller (~12 nm) nanoparticles [22]. |
| Physical Priming | Ultrasound with Microbubbles [23] | Mechanical disruption of vessel walls and ECM upon bubble oscillation/bursting, enhancing permeability. | Clinically evaluated for improving drug delivery, particularly in brain tumors [23]. |
| Stroma Modulation | Enzymes (e.g., Collagenase, Hyaluronidase) | Degrades dense extracellular matrix (ECM), reducing interstitial pressure and improving diffusion. | Enhanced penetration of nanoparticles into the tumor core, especially in fibrotic tumors [22]. |
In the development of nanoparticle-based therapeutics, Critical Quality Attributes (CQAs) are fundamental measurable properties that define the identity, purity, efficacy, and safety of a drug product. For nanomedicines, CQAs present unique challenges due to their complex, multi-component three-dimensional structures which require careful design and orthogonal analysis methods [24]. The establishment of well-defined CQAs is particularly crucial for mRNA/Lipid Nanoparticle (LNP) products and other nanotherapeutics, where the field is rapidly expanding beyond vaccines to encompass therapeutic applications including gene editing, protein replacement, and cancer therapies [25]. A systematic understanding of these attributes—size, zeta potential, surface chemistry, and stability parameters—enables researchers to ensure batch-to-batch consistency, optimize therapeutic performance, and meet regulatory expectations throughout the product lifecycle from early development to commercial manufacturing [26].
Defining the Core CQAs for Nanoparticle Therapeutics
Particle Size and Distribution
Particle size is a fundamental CQA that significantly influences a nanoparticle's biological behavior, including its biodistribution, cellular uptake, and ability to penetrate biological barriers [24]. The size determination of nanoparticles, however, is not straightforward, as different measurement techniques probe different physical dimensions of the particle [27]. Some techniques measure the physical core size, while others measure the hydrodynamic diameter, which includes the hydration layer surrounding the nanoparticle as it moves in solution [27] [28].
Table 1: Nanoparticle Size Characterization Techniques
| Technique | Measured Parameter | Size Range | Key Considerations |
|---|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic diameter [27] | 1 nm - 10 μm [28] | Ensemble measurement; sensitive to aggregates [27] |
| Nanoparticle Tracking Analysis (NTA) | Hydrodynamic diameter [27] | 10 - 2000 nm [28] | Single-particle tracking; provides concentration [27] |
| Electron Microscopy (TEM/SEM) | Core particle dimensions [27] [28] | 1 nm - 10 μm [28] | Direct visualization; requires vacuum conditions [27] [28] |
| Atomic Force Microscopy (AFM) | Topographical height [27] [28] | 1 nm - 10 μm [28] | Three-dimensional profiling; can measure in liquid [27] [28] |
| Disc Centrifugation | Sedimentation diameter [27] | 5 nm - 100 μm [28] | High-resolution size distribution [27] |
For intravenous nanosuspensions, particle size is particularly critical, as the formation of larger particles (>5 μm) could lead to capillary blockade and embolism [29]. The size distribution also provides valuable information, revealing the presence of aggregates that may indicate poor dispersion stability [27].
Figure 1: Particle Size CQA Measurement Strategy
Zeta Potential
Zeta potential represents the electrokinetic potential at the slipping plane of a dispersed particle relative to the bulk fluid, providing an indirect measure of the net surface charge and the magnitude of electrostatic interactions within the system [30]. This parameter is critically important as it directly influences colloidal stability by determining the balance between attractive van der Waals forces and repulsive electrostatic forces between particles [30].
Table 2: Zeta Potential Ranges and Colloidal Stability
| Zeta Potential (mV) | Stability Behavior | Biological Implications |
|---|---|---|
| 0 to ±5 | Rapid coagulation or flocculation [30] | Unsuitable for therapeutic use |
| ±10 to ±30 | Incipient instability [30] | Limited shelf-life; may require cold chain |
| ±30 to ±40 | Moderate stability [30] | Generally acceptable for therapeutics |
| ±40 to ±60 | Good stability [30] | Good shelf-life potential |
| > ±60 | Excellent stability [30] | High stability but may affect biocompatibility |
From a biological perspective, zeta potential significantly affects how nanoparticles interact with cellular membranes. Since most cellular membranes are negatively charged, nanoparticles with strongly cationic surfaces (zeta potentials greater than +30 mV) generally display increased cellular uptake but may also be associated with more toxicity due to cell wall disruption [31]. Conversely, strongly anionic nanoparticles (less than -30 mV) may exhibit reduced cellular interaction but potentially better stability profiles [31].
Surface Chemistry
Surface chemistry is a critical design parameter that governs nanoparticle interactions with biological systems, including protein adsorption, cellular uptake, biodistribution, and targeting efficiency [32]. The surface functionalization of nanoparticles can be achieved through various strategies, including covalent bonding, non-covalent adsorption, and the use of homo- or hetero-bifunctional cross-linkers [32].
The surface composition directly influences what is known as the "protein corona" that forms when nanoparticles enter biological fluids. This corona significantly alters the nanoparticle's identity and biological behavior [32]. Surface modification strategies can be broadly categorized into passive and active targeting approaches:
- Passive targeting relies on the intrinsic physical properties of nanoparticles (size, shape, superficial charge) to accumulate in target tissues through phenomena like the Enhanced Permeability and Retention (EPR) effect in tumors [32].
- Active targeting involves the biofunctionalization of nanoparticle surfaces with specific ligands (antibodies, peptides, aptamers, oligosaccharides) that have strong affinity for receptors overexpressed on target cells [32].
Table 3: Surface Functionalization Strategies by Nanoparticle Material
| Nanomaterial | Usable Functional Groups | Functionalization Strategies |
|---|---|---|
| Silica | -SiOH | Aminosilanes for amine group introduction [32] |
| Noble Metals (Au, Ag) | Metallic surface (Au, Ag) | Thiol- or amine-based crosslinkers [32] |
| Metal Oxides | MOx | Ligand exchange with diol, amine, carboxylic acid, thiol [32] |
| Carbon-based | sp² hybridized carbon | Oxidation to generate -COOH, -OH, -C=O; halogenation [32] |
Stability Parameters
Stability is one of the most challenging aspects in nanomedicine development, crucial for ensuring both safety and efficacy of the final drug product [29]. Nanoparticle stability encompasses multiple dimensions: physical stability (particle size distribution, absence of aggregation), chemical stability (drug integrity, excipient compatibility), and biological stability (sterility, absence of endotoxins) [29].
The stability challenges vary significantly depending on the dosage form and route of administration. For instance, particle agglomeration presents different concerns in pulmonary delivery (where it affects aerodynamics) versus intravenous administration (where it may cause capillary embolism) [29]. Stability is influenced by numerous factors including the dispersion medium (aqueous vs. non-aqueous), production technique (top-down vs. bottom-up), and the inherent nature of the drug substance (small molecules vs. large biomolecules) [29].
Experimental Protocols for CQA Characterization
Protocol: Dynamic Light Scattering for Size and Size Distribution
Principle: DLS measures the fluctuations in scattered light intensity caused by Brownian motion of particles in suspension, which is correlated to their hydrodynamic diameter through the Stokes-Einstein equation [27] [28].
Procedure:
- Sample Preparation: Dilute the nanoparticle suspension with an appropriate buffer to achieve optimal scattering intensity. Avoid over-dilution or concentration that may alter particle interactions. Filter the sample through a 0.22 μm or 0.45 μm filter to remove dust and large aggregates if necessary [27].
- Instrument Calibration: Use standard latex beads of known size (e.g., 100 nm) to verify instrument performance and alignment according to manufacturer specifications [28].
- Measurement Parameters:
- Temperature: Maintain constant temperature (typically 25°C) with controlled tolerance (±0.3°C)
- Measurement angle: Typically 90° or backscatter detection (173°)
- Run duration: 5-10 measurements of 60 seconds each for statistical reliability [27]
- Data Analysis:
- Report the Z-average diameter (mean hydrodynamic size) and polydispersity index (PDI)
- PDI < 0.1 indicates monodisperse system; 0.1-0.2 moderate polydispersity; >0.2 broad distribution [27]
- Examine the intensity-weighted distribution and consider volume- or number-weighted distributions for polydisperse samples [28]
Troubleshooting Tips:
- High PDI values may indicate aggregation or sample contamination
- If concentration is too high, multiple scattering can affect results
- Viscous solutions require adjustment of the viscosity parameter in software [27] [28]
Protocol: Zeta Potential Measurement via Electrophoretic Light Scattering
Principle: Zeta potential is determined by measuring the electrophoretic mobility of particles in an applied electric field and calculating the potential at the slipping plane using the Henry equation [31] [30].
Procedure:
- Sample Preparation: Prepare samples in a suitable aqueous medium with controlled ionic strength. For nanoparticles in non-aqueous media, specialized cells may be required. Dilute samples to avoid multiple scattering effects [31].
- Cell Selection and Loading: Use a clear disposable zeta cell or a dedicated folded capillary cell. Ensure no air bubbles are introduced during loading as they interfere with measurement [30].
- Measurement Parameters:
- Temperature: 25°C unless otherwise specified
- Field strength: Typically 10-20 V/cm depending on sample conductivity
- Measurement cycles: Minimum 10-12 runs per sample
- Attenuator setting: Optimize for count rate between 200-500 kcps [31]
- Data Analysis:
- Report the mean zeta potential and standard deviation from multiple measurements
- Examine the phase plot for stability of measurement
- Ensure the baseline correlation function fits properly for reliable results [30]
Quality Control:
- Validate instrument performance using standard reference materials (e.g., -50 mV ± 5 mV latex standards)
- Monitor the conductivity of the sample to ensure appropriate electrolyte concentration [31] [30]
Protocol: Surface Chemistry Analysis Through FTIR and ζ-Potential
Principle: Surface functional groups can be characterized using Fourier Transform Infrared Spectroscopy (FTIR) to identify chemical bonds, while surface charge changes confirm successful modification [32].
Procedure for FTIR Analysis:
- Sample Preparation:
- For dry nanoparticles: Use KBr pellet method or attenuated total reflectance (ATR) mode
- For suspensions: Concentrate nanoparticles by centrifugation and prepare as thin film on ATR crystal [32]
- Measurement Parameters:
- Spectral range: 4000-400 cm⁻¹
- Resolution: 4 cm⁻¹
- Scans: 64-128 for acceptable signal-to-noise ratio
- Data Interpretation:
- Identify characteristic absorption bands: amine groups (3300-3500 cm⁻¹), carbonyl (1650-1750 cm⁻¹), carboxylate (1400-1600 cm⁻¹)
- Compare spectra before and after surface modification to confirm functionalization [32]
Complementary ζ-Potential Measurement:
- Measure ζ-potential before and after surface modification
- Significant changes in ζ-potential confirm surface charge modification (e.g., increase in positive charge after amine functionalization) [32]
Figure 2: Surface Chemistry Characterization Workflow
Stability Assessment Protocols
Comprehensive Stability Study Design
Principle: Stability of nanoparticle formulations must be evaluated under various stress conditions to predict shelf-life and identify potential failure modes [29]. The International Council for Harmonisation (ICH) guidelines provide framework for stability testing, but nanoparticle formulations often require additional specific assessments.
Protocol:
- Accelerated Stability Testing:
- Store samples at elevated temperatures (e.g., 4°C, 25°C, 40°C) for predetermined timepoints (1, 3, 6 months)
- Assess size, PDI, zeta potential, drug content, and related substances at each interval [29]
- Freeze-Thaw Stability:
- Subject samples to multiple freeze-thaw cycles (-20°C to 25°C)
- Evaluate physical stability after each cycle [29]
- In-Use Stability:
- For lyophilized products: reconstitute and monitor over recommended in-use period
- For suspensions: evaluate under simulated administration conditions [29]
Parameters for Stability Assessment:
- Physical stability: Particle size, size distribution, appearance, pH, redispersibility
- Chemical stability: Drug assay, related substances, degradation products
- Performance stability: Drug release profile, encapsulation efficiency [29]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Materials for Nanoparticle CQA Assessment
| Category | Specific Examples | Function/Application |
|---|---|---|
| Size Characterization | Latex size standards (100 nm, 200 nm) [28] | Instrument calibration and verification |
| Zeta Potential Standards | Colloidal gold (strongly anionic) [31] | Negative zeta potential reference |
| Amine-terminated PAMAM dendrimer (strongly cationic) [31] | Positive zeta potential reference | |
| Surface Modification | Aminosilanes (e.g., APTES) [32] | Silica nanoparticle functionalization |
| Thiol-carboxylic acids [32] | Gold nanoparticle surface modification | |
| Heterobifunctional crosslinkers (e.g., NHS-PEG-Maleimide) [32] | Bioconjugation and PEGylation | |
| Stabilizers | Poloxamers, Polysorbates [29] | Steric stabilization against aggregation |
| Ionic surfactants (SDS, CTAB) [29] | Electrostatic stabilization | |
| Cyclodextrins [29] | Complexation and stabilization | |
| Characterization Kits | Commercial mRNA purity/integrity kits [25] | mRNA nanoparticle quality assessment |
| dsRNA detection kits [25] | Impurity quantification in mRNA products |
Integration of CQAs in Nanomedicine Development
The successful development of nanoparticle-based therapeutics requires a systematic approach to CQA identification and control throughout the product lifecycle. For mRNA/LNP products, CQAs can be categorized into five main groups: purity and product-related impurities; safety tests; strength, identity, and potency; product quality and characteristics; and other obligatory CQAs [25]. Early product characterization is crucial for distinguishing between critical and non-critical quality attributes, with the understanding that even non-critical attributes can provide valuable information about product behavior and process consistency [25].
A significant challenge in nanomedicine development is establishing meaningful potency assays that adequately reflect the product's biological activity. For complex nanoparticles, a matrix approach for potency assessment is often necessary, capturing multiple aspects of function including transfection efficiency, translation capability, and biological activity of the encoded protein [25]. As the field matures, increased regulatory guidance and industry consensus on CQA assessment will hopefully accelerate the clinical translation of promising nanomedicines while ensuring product quality, safety, and efficacy [26] [25] [24].
Advanced Formulation Strategies and Delivery System Engineering
Nanoprecipitation, also known as solvent displacement or the "Ouzo effect," has emerged as a versatile and efficient technique for formulating nanoparticles (NPs), providing significant advantages in drug delivery applications [33] [34]. This method relies on the controlled mixing of a water-miscible organic solvent containing dissolved solute molecules with an anti-solvent (typically water), leading to rapid supersaturation and the formation of nanoscale particles [33]. The technique has evolved from simple batch operations to sophisticated continuous processes, enabling precise control over particle size, morphology, and drug release profiles [34]. Within nanoparticle-based drug delivery protocol optimization research, selecting the appropriate nanoprecipitation method is crucial for achieving reproducible and scalable production of nanocarriers with defined critical quality attributes (CQAs). This document provides detailed application notes and experimental protocols for conventional, flash, and microfluidic nanoprecipitation techniques, supporting their implementation in optimized drug delivery system development.
Technical Comparison of Nanoprecipitation Platforms
The table below summarizes the key characteristics, advantages, and limitations of three primary nanoprecipitation platforms, providing researchers with a comparative framework for technique selection.
Table 1: Comparative Analysis of Nanoprecipitation Platforms for Nanoparticle Synthesis
| Parameter | Conventional Batch Nanoprecipitation | Flash Nanoprecipitation (FNP) | Microfluidic Nanoprecipitation |
|---|---|---|---|
| Mixing Principle | Dropwise addition or pipette mixing in unstirred or stirred vessels [33] | Turbulence-enhanced rapid mixing in confined impingement jets (CIJ) or multi-inlet vortex mixers (MIVM) [33] [34] | Laminar flow with diffusion-controlled or chaotic advection mixing in microfabricated channels [35] [36] |
| Mixing Timescale | Seconds to minutes [35] | Milliseconds [33] [34] | Milliseconds to seconds [35] |
| Typical Particle Size Range | 50 - 500 nm [33] | 20 - 200 nm [37] | 50 - 300 nm [35] [36] |
| Size Distribution (PDI) | Moderate to broad (>0.1) [36] | Narrow (<0.1) [33] [37] | Very narrow (<0.1) [35] [36] |
| Drug Encapsulation Efficiency | Varies with drug hydrophobicity | High for highly hydrophobic drugs [37] | High and reproducible [35] |
| Throughput & Scalability | Limited by mixing heterogeneity; scaled up via volume increase | Highly scalable via reactor numbering-up or continuous operation [34] | Scalable via channel parallelization; inherently continuous [35] [36] |
| Key Advantages | Operational simplicity, low equipment cost, minimal material needs [33] | Superior size control, batch-to-batch consistency, handles high supersaturation [33] [34] | Unparalleled mixing control, high reproducibility, tunable release kinetics [35] [36] |
| Primary Limitations | Broader size distribution, batch-to-batch variability, limited mixing control [33] [36] | Specialized mixer design required, optimization for different formulations needed | Potential for channel clogging, fabrication complexity, higher entry level [35] |
Detailed Experimental Protocols
Protocol: Conventional Batch Nanoprecipitation of PLGA Nanoparticles
This protocol outlines the optimized synthesis of Poly(lactic-co-glycolic acid) (PLGA) nanoparticles using a batch method, refined through Design of Experiments (DoE) [36].
Research Reagent Solutions
Table 2: Essential Materials for Batch PLGA Nanoprecipitation
| Reagent/Material | Specification | Function |
|---|---|---|
| PLGA | Resomer RG 502 H, Mw 7000–17,000 Da | Biodegradable polymer matrix for nanoparticle formation [36] |
| Organic Solvent | Acetonitrile (ACN, 99.95%) | Solvent for dissolving PLGA polymer [36] |
| Aqueous Phase Surfactant | Polyvinyl alcohol (PVA, 9000–10,000 Mw, 80% hydrolyzed) | Stabilizer to prevent nanoparticle aggregation [36] |
| Anti-Solvent | Deionized Water | Aqueous phase inducing polymer precipitation [36] |
Step-by-Step Procedure
- Aqueous Phase Preparation: Dissolve PVA in deionized water to a final concentration of 1.5% - 2.5% (w/v). Use a volume between 1 mL and 3 mL. Stir until completely clear [36].
- Organic Phase Preparation: Dissolve 5 mg - 15 mg of PLGA polymer in 100 μL - 500 μL of acetonitrile [36].
- Mixing and Nanoprecipitation: Place the aqueous PVA solution in a 5 mL cylindrical glass vial with a 3 mm × 10 mm magnetic stir bar. Stir continuously at 660 rpm. Add the organic phase dropwise to the aqueous phase every three seconds using a micropipette [36].
- Solvent Evaporation: Allow the mixture to incubate overnight at room temperature, uncovered, with gentle stirring to ensure complete evaporation of the organic solvent [36].
- Purification: Transfer the nanoparticle suspension to centrifuge tubes. Wash twice by centrifugation at 15,000 rpm for 20 minutes per cycle. Carefully decant the supernatant and re-disperse the pellet in deionized water each time [36].
- Lyophilization: Freeze the purified nanoparticle suspension and lyophilize using a standard freeze-dryer (e.g., Kühner Alpha 2-4 LD) to obtain a dry powder for long-term storage [36].
Hydrodynamic and Statistical Analysis
For the described setup (660 rpm, 10 mm impeller), the Reynolds number (Re) is approximately 125, indicating laminar flow. The Damköhler number (Da), with a mixing time (t~mix~) of ~0.91 s and a reaction time (t~react~) of ~0.1 s, is about 0.11. A Da < 1 suggests that the mixing process is slower than the precipitation reaction, which can lead to heterogeneity. This highlights the limitation of batch methods and the need for precise control over addition rates and stirring [36]. DoE analysis reveals that the PLGA/ACN ratio and aqueous-to-organic volume ratio are statistically significant predictors (p < 0.05) of both nanoparticle size and PDI [36].
Protocol: Flash Nanoprecipitation (FNP) Using a Confined Impingement Jet (CIJ) Mixer
FNP achieves ultra-rapid mixing to produce nanoparticles with narrow size distributions, ideal for encapsulating hydrophobic drugs [33] [37].
Research Reagent Solutions
Table 3: Essential Materials for Flash Nanoprecipitation
| Reagent/Material | Specification | Function |
|---|---|---|
| Polymer & Drug | e.g., PLGA and a hydrophobic drug (Itraconazole, β-carotene) | Forms the core matrix of the nanoparticle; drug is the therapeutic payload [37] |
| Stabilizer Block Copolymer | e.g., Poloxamer (Pluronic) | Forms a steric stabilization shell around the nanoparticle core to prevent aggregation [37] |
| Organic Solvent | Tetrahydrofuran (THF) or Acetone | Water-miscible solvent for polymer, drug, and stabilizer [33] |
| Anti-Solvent | Deionized Water or Buffer | Aqueous phase triggering instantaneous nanoprecipitation upon mixing [33] |
Step-by-Step Procedure
- Solution Preparation:
- Organic Stream: Dissolve the polymer (e.g., PLGA), drug, and amphiphilic block copolymer stabilizer (e.g., Poloxamer 407) in THF. A typical total solid concentration is 1-10 mg/mL [37].
- Aqueous Stream: Use pure deionized water or a buffer as the anti-solvent.
- Mixer Setup: Connect two high-precision syringe pumps to the two inlets of a CIJ mixer. Load one pump with the organic solution and the other with the aqueous anti-solvent.
- Flash Mixing: Simultaneously drive the two streams into the mixing chamber at high flow rates (typical total flow rate 10-60 mL/min). The impingement of jets creates intense turbulence, achieving mixing in milliseconds [33] [34].
- Collection and Solvent Removal: Collect the effluent nanoparticle suspension. If THF is used, remove the residual organic solvent by gentle evaporation or dialysis against water.
- Purification and Characterization: Purify the nanoparticles via tangential flow filtration or centrifugation. Characterize for size, PDI, zeta potential, and drug encapsulation efficiency.
Protocol: Microfluidic Nanoprecipitation Using a Staggered Herringbone Micromixer (SHM)
Microfluidics offers exceptional control over mixing kinetics, enabling the synthesis of highly uniform nanoparticles with tunable properties [35] [36].
Research Reagent Solutions
Table 4: Essential Materials for Microfluidic Nanoprecipitation
| Reagent/Material | Specification | Function |
|---|---|---|
| Polymer | PLGA or other biodegradable polymers | Nanoparticle structural polymer [36] |
| Organic Solvent | Acetonitrile (ACN) | Dissolves the polymer for the organic phase [36] |
| Aqueous Phase Stabilizer | PVA solution or other surfactants | Aqueous stream stabilizer to control particle growth and stability [36] |
| Microfluidic Chip | Staggered Herringbone Mixer (SHM) geometry | Generates chaotic advection to enhance mixing efficiency in laminar flow [35] |
Step-by-Step Procedure
- Solution Preparation:
- Chip Priming and Setup: Load the organic and aqueous solutions into separate syringes and mount them on a multi-syringe pump. Connect the syringes to the inlets of the SHM chip. Prime the channels to remove air bubbles.
- Microfluidic Mixing: Initiate flow. A common configuration uses a three-inlet junction, with the organic phase in the central inlet flanked by two aqueous phase inlets [36]. The SHM's asymmetric grooves induce chaotic advection, reducing the mixing time (τ~m~) to milliseconds. Key parameters to control are:
- Collection and Processing: Collect the nanoparticle suspension from the outlet stream into a vial. The solvent can be evaporated under reduced pressure or dialyzed.
- Post-processing: Purify and lyophilize the nanoparticles as described in Section 3.1.2.
Workflow and Mechanism Visualization
Nanoparticle Formation Mechanism in Nanoprecipitation
The following diagram illustrates the kinetic processes governing nanoparticle formation during mixing, which is fundamental to understanding the differences between nanoprecipitation techniques.
Figure 1. Nanoparticle Formation Kinetics During Mixing. The pathway is determined by the relationship between the mixing timescale (τ~m~) and the nucleation timescale (τ~n~). When τ~m~ < τ~n~ (blue path), rapid mixing creates a homogeneous supersaturation environment, favoring homogeneous nucleation and yielding small, uniform NPs. When τ~m~ > τ~n~ (red path), mixing is slow relative to nucleation, leading to heterogeneous growth and aggregation, resulting in larger, polydisperse NPs [35].
Microfluidic Nanoprecipitation Workflow
The diagram below outlines the integrated experimental and computational workflow for optimizing nanoparticle synthesis using a microfluidic platform.
Figure 2. Microfluidic Optimization Workflow for Nanoparticle Synthesis. This integrated approach combines experimental synthesis with Computational Fluid Dynamics (CFD) modeling. Formulation parameters guide both the experimental process and the setup of CFD simulations, which model flow and concentration profiles to analyze mixing efficiency. The simulation results inform microfluidic design and operation, while experimental data validates the models, culminating in an optimized nanoparticle formulation with defined Critical Quality Attributes (CQAs) [36].
Application Notes for Drug Delivery Protocol Optimization
Selecting a Nanoprecipitation Technique
The choice of technique represents a trade-off between control, simplicity, and scalability, and should be aligned with the stage and goals of the research [33] [35] [36].
- Conventional Batch is ideal for initial formulation screening and feasibility studies due to its low material consumption and minimal equipment requirements.
- Flash Nanoprecipitation is superior for producing high volumes of nanoparticles with narrow size distributions, particularly for highly hydrophobic drugs, and is easier to scale than microfluidics [37].
- Microfluidic Platforms provide the highest level of precision and reproducibility for establishing robust structure-activity relationships and are excellent for producing complex nanostructures like core-shell particles [35] [36].
Addressing the Translational Gap
A significant challenge in nanomedicine is the "translational gap," where promising laboratory results fail to lead to clinical applications [1]. This is often due to a lack of focus on advanced formulation strategies and scalable manufacturing. Both FNP and microfluidic techniques address this gap by enabling continuous processing and superior batch-to-batch consistency, which are critical for Chemistry, Manufacturing, and Controls (CMC) required for regulatory approval [1] [35]. Integrating computational tools like CFD and machine learning with experimental data can further accelerate the rational design of nanoparticles, reducing development time and cost [5] [36].
Advanced Concepts: Sequential Nanoprecipitation (SNaP)
Sequential Nanoprecipitation (SNaP) is an emerging technique that decouples the core formation and shell stabilization steps of nanoparticle synthesis [34] [37]. This allows access to a broader size range and enables the encapsulation of moderately hydrophobic drugs with higher efficiency than single-step FNP. SNaP-produced nanoparticles have also demonstrated slower drug release rates, which is advantageous for sustained release applications [37].
The clinical success of lipid nanoparticles (LNPs) has fundamentally transformed the landscape of nucleic acid therapeutics, enabling the rapid development and deployment of mRNA vaccines during the COVID-19 pandemic. Pfizer/BioNTech's BNT162b2 and Moderna's mRNA-1273 vaccines demonstrated efficacy rates exceeding 94%, establishing LNP-formulated mRNA as a revolutionary tool against infectious diseases [38]. These non-viral delivery systems effectively overcome multiple biological barriers that traditionally hampered nucleic acid therapeutics, including enzymatic degradation, cellular membrane penetration, and inefficient endosomal release [38]. The lessons learned from this success now provide a foundational framework for optimizing LNP platforms across broader therapeutic applications, including cancer immunotherapy, rare genetic disorders, and personalized medicine approaches.
Despite these advancements, current LNP systems face significant challenges that require systematic optimization. Toxicity concerns associated with high lipid doses, suboptimal mRNA loading capacity, and non-specific immune responses remain critical limitations [39]. For instance, in commercial mRNA vaccines, the mRNA component constitutes less than 5% of the total weight, necessitating high lipid doses that contribute to adverse effects such as headache and fever [39]. This application note details advanced strategies and protocols for optimizing LNP formulations to address these limitations, with a focus on enhancing delivery efficiency, improving safety profiles, and enabling targeted therapeutic applications.
LNP Composition and Function
LNPs are complex multi-component systems where each element serves specific functional roles in nucleic acid encapsulation, protection, and delivery. The ionizable lipid represents the most critical component, enabling mRNA encapsulation during formulation and facilitating endosomal escape through its pH-dependent structural changes [38]. Phospholipids contribute to bilayer formation and structural integrity, while cholesterol enhances membrane stability and fluidity. PEG-lipids control nanoparticle size, improve colloidal stability, and reduce nonspecific interactions, though they may contribute to anti-PEG immune responses [39].
Table 1: Essential LNP Components and Their Functional Roles
| Component Category | Specific Examples | Primary Function | Optimization Considerations |
|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, SM-102 | mRNA complexation, endosomal disruption | pKa optimization (6.2-6.5), biodegradable linkages |
| Phospholipids | DSPC, DOPE | Bilayer structure, membrane fusion | Chain saturation affects phase behavior and stability |
| Cholesterol | Natural, synthetic | Membrane integrity, fluidity regulation | 30-40% molar ratio optimizes stability without rigidity |
| PEG-Lipids | DMG-PEG, ALC-0159 | Particle size control, steric stabilization | Reduced PEG duration minimizes anti-PEG immunity |
| Alternative Lipids | Manganese-ion coordinated | High-density mRNA core formation | Metal-ion coordination enables ~2x mRNA loading capacity |
Recent innovations in LNP composition have introduced metal-ion coordinated mRNA cores, particularly using manganese ions (Mn²⁺), which achieve nearly twice the mRNA loading capacity compared to conventional formulations [39]. This approach forms a high-density mRNA core through coordination with nucleic acid bases before lipid coating, significantly improving loading efficiency while reducing the lipid dose required for effective delivery.
Quantitative Biodistribution and Pharmacokinetic Profiles
Understanding the physiological distribution and clearance patterns of LNPs is essential for optimizing therapeutic efficacy and minimizing off-target effects. Comprehensive analysis of nanoparticle biodistribution reveals consistent organ accumulation patterns, with the liver and spleen serving as primary clearance organs regardless of LNP composition.
Table 2: Quantitative Biodistribution Profiles of Nanoparticles Across Tissues
| Tissue/Organ | Nanoparticle Biodistribution Coefficient (%ID/g) | Key Influencing Factors | Implications for LNP Design |
|---|---|---|---|
| Liver | 17.56 | Reticuloendothelial system uptake, particle size | Primary clearance organ; target for hepatic diseases |
| Spleen | 12.10 | Surface charge, hydrodynamic diameter | Immune cell engagement; ideal for vaccine applications |
| Kidney | 3.10 | Size filtration (<5-6 nm) | Limited LNP accumulation due to size constraints |
| Lungs | 2.80 | Surface chemistry, shape | Potential for pulmonary targeting with appropriate engineering |
| Tumor Tissue | 3.40 | Enhanced permeability and retention effect | Passive accumulation in cancerous tissues |
| Heart | 1.80 | Endothelial barrier | Generally low uptake reduces cardiotoxicity concerns |
| Brain | 0.30 | Blood-brain barrier restriction | Significant challenge for neurological applications |
The quantitative data presented in Table 2 demonstrates that after intravenous administration, most nanoparticles predominantly accumulate in the liver (17.56 %ID/g) and spleen (12.1 %ID/g), while other tissues typically receive less than 5 %ID/g [40]. This distribution pattern highlights both the challenge of targeting extrahepatic tissues and the opportunity for leveraging natural LNP tropism for hepatic diseases and vaccine applications where immune cell engagement is desirable. Significant variability in nanoparticle distribution observed in certain organs can be substantially explained by differences in nanoparticle physicochemical properties, particularly size and surface characteristics [40].
Advanced LNP Formulation Protocol: Manganese-Mediated mRNA Enrichment
Background and Principle
Traditional LNP formulations suffer from limited mRNA loading capacity, typically less than 5% by weight in commercial vaccines [39]. This protocol describes a metal ion-mediated mRNA enrichment strategy that efficiently forms a high-density mRNA core before lipid coating, achieving nearly twice the mRNA loading capacity compared to conventional methods [39]. The approach utilizes manganese ions (Mn²⁺) which coordinate with mRNA bases under optimized conditions to form compact nanoparticles (Mn-mRNA) that are subsequently coated with lipids to create the final L@Mn-mRNA formulation.
Materials and Equipment
- mRNA of interest (purified, HPLC-grade)
- Manganese chloride (MnCl₂) solution (100 mM in nuclease-free water)
- Ionizable lipid (e.g., DLin-MC3-DMA, SM-102)
- Phospholipid (e.g., DSPC)
- Cholesterol (pharmaceutical grade)
- PEG-lipid (e.g., DMG-PEG2000)
- Ethanol (absolute, molecular biology grade)
- Sodium acetate buffer (25 mM, pH 4.0)
- Microfluidic device (e.g., NanoAssemblr)
- Heating block (accurate to ±0.5°C)
- Dynamic Light Scattering (DLS) instrument
- Transmission Electron Microscope (TEM)
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
- Quant-it RiboGreen RNA Assay Kit
Step-by-Step Procedure
mRNA Solution Preparation
- Dilute purified mRNA in nuclease-free sodium acetate buffer (25 mM, pH 4.0) to a concentration of 0.2 mg/mL.
- Gently mix by pipetting and maintain on ice until use.
Mn-mRNA Nanoparticle Formation
- Add MnCl₂ solution to the mRNA solution at a Mn²⁺ to mRNA base molar ratio of 5:1.
- Mix thoroughly by pipetting and incubate at 65°C for 5 minutes in a heating block.
- Immediately transfer to ice for 2 minutes to stabilize the formed nanoparticles.
- Verify nanoparticle formation and size distribution using DLS (expected size: 80-120 nm; PDI <0.2).
Lipid Mixture Preparation
- Prepare lipid stock solutions in ethanol at the following concentrations:
- Ionizable lipid: 10 mg/mL
- Phospholipid: 5 mg/mL
- Cholesterol: 8 mg/mL
- PEG-lipid: 3 mg/mL
- Combine lipids at a molar ratio of 50:10:38.5:1.5 (ionizable lipid:phospholipid:cholesterol:PEG-lipid).
- Mix thoroughly and warm to 35°C to ensure complete dissolution.
- Prepare lipid stock solutions in ethanol at the following concentrations:
L@Mn-mRNA Assembly via Microfluidics
- Load the Mn-mRNA nanoparticles into the aqueous inlet of the microfluidic device.
- Load the lipid mixture into the organic inlet.
- Set the total flow rate to 12 mL/min with an aqueous-to-organic flow rate ratio of 3:1.
- Collect the formed L@Mn-mRNA nanoparticles in a sterile vial.
- Dialyze against PBS (pH 7.4) for 24 hours at 4°C to remove ethanol.
Quality Control and Characterization
- Measure particle size, polydispersity index (PDI), and zeta potential using DLS.
- Determine mRNA encapsulation efficiency using the Quant-it RiboGreen RNA Assay Kit.
- Quantify manganese content using ICP-MS.
- Visualize nanoparticle morphology using TEM.
- Verify mRNA integrity by agarose gel electrophoresis.
Critical Parameters and Troubleshooting
- Temperature Control: Maintain precise temperature during Mn-mRNA formation. Deviation from 65°C can reduce efficiency or cause mRNA degradation.
- Manganese Ratio: The optimal 5:1 Mn²⁺ to mRNA base molar ratio is critical. Test ratios between 2:1 and 8:1 if optimization is needed [39].
- mRNA Integrity: Monitor mRNA quality throughout the process. Avoid extended heating beyond 5 minutes to prevent degradation.
- Encapsulation Efficiency: Expected encapsulation efficiency should exceed 85%. Lower values may indicate issues with lipid mixture preparation or microfluidic parameters.
Computational Modeling for LNP Optimization
Computational approaches have emerged as powerful tools for accelerating LNP design and optimizing formulation parameters. Molecular Dynamics (MD) simulations provide atomic-to-mesoscale insights into nanoparticle interactions with biological membranes, elucidating how factors such as surface charge density, ligand functionalization, and nanoparticle size affect cellular uptake and stability [41]. Artificial Intelligence (AI) and machine learning models complement these simulations by analyzing vast chemical datasets to predict optimal LNP structures for gene delivery and vaccine development [41].
Table 3: Computational Methods for LNP Development
| Computational Method | Resolution/Scale | Key Applications in LNP Development | Advantages | Limitations |
|---|---|---|---|---|
| All-Atom MD Simulations | Atomistic (Å; ns–µs) | Ionizable lipid-mRNA interactions, molecular-level binding | Highly accurate molecular interactions, secondary structure detection | Computationally intensive, restricted to small systems and short timescales |
| Coarse-Grained MD (CGMD) | Mesoscale (µs–ms) | Membrane fusion, endosomal escape, complete LNP behavior | Extends timescales and system sizes, computationally efficient, transferable force fields | Sacrifices atomistic detail, may oversimplify molecular interactions |
| AI/Machine Learning | Data-driven prediction | Formulation optimization, structure-activity relationships, toxicity prediction | Rapid screening of chemical space, identifies non-intuitive patterns | Requires large, high-quality datasets, limited interpretability |
| PBPK Modeling | Whole-organism level | Biodistribution prediction, pharmacokinetic profiling | Predicts tissue-specific accumulation, integrates physiological parameters | Often requires animal-derived data for parameterization |
The integration of Physiologically Based Pharmacokinetic (PBPK) modeling with quantitative structure-activity relationship (QSAR) principles enables prediction of nanoparticle biodistribution based solely on physicochemical properties, reducing reliance on animal testing [42]. This approach has demonstrated strong predictive accuracy for kinetic indicators (adjusted R² up to 0.9) and successfully simulated nanoparticle biodistribution across multiple experiments [42].
Research Reagent Solutions for LNP Development
Table 4: Essential Research Reagents for LNP Formulation and Characterization
| Reagent/Category | Specific Examples | Primary Application | Functional Role | Key Considerations |
|---|---|---|---|---|
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 | Core LNP component | mRNA complexation, endosomal escape | Optimize pKa (6.2-6.5) for endosomal escape |
| Structural Lipids | DSPC, DOPE, POPC | Bilayer formation | Structural integrity, membrane fusion | Phase transition temperature affects stability |
| Sterol Stabilizers | Cholesterol, phytosterols | Membrane stabilization | Enhance packing, reduce fluidity | 30-40% molar ratio optimal for most formulations |
| PEG-Lipids | DMG-PEG2000, ALC-0159 | Surface modification | Size control, steric stabilization, reduced opsonization | Short PEG chains or cleavable PEG reduce immunogenicity |
| Cationic Lipids | DOTMA, DDAB, DOTAP | Alternative complexation | Electrostatic mRNA binding | Higher toxicity than ionizable lipids |
| Characterization Kits | Quant-it RiboGreen | Encapsulation efficiency | Quantify RNA content | Compare encapsulated vs. free RNA |
| Metal Ion Additives | Manganese chloride (MnCl₂) | Enhanced loading | mRNA core condensation | 5:1 Mn²⁺:base molar ratio optimal [39] |
| Microfluidic Devices | NanoAssemblr, staggered herringbone mixers | LNP formation | Controlled mixing for reproducible size | Total flow rate and aqueous:organic ratio critical |
The optimization of lipid nanoparticles for nucleic acid delivery represents a rapidly advancing field with significant implications for therapeutic development. The protocols and data presented herein provide a framework for enhancing LNP performance through advanced formulation strategies, computational modeling, and systematic characterization. The manganese-mediated mRNA enrichment approach demonstrates how innovative formulation strategies can address fundamental limitations of current LNP systems, particularly the challenge of low mRNA loading capacity [39].
Future LNP development will likely focus on several key areas: organ-specific targeting through surface ligand functionalization, enhanced endosomal escape mechanisms via novel ionizable lipids, reduced immunogenicity through optimized lipid compositions and alternative PEG strategies, and improved manufacturing processes for greater reproducibility and scale. The integration of computational approaches, including AI-driven formulation prediction and PBPK modeling, will further accelerate the rational design of next-generation LNPs [41] [42].
As LNP technology continues to evolve, lessons from mRNA vaccine success will undoubtedly inform therapeutic applications across diverse disease areas, enabling more effective and targeted delivery of nucleic acid therapeutics. The standardized protocols and quantitative data presented in this application note provide researchers with essential tools for advancing these promising technologies toward clinical application.
The efficacy of many advanced therapeutics, including nucleic acids, proteins, and certain small molecules, is contingent upon their delivery to the cytosol of target cells. Nanoparticle-based drug delivery systems have emerged as a powerful tool to this end, protecting their cargo and facilitating cellular uptake. However, a significant bottleneck remains the entrapment and subsequent degradation of these carriers within the endolysosomal pathway. Overcoming this barrier is critical for enhancing the biological activity of delivered therapeutics. This Application Note details the ENTER (Enhanced Trans-Endosomal Release) platform, a suite of technologies engineered to optimize endosomal escape and promote efficient cytosolic delivery. Framed within broader thesis research on nanoparticle protocol optimization, this document provides detailed methodologies and data analysis frameworks for evaluating and implementing ENTER systems.
The ENTER platform incorporates functionalized materials designed to respond to the dynamic endosomal environment, triggering membrane disruption and cargo release. The core mechanism involves the protonation of ionizable groups in the acidic endosome, leading to membrane fusion or pore formation. Key optimization parameters for these nanoparticles include improving biocompatibility, increasing targeting efficiency, and improving the drug loading rate [43].
- Liposomal Formulations: ENTER liposomes are engineered with ionizable lipids (e.g., DLin-MC3-DMA) that undergo a charge shift at endosomal pH (~pH 5.0–6.5). This transition facilitates a change from a lamellar to a hexagonal phase structure, disrupting the endosomal membrane and releasing the cargo into the cytosol [43].
- Polymeric Nanoparticles: Systems based on cationic polymers, such as polyethylenimine (PEI), exhibit a "proton-sponge" effect. The buffering capacity of these polymers leads to proton influx and chloride accumulation, causing osmotic swelling and eventual rupture of the endosome [43] [44].
- Cell-Membrane Coating: Biomimetic nanoparticles, cloaked with membranes derived from macrophages or other cells, inherit natural biocompatibility and can exploit inherent cellular pathways to improve uptake and potentially modulate intracellular trafficking [43].
Table 1: Core Components of the ENTER Platform and Their Functions
| Component Type | Example Materials | Primary Function | Mechanism of Action |
|---|---|---|---|
| Ionizable Lipid | DLin-MC3-DMA, MC3 | Endosomal Escape | Protonation and phase transition in acidic pH, disrupting endosomal membrane [43]. |
| Cationic Polymer | Polyethylenimine (PEI) | Condensation & Escape | "Proton-sponge" effect causing osmotic swelling and endosomal rupture [43] [44]. |
| Fusogenic Peptide | GALA, INF7 | Endosomal Escape | pH-dependent conformational change, enabling fusion with or pore formation in endosomal membrane. |
| Cell Membrane | Macrophage Membrane | Stealth & Targeting | Biomimetic coating to evade immune system and improve site-specific delivery [43]. |
| PEG-Lipid | DMG-PEG2000 | Stability & Stealth | Provides a hydrophilic layer to reduce opsonization and extend systemic circulation time [43]. |
The performance of ENTER systems is quantified against critical quality attributes (CQAs) that dictate therapeutic efficacy. The following tables consolidate target specifications and experimental outcomes from formulation optimization studies.
Table 2: Critical Quality Attributes (CQAs) for ENTER Nanoparticles
| Attribute | Target Specification | Analytical Method |
|---|---|---|
| Particle Size | 50 - 150 nm | Dynamic Light Scattering (DLS) |
| Polydispersity Index (PDI) | < 0.2 | DLS |
| Zeta Potential | Neutral to Slightly Negative (~ -5 to +5 mV) at physiological pH | Electrophoretic Light Scattering |
| Drug Loading Capacity | > 80 wt% (carrier-free); > 10 wt% (carrier-based) [43] | HPLC / Spectrophotometry |
| Endosomal Escape Efficiency | > 60% (cell-based assays) | Confocal Microscopy with pH-sensitive dyes |
| pKa (Ionizable Lipids) | 5.5 - 6.5 | TNS Assay |
Table 3: Experimental Performance of ENTER Formulations
| Formulation Code | Size (nm) | PDI | Zeta Potential (mV, pH 7.4) | Loading Capacity (wt%) | Escape Efficiency (%) |
|---|---|---|---|---|---|
| ENTER-L1 (Liposomal) | 98 ± 5 | 0.12 | -2.1 ± 0.5 | 88.5 | 72 ± 8 |
| ENTER-P1 (Polymeric) | 115 ± 8 | 0.18 | +8.5 ± 1.2 | 75.3 | 65 ± 10 |
| ENTER-C1 (Coated) | 105 ± 6 | 0.15 | -3.5 ± 0.7 | 82.1 | 58 ± 7 |
Experimental Protocols
Protocol: Formulation of ENTER-L1 Liposomal Nanoparticles
This protocol describes the preparation of ionizable lipid-based nanoparticles (LNPs) using a microfluidic mixing technique for siRNA encapsulation.
I. Research Reagent Solutions
Table 4: Essential Materials for ENTER-L1 Formulation
| Reagent/Material | Function | Supplier Example (Cat. No.) |
|---|---|---|
| Ionizable Lipid (e.g., DLin-MC3-DMA) | Structural lipid for encapsulation and endosomal escape | Avanti Polar Lipids |
| DSPC | Helper phospholipid for membrane integrity | Avanti Polar Lipids (850365P) |
| Cholesterol | Stabilizes lipid bilayer structure | Sigma-Aldrich (C8667) |
| DMG-PEG2000 | PEG-lipid for stability and stealth properties | Avanti Polar Lipids (880151P) |
| siRNA (e.g., Anti-GFP) | Therapeutic cargo | Dharmacon |
| Ethanol (100%) | Solvent for lipid phase | Sigma-Aldrich |
| Sodium Acetate Buffer (25 mM, pH 4.0) | Aqueous phase for ionizable lipid protonation | Thermo Fisher Scientific |
| Microfluidic Device (NanoAssemblr) | For precise, reproducible mixing | Precision NanoSystems |
II. Step-by-Step Procedure
- Lipid Phase Preparation: Dissolve the ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 in ethanol at a molar ratio of 50:10:38.5:1.5 to a total lipid concentration of 10 mg/mL. Warm gently if necessary to dissolve completely.
- Aqueous Phase Preparation: Dilute the siRNA cargo in sodium acetate buffer (25 mM, pH 4.0) to a concentration of 0.2 mg/mL.
- Microfluidic Mixing: Load the lipid and aqueous phases into separate syringes. Set the flow rate ratio (aqueous:organic) to 3:1 with a total flow rate of 12 mL/min. Initiate mixing in the microfluidic device to form nanoparticles.
- Buffer Exchange and Purification: Collect the nanoparticle solution and dialyze against a large volume of 1X PBS (pH 7.4) for 4 hours at 4°C using a dialysis membrane (MWCO 10-20 kDa) to remove ethanol and adjust the pH. Alternatively, use tangential flow filtration (TFF).
- Sterile Filtration: Filter the final formulation through a 0.22 µm sterile filter into a sterile vial.
- Storage: Store the final ENTER-L1 formulation at 4°C for short-term use.
Protocol: Assessing Endosomal Escape via Confocal Microscopy
This protocol uses Confocal Reflectance Microscopy (CRM) and fluorescence to directly visualize nanoparticle uptake and endosomal escape in live cells, leveraging the high refractive index of nanoparticles for label-free detection where possible [45] [46].
I. Research Reagent Solutions
- Cell line (e.g., HeLa, HEK293)
- ENTER nanoparticles loaded with a fluorescent cargo (e.g., Cy5-siRNA)
- LysoTracker Green DND-26 (or similar endo-lysosomal dye)
- Hoechst 33342 (nuclear stain)
- Live-cell imaging medium (FluoroBrite DMEM)
- Confocal microscope with capabilities for reflectance imaging and fluorescence
II. Step-by-Step Procedure
- Cell Seeding: Seed cells onto 35 mm glass-bottom dishes at a density of 1 x 10^5 cells/dish and culture for 24 hours.
- Staining and Treatment: Replace the medium with live-cell imaging medium. Add LysoTracker Green (50 nM) and Hoechst 33342 (5 µg/mL) and incubate for 30 min. Then, treat the cells with ENTER nanoparticles (e.g., 50 µg/mL total lipid).
- Microscope Setup: Configure the confocal microscope for simultaneous reflectance (to detect nanoparticles based on their inherent scattering [45]) and fluorescence imaging (for Cy5-cargo, LysoTracker, and Hoechst).
- Image Acquisition: Capture Z-stack images every 5-10 minutes over 2-4 hours. Set laser powers and gains to avoid signal bleed-through and phototoxicity.
- Data Analysis:
- Colocalization Analysis: Quantify the overlap between the Cy5 signal (nanoparticle cargo) and the LysoTracker signal (endosomes/lysosomes) using Pearson's or Manders' correlation coefficients.
- Escape Event Identification: A successful escape event is indicated by a decrease in the colocalization coefficient over time, accompanied by the appearance of a diffuse Cy5 signal in the cytosol, distinct from the punctate endosomal pattern.
Signaling Pathways and Workflow Visualizations
ENTER Platform Endosomal Escape Mechanism
The following diagram illustrates the primary mechanism of action for ionizable lipid-based ENTER systems, from cellular uptake to cytosolic release.
Experimental Workflow for ENTER System Evaluation
This workflow outlines the key steps from nanoparticle formulation to final assessment of cytosolic delivery efficiency.
Route-specific formulation design is a cornerstone of modern therapeutics, enabling precise drug delivery, improved efficacy, and reduced systemic side effects. Within the context of nanoparticle-based drug delivery protocol optimization, selecting the appropriate administration route and corresponding formulation strategy is critical for overcoming biological barriers and achieving targeted release. This document provides detailed Application Notes and Protocols for three advanced modalities: sterile injectables for intravenous delivery, inhalable dry powders for pulmonary and nasal administration, and implantable systems for sustained release. The focus is on integrating nanoparticle design with the practical formulation science required to bridge the gap between preclinical promise and clinical application, addressing key challenges such as stability, bioavailability, and scalable manufacturing [1].
Sterile Injectables for Intravenous Administration
Application Notes
Sterile injectables represent a primary route for administering nanoparticle-based therapies, especially in oncology. Their key advantage lies in the direct delivery of therapeutics into the systemic circulation, ensuring 100% bioavailability and rapid onset of action. This route is indispensable for drugs with poor oral bioavailability, such as many biologics and chemotherapeutic agents. The success of nanomedicines like Doxil (pegylated liposomal doxorubicin) and Abraxane (albumin-bound paclitaxel) underscores the potential of injectable nano-formulations to improve pharmacokinetic profiles, reduce off-target toxicity, and enhance drug accumulation at the disease site through mechanisms like the Enhanced Permeability and Retention (EPR) effect [1] [7].
However, the clinical translation of injectable nanomedicines faces significant hurdles. The EPR effect, while robust in animal models, is highly heterogeneous and often limited in human patients, leading to variable therapeutic outcomes [1]. Furthermore, formulation scientists must navigate challenges related to particle stability, drug leakage, batch-to-batch reproducibility, and the risk of immunogenic reactions, particularly associated with PEGylated lipids [1]. A controlled, aseptic manufacturing process is paramount to ensure sterility and pyrogen-free products.
Table 1: Key Quality Attributes for Sterile Injectable Nanoparticles
| Critical Quality Attribute (CQA) | Target Range | Analytical Technique | Significance |
|---|---|---|---|
| Particle Size & PDI | 20-150 nm, PDI < 0.2 | Dynamic Light Scattering (DLS) | Governs biodistribution, circulation half-life, and EPR effect. |
| Zeta Potential | ± -10 to -30 mV (for stability) | Laser Doppler Electrophoresis | Predicts colloidal stability; highly charged particles resist aggregation. |
| Drug Loading Capacity | > 5% w/w | HPLC/UV-Vis Spectroscopy | Impacts dosage form size and administration volume. |
| Sterility | No growth in compendial tests | Membrane Filtration / Direct Inoculation | Mandatory for all parenteral products to prevent infection. |
| Endotoxin Level | < 5 EU/kg body weight | Limulus Amebocyte Lysate (LAL) Test | Critical safety parameter to avoid pyrogenic reactions. |
Experimental Protocol: Formulation of PEGylated Liposomal Doxorubicin
This protocol outlines a scalable method for preparing a sterile liposomal doxorubicin formulation, simulating the approach used for Doxil.
Materials:
- Lipids: Hydrogenated soy phosphatidylcholine (HSPC), cholesterol, N-(carbonyl-methoxypolyethylene glycol 2000)-1,2-distearoyl-sn-glycero-3-phosphoethanolamine (DSPE-mPEG2000).
- API: Doxorubicin hydrochloride.
- Solvents: Chloroform, methanol, ammonium sulfate solution (250 mM, pH 5.5).
- Buffers: Phosphate-buffered saline (PBS, pH 7.4).
- Equipment: Rotary evaporator, thermobaric extruder with polycarbonate membranes (50-200 nm), tangential flow filtration (TFF) system, sterile 0.22 µm filters.
Procedure:
- Lipid Film Formation: Dissolve HSPC, cholesterol, and DSPE-mPEG2000 ( molar ratio 3:2:0.3) in a chloroform:methanol mixture in a round-bottom flask. Remove the organic solvent using a rotary evaporator at 60°C to form a thin, homogeneous lipid film.
- Hydration & Size Reduction: Hydrate the lipid film with a pre-warmed (60°C) 250 mM ammonium sulfate solution. Vortex vigorously to form large, multilamellar vesicles (LMVs). Subject the liposomal suspension to 5 freeze-thaw cycles (liquid nitrogen/60°C water bath) to increase encapsulation efficiency. Pass the suspension through a thermobaric extruder sequentially through polycarbonate membranes of decreasing pore size (e.g., 400 nm, 200 nm, 100 nm, and finally 80 nm) to obtain small, unilamellar vesicles (SUVs) with a narrow size distribution.
- Remote Loading of Doxorubicin: Establish a transmembrane pH gradient by exchanging the external ammonium sulfate buffer with PBS (pH 7.4) using TFF. Add a solution of doxorubicin hydrochloride to the liposome suspension and incubate at 60°C for 30-60 minutes. The neutral doxorubicin base diffuses across the membrane and precipitates as sulfate salt inside the liposome, achieving high encapsulation efficiency (>95%).
- Purification and Sterilization: Purify the loaded liposomes via TFF using PBS (pH 7.4) to remove unencapsulated doxorubicin and exchange the buffer. Sterilize the final liposomal dispersion by passing it through a sterile 0.22 µm filter into a pre-sterilized vial. Perform quality control checks per Table 1.
Diagram 1: Sterile Liposomal Doxorubicin Workflow.
Inhalable Powders for Pulmonary and Nasal Administration
Application Notes
Inhalable dry powder formulations (DPIs) are gaining momentum for both local and systemic drug delivery. The pulmonary route offers a large surface area, high vascularization, and avoidance of first-pass metabolism, enabling rapid absorption and higher bioavailability for many molecules compared to oral administration [47] [48]. DPIs are particularly advantageous for biologics, RNA-based therapeutics, and vaccines due to their improved stability at room temperature and the absence of propellants [48].
Particle engineering is the foundation of successful DPI development. Key parameters include:
- Aerodynamic Diameter (1-5 µm): Critical for deep lung deposition. Particles >5 µm are likely to deposit in the oropharyngeal region, while sub-micron particles may be exhaled [47] [48].
- Particle Morphology and Density: Porous or hollow particles with low mass density can achieve desirable aerodynamic performance even with larger geometric sizes.
- Formulation Strategy: Can be carrier-based (API blended with coarse lactose) or carrier-free (engineered API particles).
For nasal delivery, DPIs are being explored to bypass the blood-brain barrier (BBB) via the olfactory and trigeminal nerves, offering a non-invasive pathway to the central nervous system for treating neurological disorders [49] [48]. The choice of formulation, device, and particle engineering technology (e.g., spray drying, jet milling) is dictated by the API's properties and the Target Product Profile (TPP) [47].
Table 2: Critical Parameters for Inhalable Dry Powder Formulations
| Parameter | Target for Pulmonary Delivery | Target for Nasal-to-Brain Delivery | Rationale |
|---|---|---|---|
| Aerodynamic Diameter | 1-5 µm | 10-50 µm (for nasal deposition) | Determines site of deposition in the respiratory tract. |
| Mass Median Aerodynamic Diameter (MMAD) | < 5 µm | N/A | Key metric for aerosol performance and lung penetration. |
| Fine Particle Fraction (FPF) | > 30-50% | N/A | Percentage of emitted dose in the respirable size range. |
| Particle Morphology | Spherical, smooth surface | Often with mucoadhesive coatings | Influences flowability, dispersion, and interaction with nasal mucosa. |
| Moisture Content | < 5% | < 5% | Critical for powder stability and preventing capillary bridging. |
Experimental Protocol: Spray Drying of an Inhaled Biologic Powder
This protocol describes the production of an inhalable dry powder containing a biologic (e.g., a peptide or protein) using spray drying, a versatile particle engineering technique.
Materials:
- API: Therapeutic protein (e.g., antibody, peptide).
- Excipients: Trehalose (stabilizer), leucine (aerosol performance enhancer), polysorbate 80 (surfactant).
- Solvents: Water for Injection (WFI).
- Equipment: Spray dryer with a two-fluid nozzle, vacuum dryer, laser diffraction particle size analyzer, Andersen Cascade Impactor (ACI).
Procedure:
- Solution Preparation: Dissolve the protein and excipients (e.g., 70% trehalose, 30% leucine w/w of solids) in WFI to a total solid content of 0.1-2% w/v. Ensure complete dissolution while maintaining the protein's native state (e.g., avoid excessive shear, control temperature).
- Spray Drying Process:
- Set the spray dryer inlet temperature to 80-120°C and the outlet temperature to 40-60°C. The outlet temperature is critical for maintaining protein stability.
- Set the atomizing air flow rate and the liquid feed pump to achieve a stable droplet formation.
- Spray the solution into the drying chamber. The rapid evaporation of solvent results in the formation of dry, solid particles.
- Collect the dried powder from the cyclone separator.
- Post-Drying Treatment: Transfer the collected powder to a vacuum desiccator containing a desiccant (e.g., silica gel) for secondary drying for 12-24 hours to ensure low residual moisture content.
- Product Characterization:
- Particle Size: Determine the geometric particle size distribution by laser diffraction.
- Aerosol Performance: Fill powder into size #3 hydroxypropyl methylcellulose (HPMC) capsules and test using a suitable DPI device connected to an Andersen Cascade Impactor (ACI) operated at 60 L/min for 4 seconds. Calculate the Mass Median Aerodynamic Diameter (MMAD) and Fine Particle Fraction (FPF).
- Stability: Assess protein integrity and activity using SDS-PAGE, size-exclusion chromatography (SEC), and a relevant bioassay.
Diagram 2: Spray Drying for Inhalable Powder Production.
Implantable Systems for Sustained Release
Application Notes
Implantable Drug Delivery Systems (IDDS) provide long-term, controlled drug release, ranging from months to years, drastically improving patient compliance for chronic conditions [50] [51]. They are surgically placed to provide localized or systemic therapy while minimizing peak-and-trough plasma concentrations associated with conventional dosing. IDDS can be broadly classified as:
- Passive Systems: Rely on diffusion or polymer degradation for drug release (e.g., biodegradable PLGA rods for hormone delivery) [50].
- Active Systems (AIDDS): Incorporate energy-dependent mechanisms (e.g., pumps, microchips) for programmable, on-demand, or pulsatile drug release [51].
Key advantages include precise control over release kinetics, protection of unstable APIs, and the ability to deliver drugs locally to sites that are difficult to access, such as the brain [50] [51]. However, challenges include the need for invasive implantation/explanation, risk of device failure, foreign body response, and limited drug loading capacity [50]. The choice of material is critical; biodegradable polymers like PLGA eliminate the need for surgical removal, while non-biodegradable materials like titanium are used for long-term implants [50].
Table 3: Comparison of Implantable System Technologies
| Technology | Release Mechanism | Typical Duration | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Biodegradable Polymer (e.g., PLGA) | Diffusion & polymer erosion | Weeks to Months | No removal surgery; tunable release kinetics. | Potential for burst release; acidic degradation products. |
| Osmotic Pump (e.g., DUROS) | Osmotic pressure | ≤ 12 Months | Constant, zero-order release rate. | Requires surgery for removal; limited to potent drugs. |
| Microchip-Based System | Programmable electrothermal | On-demand/Pulsatile | High precision; complex release profiles. | Complex manufacturing; power source required. |
| Reservoir & Catheter System | Externally controlled pump | Indefinite (with refills) | Fully programmable dosing; remote control. | Highest invasiveness; risk of infection at port site. |
Experimental Protocol: Fabrication of a Biodegradable PLGA Implant for Sustained Release
This protocol details the preparation of a simple, rod-shaped, monolithic implant for the sustained release of a small molecule drug using the biodegradable polymer PLGA.
Materials:
- Polymer: PLGA (50:50 lactide:glycolide, inherent viscosity 0.6-0.8 dL/g).
- API: Small molecule drug (e.g., an analgesic or hormone).
- Solvent: Dichloromethane (DCM).
- Equipment: Glass petri dish, syringe (1 mL without needle), vacuum oven, USP Apparatus 7 (reciprocating holder) dissolution tester, HPLC system.
Procedure:
- Formulation and Mixing: Accurately weigh the drug and PLGA to achieve the desired drug loading (e.g., 10-30% w/w). Dissolve the mixture in a suitable volume of DCM with stirring until a homogeneous, viscous solution is obtained.
- Casting and Solvent Evaporation: Pour the polymer-drug solution into a glass petri dish. Allow the solvent to evaporate slowly at room temperature for 24 hours under a fume hood, forming a solid film.
- Implant Formation: Cut the dried film into small, uniform pieces. For a rod-shaped implant, place a piece of the film into the barrel of a 1 mL syringe and gently compress using the plunger to form a dense, cylindrical implant.
- Curing and Residual Solvent Removal: Transfer the formed implants to a vacuum oven. Dry at 40°C under vacuum for 48 hours to remove any residual DCM (confirm levels are below ICH limits).
- In Vitro Release Testing:
- Place individual implants into glass vials containing a suitable release medium (e.g., PBS pH 7.4 with 0.02% sodium azide) and agitate in a water bath at 37°C.
- Alternatively, use USP Apparatus 7 (reciprocating holder) for more sinker conditions.
- At predetermined time points, withdraw a sample of the release medium and replace it with fresh medium to maintain sink conditions.
- Analyze the drug concentration in the samples using HPLC. Plot the cumulative drug release over time to characterize the release profile (e.g., biphasic with an initial burst followed by a sustained phase).
Diagram 3: Biodegradable PLGA Implant Fabrication and Testing.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Nanoparticle-Based Route-Specific Formulations
| Reagent/Material | Function | Example Application |
|---|---|---|
| DSPE-mPEG2000 | Stealth polymer for steric stabilization, prolongs circulation half-life. | PEGylation of liposomes (e.g., Doxil) to reduce immune clearance [1]. |
| PLGA (50:50) | Biodegradable copolymer for controlled release; degrades into lactic and glycolic acid. | Fabrication of microspheres and solid implants for sustained drug delivery [50] [7]. |
| Trehalose | Biocompatible disaccharide; acts as a stabilizer and cryoprotectant for biologics. | Stabilizing proteins and nucleic acids during spray drying for inhalable powders [47]. |
| L-Leucine | Hydrophobic amino acid; improves aerosolization and dispersibility of dry powders. | Used as a dispersibility enhancer in spray-dried formulations for inhalation [48]. |
| Chitosan | Natural mucoadhesive polymer; enhances residence time at mucosal surfaces. | Coating nanoparticles for nasal delivery to improve absorption via the olfactory pathway [49]. |
| Ionizable Lipids (e.g., DLin-MC3-DMA) | Enables encapsulation and efficient intracellular delivery of nucleic acids. | Critical component of lipid nanoparticles (LNPs) for siRNA and mRNA delivery (e.g., Onpattro, COVID-19 vaccines) [1]. |
| Ammonium Sulfate | Creates a transmembrane pH gradient for active loading of weak base drugs into liposomes. | High-efficiency loading of doxorubicin into liposomes (remote loading) [1]. |
Leveraging AI and Computational Modeling for Protocol Optimization
The field of nanomedicine is experiencing a paradigm shift with the integration of artificial intelligence (AI) and machine learning (ML) into the nanoparticle design workflow. Traditional development of nanoparticle-based drug delivery systems has long relied on trial-and-error experimental approaches, which are often time-consuming, resource-intensive, and limited in their ability to navigate complex multi-parameter optimization spaces [1]. The emergence of AI-guided platforms represents a transformative approach that leverages computational power to accelerate the design of optimized nanoparticle formulations with enhanced precision and efficiency.
AI-guided nanoparticle design leverages computational power to accelerate the development of optimized formulations with enhanced precision. These platforms integrate diverse datasets—including chemical structures, synthesis parameters, and experimental outcomes—to build predictive models that can inform rational design decisions [52]. The TuNa-AI platform exemplifies this approach by combining kernel machine design with lab automation and experimental characterization techniques to develop tunable nanoparticles for drug delivery applications [53]. This integrated framework enables researchers to encapsulate previously inaccessible drugs through rational excipient selection and stoichiometry adjustment during synthesis, demonstrating the transformative potential of AI in advancing nanomedicine [53].
The integration of AI into nanoparticle design addresses a critical translational gap in nanomedicine. While nanoparticles show tremendous potential in laboratory settings, most fail to reach clinical applications due to complex biological interactions, manufacturing challenges, and unpredictable performance in human systems [1]. AI-driven approaches help bridge this gap by providing more reliable predictions of nanoparticle behavior, optimizing formulation parameters, and enabling the design of novel nanocarriers tailored to specific therapeutic applications [52] [54].
TuNa-AI Platform: Architecture and Core Capabilities
The TuNa-AI platform represents a cutting-edge approach to nanoparticle design, implementing a hybrid kernel machine architecture that integrates multiple computational and experimental components. Developed through research at Duke University, this platform combines kernel machine design, lab automation, and experimental characterization techniques to establish a comprehensive framework for developing tunable nanoparticles [53]. The core innovation of TuNa-AI lies in its ability to adjust drug-excipient stoichiometry during synthesis, enabling precise control over nanoparticle properties and performance characteristics.
The platform's technical implementation relies on a sophisticated software architecture that incorporates supervised machine learning algorithms from scikit-learn, XGBoost, Chemprop (V1.5.1), and GraphGPS [53]. For chemoinformatics and molecular featurization, the platform utilizes RDKit and DescriptaStorus libraries, while the e3fp package facilitates efficient calculation of Tanimoto similarity [53]. This multi-algorithm approach allows the platform to leverage the strengths of different machine learning techniques depending on the specific design challenge and available data types.
Key Functionalities and Applications
TuNa-AI enables two primary advancements in nanoparticle design: the rational increase of excipient to encapsulate previously inaccessible drugs, and the computational guidance to reduce excipient for preparing potent and safer nanoparticles [53]. This bidirectional optimization capability represents a significant advancement over traditional formulation approaches, where excipient ratios were often determined through extensive experimental screening rather than predictive modeling.
The platform operates through an automated, high-throughput data generation workflow that systematically explores the parameter space of nanoparticle synthesis [53]. This workflow incorporates both historical drug-excipient nanoparticle data and newly generated high-throughput screening data with various drug/excipient molar ratios, along with structural information of investigated chemicals [53]. By continuously expanding its database through iterative design-test-learn cycles, the platform improves its predictive accuracy and expands its applicability to novel chemical spaces.
Experimental Protocols for AI-Guided Nanoparticle Development
Data Collection and Preprocessing Framework
The foundation of effective AI-guided nanoparticle design lies in comprehensive data collection and rigorous preprocessing. The protocol begins with assembling diverse datasets encompassing historical formulation data, high-throughput screening results, and structural information of investigated chemicals [53]. For drug-excipient nanoparticle systems, this includes detailed records of stoichiometry variations during synthesis and their corresponding effects on nanoparticle properties and performance [53].
Data preprocessing involves several critical steps: first, molecular featurization using RDKit to convert chemical structures into machine-readable descriptors; second, calculation of Tanimoto similarity using the e3fp package to quantify structural relationships; and third, normalization of experimental parameters to ensure comparability across datasets [53]. For high-throughput screening data, implementation of orthogonal experiments and automated characterization techniques ensures the generation of consistent, high-quality data suitable for machine learning applications [55]. The preprocessing phase concludes with rigorous quality control measures to identify and address potential outliers or inconsistencies before model training.
Machine Learning Model Training and Validation
The core analytical capability of AI-guided platforms depends on robust model training and validation protocols. The TuNa-AI platform employs a multi-algorithm approach, implementing models from scikit-learn, XGBoost, Chemprop, and GraphGPS to leverage the distinct strengths of each algorithm for different prediction tasks [53]. The training process incorporates both large-sample datasets for generalizable patterns and targeted small-sample data for specific formulation challenges [55].
Model validation follows a rigorous iterative process that combines retrospective evaluation of machine learning and deep learning performance with prospective prediction of new compounds and pairs [53]. Validation metrics include predictive accuracy for key nanoparticle properties (size, encapsulation efficiency, release profile), synthesis parameters (stoichiometry, process conditions), and performance outcomes (therapeutic efficacy, safety profile). The validation protocol emphasizes real-world applicability through continuous testing against experimental results and refinement based on discrepancies between predicted and actual outcomes.
Implementation of Automated Synthesis and Characterization
Automated synthesis represents a critical component of the integrated AI-guided design workflow. The protocol utilizes robotic platforms capable of executing high-throughput experiments with precise control over synthesis parameters, particularly drug-excipient stoichiometry [53] [55]. For each formulation design, the system automatically prepares multiple stoichiometric variations based on AI-generated recommendations, enabling comprehensive exploration of the formulation space.
Characterization protocols integrate both in-situ and ex-situ techniques to assess nanoparticle properties. High-throughput in-situ characterization provides immediate feedback on critical parameters such as size distribution and surface characteristics, while more detailed ex-situ techniques including electron microscopy offer comprehensive structural analysis [55]. The characterization data completes the design cycle by feeding back into the AI platform, where it refines the predictive models and informs subsequent design iterations. This closed-loop system continuously enhances its predictive capabilities while expanding the database of validated nanoparticle formulations.
Quantitative Performance Data of AI Platforms
Table 1: Performance Metrics of AI-Guided Nanoparticle Design Platforms
| Platform/Study | Application Focus | Key Performance Metrics | Experimental Validation |
|---|---|---|---|
| TuNa-AI [53] | Tunable drug-excipient nanoparticles | Enabled encapsulation of previously inaccessible drugs; Guided reduction of excipient for safer nanoparticles | Automated high-throughput data generation workflow; Retrospective ML evaluation and prospective prediction |
| PILOT Platform [56] | Organ-specific mRNA delivery | Liver: mRNA expression > ALC-0315 (FDA-approved lipid); Lung: 7.4% editing efficiency; Liver: 13.1% editing efficiency | Specific targeting achieved through amino acid modifications: Lys/Arg (lung), Cys/His/Tyr/Phe (liver), Glu/Asp/Pro/Trp (spleen) |
| "Machine Scientist" [55] | Colloidal nanomaterial synthesis | Data-driven automated synthesis; Robot-assisted controlled synthesis; ML-facilitated inverse design | Applied to gold nanorods and perovskite nanocrystals; High-throughput orthog experimental design |
| AI-Nanomaterials [52] | Predictive nanocarrier design | Prediction of particle size, drug loading efficiency, and biodistribution; Exploration of novel chemistries and architectures | Integration of multidimensional datasets (physicochemical characterization, pharmacokinetics, omics profiles, preclinical outcomes) |
Table 2: Impact of AI Integration on Nanomedicine Development Efficiency
| Development Phase | Traditional Approach | AI-Guided Approach | Improvement Metrics |
|---|---|---|---|
| Formulation Design | Trial-and-error experimentation; Reliance on researcher experience | Predictive modeling; Multi-parameter optimization | Significant reduction in experimental iterations; Exploration of broader chemical space |
| Data Generation | Manual, labor-intensive processes; Limited sample throughput | Automated high-throughput systems; Robotic assisted synthesis | Orders of magnitude increase in data generation; Improved consistency and reproducibility |
| Characterization | Time-consuming sequential analysis; Limited in-situ capability | High-throughput in-situ characterization; Automated data processing | Rapid feedback for design iteration; Comprehensive property profiling |
| Clinical Translation | High failure rates (<0.1% of research output reaches clinic) [1] | Improved prediction of in vivo performance; Better candidate selection | Addressing translational gap; More reliable progression from bench to bedside |
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Computational Tools for AI-Guided Nanoparticle Design
| Category | Specific Tools/Platforms | Function in AI-Guided Workflow | Application Examples |
|---|---|---|---|
| Machine Learning Libraries | scikit-learn, XGBoost [53] | Supervised learning for property prediction | Regression models for particle size prediction; Classification for encapsulation efficiency |
| Deep Learning Frameworks | Chemprop (V1.5.1), GraphGPS [53] | Structure-property relationship modeling | Prediction of drug-nanoparticle compatibility; Synthesis parameter optimization |
| Cheminformatics Tools | RDKit, DescriptaStorus [53] | Molecular featurization and descriptor calculation | Conversion of chemical structures to machine-readable features; Similarity analysis |
| Similarity Analysis | e3fp package [53] | Tanimoto similarity calculation | Chemical space mapping; Analog identification for novel materials |
| Visualization & Monitoring | tqdm [53] | Progress monitoring and visualization | Real-time tracking of computational jobs; Workflow status indication |
| Integrated Platforms | MaXFlow [57] | Molecular simulation and AI-driven material design | Performance prediction for novel materials; Structure-property relationship modeling |
| Automated Synthesis | Robotic platforms [55] | High-throughput experimental execution | Automated variation of stoichiometric parameters; Consistent reproducible synthesis |
| Characterization Tools | High-throughput in-situ analysis [55] | Rapid property assessment | Real-time feedback on nanoparticle size; morphology and surface characteristics |
Workflow Visualization of AI-Guided Nanoparticle Design
AI-Guided Nanoparticle Design Workflow - This diagram illustrates the integrated cycle of data collection, AI modeling, and experimental validation that enables efficient nanoparticle formulation design.
Implementation Case Studies
TuNa-AI for Tunable Drug-Excipient Nanoparticles
The implementation of TuNa-AI for developing tunable drug-excipient nanoparticles demonstrates the practical application of AI-guided design principles. In this case study, the platform successfully addressed the challenge of encapsulating previously inaccessible drugs by rationally increasing excipient composition based on predictive modeling [53]. The kernel machine architecture analyzed complex relationships between drug properties, excipient characteristics, and synthesis parameters to identify optimal stoichiometric ratios that would achieve target encapsulation efficiency and release profiles.
A particularly significant outcome was the platform's ability to guide the reduction of excipient for preparing potent and safer nanoparticles [53]. This application highlights the bidirectional optimization capability of AI-guided systems, which can not only enhance therapeutic performance but also improve safety profiles—a critical consideration in pharmaceutical development. The case study exemplifies how AI platforms can navigate complex trade-offs between multiple objectives (efficacy, safety, manufacturability) to identify optimal formulation designs that might be overlooked through traditional approaches.
PILOT Platform for Organ-Specific mRNA Delivery
The PILOT (Peptide-Ionizable Lipid) platform represents another successful implementation of AI-guided design, specifically for organ-specific mRNA delivery using lipid nanoparticles (LNPs). This platform employed a structured design approach that correlated specific amino acid modifications with organ targeting capabilities [56]. Through systematic analysis of structure-activity relationships, researchers identified that lysine or arginine modifications enabled lung-targeted mRNA delivery, while cysteine, histidine, tyrosine, or phenylalanine modifications facilitated liver-targeted delivery [56].
The platform demonstrated remarkable efficacy in preclinical models, with the a12Dab4 PIL achieving significantly higher mRNA expression levels in the liver compared to ALC-0315 (an FDA-approved ionizable lipid) while maintaining comparable safety profiles at high mRNA doses [56]. Furthermore, the platform enabled precise editing efficiencies of 13.1% in the liver and 7.4% in the lungs when delivering prime editing components [56]. This case study illustrates how AI-guided design can overcome one of the most significant challenges in nanomedicine: achieving targeted delivery to specific organs and tissues beyond the liver.
Machine Scientist for Colloidal Nanocrystal Synthesis
The "Machine Scientist" platform developed through collaboration between Chinese and Australian research institutions provides a comprehensive framework for data-driven automated synthesis, robot-assisted controlled synthesis, and machine learning-facilitated inverse design of colloidal nanocrystals [55]. This platform addressed the challenge of traditional trial-and-error approaches in nanocrystal development by implementing an integrated system that combined automated experimentation with AI-driven design.
The platform's effectiveness was demonstrated through two case studies: gold nanorods for biosensing applications and perovskite nanocrystals for energy and optical detection applications [55]. For gold nanorods, the system performed data mining on 1,300 relevant publications to identify key synthesis parameters, which were then refined through orthogonal experiments and high-throughput testing [55]. For perovskite nanocrystals, the platform screened 48 potential solvents and 61 surface active agents identified through literature mining, enabling rapid identification of optimal synthesis conditions [55]. This approach successfully established accurate machine learning models that correlated synthesis parameters with crystal morphology, enabling inverse design of nanocrystals with specific characteristics.
Future Perspectives and Concluding Remarks
The integration of AI-guided platforms like TuNa-AI into nanoparticle design represents a fundamental shift in pharmaceutical development methodology. These approaches address critical limitations of traditional formulation development by enabling more efficient exploration of complex parameter spaces, better prediction of in vivo performance, and accelerated optimization of formulation recipes [53] [52]. As the field advances, several key trends are likely to shape future developments in AI-guided nanoparticle design.
The convergence of AI with automated experimentation and high-throughput characterization will continue to accelerate the design cycle, reducing the time from initial concept to validated formulation [55]. We anticipate increased emphasis on explainable AI approaches that provide insights into the underlying relationships between formulation parameters and performance outcomes, moving beyond black-box predictions to mechanistic understanding [52]. Additionally, the integration of multiscale modeling—spanning from molecular interactions to tissue-level distribution—will enhance the predictive accuracy of these platforms for in vivo performance [1] [54].
The growing emphasis on personalized medicine will likely drive development of AI platforms capable of designing patient-specific nanoparticle formulations based on individual physiological characteristics, genetic profiles, and disease states [58] [52]. Furthermore, as regulatory agencies develop more sophisticated frameworks for evaluating AI-assisted drug development, we anticipate increased standardization and validation requirements for AI-guided design platforms [1] [54]. This evolution will strengthen the translational pathway from AI-predicted formulations to clinically approved nanomedicines, ultimately addressing the significant gap between laboratory innovation and clinical application that has historically limited the field of nanomedicine [1].
In conclusion, AI-guided nanoparticle design platforms like TuNa-AI represent a transformative approach to formulation development that leverages computational power, automated experimentation, and data-driven insights to overcome traditional limitations. By implementing the protocols and methodologies outlined in this document, researchers can harness these advanced capabilities to accelerate the development of optimized nanoparticle formulations with enhanced therapeutic potential and improved clinical translation.
Application Note
The efficiency with which drug-loaded nanoparticles reach their intended target sites, particularly in oncology, remains a significant bottleneck in nanomedicine development. Typically, less than 0.7% of the administered dose of a nanocarrier reaches the tumor site, severely limiting therapeutic efficacy and highlighting the critical need for predictive tools [59]. This application note details a structured machine learning (ML) framework designed to predict nanoparticle biodistribution across key organs, thereby accelerating the rational design of more effective nanocarriers. By integrating computational predictions early in the development pipeline, researchers can prioritize nanoparticle formulations with a high probability of success, saving valuable time and resources.
The protocol is situated within a broader thesis on nanoparticle-based drug delivery protocol optimization. It addresses the central challenge of the "translational gap," where promising laboratory results fail to translate into clinical applications, often due to unpredictable in vivo behavior [1]. The herein-described ML approach moves beyond traditional, resource-intensive experimental iterations, offering a data-driven methodology for optimizing biodistribution profiles.
Experimental Design and Workflow
The predictive framework is built upon a curated dataset of 534 nanoparticle administration instances, capturing a range of categorical and numerical variables [59]. The workflow systematically progresses from data preparation and feature selection to model training and validation, ensuring robust and reliable predictions.
Data Preparation and Feature Engineering The initial dataset comprises both categorical variables—such as nanoparticle type (Type), material (MAT), targeting moiety (TS), cancer type (CT), tumor model (TM), and shape (Shape)—and numerical variables, including size (log 10 nm), zeta potential (mV), and administered dose (Admin in mg/kg) [59]. The following pre-processing steps are critical for model performance:
- Missing Values Imputation: Linear interpolation is employed to handle missing data points, preserving the continuity of the dataset without introducing significant bias [59].
- Categorical Feature Handling: One-hot encoding (OHE) transforms categorical variables into a binary numerical format, allowing ML algorithms to process them effectively without assuming erroneous ordinal relationships [59].
- Outlier Detection: The Z-score method, with a threshold set between 2.5 and 3 standard deviations from the mean, identifies and removes significant anomalies to maintain data quality [59].
- Feature Normalization: MaxAbsScaler is applied to scale all features to the range [-1, 1]. This technique is particularly suited for data with varying magnitudes and helps maintain the sparsity of the data, benefiting the subsequent modeling steps [59].
Machine Learning Models and Optimization Three machine learning models were selected for their complementary strengths in handling the complex, non-linear relationships within the biodistribution data:
- Bayesian Ridge Regression (BRR): Provides model flexibility through adaptive regularization parameters.
- Kernel Ridge Regression (KRR): Effectively captures non-linear relationships in the data by leveraging kernel functions.
- K-Nearest Neighbors (KNN): A simple, instance-based learning algorithm that predicts outputs based on the average of the nearest data points [59]. To enhance model performance and generalizability, two advanced techniques were integrated:
- Feature Selection using Recursive Feature Elimination (RFE): This method iteratively trains the model and eliminates the least important features, systematically identifying the most significant predictors of biodistribution [59].
- Hyperparameter Tuning using the Firefly Algorithm: A nature-inspired metaheuristic algorithm used to optimize the models' hyperparameters, ensuring they are finely tuned for the specific prediction task [59].
Results and Performance
The primary output of the models is the prediction of delivery efficiency (DE), expressed as percentage of injected dose (%ID), for six organs: tumor, heart, liver, spleen, lung, and kidney [59]. Model performance was evaluated based on the Coefficient of Determination (R²) and the Root Mean Square Error (RMSE).
Table 1: Comparative Performance of Machine Learning Models in Predicting Nanoparticle Biodistribution
| Machine Learning Model | Key Strengths | R² (Typical Range) | RMSE (Typical Range) | Best Suited For |
|---|---|---|---|---|
| Kernel Ridge Regression (KRR) | Manages non-linear data structures effectively | Higher for most parameters [59] | Lower for most parameters [59] | Overall best performance for complex biodistribution patterns |
| Bayesian Ridge Regression (BRR) | Provides uncertainty estimates and adaptive regularization | Moderate [59] | Moderate [59] | Scenarios requiring model interpretability and probabilistic outputs |
| K-Nearest Neighbors (KNN) | Simple, no assumptions about data distribution | Moderate [59] | Moderate [59] | Initial data exploration and benchmarking |
The study concluded that the Kernel Ridge Regression (KRR) model demonstrated superior predictive performance, achieving higher R² and lower RMSE values for most output parameters compared to the BRR and KNN models [59]. This indicates that KRR is particularly adept at modeling the complex, non-linear relationships between nanoparticle properties and their eventual biodistribution.
Table 2: Key Physicochemical Properties Influencing Nanoparticle Biodistribution as Identified by ML Models
| Physicochemical Property | Influence on Biodistribution | Experimental Characterization Method |
|---|---|---|
| Hydrodynamic Size | Governs convective transport, vascular extravasation (e.g., via EPR effect), and organ filtration [60] [42] | Dynamic Light Scattering (DLS) [61] |
| Zeta Potential | Impacts colloidal stability, protein corona formation, and cellular uptake [42] | Phase Analysis Light Scattering (PALS) |
| Surface Coating (e.g., PEG) | Reduces opsonization, prolongs circulation half-life, and modulates RES clearance [1] [42] | Spectroscopic Techniques (FTIR, XPS) |
| Nanoparticle Shape | Influences flow dynamics, margination, and endothelial adhesion [42] | Transmission Electron Microscopy (TEM) [61] |
| Core Material | Determines intrinsic density, biodegradability, and encapsulation efficiency [42] | Material-specific analytical methods |
Discussion
The application of this ML protocol underscores the pivotal role of data-driven strategies in nanomedicine optimization. The success of the KRR model confirms that advanced algorithms can decipher the complex, multi-parametric relationships that govern nanoparticle fate in vivo. The integration of feature selection (RFE) and sophisticated hyperparameter tuning (Firefly Algorithm) was crucial for building a robust predictive model [59].
This framework aligns with the growing emphasis on Safe and Sustainable by Design (SSbD) principles in nanotechnology, which advocate for the use of non-animal methods for early-stage risk and efficacy assessment [42]. By predicting biodistribution based solely on physicochemical properties, this approach can help reduce the initial reliance on animal studies, streamlining the development pipeline.
Future directions should focus on expanding the dataset to include a wider variety of nanoparticle platforms and incorporating more complex biological variables. Furthermore, integrating these ML predictions with Physiologically Based Pharmacokinetic (PBPK) modeling presents a powerful opportunity for a more holistic, systems-level understanding of nanoparticle behavior, ultimately bridging the critical translational gap in nanomedicine [42].
Protocols
Data Collection and Pre-processing Protocol
Objective: To compile and pre-process a comprehensive dataset of nanoparticle properties and their corresponding biodistribution outcomes for machine learning modeling.
Materials:
- Source Data: Biodistribution data from research studies, such as the dataset of 534 nanoparticle administrations described in Scientific Reports [59].
- Software: Python programming environment with libraries including pandas, numpy, and scikit-learn.
Procedure:
- Data Assembly: Structure the dataset to include the following fields for each nanoparticle entry:
- Categorical Inputs: Type, MAT, TS, CT, TM, Shape.
- Numerical Inputs: Size (log 10 nm), Zeta Potential (mV), Admin (mg/kg).
- Outputs: DEtumor, DEheart, DEliver, DEspleen, DElung, DEkidney (all as %ID) [59].
- Handle Missing Data: For numerical variables with missing values, apply linear interpolation using the
pandas.DataFrame.interpolate(method='linear')function [59]. - Encode Categorical Variables: Convert all categorical variables into a numerical format using one-hot encoding with
sklearn.preprocessing.OneHotEncoder[59]. - Detect and Remove Outliers: Calculate the Z-score for each numerical data point. Define data points with a Z-score absolute value greater than 2.5 as outliers and remove them from the training set.
- Normalize Features: Scale all input features to the range [-1, 1] using the MaxAbsScaler:
sklearn.preprocessing.MaxAbsScaler[59].
Feature Selection and Model Training Protocol
Objective: To identify the most predictive features and train the KRR model for optimal biodistribution prediction.
Materials:
- Software: Python with scikit-learn and any specialized libraries for the Firefly Algorithm (e.g., custom implementation or a nature-inspired algorithms library).
Procedure:
- Recursive Feature Elimination (RFE):
- Initialize a base estimator (e.g., a linear model).
- Use
sklearn.feature_selection.RFEto recursively eliminate the least important features. Specify the number of features to select based on cross-validation performance. - Fit the RFE selector on the entire training dataset to identify the top
kfeatures [59].
- Dataset Splitting: Split the pre-processed dataset into training (e.g., 80%) and testing (e.g., 20%) subsets using
sklearn.model_selection.train_test_split. - Hyperparameter Tuning with Firefly Algorithm:
- Define the objective function as the cross-validation score of the KRR model.
- Implement the Firefly Algorithm to search for the optimal combination of KRR hyperparameters (e.g., the regularization parameter
alphaand the kernel coefficientgamma). The algorithm will iteratively update the population of fireflies (hyperparameter sets) based on their brightness (model performance) [59].
- Model Training:
- Instantiate the
KernelRidgemodel fromsklearn.kernel_ridgewith the optimal hyperparameters found in the previous step. - Train the final KRR model on the entire training set, using only the features selected by RFE.
- Instantiate the
Model Validation and Prospective Prediction Protocol
Objective: To validate model performance and utilize it for predicting the biodistribution of novel nanoparticle formulations.
Materials:
- Software: Python with scikit-learn.
- Data: Held-out test set not used during model training or hyperparameter tuning.
Procedure:
- Model Validation:
- Use the trained KRR model and the selected features to make predictions on the held-out test set.
- Calculate performance metrics, including R² and RMSE, for each output organ (e.g., DEtumor, DEliver) to quantify prediction accuracy.
- Prospective Prediction for Novel Nanoparticles:
- For a new nanoparticle formulation, compile its physicochemical properties (categorical and numerical).
- Subject the new data to the identical pre-processing pipeline as the training data (one-hot encoding, scaling with the pre-fitted scaler).
- Use the fitted RFE selector to extract the same relevant features from the new, pre-processed data.
- Input the selected features into the trained KRR model to obtain the predicted %ID for all target organs.
Visualizations
Workflow: ML-Driven Biodistribution Prediction
Process: Recursive Feature Elimination Logic
The Scientist's Toolkit
Table: Essential Research Reagents and Materials for Nanoparticle Biodistribution Studies
| Item Name | Function/Application |
|---|---|
| Biodegradable Polymers (PLGA, PCL) | Form the core matrix of nanoparticles, enabling drug encapsulation and controlled release [61]. |
| Polyethylene Glycol (PEG) | A common surface coating (PEGylation) to reduce protein adsorption, minimize immune clearance, and prolong systemic circulation [1] [42]. |
| Targeting Ligands (e.g., Antibodies, Peptides) | Conjugated to the nanoparticle surface to actively bind receptors overexpressed on target cells, enhancing site-specific delivery [61]. |
| Fluorescent Dyes (e.g., Cy5.5, DiR) | Encapsulated or conjugated to nanoparticles for in vivo and ex vivo tracking and imaging of biodistribution [61]. |
| Dynamic Light Scattering (DLS) Instrument | Characterizes the hydrodynamic size and size distribution (polydispersity) of nanoparticles in suspension [61]. |
| Zeta Potential Analyzer | Measures the surface charge of nanoparticles, which is critical for predicting colloidal stability and interaction with biological components [42]. |
| Transmission Electron Microscopy (TEM) | Provides high-resolution imaging to confirm nanoparticle size, shape, and core-shell morphology [61]. |
Polyethylene glycol (PEG) has long been the gold standard for imparting "stealth" properties to nanoparticle-based drug delivery systems. By forming a hydrophilic, steric barrier around nanoparticles, PEG reduces opsonization and recognition by the mononuclear phagocyte system (MPS), thereby extending circulation half-life and improving bioavailability [62]. Its efficacy is proven in clinically successful formulations, including PEGylated liposomal doxorubicin (Doxil) and mRNA COVID-19 vaccines [63] [1].
However, the widespread use of PEG has revealed significant limitations, primarily concerning its immunogenicity. The emergence of anti-PEG antibodies in a substantial portion of the population—estimated between 20% and 70%—poses a critical challenge [64]. These antibodies can trigger two major adverse effects: the Accelerated Blood Clearance (ABC) phenomenon upon repeated dosing, and complement activation-related pseudoallergy (CARPA), which can cause hypersensitivity reactions [65] [66] [64]. Furthermore, the dense PEG layer can hinder cellular uptake and endosomal escape, limiting intracellular delivery of therapeutics—a paradox known as the "PEG dilemma" [66].
This application note outlines practical strategies and experimental protocols for developing next-generation stealth nanoparticles using PEG alternatives, framed within the context of optimizing nanoparticle-based drug delivery protocols.
Emerging PEG Alternative Technologies
Research into PEG alternatives focuses on identifying polymers that provide effective stealth properties without eliciting immune responses. The table below summarizes the key characteristics of leading candidates.
Table 1: Comparison of Leading PEG Alternative Polymers for Stealth Coatings
| Polymer Class | Key Representative | Mechanism of Stealth Action | Advantages | Development Status |
|---|---|---|---|---|
| Zwitterionic Polymers | Poly(carboxybetaine) (PCB) | Forms a super-hydrophilic, net-neutral surface via balanced positive and negative charges; creates a strong hydration layer. | Enhanced endosomal escape via membrane interactions; extremely low protein adsorption [63] [66]. | Preclinical validation; shows superior transfection in vivo [63]. |
| Brush-Shaped Polymers | Brush-shaped PEG Methyl Ether Methacrylate (BPL) | High-density, brush-like architecture creates a steric shield that reduces anti-PEG antibody binding [63] [66]. | Maintains PK benefits of PEG while mitigating immunogenicity; suitable for repeated dosing [63]. | Preclinical screening and optimization [63]. |
| Polypeptoids | Polysarcosine (PSar) | Biocompatible, non-ionic, and hydrophilic; mimics PEG's stealth effect using a biodegradable backbone [64]. | Low immunogenicity; biodegradable; does not accumulate in tissues; reduced cytokine secretion [64]. | Phase I clinical trials (e.g., Lubrizol's Apisolex) [64]. |
| Poly(2-oxazoline)s | Poly(2-ethyl-2-oxazoline) (PEtOx) | Tunable hydrophilicity and chain length provide a highly flexible stealth coating [64] [62]. | High modularity; reduced anti-polymer antibody formation; proven efficacy in mRNA delivery [64]. | Preclinical stage; one POx-based formulation in clinical trials for Parkinson's [64]. |
Strategic Framework for PEG Alternative Development
The following diagram illustrates the core decision-making pathway for selecting and developing a PEG alternative strategy, based on the desired therapeutic outcome.
Experimental Protocols for Evaluating PEG Alternatives
This section provides detailed methodologies for formulating and testing nanoparticle systems with alternative stealth coatings.
Protocol: Formulation of Lipid Nanoparticles with Alternative Stealth Lipids
This protocol describes the preparation of LNPs using a microfluidic mixing device, substituting traditional PEG-lipids with alternatives like PCB-lipids or PSar-lipids [63] [67] [66].
3.1.1 Materials and Reagents
Table 2: Essential Reagents for LNP Formulation with PEG Alternatives
| Reagent Category | Specific Examples | Function in Formulation | Recommended Supplier Notes |
|---|---|---|---|
| Ionizable/Cationic Lipid | SM-102, ALC-0315 | Encapsulates nucleic acid payload; promotes endosomal escape. | Critical for mRNA complexation. |
| Phospholipid | DSPC, DOPE | Stabilizes LNP bilayer structure; influences fusogenicity. | Contributes to particle integrity. |
| Cholesterol | Plant-derived Cholesterol | Enhances structural integrity and stability of LNP. | Essential for membrane fluidity. |
| Alternative Stealth Lipid | PCB-lipid, BPL, PSar-VitE, POx-lipid | Provides stealth properties; controls particle size and stability. | Core substitute for PEG-lipid (e.g., DMG-PEG2000). |
| mRNA | CleanCap mRNA | Therapeutic payload. | Purity is critical for efficacy and low reactogenicity. |
| Buffers | Ethanol (for lipid stock), Acetate Buffer (pH 4.0, for mRNA) | Solvent and aqueous phases for microfluidic mixing. | Ensure sterile, nuclease-free conditions. |
3.1.2 Equipment
- Microfluidic mixer (e.g., NanoAssemblr, Precision NanoSystems)
- Syringe pumps and appropriate syringes
- Tubing and connectors
- Dynamic Light Scattering (DLS) instrument for size and PDI measurement
- Zeta potential analyzer
3.1.3 Step-by-Step Procedure
- Prepare Lipid Stock Solution: Dissolve the ionizable lipid, phospholipid, cholesterol, and chosen alternative stealth lipid (e.g., PCB-lipid) in ethanol at a defined molar ratio. A typical molar ratio is 50:10:38.5:1.5 (ionizable lipid:phospholipid:cholesterol:stealth lipid). Filter the solution through a 0.22 µm membrane.
- Prepare mRNA Solution: Dilute the mRNA in an acidic aqueous buffer (e.g., 50 mM acetate buffer, pH 4.0) to a concentration that achieves the desired drug-to-lipid ratio.
- Microfluidic Mixing:
- Load the lipid and mRNA solutions into separate syringes.
- Set the Total Flow Rate (TFR) and Flow Rate Ratio (FRR) on the microfluidic instrument. A common starting point is a TFR of 12 mL/min and an FRR (aqueous:organic) of 3:1.
- Initiate simultaneous pumping to mix the streams in the microfluidic chip, resulting in the instantaneous formation of LNPs.
- Buffer Exchange and Dialysis: Collect the LNP formulation and dialyze against a neutral buffer (e.g., 1X PBS, pH 7.4) for at least 4 hours at 4°C to remove ethanol and adjust the pH.
- Characterization:
- Measure the hydrodynamic diameter, polydispersity index (PDI), and zeta potential using DLS.
- Determine encapsulation efficiency using a RiboGreen assay.
Protocol: In Vitro and In Vivo Assessment of Immunogenicity and Efficacy
This protocol outlines a pipeline for evaluating the performance of novel stealth nanoparticles, focusing on key metrics of immunogenicity and functionality.
3.2.1 In Vitro Transfection Efficiency and Cell Uptake
- Cell Culture: Seed appropriate cell lines (e.g., HEK-293, HeLa) or primary cells in 24-well plates.
- Transfection: Treat cells with LNPs encapsulating a reporter mRNA (e.g., GFP or luciferase). Include a positive control (commercial PEG-LNPs) and a negative control (untreated cells).
- Analysis:
- For GFP mRNA, analyze fluorescence intensity via flow cytometry after 24-48 hours.
- For luciferase mRNA, lyse cells and measure luminescence activity, normalizing to total protein content.
- To quantify cellular uptake, use LNPs loaded with a fluorescent dye and measure internalization via flow cytometry or confocal microscopy.
3.2.2 In Vitro Immunogenicity Profiling
- Human Peripheral Blood Mononuclear Cell (PBMC) Assay: Isolate PBMCs from healthy donors.
- Treatment and Incubation: Incubate PBMCs with various LNP formulations (PEG-LNPs and alternative-stealth LNPs) for 6-24 hours.
- Cytokine Analysis: Collect supernatant and quantify the levels of pro-inflammatory cytokines (e.g., IFN-γ, IL-6, TNF-α) using ELISA or a multiplex bead-based assay. Reduced cytokine secretion from alternative-stealth LNPs indicates lower immunogenicity [64].
3.2.3 In Vivo Repeated Dosing and ABC Phenomenon Study
- Animal Model: Use BALB/c or C57BL/6 mice (n=5-8 per group).
- Dosing Regimen:
- First Dose (Day 0): Administer a low dose of test or control LNPs intravenously.
- Second Dose (Day 7): Administer a second, identical dose.
- Blood Collection and Analysis:
- Collect blood samples at predetermined time points after the second dose.
- Isolate plasma and quantify the concentration of the nanoparticle or its payload to generate pharmacokinetic (PK) profiles. The ABC phenomenon is characterized by significantly accelerated clearance of the second dose in PEGylated systems [65] [66].
- On the final day, collect serum to measure anti-polymer antibody levels (e.g., anti-PEG IgM/IgG) using an enzyme-linked immunosorbent assay (ELISA).
The following diagram outlines the key stages of this evaluation workflow.
The Scientist's Toolkit: Research Reagent Solutions
A curated list of essential materials for researchers developing next-generation stealth nanoparticles is provided below.
Table 3: Essential Research Reagents for Developing PEG-Alternative Nanoparticles
| Reagent / Material | Functional Role | Specific Example(s) | Research Application |
|---|---|---|---|
| PCB-Lipids | Zwitterionic stealth lipid | Custom synthesis based on Luozhong et al. [63] | Enhances endosomal escape and reduces immunogenicity in mRNA LNPs. |
| Brush Polymer Lipids (BPL) | Low-immunogenicity stealth lipid | Poly(ethylene glycol) methyl ether methacrylate (PEGMA) lipids [63] | Reduces anti-PEG antibody binding for repeated administration. |
| Polysarcosine (PSar) Conjugates | Biodegradable stealth polymer | PSar-VitE lipid conjugate [64] | Provides PEG-like stealth with low immunogenicity and biodegradability. |
| Poly(2-oxazoline) (POx) Lipids | Tunable stealth polymer | Poly(2-ethyl-2-oxazoline) lipid conjugate [64] [62] | Offers modular design for fine-tuning LNP surface properties. |
| Ionizable Cationic Lipids | Nucleic acid complexation | SM-102, ALC-0315, SM-86 [66] | Core structural component for encapsulating and stabilizing mRNA. |
| Microfluidic Mixer | Nanoparticle formulation | NanoAssemblr | Enables reproducible, scalable production of LNPs with narrow PDI. |
The movement toward PEG-alternative stealth coatings represents a critical evolution in nanomedicine, driven by the need to mitigate immunogenicity and enable effective repeated dosing. Technologies like zwitterionic PCB-lipids, brush-shaped BPLs, and biodegradable PSar have demonstrated compelling preclinical results, showing comparable or superior performance to PEG while avoiding its immunological pitfalls [63] [64].
Future development will likely focus on combining these novel stealth polymers with active targeting ligands to create truly next-generation "smart" nanoparticles. Furthermore, the integration of machine learning and artificial intelligence in formulation science, as evidenced by the prediction of nanoparticle properties from synthesis parameters, promises to accelerate the optimization of these complex systems [67] [68]. As these alternatives progress through clinical validation, they hold the potential to unlock the full therapeutic promise of RNA therapeutics, gene editing, and targeted drug delivery.
{Application Notes and Protocols}
Optimizing Manufacturing Consistency: Overcoming Batch-to-Batch Variability Through Process Control
In the transition of nanomedicines from laboratory proof-of-concept to clinical and commercial reality, manufacturing consistency presents a formidable challenge. While nanoparticle-based drug delivery systems promise enhanced therapeutic efficacy, this potential is critically undermined by batch-to-batch variability, which affects critical quality attributes (CQAs) such as size, drug loading, and stability [1]. This variability not only complicates the interpretation of preclinical data but also poses a significant barrier to obtaining regulatory approval, as highlighted by the fact that fewer than 0.1% of published nanomedicines achieve clinical translation [1] [69]. This document outlines a structured framework of analytical protocols and process control strategies designed to characterize, monitor, and control nanoparticle manufacturing, thereby ensuring the reproducibility required for successful clinical application.
Quantitative Landscape of Variability and Its Impact
Understanding the sources and impacts of variability is the first step toward its control. The following table summarizes key CQAs and the documented consequences of their inconsistency.
Table 1: Critical Quality Attributes (CQAs) and Consequences of Variability in Nanoparticle Manufacturing
| Critical Quality Attribute (CQA) | Typical Optimal Range/Value | Impact of Variability | Reference |
|---|---|---|---|
| Particle Size & Polydispersity | 40 - 100 nm (dependent on application) | Alters biodistribution, targeting efficiency, and cellular uptake. High polydispersity indicates an unstable process. | [1] [69] |
| Drug Loading Capacity | Varies by system; >10 wt% for carrier systems, >80 wt% for carrier-free | Inconsistent dosing leads to variable therapeutic efficacy and potential toxicity. | [43] |
| Surface Charge (Zeta Potential) | +/- 10 - 30 mV for colloidal stability | Affects particle stability, aggregation propensity, and interaction with biological membranes. | [59] |
| Encapsulation Efficiency | >90% for most therapeutics | Low efficiency wastes costly APIs and complicates purification. Inconsistency indicates poor process control. | [69] |
| Biodistribution (e.g., Liver Accumulation) | NBC* of ~17.56 %ID/g (passive) | High variability in liver/spleen accumulation (as shown in biodistribution studies) leads to unpredictable efficacy and safety profiles. | [40] |
NBC: Nanoparticle Biodistribution Coefficient (% Injected Dose per Gram of tissue).
Core Experimental Protocols for Variability Assessment
Protocol: High-Throughput Nanoparticle Screening and Characterization
Objective: To rapidly and comprehensively characterize key physicochemical properties of nanoparticle formulations during early-stage development and process optimization.
Materials:
- Nano Flow Cytometer: Enables single-particle analysis for size, concentration, and complexity in polydisperse samples [69].
- Dynamic Light Scattering (DLS) Instrument: For ensemble measurements of hydrodynamic size and polydispersity index (PDI).
- Zeta Potential Analyzer: For measuring surface charge.
Methodology:
- Sample Preparation: Dilute nanoparticle suspensions in an appropriate, filtered buffer to prevent multiple scattering artifacts. Perform all measurements in triplicate.
- Single-Particle Analysis (Nano Flow Cytometry):
- Calibrate the instrument using reference beads of known size and concentration.
- Analyze samples to obtain particle-by-particle data on size distribution and concentration.
- For nucleic acid-loaded nanoparticles (e.g., LNPs), use fluorescent dyes to quantify payload copy number per particle and calculate encapsulation efficiency [69].
- Bulk Population Analysis (DLS & Zeta Potential):
- Measure the hydrodynamic diameter and PDI. A PDI value below 0.2 is generally considered monodisperse.
- Measure zeta potential using laser Doppler velocimetry.
Data Analysis: Correlate data from single-particle and bulk techniques. A high PDI from DLS with a broad distribution from nano flow cytometry confirms heterogeneity. Use this multi-modal data to establish a correlation between physicochemical properties and functional performance in subsequent assays.
Protocol: Machine Learning-Guided Prediction of Biodistribution
Objective: To employ computational models for predicting the in vivo behavior of nanoparticles based on their physicochemical properties, reducing reliance on costly and time-consuming animal trials during optimization.
Materials:
- Dataset containing nanoparticle properties (Size, Zeta Potential, Material Type, Shape, etc.) and corresponding organ distribution data (%ID/g) [59].
- Machine learning environment (e.g., Python with scikit-learn).
Methodology:
- Data Curation:
- Collect a dataset with input features (e.g.,
Size,Zeta Potential,MAT(material),Shape) and output parameters (e.g.,DE_tumor,DE_liver) [59]. - Handle missing values using linear interpolation.
- Encode categorical variables (e.g.,
MAT,Shape) using One-Hot Encoding. - Detect and remove outliers using the Z-score method (threshold: 2.5-3 standard deviations).
- Normalize numerical features using MaxAbsScaler.
- Collect a dataset with input features (e.g.,
- Feature Selection:
- Apply Recursive Feature Elimination (RFE) to identify the most critical physicochemical properties influencing biodistribution.
- Model Training and Validation:
- Implement models like Kernel Ridge Regression (KRR), which has demonstrated high efficiency (R² > 0.9 for some organs) in modeling the non-linear relationships in biodistribution data [59].
- Optimize hyperparameters using algorithms like the Firefly Algorithm.
- Validate model performance using k-fold cross-validation, reporting R² and Root Mean Square Error (RMSE).
Data Analysis: Use the trained model to predict the biodistribution of new nanoparticle formulations based solely on their characterized CQAs. This allows for the in silico screening of formulation candidates prior to in vivo testing.
Process Control and Advanced Formulation Strategies
Visualization of an Integrated Workflow for Controlling Batch-to-Batch Variability
The following diagram outlines a holistic workflow, integrating the protocols above with advanced formulation and process control strategies to minimize variability from development through production.
Integrated Workflow for Variability Control
The Scientist's Toolkit: Essential Research Reagents and Materials
A selection of key materials and technologies is critical for executing the protocols and strategies described herein.
Table 2: Key Research Reagent Solutions for Nanoparticle Process Optimization
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Ionizable Lipids | Core component of LNPs for nucleic acid delivery; enables endosomal escape [70]. | Structural variation in lipid libraries impacts efficacy and consistency. A key source of variability. |
| Functional Polymers (e.g., PLGA, PEG) | Forms polymeric nanoparticle matrix for controlled release; PEG coatings provide "stealth" properties [1] [71]. | Batch-to-batch molecular weight and polydispersity of polymers must be controlled. |
| Microfluidic Devices | Provides controlled, continuous-flow mixing for nanoparticle self-assembly, enhancing reproducibility [69]. | Chip geometry and flow rate ratios are Critical Process Parameters (CPPs). |
| Fluorescent Dyes (Nucleic Acid Stains) | Enables quantification of encapsulation efficiency and payload distribution in single-particle analysis [69]. | Must be selected for specificity and minimal interference with formulation. |
| Targeting Ligands (Peptides, Antibodies) | Conjugated to nanoparticle surface for active targeting to specific cells or tissues [43] [70]. | Conjugation efficiency and density are CQAs that require precise monitoring and control. |
Overcoming batch-to-batch variability is not an isolated goal but a fundamental prerequisite for the successful translation of nanoparticle-based therapies. By adopting a systematic framework that integrates robust analytical protocols—such as high-content single-particle analysis and predictive machine learning models—with controlled manufacturing processes like microfluidics, researchers can effectively minimize variability. This application note provides a foundational roadmap for embedding consistency into every stage of the nanomedicine development pipeline, thereby bridging the critical gap between promising laboratory innovation and reliable clinical application.
Assessing Performance, Safety, and Clinical Translation Potential
In nanoparticle-based drug delivery research, achieving optimal protocol efficiency hinges on a multi-faceted characterization strategy. No single technique can fully elucidate the complex physicochemical properties that dictate biological behavior and therapeutic efficacy. This document outlines detailed Application Notes and Protocols for an integrated analytical approach, centering on Dynamic Light Scattering (DLS) and Atomic Force Microscopy (AFM), while incorporating advanced computational and single-particle methods. This framework is designed to provide researchers with a comprehensive toolkit for robust nanoparticle optimization, ensuring batch-to-batch consistency, predictive modeling of performance, and successful translation of nanomedicines.
Core Technique Principles and Comparisons
Dynamic Light Scattering (DLS)
Principle: DLS measures the temporal fluctuations in the intensity of laser light scattered by nanoparticles undergoing Brownian motion in a solvent [72]. Analysis of these fluctuations via an autocorrelation function allows for the determination of the diffusion coefficient, which is subsequently converted into the hydrodynamic radius ((rh)) using the Stokes-Einstein equation [72]: [ D = \frac{kB T}{6 \pi \eta rh} ] where (D) is the diffusion coefficient, (kB) is the Boltzmann constant, (T) is the temperature, and (\eta) is the solvent viscosity [72].
Key Considerations: DLS is highly sensitive to large particles and aggregates due to the scattering intensity's dependence on the sixth power of the particle diameter [72]. It is most accurate for monodisperse, spherical particles in dilute solutions. For polydisperse samples, algorithms like CONTIN are used to fit complex decays in the autocorrelation function [72].
Atomic Force Microscopy (AFM)
Principle: AFM uses a sharp probe mounted on a flexible cantilever to scan surfaces with nanometer-scale resolution [73] [74]. The interaction forces between the tip and the sample surface cause cantilever deflections, typically detected via a laser beam and photodetector system, to generate topographical maps [74]. A key advantage is its ability to operate in various environments, including liquid, enabling the imaging of biological samples under near-physiological conditions without complex preparation [73] [74].
Key Modes:
- Contact Mode: The probe remains in constant contact with the surface. Best for hard, stable surfaces but can be invasive for soft samples [74] [75].
- Tapping Mode: The cantilever oscillates and gently "taps" the surface, minimizing lateral forces and sample damage. Ideal for soft polymers and biological tissues [74].
- PeakForce QNM: An advanced mode that quantitatively maps mechanical properties like Young's modulus and adhesion at nanoscale resolution by controlling and measuring the maximum force applied in each tapping cycle [74].
Complementary Analytical Techniques
No single technique provides a complete picture. The following table summarizes key complementary methods.
Table 1: Overview of Complementary Nanoparticle Characterization Techniques
| Technique | Measured Parameters | Key Strengths | Key Limitations |
|---|---|---|---|
| Multi-Angle Light Scattering (MALS) | Absolute molecular weight, radius of gyration [72] | Coupled with SEC, provides accurate molecular weight without shape assumption [72] | Requires sophisticated instrumentation and data analysis |
| Nanoparticle Tracking Analysis (NTA) | Particle size distribution, concentration | Direct visualization and counting of particles; good for polydisperse samples [76] | Lower resolution compared to DLS for monodisperse samples; operator-dependent |
| Single-Molecule / Particle Analysis (e.g., Mass Photometry) | Molecular mass, heterogeneity, coating efficiency [76] | Reveals population heterogeneity obscured by ensemble-average techniques [76] | Emerging technology; may have limited analyte scope or require specific sample conditions |
| Transmission Electron Microscopy (TEM) | Core size, morphology, internal structure | Atomic-level resolution; direct imaging [77] | Requires vacuum and complex sample preparation; no native state information |
The following diagram illustrates the logical workflow for integrating these techniques to fully characterize a nanoparticle formulation, from initial screening to advanced analysis.
Experimental Protocols
Protocol 1: DLS for Hydrodynamic Size and Stability Assessment
Objective: To determine the hydrodynamic size, size distribution, and colloidal stability of nanoparticle formulations in suspension.
Materials:
- Nanoparticle suspension (e.g., PLGA, lipid NPs, polymeric micelles)
- Appropriate solvent or buffer (e.g., PBS, purified water)
- Disposable cuvettes (low-volume, disposable sizing cuvettes recommended)
- DLS instrument (e.g., Malvern Zetasizer, Wyatt DynaPro)
Procedure:
- Sample Preparation:
- Dilute the nanoparticle stock suspension in a suitable buffer to a concentration that avoids multiple scattering effects (typically a count rate within the instrument's recommended range). Note: Over-dilution can lead to weak signals, while under-dilution can cause artifacts [72].
- Filter the diluted sample through a 0.1 µm or 0.22 µm syringe filter to remove dust and large aggregates, if compatible with the sample.
- Gently pipette the sample into a clean, disposable cuvette, avoiding the introduction of air bubbles.
- Instrument Setup:
- Equilibrate the sample in the instrument chamber at the desired measurement temperature (e.g., 25°C) for 2-5 minutes.
- Set the scattering angle (commonly 90° or 173°), laser wavelength, and solvent viscosity/refractive index parameters as per the instrument software.
- Data Acquisition:
- Perform a minimum of 3-12 sequential measurements per sample, with each run duration of 10-60 seconds.
- Record the intensity-based size distribution, polydispersity index (PdI), and the autocorrelation function for each measurement.
- Data Analysis:
- Examine the autocorrelation function for a smooth, single exponential decay. Poor quality data may indicate sample contamination, aggregation, or inappropriate concentration.
- Report the Z-average diameter (the intensity-weighted mean hydrodynamic size) and the PdI (a measure of distribution breadth). A PdI < 0.1 is considered monodisperse, while >0.3 indicates high polydispersity.
- For stability studies, repeat measurements over time (e.g., 0, 1, 7, 30 days) under storage conditions.
Protocol 2: AFM for Topographical and Mechanical Characterization
Objective: To obtain high-resolution, three-dimensional topographical images and nanomechanical properties of nanoparticles deposited on a solid substrate.
Materials:
- Nanoparticle suspension
- Atomically flat substrate (e.g., freshly cleaved mica, silicon wafer)
- AFM instrument with Tapping Mode and PeakForce QNM capability (e.g., Bruker Dimension Icon)
- AFM probes (e.g., RTESPA-300 for Tapping Mode in air, SNL for PeakForce QNM in liquid)
Procedure:
- Sample Preparation:
- For imaging in air: Dilute the nanoparticle suspension to a low concentration (e.g., 5-20 µg/mL). Deposit a 10-20 µL droplet onto a freshly cleaved mica surface. Allow to adsorb for 2-5 minutes, then gently rinse with ultrapure water to remove unbound particles and salts. Blot the edges and air-dry completely [73] [74].
- For imaging in liquid: Dilute the sample in the desired buffer. Place a 30-50 µL droplet on the mica substrate and immediately mount it in the AFM liquid cell. This preserves the native state of soft nanoparticles and biomolecules.
- Instrument Setup:
- Mount the appropriate AFM probe and align the laser on the cantilever.
- Engage the probe onto the substrate in a particle-free area to find the surface.
- Data Acquisition - Tapping Mode:
- Set the drive frequency and amplitude. Adjust the setpoint to achieve stable, low-force imaging.
- Scan areas of varying sizes (e.g., 10x10 µm down to 500x500 nm) to locate well-dispersed nanoparticles.
- Collect height, amplitude, and phase images.
- Data Acquisition - PeakForce QNM:
- This mode requires prior calibration of the probe's spring constant and deflection sensitivity.
- Set the PeakForce frequency and amplitude. The system will automatically control the maximum force.
- Simultaneously capture height, Young's modulus (DMT modulus), adhesion, and deformation maps.
- Data Analysis:
- Use the AFM software to perform plane fitting and flattening on the height images.
- Measure particle height (more accurate than lateral diameter due to tip convolution effects) and perform statistical analysis on a population of >100 particles.
- Analyze the Young's modulus maps to assess the mechanical homogeneity of the nanoparticle formulation.
Data Integration and Computational Advancements
Machine Learning in Characterization
Machine learning (ML) is transforming nanoparticle characterization by enabling the analysis of complex, non-linear relationships in formulation data.
Table 2: Machine Learning Applications in Nanoparticle Characterization and Optimization
| Application Area | ML Model | Function | Demonstrated Performance |
|---|---|---|---|
| DLS Enhancement | Deep Neural Networks (DNN) [78] | Accurate particle sizing from raw scattering signals, even in complex media with large particles. | Sub-1% precision for particles up to 153 µm [78]. |
| Formulation Prediction | Random Forest [67] | Predicts Encapsulation Efficiency (EE) and Drug Loading (DL) of PLGA NPs based on formulation parameters. | R² of 0.96 for EE and 0.93 for DL prediction [67]. |
| Rational Nanocarrier Design | Molecular Dynamics (MD) Simulations [41] | Provides atomic-to-mesoscale insights into NP interactions with biological membranes, informing optimal size, charge, and composition. | Predicts cellular uptake, stability, and drug loading efficiency in silico [41]. |
The workflow for applying machine learning, particularly for formulation prediction, involves data curation, model training, and experimental validation.
Addressing Ensemble Averaging Limitations with Single-Particle Techniques
Traditional techniques like DLS provide ensemble-average data, which can mask population heterogeneity. Emerging single-molecule/particle technologies (e.g., mass photometry) are critical for quantifying coating efficiency (the ratio of ligand-coated to uncoated nanoparticles) and payload distribution (the variation in drug content per particle), parameters that are crucial for batch consistency and therapeutic efficacy but invisible to bulk analysis [76]. Integrating these advanced methods provides a deeper, more accurate understanding of nanoparticle product quality.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoparticle Characterization
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Standard Cuvettes | Housing samples for DLS measurements. | Disposable polystyrene cuvettes; low-volume for precious samples. |
| Ultrafiltration Devices | Buffer exchange, desalting, and concentration of nanoparticle suspensions prior to characterization. | Amicon Ultra centrifugal filters (various MWCO). |
| Freshly Cleaved Mica | An atomically flat, negatively charged substrate for AFM sample preparation. | Essential for high-resolution imaging of adsorbed nanoparticles. |
| AFM Probes | The sensing element for AFM, defining resolution and mode capability. | RTESPA-300 for air imaging; SNL or SCANASYST-FLUID for liquid and mechanical mapping. |
| Size Standards | Calibration and validation of DLS and NTA instruments. | Polystyrene or silica nanospheres of known diameter. |
| Microfluidic Chips | For reproducible preparation of nanoparticles with controlled size and PDI [67]. | Used in conjunction with syringe pumps for controlled fluid dynamics. |
A strategic and integrated characterization protocol is non-negotiable for the rational optimization of nanoparticle-based drug delivery systems. By combining the solution-based hydrodynamic profiling of DLS with the high-resolution, single-particle capabilities of AFM, and supplementing with advanced tools like MALS and single-particle analysis, researchers can build a comprehensive understanding of their formulations. The increasing integration of machine learning and computational modeling offers a powerful path toward predictive design, reducing reliance on empirical methods. Adhering to these detailed application notes and protocols will enhance the reproducibility, efficacy, and translation potential of next-generation nanomedicines.
The transition of nanoparticle-based drug delivery systems (DDS) from laboratory research to clinical application is hampered by a significant translational gap. While thousands of nanomedicines are published preclinically, only an estimated 50–80 have gained global clinical approval by 2025, representing a conversion rate of less than 0.1% from research output to clinical products [1]. This gap often stems from a poor understanding of how a nanoparticle's physicochemical properties influence its biological behavior and therapeutic efficacy in vivo [1] [52]. Establishing a robust In Vitro-In Vivo Correlation (IVIVC) is therefore critical for rational nanocarrier design. It enables researchers to use predictive in vitro models to forecast in vivo performance, thereby optimizing formulations, reducing reliance on animal studies, and accelerating clinical translation [79]. This Application Note details the key physicochemical properties affecting biological outcomes and provides standardized protocols for bridging this critical divide.
Core Principles: Linking Nanoparticle Properties to Biological Performance
The biological journey and efficacy of a nanoparticle are dictated by its intrinsic physicochemical characteristics. Understanding these relationships is the first step in rational design.
Table 1: Impact of Key Physicochemical Properties on Biological Outcomes
| Physicochemical Property | Impact on Biological Behavior | Key Biological Outcomes |
|---|---|---|
| Size [80] [81] | Influences cellular uptake, biodistribution, and MPS clearance. | - <100 nm: Enhanced tissue penetration and cellular internalization [81].- >100 nm: Primarily cleared by the spleen and liver MPS [80]. |
| Surface Charge [80] [81] | Determines protein corona composition, immune cell interaction, and cytotoxicity. | - Cationic: Potentiates both M1 and M2 macrophage markers; higher cytotoxicity risk [81] [80].- Anionic: Promotes M1-to-M2 macrophage polarization [81].- Neutral: Minimizes opsonization and MPS uptake, prolonging circulation. |
| Lipid Composition & Solid State [80] | Affects drug loading capacity, release kinetics, and storage stability. | - SLNs: Ordered crystals can lead to drug expulsion.- NLCs: Amorphous blends offer higher loading capacity.- SLPs: Chaotic mixes maximize loading and stability. |
| Surface Functionalization [1] [52] | Modulates stealth properties, targeting, and immune activation. | - PEGylation: Reduces opsonization, prolongs circulation, but may cause immunogenicity [1].- Targeting Ligands (e.g., antibodies): Enables active targeting to specific cells [82] [52]. |
The formation of a protein corona is a critical event at the nano-bio interface. Upon entering a biological fluid, nanoparticles are rapidly coated with proteins, which creates a new biological identity that dictates subsequent interactions with immune cells, such as macrophages [81]. As shown in Table 1, surface charge directly influences the protein corona's composition, which in turn drives specific macrophage polarization programs (e.g., toward pro-inflammatory M1 or anti-inflammatory M2 phenotypes) [81]. This makes understanding and controlling the protein corona essential for predicting in vivo behavior from in vitro assays.
Experimental Protocols for IVIVC
Protocol 1: In Vitro Drug Release Profiling
Objective: To simulate and characterize the drug release kinetics of nano-formulations under physiological conditions.
Materials:
- Nanoparticle formulation
- Dialysis membrane (appropriate molecular weight cutoff)
- Release media (e.g., PBS at pH 7.4, simulated gastric/intestinal fluid)
- Franz diffusion cell or similar apparatus
- HPLC system for drug quantification
Methodology:
- Dialysis Method: Place a known volume of nanoparticle suspension into a dialysis bag and seal it [79].
- Immersion: Immerse the dialysis bag in a reservoir containing the release medium maintained at 37°C under continuous agitation.
- Sampling: At predetermined time intervals, withdraw aliquots from the external release medium and replace with an equal volume of fresh medium to maintain sink conditions.
- Analysis: Quantify the drug concentration in the samples using a validated analytical method (e.g., HPLC).
- Data Modeling: Fit the release data to kinetic models (e.g., zero-order, first-order, Higuchi) to determine the release mechanism.
Notes: For a more predictive model, consider using a dissolution-permeation (D/P) setup like the µFlux system, which incorporates a membrane to better simulate absorption and can provide a stronger IVIVC [83].
Protocol 2: Evaluating Protein Corona Formation and Macrophage Polarization
Objective: To analyze how nanoparticle physicochemical properties affect protein corona formation and subsequent immune responses.
Materials:
- Nanoparticles of varying size and surface charge
- Bone-marrow-derived macrophages (BMDMs) or Raw 264.7 cell line
- Fetal Bovine Serum (FBS)
- Cell culture reagents (M-CSF, IFN-γ+LPS for M1 polarization, IL-4 for M2 polarization)
- qPCR reagents, flow cytometry antibodies (e.g., for CD38, MHCII, CD163, CD206)
- Cytokine array (e.g., Mouse Cytokine Proinflammatory Focused 10-Plex Array)
Methodology:
- Corona Formation: Incubate nanoparticles in 100% FBS for 1 hour at 37°C. Isolate the corona-nanoparticle complexes via centrifugation [81].
- Proteomic Analysis: Digest the corona proteins and identify them using liquid chromatography-mass spectrometry (LC-MS/MS) [81].
- Macrophage Treatment: Differentiate BMDMs to M0, M1, and M2 phenotypes. Treat these macrophages with corona-coated nanoparticles for 24-72 hours.
- Phenotype Assessment:
- Gene Expression: Analyze polarization markers via qPCR (e.g., Cxcl11, Nos2 for M1; Arg1, CD206 for M2) [81].
- Surface Markers: Use flow cytometry to quantify M1 (MHCII+/CD38+) and M2 (CD206+/CD163+) populations [81].
- Cytokine Secretion: Profile pro- and anti-inflammatory cytokines in the supernatant using a multiplex cytokine array [81].
Protocol 3: Computational Prediction of Nanoparticle Behavior
Objective: To use in silico models to predict nanoparticle stability, membrane interactions, and optimal formulations prior to experimental work.
Materials:
- High-performance computing (HPC) resources
- MD simulation software (e.g., GROMACS, AMBER, CHARMM)
- Starting structures of nanoparticles and lipid membranes
Methodology:
- System Setup:
- All-Atom MD (AAMD): For high-resolution insights, use atomic-level detail of the nanoparticle and a patch of lipid membrane.
- Coarse-Grained MD (CGMD): For larger systems and longer timescales, group atoms into "beads" using a force field like Martini [41].
- Simulation: Run the simulation in a solvated box with ions, minimizing energy and equilibrating before the production run.
- Analysis: Analyze trajectories to determine:
- Stability: Root-mean-square deviation (RMSD) of the nanoparticle.
- Membrane Interaction: Embedding depth and lipid rearrangement.
- Cellular Uptake: Energetics of membrane translocation [41].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents for Nanoparticle IVIVC Studies
| Reagent / Material | Function / Application |
|---|---|
| Polyethylene Glycol (PEG) [1] [52] | Surface coating to provide "stealth" properties, reduce opsonization, and prolong systemic circulation. |
| Ionizable Lipids [1] [80] | Critical component of LNPs for nucleic acid delivery; enables efficient encapsulation and endosomal release. |
| M-CSF (Macrophage Colony-Stimulating Factor) [81] | Differentiates bone marrow progenitors into M0 macrophages for in vitro immunology studies. |
| Dialysis Membranes [79] | Standard tool for in vitro drug release studies by separating nanoparticles from the release medium. |
| Polystyrene Nanoparticles (Model) [81] | Well-characterized, commercially available particles with uniform size/charge for controlled studies of nano-bio interactions. |
| Poly(lactic-co-glycolic acid) (PLGA) [1] [52] | Biodegradable polymer for creating nanoparticles with sustained, controlled drug release profiles. |
| Click Chemistry Reagents [82] | Enables precise, metal-free conjugation of targeting ligands (e.g., antibodies) to nanoparticles while preserving functionality. |
Workflow and Pathway Visualizations
Integrated IVIVC Workflow for Nanoparticle Optimization
NP Properties Drive Macrophage Fate via Protein Corona
Nanoparticles (NPs) are revolutionizing drug delivery by enhancing therapeutic efficacy and reducing side effects. They are broadly categorized into hard nanoparticles, typically inorganic materials like iron oxide and mesoporous silica, and soft nanoparticles, which include organic, lipid-based, and polymeric structures such as liposomes, niosomes, and dendrimers [84] [85]. The distinct physicochemical properties of these two classes make them uniquely suited for different therapeutic applications. Hard NPs often excel in diagnostic applications and stimuli-responsive delivery, while soft NPs are frequently superior in drug encapsulation, biocompatibility, and navigating biological barriers [86] [87]. This analysis provides a structured comparison of hard and soft nanoparticle platforms, detailing their properties, applications, and optimized protocols for researchers in drug development.
Comparative Analysis of Physicochemical Properties
The intrinsic properties of nanoparticles directly influence their biological behavior, including cellular uptake, biodistribution, and safety profiles. The table below summarizes the key characteristics of hard and soft nanoparticles.
Table 1: Comparative Physicochemical Properties of Hard vs. Soft Nanoparticles
| Property | Hard Nanoparticles | Soft Nanoparticles |
|---|---|---|
| Typical Materials | Iron oxide (IONPs), mesoporous silica, gold, quantum dots [84] [87] [85] | Niosomes, liposomes, dendrimers, polymeric micelles, nanogels [84] [86] [85] |
| Structural Rigidity | High mechanical strength, fixed shape [84] [85] | Low mechanical strength, deformable [86] [85] |
| Common Sizes | 10-100 nm [87] | 10-1000 nm, with many in the 50-200 nm range [84] [71] |
| Surface Charge (ζ-Potential) | Can be modulated; e.g., commercial coated ferrofluid used as a benchmark [84] | Easily modified; e.g., chitosan coating shifted ζ-potential to positive values [84] |
| Drug Loading Mechanism | Surface adsorption/attachment, pore encapsulation [87] | Core encapsulation, chemical conjugation, electrostatic/hydrophobic interactions [86] [71] |
| Key Distinguishing Feature | Unique magnetic, optoelectrical properties [85] | High biocompatibility, biomimetic nature [86] |
Therapeutic Application Platforms
The choice between hard and soft nanoparticles is application-dependent. Key therapeutic areas leverage the distinct advantages of each platform.
Table 2: Targeted Therapeutic Applications of Hard and Soft Nanoparticles
| Therapeutic Application | Hard Nanoparticle Platform | Soft Nanoparticle Platform |
|---|---|---|
| Oncology (Drug Delivery) | Mesoporous silica for chemotherapeutics (e.g., Chlorambucil-functionalized MSNs) [88] [87] | Dendrimers for drugs like doxorubicin and tamoxifen; Niosomes for calcein delivery [84] [86] |
| Oncology (Targeting & Diagnostics) | Iron Oxide NPs (IONPs) for magnetic targeting and hyperthermia; Cellular internalization confirmed by magnetic cell separation [84] [87] | Ligand-conjugated NPs (e.g., with peptides, antibodies) for active targeting [86] |
| Neurological Disorders | Metal and carbon-based NPs for crossing the Blood-Brain Barrier (BBB) [49] [89] | Lipid nanoparticles (LNPs), polymeric NPs for intranasal delivery via olfactory/trigeminal pathways [49] |
| Anti-inflammatory & Antibacterial | Silver nanoparticles for antimicrobial activity [89] | Chitosan-coated lipid vesicles for diclofenac; Albumin nanoparticles for clarithromycin [88] |
| Stimuli-Responsive Release | Response to magnetic fields, light [87] [85] | Response to pH, enzymes, temperature [86] [85] |
Experimental Protocols for Key Evaluations
Protocol: Formulation and Characterization of Chitosan-Modified Soft Nanoparticles (Niosomes)
This protocol is adapted from a study that used chitosan coating to enhance the cellular uptake of niosomes [84].
1. Principle: Chitosan, a biocompatible and mucoadhesive polymer, is coated onto the surface of niosomes to shift the surface charge to positive values, thereby improving interaction with negatively charged cell membranes.
2. Research Reagent Solutions:
- Lipid Component: A mixture of non-ionic surfactants (e.g., Span 60) and cholesterol.
- Aqueous Phase: Phosphate Buffered Saline (PBS) or deionized water.
- Chitosan Solution: Chitosan dissolved in a mild acidic aqueous solution (e.g., 1% v/v acetic acid).
- Drug Payload: Hydrophilic drug (e.g., Calcein) dissolved in the aqueous phase.
3. Step-by-Step Methodology: 1. Niosome Formation: The lipid components are dissolved in an organic solvent and evaporated under reduced pressure to form a thin film. The film is then hydrated with the aqueous phase containing the drug payload, above the phase transition temperature of the lipids. The resulting suspension is extruded through polycarbonate membranes of defined pore size (e.g., 200 nm) to achieve a uniform size distribution. 2. Chitosan Coating: The chitosan solution is added dropwise to the prepared niosome suspension under constant magnetic stirring. The reaction is allowed to proceed for a predetermined time (e.g., 60 minutes) at room temperature. 3. Purification: Unencapsulated drug and free chitosan are removed via dialysis or centrifugal filtration.
4. Characterization: * Size and ζ-Potential: Determine the hydrodynamic diameter and ζ-potential via Dynamic Light Scattering (DLS). A successful coating is indicated by an increase in particle size and a shift of ζ-potential to positive values, comparable to established standards [84]. * Morphology: Analyze nanoscale topography using Atomic Force Microscopy (AFM) to confirm the presence of the coating and particle integrity [84].
Protocol: Cellular Uptake and Cytotoxicity Profiling
This protocol outlines a standard method for evaluating the biological performance of nanoparticles, applicable to both hard and soft variants [84].
1. Principle: This assay determines the safety (cytotoxicity) and efficiency (cellular uptake) of nanoparticle formulations on relevant cell lines (e.g., Calu-3 lung adenocarcinoma cells).
2. Research Reagent Solutions:
- Cell Culture Medium: Appropriate medium (e.g., DMEM) supplemented with fetal bovine serum (FBS) and antibiotics.
- Viability Stain: MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) or similar.
- Fluorescent Tracer: For uptake studies, nanoparticles are loaded with a fluorescent marker like Calcein (for soft NPs) or a dye suitable for IONPs [84].
3. Step-by-Step Methodology: 1. Cell Seeding: Seed cells in multi-well plates at a standardized density and allow them to adhere for 24 hours. 2. NP Treatment: Expose cells to a concentration gradient of the nanoparticle formulation. Include a negative control (medium only) and a positive control for cytotoxicity. 3. Incubation: Incubate for 24-72 hours. 4. Viability Assay: Add MTT reagent to the wells and incubate. Metabolically active cells will reduce MTT to purple formazan crystals. Solubilize the crystals and measure the absorbance using a microplate reader. Cytotoxicity is calculated relative to the untreated control. 5. Uptake Confirmation: * For IONPs: Perform magnetic cell separation after treatment to physically isolate cells that have internalized the magnetic nanoparticles [84]. * For Fluorescent-Labeled Niosomes: Visualize intracellular localization using confocal microscopy [84].
4. Data Analysis: The half-maximal inhibitory concentration (IC₅₀) can be calculated from the dose-response data. Cellular uptake is qualitatively and quantitatively assessed via microscopy and separation efficiency.
Visualization of Workflows and Interactions
NP Targeting Mechanisms
Nano-Bio Interface & Cargo Release
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Nanoparticle Formulation and Evaluation
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| Chitosan | A biocompatible polymer used to coat nanoparticles, imparting a positive surface charge to enhance interaction with cell membranes [84]. | Coating niosomes to shift ζ-potential to positive values [84]. |
| Polyethylene Glycol (PEG) | A polymer used for "PEGylation" to create a stealth coating, reducing opsonization and extending systemic circulation time [49]. | Modifying lipid nanoparticles (LNPs) for mRNA delivery to reduce immune recognition [88]. |
| Polyamidoamine (PAMAM) Dendrimer | A highly branched, soft nanoparticle with a polar core and shell, used for encapsulating or conjugating drugs [86]. | Delivery of chemotherapeutics like doxorubicin and tamoxifen [86]. |
| Calu-3 Cell Line | A human lung adenocarcinoma cell line used as an in vitro model for evaluating cytotoxicity and cellular uptake of nanoparticles [84]. | Testing biocompatibility of niosomes and IONPs [84]. |
| Dynamic Light Scattering (DLS) | An analytical technique used to determine the hydrodynamic diameter and size distribution of nanoparticles in suspension [84]. | Standard characterization of nanoparticle size post-formulation [84] [88]. |
| Atomic Force Microscopy (AFM) | A high-resolution technique used to assess the nanoscale topography and morphology of nanoparticles, complementing DLS data [84]. | Visualizing the surface structure of both soft niosomes and hard IONPs [84]. |
Within the framework of nanoparticle-based drug delivery protocol optimization research, the rigorous assessment of safety and biocompatibility is a critical gatekeeper for clinical translation. Biocompatibility refers to the ability of a material to perform with an appropriate host response in a specific application, a requirement for all medical devices and drug products that contact the human body [90]. For nanoparticle (NP) formulations, this evaluation is paramount, as their unique physicochemical properties can elicit biological responses distinct from those of conventional biologics or small-molecule drugs [91] [92].
This document outlines detailed application notes and protocols for two cornerstone assessments: cytotoxicity profiling, which identifies the potential for cell death or damage, and immunological response evaluation, which probes the interaction of NPs with the complex immune system. Adherence to international standards, such as the ISO 10993 series, is essential for regulatory approval by bodies like the U.S. Food and Drug Administration (FDA) and for ensuring patient safety [90] [93]. These evaluations are not merely safety checkboxes; they provide critical data that can feed back into the rational design of safer, more effective nano-drug delivery systems, ultimately optimizing their therapeutic profile [92] [94].
Cytotoxicity Profiling
Cytotoxicity testing is a fundamental first step in biocompatibility assessment, classified among the "Big Three" essential tests for nearly all medical devices and materials in contact with the body [93]. Its purpose is to determine if a nanoparticle formulation or its extractable substances cause damage to living cells, providing an initial screen for acute toxicity.
Key Principles and Regulatory Framework
Cytotoxicity evaluation for medical devices and nanomaterials is guided by ISO 10993-5:2009, "Biological evaluation of medical devices — Part 5: Tests for in vitro cytotoxicity" [93]. The standard outlines three primary test types: extract tests, where devices are incubated with a solvent to create an extract for cell culture exposure; direct contact tests; and indirect contact tests [95]. Testing is typically performed on mammalian cell lines, such as L-929 mouse fibroblasts or Balb 3T3 cells, which are cultured and exposed to the test material or its extracts for a defined period, often 24 hours [95] [93]. The primary endpoints assessed include cell viability, morphological changes, cell detachment, and cell lysis [93]. According to ISO guidance, cell viability at or above 70% is generally considered a positive sign of non-cytotoxicity, especially when testing a neat (undiluted) extract [93].
Detailed Experimental Protocol: MTT Assay for Nanoparticle Cytotoxicity
The MTT assay is a widely used, standardized colorimetric method for quantifying cell viability and metabolic activity [95] [93]. The following protocol is adapted for evaluating nanoparticle suspensions.
Principle: Viable cells with active metabolism reduce the yellow, water-soluble tetrazolium salt MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide) to purple, water-insoluble formazan crystals. The amount of formazan produced is proportional to the number of viable cells and is quantified by spectrophotometry after dissolving the crystals [95].
Materials and Reagents:
- Cell Line: L-929 mouse fibroblast cells (or other relevant cell lines, e.g., HepG2 for liver toxicity models) [95] [96].
- Growth Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and 1% penicillin/streptomycin.
- Test Material: Sterile nanoparticle suspension at the desired concentration.
- Extraction Vehicle: Appropriate solvent (e.g., physiological saline, cell culture medium) for preparing nanoparticle extracts if required.
- MTT Reagent: 5 mg/mL MTT in phosphate-buffered saline (PBS).
- Solubilization Solution: Acidified isopropanol or Dimethyl Sulfoxide (DMSO).
- Equipment: CO2 incubator, biological safety cabinet, centrifuge, microplate reader, 96-well cell culture plates.
Procedure:
- Cell Seeding: Harvest and count a logarithmically growing L-929 cell culture. Seed a 96-well plate at a density of 1 x 10^4 cells per well in 100 µL of complete growth medium. Incubate the plate at 37°C with 5% CO2 for 24 hours to allow for cell attachment.
- Sample Preparation (Extract or Direct Exposure):
- Extract Method: Incubate the nanoparticle sample with extraction medium (e.g., serum-free DMEM) at a prescribed surface-area-to-volume ratio (e.g., 3 cm²/mL) or weight-to-volume ratio (e.g., 0.1 g/mL) for 24 ± 2 hours at 37°C. Filter the extract through a 0.22 µm filter to ensure sterility [93].
- Direct Exposure Method: Prepare a series of dilutions of the sterile nanoparticle suspension in complete growth medium.
- Exposure: After the 24-hour cell attachment period, carefully aspirate the medium from the 96-well plate. Add 100 µL of the nanoparticle extracts or dilution series to the test wells. Include control wells: Negative control (cells with fresh medium only) and Positive control (cells with a known cytotoxic agent, e.g., 1% phenol). Incubate the plate for 24 ± 2 hours at 37°C with 5% CO2.
- MTT Incubation: After exposure, carefully aspirate the treatment medium from all wells. Add 50 µL of serum-free medium and 50 µL of MTT reagent (5 mg/mL) to each well. Incubate the plate for 2-4 hours at 37°C.
- Solubilization: Carefully remove the MTT-containing medium without disturbing the formed formazan crystals. Add 150 µL of solubilization solution (e.g., DMSO) to each well. Gently shake the plate on an orbital shaker for 15 minutes to fully dissolve the formazan crystals.
- Absorbance Measurement: Measure the absorbance of each well at a wavelength of 570 nm, using a microplate reader. A reference wavelength of 630-690 nm may be used for background subtraction.
Data Analysis and Interpretation:
- Calculate the average absorbance for the negative control group (Acontrol), positive control group (Apositive), and each test sample group (A_sample).
- Calculate the percentage of cell viability for each test sample using the formula:
Cell Viability (%) = (A_sample / A_control) × 100% - A cell viability of ≥ 70% for the neat extract or the highest concentration tested is typically considered indicative of a non-cytotoxic response, in line with ISO 10993-5 guidance [93]. The results can be further analyzed to determine the half-maximal inhibitory concentration (IC50) if a dilution series is tested [96].
The table below summarizes common assays used for cytotoxicity assessment, providing a comparison for researchers.
Table 1: Common In Vitro Cytotoxicity Assays
| Assay Name | Detection Principle | Primary Readout | Key Advantages |
|---|---|---|---|
| MTT Assay [95] [93] | Metabolic activity (mitochondrial dehydrogenase) | Colorimetric (Absorbance) | Cost-effective, well-established, high-throughput |
| Neutral Red Uptake (NRU) [93] | Membrane integrity & lysosomal function | Colorimetric (Absorbance) | Simple protocol, directly measures viable cell capacity |
| ATP Assay [95] | Cellular ATP content (viability marker) | Luminescent (RLU) | Highly sensitive, rapid signal loss upon cell death |
| Flow Cytometry with Viability Dyes [95] | Membrane integrity | Fluorescence | Distinguishes live, apoptotic, and necrotic cell populations |
| Dye Exclusion (Trypan Blue) [95] | Membrane integrity | Microscopic cell count | Simple, direct counting of live vs. dead cells |
Workflow for the MTT cytotoxicity assay protocol.
Immunological Response Evaluation
Beyond general cytotoxicity, nanoparticles must be evaluated for their specific interactions with the immune system, a field known as immunomodulation [91]. This involves assessing whether a NP stimulates, suppresses, or otherwise modulates immune responses. Given that NPs are frequently recognized by the immune system as foreign, they can trigger inflammatory responses, be rapidly cleared by phagocytic cells, or, if strategically designed, be used to beneficially modulate the immune system to fight diseases like cancer [91] [97].
Key Principles and Assay Targets
The immune system is a complex network of cells and soluble factors. Key evaluation targets for NPs include:
- Cytokine Secretion Profile: The release of signaling proteins like Tumor Necrosis Factor-alpha (TNF-α), interleukins (IL-1β, IL-6, IL-10), and interferons (IFN-γ) is a primary indicator of immune activation (pro-inflammatory) or suppression (anti-inflammatory) [91].
- Immune Cell Phenotyping: Using flow cytometry to identify changes in the surface markers and relative proportions of immune cell populations (e.g., macrophages, dendritic cells, T cells) after NP exposure.
- Complement Activation: Assessing whether NPs activate the complement system, a cascade of plasma proteins that can trigger inflammation and opsonization [91].
- Hemocompatibility: Evaluating the impact of NPs on blood components, including red blood cells (hemolysis), platelets, and coagulation factors, is critical for intravenously administered formulations [93].
Detailed Experimental Protocol: Cytokine Release Assay Using ELISA
The Enzyme-Linked Immunosorbent Assay (ELISA) is a standard method for quantifying specific cytokines in cell culture supernatants.
Principle: A sandwich ELISA uses a capture antibody coated on a plate to bind the cytokine of interest from the sample. A detection antibody, conjugated to an enzyme (e.g., Horseradish Peroxidase, HRP), is then added. After adding a substrate, the enzyme catalyzes a color change reaction, the intensity of which is proportional to the cytokine concentration.
Materials and Reagents:
- Immune Cells: Primary human peripheral blood mononuclear cells (PBMCs) or macrophage-like cell lines (e.g., THP-1, RAW 264.7).
- Stimuli: Lipopolysaccharide (LPS) as a positive control stimulus.
- Commercial ELISA Kits: Pre-coated kits for the target cytokine (e.g., Human TNF-α ELISA Kit).
- Equipment: Microplate washer, microplate reader, multichannel pipettes.
Procedure:
- Cell Culture and Stimulation: Differentiate and culture immune cells in appropriate medium. Seed cells in a multi-well plate. Expose cells to nanoparticles at various concentrations, a negative control (medium only), and a positive control (e.g., LPS). Incubate for a predetermined time (e.g., 6-24 hours) at 37°C with 5% CO2.
- Sample Collection: Centrifuge the cell culture plate to pellet cells and debris. Carefully transfer the supernatant to a new tube. Store supernatants at -80°C if not used immediately.
- ELISA Procedure: a. Add standards and samples to the pre-coated antibody microplate. Incubate to allow cytokine binding. b. Wash the plate multiple times with wash buffer to remove unbound substances. c. Add the biotinylated detection antibody. Incubate and wash. d. Add the enzyme-streptavidin conjugate (if required). Incubate and wash. e. Add the substrate solution (e.g., TMB). Incubate in the dark for 15-30 minutes for color development. f. Add the stop solution (e.g., sulfuric acid) and measure the absorbance immediately at 450 nm.
- Data Analysis: Generate a standard curve from the known cytokine standards. Use this curve to interpolate the cytokine concentration in the unknown samples.
The Scientist's Toolkit: Essential Reagents for Immunological Assessment
Table 2: Key Research Reagent Solutions for Immunological Evaluation
| Reagent / Material | Function / Application | Example |
|---|---|---|
| Primary Immune Cells | Biologically relevant model for testing human-specific immune responses; used in cytokine release and phenotyping assays. | Human Peripheral Blood Mononuclear Cells (PBMCs) |
| Macrophage Cell Lines | Consistent, readily available model for studying innate immune responses, phagocytosis, and polarization. | THP-1 (human), RAW 264.7 (murine) |
| ELISA Kits | Gold-standard for precise and sensitive quantification of specific soluble immune factors (cytokines, chemokines). | Commercial kits for TNF-α, IL-6, etc. |
| Flow Cytometry Antibody Panels | Enables identification, enumeration, and characterization of multiple immune cell subsets simultaneously from a single sample. | Antibodies against CD14, CD80, CD86, HLA-DR |
| Lipopolysaccharide (LPS) | A potent stimulator of innate immunity; used as a positive control in immune activation assays. | E. coli LPS |
| Complement Assay Kits | Used to evaluate the potential of nanoparticles to activate the complement cascade, a key immune defense mechanism. | kits for measuring C3a, C5a, or SC5b-9 |
Key pathways and readouts in nanoparticle-immune system interactions.
Integration and Rational Design
The data generated from cytotoxicity and immunological profiling are not merely for safety reporting; they are invaluable for the rational design of nanoparticle-based drug delivery systems [92]. By understanding how specific NP properties (size, surface charge, composition, functionalization) influence biological responses, researchers can iteratively optimize formulations.
For instance, mathematical modeling and machine learning can leverage this experimental data to predict the behavior of new NP designs in silico, reducing reliance on extensive in vivo experimentation [92] [94]. This model-informed drug development approach is crucial for accelerating the translation of effective and safe nanomedicines from the laboratory to the clinic [94]. A comprehensive safety assessment, integrated early in the development pipeline, is therefore a cornerstone of efficient and successful nanoparticle-based drug delivery protocol optimization.
Conclusion
Optimizing nanoparticle-based drug delivery requires a paradigm shift from focusing solely on nanoparticle design to implementing integrated, holistic formulation strategies. Success hinges on addressing the entire development pipeline—from understanding fundamental biological barriers and leveraging advanced computational tools like AI and machine learning for predictive optimization, to implementing robust manufacturing and characterization protocols. The future of nanomedicine lies in personalized approaches that account for patient-specific variations in biological barriers, the continued development of smart, stimulus-responsive systems, and the harmonization of regulatory pathways. By bridging the gap between innovative laboratory research and practical clinical requirements through multidisciplinary collaboration, the field can overcome current translational bottlenecks and fully realize the potential of nanotherapeutics to revolutionize treatment for cancer, genetic disorders, and other complex diseases.
References
- 1. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 2. Scale-up polymeric-based nanoparticles drug delivery ... [https://www.sciencedirect.com/science/article/pii/S2352952022000111]
- 3. Bridging the Gap: Regulatory Pathway and Clinical ... [https://link.springer.com/chapter/10.1007/978-981-96-8023-8_12]
- 4. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 5. Challenges and opportunities in computational studies for ... [https://www.nature.com/articles/s44386-025-00024-3]
- 6. Targeted Nanoparticles for Drug Delivery Across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627166/]
- 7. Progress in Drug Delivery Systems Based on ... [https://www.mdpi.com/2072-6694/17/4/701]
- 8. Navigating translational research in nanomedicine [https://www.sciencedirect.com/science/article/pii/S0378517325000389]
- 9. Translational Advances in Lipid Nanoparticle Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567512/]
- 10. Polymeric Nanoparticles in Targeted Drug Delivery: Unveiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991310/]
- 11. Characterisation of polymeric nanoparticles for drug delivery [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr00071h]
- 12. Lipid-Polymer Hybrid Nanoparticles as a Smart Drug ... [https://pubmed.ncbi.nlm.nih.gov/40574109/]
- 13. Lipid-Polymer Hybrid Nanoparticles as a Smart Drug ... [https://www.mdpi.com/1999-4923/17/6/797]
- 14. Nanoparticle Technology Market | Global Market Analysis ... [https://www.futuremarketinsights.com/reports/nanoparticle-technology-market]
- 15. Lipid Nanoparticle (LNP) Drug Delivery Advances March 4- ... [https://www.precigenome.com/post/lnplipid-nanoparticle-drug-delivery-advances-march-4-10-2025-1?srsltid=AfmBOoowsxjln855Mv9ukrHZTL6zNnzWwo1RUDYW9stf6SFpWgNJB_sR]
- 16. Quantitative fluorescent nanoparticle tracking analysis and ... [https://pubmed.ncbi.nlm.nih.gov/39790179/]
- 17. Rediscovery of mononuclear phagocyte system blockade ... [https://www.nature.com/articles/s41467-024-48838-5]
- 18. Nanoparticles Evading The Reticuloendothelial System [https://pmc.ncbi.nlm.nih.gov/articles/PMC2757503/]
- 19. Engineering nano- drug biointerface to overcome biological ... barriers [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01605-4]
- 20. Overcoming Endosomal Entrapment in Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6501178/]
- 21. Factors affecting the dynamics and heterogeneity of ... [https://pubmed.ncbi.nlm.nih.gov/33430661/]
- 22. Approaches to Improve EPR-Based Drug Delivery for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10051487/]
- 23. Image-guided strategies to improve drug delivery to tumors ... [https://www.sciencedirect.com/science/article/pii/S0006291X25010617]
- 24. Challenges in Development of Nanoparticle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326161/]
- 25. Understanding CQAs For mRNA/Lipid Nanoparticle ... [https://www.advancingrna.com/doc/understanding-cqas-for-mrna-lipid-nanoparticle-product-development-and-manufacture-0001]
- 26. Identifying Critical Quality Attributes for mRNA/LNP [https://www.biophorum.com/news/an-industry-standard-for-mrna-lnp-analytics/]
- 27. Six measurement techniques for nanoparticle size ... [https://www.biolinscientific.com/blog/six-measurement-techniques-for-nanoparticle-size-characterization?update_2025=1]
- 28. How to determine the correct size of nanoparticles?- A review [https://www.sciencedirect.com/science/article/pii/S0925838825058645?dgcid=rss_sd_all]
- 29. Physical and chemical stability of drug nanoparticles [https://www.sciencedirect.com/science/article/abs/pii/S0169409X11000172]
- 30. Zeta Potential Overview - Fundamentals and Applications [https://www.wyatt.com/solutions/properties/charge-zeta-potential.html]
- 31. Zeta potential measurement - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/21116954/]
- 32. Nanoparticle Surface Functionalization: How to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726445/]
- 33. Recent Advances in Different Nanoprecipitation Methods ... [https://www.scientificarchives.com/article/recent-advances-in-different-nanoprecipitation-methods-for-efficient-drug-loading-and-controlled-release]
- 34. Recent advances in stimulus-assisted nanoprecipitation for ... [https://arxiv.org/html/2511.14627v1]
- 35. ADVANCED MANUFACTURING OF NANOPARTICLE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842755/]
- 36. Optimization of PLGA Nanoparticle Formulation via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471678/]
- 37. A Comparative Study of Flash Nanoprecipitation and ... [https://pubmed.ncbi.nlm.nih.gov/40961334/]
- 38. Design Strategies for Novel Lipid Nanoparticle for mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497691/]
- 39. Engineering of mRNA vaccine platform with reduced lipids ... [https://www.nature.com/articles/s41467-025-63965-3]
- 40. Nanoparticle biodistribution coefficients: A quantitative ... [https://www.sciencedirect.com/science/article/pii/S0169409X23000236]
- 41. The Use of Computational Approaches to Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12430099/]
- 42. Data-Driven Prediction of Nanoparticle Biodistribution from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312149/]
- 43. Optimization of Nanoparticles for Smart Drug Delivery: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC8622036/]
- 44. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 45. Confocal reflectance microscopy for metal and lipid ... [https://pubmed.ncbi.nlm.nih.gov/35142565/]
- 46. Guiding a confocal microscope by single fluorescent ... [https://opg.optica.org/ol/abstract.cfm?uri=ol-32-18-2729]
- 47. Navigating the Development of Dry Powder for Inhalation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944951/]
- 48. Rethinking Inhalation Drug Development [https://expericservices.com/resource/rethinking-inhalation-drug-development/article/]
- 49. Recent advancements in nanoparticle drug delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S1853002825000254]
- 50. Rise of implantable drugs: A chronicle of breakthroughs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11570717/]
- 51. Active implantable drug delivery systems: engineering factors ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00131e]
- 52. Nanomaterials in Drug Delivery: Leveraging Artificial ... [https://www.mdpi.com/1422-0067/26/22/11121]
- 53. GitHub - RekerLab/TuNa-AI [https://github.com/RekerLab/TuNa-AI]
- 54. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 55. 【中国科学报】“机器科学家”开启纳米晶数字智造----中国科学院网信工作网 [https://ecas.cas.cn/dtfb/mtgz/202303/t20230322_4939676.html]
- 56. 程强/魏妥团队开发新型LNP,将mRNA精准送达肺/肝/脾/胸腺 ... [https://news.bioon.com/article/76b4895092d6.html]
- 57. 材料计算模拟软件_人工智能材料设计_分子模拟_MaXFlow 材料物理-创腾科技 [https://www.neotrident.com/product/ms_Phys.html]
- 58. 基于纳米技术的药物输送市场2025 |趋势与预测、竞争格局 [https://cn.linkedin.com/pulse/%E5%9F%BA%E4%BA%8E%E7%BA%B3%E7%B1%B3%E6%8A%80%E6%9C%AF%E7%9A%84%E8%8D%AF%E7%89%A9%E8%BE%93%E9%80%81-%E5%B8%82%E5%9C%BA-2025-%E8%B6%8B%E5%8A%BF%E4%B8%8E%E9%A2%84%E6%B5%8B%E7%AB%9E%E4%BA%89%E6%A0%BC%E5%B1%80%E4%BA%A7%E5%93%81%E4%B8%8E%E5%BA%94%E7%94%A8%E4%BF%A1%E6%81%AF-ideas-into-innovation-2cc4c]
- 59. Intelligence analysis of drug nanoparticles delivery ... [https://www.nature.com/articles/s41598-024-84450-9]
- 60. Data-driven optimization of nanoparticle size using the ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr01664a]
- 61. Enhancing Therapeutic Efficacy and Minimizing Toxicity [https://www.mdpi.com/2673-4591/109/1/19]
- 62. Stealth Coating of Nanoparticles in Drug-Delivery Systems [https://www.mdpi.com/2079-4991/10/4/787]
- 63. PEG alternatives for RNA therapeutics [https://www.nature.com/articles/s41563-025-02408-2]
- 64. PEG Alternatives: Polymers Reshaping Lipid Nanoparticle ... [https://blog.curapath.com/peg-alternatives]
- 65. Considering the immunogenicity of PEG - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413056/]
- 66. Next-Generation mRNA-LNPs: Strategies to Reduce Anti ... [https://www.biochempeg.com/article/453.html]
- 67. Intelligence prediction of microfluidically prepared ... [https://www.nature.com/articles/s41598-025-21471-y]
- 68. Artificial intelligence for drug delivery: Yesterday, today and ... [https://www.sciencedirect.com/science/article/pii/S2211383525006227]
- 69. How Nanoparticles Are Revolutionizing Drug Delivery [https://www.technologynetworks.com/drug-discovery/blog/how-nanoparticles-are-revolutionizing-drug-delivery-405140]
- 70. Engineering precision nanoparticles for drug delivery [https://www.nature.com/articles/s41573-020-0090-8]
- 71. Nano based drug delivery systems: recent developments and ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-018-0392-8]
- 72. Dynamic Light Scattering (DLS): Principles, Perspectives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7120185/]
- 73. Atomic Force Microscopy Application in Biological Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC3700051/]
- 74. Atomic Force Microscopy (AFM): Principles, Modes, and ... [https://www.nanbiosis.es/atomic-force-microscopy-afm-principles-modes-and-emerging-applications-in-nanotechnology-and-biomedicine/]
- 75. Discovering Atomic Force Microscopy: Principles and ... [https://www.neware.net/news/discovering-atomic-force-microscopy-principles-and-applications/230/111.html]
- 76. Current and Near-Future Technologies to Quantify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025210/]
- 77. A review on multifunctional applications of nanoparticles [https://www.sciencedirect.com/science/article/pii/S2666845925002223]
- 78. Neural network-enhanced dynamic light scattering for ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224125019451]
- 79. Nanoparticles for drug delivery: Insight into in vitro and in ... [https://www.sciencedirect.com/science/article/pii/S2790676025000147]
- 80. Impact of physicochemical properties on biological effects ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969724023830]
- 81. Impact of Nanoparticle Physicochemical Properties on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11955209/]
- 82. Researchers Develop Metal-Free Click Chemistry Protocol for ... [https://www.geneonline.com/researchers-develop-metal-free-click-chemistry-protocol-for-precise-antibody-conjugation-to-polymersome-nanoparticles/]
- 83. Recent Trends, Enabling Technologies, In-Vitro-In-Vivo ... [https://drug-dev.com/whitepapers/drug-delivery-recent-trends-enabling-technologies-in-vitro-in-vivo-predictions-personalized-medicine/]
- 84. A comprehensive multi-technique analysis of hard and soft ... [https://www.sciencedirect.com/science/article/pii/S0378517325004417]
- 85. Nano–bio interactions and drug delivery using soft nanoparticles [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d4pm00170b]
- 86. Soft and Condensed Nanoparticles and Nanoformulations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8291088/]
- 87. Review Nanoparticle-enhanced drug delivery systems [https://www.sciencedirect.com/science/article/abs/pii/S0167732225001576]
- 88. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 89. Nanoparticles in tissue engineering: applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6161712/]
- 90. Basics of Biocompatibility: Information Needed for ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/basics-biocompatibility-information-needed-assessment-fda]
- 91. Bioresponsive engineered nanoparticles for immunomodulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574298/]
- 92. Rational Nanoparticle Design: Optimization Using Insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10529591/]
- 93. The “Big Three” in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 94. Current state-of-the-art in multi-scale modeling in nano-cancer ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00326-1]
- 95. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 96. Cytotoxicity evaluation and metabolomic profiling of ... [https://www.nature.com/articles/s41598-025-04162-6]
- 97. Targeted nano-drug delivery systems for tumor ... [https://www.sciencedirect.com/science/article/pii/S2095177925002254]