Overcoming the Blood-Brain Barrier: Advanced Drug Delivery Strategies for Neurodegenerative Diseases
This article provides a comprehensive analysis of the latest strategies to overcome the blood-brain barrier (BBB) for effective drug delivery to the central nervous system.
Overcoming the Blood-Brain Barrier: Advanced Drug Delivery Strategies for Neurodegenerative Diseases
Abstract
This article provides a comprehensive analysis of the latest strategies to overcome the blood-brain barrier (BBB) for effective drug delivery to the central nervous system. Tailored for researchers and drug development professionals, it explores the foundational biology of the BBB, evaluates cutting-edge methodological approaches like receptor-mediated transcytosis and focused ultrasound, addresses critical troubleshooting and optimization challenges in translational research, and offers a comparative validation of emerging technologies. The content synthesizes recent preclinical advances, clinical trial data, and industry trends to present a holistic view of the rapidly evolving landscape in neurotherapeutics.
The Blood-Brain Barrier: Understanding the Guardian of the CNS
Anatomical and Cellular Composition of the Neurovascular Unit
Frequently Asked Questions (FAQs)
Q1: What is the neurovascular unit (NVU) and why is it critical for central nervous system drug delivery?
The neurovascular unit (NVU) is a multicellular complex that forms a functional interface between the blood circulation and the central nervous system (CNS). It serves as the structural and physiological basis for the blood-brain barrier (BBB) [1] [2]. The primary function of the NVU is to maintain CNS homeostasis by regulating the delicate brain microenvironment, protecting neural tissue from toxins and pathogens, and controlling the passage of nutrients and metabolites [1] [3]. For drug delivery, the NVU presents a significant challenge because its tightly regulated barrier properties prevent more than 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from reaching the brain [3] [4]. Understanding its composition is therefore essential for developing strategies to overcome this barrier for treating neurological disorders.
Q2: Which specific cell types form the core components of the NVU?
The NVU consists of a core ensemble of specialized cells working in concert. The key cellular components include:
- Brain Microvascular Endothelial Cells (BMECs): These cells line the cerebral blood vessels and form the primary physical barrier through tight junctions, drastically limiting paracellular transport [3] [4].
- Pericytes: These mural cells are embedded in the basement membrane and are central to regulating vasomotion, cerebral blood flow, and maintaining BBB stability [3] [2].
- Astrocytes: Their star-shaped end-feet extensively cover the abdominal surface of blood vessels. They provide structural and metabolic support to endothelial cells and help regulate BBB function [3] [2].
- Neurons: As the "pacemakers" of the NVU, neurons signal their metabolic demands, which in turn regulates vascular tone and blood flow to meet energy requirements [1] [5].
- Microglia and Oligodendrocytes: These glial cells contribute to immune surveillance and axonal myelination, respectively, further supporting the NVU's integrated function [2].
Q3: Our drug candidate shows poor penetration in an in vivo model. What are the primary barrier functions of the NVU that could explain this?
The NVU limits drug penetration through several coordinated mechanisms:
- Physical Barrier: Tight junctions (composed of proteins like claudin, occludin, and ZO-1) between endothelial cells severely restrict the paracellular (between cells) diffusion of most molecules [6] [3].
- Transport Barrier: Selective transport systems allow only specific substances to cross.
- Efflux Pumps: ATP-binding cassette (ABC) transporters like P-glycoprotein (P-gp) actively pump a wide range of foreign compounds, including many drugs, back into the bloodstream [6] [4].
- Nutrient Transporters: Carrier-mediated transport (CMT) systems exist for essential nutrients (e.g., GLUT1 for glucose), but they are highly selective [7] [4].
- Enzymatic Barrier: The endothelial cells exhibit enzymatic activity capable of degrading certain molecules before they can cross the BBB [6].
- Receptor-Mediated Control: Specific receptors facilitate the transcytosis of large molecules (e.g., via transferrin receptor), but this process is tightly regulated [4].
The table below summarizes the key quantitative barriers a drug may encounter.
Table 1: Key Barrier Properties of the Neurovascular Unit Impacting Drug Delivery
| Barrier Type | Key Components | Functional Impact on Drugs |
|---|---|---|
| Physical Barrier | Tight Junctions (Claudin-5, Occludin) [8] | Prevents paracellular diffusion of >95% of potential therapeutics [7]. |
| Efflux Transport | P-glycoprotein (P-gp), BCRP, MRPs [6] [4] | Recognizes and actively effluxes >60% of marketed drugs [7]. |
| Size/Lipophilicity Limit | Continuous endothelial membrane [7] | Effectively restricts passive diffusion to small (<400-600 Da), lipophilic molecules [3]. |
| Enzymatic Degradation | Cytochrome P450 enzymes and others [6] | Metabolizes drugs at the barrier, reducing bioavailability [6]. |
Q4: We observe regional differences in drug delivery efficacy in the brain. Is the NVU uniform throughout the CNS?
No, the NVU exhibits significant regional heterogeneity, which can lead to varying drug delivery outcomes [8]. Key differences include:
- Gray vs. White Matter: The metabolic demands and vascular architecture differ. Glucose consumption is 2–4 times greater in synapse-rich gray matter [8]. Some evidence suggests endothelial cells in white matter form a tighter paracellular barrier under normal conditions but may be more susceptible to pathological hyperpermeability [8].
- Vascular Tree Location: The properties of NVU cells vary along the arteriole-capillary-venule axis. For example, gene expression in endothelial cells and the phenotypes of pericytes differ depending on their position [8].
- Circumventricular Organs (CVOs): Regions like the area postrema lack a tight BBB, allowing a more active exchange between blood and the CNS, which can be exploited for drug delivery [6] [8].
This heterogeneity means that a one-size-fits-all approach to brain drug delivery is unlikely to be successful.
Troubleshooting Common Experimental Challenges
Q5: Our in vitro BBB model shows unusually low transendothelial electrical resistance (TEER). What could be the cause?
Low TEER indicates a leaky barrier, often due to incomplete formation or damage to tight junctions. Consider the following troubleshooting steps:
- Verify Cell Source and Quality: Primary BMECs or stem cell-derived BMECs should express high levels of tight junction proteins (claudin-5, occludin). Check protein expression via immunocytochemistry [2].
- Review Co-culture Conditions: A proper NVU model often requires co-culture with pericytes and astrocytes, which secrete signaling factors that enhance barrier integrity. Ensure your model includes these supportive cells or their conditioned media [3] [2].
- Check Culture Duration: TEER can take several days to reach a stable, high plateau. Measure TEER over time to ensure the model has matured sufficiently.
- Assess Media Components: Certain growth factors (e.g., VEGF) can increase permeability. Use specialized media formulations designed to promote a barrier phenotype, often involving hydrocortisone and cAMP analogs.
Q6: In our animal studies, how can we distinguish if a drug is crossing the BBB via passive diffusion or active transport?
Distinguishing the transport mechanism is key for optimization. The following experimental approaches can be used:
- Inhibitor Studies: Use specific inhibitors for transport pathways.
- To test for efflux by P-gp, co-administer a known P-gp inhibitor like verapamil or elacridar. An increase in brain concentration of your drug suggests it is a P-gp substrate [6].
- To test for carrier-mediated transport (CMT), use an excess of a natural substrate (e.g., D-glucose for GLUT1). A reduction in your drug's uptake suggests it uses that transporter [4].
- Saturability Assay: Administer increasing doses of the drug. Active transport processes (both influx and efflux) are saturable, while passive diffusion is not. A non-linear relationship between plasma exposure and brain uptake suggests an active process [4].
- Enantiomer Comparison: If your drug is a racemic mixture, test the brain uptake of individual enantiomers. Carrier systems are often stereospecific, while passive diffusion is not.
Table 2: Experimental Protocols for Investigating Drug Transport Mechanisms
| Target Mechanism | Experimental Approach | Key Reagents & Methods | Interpretation of Positive Result |
|---|---|---|---|
| P-gp Efflux | Co-administration with P-gp inhibitor [6] | Elacridar (GW572016) or Tariquidar; administered IV or IP prior to drug. | Significant increase in brain-to-plasma ratio compared to control. |
| Carrier-Mediated Influx | Saturation and competition studies [4] | Co-perfusion with high concentration of natural substrate (e.g., glucose for GLUT1). | Significant reduction in drug uptake in the brain. |
| Receptor-Mediated Transcytosis | Ligand competition assay [4] | Co-administration with excess unlabeled ligand (e.g., transferrin for TfR). | Reduction in brain uptake of the drug candidate. |
| General Active Transport | Dose-dependence study [4] | IV administration of drug across a wide dose range. | Non-linear (saturable) brain uptake kinetics. |
Key Signaling Pathways and Experimental Workflows
The following diagram illustrates the coordinated signaling between major cell types within the NVU that maintains barrier integrity and regulates blood flow.
NVU Signaling Network
Detailed Protocol: Assessing the Role of a Specific Receptor in RMT
Objective: To validate whether a drug conjugate targeting the Transferrin Receptor (TfR) undergoes Receptor-Mediated Transcytosis (RMT) across an in vitro BBB model.
- Model Establishment: Use a well-characterized in vitro BBB model, such as a Transwell system with primary BMECs or induced pluripotent stem cell (iPSC)-derived BMECs, preferably in co-culture with astrocytes and/or pericytes. Validate model integrity by measuring TEER (>150 Ω·cm² is often acceptable) [2].
- Ligand Conjugation: Conjugate your drug payload to a validated ligand for the target receptor (e.g., an anti-TfR antibody or the transferrin protein itself).
- Competitive Inhibition Assay:
- Pre-incubate the BMECs with a large excess (e.g., 10-100x molar ratio) of unlabeled ligand (e.g., apo-transferrin) for 30-60 minutes to saturate the receptors.
- Add the fluorescently or radio-labeled drug conjugate to the apical (blood) compartment.
- Incubate for a set time (e.g., 2-4 hours).
- Sample Collection and Analysis: Collect samples from the basolateral (brain) compartment. Quantify the amount of drug conjugate that has translocated using an appropriate method (e.g., fluorescence, radioactivity, LC-MS).
- Data Interpretation: A statistically significant reduction in the transport of the drug conjugate in the competition group compared to the control (no competitor) provides strong evidence that transport is specifically mediated by the TfR pathway.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Neurovascular Unit and BBB Permeability Research
| Reagent / Tool | Primary Function in Experiment | Example Specifics & Notes |
|---|---|---|
| Primary BMECs / iPSC-BMECs | Form the core barrier layer in in vitro models [2]. | Must express high levels of tight junction proteins and functional efflux transporters. |
| Transwell/Cell Culture Inserts | Provide a semi-permeable membrane for co-culture and permeability assays [2]. | Polycarbonate or polyester membranes with 0.4-3.0 µm pores are standard. |
| TEER Measurement System | Quantifies the integrity and tightness of the cellular barrier in real-time [2]. | Uses a voltmeter and electrodes (chopstick or EndOhm). TEER >150 Ω·cm² is a common quality threshold. |
| P-gp Inhibitors (e.g., Elacridar) | Pharmacologically blocks the P-glycoprotein efflux pump to assess its role in limiting drug uptake [6]. | Used in both in vitro and in vivo studies. |
| Tight Junction Protein Antibodies | Visualize and quantify (via ICC/IHC) the expression and localization of claudin-5, occludin, ZO-1 [8] [3]. | Critical for validating the quality of in vitro models and assessing BBB damage in tissue. |
| Paracellular Tracers (e.g., FITC-Dextran) | Measure nonspecific paracellular leakage in in vitro models or in vivo [7]. | Commonly used sizes are 4 kDa and 70 kDa. |
| In Vivo Imaging Agents | Visualize BBB disruption and drug distribution in animal models [2]. | Includes Evans Blue dye, MRI contrast agents (Gadolinium), and PET tracers. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary cellular components that contribute to the blood-brain barrier's physiological barrier function? The BBB's barrier function is primarily established by specialized brain microvascular endothelial cells that are interconnected by tight junctions [9] [10]. These endothelial cells are supported by and interact with pericytes embedded in the capillary basement membrane and the end-feet of astrocytes [9] [3] [11]. This multicellular ensemble, often referred to as the neurovascular unit, works in concert to create a highly selective barrier [10].
FAQ 2: Which specific tight junction proteins are most critical for maintaining the high electrical resistance and low paracellular permeability of the BBB? Claudin-5 is recognized as the dominant tight junction protein at the BBB and is particularly critical for sealing the paracellular pathway to small molecules [10]. Other key proteins include occludin and the junctional adhesion molecule (JAM-A), all of which are stabilized to the endothelial cell membrane by scaffolding proteins like zonula occludens-1 (ZO-1) [10] [12]. The balance and interaction between these proteins, rather than the level of a single protein alone, are crucial for overall tight junction integrity [10].
FAQ 3: How do efflux transporters at the BBB limit the brain penetration of therapeutic drugs, and which one is most commonly associated with multidrug resistance? Efflux transporters are ATP-dependent pumps located on the luminal membrane of brain endothelial cells that actively transport a wide range of xenobiotics back into the blood circulation [13] [4]. The most prominent and well-studied efflux transporter is P-glycoprotein (P-gp), which is associated with multidrug resistance and can limit the distribution of many beneficial CNS therapeutics [13] [3] [14].
FAQ 4: What types of metabolic enzymes are present at the BBB, and what is their role? The BBB expresses a complement of drug-metabolizing enzymes that form a metabolic barrier [10]. These enzymes are capable of inactivating therapeutics or altering their chemical structure during the process of crossing the endothelial cells, thereby reducing the amount of active drug that reaches the brain parenchyma [10].
FAQ 5: Under what pathological conditions does the integrity of the BBB become compromised? BBB integrity can be compromised in a wide range of acute and chronic neurological conditions [9] [13]. Key examples include:
- Neurodegenerative diseases: Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis [15] [13].
- Acute insults: Ischemic stroke, traumatic brain injury, and hypoxic-ischemic encephalopathy [9] [13].
- Other conditions: High-grade gliomas, multiple sclerosis, and hepatic encephalopathy [9] [11]. This dysfunction often involves disruption of tight junctions and increased permeability.
Troubleshooting Guides
Guide 1: Investigating P-gp Mediated Efflux of a Lead Compound
Problem: A promising small molecule drug shows excellent potency in cellular assays but demonstrates poor brain penetration in vivo, despite favorable molecular weight and lipophilicity.
Investigation Hypothesis: The compound is a substrate for the P-glycoprotein (P-gp) efflux pump, limiting its brain accumulation.
Step-by-Step Experimental Protocol:
Step 1: In Vitro Transport Assay
- Objective: To assess the compound's directional transport and potential for active efflux.
- Method: Use a validated model of the BBB, such as MDCK-MDR1 or hCMEC/D3 cells seeded on Transwell inserts. The MDCK-MDR1 cell line is a canine kidney epithelial cell line engineered to overexpress human P-gp.
- Procedure:
- Seed cells on permeable membrane supports and culture until a confluent monolayer with high TEER is formed.
- Add the test compound to either the apical (A) or basolateral (B) compartment in a transport buffer (e.g., HBSS or PBS, pH 7.4).
- Incubate at 37°C and sample from the opposite compartment at predetermined time points (e.g., 30, 60, 90, 120 minutes).
- Analyze samples using LC-MS/MS or HPLC to determine compound concentration.
- Data Analysis: Calculate the apparent permeability (Papp) and the efflux ratio (ER).
- Papp (cm/s) = (dQ/dt) / (A × C0), where dQ/dt is the rate of permeation, A is the membrane surface area, and C0 is the initial donor concentration.
- ER = Papp (B to A) / Papp (A to B).
- An ER > 2 suggests active efflux.
Step 2: Confirmatory Assay with P-gp Inhibition
- Objective: To confirm that the observed efflux is specifically mediated by P-gp.
- Method: Repeat the transport assay in the presence of a selective and potent P-gp inhibitor (e.g., Zosuquidar (LY335979) or Tariquidar).
- Procedure:
- Pre-incubate the cell monolayers with the inhibitor (e.g., 2 µM Zosuquidar) for a set time (e.g., 1 hour).
- Perform the A-to-B and B-to-A transport assays as in Step 1, maintaining the inhibitor in the buffer throughout the experiment.
- Data Analysis: Recalculate the ER in the presence of the inhibitor. A significant reduction in the ER (towards a value of 1) confirms P-gp-mediated efflux.
Step 3: In Vivo Validation
- Objective: To confirm P-gp efflux activity in a live animal model.
- Method: Conduct a pharmacokinetic study in wild-type mice with and without a P-gp inhibitor.
- Procedure:
- Administer a P-gp inhibitor (e.g., Tariquidar, 15 mg/kg, i.v.) or vehicle to the animals.
- After a predetermined time, administer the test compound (i.v. or p.o.).
- Collect blood and brain samples at multiple time points post-dosing.
- Determine the plasma and brain concentrations of the compound using a validated bioanalytical method.
- Data Analysis: Calculate the brain-to-plasma ratio (Kp) for both groups.
- Kp = (AUCbrain) / (AUCplasma), where AUC is the area under the concentration-time curve.
- A statistically significant increase in the Kp in the inhibitor-treated group compared to the control group provides in vivo evidence that the compound is a P-gp substrate.
Interpretation of Results: A compound is classified as a P-gp substrate if it demonstrates an efflux ratio > 2 in vitro, which is significantly diminished by a P-gp inhibitor, and shows a significantly increased brain penetration in vivo when co-administered with a P-gp inhibitor.
Guide 2: Assessing Tight Junction Integrity In Vitro
Problem: A novel drug delivery strategy (e.g., a nanoparticle formulation) is intended to transiently and safely modulate the BBB to improve drug delivery. You need to evaluate its potential impact on BBB integrity.
Investigation Hypothesis: The formulation may compromise BBB integrity by disrupting tight junction complexes.
Step-by-Step Experimental Protocol:
Step 1: Real-time Monitoring of Barrier Integrity
- Objective: To continuously and non-invasively monitor the integrity of the endothelial cell monolayer.
- Method: Use an Electrical Cell-substrate Impedance Sensing (ECIS) system or a voltohmmeter to measure Transendothelial Electrical Resistance (TEER).
- Procedure:
- Grow brain endothelial cells (e.g., hCMEC/D3) on gold electrode arrays or Transwell inserts designed for TEER measurement.
- Monitor TEER until it reaches a stable, high value (e.g., >150 Ω×cm² for many models), indicating a tight monolayer.
- Apply the test formulation to the apical compartment. Include a positive control (e.g., calcium-free medium to disrupt junctions) and a negative control (vehicle/blank buffer).
- Record TEER values at frequent intervals (e.g., every 15-30 minutes) for up to 24 hours.
- Data Analysis: Express TEER as a percentage of the pre-treatment value. A significant and rapid drop in TEER indicates a loss of barrier integrity.
Step 2: Assessment of Paracellular Permeability
- Objective: To functionally quantify the flux of paracellular markers across the monolayer.
- Method: Perform a permeability assay using fluorescent or radiolabeled tracers of different sizes after treatment.
- Procedure:
- After treating cells as in Step 1, add a membrane-impermeable paracellular tracer to the donor compartment (apical for A-to-B flux). Common tracers include:
- Sodium fluorescein (376 Da): For small molecule permeability.
- FITC-Dextran (4 kDa or 10 kDa): For larger molecule permeability.
- Incubate for a set time (e.g., 30-60 minutes) at 37°C.
- Sample from the acceptor compartment and measure fluorescence/radioactivity.
- After treating cells as in Step 1, add a membrane-impermeable paracellular tracer to the donor compartment (apical for A-to-B flux). Common tracers include:
- Data Analysis: Calculate the Papp for the tracer. A significant increase in Papp for the treated group compared to the negative control confirms increased paracellular leak.
Step 3: Immunofluorescence Analysis of Tight Junction Proteins
- Objective: To visually assess the morphological impact on tight junction complexes.
- Method: Use confocal microscopy to examine the localization and continuity of key tight junction proteins.
- Procedure:
- At the end of the treatment period, wash cells and fix with paraformaldehyde (e.g., 4% for 15 min).
- Permeabilize cells with Triton X-100 (e.g., 0.1% for 10 min) and block with serum (e.g., 5% BSA for 1 hour).
- Incubate with primary antibodies against tight junction proteins (e.g., anti-claudin-5, anti-occludin, anti-ZO-1) overnight at 4°C.
- Incubate with fluorescently labeled secondary antibodies (e.g., Alexa Fluor 488, 568) for 1 hour at room temperature. Include a nuclear stain (e.g., DAPI).
- Image using a confocal microscope.
- Data Analysis: In an intact barrier, ZO-1, claudin-5, and occludin appear as continuous, sharply defined bands at the cell borders. Disruption is characterized by fragmentation, discontinuity, or internalization of these signals.
Interpretation of Results: A formulation that causes a drop in TEER, an increase in paracellular tracer flux, and discontinuous tight junction immunostaining is likely disrupting BBB integrity. The combination of functional and morphological data provides a comprehensive assessment.
Quantitative Data Tables
Table 1: Common Tracer Molecules for Assessing BBB Paracellular Permeability
| Tracer Molecule | Molecular Weight (Da) | Key Properties | Application in BBB Research |
|---|---|---|---|
| Sodium Fluorescein | 376 | Hydrophilic, fluorescent | A standard small molecule tracer to assess minor changes in paracellular permeability [10]. |
| FITC-Dextran 4k | 4,000 | Hydrophilic, fluorescently labeled polysaccharide | Used to model the passage of small biologics and assess more significant barrier disruption [10]. |
| FITC-Dextran 10k | 10,000 | Hydrophilic, fluorescently labeled polysaccharide | A larger tracer to probe major barrier breakdown, relevant for larger therapeutic molecules [10]. |
| Evans Blue | 961 | Binds serum albumin, forming a ~68 kDa complex | A classic in vivo tracer; the albumin complex is used to visualize and quantify gross leakage of proteins [10]. |
| Sucrose | 342 | Radiolabeled (e.g., 14C-sucrose), hydrophilic | A non-metabolized small molecule tracer providing high sensitivity in quantitative permeability studies [10]. |
Table 2: Key Efflux Transporters at the BBB and Their Substrates
| Transporter | Primary Location | Representative Substrates (Therapeutics) | Impact on Drug Delivery |
|---|---|---|---|
| P-glycoprotein (P-gp/ABCB1) | Luminal membrane | Chemotherapeutics (doxorubicin, paclitaxel), HIV protease inhibitors (ritonavir), antibiotics (erythromycin) [13] [14] | Major obstacle for a wide range of small molecule drugs; contributes to multidrug resistance in brain tumors and other CNS diseases. |
| Breast Cancer Resistance Protein (BCRP/ABCG2) | Luminal membrane | Chemotherapeutics (mitoxantrone, topotecan), tyrosine kinase inhibitors (imatinib) [4] | Often works in concert with P-gp; limits penetration of many targeted therapy agents. |
| Multidrug Resistance-Associated Proteins (MRPs/ABCC family) | Luminal / Basolateral membranes | Anticonvulsants (phenytoin), methotrexate, conjugated organic anions [4] | Contributes to the efflux of anionic drugs and drug conjugates, impacting treatment of epilepsy and cancer. |
Signaling Pathways and Experimental Workflows
Tight Junction Regulation Pathway
In Vitro BBB Model Workflow
Research Reagent Solutions
Table 3: Essential Reagents for Investigating BBB Physiological Barriers
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| hCMEC/D3 Cell Line | A widely used, well-characterized human immortalized brain endothelial cell line for in vitro BBB models [4]. | Represents many key BBB properties but requires induction for high TEER; lower baseline TEER than in vivo. |
| MDCK-MDR1 Cell Line | Canine kidney cells overexpressing human P-gp; a standard model for high-throughput efflux transporter studies [13]. | Not of brain origin; used primarily for transporter interaction screening rather than full BBB mimicry. |
| Claudin-5 Antibody | Immunodetection of the critical tight junction protein for assessing junctional integrity via IF or WB [10]. | Specificity is critical; results should be interpreted alongside functional data (TEER, permeability). |
| P-gp Inhibitors (e.g., Zosuquidar, Tariquidar) | Selective pharmacological blockers used to confirm P-gp substrate status in transport and in vivo studies [13]. | Concentration must be optimized to avoid non-specific effects; verify selectivity for P-gp over other transporters. |
| Paracellular Tracers (e.g., FITC-Dextran 4k) | Hydrophilic, size-defined molecules used to quantify functional paracellular permeability [10]. | A panel of tracers of different sizes (e.g., 4k, 10k, 70k Da) can provide information on the size selectivity of barrier opening. |
| Transwell Inserts | Permeable supports for growing endothelial cell monolayers and performing transport assays. | Pore size (e.g., 0.4 µm, 1.0 µm) and membrane material (e.g., polyester, polycarbonate) can influence cell growth and assay outcomes. |
FAQ: Blood-Brain Barrier Fundamentals and Dysfunction
Q1: What is the primary function of the BBB, and why is it a major challenge for drug development in neurodegenerative diseases?
The blood-brain barrier (BBB) is a highly selective semi-permeable border that protects the central nervous system (CNS). It maintains brain homeostasis by preventing harmful substances in the blood from entering the brain while regulating the transport of nutrients [4] [16]. Its structure, composed of brain microvascular endothelial cells connected by tight junctions, along with pericytes, astrocytes, and a basement membrane, creates a formidable physical and metabolic barrier [4]. This protective function becomes a major therapeutic challenge because it blocks over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics, such as proteins, antibodies, and gene therapies, from reaching the brain in effective concentrations [15] [4] [16].
Q2: How does BBB dysfunction contribute to the pathogenesis of Alzheimer's disease?
BBB dysfunction plays a key role in Alzheimer's disease (AD) pathogenesis through multiple interconnected mechanisms. Structurally, the barrier deteriorates, particularly in the hippocampus, with this degradation being more pronounced in patients with mild cognitive impairment (MCI) than in healthy controls [17]. Key molecular changes include reduced levels of LRP-1 (a transporter that clears amyloid-β from the brain) and increased levels of RAGE (a receptor that facilitates amyloid-β influx into the brain), leading to impaired amyloid-β clearance and accumulation [17]. This dysfunction triggers neuroinflammation and oxidative stress, which can further enhance the activity of β- and γ-secretases, increasing amyloid-β production and creating a vicious cycle of pathology and barrier impairment [17]. Recent CSF proteomic research has even identified a specific AD subtype primarily driven by BBB dysfunction, emphasizing its central role in the disease [17].
Q3: What are the common pathways of BBB dysfunction across Alzheimer's, Parkinson's, and ALS?
While each disease has unique features, common pathways of BBB dysfunction link these neurodegenerative pathologies. Neuroinflammation is a universal hallmark, characterized by the activation of endothelial cells and the release of cytokines that compromise barrier integrity [15] [4]. Impaired clearance of toxic proteins—such as amyloid-β in AD, α-synuclein in PD, and SOD1 in ALS—is another shared mechanism, often involving dysregulation of specific transporters at the BBB [15] [17]. Furthermore, a loss of tight junction integrity leads to increased paracellular permeability across these diseases [4]. The choroid plexus, which forms the blood-CSF barrier, also shows dysfunction in AD and likely in other neurodegenerative conditions, contributing to altered CSF production and impaired immune surveillance [18] [17].
FAQ: Advanced Models and Diagnostic Tools
Q4: What novel biomarkers are emerging for detecting BBB dysfunction in patients?
Research is moving beyond classical amyloid and tau biomarkers to identify blood-based biomarkers (BBMs) related to brain barrier failure. Promising candidates include [17]:
- Neurofilament Light (NfL): Associated with neuroinflammation, demyelination, and axonal degradation.
- Glial Fibrillary Acidic Protein (GFAP): An indicator of neuroinflammation and astrocyte activation.
- Transactive Response DNA-binding Protein 43 (TDP-43): Implicated in tau-independent neurodegeneration.
- Complement Component 3 (C3): Involved in neuroinflammatory pathways.
Advanced MRI techniques can also measure the volume and structural integrity of the choroid plexus. Studies have found that an enlarged choroid plexus volume and reduced structural integrity are correlated with higher levels of p-tau181, NfL, and GFAP, suggesting these imaging measures can serve as non-invasive proxies for BBB and blood-CSF barrier dysfunction even in early-stage AD [17].
Q5: What in vivo and in vitro models are best for studying BBB dysfunction and drug penetration?
The choice of model depends on the specific research question. The table below summarizes key models and their applications.
Table 1: Experimental Models for Studying BBB Dysfunction and Drug Penetration
| Model Type | Key Features | Best Use Cases | Limitations |
|---|---|---|---|
| In Vivo Animal Models | Provides a full physiological context, including all cell types of the neurovascular unit and blood flow [4]. | Studying complex disease pathogenesis, whole-body pharmacokinetics, and efficacy of novel delivery systems [19]. | Interspecies differences in BBB biology; ethical and cost concerns. |
| In Vitro Static Models (e.g., Transwell assays) | Cultured brain endothelial cells on a permeable filter. Low-cost, high-throughput screening of permeability [4]. | Initial assessment of passive diffusion or transporter-mediated uptake; mechanistic studies. | Lack of fluid flow and crucial cellular interactions; often overestimates permeability. |
| Advanced In Vitro Models (e.g., microfluidic "BBB-on-a-chip") | Incorporates fluid shear stress and co-culture with pericytes and astrocytes for a more physiologically relevant barrier [4]. | Detailed study of barrier function and cell-cell interactions under controlled conditions. | More complex and expensive to set up than static models. |
| AI-Powered In Vivo Screening (e.g., Manifold Bio's mDesign) | Uses barcoded protein libraries screened in live animals; AI learns from real physiological data [19]. | High-throughput, predictive screening of thousands of potential "brain shuttle" constructs in a physiological environment. | Cutting-edge technology, not yet widely available; requires specialized expertise. |
FAQ: Therapeutic Strategies and Troubleshooting
Q6: What are the most promising strategies for delivering therapeutics across the BBB?
Strategies can be classified as passive or active targeting, with active and disruption-based methods showing the most promise for large molecules.
Table 2: Promising Strategies for Delivering Therapeutics Across the BBB
| Strategy | Mechanism | Therapeutic Payload | Development Stage |
|---|---|---|---|
| Receptor-Mediated Transcytosis (RMT) | Uses ligands (antibodies, peptides) to bind receptors (TfR, insulin receptor) on BBB, hijacking natural transport [15] [20] [4]. | Antibodies, proteins, oligonucleotides [20] [16]. | Clinical/Commercial (e.g., JCR Pharma's Hunter syndrome drug) [20]. |
| Biomimetic Nanoparticles | Synthetic nanoparticles disguised with natural membranes (e.g., RBCs, leukocytes, stem cells) to evade immune system and target inflammation [21] [22]. | Small molecule drugs, nucleic acids, proteins. | Preclinical research (e.g., platelet膜纳米颗粒 for stroke) [21]. |
| Cell-Mediated "Trojan Horse" | Uses living cells (e.g., immune cells) that naturally traverse the BBB to carry therapeutic cargo [15] [18]. | Various, including neurotrophic factors. | Preclinical research. |
| Focused Ultrasound (FUS) | Temporarily and reversibly disrupts BBB tight junctions using ultrasound waves, often with microbubbles [15]. | Antibodies, chemotherapy. | Clinical trials. |
| Viral Vectors | Engineered viruses (e.g., AAV) modified to target BBB receptors for gene delivery [15] [20]. | Gene therapies, CRISPR-Cas9 [15]. | Preclinical and early clinical trials. |
Q7: Our therapeutic antibody shows excellent target engagement in vitro but no efficacy in vivo. What could be wrong?
This common issue almost always points to a BBB delivery failure. Potential solutions and investigations include:
- Quantify Brain Uptake: Measure the actual concentration of the antibody in the brain parenchyma after systemic administration. It is likely extremely low (<0.1% of injected dose) [20].
- Employ a "Brain Shuttle": Re-engineer the antibody by fusing it to a ligand that binds a highly expressed BBB receptor, such as the transferrin receptor (TfR). This engages receptor-mediated transcytosis (RMT) to actively ferry the antibody across the endothelial cells. Roche's Trontinemab, a TfR-targeting anti-amyloid antibody, showed 3-fold greater plaque clearance efficiency at one-fifth the dose of its unmodified counterpart [20].
- Leverage AI for Design: Consider using advanced platforms like Manifold Bio's mDesign, which uses in vivo screening and AI to design highly effective BBB-shuttling components, optimizing for real-world physiological conditions [19].
- Check for Efflux: While more common for small molecules, ensure your antibody is not being actively exported by efflux transporters at the BBB.
Q8: We are using nanoparticle carriers, but they are being cleared by the immune system before reaching the brain. How can we improve their circulation time?
This is a key challenge in nanomedicine. The most effective strategy is to use biomimetic camouflage.
- PEGylation: Coating nanoparticles with polyethylene glycol (PEG) creates a "stealth" layer that reduces protein adsorption and recognition by immune cells, prolonging circulation [21] [22].
- Cell Membrane Coating: Wrapping nanoparticles in membranes derived from red blood cells (RBCs) is highly effective. The RBC membrane displays "self-markers" like CD47, which signals immune cells to avoid phagocytosis, significantly reducing clearance [21] [22]. Other membranes, such as those from leukocytes or platelets, can also provide immune evasion while adding active targeting capabilities to inflamed brain endothelium [21].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for BBB and Neurodegenerative Disease Research
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| BBB In Vitro Model Kits | To establish a human-relevant barrier for permeability and mechanistic studies. | Commercially available primary human brain microvascular endothelial cells, pericytes, and astrocytes. Microfluidic "BBB-on-chip" kits are also emerging. |
| Ligands for RMT | To functionalize therapeutics or carriers for active BBB crossing. | Transferrin Receptor (TfR) binders: Monoclonal antibodies or binding peptides. RVG29 peptide: Binds neuronal acetylcholine receptor for neuronal targeting [21] [22]. Angiopep-2: Targets LRP1 receptor on BBB [22]. |
| Biomimetic Coating Materials | To create "stealth" and targeted nanoparticles with improved pharmacokinetics. | PEG-lipids for PEGylation [22]. Isolated cell membranes from RBCs, leukocytes, or platelets [21] [22]. Recombinant ApoE for lipoprotein-mimicking nanoparticles targeting BBB receptors [22]. |
| Blood-Based Biomarker Assays | For non-invasive diagnosis and monitoring of BBB dysfunction and neurodegeneration. | Commercial immunoassays (ELISA, SIMOA) for p-tau181, p-tau217, GFAP, NfL. FDA-cleared blood tests like Lumipulse G (p-tau217/Aβ42 ratio) [17]. |
| Viral Vectors for CNS Gene Delivery | To deliver genetic material (e.g., CRISPR-Cas9, ASOs, therapeutic genes) to the brain. | Adeno-associated virus (AAV) serotypes with tropism for the CNS (e.g., AAV9, AAV-PHP.eB). Engineered AAVs with capsids modified to enhance BBB transit (e.g., via TfR targeting) [15] [20]. |
Visualizing Key Pathways and Workflows
The following diagrams illustrate core concepts and experimental workflows in BBB research.
Diagram 1: BBB Dysfunction in Neurodegeneration
This diagram summarizes the key pathological mechanisms of BBB breakdown in diseases like Alzheimer's.
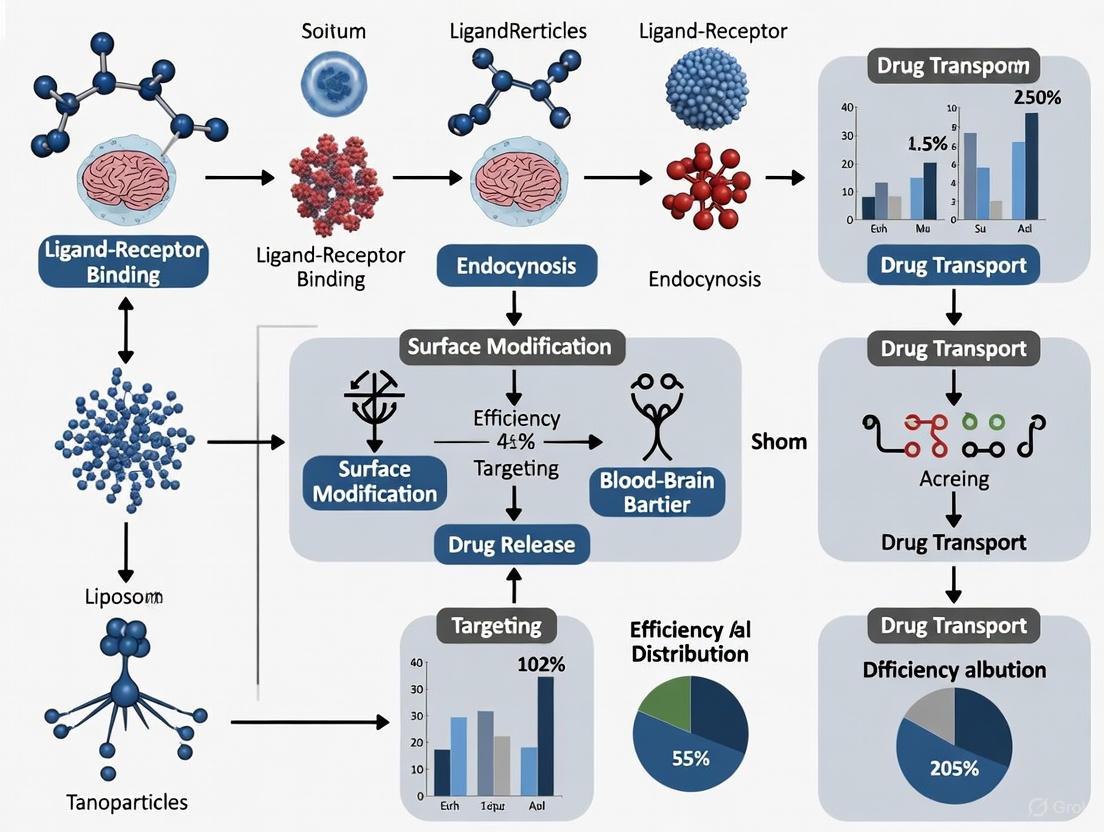
Diagram 2: Drug Delivery Strategies Workflow
This flowchart outlines the decision-making process for selecting a BBB drug delivery strategy based on the therapeutic payload.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary natural transport mechanisms for crossing the BBB that can be exploited for drug delivery?
The blood-brain barrier (BBB) has several innate transport pathways that can be co-opted for drug delivery [3] [4]:
- Receptor-Mediated Transcytosis (RMT): This mechanism allows large molecules to cross the BBB by binding to specific receptors on the endothelial cell surface, such as the transferrin receptor or insulin receptor. The molecule is engulfed in a vesicle and transported across the cell [15] [23].
- Carrier-Mediated Transport (CMT): This system uses protein carriers to shuttle essential small molecules, such as glucose and amino acids, across the BBB. Drugs structurally similar to these nutrients can use these transporters [4] [23].
- Adsorptive-Mediated Transcytosis (AMT): This is a non-specific charge-based interaction where positively charged molecules (cationic proteins or cell-penetrating peptides) interact with the negatively charged cell membrane, triggering vesicle formation and transport across the endothelium [4].
FAQ 2: My engineered nanoparticles show good binding to BBB receptors in vitro but poor brain uptake in vivo. What could be the issue?
This common problem can arise from several factors [15] [24]:
- Protein Corona Formation: Upon intravenous administration, nanoparticles can be coated with serum proteins, which may mask the targeting ligands and prevent receptor recognition.
- Rapid Clearance by the Reticuloendothelial System (RES): Nanoparticles may be sequestered by the liver and spleen before reaching the brain.
- Insufficient Ligand Density or Binding Affinity: The number of targeting molecules on the nanoparticle surface or their strength of binding may be insufficient to compete with natural ligands.
- Off-Target Binding: The targeting ligand may bind to its receptor on other tissues, reducing the dose available for BBB crossing.
FAQ 3: How can I determine if my drug is a substrate for efflux pumps like P-glycoprotein (P-gp)?
Several experimental approaches can identify efflux pump substrates [25] [23]:
- In Vitro Transport Assays: Use cultured brain endothelial cell monolayers. Measure the bidirectional permeability (A-to-B vs. B-to-A) of your drug. A significantly higher B-to-A flux suggests active efflux.
- Inhibition Studies: Co-incubate the drug with a known efflux pump inhibitor (e.g., verapamil for P-gp). A subsequent increase in A-to-B permeability or brain uptake confirms involvement of that transporter.
- In Vivo Studies in Knockout Animals: Compare the brain concentration of the drug in wild-type mice versus mice lacking the specific efflux transporter gene (e.g., Mdr1a/b-/- for P-gp). A higher concentration in the knockout animals indicates the drug is an efflux substrate.
FAQ 4: What are the key considerations when choosing a ligand for receptor-mediated transcytosis?
Selecting an appropriate ligand is critical for success [15] [11]:
- Receptor Specificity and Expression: The receptor should be highly and exclusively expressed on the BBB endothelium to minimize off-target effects.
- Ligand Affinity: The ligand should have high affinity for the receptor, but not so high that it prevents the release of the cargo on the abluminal (brain) side.
- Immunogenicity: Antibody-based ligands may trigger immune responses. Smaller peptide ligands or antibody fragments (e.g., scFv) are often less immunogenic.
- Cargo Capacity: The receptor-ligand system must be able to internalize and transport the size and type of your drug cargo (e.g., small molecule, protein, or nanoparticle).
Troubleshooting Guides
Problem: Low Transcytosis Efficiency Despite High Cellular Uptake
Symptoms*: Your targeted delivery system shows good internalization into brain endothelial cells in vitro, but the cargo fails to appear in the brain parenchyma in vivo. The cargo seems trapped within the cells.
| Possible Cause | Diagnostic Experiments | Potential Solutions |
|---|---|---|
| Lysosomal Trapping/Degradation | - Use lysotracker dyes to check co-localization with lysosomes.- Measure cargo integrity after cellular uptake. | - Incorporate endosomolytic peptides or polymers (e.g., pH-sensitive histidine-rich peptides) to promote endosomal escape [11].- Use ligands that traffic through non-degradative pathways. |
| Inefficient Vesicle Trafficking | - Use live-cell imaging to track vesicle movement.- Inhibit key trafficking proteins (e.g., with dynamin inhibitors) and measure the effect on transcytosis. | - Optimize ligand properties (size, valency) to steer vesicle fate towards transcytosis rather than recycling [3]. |
| Ligand-Receptor Complex Does Not Dissociate | - Use surface plasmon resonance (SPR) to measure binding kinetics at different pH levels.- Check if the ligand is recycled back to the luminal surface. | - Engineer ligands with pH-sensitive binding that release the receptor in the slightly more acidic endosomal environment [15]. |
Problem: Nanoparticle Toxicity and Immunogenicity
Symptoms*: In vivo experiments show signs of inflammation, activation of immune cells, or toxicity in the liver and spleen.
| Possible Cause | Diagnostic Experiments | Potential Solutions |
|---|---|---|
| Material Biocompatibility | - Test different nanoparticle materials for in vitro cell viability (MTT assay).- Check for complement activation in serum. | - Switch to biodegradable and biocompatible materials (e.g., PLGA, lipids, chitosan) [14] [24].- Use PEGylation to create a "stealth" coating and reduce immune recognition. |
| Ligand-Induced Immune Response | - Screen for anti-ligand antibodies in serum after repeated administration.- Measure cytokine levels (e.g., TNF-α, IL-6). | - Use humanized antibodies or fully human ligands to reduce immunogenicity.- Consider using small peptide ligands instead of full antibodies. |
| Oxidative Stress | - Measure reactive oxygen species (ROS) production in treated cells.- Check markers of oxidative stress in tissues (e.g., lipid peroxidation). | - Co-incorporate antioxidants (e.g., curcumin, resveratrol) into the nanoparticle formulation [14]. |
Quantitative Data Tables
Table 1: Key Natural Transport Pathways at the BBB
| Transport Mechanism | Physiological Function | Engineered Ligand/Targeting Moelty | Typical Payload Size | Key Limitations |
|---|---|---|---|---|
| Receptor-Mediated Transcytosis (RMT) | Uptake of large proteins (e.g., insulin, transferrin). | Anti-TfR antibody, Angiopep-2 (targeting LRP1), RI7217 (targeting TfR). | Antibodies, nanoparticles, proteins. | Potential competition with endogenous ligands; risk of saturating natural pathways [15] [3]. |
| Carrier-Mediated Transport (CMT) | Transport of essential nutrients (e.g., glucose, amino acids). | Levodopa (via LAT1), modified nucleosides. | Small molecules (< 500 Da). | Highly specific to substrate structure; limited to small molecules [25] [23]. |
| Adsorptive-Mediated Transcytosis (AMT) | Not a natural physiological pathway for specific molecules. | Cationic proteins (e.g., albumin), cell-penetrating peptides (e.g., TAT). | Proteins, nanoparticles, nucleic acids. | Low specificity; potential cytotoxicity due to non-specific membrane interaction [4]. |
Table 2: Comparison of Nanocarrier Platforms for Exploiting Natural Transport
| Nanocarrier Type | Material Examples | Compatible Transport Mechanisms | Key Advantages | Key Challenges |
|---|---|---|---|---|
| Lipid-Based | Liposomes, Solid Lipid Nanoparticles (SLNs), Lipid Nanoparticles (LNPs). | RMT, AMT. | High biocompatibility and biodegradability; high drug loading capacity [4] [24]. | Potential stability issues in circulation; batch-to-batch variability. |
| Polymeric | PLGA, Chitosan, PEG. | RMT, AMT. | Controlled release kinetics; surface easily functionalized [14]. | Risk of polymer-associated toxicity; degradation products must be non-toxic. |
| Biological | Exosomes, Albumin Nanoparticles. | Innate RMT (if derived from specific cells). | Low immunogenicity; natural targeting capabilities [15] [6]. | Difficulties in large-scale production and drug loading. |
Experimental Protocols
Protocol 1: In Vitro Assessment of RMT Using a BBB Co-culture Model
Objective*: To evaluate the transcytosis efficiency and pathway of a ligand-decorated nanoparticle across a simulated BBB.
Materials*:
- Cell Culture: Primary human brain microvascular endothelial cells (HBMECs), pericytes, and astrocytes.
- Transwell Plates: (e.g., 12-well, 3.0 µm pore size).
- Targeted Nanoparticles: Your ligand-decorated nanoparticles and non-targeted controls.
- Inhibitors: Chlorpromazine (clathrin-mediated endocytosis inhibitor), Filipin (caveolae-mediated endocytosis inhibitor), excess free ligand (for competitive inhibition).
Procedure*:
- Model Establishment: Seed HBMECs on the apical side of the Transwell insert. Culture pericytes and astrocytes on the basolateral side to create a neurovascular unit co-culture. Allow the model to mature for 5-7 days, monitoring Trans-Endothelial Electrical Resistance (TEER) until it exceeds 150 Ω·cm² [23].
- Transport Assay:
- a. Replace the medium in both compartments with fresh pre-warmed buffer.
- b. Add your nanoparticle suspension to the apical (donor) compartment.
- c. At predetermined time points (e.g., 30, 60, 120 min), collect small samples from the basolateral (acceptor) compartment and replace with fresh buffer.
- d. Measure the concentration of nanoparticles or their cargo in the samples using a relevant method (e.g., fluorescence, HPLC).
- Inhibition Studies: Pre-incubate the HBMECs with the various inhibitors for 30-60 minutes before repeating step 2. A significant reduction in transport with a specific inhibitor indicates the primary pathway used.
- Data Analysis: Calculate the apparent permeability coefficient (Papp) and the percentage of transported dose. Compare targeted vs. non-targeted and inhibited vs. non-inhibited conditions.
Protocol 2: Validating Efflux Pump Interaction
Objective*: To determine if a new chemical entity (NCE) is a substrate for P-glycoprotein (P-gp).
Materials*:
- In Vitro System: MDCKII or LLC-PK1 cell lines overexpressing human MDR1 (P-gp).
- Test Compound: Your NCE, with a known P-gp substrate (e.g., digoxin) as a positive control.
- Inhibitor: A specific P-gp inhibitor like zosuquidar (LY335979) or verapamil.
- LC-MS/MS or other sensitive analytical equipment for compound quantification.
Procedure*:
- Cell Seeding: Seed MDR1-transfected cells on Transwell filters and culture until a confluent monolayer with high TEER is formed.
- Bidirectional Transport:
- a. A-to-B Direction: Add the NCE to the apical compartment and measure its appearance in the basolateral compartment over time.
- b. B-to-A Direction: Add the NCE to the basolateral compartment and measure its appearance in the apical compartment over time.
- Inhibition: Repeat the bidirectional transport assay in the presence of a P-gp inhibitor added to both compartments.
- Data Analysis:
Signaling Pathways and Workflows
Diagram 1: Receptor-Mediated Transcytosis (RMT) Pathway
Diagram 2: Drug Delivery System Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Natural Transport Mechanisms
| Reagent / Tool | Function / Application | Example Supplier / Catalog (for reference) |
|---|---|---|
| hCMEC/D3 Cell Line | Immortalized human brain endothelial cell line for in vitro BBB models. | Merck (formerly Sigma-Aldrich) |
| Anti-Human TfR Antibody | Ligand for targeting the Transferrin Receptor (TfR) in RMT studies. | BioLegend (clone #289108) or R&D Systems |
| Angiopep-2 Peptide | A peptide ligand that targets the LRP1 receptor on the BBB. | Tocris Bioscience (Cat. # 7313) or custom peptide synthesis companies. |
| P-glycoprotein (P-gp) Inhibitors (e.g., Zosuquidar, Verapamil) | To chemically inhibit P-gp efflux activity in transport assays. | Tocris Bioscience (Zosuquidar, Cat. # 4453) |
| MDCKII-MDR1 Cells | Canine kidney cells overexpressing human P-gp for standardized efflux assays. | Netherlands Cancer Institute (NKI) or commercial providers. |
| Dylight 650 NHS Ester | Fluorescent dye for labeling antibodies, peptides, or nanoparticles for tracking. | Thermo Fisher Scientific |
| CLIP-tag / SNAP-tag Technology | Enzyme-based protein labeling systems for site-specifically labeling targeting ligands. | New England Biolabs (NEB) |
| Poly(D,L-lactide-co-glycolide) (PLGA) | Biodegradable polymer for fabricating nanoparticles for drug encapsulation. | Lactel Absorbable Polymers (DURECT Corporation) |
| Lipoid S100 | Phosphatidylcholine from soybean lecithin for formulating liposomes and lipid nanoparticles. | Lipoid GmbH |
Breaking Through: A Toolkit of Advanced BBB Crossing Technologies
Troubleshooting Guides
Troubleshooting Low Brain Delivery Efficiency
Problem: Your RMT-targeting construct shows insufficient brain accumulation despite high plasma concentration.
| Possible Cause | Diagnostic Experiments | Potential Solutions |
|---|---|---|
| Low RMT receptor affinity | Perform Surface Plasmon Resonance (SPR) to measure binding affinity (KD). Compare to positive controls (e.g., TfR antibody with KD ~1-10 nM) [26]. | Affinity maturation via phage display or yeast display libraries. Optimize binding valency (e.g., bivalent vs. monovalent) [26] [27]. |
| Lysosomal degradation | Co-localization studies using immunofluorescence staining for LAMP1/LAMP2 (lysosomal markers) in brain endothelial cells [28]. | Engineer pH-dependent binding to dissociate from the receptor in early endosomes, promoting transcytosis over recycling/degradation [28] [26]. |
| High off-target binding | Quantitative biodistribution study in peripheral tissues (e.g., liver, spleen) [26]. | Select brain-enriched RMT targets (e.g., CD98hc, Basigin). Use antibodies with lower peripheral organ uptake profiles [26]. |
| Inefficient endocytosis | Measure cellular internalization kinetics using flow cytometry or confocal microscopy in hCMEC/D3 cells (human brain endothelial cell line) [28]. | Screen multiple antibody clones against different epitopes on the RMT receptor to identify those promoting efficient clathrin-mediated endocytosis [28]. |
Troubleshooting Safety and Toxicity Issues
Problem: Observed peripheral toxicity or unexpected pharmacological effects during in vivo studies.
| Possible Cause | Diagnostic Experiments | Potential Solutions |
|---|---|---|
| TfR-mediated erythrocyte depletion | Complete blood count (CBC) analysis, particularly monitoring reticulocyte counts [26]. | Engineer anti-TfR antibodies with reduced FcγR binding (e.g., aglycosylated Fc) to minimize effector function on red blood cells [26]. |
| IR/IGF1R-mediated metabolic effects | Frequent blood glucose monitoring during and after antibody infusion [26]. | Use lower affinity anti-IR antibodies (ED50 ~0.25-0.5 nM) and administer with dextrose supplementation [26]. |
| Target-mediated peripheral drug disposition | Compare plasma pharmacokinetics in wild-type vs. receptor-knockout mice [26]. | Optimize dosing regimen (e.g., higher dose, less frequent administration) to saturate peripheral sinks. |
| Immune activation (e.g., ARIA in AD) | MRI monitoring for amyloid-related imaging abnormalities (ARIA) [27]. | Optimize antibody dose and infusion protocol; consider pre-treatment with anti-inflammatory agents. |
Frequently Asked Questions (FAQs)
Q1: What are the key advantages and disadvantages of TfR, CD98hc, and IGF1R as RMT targets?
- TfR (Transferrin Receptor):
- Advantages: High expression on BBB; well-validated with multiple clinical candidates (e.g., Denali's TV platform, JR-141) [26] [27].
- Disadvantages: High peripheral expression (e.g., liver, spleen) causing off-target effects; potential for reticulocyte depletion; expression may decrease in aged or diseased brain [26].
- CD98hc:
- Advantages: Identified via omics as highly expressed on mouse BECs; antibodies show significant brain enrichment [26].
- Disadvantages: Less clinical validation compared to TfR; broader biological functions may complicate safety profile.
- IGF1R (Insulin-like Growth Factor 1 Receptor):
- Advantages: Slightly more abundant BBB expression compared to TfR; successful application in bispecific antibodies (e.g., SAR446159/ABL301 for Parkinson's) [26] [29].
- Disadvantages: Potential for metabolic side effects similar to IR, though engineered VHHs (e.g., IGF1R4) can achieve dose-dependent responses [26].
Q2: How do I validate successful transcytosis versus simple endothelial cell binding and uptake?
A multi-step validation workflow is crucial [28] [26]:
- In vitro BBB models: Use a validated transwell system with human brain endothelial cells (e.g., hCMEC/D3). Measure apparent permeability (Papp) and compare to negative controls. Inhibit key RMT pathways (e.g., with receptor-blocking antibodies) to confirm specificity.
- Cellular trafficking studies: Perform immunofluorescence co-localization with endosomal (EEA1, RAB5), recycling (RAB11), and lysosomal (LAMP1) markers to track the intracellular journey.
- In vivo brain uptake measurement: After intravenous injection in mice, calculate the %Injected Dose per gram of brain (%ID/g) at multiple time points. A value significantly higher than a non-targeting control antibody (e.g., >0.5-1% ID/g) indicates successful transport.
- Perfusion: Perfuse animals with buffer prior to brain collection to remove blood pool antibody, ensuring measurement of parenchymal delivery rather than vascular binding.
Q3: What is the impact of binding affinity on RMT efficiency? Is higher affinity always better?
No, higher affinity is not always better. The relationship between affinity and brain uptake often follows a "sweet spot" [26]:
- Very High Affinity: Can cause the "binding site barrier" effect, where the antibody is sequestered on the luminal side of the BBB and does not release into the brain parenchyma.
- Very Low Affinity: Fails to efficiently engage the receptor for endocytosis.
- Optimal Affinity: Typically in the low nanomolar range (e.g., 1-10 nM), allowing for efficient receptor engagement, internalization, and subsequent release within the endosomal system or at the abluminal side. Affinity must be optimized for each specific RMT target and antibody format.
Q4: Which antibody formats are most suitable for RMT-based delivery?
The choice depends on the therapeutic cargo and desired pharmacokinetics [26]:
- Full-length IgGs: Suitable for fusing to protein therapeutics (e.g., enzyme replacement therapies like valanafusp alpha). The Fc domain can be engineered to reduce effector function.
- Single-chain variable fragments (scFvs) and VHHs (nanobodies): Smaller size may improve tissue penetration. Often used as the targeting moiety in bispecific antibodies (e.g., the IGF1R-targeting scFv in SAR446159) [29].
- Bispecific Antibodies: One arm targets the RMT receptor (e.g., TfR, IGF1R), while the other arm engages the therapeutic target in the brain (e.g., α-synuclein, BACE1) [27] [29]. This is the most common format for delivering therapeutic antibodies across the BBB.
Table 1: Key Quantitative Data for Featured RMT Targets and Reagents
| RMT Target | Representative Agent / Format | Key Quantitative Metric | Value / Affinity | Reference / Context |
|---|---|---|---|---|
| TfR | Pabinafusp alfa (JR-141) | Clinical Outcome | Approved in Japan for MPS-II (Hunter syndrome) | [26] |
| TfR | Denali TfR Transport Vehicle (TV) | Brain Uptake (%ID/g) | High concentration and broad distribution in rodent and NHP brains | [26] |
| IR | AGT-181 (Valanafusp alpha) | Binding Affinity (ED50) | 0.25 - 0.5 nM | [26] |
| IR | AGT-181 | Clinical Dosing | 0.3 - 6 mg/kg in trials (with nutritional supplements) | [26] |
| IGF1R | VHH IGF1R4 | Functional Response | Dose-dependent, pharmacologically relevant response to galanin | [26] |
| IGF1R | SAR446159 (1E4 + IGF1R scFv) | Binding Affinity (to α-Syn PFFs) | Sub-picomolar (approaching SPR limit) | [29] |
| General BBB | Typical Antibody | Brain Uptake (%ID/g) | ~0.1 - 0.5% | [29] |
Table 2: Essential Research Reagent Solutions for RMT Experiments
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| hCMEC/D3 Cell Line | An immortalized human brain endothelial cell line for in vitro BBB models and transcytosis assays. | Requires specific culture conditions and coating (collagen I & fibronectin). Can form relatively tight monolayers. |
| Anti-TfR Antibodies (various clones) | To target the transferrin receptor for RMT. Used as positive controls or building blocks for bispecifics. | Clone selection is critical; different clones have vastly different transcytosis capabilities and potential for toxicity. |
| Anti-IGF1R VHHs (e.g., IGF1R4) | Single-domain antibodies for targeting IGF1R. Can be engineered into bispecific formats. | Offer potential for high brain uptake and reduced side effects compared to some anti-TfR approaches. |
| Anti-CD98hc Antibodies | To target the CD98 heavy chain, an emerging RMT target identified via omics. | Show significant brain enrichment in preclinical models; useful for exploring novel pathways. |
| Recombinant α-Syn Preformed Fibrils (PFFs) | For in vitro and in vivo modeling of synucleinopathies when testing therapeutics like SAR446159. | Essential for testing the functional efficacy of delivered therapeutics in disease-relevant models. |
| LAMP1 / LAMP2 Antibodies | Lysosomal markers for immunofluorescence to assess if RMT cargo is being degraded vs. transcytosed. | Crucial for troubleshooting low brain delivery efficiency. |
| RAB5 / RAB11 Antibodies | Markers for early endosomes and recycling endosomes, respectively. Used to track intracellular trafficking. | Helps map the intracellular route of the RMT cargo and identify trafficking bottlenecks. |
Experimental Protocols
Protocol:In VitroTranscytosis Assay Using hCMEC/D3 Cells
This protocol measures the ability of an RMT-targeting antibody to cross a monolayer of human brain endothelial cells [28] [26].
Materials:
- hCMEC/D3 cells (passage 25-35)
- Collagen I (rat tail), fibronectin
- EGM-2 MV culture medium
- 12-well or 24-well transwell plates (polycarbonate membranes, pore size)
- Hanks' Balanced Salt Solution (HBSS)
- Test articles: RMT-targeting antibody, isotype control antibody
- Anti-human IgG antibody for ELISA quantification
Procedure:
- Coating: Coat transwell inserts with collagen I (150 µg/mL) and fibronectin (10 µg/mL) in PBS for 2 hours at 37°C.
- Cell Seeding: Trypsinize hCMEC/D3 cells and seed onto the apical (upper) chamber of the coated inserts at a density of 50,000-100,000 cells/cm². Maintain the cells for 5-7 days, changing the medium every 2 days, to form a confluent, polarized monolayer.
- Integrity Check: Measure the Trans-Endothelial Electrical Resistance (TEER) using a volt-ohm meter. Accept only monolayers with TEER >30 Ω·cm² for the assay.
- Assay Setup: Warm HBSS to 37°C. Replace the medium in both apical and basolateral chambers with pre-warmed HBSS. Incubate for 30 min.
- Dosing: Add the test antibody (e.g., 10 µg/mL) to the apical chamber (donor compartment). The basolateral chamber serves as the receiver (acceptor compartment).
- Incubation: Place the plate in a 37°C incubator with 5% CO₂. Gently shake the plate on an orbital shaker (50-100 rpm).
- Sampling: At predetermined time points (e.g., 30, 60, 120 min), remove a sample (e.g., 100 µL) from the basolateral chamber. Replace with an equal volume of fresh pre-warmed HBSS.
- Quantification: Determine the concentration of the test antibody in the basolateral samples using a specific ELISA (e.g., using an anti-human IgG capture antibody).
- Data Analysis: Calculate the Apparent Permeability (Papp) using the formula: Papp (cm/s) = (dQ/dt) / (A * C₀) where dQ/dt is the transport rate (µg/s), A is the surface area of the membrane (cm²), and C₀ is the initial concentration in the donor chamber (µg/mL).
Protocol: Validating Brain Uptake and PharmacodynamicsIn Vivo
This protocol outlines the key steps to validate the in vivo efficacy of an RMT-delivered therapeutic, such as an α-synuclein aggregate-binding antibody [29].
Materials:
- Wild-type or disease model mice (e.g., α-syn PFF-injected mice)
- Test articles: RMT-bispecific antibody (e.g., SAR446159), non-targeting control antibody
- Saline for injection
- Heparinized capillary tubes and/or EDTA-coated tubes for blood collection
- Perfusion pump and PBS
- Tissue homogenizer
Procedure:
- Dosing: Administer a single intravenous bolus injection of the test antibody (typical dose: 5-30 mg/kg) via the tail vein. Include a group injected with a non-targeting control antibody.
- Blood Collection: At specified time points post-injection (e.g., 5 min, 1h, 6h, 24h), collect blood samples via retro-orbital bleeding or cardiac puncture. Centrifuge to obtain plasma. Store at -80°C until analysis.
- Terminal Perfusion and Tissue Collection: At the end of the study (e.g., 24h), deeply anesthetize the animals. Perfuse transcardially with 20-30 mL of ice-cold PBS to clear the brain vasculature of blood.
- Brain Harvesting: Decapitate the animal and rapidly remove the brain. Weigh the whole brain or dissect into regions of interest (e.g., cortex, striatum, midbrain). Snap-freeze in liquid nitrogen.
- Tissue Homogenization: Homogenize brain tissues in a suitable buffer (e.g., RIPA buffer with protease inhibitors) at a consistent weight/volume ratio (e.g., 1:4 w/v). Centrifuge the homogenate to obtain a clear supernatant.
- Bioanalysis:
- Antibody Concentration: Quantify the concentration of the human antibody in both plasma and brain homogenate using a specific sandwich ELISA. Calculate the %Injected Dose per gram of brain tissue (%ID/g).
- Pharmacodynamic Readout: Depending on the therapeutic target, perform additional assays on the brain homogenate. For an α-synuclein antibody like SAR446159, this could be:
- ELISA: Measure levels of specific forms of α-syn (e.g., phosphorylated, oligomeric).
- Western Blot: Analyze changes in α-syn aggregation state.
- Immunohistochemistry: Assess clearance of pathological aggregates and reduction in pathology score.
- Data Analysis: Compare brain uptake (%ID/g) and pharmacodynamic effects between the RMT-bispecific group and the control group to demonstrate target engagement and therapeutic efficacy.
Signaling Pathways and Workflows
Diagram 1: The RMT Pathway and Key Engineering Decision Points. This diagram visualizes the intracellular journey of an RMT-targeting antibody, highlighting the critical sorting decision in the early endosome that determines the success of transcytosis into the brain parenchyma versus recycling or degradation.
Diagram 2: RMT Antibody Development and Validation Workflow. This flowchart outlines the key experimental stages for developing an RMT-based therapeutic, integrating critical troubleshooting feedback loops for when experiments yield suboptimal results.
Core Design Principles for Effective BBB Shuttles
Bispecific antibody shuttles are engineered to overcome the fundamental challenge of the blood-brain barrier (BBB), which restricts over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from entering the central nervous system [15] [4]. Their design centers on harnessing endogenous transport pathways, primarily Receptor-Mediated Transcytosis (RMT), to facilitate active transport into the brain.
Table 1: Key Design Principles for Bispecific Antibody Shuttles
| Design Principle | Objective | Molecular Implementation | Rationale and Impact |
|---|---|---|---|
| Targeting RMT (e.g., TfR1) | Utilize natural BBB transport mechanisms | Engineered binding domain (e.g., single-chain variable fragment) against Transferrin Receptor 1 [30] | Enables active transport across the tightly joined endothelial cells of the BBB. |
| Affinity Optimization | Balance BBB penetration and target engagement | Moderate affinity (e.g., ~100 nM) for TfR1 to facilitate release after transcytosis [30] | High TfR1 affinity can trap the antibody on vascular endothelium or neurons, reducing therapeutic availability. |
| Binding Valency | Promote efficient transport and release | Monovalent binding to TfR1 [30] | Prevents bivalent cross-linking, which leads to lysosomal degradation and reduces brain exposure. |
| pH-Sensitive Binding | Enhance release within the acidic endosome | Engineering TfR1-binding domain to lose affinity at endosomal pH (~6.0) [30] | Promotes dissociation from TfR1 during transcytosis, freeing the antibody to engage its therapeutic target in the brain parenchyma. |
| Differential Affinity | Ensure correct cellular targeting | Higher affinity for the therapeutic target (e.g., Aβ) than for TfR1 [30] | Prevents the shuttle from being "captured" by TfR1-expressing cells instead of reaching its pathological target. |
The selection of the shuttle target is critical. The Transferrin Receptor 1 (TfR1) is the most clinically validated target for this purpose due to its high expression on brain capillary endothelial cells and well-characterized transcytosis pathway [30]. A leading example is trontinemab, an investigational Brainshuttle bispecific antibody that combines an amyloid-beta-binding antibody with a TfR1 shuttle module [31] [32].
The following diagram illustrates the primary mechanism of action for a TfR1-bispecific antibody shuttle.
Troubleshooting Common Experimental and Development Issues
Despite a rational design, developers often encounter specific challenges. Below is a guide to diagnosing and resolving these issues.
Table 2: Troubleshooting Guide for Bispecific Antibody Shuttles
| Problem | Potential Root Cause | Recommended Solution |
|---|---|---|
| Low Brain Penetration | Excessive affinity/avidity for TfR1 | Weaken TfR1-binding affinity; ensure monovalent, pH-sensitive binding [30]. |
| Incorrect TfR1 binding epitope | Screen TfR1-binding domains that do not compete with endogenous transferrin. | |
| High Peripheral Toxicity or Rapid Clearance | Uptake in TfR1-rich peripheral tissues (e.g., spleen, bone marrow) | Optimize TfR1 affinity to minimize peripheral binding while retaining brain uptake [30]. |
| Immunogenicity against the shuttle component | Implement humanization strategies and screen for pre-existing antibodies. | |
| Inefficient Target Engagement in Brain | Shuttle captured by TfR1 on neurons | Ensure therapeutic target affinity is significantly higher than TfR1 affinity [30]. |
| Instability or aggregation in CNS environment | Improve thermal and colloidal stability via formulation and protein engineering [33]. | |
| Product-Related Impurities (Aggregates, Fragments) | Inherent instability of the bispecific format | Optimize cell culture conditions and purification; use protein engineering to improve stability [33] [34]. |
| Incorrect chain pairing during expression | Utilize platform technologies like "Knobs-into-Holes" and "CrossMab" to enforce correct assembly [35]. | |
| Inconsistent In Vivo Efficacy | Limited penetration into target brain region | Consider that different shuttles may have varying distribution profiles; explore other RMT targets. |
| Animal model does not fully recapitulate human BBB biology | Validate findings in multiple, translationally relevant models. |
Detailed Experimental Protocol: Assessing Brain Uptake and Target Engagement
This protocol outlines the key steps for the production and preclinical validation of a bispecific antibody shuttle, from expression to functional analysis in vivo.
Experimental Workflow: From Gene to Functional Validation
Phase 1: Molecular Construction and Expression
- Step 1.1 – Vector Design: Clone genes encoding the variable domains for the therapeutic target (e.g., Aβ) and the BBB shuttle target (e.g., TfR1) into a single mammalian expression vector. Use a system that facilitates correct heavy and light chain pairing, such as Knobs-into-Holes for the Fc region and a common light chain or CrossMab technology for the Fab arms [35] [34].
- Step 1.2 – Transfection and Expression: Transfect the construct into a mammalian cell line, typically CHO (Chinese Hamster Ovary) cells, using methods like electroporation or lipid-based transfection. Maintain cells in a bioreactor under optimized conditions (temperature, pH, dissolved oxygen) to maximize yield and minimize aggregation [34] [35].
Phase 2: Downstream Purification
- Step 2.1 – Capture: Clarify the cell culture supernatant via centrifugation and filtration. Perform initial capture using Protein A affinity chromatography, which binds the antibody's Fc region [35].
- Step 2.2 – Polish: Due to the complex structure of bispecifics, a multi-step purification process is often necessary. Use additional chromatographic methods like ion exchange chromatography or hydrophobic interaction chromatography to remove product-related impurities like homodimers, fragments, and aggregates [34].
Phase 3: In Vitro Characterization
- Step 3.1 – Binding Affinity: Validate binding kinetics using Surface Plasmon Resonance (SPR). Determine the affinity (KD) for both the therapeutic target and TfR1. Confirm that the affinity for the therapeutic target is higher than for TfR1 [30] [34].
- Step 3.2 – Functional Assay: Employ an in vitro BBB model, such as a transwell system with a monolayer of brain endothelial cells (e.g., hCMEC/D3). Apply the bispecific antibody to the apical compartment and measure the rate of transcytosis to the basolateral side, comparing it to a control monoclonal antibody [30].
Phase 4: In Vivo Validation
- Step 4.1 – Dosing: Administer the bispecific antibody intravenously to animal models (e.g., transgenic mice for Alzheimer's disease) at a therapeutically relevant dose (e.g., 1-10 mg/kg). Include a control group receiving a conventional monospecific antibody [31].
- Step 4.2 – Tissue Collection: At predetermined time points post-dosing, euthanize the animals and collect plasma, whole brain, and peripheral organs. Perfuse animals with saline to remove blood from the vasculature and ensure measured brain concentrations represent parenchymal delivery.
Phase 5: Bioanalytical and Functional Analysis
- Step 5.1 – Quantify Brain Exposure: Homogenize brain tissue and quantify antibody concentration using a specific ELISA that detects the bispecific format. Calculate the brain-to-plasma ratio to demonstrate enhanced penetration over conventional antibodies [30].
- Step 5.2 – Assess Target Engagement: For an anti-Aβ shuttle like trontinemab, use amyloid PET imaging or immunohistochemistry to quantify the reduction in plaque burden after repeated dosing. In clinical studies, a reduction below the 24 centiloid threshold is a key metric of efficacy [31] [32].
- Step 5.3 – Monitor Safety: Routinely conduct MRI scans to monitor for Amyloid-Related Imaging Abnormalities (ARIA), including ARIA-E (edema) and ARIA-H (microhemorrhages), which are known class effects of amyloid-lowering therapies [31] [36].
Frequently Asked Questions (FAQs)
Q1: Why is monovalent binding to TfR1 preferred for bispecific antibody shuttles? Monovalent binding prevents the antibody from cross-linking TfR1 receptors on the endothelial cell surface. Bivalent binding, with its higher avidity, often leads to the shuttle being trafficked to the lysosome for degradation rather than being transcytosed across the cell. Monovalent, medium-affinity binding optimizes the shuttle for release and delivery into the brain parenchyma [30].
Q2: What are the critical quality attributes (CQAs) to monitor during bispecific shuttle production? Beyond standard antibody CQAs, you must closely monitor:
- Correct Chain Association: Use assays to confirm the proper heterodimer formation and absence of homodimers.
- Binding Activity for Both Targets: Ensure both antigen-binding sites are functional and have the correct affinity.
- Aggregation and Fragmentation: These molecules can be prone to instability, so use size-exclusion chromatography (SEC) and capillary electrophoresis to monitor for aggregates and fragments [33] [34].
- Charge Variants: Analyze by imaged capillary isoelectric focusing (icIEF) to ensure product consistency.
Q3: Our shuttle shows excellent brain uptake in mice but fails in a higher species. What could be wrong? A common issue is a lack of cross-reactivity of the TfR1-binding domain. The shuttle's binding domain must be engineered to recognize TfR1 from the species used in your preclinical models and human TfR1. Always verify binding affinity and transcytosis efficiency in in vitro models expressing the human receptor before moving into clinical development [30].
Q4: How is clinical efficacy validated for a bispecific antibody shuttle in Alzheimer's disease? In clinical trials, efficacy is multi-faceted. For anti-amyloid shuttles like trontinemab, key endpoints include:
- Biomarker Efficacy: Rapid and significant reduction of amyloid plaques measured by amyloid PET (e.g., achieving amyloid-negative status) [31] [32].
- Clinical Efficacy: Slowing of cognitive and functional decline, measured by scales like the Clinical Dementia Rating–Sum of Boxes (CDR-SB), compared to placebo over 18 months [31] [36].
- Pharmacodynamic Effects: Reduction of downstream biomarkers like CSF/plasma pTau181 and pTau217 [31] [32].
Q5: What formulation strategies can improve the stability of bispecific antibody shuttles? BsAbs are often less stable than traditional mAbs. A proactive formulation strategy is essential:
- Early Developability Assessment: Screen for stability liabilities during candidate selection.
- Excipient Screening: Use high-throughput screening to identify optimal buffer conditions, pH, and stabilizers (e.g., sugars, surfactants, amino acids) that minimize aggregation and viscosity.
- Forced Degradation Studies: Subject the drug substance to stress conditions (e.g., thermal, mechanical) to identify degradation pathways and refine the formulation [33].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bispecific Shuttle Development
| Reagent / Material | Function in Development | Example & Notes |
|---|---|---|
| Mammalian Expression System | Produces correctly folded, glycosylated bispecific antibodies for research and pre-clinical use. | CHO (Chinese Hamster Ovary) Cells: Industry standard for therapeutic protein production due to proper post-translational modification [34] [35]. |
| Knobs-into-Holes Technology | Promotes correct heavy chain heterodimerization in IgG-like bispecifics, minimizing homodimer impurities. | A protein engineering technique that introduces complementary mutations in the CH3 domain of the Fc region [35]. |
| CrossMab Technology | Solves the light chain mispairing problem in IgG-like bispecifics by swapping domains between heavy and light chains. | A platform technology (Roche) that ensures the correct light chain pairs with its cognate heavy chain [35]. |
| Surface Plasmon Resonance (SPR) | Characterizes binding affinity (KD), kinetics (kon, koff), and specificity for both TfR1 and the therapeutic target. | Instruments like Biacore provide critical data for optimizing the affinity balance between the two targets [34]. |
| In Vitro BBB Model | Provides a high-throughput system for initial screening of shuttle transcytosis efficiency. | hCMEC/D3 Cell Line: A well-characterized human brain endothelial cell line that forms a fairly tight barrier when cultured on transwell filters [30]. |
| Anti-idiotype Antibodies | Enables the specific detection and quantification of the bispecific antibody in complex matrices like plasma and brain homogenate. | Custom-generated antibodies that bind to the unique paratope of the bispecific shuttle, essential for PK/PD studies [34]. |
Focused Ultrasound with Microbubbles for Targeted and Reversible BBB Disruption
Troubleshooting Guides
Table 1: Common Experimental Problems and Solutions
| Problem Category | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Insufficient BBB Opening | No gadolinium enhancement on T1w MRI post-FUS [37] | • Acoustic pressure too low [37]• Microbubble dose insufficient or expired [38]• Skull-induced attenuation/aberration [37] | • Systematically increase Peak Negative Pressure (PNP) within safe bounds (e.g., 0.2-0.6 MPa in mice) [39]• Titrate microbubble dose; confirm concentration and viability [38]• Use neuronavigation or MR-guidance for targeting; employ aberration correction algorithms [37] |
| Heterogeneous or patchy BBB opening [37] | • Unstable microbubble cavitation [37]• Inhomogeneous magnetic field during MRI [37] | • Implement Passive Cavitation Detection (PCD) for real-time feedback to maintain stable cavitation [39]• Perform MRI shimming and use quantitative T1 mapping sequences over qualitative T1-weighted imaging [37] [40] | |
| Safety & Tissue Damage | Microhemorrhages on SWI or T2* MRI [39] | • Inertial cavitation from excessive PNP [37]• Microbubble dose too high [38] | • Lower PNP immediately; use PCD to monitor for broadband emissions indicating inertial cavitation [39]• Reduce microbubble dose [38] |
| Hyperintensity on T2w MRI (indicating edema) [39] | • Inflammatory response to procedure [38]• Excessive mechanical energy deposition [37] | • Optimize acoustic parameters to minimize stable cavitation at high PNPs, particularly in disease models [39]• Consider animal sex; female mice show elevated pro-inflammatory markers post-FUS [38] | |
| Significant neuroinflammation | • Robust innate immune activation [41]• Multiple treatment sessions | • Monitor cytokine levels; multiple treatments may not increase pro-inflammatory markers and can elevate anti-inflammatory eNOS [38] | |
| Procedure & Delivery | Inconsistent drug delivery efficacy | • Poor temporal synchronization between FUS and drug/admin circulation [40]• Drug molecule size too large for the level of BBB opening [37] | • Inject therapeutic agent immediately before or during sonication [40]• Characterize BBB opening size (e.g., using different sized MR agents); FUS typically allows passage of particles <65 nm [37] |
| Unreliable BBB closure assessment | • Incorrect timing of post-procedure imaging [37] | • Perform T1w-CE MRI at multiple time points (e.g., immediately post, 4h, 24h) to confirm closure, which typically occurs within 4-6 hours [37] |
Table 2: Optimization Parameters for FUS-BBB Experiments
| Parameter | Typical Preclinical Range | Impact on Efficacy & Safety | Monitoring & Control Method |
|---|---|---|---|
| Peak Negative Pressure (PNP) | 0.2 - 0.6 MPa (mice) [39] | Efficacy: Higher PNP increases BBB opening volume/degree [39].Safety: High PNP risks inertial cavitation, microhemorrhages, edema [37] [39]. | • Passive Cavitation Detection (PCD) to avoid inertial cavitation (broadband emissions) [39].• Post-procedure T2w MRI and SWI for edema/bleeds [39]. |
| Microbubble Dose | Varies by type (e.g., 1x10^7 - 1x10^8 bubbles/kg) [38] | Efficacy: Sufficient dose is crucial for consistent opening [38].Safety: High dose drives pro-inflammatory cytokine response [38]. | • Titrate to minimum effective dose.• Measure inflammatory markers (e.g., cytokines) 24h post-treatment [38]. |
| Burst Length & PRF | e.g., 10 ms burst, 1-10 Hz PRF [37] | Efficacy: Magnitude of disruption decreases with shorter burst lengths [37].Safety: Longer bursts/ higher PRF may increase bioeffects. | • Keep pulse repetition frequency (PRF) and burst length constant once a safe, effective combination is found [37]. |
| Therapeutic Agent | Small molecules to biologics (1 kDa - 150 kDa) [40] | Efficacy: FUS enhances delivery rate (e.g., 4.6-fold for 1 kDa, 2.7-fold for 17 kDa molecules) [40]. Larger molecules may require higher PNP. | • Use quantitative T1 mapping to measure concentration of co-administered Gd-based tracer as surrogate [40]. |
Frequently Asked Questions (FAQs)
What is the most reliable method to confirm and quantify BBB opening in real-time?
A: While gadolinium enhancement on T1-weighted MRI is the gold standard for post-hoc confirmation [37], Passive Cavitation Detection (PCD) is critical for real-time assessment and control. PCD analyzes the acoustic emissions from oscillating microbubbles during sonication. Stable cavitation (characterized by harmonic and ultraharmonic signals) is associated with safe and effective BBB opening, while inertial cavitation (characterized by broadband noise) signals a high risk of vascular damage and microhemorrhages [39]. Implementing PCD feedback loops to maintain stable cavitation is the best practice for ensuring consistent and safe BBB opening.
How long does the BBB remain open after FUS+MB, and how do I verify it has closed?
A: The BBB opening is transient and typically closes within 4 to 6 hours in rodents, with integrity fully restored within 24 hours [37] [41]. To verify closure:
- Method: Use T1-weighted contrast-enhanced (T1w-CE) MRI.
- Protocol: Acquire images immediately after the procedure and again at 4-6 hours and 24 hours post-FUS. The disappearance of the hyperintense signal (gadolinium enhancement) at the target site confirms BBB closure [37]. A quantitative approach using T1 mapping can provide more precise data on contrast agent clearance over time [40].
Can FUS-BBB be safely applied to diseased brains with an already compromised BBB?
A: Evidence suggests yes, but with caution. Studies on cerebral cavernous malformation (CCM) models, which have abnormally permeable vasculature, show that FUS-MB can safely further enhance permeability without acutely inducing growth or bleeding [39] [40]. However, the diseased microenvironment may alter the response; for instance, CCM mice showed enhanced stable cavitation at higher PNPs [39]. It is crucial to:
- Conduct pilot studies to re-establish safe acoustic parameters for your specific disease model.
- Employ rigorous safety monitoring with SWI and T2w MRI post-treatment [39].
What are the primary causes of tissue damage, and how can they be mitigated?
A: The primary mechanisms are:
- Inertial Cavitation: The violent collapse of microbubbles causing vascular rupture and microhemorrhages. Mitigation: Use PCD to monitor and avoid broadband emissions by lowering PNP [37] [39].
- Inflammatory Response: The procedure can trigger a localized immune response. Mitigation: Optimize microbubble dose, as high doses are a key driver of pro-inflammatory cytokines [38]. Interestingly, multiple treatments may not be cumulative in terms of inflammation and can stimulate anti-inflammatory pathways [38].
- Oedema: Fluid buildup due to mechanical stress or inflammation. Mitigation: Avoid excessively high PNP, especially in repeat treatment regimens [39].
Are there sex-specific differences in the response to FUS-BBB opening?
A: Emerging data indicates yes. A 2025 study found that while the level of BBB disruption and microglia activation was similar between sexes, female mice showed significantly elevated levels of cytokine and chemokine markers 24 hours post-treatment compared to males [38]. This suggests that the inflammatory response to the procedure may be sex-dependent. Researchers should account for sex as a biological variable in experimental design and safety outcome analyses.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Equipment for FUS-BBB Research
| Item | Function & Role in FUS-BBB | Key Considerations |
|---|---|---|
| FUS System with PCD | Generates and focuses ultrasound waves; PCD monitors microbubble cavitation in real-time for safety and consistency [39]. | • Choose pre-clinical systems compatible with your animal model and MRI. • PCD capability is essential for feedback control. |
| Microbubble Contrast Agent | Intravenously injected agents that oscillate in the ultrasound field, mechanically disrupting tight junctions to open the BBB [37]. | • Use clinically approved types (e.g., Definity) for translational relevance. • Dose and concentration are critical variables for efficacy and inflammation [38]. |
| MRI Contrast Agent (Gadolinium-based) | Small molecules (e.g., MultiHance, ~1 kDa) that leak into brain parenchyma upon BBB opening, creating hyperintensity on T1-weighted MRI for visualization and quantification [37] [40]. | • Can also be used as a surrogate to measure delivery kinetics for small molecule drugs [40]. |
| High-Field MRI Scanner | Provides anatomical guidance for FUS targeting and is used with specific sequences to confirm BBB opening, assess safety, and quantify delivery [37]. | • Essential sequences: T1w-CE (efficacy), T2w (edema), SWI (microhemorrhages). • Quantitative T1 mapping is superior for precise concentration measurements [40]. |
Experimental Workflow & Protocol Diagrams
FUS-BBB Opening and Assessment Workflow
Cavitation Monitoring and Response Logic
Frequently Asked Questions (FAQs) & Troubleshooting Guides
This section addresses common challenges researchers face when developing and working with nanocarrier systems for drug delivery across the blood-brain barrier (BBB).
General Nanocarrier Development and Characterization
Q1: What is the optimal size range for nanocarriers to cross the BBB effectively?
A: The size of nanoparticles is critical for traversing the BBB. The ideal range is typically between 10 to 100 nanometers [42].
- Too Small (<5 nm): Nanoparticles smaller than 5 nm are likely to be rapidly cleared by the kidneys, reducing their circulation time [42].
- Too Large (>100 nm): Larger particles may have difficulty penetrating deeply into brain tissue. Studies show that 10 nm particles can be visualized in the brain, while 100 nm particles show deeper penetration in injured areas [42].
Q2: How does surface charge (zeta potential) influence nanocarrier performance?
A: The surface charge, measured as zeta potential, significantly impacts stability, cellular uptake, and biodistribution [43].
- High Positive or Negative Charge: A high zeta potential (typically > |±30| mV) helps prevent aggregation by creating strong electrostatic repulsion between particles, thereby improving colloidal stability [43].
- Cationic Surfaces: Positively charged nanocarriers often show enhanced cellular uptake through adsorptive-mediated transcytosis, as they interact electrostatically with the negatively charged cell membrane of BBB endothelial cells [44] [45]. However, highly positive charges can also lead to increased non-specific binding and toxicity.
Q3: Our nanocarriers are aggregating in solution. What are the primary causes and solutions?
A: Aggregation is a common issue often linked to surface properties and the environment.
- Low Zeta Potential: If the absolute value of the zeta potential is too low, electrostatic repulsion is insufficient to prevent aggregation. Consider modifying the surface chemistry to increase charge [43].
- Hydrophobicity: Highly hydrophobic surfaces can cause particles to aggregate in aqueous solutions. Solutions include:
- Improper Storage: Store nanocarrier dispersions at 4°C and avoid repeated freeze-thaw cycles. Brief sonication or vortexing before use can often re-disperse aggregates.
Targeting and Payload Delivery
Q4: What are the primary mechanisms for nanocarrier transport across the BBB?
A: Nanocarriers utilize several transcytosis pathways to cross the BBB endothelial cells [3] [4]:
- Receptor-Mediated Transcytosis (RMT): Nanocarriers are surface-functionalized with ligands (e.g., transferrin, insulin) that bind to specific receptors on the BBB, triggering internalization and transport. This is a highly selective and efficient strategy [46] [4].
- Adsorptive-Mediated Transcytosis (AMT): This relies on electrostatic interactions between cationic charges on the nanocarrier surface (e.g., from cell-penetrating peptides like PepH3) and the negatively charged glycocalyx on the endothelial cells [44] [45]. It is less specific but can achieve high uptake.
- Cell-Mediated Transcytosis: Utilizing cells, such as immune cells, that have inherent BBB crossing abilities to ferry nanocarriers into the brain [3].
Q5: We are encapsulating nucleic acid therapeutics (e.g., siRNA, ASOs). How can we improve their stability and delivery efficiency?
A: Nucleic acids are prone to nuclease degradation and have poor cellular uptake. Key strategies include:
- Chemical Modifications: Incorporate modifications into the nucleic acid structure itself, such as 2'-O-methyl (2'-OMe), 2'-fluoro (2'-F), phosphorothioate (PST) linkages, and locked nucleic acids (LNA) to dramatically enhance nuclease resistance and binding affinity [48].
- Protective Nanocarriers: Encapsulation within nanocarriers like exosomes, liposomes, or polymeric NPs provides a physical shield against degradation [48].
- Surface Functionalization: Conjugating targeting ligands (e.g., peptides, antibodies) to the nanocarrier surface promotes specific uptake into brain endothelial cells via RMT [46] [48].
Analytical and Technical Challenges
Q6: Which techniques are most suitable for characterizing the size and morphology of nanocarriers?
A: A combination of techniques is recommended for comprehensive characterization [43]:
- Dynamic Light Scattering (DLS): The primary technique for determining hydrodynamic diameter and polydispersity index (PDI) in solution. It is ideal for monomodal, spherical samples but can be unreliable for polydisperse or non-spherical particles without a prior fractionation step like asymmetrical flow field-flow fractionation (AF4) [43].
- Electron Microscopy (SEM/TEM): Provides direct, high-resolution images of nanoparticle morphology, size, and structure. Used to confirm results from DLS [43].
- Atomic Force Microscopy (AFM): Allows particle size measurement and topographic mapping with ultra-high resolution without the need for conductive coatings, making it suitable for delicate biological and polymeric nanocarriers [43].
Q7: Our in vitro BBB model shows low transcytosis efficiency. What factors should we check?
A: Low transcytosis can stem from multiple factors in your model system:
- Barrier Integrity: Confirm the formation of tight junctions by measuring transendothelial electrical resistance (TEER). A high TEER value indicates a intact, functional barrier [3].
- Cell Model Validation: Ensure your endothelial cells express the relevant receptors (e.g., transferrin receptor, insulin receptor) if you are using a ligand-mediated targeting approach [46].
- Nanocarrier Properties: Verify the size, charge, and ligand density of your nanocarriers. Aggregation or inappropriate surface chemistry can hinder transport.
- Experimental Conditions: Uptake and transcytosis are often temperature-dependent active processes. Ensure experiments are conducted at 37°C, as efficiency will be reduced at 4°C due to inhibited metabolic activity [44] [45].
Detailed Experimental Protocols
This section provides detailed methodologies for key experiments cited in recent literature.
Protocol: Preparation and Characterization of PepH3-Modified Niosomes
This protocol is adapted from research demonstrating enhanced BBB crossing using peptide-tagged nanocarriers [44] [45].
Aim: To formulate non-ionic surfactant vesicles (niosomes) tagged with the PepH3 brain shuttle peptide and characterize their physicochemical properties.
Materials:
- Lipids/Surfactants: Span 60 (Sorbitan monostearate), Solulan C24 (Cholesteryl poly-24-oxyethylene ether), Cholesterol.
- Peptide: DSPE-PEG(2000)-PepH3 (AGILKRW) peptide.
- Solvents: Chloroform, Ethanol.
- Hydration Buffer: Phosphate Buffered Saline (PBS), pH 7.4.
- Cargo: Texas Red-labeled Bovine Serum Albumin (TR-BSA) or a therapeutic single-domain antibody (sdAb).
- Equipment: Round-bottom flask, rotary evaporator, water bath sonicator, syringe filters (0.45 µm and 0.2 µm), ultracentrifuge.
Methodology:
- Dissolution of Lipid Film: In a round-bottom flask, dissolve Span 60, Solulan C24, and cholesterol in a hot 1:2 mixture of chloroform and ethanol. For PepH3-tagged niosomes (N-PepH3), add DSPE-PEG-PepH3 peptide (4.5% w/w of total lipids) to this mixture [44].
- Film Formation: Remove the organic solvents using a rotary evaporator connected to a vacuum pump to form a thin, dry lipid film on the inner wall of the flask.
- Hydration: Hydrate the dry lipid film with PBS containing the desired cargo (e.g., 0.1 mg/mL TR-BSA). Heat the mixture to 45°C in a water bath and sonicate for 1 hour.
- Extrusion and Purification: Sequentially filter the niosome suspension through 0.45 µm and 0.2 µm syringe filters. Remove non-entrapped cargo by ultracentrifugation at 123,249 × g for 3 hours at 4°C.
- Resuspension: Carefully remove the supernatant. Weigh the pellet and resuspend it in an appropriate culture medium to a final concentration of 100 mg/mL for subsequent experiments.
Characterization:
- Encapsulation Efficiency (EE %): Determine indirectly by measuring the amount of unencapsulated cargo in the supernatant after ultracentrifugation using spectrofluorometry (for fluorescent cargo) or Western Blot (for proteins). Calculate EE% = [(Initial cargo amount - Supernatant cargo amount) / Initial cargo amount] × 100 [44].
- Size and Zeta Potential: Dilute the niosomes in PBS or distilled water (e.g., to 5 mg/mL). Measure the hydrodynamic diameter, polydispersity index (PDI), and zeta potential using Dynamic Light Scattering (DLS) [44] [45].
- Stability and Protein Corona: Incubate niosomes in human plasma (1:1 dilution) at 37°C for various time points (10 min to 24 h). Wash and measure changes in size and zeta potential via DLS to assess protein corona formation and colloidal stability [44].
Protocol: Assessing Transcytosis Across an In Vitro BBB Model
Aim: To evaluate the ability of developed nanocarriers to cross a cultured model of the blood-brain barrier.
Materials:
- In Vitro BBB Model: A co-culture system of brain microvascular endothelial cells (e.g., hCMEC/D3 line or primary cells) with astrocytes and/or pericytes.
- Transwell Plates (e.g., 12-well, 1.12 cm² surface area, 1.0 µm pore size).
- Test Formulations: Fluorescently labeled nanocarriers (e.g., N-PepH3 vs. non-targeted controls).
- Inhibitors: Endocytosis inhibitors (e.g., chlorpromazine for clathrin-mediated, amiloride for macropinocytosis), metabolic inhibitors (e.g., sodium azide).
Methodology:
- Model Validation: Grow endothelial cells on Transwell filters until a confluent monolayer is formed. Measure TEER regularly using an volt/ohm meter to ensure barrier integrity (typically TEER > 150 Ω×cm² for many models) [3].
- Uptake and Transcytosis Assay:
- Add fluorescent nanocarriers to the apical (luminal) compartment.
- Incubate at 37°C (and 4°C as a negative control) for a set time (e.g., 2-4 hours).
- Collect samples from the basolateral (abluminal) compartment at defined time points.
- Quantify the amount of translocated nanocarriers or cargo in the basolateral medium using fluorescence spectroscopy, ELISA, or other suitable techniques.
- Inhibition Studies: Pre-treat the BBB model with endocytosis or metabolic inhibitors for 30-60 minutes before adding the nanocarriers to investigate the mechanism of uptake [44] [45].
- Cellular Uptake and Localization: After the experiment, fix the endothelial cells and perform immunofluorescence staining for organelles (e.g., early endosomes, lysosomes, Golgi apparatus, endoplasmic reticulum) to determine the intracellular trafficking pathway of the nanocarriers [44] [45].
Research Reagent Solutions
The following table details key reagents and their functions for developing and testing brain-targeted nanocarriers, as featured in the cited research.
Table 1: Essential Research Reagents for Nanocarrier Development and BBB Studies
| Reagent / Material | Function / Application | Key Characteristics & Examples |
|---|---|---|
| PepH3 Peptide (AGILKRW) [44] [45] | Cationic brain shuttle peptide for adsorptive-mediated transcytosis (AMT). | Derived from Dengue virus capsid protein; enhances nanoparticle uptake and transcytosis across BBB models. |
| DSPE-PEG(2000) [44] | Lipid-polymer conjugate for surface functionalization. | Used to anchor targeting peptides (like PepH3) to lipid-based nanocarriers; PEG chain provides stealth properties. |
| Span 60 & Cholesterol [44] | Core components of niosomal nanocarriers. | Form stable, biocompatible, and biodegradable vesicular structures for encapsulating hydrophilic/hydrophobic drugs. |
| Single-Domain Antibody (sdAb) [44] [45] | Model therapeutic biomolecule cargo. | Small size (~14 kDa), high stability; used for targeting specific antigens in the brain (e.g., Aβ oligomers in Alzheimer's). |
| Dynamic Light Scattering (DLS) Instrument [43] [44] | Characterizes hydrodynamic size, PDI, and zeta potential. | Essential for quality control; ensures nanocarriers are within the optimal 10-100 nm range and have a stable surface charge. |
| Transwell Permeability System [44] [3] | In vitro model for assessing BBB permeability and transcytosis. | Enables high-throughput screening of nanocarrier transport under controlled conditions. |
Signaling Pathways and Experimental Workflows
Nanocarrier Transcytosis Pathways Across the BBB
This diagram illustrates the primary mechanisms by which functionalized nanocarriers cross the Blood-Brain Barrier.
Workflow for Nanocarrier Preparation and Evaluation
This diagram outlines a standard experimental workflow for developing and testing brain-targeted nanocarriers, from formulation to in vitro validation.
Troubleshooting Guide: AAV Vectors
Q1: My AAV vector is not achieving sufficient transduction efficiency in the target tissue. What could be the cause? Inefficient AAV transduction can stem from incorrect serotype selection, pre-existing immunity, or issues with vector dosage and administration.
- Cause 1: Incorrect Serotype Selection. Different AAV serotypes have distinct tissue tropisms. Using a serotype not optimized for your target organ will result in poor delivery [49] [50].
- Cause 2: Pre-existing Neutralizing Antibodies (NAbs). A significant proportion of the human population has pre-existing NAbs against common AAV serotypes, which can bind to and inactivate the viral vector before it reaches the target cells [50] [51].
- Cause 3: Inadequate Vector Dose or Administration Route. The potency of AAV vectors is dose-dependent, and the route of administration (e.g., intravenous, intramuscular, intrathecal) critically affects biodistribution [52].
Solution:
- Serotype Selection: Refer to the table below to choose a serotype with known tropism for your target tissue. Consider using screening kits to test multiple serotypes side-by-side in your model system [52].
- Pre-screen for NAbs: In preclinical models, screen for pre-existing NAbs against your chosen AAV serotype. In a clinical context, patient screening may be necessary [50].
- Optimize Dose and Route: Conduct a pilot dose-escalation study to determine the minimum effective dose. Ensure the administration route is optimal for reaching the target tissue [52].
Q2: I need to deliver a large transgene that exceeds AAV's packaging capacity. What are my options? The natural packaging capacity of AAV is limited to approximately 4.7 kilobases (kb) for single-stranded vectors, making the delivery of large genes a significant challenge [53] [50] [52].
- Cause: The small icosahedral capsid of AAV physically constrains the size of the DNA that can be packaged [53].
Solution:
- Utilize Oversized Vectors: Some studies indicate that recombinant AAV genomes slightly larger than 5 kb can be packaged, albeit with reduced efficiency [53].
- Employ Dual AAV Vectors: Split the large transgene into two separate AAV vectors. Upon co-infection of the same cell, the full-length transcript can be reconstituted through various mechanisms like trans-splicing or overlapping fragmentation [53].
- Consider Miniaturized Transgenes: Engineer a shortened, yet functional, version of your gene (e.g., a mini-dystrophin for Duchenne muscular dystrophy) that fits within the AAV cargo limit [51].
Q3: My AAV preparation has a low functional titer. What factors affect this during production? The ratio of total viral particles (VP) to functional, genome-containing particles (GC) is a critical quality attribute for AAV preparations.
- Cause 1: Inefficient Genome Packaging. During vector production, a large number of empty capsids (lacking the therapeutic genome) are generated. These non-functional particles contribute to the total VP count but not to transduction [53] [52].
- Cause 2: Purity and Storage Conditions. Impurities from the production process or repeated freeze-thaw cycles can degrade the virus and reduce functional titer [52].
Solution:
- Optimize Production System: Ensure the Rep/Cap and helper plasmids are well-balanced in your transient transfection system to support efficient capsid assembly and genome packaging [53].
- Improve Purification: Use advanced chromatography methods (e.g., ion-exchange) or density gradient centrifugation to separate empty capsids from full ones [49] [52].
- Proper Storage and Handling: Aliquot purified AAV vectors and store them at -80°C. Avoid repeated freeze-thaw cycles by using single-use aliquots [52].
AAV Serotype Selection Guide
Table 1: Common AAV Serotypes and Their Tissue Tropisms
| Serotype | Primary Receptor | Tissue Tropism | Key Characteristics |
|---|---|---|---|
| AAV1 | Sialic acid [49] | Skeletal muscle, heart, CNS [49] | First viral vector approved for gene therapy; high tropism for skeletal muscle [49]. |
| AAV2 | HSPG [49] | Liver, kidney, retina, CNS [49] | The most extensively studied serotype; requires multiple coreceptors for cell entry [49]. |
| AAV5 | Sialic acid [49] | Retina, CNS, lung [49] | Used in approved drugs like Hemgenix (hemophilia B); structurally distinct from other serotypes [49]. |
| AAV8 | Laminin receptor [50] | Liver, pancreas, muscle [50] | Highly efficient for hepatocyte transduction; often used for liver-directed gene therapy [50]. |
| AAV9 | Galactose [50] | CNS, heart, liver, muscle [49] [50] | Effectively crosses the blood-brain barrier; used in Zolgensma for spinal muscular atrophy [49] [50]. |
Experimental Protocol: AAV Serotype Tropism ScreeningIn Vivo
Objective: To empirically determine the most efficient AAV serotype for transducing a specific target tissue in a murine model.
Materials:
- AAV serotype testing kit (e.g., AAV1, 2, 5, 8, 9) each encoding a reporter gene like GFP or luciferase under a ubiquitous promoter (e.g., CAG or CBA) [52].
- Experimental animal model (e.g., C57BL/6 mice).
- Appropriate injection equipment (e.g., syringes, infusion pumps).
Methodology:
- Vector Administration: Divide animals into groups (n≥5). Administer a standardized dose (e.g., 1x10^11 vector genomes per animal) of each AAV serotype via the intended route (e.g., intravenous via tail vein for systemic delivery, or intrathecal for CNS delivery).
- Incubation: Allow 3-4 weeks for robust transgene expression to develop.
- Tissue Analysis:
- Imaging: For luciferase reporters, perform in vivo bioluminescence imaging to visualize global biodistribution.
- Harvest: Euthanize animals and harvest the target tissues (e.g., liver, brain, muscle).
- Quantification: Analyze transgene expression by qPCR (for vector genome copy number) and Western blot/immunohistochemistry (for protein expression levels). For GFP, analyze via fluorescence microscopy or flow cytometry.
Interpretation: The serotype yielding the highest transgene expression in the target tissue, with minimal off-target expression, is the optimal candidate for further studies.
AAV Serotype Screening Workflow
Troubleshooting Guide: Antisense Oligonucleotides (ASOs)
Q1: My ASO shows high efficacy in cell culture but fails in animal models. Why might this be happening? This common problem often relates to poor stability, inadequate biodistribution, or inefficient cellular uptake in vivo.
- Cause 1: Nuclease Degradation. Unmodified oligonucleotides are rapidly degraded by nucleases in the bloodstream [54].
- Cause 2: Poor Biodistribution and Pharmacokinetics. Without a delivery system, ASOs may not accumulate in the target organ or may be rapidly cleared by the kidneys [54].
- Cause 3: Inefficient Endosomal Escape. ASOs are internalized into cells via endocytosis. It is estimated that only 1–2% of molecules escape the endosomal system to reach their cytoplasmic or nuclear targets; the rest are trafficked to lysosomes for degradation [55].
Solution:
- Chemical Modifications: Incorporate phosphorothioate (PS) backbones and sugar modifications (e.g., 2'-O-Methyl (2'-OMe), 2'-O-Methoxyethyl (2'-MOE), or Locked Nucleic Acid (LNA)) to enhance nuclease resistance and binding affinity [54] [55].
- Utilize Delivery Systems: Formulate ASOs with lipid nanoparticles (LNPs) or conjugate them to targeting ligands (e.g., peptides, antibodies) to improve delivery to specific tissues [54].
- Modify Endosomal Trafficking: Recent research suggests that knocking out genes involved in endosome-to-Golgi retrograde transport, such as AP1M1, can delay lysosomal degradation of ASOs and significantly enhance their functional activity by increasing endosomal escape [55].
Q2: I am observing unexpected toxicities or off-target effects with my ASO. What could be the reason? ASO-mediated toxicity can stem from sequence-dependent or -independent effects.
- Cause 1: Immune Stimulation. Certain ASO sequences, particularly those with CpG motifs, can trigger innate immune responses via Toll-like receptors (TLRs) [54].
- Cause 2: Off-Target Hybridization. The ASO may bind to RNA sequences with partial complementarity, leading to unintended silencing or modulation of non-target genes [54].
- Cause 3: Protein Binding. The PS backbone can cause non-sequence-specific binding to cellular proteins, potentially leading to cytotoxic effects [54].
Solution:
- Careful Sequence Design: Use bioinformatics tools to screen the ASO sequence for potential immune-stimulatory motifs and off-target binding sites.
- Optimize Chemistry: Using advanced chemistries like LNA or cEt (constrained ethyl) allows for shorter ASO sequences, which can improve specificity and reduce protein binding.
- Dose Titration: Identify the minimum effective dose to minimize saturation of protein binding and other non-specific effects.
Experimental Protocol: Functional Validation of ASO Activity via a Splicing Reporter Assay
Objective: To screen and validate the efficacy of splice-switching ASOs using a cellular reporter system.
Materials:
- HEK293 or other relevant cell line stably expressing a CRISPR/Cas9 nuclease.
- EGFP Splicing Reporter (EGFPsr) construct. This construct contains an aberrantly spliced EGFP gene that can be corrected by a functional SS-ASO, leading to GFP expression [55].
- ASOs to be tested (e.g., candidate SS-ASOs).
- Transfection or electroporation reagents.
- Flow cytometer or high-content imager.
Methodology:
- Cell Culture: Maintain the HEK293-Cas9-EGFPsr cells in standard DMEM medium supplemented with fetal bovine serum.
- ASO Delivery: Seed cells in a 24-well or 96-well plate. The next day, transfert or electroporate the cells with a range of ASO concentrations (e.g., 10 nM to 100 nM). Include a negative control (scrambled ASO) and a positive control (known effective ASO if available).
- Incubation: Incubate the cells for 24-48 hours to allow for ASO uptake, splicing correction, and GFP expression.
- Analysis:
- Flow Cytometry: Harvest the cells and analyze them using a flow cytometer to quantify the percentage of GFP-positive cells and the mean fluorescence intensity.
- Imaging: Use high-content imaging to visualize and quantify GFP expression at a single-cell level.
Interpretation: A successful SS-ASO will produce a dose-dependent increase in the percentage of GFP-positive cells and the fluorescence intensity, confirming its nuclear delivery and functional activity.
ASO Splicing Reporter Assay Pathway
Troubleshooting Guide: Overcoming the Blood-Brain Barrier (BBB)
Q1: How can I enhance the delivery of AAV vectors across the Blood-Brain Barrier for CNS disorders? The BBB is a major obstacle for gene therapy of neurological diseases, but certain AAV serotypes and engineered capsids show promise.
- Cause: The BBB is a semi-permeable membrane comprising endothelial cells, pericytes, and astrocytes connected by tight junctions. It prevents more than 98% of small-molecule drugs and all large biologics from entering the brain [3].
Solution:
- Select BBB-Penetrant Serotypes: AAV9 and certain variants of AAVrh.10 have demonstrated a natural ability to cross the BBB following intravenous administration, making them preferred choices for global CNS gene delivery [49] [50].
- Utilize Receptor-Mediated Transcytosis (RMT): Engineer AAV capsids to display ligands or peptides that bind to receptors highly expressed on the BBB (e.g., transferrin receptor). This can actively shuttle the vector across the endothelial cells [3] [50].
- Employ Capsid Engineering: Use directed evolution or AI-guided design (e.g., Dyno Therapeutics, Voyager Therapeutics) to select for novel AAV capsids with enhanced BBB penetration and neuronal tropism. Some engineered capsids show a 50- to 100-fold improvement over natural AAV9 [51].
Q2: What strategies can be used to deliver ASOs across the BBB? Direct delivery methods are often required for ASOs to reach therapeutic concentrations in the brain.
- Cause: Like other large molecules, ASOs are effectively excluded from the brain by the intact BBB [54] [56].
Solution:
- Intrathecal or Intracerebroventricular (ICV) Injection: Bypass the BBB entirely by injecting the ASO directly into the cerebrospinal fluid (CSF). This is the route used by several approved ASO drugs for neurological diseases like Spinal Muscular Atrophy (Nusinersen) [56].
- Biolistic Delivery (Loading into CSF): Techniques involving convection-enhanced delivery can also be used to improve distribution within the brain parenchyma following direct injection [56].
- Liposomal Formulation: Encapsulating ASOs in stable liposomal formulations, such as BP1001, can improve their stability in biological fluids and may enhance delivery to target sites, though crossing the BBB remains a challenge [54].
Research Reagent Solutions for BBB and Delivery Studies
Table 2: Key Reagents for Gene Therapy and Oligonucleotide Delivery Research
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| AAV Serotype Kits | Empirical screening of tissue tropism | Commercially available kits containing AAV-GFP for multiple serotypes (e.g., AAV1, 2, 5, 8, 9) for side-by-side comparison [52]. |
| Chemically Modified ASOs | Enhance stability, affinity, and reduce immunogenicity | Phosphorothioate (PS) backbone, 2'-MOE, 2'-OMe, or LNA modifications [54] [55]. |
| EGFPsr Splicing Reporter Cell Line | Functional validation of splice-switching ASO activity | HEK293-Cas9-EGFPsr cells enable high-throughput screening and mechanistic studies of ASO delivery [55]. |
| Liposomal Formulations | Improve ASO stability and cellular uptake | BP1001 is a liposome-incorporated Grb2 antisense oligodeoxynucleotide in clinical trials, demonstrating enhanced biodistribution [54]. |
| Engineered AAV Capsids | Achieve enhanced BBB penetration and cell-type specificity | AI-designed capsids (e.g., from Dyno Therapeutics) or those from directed evolution platforms (e.g., Voyager's TRACER) [51]. |
The blood-brain barrier (BBB) represents one of the most significant challenges in treating central nervous system (CNS) disorders. This protective barrier, composed of endothelial cells, tight junctions, pericytes, and astrocytes, effectively prevents more than 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from entering the brain from the bloodstream [4] [3] [57]. This severely limits treatment options for conditions such as Alzheimer's disease, Parkinson's disease, brain tumors, and depression. Intranasal (IN) administration has emerged as a powerful, non-invasive strategy to bypass the BBB entirely, enabling direct delivery of therapeutic agents to the brain within minutes [58] [59]. This method leverages the unique anatomical connections between the nasal cavity and the brain, offering researchers a promising alternative to invasive delivery methods that are often impractical for human use due to safety, convenience, and cost considerations [58].
This technical support guide provides essential information for researchers implementing intranasal delivery methodologies, including troubleshooting common experimental issues, detailed protocols, and key resources to optimize delivery efficiency for CNS-targeted therapeutics.
Troubleshooting Common Intranasal Delivery Challenges
Q1: Our intranasally administered therapeutic shows poor delivery efficiency to the brain. What factors should we investigate?
A: Several factors can significantly impact brain delivery efficiency. Please systematically check the following, which are summarized in the table below:
- Formulation and Drug Properties: The molecular size, lipophilicity, and stability of your therapeutic agent are critical. The formulation itself can be optimized using mucoadhesive agents or permeability enhancers.
- Administration Technique: The administration volume and the location of deposition within the nasal cavity are crucial. The olfactory region is the primary gateway for direct nose-to-brain transport.
- Physiological Barriers: The nasal cavity's natural defense mechanisms, namely mucociliary clearance and enzymatic degradation, can rapidly remove or break down your drug before it reaches the brain.
Table 1: Troubleshooting Poor Brain Delivery Efficiency
| Category | Specific Factor | Impact & Mechanism | Potential Solutions |
|---|---|---|---|
| Formulation & Drug Properties | Molecular Size/Weight | Larger molecules (>1000 Da) diffuse more slowly [3]. | Consider using nanocarriers (e.g., liposomes, chitosan nanoparticles) to encapsulate and transport large molecules [60] [59]. |
| Lipophilicity/Solubility | Hydrophilic drugs have low membrane permeability [3]. | Modify drug structure or formulation to improve lipophilicity, or use absorption enhancers. | |
| Enzymatic Stability | Susceptibility to degradation by nasal mucosal enzymes reduces bioavailability [59] [61]. | Use enzyme inhibitors in the formulation or design more stable drug analogs (e.g., PEGylation) [61]. | |
| Administration Technique | Administration Volume | Excessive volume leads to swallowing or lung aspiration [60]. | For mice/rats: 10-20 µL total volume, divided between nostrils [60].For humans: 100-150 µL per nostril is the maximum [60]. |
| Deposition Site | Failure to reach the olfactory region prevents direct transport [62]. | Use specialized delivery devices; position animal head correctly (e.g., supine position at a specific angle) to maximize olfactory deposition. | |
| Physiological Barriers | Mucociliary Clearance | Rapidly clears drugs from the nasal cavity (within 15-20 minutes) [60]. | Incorporate mucoadhesive polymers (e.g., chitosan, gelatin) to increase residence time [60] [59]. |
| Limited Permeability | The nasal epithelium itself is a barrier, especially for large or charged molecules. | Add permeation enhancers (e.g., cyclodextrins, surfactants) to temporarily disrupt tight junctions [61] [57]. |
Q2: We are observing high variability in brain drug concentrations between subjects in our animal studies. How can we improve consistency?
A: Subject variability is a common challenge. To improve consistency:
- Standardize the administration procedure: Ensure the animal's head position, angle, and the rate of droplet application are identical for every administration. The supine position is often used to promote flow toward the olfactory region [62].
- Control nasal cavity health: Avoid using animals with nasal congestion or infections, as these conditions alter mucosal properties and clearance rates. The overall health of the nasal epithelium significantly affects absorption [59].
- Account for physiological cycles: Be aware that the nasal cycle (alternating congestion and decongestion of nostrils) can affect deposition and absorption patterns [62].
- Use anesthetics carefully: Some anesthetics can suppress the ciliary beat frequency, thereby affecting mucociliary clearance. Use the same anesthetic protocol consistently throughout the study [62].
Q3: What are the primary pathways for direct nose-to-brain drug transport, and how can we confirm which pathway our drug is using?
A: The two primary direct pathways are the olfactory nerve pathway and the trigeminal nerve pathway.
- The Olfactory Pathway: This is the most important route for bypassing the BBB [58] [57]. It involves transport from the olfactory epithelium in the nasal cavity, through the cribriform plate, to the olfactory bulb and more distant brain regions like the hippocampus. This pathway can be intraneuronal (slower, involving axonal transport) or extraneuronal (faster, via diffusion in the perineuronal space) [61] [57].
- The Trigeminal Pathway: This pathway delivers drugs to the brainstem and caudal regions via the ophthalmic and maxillary branches of the trigeminal nerve, which innervate the respiratory epithelium [58] [59].
Diagram: Primary Neural Pathways for Intranasal Drug Delivery to the Brain
To confirm the pathway, researchers often use techniques like radioactive or fluorescent labeling of the drug and track its spatial and temporal distribution in the brain and CSF. Rapid appearance (within minutes) in the olfactory bulb or brainstem suggests extraneuronal transport along the olfactory or trigeminal pathways, respectively [58] [61]. Histological analysis can provide visual confirmation of the drug along these nerve tracts.
Frequently Asked Questions (FAQs) on Intranasal Methodology
Q: What types of therapeutics are suitable for intranasal delivery? A: A remarkably wide variety of therapeutics have been successfully delivered intranasally, including small molecules, peptides, proteins, and even large macromolecules. Examples from the literature include insulin [58] [61], nerve growth factor (NGF) [58], exendin [61], antidepressants [59], and genes [58]. The key is that the molecule must be potent enough to exert its effect at the nanomolar concentration range typically achieved in the brain via this route [58].
Q: Can intranasal delivery be used for large molecules like monoclonal antibodies? A: While the direct pathways are size-limited, advanced formulation strategies are being developed to deliver large molecules. Nanocarrier systems such as liposomes, polymeric nanoparticles, and nanoemulsions can encapsulate large biologics like antibodies, protecting them from degradation and facilitating their transport across the nasal epithelium [60] [63]. However, intranasal delivery of large therapeutics remains a significant challenge and is an active area of research.
Q: How does intranasal delivery compare to other strategies for overcoming the BBB? A: Intranasal delivery offers a unique balance of non-invasiveness and direct access to the CNS. The table below compares it to other prominent strategies.
Table 2: Comparison of Strategies to Overcome the Blood-Brain Barrier
| Strategy | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Intranasal Administration | Bypasses BBB via olfactory/trigeminal nerves [58]. | Non-invasive; rapid delivery (minutes); avoids first-pass metabolism; reduces systemic side effects [58] [57]. | Limited dosing volume; mucociliary clearance; potential nasal irritation [59] [61]. |
| Receptor-Mediated Transcytosis (RMT) | Uses ligands to "hijack" endogenous BBB transport systems (e.g., transferrin receptor) [4] [3]. | Can target specific receptors; suitable for a range of drug sizes. | Requires complex drug conjugation; potential for off-target effects; transport efficiency can be variable. |
| Focused Ultrasound (FUS) | Temporarily and reversibly disrupts BBB tight junctions using ultrasound and microbubbles [63]. | Highly localized and reversible BBB opening; can deliver very large molecules. | Invasive device required; risk of micro-hemorrhages or neuroinflammation; still largely experimental. |
| Nanoparticle Carriers | Encapsulates drugs in nano-sized carriers that can cross BBB via various mechanisms [60] [4]. | Protects drug; can be engineered for active targeting; improves pharmacokinetics. | Complexity of manufacture; potential long-term toxicity concerns; batch-to-batch variability. |
Q: What are the critical parameters for formulating a stable and effective intranasal solution? A: Key formulation parameters include:
- pH and Osmolarity: The formulation should be isotonic and have a pH between 5.5 and 6.5 to minimize nasal irritation and ciliotoxicity [57].
- Viscosity: Moderate viscosity can improve residence time, but excessive viscosity can hinder diffusion to the olfactory epithelium.
- Preservatives and Stabilizers: These are essential for multi-dose formulations and for stabilizing sensitive molecules like peptides and proteins against enzymatic degradation [59].
Essential Experimental Protocols
Protocol: Intranasal Administration in Rodent Models
This protocol is adapted from established methodologies cited in the literature [58] [59] [57].
Objective: To safely and effectively administer a therapeutic agent to the brain of a rodent (mouse/rat) via the intranasal route.
Materials:
- Therapeutic agent in solution (appropriate viscosity and pH)
- Micropipette with fine, low-retention tips
- Anesthetic equipment (e.g., isoflurane setup)
- Animal warming pad
- Timer
Procedure:
- Anesthetize the animal: Use a short-acting anesthetic like isoflurane. Ensure the animal is in a surgical plane of anesthesia (no response to toe pinch) but avoid deep anesthesia that suppresses respiration.
- Position the animal: Place the animal on its back (supine position) on a warming pad. The head should be in a natural, non-extended position. Some protocols recommend a specific head angle (e.g., 45-70 degrees) to promote flow toward the olfactory region.
- Administer the solution:
- Calculate the dose: The total administration volume should not exceed 10-20 µL for a mouse and 20-40 µL for a rat.
- Divide the dose: Administer the total volume in alternating drops (2-4 µL per drop) between the two nostrils. Allow the animal to inhate each droplet fully before administering the next. This is critical to prevent aspiration into the lungs.
- Delivery technique: Place the pipette tip just inside the nostril without occluding it, and gently expel the droplet. The animal's inhalation will draw the liquid in.
- Recovery: Keep the animal in the supine position for 1-2 minutes after administration to facilitate absorption. Then, place it in a clean cage on its side and monitor until fully recovered from anesthesia.
Troubleshooting Notes:
- If the animal sneezes out the solution, the volume per drop may be too large or the formulation may be irritating.
- If the animal shows signs of respiratory distress, the solution may have been aspirated into the lungs. Re-evaluate the volume and administration technique.
Protocol: Formulating Chitosan-Based Nanoparticles for Peptide Delivery
This protocol outlines the preparation of chitosan nanoparticles, a common mucoadhesive delivery system [60] [59].
Objective: To prepare chitosan nanoparticles encapsulating a model peptide (e.g., insulin) for enhanced intranasal delivery.
Materials:
- Chitosan (low or medium molecular weight)
- Tripolyphosphate (TPP) solution
- Peptide/protein drug (e.g., insulin)
- Acetic acid solution
- Magnetic stirrer
- Syringe and filter (0.45 µm or 0.22 µm)
Procedure:
- Prepare Chitosan Solution: Dissolve chitosan in a 1% (v/v) acetic acid solution to a final concentration of 1-2 mg/mL under magnetic stirring until fully dissolved. Filter the solution.
- Prepare TPP Solution: Dissolve TPP in deionized water to a concentration of 0.5-1.0 mg/mL.
- Ionic Gelation: Under constant stirring, add the TPP solution dropwise to the chitosan solution. A typical chitosan-to-TPP volume ratio is 5:1, but this should be optimized. The formation of nanoparticles will be indicated by the solution becoming opalescent.
- Drug Loading: For active encapsulation, the drug can be added to the TPP solution before mixing with chitosan. For passive loading, the drug can be incubated with the pre-formed nanoparticles.
- Purification: Centrifuge the nanoparticle suspension at high speed (e.g., 15,000 rpm for 30 minutes) to pellet the nanoparticles. Resuspend the pellet in a buffer of desired pH and osmolarity for administration.
Key Parameters for Success:
- The pH of both solutions significantly affects nanoparticle size and stability.
- The stirring speed during ionic gelation controls the size of the nanoparticles.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents and Materials for Intranasal Drug Delivery Research
| Category / Item | Specific Examples | Function & Rationale | Key References |
|---|---|---|---|
| Mucoadhesive Polymers | Chitosan, Gelatin, Hyaluronic Acid, Carbopol | Increases residence time in nasal cavity by adhering to mucosal layer; can open tight junctions (chitosan) [60] [59]. | [60] [59] [57] |
| Permeation Enhancers | Cyclodextrins (α, β, HP-β-CD), Bile Salts, Phosphatidylcholine | Temporarily and reversibly increase permeability of nasal epithelium; can also aid in drug solubility and stability [61]. | [61] |
| Nanocarrier Systems | Liposomes, Solid Lipid Nanoparticles (SLNs), Nanoemulsions, Polymeric NPs (PLGA, Chitosan) | Protects therapeutic agent from enzymatic degradation; enhances absorption; can be engineered for targeted delivery [60] [59]. | [60] [59] [63] |
| Enzyme Inhibitors | Protease Inhibitors (e.g., Aprotinin), Aminopeptidase Inhibitors | Protects peptide and protein drugs from degradation by nasal mucosal enzymes, thereby increasing bioavailability [59]. | [59] |
| Targeting Agents | Albumin, Specific Peptides (e.g., TAT), Cyclodextrins | Can be used to alter the distribution of the drug within the brain, directing it toward specific regions (e.g., hypothalamus) and away from others [61]. | [61] |
From Bench to Bedside: Navigating Translational Challenges and Optimizing Delivery
Mitigating Immunogenicity and Off-Target Effects of Biologic Shuttles
FAQs and Troubleshooting Guides
Immunogenicity
FAQ 1: What are the primary mechanisms that cause an immune response against biologic shuttles?
The immunogenicity of biologic shuttles, such as monoclonal antibodies, is primarily driven by two pathways [64] [65]:
- T-Cell Dependent Pathway: Antigen-presenting cells (APCs) internalize the therapeutic biologic. They process it and present peptide fragments (T-cell epitopes) on their surface via MHC Class II molecules. This presentation activates CD4+ T-helper cells, which in turn stimulate B cells to differentiate into plasma cells, leading to the production of anti-drug antibodies (ADAs) [64].
- T-Cell Independent Pathway: Biologics with multiple, repetitive epitopes can directly cross-link B-cell receptors (BCRs) on the surface of B cells. This direct activation triggers B cells to differentiate into plasma cells and produce ADAs, typically of the IgM type, which are shorter-lived and lower affinity than those generated via the T-cell pathway [64] [65].
The following diagram illustrates these immune activation pathways:
FAQ 2: What key factors intrinsic to the biologic shuttle contribute to immunogenicity?
Several product-related factors can increase the immunogenicity risk of a biologic shuttle [65]:
- Non-Human Sequences: The presence of murine or other non-human protein sequences, even in partially humanized biologics, is readily recognized as foreign by the human immune system [65].
- Aggregates: The formation of high molecular-weight aggregates is a critical risk factor. Aggregates can enhance immune recognition by both T-cell dependent and independent pathways, acting as a potent stimulator of ADA formation [65].
- Product-Related Impurities: Host Cell Proteins (HCPs) that co-purify with the biologic during manufacturing can act as immunogenic adjuvants. A notable example is the HCP PLBL2 found in some lebrikizumab preparations, which led to high ADA rates in clinical trials [65].
- High Isoelectric Point (pI): Biologics with a high pI (positively charged) are more prone to nonspecific binding and uptake by APCs, increasing the chance of immune presentation [65].
- Post-Translational Modifications (PTMs): Altered glycosylation patterns or other PTMs that differ from natural human proteins can create novel epitopes recognized as foreign [65].
FAQ 3: What engineering and formulation strategies can I use to reduce immunogenicity?
Multiple strategies have been developed to de-immunize biologic therapeutics:
- Humanization: This process involves replacing non-human sequences of a biologic (e.g., a murine antibody) with human counterparts. Techniques include Complementarity-Determining Region (CDR) grafting, where only the antigen-binding CDRs are retained from the non-human source, and Specificity-Determining Residue (SDR) grafting, which is even more minimalistic. Fully human antibodies can also be generated using transgenic mice or phage display libraries [65].
- De-immunization: This involves identifying and modifying T-cell epitopes within the protein sequence using in silico tools and experimental assays to eliminate regions that could be presented by MHC II and activate T-cells [66] [65].
- PEGylation: Conjugating the biologic with polyethylene glycol (PEG) can shield immunogenic epitopes, reduce aggregation, and increase hydrodynamic size, thereby reducing immune recognition and clearance. However, the potential for anti-PEG antibodies must be considered [64].
- Nanoparticle Encapsulation: Formulating the biologic within nanoparticles can physically hide it from the immune system. Nanoparticles can be engineered to be "stealth" or to promote tolerogenic immune responses [64].
- Controlling Aggregation: Optimizing manufacturing, formulation, and storage conditions is crucial to minimize aggregate formation. This includes careful control of pH, ionic strength, and temperature, and the use of appropriate stabilizers [65].
The table below summarizes the impact of different antibody engineering strategies on immunogenicity:
Table 1: Impact of Antibody Engineering on Immunogenicity
| Engineering Strategy | Description | Key Impact on Immunogenicity |
|---|---|---|
| Chimerization | Mouse variable regions fused to human constant regions. | Reduces immunogenicity compared to murine antibodies, but residual mouse sequences can still cause HACA responses. |
| Humanization | Only CDRs are of mouse origin, framework is human. | Significantly lower immunogenicity than chimeric antibodies. |
| CDR Grafting | A type of humanization; transfers only CDRs to a human antibody scaffold. | Further reduces immunogenic risk by minimizing non-human sequence footprint. |
| Fully Human | Antibody sequences entirely derived from human sources. | Lowest theoretical immunogenicity, but can still elicit ADAs due to unique idiotypes or aggregates. |
Off-Target Effects
FAQ 4: What are the different types of off-target effects in biologic shuttles, and how are they defined?
For biologic shuttles, "off-target" effects extend beyond the classic genetic editing context and primarily refer to on-target off-tumor toxicity [66]. This occurs when the shuttle correctly binds to its intended target antigen, but that antigen is also expressed on the surface of healthy cells or tissues. When a potent cytotoxic payload is delivered to these healthy cells, it causes dose-limiting toxicity. This is a significant hurdle for Antibody-Drug Conjugates (ADCs) and immunotoxins [66].
FAQ 5: What strategies can I employ to minimize on-target off-tumor toxicity?
Advanced engineering strategies focus on making the activity of the biologic shuttle conditional upon the tumor microenvironment (TME):
- Affinity and Valency Modulation: Reducing the binding affinity or valency (e.g., creating monovalent binders instead of bivalent) of the targeting moiety can exploit the differential antigen density between tumor cells (high) and healthy cells (low). The shuttle may only achieve stable, productive binding on cells with high antigen density [66].
- Conditionally Active Biologics: These shuttles are designed to be inactive in normal physiological conditions but become activated specifically in the TME. This activation can be triggered by TME-specific proteases that cleave a masking peptide from the shuttle's binding site [66].
- Split Toxin Systems: The toxic payload and the cell-targeting moiety are administered as two separate, inactive components. They only assemble into an active immunotoxin inside the tumor cell, leveraging the unique intracellular environment or the proximity provided by co-internalization. This drastically reduces systemic toxicity [66].
The workflow for designing a shuttle with reduced off-target effects involves several key steps:
FAQ 6: What experimental methods are used to detect and quantify off-target effects?
A combination of in silico prediction and rigorous experimental validation is required. While many methods were developed for CRISPR, the principles of thorough off-target assessment are universal. It is critical to use a combination of methods as no single assay can capture all potential off-target events [67].
Table 2: Experimental Methods for Off-Target Assessment
| Method Type | Method Name | Key Principle | Key Strength | Key Limitation |
|---|---|---|---|---|
| Cell-Free | CIRCLE-seq | Uses circularized genomic DNA; nuclease digestion and sequencing identifies cleavage sites. | High sensitivity; works on any DNA sample; dose-response capable. | Lacks cellular chromatin context. |
| Cell-Based | GUIDE-seq | Uses integration of double-stranded oligodeoxynucleotides to mark double-strand break sites in cells. | Unbiased, genome-wide detection in living cells. | Lower sensitivity than cell-free methods; delivery optimization needed. |
| Targeted | LAM-HTGTS | Primers from known on-target sites capture translocations and structural variations. | Detects structural variations (SVs) like large deletions. | Requires a priori knowledge of potential off-target sites. |
Blood-Brain Barrier (BBB) Specific Challenges
FAQ 7: How does the Blood-Brain Barrier complicate the immunogenicity and off-target profile of biologic shuttles?
The BBB adds a layer of complexity as it is a highly selective barrier that prevents >98% of small molecules and nearly 100% of large-molecule drugs from entering the central nervous system (CNS) [15] [4]. To overcome this, shuttles often use receptors like Transferrin Receptor (TfR) or Insulin Receptor to achieve brain penetration via Receptor-Mediated Transcytosis (RMT) [15] [4] [24]. However, these receptors are also expressed on peripheral tissues. Therefore, a shuttle engineered for high TfR affinity to enhance brain delivery may simultaneously increase its uptake in healthy tissues like the liver, potentially exacerbating on-target off-tumor toxicity outside the CNS [66] [24]. Furthermore, strategies that temporarily disrupt the BBB to improve drug delivery can also allow the entry of immune cells and other blood-borne factors, potentially altering the local immune environment and the immunogenic profile of the therapy [15].
FAQ 8: What strategies are emerging to improve the specificity of CNS-targeted shuttles?
Beyond the general strategies listed in FAQ 5, CNS-specific approaches are being developed:
- Affinity Tuning for RMT: For receptors like TfR, there is an "affinity threshold". Very high-affinity shuttles tend to get trapped at the BBB endothelial cell without fully transcytosing into the brain parenchyma. Engineering shuttles with moderate affinity can enhance overall brain delivery and reduce peripheral sink effects [15].
- Dual-Targeting Approaches: Shuttles can be designed to require binding to two different antigens for full activation or uptake, a combination more likely to be unique to the target diseased brain cells [66].
- Exploiting BBB Pathophysiology: In many neurological disorders, the BBB becomes compromised or "leaky." Shuttles can be sized to passively extravasate in diseased areas while being excluded from healthy brain tissue with an intact BBB [24].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Evaluating and Mitigating Immunogenicity and Off-Target Effects
| Reagent / Tool | Function / Application | Key Consideration |
|---|---|---|
| TfR-Binding Moieties | Facilitates Receptor-Mediated Transcytosis across the BBB. | Affinity must be carefully tuned; high affinity may reduce brain penetration. |
| Protease-Cleavable Linkers | Connects targeting moiety to payload; cleaved by TME-specific proteases (e.g., MMPs). | Enables conditionally active shuttles, reducing offtumor toxicity. |
| PEGylation Reagents | Conjugates PEG polymers to the biologic to shield epitopes and reduce aggregation. | Choose molecular weight and chemistry carefully; monitor for anti-PEG antibodies. |
| "Stealth" Nanoparticles | (e.g., PLGA, Liposomes) Encapsulates biologics to hide them from immune surveillance. | Surface functionalization (e.g., with PEG or CD47 mimetics) enhances circulation time. |
| ADA Assay Kits | (e.g., ELISA, MSD) Detects and quantifies Anti-Drug Antibodies in serum/plasma. | Should be drug-tolerant to detect ADAs in the presence of circulating drug. |
| Host Cell Protein (HCP) Kits | ELISA kits using polyclonal antibodies against HCPs from specific production cell lines. | Critical for monitoring process-related impurities that act as immunogenic adjuvants. |
| In silico T-cell Epitope Prediction Tools | Software to predict peptide binding to common MHC Class II alleles. | Used for deimmunization by design during early protein engineering stages. |
Engineering for Optimal Binding Avidity and Brain Retention
### Frequently Asked Questions (FAQs)
FAQ 1: Why does my bispecific antibody show high brain uptake in wild-type mice but fails to effectively treat brain tumors in our disease model? This is a common challenge often rooted in the "binding site barrier" effect. At therapeutic doses (typically 5–50 mg/kg), an antibody with excessively high affinity for a BBB receptor, like the transferrin receptor (TfR), can become trapped on the vascular endothelium. It binds so strongly to the receptor on the luminal side that it cannot complete its journey across the endothelial cell via transcytosis, thereby failing to reach the brain parenchyma in therapeutic quantities. The optimal affinity for therapeutic doses is typically a moderate one, which allows for both effective binding and efficient release into the brain [68] [69].
FAQ 2: Our in vitro binding data for a new TfR-binding vector is excellent, but in vivo brain delivery is poor. What could be the cause? Several factors beyond simple binding affinity can cause this discrepancy. First, check the valency of your construct. A bivalent anti-TfR antibody can cross-link receptors, potentially leading to lysosomal degradation rather than transcytosis. Using a monovalent binding format can promote transcytosis. Second, consider engineering pH-sensitive binding. Vectors that bind tightly to TfR at neutral blood pH but release in the acidic environment of the endosome are more likely to be transported across the cell and released into the brain rather than recycled back to the blood or degraded. Finally, the choice of target receptor is crucial; ensure TfR is the most appropriate pathway for your specific experimental model and therapeutic goal [68] [69].
FAQ 3: How do I decide whether to use a high-affinity or moderate-affinity TfR binder for my application? The choice is fundamentally dictated by your dose. The following table summarizes the key considerations:
| Factor | High-Affinity Binder | Moderate-Affinity Binder |
|---|---|---|
| Recommended Dose | Tracer doses (< 1 mg/kg) [68] | Therapeutic doses (5–50 mg/kg) [68] |
| Primary Mechanism | Efficient capture at the BBB, beneficial for imaging diagnostics [68] | Balanced binding and release, preventing capillary entrapment and enabling transcytosis of larger therapeutic doses [68] [69] |
| Typical Application | ImmunoPET radioligands for diagnostics [68] | Delivery of therapeutic biologics (e.g., enzymes, antibodies) [68] |
FAQ 4: What are the primary mechanisms of drug resistance in epilepsy that could affect drug retention in the brain? Pharmacoresistant epilepsy is often linked to overexpression and overactivity of efflux transporters at the BBB, such as P-glycoprotein (Pgp) and breast cancer-resistant protein (BCRP). These ATP-dependent pumps actively transport a wide range of anti-seizure medications back into the bloodstream, reducing their concentration in the brain. Additionally, local overexpression of cytochrome P450 drug-metabolizing enzymes in the brain can degrade drugs before they reach their target [6].
### Troubleshooting Guides
Problem: Low Brain Uptake of a Therapeutic Bispecific Antibody at Tracer Doses
Question: My bispecific antibody, designed for diagnostic imaging, shows unexpectedly low brain uptake in the wild-type mouse model, even at tracer doses. What should I investigate?
Solution:
- Investigate Binding Affinity: The prevailing hypothesis for tracer doses is that stronger TfR affinity enhances brain uptake. Engineer higher-affinity variants of your TfR-binding moiety (e.g., the 8D3 antibody) and test them in a systematic comparison. A study using point mutations (Y32A and Y52A) in the complementarity-determining regions (CDRs) of 8D3 created a range of affinities (e.g., 10 nM, 20 nM, 240 nM), demonstrating that the highest affinity (10 nM) provided the best brain uptake at tracer doses [68].
- Verify Target Engagement: Ensure your antibody's second arm (the therapeutic or diagnostic arm) is not interfering with the TfR-binding function. Use surface plasmon resonance (SPR) or similar techniques to confirm the affinity of the final bispecific molecule for both TfR and your target antigen.
- Check Pharmacokinetics: Perform a detailed time-course analysis of radioiodinated antibodies in blood, brain, and peripheral organs. The higher-affinity variant should show a higher initial brain concentration. If it clears from the brain too quickly, it may indicate insufficient engagement with the intrabrain target [68].
Problem: Rapid Clearance and Poor Retention of Drug in the Brain Parenchyma
Question: Our drug delivery system successfully crosses the BBB but is rapidly cleared, failing to achieve a sustained therapeutic effect. How can we improve brain retention?
Solution:
- Counter Efflux Transporters: If your drug is a substrate for efflux pumps like Pgp or BCRP, consider co-administering efflux inhibitors or modifying the drug's chemical structure to make it a less favorable substrate [6] [3].
- Utilize Controlled-Release Systems: Encapsulate your drug within a carrier system that provides sustained release. This ensures a continuous supply of the therapeutic agent after the initial delivery system has crossed the BBB. Examples include:
- Engage with Intrabrain Targets: For bispecific antibodies, ensure the arm targeting the brain pathology (e.g., amyloid-beta for Alzheimer's) has high affinity. Once across the BBB, strong binding to the abundant pathological target (e.g., amyloid plaques) will sequester the therapeutic agent in the brain, slowing its clearance and improving retention and diagnostic signal [68].
### Experimental Protocols
Protocol 1: Evaluating TfR Affinity Variants for Brain Uptake
Aim: To compare the brain uptake of bispecific antibody variants with different affinities for the transferrin receptor in a mouse model.
Materials:
- Research Reagent Solutions:
- Bispecific Antibodies: Bapi-8D3 variants with different TfR affinities (e.g., 10 nM, 20 nM, 240 nM) [68].
- Iodination Reagent: Iodine-125 (¹²⁵I) or iodine-124 (¹²⁴I) for radio-labeling.
- Animal Model: Wild-type mice and relevant disease model mice (e.g., AppNL-G-F for Alzheimer's pathology).
- Buffer: Phosphate-buffered saline (PBS) or another suitable formulation for injection.
- Gamma Counter and/or PET Scanner for quantification.
Methodology:
- Antibody Production and Labeling:
- Engineer bispecific antibodies using knob-into-hole technology. Create affinity variants by introducing point mutations (e.g., Y32A, Y52A) in the CDRs of the anti-TfR arm (e.g., 8D3) [68].
- Purify the antibodies from cell culture supernatant using a method like protein A or protein G affinity chromatography.
- Radiolabel the purified antibodies with ¹²⁵I for ex vivo biodistribution studies or ¹²⁴I for in vivo PET imaging.
- In Vivo Administration and Biodistribution:
- Divide mice into groups, each receiving a single intravenous injection of a different radiolabeled affinity variant at a tracer dose (< 1 mg/kg).
- At predetermined time points post-injection (e.g., 2, 6, 24, 48, 72 hours), euthanize the mice and collect blood, brain, and other organs of interest.
- Ex Vivo Analysis:
- Weigh the collected tissues and measure radioactivity using a gamma counter.
- Calculate the percentage of injected dose per gram of tissue (%ID/g) for each sample to compare biodistribution and brain uptake across the different affinity variants [68].
- In Vivo PET Imaging (Optional):
- Inject the ¹²⁴I-labeled antibody variant with the strongest TfR affinity into disease model and wild-type mice.
- Acquire PET images at various time points to visually assess and quantify brain uptake and its distribution over time.
Protocol 2: Testing the Impact of Efflux Transporters on Brain Retention
Aim: To determine if a drug candidate is a substrate for efflux transporters at the BBB and to assess the effect of transporter inhibition on brain retention.
Materials:
- Research Reagent Solutions:
- Test Compound: Your drug candidate.
- Efflux Transporter Inhibitors: e.g., Tariquidar (Pgp inhibitor) or Ko143 (BCRP inhibitor).
- In Vitro BBB Model: e.g., a monolayer of brain endothelial cells (like hCMEC/D3) grown on a transwell insert.
- Animal Model: Wild-type mice and/or transporter knockout mice (e.g., Mdr1a/b⁻/⁻).
Methodology:
- In Vitro Transport Assay:
- Culture brain endothelial cells on transwell filters until a tight monolayer with high electrical resistance is formed.
- Add your drug candidate to the donor compartment (e.g., apical side for Pgp assessment).
- Measure the apparent permeability (Papp) from the apical-to-basolateral (A-B) and basolateral-to-apical (B-A) directions. A efflux ratio (B-A Papp / A-B Papp) significantly greater than 2 suggests active efflux.
- Repeat the experiment in the presence of a selective efflux transporter inhibitor. A significant reduction in the efflux ratio confirms your drug is a substrate for that transporter [6] [3].
- In Vivo Pharmacokinetic Study:
- Administer your drug candidate to wild-type mice with and without pre-treatment with an efflux transporter inhibitor.
- At set time points, collect blood and brain samples.
- Measure drug concentrations in plasma and brain homogenate using LC-MS/MS.
- Calculate the brain-to-plasma ratio (Kp). A statistically significant increase in Kp in the inhibitor-treated group indicates that efflux transport limits your drug's brain retention [6].
### Data Presentation
Table 1: Pharmacokinetic Profile of Anti-TfR Bispecific Antibody Affinity Variants in Mice
Data adapted from a study investigating TfR affinity impact on brain uptake at tracer doses. Values are representative of %ID/g at 2 hours post-injection [68].
| Bispecific Antibody Variant | TfR Affinity (KD) | Brain Uptake (%ID/g) | Blood Concentration (%ID/g) | Brain-to-Blood Ratio |
|---|---|---|---|---|
| Bapi-8D3 (High Affinity) | 10 nM | 4.5 | 25.1 | 0.18 |
| Bapi-8D3 (Medium Affinity) | 20 nM | 3.8 | 24.5 | 0.16 |
| Bapi-8D3 (Low Affinity) | 240 nM | 2.1 | 26.3 | 0.08 |
Table 2: Key Research Reagent Solutions for TfR-Mediated Brain Delivery Studies
| Reagent / Material | Function / Explanation | Example Use Case |
|---|---|---|
| Knob-into-Hole Technology | An protein engineering method to facilitate the correct assembly of bispecific antibodies by introducing complementary mutations in the Fc regions of two different antibodies [68] [70]. | Production of full-length, monovalent bispecific IgG antibodies targeting TfR and a CNS antigen [68]. |
| LALA-PG Mutations | Fc region mutations (L234A/L235A/P329G) that reduce effector function by minimizing binding to Fcγ receptors and complement C1q, thereby lowering potential immunogenicity and off-target cell activation [68] [70]. | Engineering of therapeutic antibodies for brain delivery to focus on target engagement rather than immune activation [68]. |
| Affinity-Engineered Anti-TfR Antibodies | Vectors (e.g., 8D3 antibody variants) with precisely modulated binding strength to TfR through point mutations in complementarity-determining regions (CDRs) to optimize transcytosis efficiency [68] [69]. | Systematic comparison of high, medium, and low-affinity binders to determine the optimal construct for a specific dosing regimen (tracer vs. therapeutic) [68]. |
### Signaling Pathways and Workflow Visualizations
Addressing Species Differences with Humanized Mouse Models for Accurate Preclinical Testing
Frequently Asked Questions
What is a humanized mouse model? A humanized mouse model is a immunodeficient mouse that has been engrafted with functioning human genes, cells, tissues, or microbiota. These models are used as preclinical tools to more accurately study human-specific biological processes, such as immune responses to cancer or the efficacy of drugs designed to cross the human blood-brain barrier (BBB) [71].
Why are humanized mouse models critical for blood-brain barrier research? The BBB is a major obstacle for treating central nervous system (CNS) disorders, as it prevents more than 98% of small-molecule drugs and nearly all large-molecule therapeutics from entering the brain [3] [4]. Humanized models allow researchers to study drug delivery across a human-like BBB in a live animal system, providing critical data that cannot be obtained from standard mouse models due to species differences in the structure and function of the BBB [72].
Which humanized mouse model is best for my study on brain-targeted therapeutics? The "best" model depends on your research question and timeline. The following table compares the key characteristics of the three main humanization methods to help you decide.
| Model Type | Human Component Source | Key Advantages | Key Limitations & Common Issues | Ideal for BBB/Drug Delivery Studies? |
|---|---|---|---|---|
| Hu-PBL (Human Peripheral Blood Leucocytes) [72] [71] | Peripheral Blood Mononuclear Cells (PBMCs) | Rapid reconstitution of mature human T cells; cost-effective; simple establishment [72]. | Develops severe Graft-versus-Host Disease (GvHD), limiting the experimental window to a few weeks; lacks other immune cell lineages like B cells [72] [71]. | No, due to short lifespan and incomplete immune reconstruction. |
| Hu-SRC (Hematopoietic Stem Cell) [72] [71] | CD34+ Hematopoietic Stem Cells (HSCs) from umbilical cord blood, fetal liver, or mobilized peripheral blood [72]. | Multilineage development of human immune cells (T, B, NK cells); long-term stability (up to 12+ weeks); less prone to GvHD [72] [71]. | Human T cells mature in the murine thymus, leading to MHC restriction instead of human HLA restriction; requires sub-lethal irradiation of newborn mice [72]. | Yes, for long-term studies assessing multi-dose regimens and chronic efficacy. |
| Hu-BLT (Bone Marrow, Liver, Thymus) [72] | Fetal liver and thymus tissue along with HSCs | Considered the "gold standard" for completeness; generates a human thymic niche for proper HLA-restricted T-cell education [72]. | Technically complex; expensive; involves ethical considerations regarding the use of fetal tissue [72]. | Yes, for studies requiring the most accurate human immune response. |
I am observing low engraftment of human immune cells in my Hu-SRC model. What could be wrong? Low engraftment can be caused by several factors related to the source of HSCs and the recipient mouse. For best results:
- HSC Source: Use HSCs from fetal liver or umbilical cord blood, which have been shown to colonize more effectively than those from adult bone marrow [72].
- Recipient Age: Utilize immunodeficient newborn mice (within 72 hours of birth) for intrahepatic HSC injection, as this promotes better engraftment and T-cell maturation [72].
- Irradiation: Ensure proper sub-lethal γ-irradiation of the recipient mouse prior to transplantation. This step is indispensable as it depletes murine HSCs and creates "space" for the human cells to engraft [72].
My PBMC-engrafted mice are developing GvHD too quickly, ending my study prematurely. How can I delay this? GvHD is a common and expected issue in Hu-PBL models due to the reaction of mature human T cells against mouse tissues. To mitigate this:
- Use MHC-deficient mice: Employ immunodeficient mice that also have a genetic knock-out of the murine Major Histocompatibility Complex (MHC). This can prolong the survival of the mice by reducing xenoreactivity [72].
- Pre-deplete CD4+ T cells: Pre-depleting CD4+ T cells from the PBMC inoculum has been shown to alleviate GVHD symptoms, though this will, of course, change the nature of the immune response you are studying [72].
Troubleshooting Common Experimental Issues
Issue #1: Inconsistent Drug Delivery Across the BBB in Humanized Models
- Problem: High variability in brain drug concentration between individual humanized mice, leading to unreliable data.
- Solution:
- Verify BBB Integrity: Before dosing, confirm that your humanized model has a fully intact BBB. Some models or conditions may have a "leaky" BBB, which does not accurately represent the primary challenge in CNS drug delivery.
- Select the Right Administration Route: Consider advanced methods beyond simple intravenous (I.V.) injection. Intranasal administration can bypass the BBB entirely by delivering drugs directly to the brain via the olfactory nerve [3].
- Utilize Nanoparticle Carriers: Use drug delivery systems designed to cross the BBB. For example, chitosan–lecithin nanoparticles loaded with phenytoin have been successfully used for intranasal delivery in mice to improve brain uptake [6]. Conjugating drugs to ligands that bind to receptors on the BBB (e.g., transferrin receptor) can also enable receptor-mediated transcytosis [3] [4].
Issue #2: Poor Tumor Engraftment or Growth in Humanized Models for Brain Cancer Studies
- Problem: Human-derived brain tumor cells fail to engraft or show stunted growth in your humanized mouse model.
- Solution:
- Confirm Immune Cell Reconstitution: Do not inject tumor cells until you have confirmed successful human immune system engraftment. The criterion is typically >25% human CD45+ cells in the peripheral blood [72].
- Use Patient-Derived Xenografts (PDX): For a more clinically relevant model, use patient-derived tumor cells (PDX) instead of immortalized cell lines. PDXs better recapitulate the tumor microenvironment and biological characteristics of human cancers [72].
- Co-engraft Supporting Cells: Consider co-transplanting human stromal cells or cytokines that support tumor growth and create a more human-like tumor niche.
Issue #3: Unable to Model Human-Specific Immune Interactions at the BBB
- Problem: The murine components of the model are interfering with the study of human immune cell migration and interaction with the BBB.
- Solution:
- Use Genetically Humanized Models (GEMs): Employ mice that have been genetically engineered to express key human cytokines (e.g., IL-2, IL-3, IL-6, IL-15). These cytokines support the differentiation and survival of specific human immune cell types that may not be supported by mouse versions alone [71].
- Combine with Hu-SRC/Hu-BLT Models: Generate humanized mice on a genetically humanized background (e.g., NOG-EXL mice). This provides a more complete human immune system and the human cytokine signals needed for its maintenance, leading to more accurate interactions with the human-like BBB [71].
The Scientist's Toolkit: Essential Reagents and Models
The following table details key materials and their applications in setting up experiments with humanized mouse models for BBB research.
| Item | Function & Application in BBB Research | Example & Notes |
|---|---|---|
| Immunodeficient Mouse Strains | Serves as the foundational host for engrafting human cells. The level of immunodeficiency is critical for success. | NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl) and NOG (NOD.Cg-Prkdcscid Il2rgtm1Sug) are widely used; they lack T, B, and NK cells, allowing for high engraftment efficiency [72] [71]. |
| CD34+ Hematopoietic Stem Cells (HSCs) | The source for reconstructing a multi-lineage human immune system in the Hu-SRC model. | Sourced from umbilical cord blood or fetal liver for superior engraftment potential [72] [71]. |
| Human Cytokines | Supports the development, survival, and function of specific human immune cell lineages in the mouse host. | Genetically humanized models (e.g., NOG-EXL) express human cytokines like GM-CSF and IL-3 to support myeloid cells [71]. |
| Brain-Targeting Nanoparticles | Carrier systems designed to transport therapeutic drugs across the BBB. | Liposomes, polymeric nanoparticles, and exosomes can be surface-functionalized with targeting ligands (e.g., T7 peptide) to facilitate receptor-mediated transcytosis across the BBB [6] [3]. |
| P-glycoprotein (P-gp) Inhibitors | Used to investigate the role of efflux transporters in limiting brain drug delivery. | Compounds like tariquidar can be co-administered with a drug to see if inhibiting this major efflux pump increases its brain concentration [6] [4]. |
Experimental Workflow and Key Pathways
The following diagram illustrates the strategic workflow for designing a study using humanized mice to evaluate a novel brain-targeted therapeutic.
Strategic Workflow for Humanized Mouse BBB Studies
A critical challenge in the Hu-SRC model is that T cells mature in the mouse thymus, making them restricted to murine MHC rather than human HLA. This limits the study of HLA-dependent immune responses. The following diagram outlines this limitation and a modern solution using advanced models.
T-Cell Education Pathway in Humanized Models
Troubleshooting Guides for Researchers
FAQ: Overcoming Scaling Challenges
Q1: What are the most critical parameters to monitor when scaling up a nanoparticle-based drug delivery system? A robust scale-up requires careful monitoring of Critical Quality Attributes (CQAs). Key parameters include:
- Particle Size and Polydispersity Index (PDI): Ensure consistency and batch-to-batch uniformity. An increase in PDI often signals poor mixing or aggregation during scale-up.
- Zeta Potential: Indicates colloidal stability; a shift may suggest incomplete ligand conjugation or impurity incorporation.
- Drug Loading and Encapsulation Efficiency: Must be maintained to ensure therapeutic efficacy. A drop can point to changes in process kinetics.
- In Vitro Drug Release Profile: A change in the release kinetics can indicate alterations in nanoparticle structure or crystallinity.
Q2: Our formulation shows excellent efficacy in small-scale in vitro BBB models but fails in vivo. What could be the cause? This common challenge often stems from several factors:
- Inadequate BBB Penetration: The in vitro model may not fully replicate the complex cellular interactions and efflux transporter activity of the in vivo BBB. Re-evaluate your targeting strategy (e.g., using ligands for transferrin or insulin receptors) [15].
- Rapid Clearance: The nanoparticles may be opsonized and cleared by the mononuclear phagocyte system (MPS) before reaching the brain. Consider modifying surface properties with hydrophilic polymers like PEG to improve circulation time [3].
- Payload Loss: Instability during storage or in the bloodstream can lead to premature drug release. Investigate the stability of your formulation under physiological conditions.
Q3: How can we improve the stability and shelf-life of complex biologic formulations for CNS delivery? Stability is paramount for clinical translation. Strategies include:
- Formulation Optimization: Use appropriate buffering agents, stabilizers, and cryoprotectants (e.g., sucrose, trehalose) for lyophilization.
- Advanced Analytics: Employ techniques like differential scanning calorimetry (DSC) to understand the physical state of the drug and excipients.
- Quality by Design (QbD): Implement QbD principles early in development to identify and control critical process parameters that impact stability [73].
Q4: We are experiencing high batch-to-batch variability in our ligand-conjugated nanoparticles. How can we improve consistency? Variability often arises from inconsistent conjugation chemistry. To address this:
- Process Control: Tightly control reaction conditions such as temperature, pH, molar ratios, and reaction time.
- Purification: Implement robust and reproducible purification methods (e.g., tangential flow filtration) to remove unreacted ligands and by-products consistently.
- Real-time Monitoring: Use inline or at-line analytics to monitor the conjugation reaction progress, enabling better process control [74].
Troubleshooting Common Scaling Issues
Problem: Particle Aggregation During Scale-Up
- Diagnostic Questions:
- Does aggregation occur during a specific unit operation (e.g., mixing, solvent removal)?
- Has the zeta potential changed compared to small-scale batches?
- Are there new impurities in the raw materials?
- Root Cause: Inefficient mixing leading to localized high concentrations during nanoparticle formation; or, shear forces during pumping that damage particle structure.
- Solutions:
- Process: Optimize mixing speed and geometry. Transition from magnetic stirring to controlled impeller-based mixing.
- Formulation: Adjust surfactant concentration or type to improve stabilization. Ensure the formulation is isotonic.
- Equipment: Use equipment with similar geometric design (e.g., aspect ratio, impeller type) between small and large scale to maintain consistent shear profiles.
Problem: Significant Drop in Drug Loading Efficiency at Large Scale
- Diagnostic Questions:
- Is the encapsulation efficiency lower, or is the total payload lost?
- Has the process time for solvent evaporation or diffusion increased?
- Are the raw material specifications (e.g., polymer molecular weight distribution) identical to those used in development?
- Root Cause: Altered kinetics of nanoparticle formation, leading to premature drug diffusion; or, chemical degradation of the Active Pharmaceutical Ingredient (API) under new process conditions.
- Solutions:
- Process: Shorten the solvent removal time by optimizing temperature and pressure. Ensure the scale-up process maintains a similar surface-to-volume ratio for efficient solvent diffusion.
- API: Explore salt forms or co-crystals of the API to improve lipophilicity and retention within the nanoparticle matrix [73].
- Analysis: Conduct a root-cause analysis of the API's stability under process conditions.
Problem: Inconsistent In-Vitro Performance (BBB Permeation) Between Batches
- Diagnostic Questions:
- Are the CQAs (size, PDI, zeta) within the validated range?
- Is the ligand density on the nanoparticle surface consistent between batches?
- Has the performance of the in-vitro BBB model itself been validated with control compounds?
- Root Cause: Inconsistent surface functionalization (ligand density or orientation); or, subtle changes in nanoparticle composition affecting protein corona formation and subsequent cellular interactions.
- Solutions:
- Analytics: Develop and employ a reliable quantitative assay for ligand density (e.g., using HPLC, fluorescence spectroscopy).
- Purification: Ensure the purification process consistently removes non-conjugated ligands.
- Characterization: Use advanced techniques like surface plasmon resonance (SPR) to confirm the binding affinity of functionalized nanoparticles to their target receptor.
Quantitative Data for Scaling Complex Formulations
Table 1: Key Physicochemical Attributes and Their Scalability Considerations
| Critical Quality Attribute (CQA) | Target Range (Typical) | Impact of Poor Control | Scalability Consideration |
|---|---|---|---|
| Particle Size | 50-200 nm | Altered biodistribution, BBB penetration | Mixing efficiency and shear force during homogenization are scale-dependent. |
| Polydispersity Index (PDI) | <0.2 | Batch inconsistency, variable drug release | Kinetics of nanoparticle formation change with volume; requires process adjustment. |
| Zeta Potential | ±10 to ±30 mV | Physical instability, aggregation | Sensitive to impurity profiles and buffer composition at large scale. |
| Drug Loading | >5% (w/w) | Reduced therapeutic efficacy, increased excipient burden | Scale-up of solvent diffusion/evaporation can alter encapsulation efficiency. |
| Endotoxin Level | <0.25 EU/mL (for injectables) | Pyrogenic response, toxicology failure | Requires stringent process controls and validated depyrogenation steps at all scales. |
Table 2: Comparison of Selected BBB Drug Delivery Strategies and Scalability [15] [7]
| Delivery Strategy | Mechanism | Key Advantage | Scalability Challenge |
|---|---|---|---|
| Receptor-Mediated Transcytosis | Uses nanoparticle-conjugated ligands (e.g., targeting Transferrin Receptor) to hijack endogenous transport pathways. | High target specificity. | Reproducible and consistent ligand conjugation at manufacturing scale; high cost of ligands. |
| Cell-Penetrating Peptides | Utilizes cationic or amphipathic peptides to facilitate cellular uptake. | Broadly applicable to various cargos. | Potential for immunogenicity; controlling the "trojan horse" effect precisely during scale-up. |
| Focused Ultrasound (FUS) | Temporarily disrupts the BBB using microbubbles and ultrasound waves. | Non-invasive, spatiotemporal control. | Complex device-based regimen; integrating drug administration with FUS treatment in a clinical workflow. |
| Nanoparticle Material (e.g., PLGA) | Protects drug payload and can be engineered for controlled release and surface functionalization. | Well-established chemistry, biocompatible. | Reproducibility of polymer synthesis and nanoparticle properties (size, release profile) at scale. |
Experimental Protocols for Scalable Processes
Protocol 1: Scalable Synthesis of Targeted Nanoparticles via Nanoprecipitation
Objective: To reproducibly manufacture ligand-targeted polymeric nanoparticles for BBB delivery at a scalable (1L) batch size.
Materials:
- Polymer: PLGA-PEG-COOH (e.g., 50:50, 15kDa-5kDa)
- Ligand: Transferrin (Tf) or a peptide targeting the Transferrin Receptor (TfR)
- Coupling Reagents: N-(3-Dimethylaminopropyl)-N'-ethylcarbodiimide (EDC), N-Hydroxysuccinimide (NHS)
- Solvents: Acetone (for organic phase), Di-water (for aqueous phase)
- Equipment: Jacketed reactor with overhead stirring, peristaltic pump, sonicator (probe)
Methodology:
- Ligand Conjugation (Pre-functionalization):
- Activate the carboxylic acid end-group of PLGA-PEG-COOH by reacting with EDC and NHS in MES buffer (pH 6.0) for 15 minutes at room temperature.
- Add the ligand (Tf or TfR peptide) to the activated polymer solution and react for 4 hours under gentle stirring.
- Purify the conjugated polymer (PLGA-PEG-Ligand) by dialysis or tangential flow filtration against water, then lyophilize for storage.
Nanoparticle Formation (Scale-Up):
- Dissolve the drug and a blend of plain PLGA and PLGA-PEG-Ligand in acetone (organic phase).
- Fill the jacketed reactor with the aqueous phase (typically water or a weak buffer) and set the temperature to a defined set-point (e.g., 15°C).
- Using a peristaltic pump, add the organic phase to the rapidly stirring aqueous phase at a controlled, fixed rate (e.g., 1 mL/min per 100mL of aqueous phase).
- Continue stirring for 3-4 hours to allow for complete solvent evaporation and nanoparticle hardening.
Purification and Concentration:
- Concentrate and exchange the nanoparticle suspension into the final storage buffer using tangential flow filtration (TFF) with an appropriate molecular weight cut-off (MWCO) membrane.
Validation:
- Characterize the final product for particle size, PDI, zeta potential, drug loading, and ligand density.
- Confirm targeting efficacy using an in vitro BBB model (see Protocol 2).
Protocol 2: Establishing a High-Throughput In-Vitro BBB Model for Formulation Screening
Objective: To create a reproducible and scalable in vitro model for high-throughput screening of formulation permeability across the BBB.
Materials:
- Cell Lines: Primary human brain microvascular endothelial cells (HBMECs) or immortalized cell line (e.g., hCMEC/D3)
- Transwell Inserts: 12-well or 24-well plates with porous polyester membranes (e.g., 1µm pore size)
- Assay Medium: Endothelial cell growth medium, with or without astrocytes-conditioned medium
- Measurement Tools: TEER (Transepithelial Electrical Resistance) meter, fluorescent markers (e.g., sodium fluorescein for integrity check), LC-MS/MS for drug quantification
Methodology:
- Cell Seeding and Culture:
- Coat Transwell inserts with collagen IV and fibronectin.
- Seed HBMECs at a high density (e.g., 100,000 cells/cm²) on the apical side of the insert.
- Culture the cells for 5-7 days, allowing them to form a confluent monolayer. Change the medium every 2 days.
Barrier Integrity Validation:
- Measure TEER daily using a volt-ohm meter. Only use models with TEER values exceeding a set threshold (e.g., 150 Ω·cm²) for experiments.
- Perform a sodium fluorescein permeability assay to confirm low paracellular transport.
Permeability Study:
- Add your nanoparticle formulation (at a therapeutically relevant concentration) to the apical (donor) compartment.
- At predetermined time points (e.g., 30, 60, 120, 240 minutes), sample from the basolateral (receiver) compartment.
- Quantify the amount of drug that has traversed the monolayer using a sensitive analytical method (e.g., HPLC, LC-MS/MS).
- Calculate the apparent permeability coefficient (Papp).
Validation:
- Include control compounds with known high (e.g., propranolol) and low (e.g., atenolol) permeability to validate the model's performance in each experiment.
Visualizing Workflows and Pathways
Scalable Nanoparticle Development Workflow
Receptor-Mediated Transcytosis Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Developing BBB-Shuttling Formulations
| Reagent / Material | Function / Role | Key Consideration |
|---|---|---|
| PLGA-PEG Copolymers | Biodegradable polymer backbone for nanoparticle formation; PEG provides "stealth" properties. | Batch-to-batch consistency, acid-end group for ligand conjugation, PEG length affecting "stealth" effect. |
| Targeting Ligands (e.g., Transferrin, TfR Antibodies, Peptides) | Mediates receptor-specific binding and transcytosis across the BBB endothelium [15]. | Binding affinity, immunogenicity, cost, and scalability of conjugation chemistry. |
| Lipid Nanoparticles (LNPs) | Versatile platform for encapsulating a wide range of therapeutics, including small molecules and nucleic acids (mRNA, siRNA) [15]. | Scalability of microfluidics mixing; stability of the final LNP product. |
| Cell-Penetrating Peptides (CPPs e.g., TAT) | Enhances cellular uptake of cargo through adsorptive-mediated transcytosis [3]. | Can lack specificity; potential for toxicity at high concentrations. |
| P-glycoprotein (P-gp) Inhibitors | Co-administered to block efflux pumps and increase brain concentration of certain drugs [7]. | Risk of increasing toxicity by allowing unwanted compounds into the brain. |
| Functionalized Exosomes | Natural nanovesicles with innate biocompatibility and potential for homing to specific tissues. | Scalable production and isolation, efficient loading of therapeutic cargo. |
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: Why does my model system show no permeability for a drug that previously demonstrated some BBB penetration? A lack of assay window often stems from instrumental setup errors or cell model integrity issues. First, verify your microplate reader's configuration, particularly the emission filter selection for TR-FRET-based assays, as incorrect filters are a primary failure point [75]. For cellular models, confirm that your BBB co-culture (endothelial cells, astrocytes, pericytes) maintains tight junction integrity; check transendothelial electrical resistance (TEER) values regularly. A drop in TEER indicates compromised tight junctions, leading to abnormally high, non-physiological permeability [3] [4]. Ensure efflux transporters (e.g., P-gp) are functioning correctly, as their upregulation can unexpectedly reduce net drug accumulation [4] [14].
Q2: What are the primary reasons for significant variability in EC50/IC50 values for the same compound between different laboratories? The most common source of EC50/IC50 variation is differences in stock solution preparation (e.g., 1 mM stocks made in different labs) [75]. Other factors include:
- Cellular Context: The compound may target an inactive kinase form, or an upstream/downstream kinase in cell-based assays, unlike in purified enzyme assays [75].
- Assay Conditions: Small variations in serum concentration, pH, or incubation time can impact results.
- Data Analysis: Inconsistent normalization methods between datasets. Always use ratiometric data analysis (acceptor/donor signal) for TR-FRET to account for pipetting variances and reagent lot differences [75].
Q3: How can I determine if my nanoparticle formulation is successfully utilizing receptor-mediated transcytosis (RMT) versus simply disrupting the BBB? To confirm RMT, employ these experimental controls:
- Ligand Competition: Co-incubate with an excess of free ligand (e.g., transferrin for TfR-targeting). A significant reduction in nanoparticle translocation indicates a specific, competitive RMT process.
- Inhibition of Endocytic Pathways: Use chemical inhibitors of clathrin-mediated endocytosis (e.g., chlorpromazine). A decrease in uptake suggests an RMT mechanism.
- Characterization of Barrier Integrity: Monitor TEER and paracellular permeability markers (e.g., sucrose flux) throughout the experiment. Stable TEER values and low sucrose flux rule out non-specific barrier disruption [15] [3] [24]. Post-experiment, analyze the cells for tight junction protein expression (claudin-5, occludin) via immunofluorescence to visually confirm junctional integrity [4].
Q4: When combining focused ultrasound (FUS) with nanoparticle delivery, how can I ensure consistency and safety between treatment sessions? Implement a robust quality assurance (QA) protocol based on passive acoustic detection to monitor the FUS-induced BBB opening procedure. One clinical study demonstrated that such a protocol could achieve QA standards in 9 out of 10 glioma patients. Key steps include [76]:
- Acoustic Coupling Check: Verify the quality of the acoustic coupling between the transducer and the skull. Be prepared to repeat the coupling procedure until QA is successfully passed.
- Microbubble Monitoring: Use real-time acoustic feedback to monitor microbubble activity, which helps standardize the level of BBB disruption and prevent over-exposure that could lead to vascular damage or edema.
- Dosimetry: Carefully control the parameters of ultrasound pressure, microbubble dose, and sonication time based on pre-established safety curves.
Troubleshooting Common Experimental Issues
Problem 1: Lack of Assay Window in a Z'-LYTE Kinase Assay Potential Causes & Solutions:
- Cause A: Instrument Setup Failure. The instrument may not be configured correctly for the assay's fluorescence detection.
- Solution: Refer to instrument setup guides for TR-FRET compatibility. Test the plate reader's setup using control reagents provided with the assay kit before running your experimental samples [75].
- Cause B: Development Reaction Failure. The development enzyme is not functioning optimally.
- Solution: Perform a control development reaction. Without exposing the 100% phosphopeptide control to the development reagent, it should give the lowest ratio. The 0% phosphopeptide (substrate) exposed to a 10x higher concentration of development reagent should give the highest ratio. A lack of difference indicates a problem with the development reagent dilution or stability [75].
Problem 2: High Variability in Nanoparticle Biodistribution Studies Potential Causes & Solutions:
- Cause A: Nanoparticle Aggregation. This leads to inconsistent dosing and capillary occlusion.
- Solution: Characterize nanoparticle size (dynamic light scattering) and zeta potential before each in vivo administration. Implement stringent filtration (e.g., 0.22 µm filter) post-suspension and ensure homogeneous resuspension before injection [24].
- Cause B: Inconsistent Animal Model. The state of the BBB can vary with age, sex, and pathology.
- Solution: Use age- and sex-matched animal cohorts. For disease models, use a validated method (e.g., MRI, immunohistochemistry for tight junction proteins) to confirm that the BBB phenotype is at the desired stage of impairment or integrity at the time of experimentation [76].
Problem 3: Unexpected Toxicity in In Vivo Models Following Combination Therapy (e.g., Immunotherapy + Nanocarrier) Potential Causes & Solutions:
- Cause A: Off-Target Immune Activation. The combination may have synergistic effects that trigger a systemic inflammatory response.
- Solution: Administer the therapies in a staggered sequence rather than concurrently to identify the toxic component. Closely monitor serum cytokine levels and perform extensive histopathology on major organs (liver, spleen, lungs) [77].
- Cause B: "Priming" of the Innate Immune System. Nanocarriers or certain immunotherapies can prime the immune system, leading to an exaggerated response upon subsequent dosing.
Experimental Protocols for Key Methodologies
Protocol 1: Establishing a Co-Culture Blood-Brain Barrier Model for Permeability Screening
This protocol outlines the steps to create an in vitro BBB model using brain endothelial cells, astrocytes, and pericytes for preliminary testing of combination strategies [3] [4].
Key Materials:
- Cells: Human Brain Microvascular Endothelial Cells (HBMECs), primary human astrocytes, human brain vascular pericytes.
- Cultureware: 12-well Transwell plates (0.4 µm pore size, polyester membrane).
- Media: Endothelial cell growth medium (e.g., EGM-2), astrocyte medium (e.g., ScienCell #1801), pericyte medium (e.g., ScienCell #1201).
Procedure:
- Day 1: Seeding Astrocytes and Pericytes. Coat the bottom of the Transwell plate with poly-L-lysine (5 µg/mL). Seed astrocytes at a density of 2.0 x 10^4 cells/cm² in the bottom chamber. Seed pericytes on the underside of the Transwell insert membrane at 1.0 x 10^4 cells/cm². Culture for 24 hours.
- Day 2: Seeding Endothelial Cells. Coat the inside of the Transwell insert with collagen IV (100 µg/mL). Seed HBMECs on the inside of the insert at a density of 5.0 x 10^4 cells/cm².
- Days 3-7: Maintenance and Validation. Change media every 48 hours. Monitor the integrity of the endothelial layer daily by measuring the Transendothelial Electrical Resistance (TEER) using an epithelial voltohmmeter. A TEER value >150 Ω·cm² is typically indicative of a competent barrier.
- Day 7+: Permeability Assay. Use only models with stable, high TEER. Add your test compound/nanoparticle to the apical (donor) compartment. Collect samples from the basolateral (receiver) compartment at predetermined time points (e.g., 30, 60, 120 min). Analyze samples via HPLC-MS or fluorescence to calculate the apparent permeability coefficient (P_app).
Protocol 2: Conjugating Targeting Ligands to Nanoparticles for RMT
This protocol describes the chemical conjugation of a targeting ligand (e.g., Transferrin, Tf) to the surface of polymeric nanoparticles (e.g., PLGA) [15] [24].
Key Materials:
- Nanoparticles: Pre-formed, carboxylic acid-terminated PLGA nanoparticles.
- Ligand: Human transferrin (Tf).
- Chemicals: 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC), N-Hydroxysuccinimide (NHS), Phosphate Buffered Saline (PBS), Dialysis tubing (MWCO 100kDa).
Procedure:
- Activation of Nanoparticles: Resuspend 10 mg of PLGA nanoparticles in 2 mL of MES buffer (0.1 M, pH 6.0). Add EDC (20 mM final concentration) and NHS (10 mM final concentration). React for 15 minutes at room temperature with gentle stirring to activate the surface carboxyl groups.
- Purification: Purify the activated nanoparticles from excess EDC/NHS by centrifugation (15,000 rpm, 20 minutes) and resuspend in 2 mL of PBS (pH 7.4).
- Ligand Conjugation: Add a 50-fold molar excess of transferrin (relative to estimated surface COOH groups) to the nanoparticle suspension. React for 2 hours at room temperature under gentle stirring.
- Quenching and Final Purification: Quench the reaction by adding 100 µL of 1 M glycine and stirring for 10 minutes. Purify the Tf-conjugated nanoparticles via dialysis (against PBS, 24 hours) to remove unreacted transferrin. Characterize the final product for size, zeta potential, and ligand density (e.g., via BCA assay for surface protein).
Quantitative Data for Combination Strategies
Table 1: Efficacy Metrics of Approved Combination Immunotherapies (Oncology)
| Combination Regimen | Control Arm | Tumor Type | No. of Patients | Grade 3-5 Toxicity (%) | Median PFS (Months) | Median OS (Months) |
|---|---|---|---|---|---|---|
| Nivolumab + Ipilimumab [78] | Nivolumab alone | Metastatic Melanoma | 314 (combo arm) | 60% | 11.5 | Not Reached |
| Pembrolizumab + Chemo [78] | Cetuximab + Chemo | HNSCC | 281 (combo arm) | 85% | 4.9 | 13.0 |
| Atezolizumab + Cobimetinib + Vemurafenib [78] | Cobimetinib + Vemurafenib | BRAF-mutated Melanoma | 256 (combo arm) | 80% | 15.1 | Not Reported |
Table 2: Key Properties of Nanocarriers for Brain Delivery [14] [24]
| Nanocarrier Type | Typical Size Range | Key Advantages | Key Challenges for BBB Delivery |
|---|---|---|---|
| Liposomes | 80-150 nm | High drug loading, biocompatible, facile surface modification. | Rapid clearance by MPS, potential stability issues in serum. |
| Polymeric NPs (e.g., PLGA) | 50-200 nm | Controlled release kinetics, tunable degradation. | Polymer batch-to-batch variability, complexity of scaling up. |
| Solid Lipid NPs (SLNs) | 50-300 nm | Improved stability over liposomes, no organic solvents used. | Limited drug loading capacity, potential for drug expulsion during storage. |
| Dendrimers | 5-10 nm | Monodisperse size, multivalent surface for functionalization. | Toxicity concerns at higher generations, complex synthesis. |
Visualizing Core Concepts
Diagram: Multi-Mechanism Strategy for BBB Penetration
Multi-Mechanism BBB Penetration Strategy
Diagram: Experimental Workflow for Validating Combination Strategies
Combination Strategy Validation Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for BBB Drug Delivery Research
| Item | Primary Function | Example Application |
|---|---|---|
| Brain Microvascular Endothelial Cells | Core functional unit of the in vitro BBB; forms tight junctions. | Establishing monoculture or co-culture permeability models [3] [4]. |
| Recombinant R-Spondin1, Noggin, EGF | Critical growth factors for organoid culture maintenance. | Generating and sustaining patient-derived organoids for personalized drug screening [79]. |
| EDC / NHS Crosslinkers | Zero-length crosslinkers for conjugating ligands to nanocarriers. | Covalently attaching targeting moieties (e.g., Transferrin) to nanoparticle surfaces [24]. |
| Claudin-5 / Occludin Antibodies | Immunostaining markers for tight junction integrity. | Visualizing and quantifying the quality of BBB models via fluorescence microscopy [3] [4]. |
| P-glycoprotein (P-gp) Substrates/Inhibitors | Probes for assessing active efflux transporter activity. | Determining the contribution of efflux pumps to drug permeability in BBB models [4] [14]. |
| TR-FRET Compatible Microplate Reader | Instrument for time-resolved Förster resonance energy transfer assays. | Running high-throughput kinase activity assays and other biochemical screens [75]. |
Weighing the Evidence: Preclinical and Clinical Validation of BBB Platforms
Technical Support Center
Q1: What are the core technological principles behind these brain-targeting platforms?
A: Each platform employs a distinct strategy to ferry therapeutic cargo across the blood-brain barrier (BBB).
- Roche's Brainshuttle and Denali's ATV (Antibody Transport Vehicle) both exploit receptor-mediated transcytosis (RMT). They are engineered to bind to specific transport receptors, such as the transferrin receptor (TfR1), which are naturally expressed on the BBB [80] [81] [82]. This binding hijacks the natural transport system to shuttle therapeutic molecules from the blood into the brain parenchyma.
- AAV-based platforms (like those referenced from Takara Bio and Caltech) utilize engineered viral capsids to facilitate CNS delivery [83] [84]. Following intravenous administration, these capsids can cross the BBB and transduce brain cells, enabling the delivery of genetic material.
Q2: What types of therapeutic cargo can each platform deliver?
A: The platforms are optimized for different classes of therapeutics.
- Brainshuttle & Denali's ATV: Primarily designed for the delivery of large biomolecules. Brainshuttle has been used to deliver antibodies [80] [82], while Denali's ATV platform is designed for antibodies, enzymes, proteins, and oligonucleotides [81].
- AAV Vectors: Specialized in gene delivery. They are used to transport genetic material (transgenes) into cells to enable long-term protein expression [83].
Q3: What quantitative improvements in brain exposure have been demonstrated?
A: Preclinical data show significant enhancements over conventional methods.
- Denali's ATV: In animal models, therapeutics using the ATV technology demonstrated more than 10- to 30-fold greater brain exposure compared to similar molecules without the technology [81].
- Roche's Brainshuttle: In a study with non-human primates, the Brainshuttle-based antibody trontinemab showed a 4–18-fold increase in brain exposure compared to the conventional antibody gantenerumab [80].
Q4: My AAV experiment resulted in low CNS transduction. What could be the cause?
A: Low transduction can result from several factors [84]:
- Mouse Strain Incompatibility: Certain engineered AAV capsids (e.g., AAV-PHP.B) require the mouse protein LY6A for efficient CNS transduction. Ensure your mouse strain (e.g., C57BL/6J) expresses the permissive form of this receptor.
- Suboptimal Dosing: The dose may be too low. For AAV-PHP.eB in adult mice, common doses range from 1x10^11 to 5x10^11 vector genomes (vg) per mouse.
- Incorrect Administration: Ensure intravenous injections (retro-orbital or tail vein) are performed correctly.
- Low Titer or degraded virus: Always re-titer your virus after shipping or long-term storage, as freeze-thaw cycles can degrade titer.
Q5: The auxiliary brake light on my CANsmart system is not functioning. What should I check?
A: This issue is unrelated to biomedical BBB platforms and pertains to a motorcycle accessory controller. Please consult the manufacturer's troubleshooting guide for circuit checks, fuse status, and software settings [85].
Quantitative Data Comparison
Table 1: Key Quantitative Metrics for Brain-Targeting Platforms
| Metric | Roche Brainshuttle | Denali ATV | AAV Vectors (General) |
|---|---|---|---|
| Reported Increase in Brain Exposure | 4-18 fold (in NHP) [80] | 10-30 fold (in animal models) [81] | Varies by serotype and capsid |
| Standard Experimental Dose (Mice) | Not Specified | Not Specified | 1x10^11 - 1x10^12 vg (IV) [84] |
| Time to Peak Expression | Not Specified | Not Specified | 2-4 weeks post-injection [84] |
| Primary Cargo | Antibodies [80] | Antibodies, Enzymes, Oligos [81] | Genetic Material (Genes) [83] |
| Core Technology | TfR1-Binding Bispecific Ab [80] | Engineered Fc Domain (e.g., TfR binding) [81] | Engineered Viral Capsid [84] |
Table 2: AAV Serotype and Promoter Selection Guide for CNS Targets
| Target Cell Population | Recommended AAV Serotype | Recommended Promoter | Notes |
|---|---|---|---|
| Broad CNS Neurons | AAV-PHP.eB [84] | CAG (strong, ubiquitous) [84] | Use in LY6A-permissive mouse strains. |
| Astrocytes | AAV-PHP.eB [84] | GfABC1D [84] | Provides efficient and selective expression. |
| General CNS | AAV9 [84] | CAG or Synapsin | Broad tropism, works in many species. |
| Peripheral & CNS | AAV-PHP.S [84] | CAG | Broad off-target transduction similar to AAV9. |
Experimental Protocols
Protocol 1: In Vivo Evaluation of AAV-Mediated Gene Delivery to the Mouse CNS
This protocol outlines the steps for systemic administration of AAV vectors for brain transduction in mice [84].
- Virus Preparation: Thaw AAV vector on ice. Dilute if necessary in DPBS or saline to achieve the desired dose in a volume of 40-80 µl per mouse. Do not exceed 150 µl for a 25g mouse.
- Animal Preparation: Use 6-8 week old adult mice. Anesthetize the mouse according to your institution's approved animal care protocol.
- Intravenous Injection: Perform a retro-orbital sinus injection or tail vein injection.
- For retro-orbital: Gently insert a sterile insulin syringe with a ½-inch 29G needle into the retro-orbital sinus and slowly depress the plunger.
- Recovery and Observation: Place the mouse in a clean cage on a warm pad until it fully recovers from anesthesia. Monitor for any immediate adverse effects.
- Incubation: Allow 2-4 weeks for transgene expression to reach peak levels.
- Tissue Analysis: Harvest brain tissue and analyze transgene expression via immunohistochemistry, Western blot, or other appropriate methods.
Protocol 2: Testing Brainshuttle-Mediated Antibody Delivery in Non-Human Primates
This protocol is derived from the methods used in the trontinemab (Brainshuttle) study [80].
- Test Article Administration: Administer the Brainshuttle-antibody fusion molecule (e.g., 10 mg/kg) or a control conventional antibody (e.g., 20 mg/kg) via a single intravenous bolus injection to NHPs (Macaca fascicularis).
- Sample Collection: Collect plasma and cerebrospinal fluid (CSF) at multiple time points post-dose for pharmacokinetic (PK) analysis. At terminal time points, perfuse animals and collect brain tissue.
- Tissue Processing: Homogenize brain tissue for quantitative PK analysis via ELISA. Additionally, flash-freeze brain regions for immunohistochemistry (IHC).
- Analysis:
- PK Modeling: Use nonlinear mixed-effects modeling on homogenate data to estimate brain exposure parameters, correcting for residual blood content.
- IHC: Perform immunofluorescence staining on brain sections to visualize and quantify antibody uptake into the brain endothelium and parenchyma, assessing distribution homogeneity.
Signaling Pathways and Workflows
Brainshuttle/ATV Transcytosis Mechanism
AAV-Mediated Gene Delivery Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Item | Function / Explanation | Example / Source |
|---|---|---|
| HEK 293T Cells | Production of AAV vectors. This cell line is highly transfectable and supports high levels of viral protein expression for generating high-titer AAV [83]. | AAVpro 293T Cell Line (Takara), HEK 293T/17 (ATCC CRL-11268) [83]. |
| AAV Purification Kit | Purification of AAV particles from cell lysates. Provides a faster and simpler alternative to traditional ultracentrifugation methods [83]. | AAVpro Purification Kit (All Serotypes) [83]. |
| AAV Titration Kit | Quantification of viral titer (vector genomes per mL) using real-time PCR. Essential for standardizing doses in animal experiments [83]. | AAVpro Titration Kit (for Real Time PCR) Ver.2 [83]. |
| Transferrin Receptor (TfR1) | Key receptor target for RMT. Binding to TfR1 is the core mechanism for the Brainshuttle and Denali ATV platforms to gain access to the brain [80] [81]. | N/A (Biological target) |
| Engineed AAV Capsids | Serotypes with enhanced CNS tropism. These are critical for efficient gene delivery to the brain after systemic administration [84]. | AAV-PHP.eB (broad CNS), AAV-PHP.S (PNS & CNS) [84]. |
| Cell-Type Specific Promoters | Drive transgene expression in specific brain cell types. Allows for targeted expression even with broadly transducing capsids [84]. | GfABC1D (astrocytes), CAG (ubiquitous), Synapsin (neurons) [84]. |
FAQs: Troubleshooting Blood-Brain Barrier Drug Delivery
Q1: Our antibody therapeutic shows poor brain penetration in preclinical models. What advanced strategies can improve delivery?
A1: Leverage receptor-mediated transcytosis (RMT) platforms, such as the Brainshuttle technology. This approach engineers bispecific antibodies that bind both your target (e.g., amyloid-beta) and a endogenous BBB transporter, like the transferrin receptor (TfR1). This "Trojan horse" mechanism actively shuttles the therapeutic antibody across the BBB, dramatically increasing brain concentration and allowing for lower, safer systemic doses compared to conventional antibodies [86] [87]. Be aware that TfR1-targeting can be associated with manageable side effects like infusion reactions and anemia [87].
Q2: We are developing an antisense oligonucleotide (ASO) for a genetic neurodegenerative disease. How can we achieve effective central nervous system delivery?
A2: For genetically-defined targets, consider intrathecal administration of ASOs. This approach, validated by the approved drug Tofersen for SOD1-ALS, delivers the therapy directly into the cerebrospinal fluid, bypassing the BBB entirely [88] [89]. For systemic administration, explore conjugating your ASO to a BBB-targeting moiety. Recent research has demonstrated the feasibility of using the TfR to transport ASOs across the BBB in vivo [87]. Monitor biomarkers like Neurofilament Light Chain (NfL) to confirm target engagement and biological effect [89].
Q3: When using focused ultrasound (FUS) for BBB opening, how do we monitor the procedure's safety and efficacy in real-time?
A3: Implement a multi-modal imaging protocol. MRI-guided FUS is the standard for precise targeting. Administer a gadolinium-based contrast agent and use T1-weighted contrast-enhanced (T1w-CE) MRI immediately after sonication to visually confirm and quantify BBB opening via signal hyperintensity [37]. For safety, monitor for potential tissue heating with MR thermometry and control the acoustic energy to avoid inertial cavitation of microbubbles, which can cause vascular damage [37]. Long-circulating nanoparticles are often essential to maximize delivery during the transient BBB opening window [90].
Quantitative Clinical Outcomes at a Glance
Table 1: Clinical Trial Outcomes for Trontinemab and Tofersen
| Therapeutic Agent | Indication | Key Trial Phase | Primary Efficacy Outcome | Key Safety Outcome | BBB Delivery Technology |
|---|---|---|---|---|---|
| Trontinemab | Alzheimer's Disease | Phase 1b/2a (Brainshuttle AD) | At 3.6 mg/kg: 91% of participants became amyloid PET-negative (≤24 centiloids) after 28 weeks [31] [91]. | ARIA-E rate: <5% in blinded data (N=4/149 across 1.8 and 3.6 mg/kg cohorts); all cases were mild [31] [91]. | Brainshuttle Platform (TfR1-mediated transcytosis) [91] [87] |
| Tofersen | SOD1-ALS | Phase 3 (VALOR & Open-Label Extension) | Sustained reduction of SOD1 protein & neurofilament light chain (NfL); 52% slower disease progression vs. expected in a real-world study [88] [89]. | Generally safe and well-tolerated; primary risk is associated with intrathecal administration procedure [88] [89]. | Intrathecal Delivery (Direct CSF administration) [88] |
Table 2: Technical Parameters for Focused Ultrasound-Mediated BBB Opening
| Parameter | Considerations & Typical Measurements | Imaging for Efficacy/Safety |
|---|---|---|
| Microbubbles (MBs) | FDA-approved ultrasound contrast agents; oscillate in ultrasound field [37] [90]. | T1-weighted Dynamic Contrast-Enhanced (DCE-) MRI to quantify BBB opening dynamics [37]. |
| Acoustic Pressure | Must be controlled to induce stable cavitation of MBs; inertial cavitation can cause vascular damage [37]. | MR thermometry to monitor for tissue heating [37]. |
| BBB Closure | Typically occurs within hours; transient and reversible [37] [90]. | Repeat T1w-CE MRI at 24 hours to confirm BBB reclosure [37]. |
| Therapeutic Window | Use long-circulating nanoparticles (e.g., PEG-PBAE NPs) to co-administer with FUS for maximal brain accumulation [90]. | PET imaging can be used to assess subsequent drug delivery [37]. |
Experimental Protocol: Focused Ultrasound-Mediated Nucleic Acid Delivery
This protocol outlines the methodology for targeted brain delivery of nucleic acids using FUS and long-circulating nanoparticles, based on a cited preclinical study [90].
Workflow Aim: To achieve site-specific gene editing in the mouse brain via systemic administration.
Step-by-Step Methodology:
- Nanoparticle (NP) Formulation: Engineer biodegradable poly(β-amino ester) (PBAE) polymers. Formulate NPs by compacting mRNA (e.g., encoding CRISPR-Cas9 and sgRNA) with a blend of PBAE and PEG-PBAE polymers to create PEG-PBAE/mRNA NPs. Characterize NPs for size (~60-65 nm), surface charge (~+2 mV), and colloidal stability in serum [90].
- Animal Preparation: Anesthetize male C57BL/6 mice and secure them in a stereotactic frame compatible with the FUS transducer.
- Systemic Administration: Administer the PEG-PBAE/mRNA NPs via tail vein injection at a nucleic acid dose of 0.5 mg/kg [90].
- Microbubble Injection: Intravenously inject clinically approved microbubbles.
- FUS Application: Use an MRI-guided FUS system to target a specific brain coordinate. Apply low acoustic pressure to induce stable cavitation of the microbubbles, temporarily disrupting the BBB without causing inertial cavitation and vascular damage [37] [90].
- Confirmation of BBB Opening: Immediately after sonication, perform T1-weighted contrast-enhanced (T1w-CE) MRI after injecting a gadolinium-based contrast agent. A hyperintense signal in the targeted region confirms successful and localized BBB opening [37].
- Analysis of Delivery and Effect:
- Efficacy: After 24-48 hours, sacrifice the animals and analyze the FUS-targeted brain region for reporter protein expression or CRISPR-Cas9-mediated genome editing using immunohistochemistry, Western blot, or next-generation sequencing.
- Safety: Analyze adjacent brain sections for markers of vascular damage (e.g., fibrinogen extravasation) or inflammation (e.g., glial activation) to confirm the procedure's safety profile [37].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Advanced BBB Drug Delivery Research
| Reagent / Material | Function / Rationale | Example Application |
|---|---|---|
| Bispecific Antibody Constructs | Engineered to bind both a BBB receptor (e.g., TfR1) and a CNS target; enables receptor-mediated transcytosis. | Trontinemab: Gantenerumab antibody fused to a TfR1-binding Fab fragment [91] [87]. |
| Antisense Oligonucleotides (ASOs) | Synthetic single-stranded nucleotides designed to selectively bind and modulate RNA targets. | Tofersen: Binds SOD1 mRNA to reduce production of mutant SOD1 protein in ALS [88] [89]. |
| Gas-Filled Microbubbles | FDA-approved ultrasound contrast agents; oscillate in an ultrasound field to mechanically disrupt the BBB. | Used as a cavitation agent in conjunction with FUS to transiently and reversibly open the BBB [37] [90]. |
| Long-Circulating Nanoparticles (e.g., PEG-PBAE NPs) | Polyethylene glycol (PEG) coating provides "stealth" properties, reducing clearance and enhancing systemic circulation time. | Co-administered with FUS to deliver nucleic acid payloads (pDNA, mRNA) across the opened BBB [90]. |
| Gadolinium-Based Contrast Agents | Small molecules that, when leaking into the brain parenchyma, cause hyperintensity on T1-weighted MRI scans. | The gold-standard method for visualizing, quantifying, and confirming the location and volume of FUS-induced BBB opening [37]. |
FAQs: Core Pharmacokinetic Concepts for Bispecific Antibodies
FAQ 1: What is the primary mechanism that enables bispecific antibodies to cross the blood-brain barrier (BBB) effectively?
The primary mechanism is receptor-mediated transcytosis (RMT), which hijacks endogenous transport systems at the BBB. The most widely used system targets the transferrin receptor 1 (TfR1) [30] [92]. A bispecific antibody is engineered with one arm binding to TfR1 to facilitate transport across the brain endothelial cells, and the other arm binding to the therapeutic target in the brain (e.g., amyloid-beta in Alzheimer's disease) [27]. This approach results in significantly higher and more uniform brain concentrations compared to conventional monoclonal antibodies [30].
FAQ 2: How do the affinity and valency of TfR1-binding impact brain delivery and distribution?
Optimizing affinity and valency is critical for efficient transcytosis and target engagement.
- Affinity: Moderate affinity for TfR1 is generally beneficial. Antibodies with very high affinity may become trapped on the vascular endothelium, reducing their ability to complete transcytosis and enter the brain parenchyma [30] [92].
- Valency: Monovalent binding to TfR1 is often preferred over bivalent binding. Monovalent binding promotes receptor recycling and productive transport across the BBB, whereas bivalent binding can cause receptor clustering and degradation, hindering transcytosis [30] [92].
- Target Engagement: The affinity for TfR1 should be lower than the affinity for the primary therapeutic target in the brain. This ensures that once the antibody crosses the BBB, it dissociates from TfR1 and can engage its intended pathological target [30].
FAQ 3: What are the key pharmacokinetic differences between full-sized IgG bispecific antibodies and smaller bispecific formats?
The size and structure of the bispecific molecule significantly influence its systemic clearance, brain entry, and intrabrain distribution, as shown in comparative studies [93].
Table: Pharmacokinetic Comparison of Bispecific Antibody Formats
| Parameter | Full-sized IgG Bispecific (e.g., mAb3D6-scFv8D3, 210 kDa) | Smaller Bispecific Format (e.g., di-scFv3D6-8D3, 58 kDa) |
|---|---|---|
| Systemic Clearance | Slower clearance from blood [93] | Faster clearance from blood [93] |
| Brain Cmax | Higher maximum brain concentration [93] | Lower maximum brain concentration [93] |
| Parenchymal Delivery | Slower delivery to brain parenchyma [93] | Faster delivery to brain parenchyma; larger parenchymal-to-capillary ratio [93] |
| Elimination from Brain | Net elimination from brain at a later time point [93] | Net elimination from brain at an earlier time point [93] |
| FcRn Interaction | Interacts with FcRn, prolonging serum half-life [93] | Lacks Fc region, so no FcRn recycling, leading to shorter half-life [93] |
FAQ 4: After crossing the BBB, what factors influence the distribution and clearance of bispecific antibodies within the brain?
Post-transcytosis dynamics are complex and influenced by several factors:
- Distribution: Smaller antibody formats (e.g., single-domain antibodies, scFvs) generally show more diffuse and deeper penetration into the brain parenchyma compared to full-sized IgGs, due to less hindered diffusion in the extracellular space [93].
- Retention: Binding to the specific target antigen in the brain (e.g., amyloid plaques) can significantly increase the retention time of the antibody within the brain [30].
- Clearance Pathways: Antibodies can be cleared from the brain via bulk flow through perivascular spaces or other interstitial fluid pathways, or through catabolic degradation within brain cells [93]. The elimination rate from the brain parenchyma may not always directly correlate with the molecule's size or its systemic clearance rate [93].
Troubleshooting Common Experimental Challenges
Challenge 1: Low Brain Uptake of Bispecific Antibody
- Potential Cause: The TfR1-binding arm has an affinity that is too high, causing the antibody to be sequestered at the BBB rather than being transported across it [30] [92].
- Solution: Re-engineer the TfR1-binding arm to have a lower, monovalent affinity. Consider implementing pH-sensitive binding, which promotes dissociation from TfR1 in the acidic environment of the endosome, enhancing release into the brain parenchyma [30] [92].
Challenge 2: Inefficient Target Engagement Despite Demonstrated Brain Uptake
- Potential Cause: The bispecific antibody has a higher affinity for TfR1 than for its therapeutic target. This causes it to remain bound to TfR1-expressing cells (e.g., neurons) after transcytosis, instead of engaging the intended pathological target [30].
- Solution: Optimize the binding kinetics so that the affinity for the therapeutic target is stronger than the affinity for TfR1. This ensures effective release from the transporter and engagement with the disease target [30].
Challenge 3: Rapid Systemic Clearance Limiting Brain Exposure
- Potential Cause: Using a bispecific format that lacks an Fc region (e.g., scFv-based constructs), preventing interaction with the neonatal Fc receptor (FcRn) that is responsible for recycling antibodies and extending their plasma half-life [93].
- Solution: For indications requiring sustained systemic exposure, consider using an IgG-based bispecific format that retains a functional Fc region capable of binding to FcRn [93].
Experimental Protocols for Assessing Brain Pharmacokinetics
Protocol 1: In Vivo Brain Uptake and Pharmacokinetics Study in Mice
This protocol outlines the key steps for quantitatively measuring the brain entry, distribution, and clearance of a radiolabeled bispecific antibody [93].
- Antibody Radiolabeling: Label the bispecific antibody with a radioisotope such as Iodine-125 (¹²⁵I) using the Chloramine-T method. Purify the labeled antibody from free iodine using a size-exclusion column (e.g., NAP-5) [93].
- Animal Dosing and Tissue Collection:
- Inject groups of wild-type mice (e.g., C57/Bl6) intravenously with the radiolabeled antibody.
- Euthanize animals at multiple time points post-injection (e.g., 2, 4, 6, 8, 12, 16, 24 hours) to establish a pharmacokinetic profile.
- Collect blood via cardiac puncture, and perfuse the animals transcardially with ice-cold saline to clear blood from the cerebral vasculature.
- Harvest the brain and other peripheral organs of interest [93].
- Quantitative Analysis:
- Measure radioactivity in the blood, brain, and other tissues using a gamma counter.
- Calculate the percentage of the injected dose per gram of tissue (%ID/g) for each sample [93].
- Capillary Depletion: To distinguish antibody that has entered the brain parenchyma from antibody remaining in the capillaries, homogenize the brain in a buffer and separate the capillary fraction from the parenchymal supernatant via dextran density centrifugation. Measure radioactivity in both fractions [93].
- Spatial Distribution Analysis: Perform ex vivo autoradiography or nuclear track emulsion on brain sections to visualize the spatial distribution of the radiolabeled antibody throughout different brain regions [93].
The workflow for this protocol is summarized in the diagram below:
Protocol 2: In Vitro BBB Penetration Assay using 3D Assembloids
This method uses a more physiologically relevant 3D in vitro model to screen antibody penetration potential [94].
- Model Establishment:
- Use a microwell plate (e.g., Millicell Microwell 96-well plate) designed for 3D culture.
- Seed brain endothelial cells, pericytes, and astrocytes simultaneously into the microwells.
- Allow the cells to self-assemble into BBB assembloids over 48 hours. A mature assembloid will show distinct layers: endothelial cells on the outside, surrounding pericytes, which in turn surround a core of astrocytes [94].
- Antibody Incubation: Incubate the assembloids with the bispecific antibody of interest for a set period (e.g., up to 6 hours) [94].
- Fixation and Staining: Fix the assembloids and immunostain them directly in the plate.
- Use markers for each cell type: P-gP (endothelial cells), NG2 (pericytes), GFAP (astrocytes), and DAPI (nuclei).
- Use a fluorescently labeled secondary antibody to detect the test bispecific antibody [94].
- Imaging and Quantification: Image the assembloids using confocal microscopy. Quantify the antibody penetration by measuring the fluorescent intensity from the outer endothelial layer towards the inner astrocyte core, comparing it to control antibodies (e.g., a non-targeting human IgG) [94].
The Scientist's Toolkit: Key Reagents and Models
Table: Essential Tools for Bispecific Antibody BBB Research
| Tool / Reagent | Function and Utility in Research |
|---|---|
| Anti-TfR1 Binding Moieties | Critical component of the bispecific antibody for engaging the TfR1-mediated transcytosis pathway. Cross-species single-domain antibodies (VHHs) are often used [92]. |
| Radiolabels (e.g., ¹²⁵I) | Allow for highly sensitive and quantitative tracking of antibody distribution in vivo and ex vivo using gamma counting and autoradiography [93]. |
| ³H-/¹⁴C-labeled Inulin | A radiolabeled polysaccharide used as a vascular space marker in capillary depletion experiments to assess the efficiency of vascular perfusion [93]. |
| BBB Assembloids (3D in vitro model) | A multicellular, high-throughput in vitro model comprising endothelial cells, astrocytes, and pericytes. Useful for initial screening of antibody penetration and cell-specific binding [94]. |
| Capillary Depletion Protocol | An ex vivo method that separates brain capillaries from the parenchyma, allowing researchers to distinguish antibody that has truly entered the brain from antibody retained in the vasculature [93]. |
| ImmunoPET Imaging | A non-invasive in vivo imaging technique (e.g., using ⁸⁹Zr-labeled antibodies) that enables longitudinal tracking of antibody biodistribution and target engagement in the same subject over time [30] [92]. |
The process of TfR1-mediated transcytosis, a central mechanism for bispecific antibody brain delivery, involves several key steps as illustrated below:
Frequently Asked Questions (FAQs)
Q1: What are the key quantitative imaging biomarkers for assessing Blood-Brain Barrier (BBB) permeability, and how do they differ between MRI and PET?
A1: The key quantitative biomarkers are the transfer constant (Ktrans) for Dynamic Contrast-Enhanced MRI (DCE-MRI) and the permeability-surface area product (PS) and transport rate (K1) for PET. Their characteristics and applications are summarized in the table below.
Table 1: Key Quantitative Biomarkers for BBB Permeability Imaging
| Imaging Modality | Key Biomarker(s) | Typical Agent/Radiotracer | Normal BBB Permeability Range | Interpretation & Context |
|---|---|---|---|---|
| DCE-MRI | Transfer Constant (Ktrans) | Gd-DOTA (<1 nm) | ~0.16 - 0.94 × 10⁻³ min⁻¹ [95] | Measures passive leakage; higher values indicate structural disruption. |
| DCE-MRI | Transfer Constant (Ktrans) | AGuIX Nanoparticles (~5 nm) | ~0.16 - 0.94 × 10⁻³ min⁻¹ [95] | More sensitive to subtle permeability changes due to larger size. |
| PET | Permeability-Surface Area (PS) & Transport Rate (K1) | ¹¹C-Butanol | ~0.427 ml/min/cm³ (K1 in grey matter) [96] | A flow tracer; K1 approximates cerebral blood flow (CBF). |
| PET | Permeability-Surface Area (PS) & Transport Rate (K1) | ¹⁸F-FDG | ~0.173 ml/min/cm³ (K1 in grey matter) [96] | Reflects transport via GLUT1 transporters; PS is ~10⁻¹ ml/min/cm³ [96]. |
| PET | Permeability-Surface Area (PS) & Transport Rate (K1) | ¹⁸F-Fluciclovine | Lower than ¹⁸F-FDG & ¹¹C-Butanol [96] | Reflects transport via specific amino acid transporters. |
Q2: Our preclinical DCE-MRI data shows minimal Ktrans increase after focused ultrasound. Is the BBB opening insufficient, or is our methodology flawed?
A2: Several methodological factors could lead to an underestimation of BBB opening:
- Contrast Agent Size: Standard small-molecule gadolinium chelates (e.g., Gd-DOTA, <1 nm) may be less sensitive to subtle permeability changes. Using larger nanoparticles like AGuIX (~5 nm) can provide a higher dynamic range and significantly better sensitivity for detecting permeability changes, as demonstrated in stroke models [95].
- Temporal Resolution: DCE-MRI requires high temporal resolution to accurately capture the rapid kinetics of contrast agent arrival and passage. Inadequate sampling can lead to errors in Ktrans calculation.
- Model Selection: Using an inappropriate pharmacokinetic model for your data can yield inaccurate results. Ensure the model (e.g., Tofts, Extended Tofts) aligns with the physiology being studied.
Q3: Why would we need a new PET method when the established dual-tracer approach for measuring BBB permeability already exists?
A3: The conventional dual-tracer method, which requires one PET scan for the target tracer and another for a blood flow tracer (e.g., ¹⁵O-water), faces significant practical hurdles that limit its clinical and research application [96] [97]:
- Logistical Complexity: Coordinating two separate scans is costly and time-consuming.
- Short Half-Lives: Many flow tracers have very short half-lives (e.g., ² minutes for ¹⁵O), necessitating an on-site cyclotron, which is an expensive piece of equipment not available at most hospitals [97].
- The new single-scan, High-Temporal-Resolution (HTR) PET method, enabled by total-body scanners like EXPLORER, overcomes these limitations. It uses advanced kinetic modeling on early dynamic data (1-2 second frames) from a single tracer injection to jointly estimate both cerebral blood flow (CBF) and the tracer-specific transport rate (K1), from which PS is derived [96] [97].
Q4: Can these imaging techniques monitor the efficacy of a drug intended to protect the BBB?
A4: Yes, quantitative Ktrans from DCE-MRI can serve as a pharmacodynamic biomarker to monitor therapeutic response. For example, in a non-human primate stroke model, treatment with ciclosporin A resulted in a statistically significant reduction in Ktrans for both Gd-DOTA and AGuIX nanoparticles within the ischemic lesion compared to the placebo group. This demonstrated the drug's protective effect on the BBB in the context of ischemia-reperfusion injury [95].
Troubleshooting Guides
Issue 1: Low Signal-to-Noise or Poor Sensitivity in Detecting BBB Modulation
Potential Causes and Solutions:
- Cause: Suboptimal Contrast Agent.
- Solution: For DCE-MRI, consider switching from small clinical gadolinium chelates (Gd-DOTA) to ultra-small nanoparticles like AGuIX. Their larger size (~5 nm) makes their passage more sensitive to subtle changes in BBB permeability, providing a stronger and more quantifiable signal for a given level of disruption [95].
- Cause: Inadequate Temporal or Spatial Resolution.
- Solution: For PET, employ a high-temporal-resolution (HTR) dynamic imaging protocol (1-2 second frames) enabled by modern total-body scanners. This is crucial for accurately resolving the tracer's first pass and for applying advanced kinetic models like the Adiabatic Approximation to the Tissue Homogeneity (AATH) model to jointly estimate CBF and K1 [96].
Issue 2: Inconsistent or Physiologically Implausible Kinetic Modeling Results
Potential Causes and Solutions:
- Cause: Use of an Oversimplified Kinetic Model.
- Solution: When analyzing HTR PET data, the standard one-tissue compartment model may be insufficient. Implement the AATH model, which accounts for the finite intravascular transit time of the tracer, providing more robust and physiologically accurate estimates of CBF and K1 [96].
- Cause: Inaccurate Arterial Input Function (AIF).
- Solution: Leverage the capabilities of a long axial field-of-view PET scanner (e.g., EXPLORER) to derive an image-based AIF directly from the ascending aorta, synchronized with the brain data. This non-invasive approach avoids the need for error-prone invasive arterial blood sampling and minimizes delay and dispersion effects [96].
Experimental Protocols
Protocol 1: Quantifying BBB Permeability to Nanoparticles in a Preclinical Stroke Model Using DCE-MRI
This protocol is adapted from a study using a non-human primate model of middle cerebral artery occlusion [95].
1. Experimental Setup:
- Animal Model: Establish an endovascular stroke model (e.g., middle cerebral artery occlusion) with reperfusion via mechanical thrombectomy.
- Contrast Agents: Prepare both a small molecule agent (Gd-DOTA, <1 nm) and AGuIX nanoparticles (~5 nm, ~10 kDa). AGuIX nanoparticles are composed of a polysiloxane network and gadolinium chelates, providing high relaxivity and potential for radiolabelling [95].
- Imaging System: A PET-MRI scanner is required if combining with PET imaging.
2. Imaging Procedure:
- Baseline Scan: Acquire a pre-contrast MRI for baseline signal intensity.
- Contrast Injection: Administer a clinical dose of the contrast agent via intravenous bolus.
- Dynamic Acquisition: Immediately initiate a DCE-MRI sequence with high temporal resolution to track the passage of the contrast agent through the brain vasculature over time.
3. Data Analysis:
- Region of Interest (ROI): Manually or automatically delineate the ischemic core, the peri-infarct area (ischemic growth area), and the contralateral healthy hemisphere.
- Pharmacokinetic Modeling: Fit the signal intensity time curves from each ROI to a pharmacokinetic model (e.g., the Tofts model) to compute the volume transfer constant, Ktrans (min⁻¹).
- Statistical Comparison: Compare Ktrans values between the ischemic and contralateral hemispheres. To assess treatment, compare Ktrans in the ischemic region between drug-treated and placebo groups.
Experimental Workflow for Preclinical DCE-MRI BBB Assessment
Protocol 2: Single-Scan Quantification of Molecular BBB Permeability in Humans Using HTR PET
This protocol outlines the novel method for measuring the permeability-surface area product (PS) of any molecular radiotracer using a single PET scan [96].
1. Subject Preparation and Tracer Injection:
- Radiotracer Selection: Choose a PET radiotracer based on the molecular transport mechanism of interest (e.g., ¹⁸F-FDG for GLUT1, ¹⁸F-fluciclovine for amino acid transporters).
- Injection: Administer the radiotracer as an intravenous bolus.
2. Image Acquisition:
- Scanner: Use a total-body PET scanner with long axial field-of-view (e.g., uEXPLORER).
- Dynamic Scan Protocol: Initiate a high-temporal-resolution dynamic scan simultaneously with the tracer injection. The recommended protocol is 60 frames x 1 second, immediately followed by 30 frames x 2 seconds, covering the first two minutes post-injection [96].
3. Image-Derived Input Function:
- AIF Extraction: From the dynamic images, draw a volume of interest (VOI) over the ascending aorta to obtain a high-fidelity, image-derived arterial input function, eliminating the need for arterial blood sampling [96].
4. Kinetic Modeling and Analysis:
- Model Fitting: For each voxel or region of interest, fit the early time-activity curves (first 2 minutes of data) using the Adiabatic Approximation to the Tissue Homogeneity (AATH) model.
- Parameter Estimation: The AATH model jointly estimates five key parameters from the single HTR scan:
- CBF: Cerebral Blood Flow
- K1: Tracer-specific unidirectional transport rate from blood to brain
- k2: Clearance rate from brain to blood
- Tc: Mean vascular transit time
- td: Time delay
- PS Calculation: The permeability-surface area product can be derived from the estimated CBF and K1 values.
Workflow for Single-Scan HTR PET BBB Permeability Quantification
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for BBB Permeability Experiments
| Item Name | Function/Application | Key Characteristics |
|---|---|---|
| AGuIX Nanoparticles | Theranostic contrast agent for sensitive DCE-MRI of BBB permeability [95]. | ~5 nm diameter, polysiloxane network with gadolinium chelates, high r1 relaxivity, potential for radiolabelling (PET), fast renal clearance. |
| ¹⁸F-FDG (Fluorodeoxyglucose) | PET radiotracer to assess BBB transport via GLUT1 transporters and cerebral metabolism [96]. | Well-characterized radiotracer; BBB permeability-surface area product is on the order of 10⁻¹ ml/min/cm³. |
| ¹⁸F-Fluciclovine | PET radiotracer to assess BBB transport via amino acid transporters [96]. | Used to study specific nutrient transport systems at the BBB. |
| Ciclosporin A | Reference compound for testing BBB-protective therapeutics in preclinical models [95]. | Drug shown to significantly reduce Ktrans (BBB leakage) in a stroke reperfusion model. |
| uEXPLORER Total-Body PET Scanner | Imaging system enabling High-Temporal-Resolution (HTR) dynamic PET for single-scan BBB permeability quantification [96] [97]. | Long axial field-of-view, ultra-high sensitivity, allows for image-derived input function and frame rates of 1-2 seconds. |
| Adiabatic Approximation to the Tissue Homogeneity (AATH) Model | Advanced kinetic model for analyzing HTR PET data [96]. | Accounts for intravascular tracer transit time; jointly estimates CBF and K1 from a single scan. |
This technical support document addresses the critical challenge of Amyloid-Related Imaging Abnormalities (ARIA) in the context of novel Alzheimer's disease (AD) therapeutics, particularly anti-amyloid monoclonal antibodies (mAbs). The recent approval of agents like Lecanemab and Donanemab represents a promising therapeutic advance; however, their efficacy is coupled with a significant risk of ARIA, creating a crucial safety-efficacy trade-off that researchers must navigate [63].
The table below summarizes the core relationship between enhanced therapeutic efficacy and the emergence of ARIA as a primary adverse event.
| Therapeutic Goal | Associated Efficacy | Primary Safety Risk (ARIA) | Key Risk Factors |
|---|---|---|---|
| Enhanced amyloid plaque clearance via mAbs (e.g., Lecanemab, Donanemab) | Enables microglial-mediated phagocytosis of protofibrils and plaques [63] | Amyloid-Related Imaging Abnormalities (ARIA) [63] | • ApoE ε4 carrier status (≈15% incidence in homozygotes) [63]• Dose-dependent effects (ARIA-Edema) [63] |
The following sections provide a detailed troubleshooting guide and resource toolkit to support your research and development efforts in overcoming this central challenge.
↑ Frequently Asked Questions (FAQs) & Troubleshooting Guide
FAQ 1: Why is ARIA a predominant safety concern for novel Anti-Amyloid therapies?
- The Issue: Researchers observe a high incidence of ARIA in clinical trials for biologics targeting amyloid-beta.
- The Explanation: ARIA is believed to be an anti-amyloid mAb class effect. The mechanism involves enhanced phagocytosis of amyloid plaques, which can lead to increased vascular permeability and edema (ARIA-E) or the removal of amyloid from fragile cerebral blood vessels, resulting in microhemorrhages (ARIA-H) [63]. This is a direct consequence of the drug's intended pharmacodynamic action.
- Troubleshooting & Risk Mitigation:
- Stratify Patient Populations: Prioritize ApoE genotyping in trial design. The incidence of ARIA is significantly higher in homozygote ApoE ε4 carriers (approximately 15%) [63].
- Implement Dosing Titration: Consider initiating treatment with a lower dose and gradually escalating to the full maintenance dose to mitigate the risk and severity of ARIA, particularly ARIA-Edema, which has been observed to be partly dose-dependent [63].
- Establish Rigorous MRI Monitoring Protocols: Develop a mandatory and frequent MRI monitoring schedule for early detection of ARIA, especially during the first few months of treatment and following any dose increase.
FAQ 2: The Blood-Brain Barrier (BBB) severely limits drug delivery. How can we enhance brain penetration without exacerbating risks like ARIA?
- The Issue: Low BBB penetration for large molecules (>98% of small-molecule drugs and nearly 100% of larger therapeutics are restricted) leads to subtherapeutic drug concentrations in the brain, requiring high systemic doses that may increase off-target side effects [7] [4].
- The Explanation: The BBB is a complex structure of endothelial cells with tight junctions, pericytes, and astrocyte end-feet that protect the brain but also impede therapeutics [3] [11]. Novel delivery strategies aim to overcome this barrier more efficiently, which could potentially allow for lower and safer systemic dosing.
- Troubleshooting & Potential Solutions:
- Strategy: Focused Ultrasound (FUS) with Microbubbles
- Protocol: Systemically inject microbubbles and apply low-intensity FUS to a targeted brain region. The microbubbles oscillate, temporarily and reversibly disrupting the BBB's tight junctions [63].
- Considerations: Preclinical data shows this can enhance mAb delivery. However, the act of BBB disruption itself requires careful safety assessment in the context of ARIA risk [63].
- Strategy: Receptor-Mediated Transcytosis (RMT)
- Protocol: Engineer therapeutics or nanocarriers to display ligands (e.g., targeting the transferrin or insulin receptor). This hijacks the brain's natural nutrient transport system to ferry drugs across the endothelial cells [63] [3].
- Considerations: This is a non-invasive, targeted strategy that could improve brain uptake without broadly disrupting the BBB, potentially offering a better safety profile [11].
- Strategy: Nanoparticle Carrier Systems
- Protocol: Encapsulate drugs in nanoparticles (e.g., polymeric, lipid-based). Surface modifications with targeting ligands (peptides, antibodies) or PEGylation can further enhance BBB crossing and targeting [63] [98] [11].
- Considerations: This approach can protect the drug, allow for controlled release, and reduce systemic exposure. The safety of long-term accumulation of some nanocarriers requires further study [98].
- Strategy: Focused Ultrasound (FUS) with Microbubbles
FAQ 3: What key reagents and methodologies are essential for studying BBB penetration and ARIA-related pathways?
- The Issue: A lack of standardized tools and models for evaluating both drug delivery efficiency and associated safety signals like vascular injury.
- The Explanation: A multi-faceted approach is needed, combining advanced in vitro, in vivo, and analytical techniques.
- Troubleshooting & Research Reagent Solutions: The following table details key reagents and their applications in this field.
| Research Reagent / Material | Primary Function in Research | Key Application Notes |
|---|---|---|
| In Vitro BBB Models (e.g., co-culture of brain endothelial cells, pericytes, astrocytes) [3] | Mimics human BBB physiology for high-throughput screening of permeability and transcytosis mechanisms [3]. | Critical for initial assessment of candidate molecules and delivery systems before moving to complex in vivo studies. |
| ApoE ε4 Transgenic Mice | Preclinical model to investigate the heightened risk of ARIA in a genetically susceptible background [63]. | Essential for evaluating the safety profile of new therapeutics and delivery methods in a high-risk context. |
| Microbubbles for FUS [63] | Used in conjunction with Focused Ultrasound to induce temporary, localized BBB opening in preclinical models. | Allows investigation of enhanced drug delivery and its direct physiological consequences on the neurovasculature. |
| Ligands for RMT (e.g., anti-Transferrin Receptor antibodies) [63] [4] | Functionalized onto drug cargo or nanoparticles to facilitate receptor-mediated transport across the BBB endothelium. | A key reagent for developing "Trojan horse" strategies to improve brain uptake of biologics. |
| Zr-89 for Immuno-PET [63] | Radioisotope for labeling antibodies (e.g., with desferrioxamine, DFO). Enables non-invasive, quantitative tracking of mAb biodistribution and brain uptake. | Provides critical pharmacokinetic and biodistribution data for novel therapeutics and delivery methods in vivo. |
↑ Essential Experimental Protocols & Workflows
↑ Protocol 1: Evaluating Drug Delivery Using Focused Ultrasound (FUS)
This protocol outlines a methodology for assessing the enhancement of therapeutic delivery to the brain using FUS.
1. Materials and Reagents:
- Animal model (e.g., transgenic AD mouse)
- FUS system with image guidance (e.g., MRI-guided FUS)
- Intravenous microbubble suspension (e.g., DEFINITY)
- Therapeutic agent of interest (e.g., fluorescently tagged or radio-labeled mAb)
- MRI contrast agent (e.g., Gadodiamide) for confirming BBB opening
2. Step-by-Step Workflow: 1. Anesthetize and Position Animal: Secure the animal in a stereotactic frame compatible with the FUS transducer and imaging system. 2. Administer Microbubbles: Inject microbubbles intravenously as a bolus. 3. Apply FUS: Target the desired brain region with low-intensity FUS pulses. Sonicate after microbubble injection to induce stable cavitation and transient BBB opening [63]. 4. Confirm BBB Disruption: Administer an MRI contrast agent and perform T1-weighted imaging to confirm localized BBB opening via signal enhancement in the targeted region. 5. Administer Therapeutic: Inject the therapeutic agent intravenously. 6. Tissue Analysis: After a predetermined circulation time, perfuse the animal and collect brain tissue for analysis (e.g., fluorescence imaging, gamma counting, immunohistochemistry) to quantify drug delivery.
The following diagram illustrates the core mechanism of this protocol.
↑ Protocol 2: Monitoring mAB Pharmacokinetics and ARIA with Immuno-PET/MRI
This protocol describes a non-invasive method for tracking a therapeutic antibody's brain uptake and subsequent pathological responses.
1. Materials and Reagents:
- Animal model or human subjects
- Therapeutic mAb (e.g., anti-amyloid antibody)
- Zirconium-89 (⁸⁹Zr) isotope
- Chelator (e.g., desferrioxamine, DFO)
- PET/MRI imaging system
2. Step-by-Step Workflow: 1. Radiolabel mAb: Conjugate the therapeutic mAb with the chelator DFO. Radiolabel the DFO-mAb conjugate with ⁸⁹Zr and purify the product [63]. 2. Inject Radioligand: Administer the ⁸⁹Zr-labeled mAb intravenously at a therapeutically relevant dose. 3. Acquire Serial PET Scans: Conduct longitudinal PET imaging at multiple time points (e.g., 6, 24, 48, 72 hours post-injection) to non-invasively monitor and quantify the mAb's accumulation in the brain [63]. 4. Acquire Coregistered MRI: Perform high-resolution T2-weighted and T2*-weighted/GRE MRI scans in tandem with PET to screen for the emergence of ARIA-E (vasogenic edema) and ARIA-H (microhemorrhages), respectively. 5. Data Analysis: Co-register PET and MRI data. Quantify brain uptake of the mAb from PET data and correlate these values spatially and temporally with the presence of ARIA identified on MRI.
The workflow for this integrated imaging approach is mapped below.
↑ The Scientist's Toolkit: Key Research Reagent Solutions
The following table expands on the essential materials required for advanced research in this field, building on the reagents mentioned in the FAQs.
| Research Reagent / Material | Primary Function in Research | Key Application Notes |
|---|---|---|
| In Vitro BBB Models [3] | Mimics human BBB physiology for high-throughput screening of permeability and transcytosis. | Allows for initial, rapid assessment of candidate molecules and delivery systems. |
| ApoE ε4 Transgenic Mice [63] | Preclinical model to investigate the heightened risk of ARIA in a genetically susceptible background. | Essential for evaluating the safety profile of new therapeutics in a high-risk context. |
| Microbubbles for FUS [63] | Used with Focused Ultrasound to induce temporary, localized BBB opening in preclinical models. | Enables the study of enhanced drug delivery and its direct physiological consequences. |
| Ligands for RMT [63] | Functionalized onto drug cargo or nanoparticles to facilitate receptor-mediated transport across the BBB. | A key reagent for developing "Trojan horse" strategies to improve brain uptake of biologics. |
| Zr-89 for Immuno-PET [63] | Radioisotope for labeling antibodies. Enables non-invasive, quantitative tracking of mAb biodistribution. | Provides critical pharmacokinetic and biodistribution data for novel therapeutics in vivo. |
| Anti-Amyloid mAbs (e.g., Lecanemab) [63] | Reference therapeutic for studying efficacy (amyloid reduction) and liability (ARIA induction). | Serves as a positive control in models designed to assess novel delivery systems or safety mitigations. |
| PEGylated Liposomes [98] [4] | Versatile nanoparticle platform for drug encapsulation, improving circulation time and enabling surface modification. | A foundational material for constructing custom nanocarrier-based delivery systems. |
Conclusion
The field of BBB drug delivery is undergoing a transformative shift, moving from insurmountable challenge to a tractable engineering problem. The convergence of receptor-mediated shuttles, physical disruption techniques, and sophisticated nanocarriers provides a powerful, multi-pronged arsenal. Future progress hinges on interdisciplinary collaboration, the development of refined preclinical models that accurately predict human outcomes, and a deepened understanding of disease-specific BBB alterations. The integration of AI-driven carrier design and patient-specific precision medicine approaches promises to usher in a new era of effective therapeutics for neurodegenerative diseases, turning past failures into future successes.
References
- 1. Research developments in the neurovascular unit and the blood‑brain barrier (Review) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11956146/]
- 2. Construction and imaging of a neurovascular unit model - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8820720/]
- 3. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 4. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 5. The neurovascular unit - concept review - PubMed [https://pubmed.ncbi.nlm.nih.gov/24629161/]
- 6. Drug Delivery Challenges in Brain Disorders across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8698904/]
- 7. Evolving Drug Delivery Strategies to Overcome the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4900538/]
- 8. Navigating Regional Heterogeneity of the Neurovascular Unit [https://pmc.ncbi.nlm.nih.gov/articles/PMC8277940/]
- 9. Anatomy, Head and Neck: Blood Brain Barrier - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK519556/]
- 10. Structure, Function, and Regulation of the Blood-Brain ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00914/full]
- 11. Drug Delivery Across the Blood–Brain Barrier: A New Strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11677317/]
- 12. Blood–brain barrier [https://en.wikipedia.org/wiki/Blood%E2%80%93brain_barrier]
- 13. Physiology, Blood Brain Barrier - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557721/]
- 14. Frontiers and Challenges in Brain Drug Delivery [https://www.sciencedirect.com/science/article/abs/pii/S1773224725011621]
- 15. Overcoming the Blood–Brain Barrier: Advanced Strategies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388969/]
- 16. 腦部穿梭技術突破血腦屏障為腦部疾病治療帶來新希望 [https://geneonline.news/%E8%85%A6%E9%83%A8%E7%A9%BF%E6%A2%AD%E6%8A%80%E8%A1%93%E7%AA%81%E7%A0%B4%E8%A1%80%E8%85%A6%E5%B1%8F%E9%9A%9C%E7%82%BA%E8%85%A6%E9%83%A8%E7%96%BE%E7%97%85%E6%B2%BB%E7%99%82%E5%B8%B6%E4%BE%86%E6%96%B0/]
- 17. Bridging the barrier: insights into blood biomarkers and ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00829-4]
- 18. 免疫细胞的脑归巢及其与神经退行性疾病的关系研究进展 [https://journal.dmu.edu.cn/article/doi/10.11724/jdmu.2025.02.08?viewType=HTML]
- 19. Roche押注AI脑递送平台- 刘玉娥的博文 - 手机版 [https://wap.sciencenet.cn/blog-3592244-1508896.html]
- 20. 脑内药物递送技术研发进入快车道 [https://www.stdaily.com/web/gdxw/2025-06/23/content_358722.html]
- 21. 综述:仿生脑靶向药物递送系统在脑部疾病治疗中的应用 [https://www.ebiotrade.com/newsf/2025-7/20250705081338022.htm]
- 22. 非病毒纳米载体改善血脑屏障通透性以增强脑部疾病治疗 ... [https://www.ebiotrade.com/newsf/2025-10/20251019081957625.htm]
- 23. Blood-brain barrier transport machineries and targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5326671/]
- 24. Precision targeting of the CNS: recent progress in brain ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03578c]
- 25. Current Strategies for Brain Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5858162/]
- 26. Strategies to identify, engineer and validate antibodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842915/]
- 27. Receptor-mediated drug delivery of bispecific therapeutic ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2023.1227816/full]
- 28. Receptor-mediated transcytosis for brain delivery of therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363266/]
- 29. A brain-shuttled antibody targeting alpha synuclein ... [https://www.nature.com/articles/s41531-025-01117-6]
- 30. Bispecific brain-penetrant antibodies for treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413732/]
- 31. Roche presents new insights in Alzheimer's disease ... [https://www.roche.com/media/releases/med-cor-2025-07-28]
- 32. Genentech: Press Releases | Thursday, Apr 3, 2025 [https://www.gene.com/media/press-releases/15057/2025-04-03/genentech-and-roche-present-novel-therap]
- 33. Managing CMC Complexity of Bispecifics: A Practical Guide [https://www.leukocare.com/blog/managing-cmc-complexity-of-bispecifics]
- 34. Trends and challenges in bispecific antibody production [https://www.sciencedirect.com/science/article/abs/pii/S0021967325000718]
- 35. Production of Bispecific Antibodies: 6 steps from Design to ... [https://www.evitria.com/journal/antibodies/bispecific-antibody-production/]
- 36. Recent Advances in Antibody Therapy for Alzheimer's ... [https://www.mdpi.com/1422-0067/26/13/6271]
- 37. Imaging strategies to assess efficacy and safety of ... - Nature [https://www.nature.com/articles/s44384-025-00024-7]
- 38. Characterization of focused ultrasound blood-brain barrier ... [https://www.sciencedirect.com/science/article/pii/S0753332224016482]
- 39. Focused ultrasound-microbubble treatment arrests the ... [https://www.nature.com/articles/s41551-025-01390-z]
- 40. Focused ultrasound augments the delivery and penetration ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500481X]
- 41. Focused Ultrasound – Blood-Brain Barrier [https://www.alzforum.org/therapeutics/focused-ultrasound-blood-brain-barrier]
- 42. Recent advances in potential drug nanocarriers for CNS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639991/]
- 43. Nanocarrier Drug Delivery Systems: Characterization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9026217/]
- 44. PepH3-modified nanocarriers for delivery of therapeutics ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-025-00641-0]
- 45. PepH3-modified nanocarriers for delivery of therapeutics ... [https://pubmed.ncbi.nlm.nih.gov/40170024/]
- 46. Targeted Nanoparticles for Drug Delivery Across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627166/]
- 47. Nanocarrier - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/nanocarrier]
- 48. Exosomes as nanocarriers for brain-targeted delivery of ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03528-2]
- 49. Various AAV Serotypes and Their Applications in Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000783/]
- 50. Adeno-associated virus as a delivery vector for gene ... [https://www.nature.com/articles/s41392-024-01780-w]
- 51. A Visual Guide to Gene Delivery - by Eryney Marrogi [https://www.asimov.press/p/gene-delivery]
- 52. FAQ: AAV, Adenovirus & More [https://www.vectorbiolabs.com/resources/faqs/]
- 53. Understanding capsid assembly and genome packaging for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9910337/]
- 54. The Challenges and Strategies of Antisense Oligonucleotide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8072990/]
- 55. A CRISPR/Cas9 screen reveals proteins at the endosome- ... [https://www.nature.com/articles/s41467-025-61039-y]
- 56. Traversing the Blood–Brain Barrier: Challenges and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK507360/]
- 57. Research progress in brain-targeted nasal drug delivery [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2023.1341295/full]
- 58. Intranasal delivery bypasses the blood-brain barrier to target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2604883/]
- 59. Design and Application in Delivery System of Intranasal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7779764/]
- 60. Intranasal drug delivery: Pathways, challenges, and ... [https://www.sciencedirect.com/science/article/abs/pii/S177322472500228X]
- 61. Intranasal Delivery of Proteins and Peptides in the Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476983/]
- 62. A Review of the Current Status and Future Trajectories [https://pubmed.ncbi.nlm.nih.gov/40524468/]
- 63. Drug delivery strategies to cross the blood-brain barrier in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321624/]
- 64. Nanotechnology Approaches for Mitigating Biologic ... [https://www.mdpi.com/1999-4923/17/7/888]
- 65. Reducing Immunogenicity by Design: Approaches to ... [https://link.springer.com/article/10.1007/s40259-023-00641-2]
- 66. Strategies to mitigate the on- and off-target toxicities of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9344849/]
- 67. evaluating and mitigating off-target effects in CRISPR gene ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1339189/full]
- 68. High-affinity transferrin receptor binding improves brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369151/]
- 69. Protein engineering approaches for regulating blood–brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0959440X16301397]
- 70. Antibody Structure and Function: The Basis for Engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6963682/]
- 71. Humanized Mice: Advancing Translational Preclinical ... [https://www.taconic.com/resources/methods-generating-humanized-mice]
- 72. Humanized mouse model: a review on preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7783739/]
- 73. Mastering complex small molecule APIs and formulations [https://www.patheon.com/us/en/insights-resources/blog/mastering-complex-api-and-formulations.html]
- 74. Transforming Clinical Bioanalysis for Manufacturing ... [https://www.biopharminternational.com/view/transforming-clinical-bioanalysis-for-manufacturing-scalability]
- 75. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 76. Understanding the blood brain barrier: current state and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121414/]
- 77. Combinational therapeutic strategies to overcome ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1546717/full]
- 78. Development of Immunotherapy Combination Strategies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8178168/]
- 79. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]
- 80. Delivery of the Brainshuttle™ amyloid-beta antibody fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10572082/]
- 81. Biogen Exercises Option with Denali to Develop and ... [https://investors.biogen.com/news-releases/news-release-details/biogen-exercises-option-denali-develop-and-commercialize]
- 82. What's this Roche Brain Shuttle all about? [https://www.cureffi.org/2014/01/16/whats-this-roche-brain-shuttle-all-about/]
- 83. Frequently asked questions about AAV delivery [https://www.takarabio.com/learning-centers/gene-function/viral-transduction/adeno-associated-virus/aav-faqs?srsltid=AfmBOookp1sp_68nZt5W0XnDIyRuJF3Te-lVGfkKHEk3SAOp359Jplyg]
- 84. AAV Frequently asked questions [https://clover.caltech.edu/aav/faq]
- 85. DENALI CANsmart™ - The Best CANbus Controller On ... [https://denalielectronics.com/pages/denali-cansmart-canbus-controller]
- 86. Trojan Horse: Carrying Alzheimer's Antibodies Into the Brain | Being Patient [https://beingpatient.com/alzheimers-antibodies-blood-brain-barrier/]
- 87. Breaking Barriers: Delivering Therapeutics to the Brain in Alzheimer’s Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321621/]
- 88. Tofersen [https://www.mndassociation.org/research/clinical-trials/treatment-trials/tofersen]
- 89. Tofersen Shows Promising Results in SOD1 ... [https://www.targetals.org/2025/03/04/tofersenstudy/]
- 90. Focused Ultrasound-Mediated Blood-Brain Barrier Opening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11792178/]
- 91. Roche Spells Out Phase Three Plans for Trontinemab [https://globalalzplatform.org/2025/08/22/alz-forum-roche-spells-out-phase-three-plans-for-trontinemab/]
- 92. The Blood-Brain Barrier: Approaches for Antibody Biologic ... [https://www.biointron.com/antibody-industry-trends/november-2025-blood-brain-barrier-approaches-for-antibody-biologic-delivery.html]
- 93. Brain pharmacokinetics of two BBB penetrating bispecific ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-021-00257-0]
- 94. BBB Antibody Penetration Assay with Millicell® Plates [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/blood-brain-barrier-antibody-penetration-assay?srsltid=AfmBOop62fpLDuHUoV5qzqIXS9n3OOHCBVc6RJevjUNz9t1P7Dwb7oWU]
- 95. PET-MRI nanoparticles imaging of blood–brain barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7716090/]
- 96. Quantitative PET imaging and modeling of molecular blood ... [https://www.nature.com/articles/s41467-025-58356-7]
- 97. EXPLORER total body PET scanner helps detect brain ... [https://health.ucdavis.edu/patients-visitors/news/headlines/explorer-total-body-pet-scanner-helps-detect-brain-disease/2025/04]
- 98. Challenges and material innovations in drug delivery to ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225000997]