Revolutionizing Drug Discovery: How Microfluidic Devices Enable High-Throughput Screening and Precision Medicine
This article explores the transformative role of microfluidic technology in high-throughput drug discovery and development.
Revolutionizing Drug Discovery: How Microfluidic Devices Enable High-Throughput Screening and Precision Medicine
Abstract
This article explores the transformative role of microfluidic technology in high-throughput drug discovery and development. It provides researchers, scientists, and drug development professionals with a comprehensive analysis of how Lab-on-a-Chip systems, organ-on-chip models, and droplet microfluidics are overcoming the limitations of traditional methods. The scope covers foundational principles, key methodological applications in screening and toxicity testing, practical strategies for troubleshooting common device challenges, and rigorous approaches for validating microfluidic platforms against established standards. By integrating the latest research and commercial trends, this resource serves as a practical guide for leveraging microfluidics to accelerate pharmaceutical R&D, reduce costs, and advance personalized medicine.
Microfluidics 101: Core Principles and Why It's a Game-Changer for Modern Drug Discovery
Microfluidics is the science and technology of systems that process or manipulate small volumes of fluids (10⁻⁹ to 10⁻¹⁸ liters), using channels with dimensions ranging from tens to hundreds of micrometers [1]. This field has revolutionized various aspects of the pharmaceutical industry, including drug discovery, development, and analysis [1]. The key concept involves integrating laboratory operations into a simple micro-sized system, a principle often referred to as "Lab-on-a-Chip" (LOC) or "Micro-Total Analysis Systems" (µTAS) [2]. Fluids at this microscale behave differently than at macroscopic scales, with factors such as laminar flow, capillary effects, and surface tension dominating their behavior [3]. These unique characteristics are leveraged to create powerful tools for high-throughput drug discovery research, enabling scientists to conduct extremely precise experiments and evaluate biological samples with unmatched precision [1].
Fundamental Principles and Advantages
Microfluidic systems exploit the distinct physical and chemical properties of liquids and gases at the microscale. The flow is typically laminar, which allows for highly predictable fluid behavior and precise control over the microenvironment [3]. This precise control enables the creation of highly efficient and reproducible systems for chemical reactions and biological assays.
The table below summarizes the core advantages of microfluidic systems over conventional macroscopic methods, particularly in the context of drug discovery research.
Table 1: Key Advantages of Microfluidic Systems in Drug Discovery
| Advantage | Impact on Drug Discovery Research |
|---|---|
| Minimal Reagent Consumption | Reduces global cost of applications; enables work with precious or expensive compounds [4] [2]. |
| High-Throughput Screening | Allows thousands of tests to be run in parallel, dramatically accelerating the hit identification and optimization phases [1] [5]. |
| Enhanced Parameter Control | Provides superior control over the cellular microenvironment (e.g., shear stress, concentration gradients), leading to more physiologically relevant data [3] [2]. |
| Fast Reaction Times | Shortens experimental times due to small volumes and short diffusion distances [4] [5]. |
| Process Automation & Integration | Automates multi-step reactions within a single device, minimizing manual handling and improving reproducibility [5] [2]. |
| Excellent Data Quality | High precision and controllability lead to robust and high-quality data [2]. |
Applications in High-Throughput Drug Discovery
Microfluidic technology has become a transformative tool across the entire drug discovery and development pipeline, from initial target selection to preclinical studies [4].
Target Selection and Validation
The first step in drug discovery is to identify a biological target, such as a protein, that can be modulated by a drug molecule [4]. Microfluidic devices facilitate this by enabling high-sensitivity protein analysis.
- Protein Analysis in Single Cells: Integrated devices can manipulate, lyse, label, separate, and quantify the protein contents of individual cells, which is crucial for understanding signal transduction pathways [4].
- Protein Crystallization: Microfluidic platforms, such as those using droplet-based generators or free interface diffusion, allow for high-throughput protein crystallization trials with minimal sample consumption, aiding in structural characterization of targets [4].
- Ligand-Binding Studies: These devices characterize molecular interactions (e.g., IC₅₀, Kd) with high sensitivity and throughput, identifying promising drug-target interactions early on [4].
Hit Identification and Optimization
This phase involves screening vast libraries of compounds to identify "hit" molecules that interact with the selected target. Microfluidics excels here.
- High-Throughput Screening (HTS): Microfluidic multiplexed systems containing thousands of microchambers, microwell arrays, or microvalves perform HTS with higher sensitivity and shorter reaction times compared to conventional methods, while significantly reducing reagent volumes and costs [1] [5].
- Droplet-Based Microfluidics: By encapsulating individual cells or reagents in picoliter droplets, millions of distinct experiments can be conducted in parallel, vastly increasing screening throughput [4] [5].
Preclinical Studies: Organs-on-Chips
A major innovation in microfluidics is the development of Organ-on-a-Chip (OoC) models. These are 3D microdevices that aim to replicate the key functions of living human organs, providing more physiologically relevant and human-predictive data than traditional 2D cell cultures or animal models [3] [2].
- Heart-on-Chip (HoC): These systems use microchannels, often made of PDMS, to create microenvironments that mimic the heart's architecture and mechanical forces, such as pulsatile flow and shear stress [3]. They incorporate 3D co-cultures of cardiomyocytes, endothelial cells, and fibroblasts, allowing for detailed study of cardiac disease models and drug responses [3].
- Multi-Organ Chips: Integrated systems (e.g., heart-liver platforms) enable researchers to study systemic drug effects, metabolism, and toxicity in a interconnected human-relevant system [3].
- Personalized Medicine: The incorporation of patient-derived induced pluripotent stem cells (iPSCs) into these chips allows for the creation of personalized disease models and the testing of therapeutic strategies on a patient-specific cellular phenotype [3].
Experimental Protocols
Protocol 1: High-Throughput Drug Screening Using a Microwell Array Chip
This protocol describes a method for screening a compound library against a cellular target.
Workflow Overview:
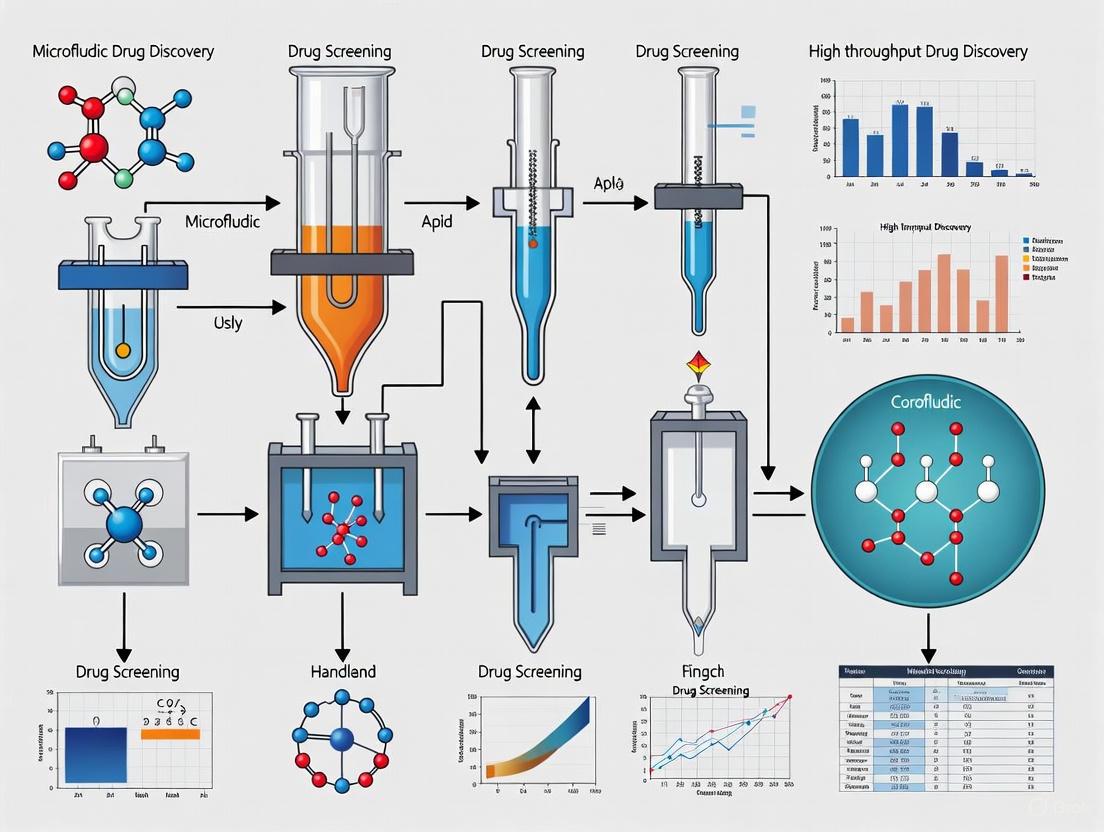
Diagram Title: High-Throughput Screening Workflow
Materials:
- Microwell Array Chip: A microfluidic device containing a dense array of nanoliter-scale wells.
- Pressure-Based Flow Controller: Provides stable and pulsation-free flow for cell loading (e.g., Fluigent or Elveflow systems) [5] [2].
- Cell Line: Stably transfected with a fluorescent reporter for the target pathway.
- Compound Library: Dissolved in DMSO at a standard concentration.
- Automated Fluid Handling System: For sequential injection of multiple reagents (e.g., Fluigent Aria) [5].
- High-Content Fluorescence Imaging System.
Procedure:
- Chip Priming: Connect the microfluidic chip to the pressure controller. Prime all channels with sterile PBS buffer to remove air bubbles and wet the surfaces [5].
- Cell Seeding: Introduce a homogeneous cell suspension into the chip's inlet reservoir. Use a low, constant pressure to flow cells into the microwells, aiming for single-cell occupancy in each well. Stop flow and allow cells to settle for 15-30 minutes [5].
- Compound Introduction: Use an automated multiplexer to sequentially introduce compounds from the library into the chip. Each compound is perfused through the microwell array at a defined concentration for a set duration [5].
- Incubation: Maintain the chip at 37°C and 5% CO₂ for 24-72 hours to allow for cellular response.
- Staining and Imaging: Introduce a fluorescent viability or apoptosis stain (e.g., Calcein-AM / Propidium Iodide) into the chip. After incubation, acquire high-resolution images of each microwell using an automated microscope [3].
- Data Analysis: Quantify fluorescence intensity per well using image analysis software (e.g., ImageJ, CellProfiler). Normalize data to positive and negative controls. Compounds showing significant activity above a defined threshold are identified as "hits."
Protocol 2: Generating Liposomal Nanoparticles via a Microfluidic Mixer
This protocol details the synthesis of monodisperse lipid nanoparticles (LNPs) for drug delivery using a hydrodynamic flow-focusing device.
Workflow Overview:
Diagram Title: LNP Synthesis via Flow-Focusing
Materials:
- Microfluidic Mixer Chip: A chip with a flow-focusing or T-junction geometry.
- Precision Syringe Pumps or Pressure Controllers: Critical for maintaining stable flow rates of the aqueous and organic phases to ensure monodisperse particle size [1] [5].
- Lipids: e.g., DSPC, Cholesterol, PEG-lipid.
- Hydration Buffer: e.g., 20 mM HEPES, 150 mM NaCl, pH 7.4.
- Dialysis Tubing.
Procedure:
- Solution Preparation: Dissolve the lipid mixture in pharmaceutical-grade ethanol at a concentration of 5-20 mg/mL. Prepare the aqueous buffer and filter both solutions through a 0.22 µm membrane.
- System Setup: Load the lipid and aqueous solutions into separate syringes. Connect the syringes to the chip inlets via tubing. Place a collection tube at the outlet.
- Particle Generation: Simultaneously inject the lipid (organic) and aqueous solutions into the chip. The flow-focusing geometry hydrodynamically focuses the organic stream, causing rapid mixing and lipid precipitation, forming nanoparticles. The flow rate ratio (aqueous:organic) is the key parameter controlling size and polydispersity. A typical total flow rate is 1-10 mL/min [1].
- Collection and Dialysis: Collect the nanoparticle suspension from the outlet. Transfer to dialysis tubing and dialyze against a large volume of hydration buffer for 12-24 hours to remove ethanol.
- Characterization: Analyze the final LNP preparation for size, polydispersity index (PDI), and zeta potential using dynamic light scattering. Encapsulation efficiency can be determined using a method like HPLC.
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and reagents commonly used in microfluidic drug discovery applications.
Table 2: Essential Research Reagents and Materials for Microfluidic Drug Discovery
| Item | Function/Application | Key Considerations |
|---|---|---|
| PDMS (Polydimethylsiloxane) | Elastomeric polymer for rapid prototyping of microfluidic chips via soft lithography [3]. | Biocompatible, gas-permeable, but can absorb small hydrophobic molecules [3]. |
| iPSC-Derived Cardiomyocytes | Patient-specific cells for creating physiologically relevant Heart-on-Chip models and personalized drug testing [3]. | Requires rigorous characterization of maturity and electrophysiological functionality [3]. |
| Extracellular Matrix Hydrogels | (e.g., Matrigel, Collagen, Fibrin) Provide a 3D scaffold for cell culture in Organ-on-Chip devices, mimicking the in vivo microenvironment [3]. | Batch-to-batch variability; polymerization conditions must be optimized for microchannels. |
| Fluorescent Calcium Indicators | (e.g., Fluo-4, Fura-2) Used for real-time monitoring of electrophysiology and calcium handling in heart-on-chip models [3]. | Dye loading concentration and incubation time must be optimized to avoid cytotoxicity. |
| Pressure-Based Flow Controllers | Provide stable, pulsation-free fluid delivery for cell culture perfusion, reagent introduction, and droplet generation [5] [2]. | Superior flow stability and responsiveness compared to syringe pumps for many applications [5]. |
| Lipid Mixtures | (e.g., DSPC, Cholesterol, PEG-lipid) Raw materials for the synthesis of lipid nanoparticles (LNPs) for drug encapsulation and delivery [1]. | Purity and composition directly impact LNP stability, size, and encapsulation efficiency [1]. |
In the pursuit of accelerating drug discovery, microfluidic technology has emerged as a transformative platform, enabling high-throughput screening (HTS) with unprecedented precision and efficiency. The physical behavior of fluids at the microscale fundamentally differs from macroscale phenomena, governed by unique principles that can be harnessed to create highly controlled microenvironments. This application note details three key physical principles—laminar flow, diffusion, and capillary action—that underpin the design and operation of microfluidic devices for drug discovery research. We provide experimental protocols, quantitative data summaries, and practical guidance to enable researchers to leverage these phenomena for advanced screening applications, with a specific focus on generating precise concentration gradients for cytotoxicity assays.
Core Physical Principles and Their Manipulation
Laminar Flow
In microfluidic systems, the flow of fluids is typically laminar rather than turbulent. In laminar flow, fluid moves in parallel, steady layers with no disruption between them [6]. This phenomenon arises from the low Reynolds number (Re), a dimensionless parameter that represents the ratio of inertial forces to viscous forces [6]. For microchannels, Re is usually far below 2000, the threshold below which flow remains laminar [6].
- Key Application: Laminar flow allows for the precise manipulation of fluid streams without turbulent mixing. This is exploited in gradient generators to create defined, stable concentration profiles of drugs or test compounds by controlling the volumetric merging of adjacent fluid streams [7]. A recent study utilized this principle to achieve stable gradient generation within 30 seconds for high-throughput cancer drug screening [7].
Diffusion
Diffusion is the process by which molecules move from an area of high concentration to an area of low concentration due to random thermal motion [8]. In microfluidic systems, it is the primary mechanism for molecular mixing when two or more fluid streams are brought into contact. The rate of diffusion is significantly influenced by the diffusion coefficient of the molecule and the interfacial contact area between fluid streams [8].
- Key Application: In drug screening, diffusion governs the transport of drug molecules from flow channels into 3D cell cultures or tissue constructs within organ-on-a-chip devices, more accurately mimicking the physiological delivery of therapeutics in vivo [9] [10]. This enables more physiologically relevant assessment of drug efficacy and toxicity compared to static well-plate assays.
Capillary Action
Capillary action, or capillarity, is the ability of a liquid to flow in narrow spaces without the assistance of, or even against, external forces like gravity [11]. This spontaneous wicking is driven by the interplay between cohesive forces (within the liquid) and adhesive forces (between the liquid and the channel walls) [11] [12]. The strength of capillary flow is inversely related to the channel diameter.
- Key Application: Capillary action is the driving force in passive microfluidic systems, such as lateral flow assays and paper-based microfluidic devices [6]. This enables the development of simple, pump-free, and portable diagnostic and screening tools, reducing the need for complex and expensive external instrumentation [6].
Table 1: Quantitative Summary of Key Physical Parameters at the Microscale
| Physical Principle | Governing Parameter | Typical Value/Formula | Impact on Drug Screening Applications |
|---|---|---|---|
| Laminar Flow | Reynolds Number (Re) | ( Re = \frac{\rho v D}{\mu} ) [6]Where ( \rho )=density, ( v )=velocity, ( D )=characteristic diameter, ( \mu )=viscosity.Re < 2000 for laminar flow. | Enables precise fluid stream control and stable gradient generation for high-throughput dose-response studies [7]. |
| Diffusion | Diffusion Coefficient (D) | Varies by molecule and medium.e.g., Small molecules in water: ~10⁻⁹ m²/s.Governs mixing and interstitial transport. | Critical for nutrient and drug delivery in 3D cell cultures; can be a rate-limiting step in organ-on-a-chip models [9]. |
| Capillary Action | Capillary Pressure (Pc) | ( P_c = \frac{2\gamma \cos\theta}{r} ) [12]Where ( \gamma )=surface tension, ( \theta )=contact angle, ( r )=pore radius. | Eliminates the need for pumps in passive devices, simplifying design and reducing costs for point-of-care test applications [6]. |
Experimental Protocol: Generating a Drug Concentration Gradient for High-Throughput Screening
This protocol details the use of a laminar flow-based microfluidic concentration gradient generator (MCGG) for high-throughput drug cytotoxicity screening, adaptable for 96-well plate formats [7].
Research Reagent Solutions & Materials
Table 2: Essential Materials and Reagents for Microfluidic Gradient Generation
| Item | Function/Description | Application Note |
|---|---|---|
| Cycle Olefin Polymer (COP) | Substrate for device fabrication; offers high optical clarity and low autofluorescence. | Preferred for high-throughput screening due to excellent biocompatibility and optical properties for imaging [7]. |
| Polydimethylsiloxane (PDMS) | Elastomeric material for device fabrication; gas-permeable, biocompatible, and flexible. | Requires plasma oxidation or surface coating (e.g., fibronectin) to render it hydrophilic for improved cell adhesion [9]. |
| Bovine Serum Albumin (BSA) Solution | Model protein solution for validating gradient generation and device performance. | Used in initial device calibration to confirm concentration profile accuracy without consuming expensive drug compounds [7]. |
| Drug Stock Solutions | Compounds for screening (e.g., chemotherapeutic agents). | Prepare in appropriate solvent (e.g., DMSO) and dilute in cell culture medium immediately before use, ensuring final solvent concentration is non-cytotoxic. |
| Cell Culture Medium | Supports cell viability during the assay. | Must be sterile and compatible with the microfluidic device material to prevent bubble formation and nonspecific adsorption. |
Step-by-Step Procedure
Device Priming: Connect the outlet of the microfluidic MCGG device to a syringe pump via sterile tubing. Slowly prime all channels with 1X phosphate-buffered saline (PBS) or serum-free culture medium to remove air bubbles and wet the channel surfaces. Ensure all waste reservoirs are empty.
Gradient Generation & Validation:
- Prepare two input solutions: Reservoir A containing the drug dissolved in cell culture medium, and Reservoir B containing medium only.
- Load these solutions into their respective input syringes. Initiate flow using the syringe pump at a constant, low flow rate (e.g., 5-50 µL/min) to establish laminar flow conditions [7].
- To validate the gradient, first run the device with a BSA solution in Reservoir A and PBS in Reservoir B. Collect output from different gradient channels and measure the BSA concentration (e.g., via spectrophotometry) to confirm it matches the theoretical profile.
Cell Exposure & On-Chip Incubation:
- Seed the output microchambers or a connected 96-well plate with the target cancer cells (e.g., HCT116 colorectal carcinoma cells) at a standardized density and allow them to adhere overnight in a CO₂ incubator.
- Connect the primed and validated MCGG device to the cell culture platform. Run the drug and medium streams to expose the cells to the generated concentration gradient for a predetermined period (e.g., 24-72 hours).
Viability Assessment & Analysis:
- After exposure, carefully aspirate the medium from the output chambers.
- Add a cell viability indicator (e.g., AlamarBlue or MTT reagent) diluted in fresh medium to the cells.
- Incubate according to the reagent manufacturer's instructions and measure the fluorescence or absorbance.
- Plot cell viability against drug concentration to determine the half-maximal inhibitory concentration (IC₅₀) value for the tested drug.
The following workflow diagram illustrates the key stages of this protocol:
Diagram 1: High-Throughput Drug Screening Workflow
Device Design and Operational Considerations
The physical principles dictate specific design choices. The relationship between channel geometry and the dominant physical phenomena is critical for robust device operation.
Diagram 2: From Principle to Design
The deliberate application of laminar flow, diffusion, and capillary action provides the foundation for sophisticated, high-throughput microfluidic drug screening platforms. Laminar flow enables the generation of precise and stable concentration gradients, diffusion governs physiologically relevant molecular transport in 3D cellular microenvironments, and capillary action facilitates the development of simple, passive devices. By integrating these principles into device design and experimental protocols as outlined, researchers can significantly enhance the efficiency, predictive power, and translational potential of their drug discovery pipeline.
The Evolution from Manual Methods to Automated High-Throughput Systems
The trajectory of drug discovery has been fundamentally reshaped by the transition from manual, low-capacity laboratory techniques to sophisticated, automated high-throughput systems. This evolution began to take shape in the late 20th century, revolutionizing traditional methods that were labor-intensive and time-consuming, often limited to processing just 20–50 compounds per week per laboratory [13] [14]. The driving force behind this transformation was the advent of recombinant DNA technology, which provided access to novel therapeutic targets that existing screening methods were inadequate to address [14]. This technological singularity created the essential conditions for high-throughput screening (HTS) to emerge as a practical solution for rapidly testing hundreds of thousands of compounds against new biological targets [14].
The paradigm has further advanced with the integration of microfluidic technologies, which represent a significant leap in miniaturization and automation. These systems enable unprecedented precision in fluid handling and environmental control while reducing reagent consumption by up to 150-fold compared to conventional well-plate formats [15]. This application note examines the key technological milestones in this evolution, with a specific focus on microfluidic platforms that now enable high-content screening at scales previously unattainable, providing researchers with powerful tools for accelerating therapeutic development.
Technological Milestones in Automation and Miniaturization
The Genesis of High-Throughput Screening
The earliest HTS systems emerged in the mid-1980s, with pioneering work at Pfizer demonstrating a radical departure from traditional screening methods. The initial system, operational by 1986, substituted fermentation broths with dimethyl sulphoxide (DMSO) solutions of synthetic compounds, utilizing 96-well plates and reduced assay volumes of 50-100μl [14]. This approach dramatically increased screening capacity from approximately 20-50 compounds per week per lab to over 7,000 compounds weekly by 1989 [14]. The transition from single tubes to array formats and from dry compounds requiring custom solubilization to pre-plated compound libraries in DMSO established the fundamental framework upon which all subsequent HTS technologies have been built [14].
Progression to Ultra-High-Throughput Systems
The relentless drive for greater throughput and efficiency has propelled continual innovation in HTS platforms, as detailed in Table 1.
Table 1: Evolution of HTS Throughput and Miniaturization
| Era | Format | Typical Volume | Throughput (compounds/day) | Key Enabling Technologies |
|---|---|---|---|---|
| Pre-HTS (1980s) | Single test tubes | ~1 mL | 20-50 | Manual pipetting, spectrophotometers [14] |
| Early HTS (1990s) | 96-well plates | 50-100 μL | 1,000-10,000 | Robotic liquid handlers, plate readers [14] |
| Standard HTS (2000s) | 384-well plates | 5-50 μL | 10,000-100,000 | Automated plate handlers, advanced detection systems [16] |
| Ultra-HTS (2010s+) | 1536-well plates | 1-2 μL | >300,000 | Acoustic dispensing, microfluidics [16] |
| Microfluidic HCS (Recent) | Microfluidic chambers | <1 μL (picoliter-nanoliter scale) | Varies (10,000+ individual cell experiments/device) | Integrated membrane valves, soft lithography [15] |
This progression has been characterized by exponential increases in processing capability alongside dramatic reductions in reagent consumption. The emergence of ultra-high-throughput screening (uHTS) pushed throughput to over 300,000 compounds daily, while microfluidic platforms have enabled screening at unprecedented levels of miniaturization, reducing reagent volumes to the picoliter range [17] [16].
Microfluidic Platforms for High-Throughput Screening
Active-Matrix Digital Microfluidics (AM-DMF)
A transformative advancement in liquid handling, Active-Matrix Digital Microfluidics (AM-DMF) leverages semiconductor-derived electrode arrays to dynamically control thousands of micrometre-scale droplets [17]. This technology enables various programmable operations—including droplet generation, transport, mixing, and dilution—with unparalleled accuracy [17]. Unlike continuous-flow microfluidics, AM-DMF manipulates discrete droplets on a surface without channels, allowing for precise individual control of each droplet's trajectory and processing. The architecture has evolved through several generations: from passive-matrix (DMF 1.0) to active-matrix (DMF 2.0), gate-on-array (DMF 2.5), and finally to integrated circuit-driven (DMF 3.0) systems, each iteration enhancing scalability and control precision [17]. This platform is particularly valuable for applications requiring high-throughput manipulation of precious samples, such as single-cell analysis, genomics, and drug screening [17].
Microfluidic High-Content Cell Screening (HCS)
Microfluidic technology has extended beyond traditional compound screening to enable high-content screening (HCS) with single-cell resolution. These platforms integrate all aspects of cellular experimentation—including cell culture, stimulation, staining, and imaging—within a single miniaturized device [15]. A representative device design fabricated from polydimethylsiloxane (PDMS) incorporates 32 separate compartments linked to multiple inlets and outlets, with fluid flow controlled by a manifold of integrated membrane valves [15]. In a typical experiment, approximately 300 cells are loaded into each compartment, enabling nearly 10,000 individual cell experiments in a single device [15]. This platform allows researchers to expose different compartments to varying combinations or concentrations of exogenously added factors for different durations, followed by fixation, immunochemical staining, and automated imaging [15].
Table 2: Research Reagent Solutions for Microfluidic HCS
| Reagent/Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Device Material | Polydimethylsiloxane (PDMS) | Biocompatible, optically transparent elastomer for device fabrication [15] |
| Cell Culture Substrate | Extracellular Matrix (ECM) Proteins (e.g., Collagen, Fibronectin) | Surface coating to promote cell adhesion and mimic physiological environment [18] |
| Staining Reagents | Fluorophore-conjugated Antibodies, DNA Dyes (e.g., DAPI), Cell Viability Indicators (e.g., Calcein-AM) | Immunocytochemical staining for protein localization and concentration; assessment of cell viability and structure [15] |
| Fixation Reagent | Paraformaldehyde (PFA) | Cross-linking fixative to preserve cellular architecture and protein localization prior to staining [15] |
| Signal Detection Probes | Specific Antibodies, In Situ Hybridization Probes | Primary readouts for localization and concentration of signaling proteins or mRNA [15] |
Protocol: Implementing a Microfluidic HCS Assay for Cell Signaling Analysis
Device Preparation and Cell Loading
- Device Priming: Flush all microfluidic channels with a biocompatible buffer, such as phosphate-buffered saline (PBS), to remove air bubbles and condition the surface.
- Surface Coating (Optional): For adherent cells, introduce an appropriate extracellular matrix protein solution (e.g., collagen or fibronectin at 10-100 μg/mL concentration) into the device and incubate for 1-2 hours at 37°C to promote cell adhesion [18].
- Cell Suspension Preparation: Trypsinize and resuspend adherent cells in appropriate culture medium to a final density of 5-10 × 10^6 cells/mL. The optimal density must be determined empirically to achieve approximately 300 cells per compartment [15].
- Cell Loading: Introduce the cell suspension into the device's main inlet channel using a precision syringe pump or pneumatic pressure system. Actuate membrane valves to partition and isolate individual compartments, trapping cells within each experimental unit [15].
- Cell Adhesion Period: Allow the device to remain under static conditions in a humidified 37°C, 5% CO2 incubator for 4-24 hours to enable cell attachment and stabilization.
Compound Handling and Stimulation
- Compound Library Preparation: Prepare solutions of compounds or biological agents in assay-compatible medium at 100-1000× the desired final concentration, accounting for the high dilution factor within the microfluidic device.
- Automated Stimulation: Using the integrated valve control system, program the device to expose each compartment to different combinations or concentrations of stimulants (e.g., receptor ligands, cytokines, or small molecule inhibitors). The system can deliver these stimuli in various patterns—including step changes, concentration gradients, or complex temporal pulses—to mimic physiological or pharmacological conditions [15].
- Incubation: Maintain the device at 37°C, 5% CO2 for the prescribed stimulation period, which can range from minutes for early signaling events to hours or days for longer-term responses.
Fixation, Staining, and Imaging
- Fixation: Introduce a fixative solution (e.g., 4% paraformaldehyde in PBS) into the device and incubate for 15-20 minutes at room temperature.
- Permeabilization and Blocking: Flush the device with a permeabilization/blocking buffer (e.g., PBS containing 0.1% Triton X-100 and 1-5% bovine serum albumin) to permeabilize cell membranes and reduce non-specific antibody binding.
- Immunofluorescence Staining: Introduce primary antibodies diluted in blocking buffer and incubate for 2 hours at room temperature or overnight at 4°C. Follow with multiple wash steps, then introduce fluorophore-conjugated secondary antibodies and counterstains (e.g., DAPI for nuclei, phalloidin for actin) for 1-hour incubation [15].
- Automated Imaging: Mount the device on a motorized microscope or high-content fluorescence scanner. Acquire images of each compartment using appropriate fluorescence filter sets for each channel. The high cell number per condition (typically hundreds of cells) enables robust statistical analysis of cellular responses [15].
Data Analysis and Hit Identification
- Image Analysis: Utilize automated image analysis software to extract quantitative features from each cell, including subcellular protein localization and concentration, cell shape and size, and other morphological parameters.
- Statistical Comparison: Compare the distributions of these readouts across hundreds of cells exposed to the same experimental condition to identify statistically significant differences between treatment groups.
- Hit Selection: Apply appropriate statistical thresholds (e.g., Z-score > 3 or p-value < 0.01) to identify compounds or conditions that produce biologically significant effects, while controlling for false positives using methods such as p-value distribution analysis (PVDA) [19].
Quantitative HTS Data Analysis Considerations
The transition to quantitative HTS (qHTS), which generates full concentration-response curves for thousands of compounds simultaneously, presents significant statistical challenges [20]. The Hill equation (HEQN) remains the most widely used nonlinear model for describing qHTS response profiles, estimating parameters including baseline response (E0), maximal response (E∞), half-maximal activity concentration (AC50), and shape parameter (h) [20]. However, parameter estimation—particularly for AC50—is highly variable when the tested concentration range fails to include at least one of the two HEQN asymptotes [20]. Statistical simulations demonstrate that AC50 estimates can span several orders of magnitude when assay conditions are suboptimal, emphasizing the critical importance of appropriate study design and the potential need for alternative approaches to characterize concentration-response relationships [20].
The evolution from manual methods to automated high-throughput systems represents a fundamental paradigm shift in biomedical research and drug discovery. This journey—from processing dozens of compounds weekly in individual test tubes to manipulating thousands of droplets in parallel on microfluidic chips—has dramatically accelerated the pace of therapeutic development [13] [14] [17]. Microfluidic platforms, including AM-DMF and integrated HCS devices, now provide unprecedented capabilities for miniaturization, environmental control, and single-cell resolution [17] [15]. These technologies enable researchers to conduct sophisticated experiments with massive reductions in reagent consumption and cellular material requirements, making previously prohibitive screening campaigns both feasible and cost-effective [15]. As these systems continue to evolve, incorporating advances in artificial intelligence, sensor integration, and material science, they will further empower researchers to tackle increasingly complex biological questions and accelerate the delivery of novel therapeutics to patients.
Application Notes
The adoption of microfluidic technologies in high-throughput drug discovery is driven by three core advantages: miniaturization, significantly reduced reagent consumption, and enhanced precision in controlling the cellular and chemical microenvironment. These features directly address major inefficiencies in traditional drug screening, offering a more predictive and cost-effective preclinical research model [21] [22].
Miniaturization for High-Throughput Screening
Miniaturization via lab-on-a-chip (LoC) and droplet microfluidic platforms enables a massive increase in experimental throughput. These systems transform benchtop procedures into microscale, parallelized operations, allowing researchers to screen thousands to millions of compounds or cellular samples in a single, automated run [23] [21]. This is crucial for exploring vast chemical and biological spaces in early drug discovery.
Key Quantitative Impacts of Miniaturization: Table: Throughput and Scale Comparison of Screening Platforms
| Screening Platform | Assay Volume | Throughput | Key Application |
|---|---|---|---|
| Traditional Microtiter Plate | Microliter to milliliter [24] | ~10^3-10^4 clones per campaign [25] | Standard low-throughput screening |
| Droplet Microfluidics | Femtoliter to nanoliter droplets [21] [25] | >300,000 clones in a single experiment [21] | Ultrahigh-throughput enzyme and antibody screening |
| Integrated LoC Systems | Nanoliter-scale chambers [23] | >10,000 high-resolution images in under one hour [21] | High-content cellular analysis and functional readouts |
Drastic Reduction in Reagent and Sample Consumption
The core benefit of reduced volumes is a dramatic decrease in reagent costs and the consumption of precious samples, such as patient-derived cells or novel chemical compounds. Assays performed in picoliter or nanoliter droplets instead of microliter wells can reduce reagent consumption by orders of magnitude [21]. This miniaturization makes large-scale screening campaigns economically viable and enables more research with limited biological samples.
Key Quantitative Impacts of Reagent Reduction: Table: Economic and Practical Benefits of Volume Reduction
| Parameter | Traditional Workflow | Microfluidic Workflow | Impact |
|---|---|---|---|
| Reagent Cost per Assay | High (microliter/milliliter scale) | >1000-fold reduction (nanoliter/picoliter scale) [21] | Enables large-scale screening within budget constraints |
| Sample Requirement | Large volumes | Minimal cell numbers or compound mass | Facilitates work with patient-derived and primary cells [22] |
| Waste Generation | Significant | Minimal | Reduces environmental and disposal costs |
Enhanced Precision and Control
Microfluidic devices provide unparalleled precision in controlling the cellular and chemical microenvironment. Key principles like laminar flow and diffusion-based mixing allow for the generation of highly stable concentration gradients and the precise manipulation of cells [23]. This level of control is fundamental for creating physiologically relevant models and obtaining high-quality, reproducible data.
Key Areas of Enhanced Precision:
- Concentration Gradients: Microfluidic gradient generators enable simultaneous testing of multiple drug concentrations on a single chip with high fidelity, rapidly identifying optimal therapeutic doses [21].
- Tissue-Specific Microenvironments: Organs-on-chips (OoCs) use microfluidic flow and 3D architectures to replicate tissue-specific mechanics and cellular interactions, improving the physiological relevance of toxicity and efficacy testing [23] [22].
- Single-Cell Analysis: Droplet-based encapsulation creates millions of isolated picoliter reactors, enabling functional readouts and screening at the single-cell level with high resolution [21] [25].
Experimental Protocols
Protocol 1: Ultrahigh-Throughput Screening of Enzyme Libraries via Droplet Microfluidics
This protocol describes an activity-based screen of a metagenomic ketoreductase (KRED) library using droplet microfluidics and fluorescence-activated cell sorting (FACS) [25].
Research Reagent Solutions
Table: Essential Reagents for Droplet-Based Enzyme Screening
| Item | Function | Example/Note |
|---|---|---|
| Fluorogenic Substrate | Enzyme activity reporter; fluorescence increases upon reaction. | e.g., alcohol 3 [25] |
| Cofactor | Essential for enzymatic redox reaction. | NAD+ or NADP+ [25] |
| Water-in-Oil (w/o) Emulsion Reagents | Creates stable, monodisperse aqueous droplets in a continuous oil phase. | Surfactants and oil for droplet generation and stability [25] |
| Cell Lysis Reagents | Releases intracellular enzymes for activity assay. | Benzonase and lysozyme [25] |
| Culture Media | Supports cell growth and protein expression. | ZY autoinduction medium [25] |
Workflow Diagram
Step-by-Step Procedure
Library Preparation and Induction
- Transform an E. coli metagenomic library for expression of KRED variants.
- Grow clones in ZY autoinduction medium to express the enzymes.
Droplet Generation and Incubation
- Resuspend the cell library in a buffer containing the fluorogenic alcohol substrate (e.g., 1 mM alcohol 3) and necessary cofactors.
- Use a microfluidic flow-focusing device to encapsulate single cells into water-in-oil droplets with an average occupancy of 0.1 cells/droplet. The final assay volume is in the picoliter range (e.g., 660 pL) [21] [25].
- Collect the emulsion and incubate for 48 hours at 30°C with orbital shaking (100 rpm) for enzyme expression and reaction.
Droplet Analysis and Sorting
- After incubation, re-emulsify the primary w/o emulsion into a water-in-oil-in-water (w/o/w) double emulsion compatible with FACS.
- Analyze and sort the droplets using a flow cytometer equipped with a 405 nm laser and a 525/50 nm emission filter.
- Set a fluorescence threshold to identify and sort droplets containing active KRED enzymes.
Hit Recovery and Validation
- Collect sorted droplets into growth media, break the emulsion, and plate the cells on LB agar plates.
- After growth, pick colonies and re-assay for activity in a 96-well plate format to confirm hits.
- Sequence plasmids from validated hits to identify novel KRED genes.
Protocol 2: High-Content Drug Screening on a Cartilage-on-Chip Platform
This protocol uses a microfluidic chip with an integrated gradient generator and parallel culture chambers for high-fidelity dose-response studies on tissue models [21].
Research Reagent Solutions
Table: Essential Reagents for Organ-on-Chip Drug Screening
| Item | Function | Example/Note |
|---|---|---|
| Chondrocytes or Cell Line | Primary cells or cell line representing the target tissue. | Primary chondrocytes for cartilage modeling [21] |
| Extracellular Matrix (ECM) Hydrogel | Provides a 3D, physiologically relevant scaffold for cell culture. | Collagen, Matrigel, or alginate [22] |
| Drug Solution | The therapeutic compound for testing. | e.g., Resveratrol [21] |
| Culture Media | Maintains cell viability and function during the experiment. | Standard media supplemented as required. |
| Cell Viability/Cell Death Stains | Enables quantitative assessment of drug efficacy and toxicity. | e.g., Live/Dead assay kits [22] |
Workflow Diagram
Step-by-Step Procedure
Device Priming and Cell Loading
- Sterilize the polycarbonate or PDMS microfluidic device. To minimize small molecule absorption, consider using alternative polymers like polycarbonate [22].
- Prepare a suspension of chondrocytes in an ECM hydrogel precursor (e.g., GelMA).
- Load the cell-laden hydrogel into the parallel culture chambers of the chip and crosslink to form a stable 3D tissue construct.
Concentration Gradient Generation and Drug Perfusion
- Prepare a stock solution of the drug candidate (e.g., Resveratrol).
- Use the integrated microfluidic gradient generator to create a linear dilution of the drug stock, producing a range of concentrations that are simultaneously perfused through the parallel culture chambers.
- Maintain dynamic flow using a syringe or peristaltic pump to perfuse the drug gradients and fresh media through the cultures for the desired duration (e.g., 72 hours), mimicking physiological shear stress.
Functional Readouts and Analysis
- High-Content Imaging: After treatment, perform live/dead staining and acquire high-resolution images of each chamber using an automated microscope. Quantify cell viability and morphology for each drug concentration.
- Biochemical Analysis: Extract RNA or proteins from the on-chip cultures for transcriptomic or proteomic profiling to understand drug response mechanisms [21].
- Data Integration: Integrate viability and 'omics data to identify the optimal scaffold-doping dose or the IC50 value of the drug, providing a dose-response profile that closely reflects human physiology.
Market Landscape and Growth Projections for Pharma and Biotech Applications
The global microfluidics market is demonstrating robust growth, driven by its increasing adoption in pharmaceutical and biotechnology research. This technology, which involves manipulating small fluid volumes within microscale channels, is revolutionizing drug discovery and development by enabling high-throughput screening with unparalleled precision and efficiency. [23] [26]
Market analyses project a consistent upward trajectory. The market was valued between USD 21.36 billion and USD 22.43 billion in 2024 and is expected to advance at a compound annual growth rate (CAGR) of 7.8% to 15.5%, culminating in a projected value of USD 32.67 billion to USD 65.9 billion by 2029-2032. This growth is fueled by the rising demand for point-of-care diagnostics, increased need for efficient sample analysis, and continuous technological innovations. [26] [27]
Table 1: Global Microfluidics Market Size Projection (2022-2032)
| Year | Market Size (USD Billion) |
|---|---|
| 2022 | 19.3 |
| 2023 | 21.9 |
| 2024 | 24.5 |
| 2025 | 28.6 |
| 2026 | 32.9 |
| 2027 | 36.8 |
| 2028 | 39.8 |
| 2029 | 45.0+ |
| 2030 | 50.5 |
| 2031 | 57.2 |
| 2032 | 65.9 |
The broader pharmaceutical context shows that 75% of global life sciences executives express optimism about 2025, with 68% anticipating revenue increases and 57% predicting margin expansions. This optimism persists despite industry challenges, including pricing pressures and a significant patent cliff threatening over USD 300 billion in sales through 2030. [28]
Key Market Segments and Applications
Product and Material Segmentation
Microfluidic components account for the largest market share, with microfluidic chips leading this segment. These chips, which form the core of microfluidic systems, are miniaturized devices with etched channels and chambers that precisely control fluid volumes ranging from microliters to nanoliters. [27]
Table 2: Microfluidics Market by Material Type (2024)
| Material | Market Share | Key Characteristics |
|---|---|---|
| PDMS (Polydimethylsiloxane) | 49% | Flexible, biocompatible, oxygen permeable, easy fabrication |
| Glass | 27% | Excellent optical clarity, chemical resistance, high precision |
| Silicon | 18% | High precision, durable, suitable for complex architectures |
| Other Materials | 6% | Includes polymers, paper, and hybrid composites |
The dominance of PDMS is attributed to its flexibility, biocompatibility, and suitability for rapid prototyping. However, alternative materials like PMMA (polymethyl methacrylate) are gaining traction due to superior optical clarity, chemical resistance, and cost-effectiveness for specific applications. [26] [27]
Application in Pharmaceutical and Biotech Workflows
Microfluidics technology has penetrated multiple facets of pharmaceutical research and development:
Drug Discovery and Screening: Microfluidic devices enable high-throughput screening (HTS) with significantly reduced reagent consumption and experimental time compared to traditional methods like 96-well plates. They facilitate precision dosing and create physiologically relevant microenvironments for cells and tissues, providing more accurate drug efficacy assessments. [1]
Organ-on-Chip Technology: Advanced platforms such as heart-on-chip (HoC) systems replicate human cardiac physiology with remarkable fidelity. These systems incorporate 3D co-cultures of key cardiac cell types (cardiomyocytes, endothelial cells, fibroblasts) in spatially designed arrangements, replicating native multicellular architecture and electromechanical coupling properties essential for accurate disease modeling and drug testing. [3]
Drug Delivery Systems: Microfluidics enables the generation of highly stable, uniform, monodispersed drug carrier particles with higher encapsulation efficiency compared to bulk methods. The technology allows precise control over nanoparticle size and composition, crucial for optimizing drug bioavailability and targeted delivery. [1] [29]
Diagnostics and Point-of-Care Testing: Lab-on-a-chip (LOC) devices miniaturize complex laboratory workflows into compact platforms for applications including infectious disease testing, PCR, genetic screening, and multi-analyte detection. Their portability and minimal reagent requirements make them ideal for resource-limited settings. [23]
Experimental Protocols
Protocol 1: Heart-on-Chip Platform for Cardiotoxicity Screening
Objective: To establish a reproducible heart-on-chip model for assessing drug-induced cardiotoxicity using patient-derived induced pluripotent stem cell (iPSC)-cardiomyocytes.
Materials:
- PDMS-based microfluidic device with integrated microchannels
- Patient-derived iPSC-cardiomyocytes
- Cardiac fibroblasts and endothelial cells
- Culture medium supplemented with growth factors
- Extracellular matrix (ECM) hydrogel (e.g., Matrigel, collagen)
- Real-time biosensors for electrophysiological monitoring
- Test compounds and control articles
Procedure:
- Device Preparation: Fabricate microfluidic devices using soft lithography with PDMS. Sterilize devices using UV irradiation or autoclaving.
- Cell Seeding and Culture:
- Prepare cell suspension containing iPSC-cardiomyocytes, cardiac fibroblasts, and endothelial cells at a ratio of 70:15:15 in ECM hydrogel.
- Introduce cell-hydrogel mixture into the microfluidic chamber at a density of 20-30 million cells/mL.
- Allow gel polymerization for 30 minutes at 37°C.
- Perfuse with culture medium at a flow rate of 0.1-1 μL/s to mimic physiological shear stress.
- Maturation Phase: Maintain the construct under continuous perfusion for 7-14 days to allow tissue maturation and functional synchronization.
- Functional Assessment:
- Monitor contractility using integrated motion sensors or video analysis.
- Record electrophysiological parameters using embedded microelectrodes.
- Measure biomarker secretion (e.g., troponin, BNP) via integrated biosensors.
- Compound Testing:
- Expose tissues to test compounds via perfusion medium.
- Include positive (e.g., doxorubicin for cardiotoxicity) and negative controls.
- Monitor functional parameters continuously for 72 hours.
- Assess viability using calibrated ATP-based assays.
- Data Analysis:
- Quantify changes in beating frequency, contractile force, and conduction velocity.
- Determine IC50 values for functional parameters.
- Compare biomarker release profiles between treatments.
Protocol 2: Microfluidic Synthesis of Drug-Loaded Nanoparticles
Objective: To fabricate uniform, monodispersed drug-loaded lipid nanoparticles using a staggered herringbone micromixer (SHM) design.
Materials:
- PDMS or PMMA microfluidic chip with SHM pattern
- Lipid mixture in ethanol (e.g., POPC, cholesterol, triolein)
- Aqueous phase containing therapeutic agent (e.g., siRNA, small molecule drug)
- Precision syringe pumps with flow rate control
- Collection vial with appropriate buffer
- Dynamic light scattering instrument for size characterization
- HPLC system for encapsulation efficiency analysis
Procedure:
- Device Preparation:
- Fabricate SHM device using soft lithography or hot embossing.
- Condition channels with appropriate solvent prior to use.
- Solution Preparation:
- Prepare lipid solution in ethanol at 10-20 mg/mL concentration.
- Dissolve therapeutic agent in aqueous buffer (e.g., citrate, phosphate) at target concentration.
- System Setup:
- Load lipid solution into glass syringe connected to inlet 1.
- Load aqueous phase into glass syringe connected to inlet 2.
- Mount syringes in precision pumps and connect to microfluidic device.
- Place collection vial at outlet port.
- Nanoparticle Formation:
- Initiate flow with defined flow rate ratio (FRR = 3:1 aqueous-to-organic phase).
- Set total flow rate to 10-20 mL/min initially.
- Collect nanoparticle suspension in vial containing 5x volume of dilution buffer.
- Process Optimization:
- Systematically vary flow rate ratio (1:1 to 5:1) to optimize particle size.
- Adjust total flow rate to control mixing efficiency.
- Modify lipid composition to alter encapsulation properties.
- Characterization:
- Determine particle size and polydispersity index by dynamic light scattering.
- Measure zeta potential using electrophoretic light scattering.
- Quantify drug encapsulation efficiency via HPLC after removal of unencapsulated drug.
- Assess stability over 14 days at 4°C and 25°C.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Microfluidic Applications
| Reagent/Material | Function | Application Examples |
|---|---|---|
| PDMS (Polydimethylsiloxane) | Flexible polymer for device fabrication; biocompatible and oxygen permeable | Organ-on-chip devices, droplet generators, micromixers |
| PMMA (Polymethyl methacrylate) | Rigid polymer with excellent optical clarity; chemical resistant | Microfluidic chips for diagnostics, high-throughput screening devices |
| Extracellular Matrix Hydrogels (Matrigel, collagen) | Provide 3D scaffold for cell culture; mimic in vivo microenvironment | Organ-on-chip models, 3D cell culture, tissue barrier models |
| Lipid Mixtures (POPC, cholesterol, PEG-lipids) | Form self-assembling nanostructures for drug encapsulation | Lipid nanoparticle synthesis, nucleic acid delivery systems |
| Fluorescent Tags and Biosensors | Enable real-time monitoring of cellular responses and analyte detection | High-content screening, metabolic activity assays, biomarker detection |
| Surface Modification Reagents (PLL-g-PEG, silanes) | Modify channel surface properties to control cell adhesion or prevent non-specific binding | Cell patterning, reduction of analyte adsorption, enhanced biocompatibility |
Future Outlook and Strategic Implications
The microfluidics field is positioned for continued expansion and technological advancement. Several emerging trends are likely to shape its future development:
Integration with Artificial Intelligence: AI-driven microfluidics is emerging as a powerful combination, enabling intelligent experimental design, real-time process optimization, and advanced data analysis from high-content screening assays. [23] [28]
Multi-Organ Chip Systems: The development of integrated multi-organ platforms (e.g., heart-liver chips) allows researchers to study systemic drug metabolism and organ-specific toxicity in ways that were previously impossible, addressing critical needs in managing polypharmacy. [3]
Point-of-Care Diagnostics: Digital microfluidics, which uses electric fields to manipulate individual droplets on an open surface, offers a more adaptable platform for clinical diagnostics, potentially enabling rapid testing in resource-limited settings. [27]
Personalized Medicine Applications: The incorporation of patient-derived iPSCs into organ-on-chip platforms enables creation of truly individualized disease models, opening new frontiers for personalized therapeutic testing and precision medicine. [3]
For researchers and drug development professionals, understanding these market dynamics and mastering the associated experimental protocols is becoming increasingly crucial. The ability to leverage microfluidic technologies effectively will provide significant advantages in accelerating drug discovery pipelines, enhancing predictive accuracy, and ultimately bringing safer, more effective therapies to patients faster.
From Concept to Lab: Implementing Microfluidic Systems for Advanced Screening and Assays
High-Throughput Screening (HTS) has fundamentally transformed the pace and efficiency of therapeutic discovery since its emergence in the mid-1980s, reducing months of manual work to days by enabling the parallel testing of thousands of compounds [30]. By definition, HTS simultaneously analyzes thousands of samples for biological activity at the cellular, pathway, or molecular level, with a screen considered "high throughput" when it conducts over 10,000 assays per day [30]. The primary goal of HTS is to rapidly identify active compounds, proteins, or genes—collectively known as "hits"—that modulate a specific biomolecular pathway [31] [30]. This technique has expanded from its pharmaceutical industry origins into diverse research fields including synthetic biology, tissue engineering, and regenerative medicine [30].
The adoption of miniaturized assay formats such as 1536-well plates, advanced automation, robotics, and sophisticated data analysis tools has been crucial to this evolution [32] [30]. More recently, quantitative HTS (qHTS) has emerged as a powerful advancement, allowing researchers to test compounds across multiple concentrations simultaneously, thereby generating concentration-response data that provides richer information on compound activity and potency [20] [30]. When framed within the context of microfluidic devices for drug discovery, HTS platforms gain enhanced capabilities for manipulating small fluid volumes with high precision, enabling more complex and information-rich experiments [23].
HTS Platform Architectures
HTS platforms integrate multiple components into a cohesive system designed for automated, rapid experimentation. The architecture determines the platform's capabilities, throughput, and suitability for specific applications.
Traditional and Microtiter Plate-Based Systems
Traditional HTS relies heavily on microtiter plate formats and robotic liquid handling systems. The evolution from 96-well to 1536-well plates and beyond has significantly increased throughput while reducing reagent consumption and cost [32] [30]. These systems typically incorporate:
- Automated liquid handlers for precise compound and reagent dispensing
- Robotic plate handlers to transport plates between instruments
- High-sensitivity detectors to capture assay signals [20] [32]
- Environmental controllers to maintain optimal conditions for biological assays
This architecture supports a wide range of assay types, including biochemical, cell-based, and phenotypic screens. However, it faces limitations in reagent consumption, operational complexity for complex assays, and fluid handling precision at very small volumes [32].
Microfluidic and Lab-on-a-Chip Systems
Microfluidics, the science of manipulating small fluid volumes (microliter to picoliter range) within channels less than 1 millimeter wide, enables the development of lab-on-a-chip (LoC) devices that integrate multiple laboratory functions into a single, compact platform [23]. These systems offer several distinct advantages for HTS:
- Minimal reagent and sample consumption
- Faster analysis and processing times
- High precision and reproducibility due to exact fluid control
- Portability and compact design
- Integrated, automated workflows [23]
Key microfluidic architectures for HTS include:
- Continuous-flow chips: Utilize microchannels to move fluids for mixing, separation, and chemical reactions
- Droplet-based microfluidics: Create isolated picoliter compartments for single-cell analysis or digital PCR, enabling ultra-high-throughput screening [23]
- Paper-based microfluidics: Provide low-cost, disposable diagnostic tools suitable for point-of-care testing [23]
- Valved microfluidic chips: Incorporate integrated microvalves to automate and control complex fluidic operations [23]
Active-Matrix Digital Microfluidics (AM-DMF)
A transformative evolution in microfluidics, Active-Matrix Digital Microfluidics (AM-DMF) leverages semiconductor-derived electrode arrays to dynamically control thousands of micrometre-scale droplets independently and in parallel [17]. This architecture represents a significant advancement over conventional microchannel-based systems and earlier passive-matrix approaches.
AM-DMF enables various programmable operations—including droplet generation, transport, mixing, merging, splitting, and dilution—with unparalleled accuracy [17]. The technology has evolved through several generations:
- DMF 1.0 (Passive-Matrix): Early digital microfluidics with limited scalability
- DMF 2.0 (Active-Matrix): Introduced thin-film transistors (TFTs) for enhanced control of larger droplet arrays
- DMF 2.5 (Gate-on-Array): Further improved integration and control capabilities
- DMF 3.0 (Integrated Circuit-Driven): Currently emerging with full integration of driving circuits for highest performance [17]
This progression has been a key driver in advancing the commercialization of microfluidic technology for high-throughput biological applications [17].
Table 1: Comparison of HTS Platform Architectures
| Architecture | Throughput Potential | Volume Range | Key Advantages | Common Applications |
|---|---|---|---|---|
| Microtiter Plate-Based | 10,000 - 100,000 assays/day [30] | Microliter | Established protocols, compatible with diverse assays | Compound screening, target validation |
| Continuous-Flow Microfluidics | Moderate to High | Nanoliter to Microliter | Precise fluid control, integrated functions | Chemical synthesis, cell analysis [23] |
| Droplet-Based Microfluidics | Very High (kHz rates) | Picoliter | Massive parallelism, single-cell resolution | Single-cell analysis, digital PCR [23] |
| Active-Matrix DMF | High (parallel droplet control) | Nanoliter (e.g., 0.5 nL [17]) | Dynamic reconfigurability, programmability | Genomics, single-cell analysis, diagnostics [17] |
Core HTS Workflows
The HTS process comprises multiple interconnected stages, from initial planning to hit confirmation. Successful implementation requires careful coordination across these phases.
Assay Development and Library Design
The foundation of any HTS campaign lies in robust assay development and strategic library design. The scientific objective must be clearly defined, typically categorized as either optimization (enhancing a target property by tuning material structure or processing) or exploration (mapping a structure-property relationship to build predictive models) [33].
Feature selection involves identifying relevant variables—both intrinsic (e.g., polymer composition, architecture, sequence patterning, molecular weight) and extrinsic (e.g., sample preparation protocols, substrate choice) [33]. For combinatorial libraries, careful consideration of variable discretization (subdividing features into intervals across the desired range) and design space size is crucial for managing experimental complexity [33].
Assay development must address:
- Biological relevance to the target pathway or phenotype
- Robustness and reproducibility under automated conditions
- Compatibility with detection systems and automation platforms
- Signal-to-noise optimization to ensure sufficient window for hit identification [31]
Screening Execution and Hit Identification
The screening phase involves running the actual experiments and identifying candidate hits based on established criteria.
Table 2: Key Steps in HTS Screening Execution
| Step | Description | Technical Considerations |
|---|---|---|
| Sample Preparation | Reformating compound libraries into assay-ready plates | Miniaturization (1536-well plates), DMSO tolerance, compound stability [32] [30] |
| Liquid Handling | Transferring compounds, reagents, and cells | Automation, precision (CV < 10%), compatibility with assay volumes |
| Assay Incubation | Allowing biological reaction to proceed | Environmental control (temperature, CO₂, humidity), timing synchronization |
| Signal Detection | Measuring assay endpoint or kinetic reads | Detection modality (luminescence, fluorescence, absorbance), sensitivity, dynamic range |
| Hit Identification | Selecting compounds with significant activity | Statistical criteria (e.g., >3σ from mean), normalization methods (Z-score, B-score) [31] |
In qHTS, concentration-response curves are generated simultaneously for thousands of compounds, typically modeled using the Hill equation (Equation 1) to estimate key parameters like AC₅₀ (concentration for half-maximal response) and E_max (maximal response) [20]:
Where Ri is the measured response at concentration Ci, E₀ is the baseline response, E_∞ is the maximal response, and h is the Hill slope [20].
However, parameter estimates from the Hill equation can be highly variable when the tested concentration range fails to include at least one of the two asymptotes, when responses are heteroscedastic, or when concentration spacing is suboptimal [20]. False positives and false negatives remain significant challenges, as truly null compounds may appear active due to random variation, while truly active compounds with "flat" profiles may be missed [20].
HTS Data Analysis and Hit Validation
Data analysis transforms raw screening data into meaningful biological insights. The process involves multiple quality control steps to address systematic variation inherent in automated screening processes [31].
Traditional plate controls-based and non-controls-based statistical methods have been widely used for HTS data processing and active identification [31]. More recently, improved robust statistical methods have been introduced to reduce the impact of systematic row/column effects, though these can sometimes be misleading and result in more false positives or false negatives if applied inappropriately [31].
A recommended three-step statistical decision methodology includes:
- Determining the most appropriate HTS data-processing method and establishing criteria for quality control review from assay signal window and DMSO validation tests
- Performing a multilevel statistical and graphical review of screening data to exclude results outside quality control criteria
- Applying the established active criterion to quality-assured data to identify active compounds [31]
Secondary screening provides critical hit validation through more physiologically relevant models, including:
- Cell-based assays for cellular activity and selectivity
- ADMET assays (absorption, distribution, metabolism, excretion, toxicity) for preliminary pharmacokinetic assessment
- Biophysical assays to confirm direct target engagement [30]
Experimental Protocols
Protocol 1: Quantitative HTS (qHTS) with Concentration-Response Analysis
This protocol describes the process for running a qHTS campaign and analyzing the resulting concentration-response data [20].
Materials and Reagents
- Compound library (typically 10,000-100,000 compounds)
- Assay reagents specific to biological target
- Cell line (if cell-based assay)
- Solvent controls (DMSO, buffer)
- Reference controls (positive/negative)
Procedure
- Assay Preparation
- Format compound library in 1536-well plates using acoustic dispensing or pintool transfer
- Include control wells (16-32 wells/plate) for background, positive control, and negative control
- Use concentration ranges spanning at least 4 orders of magnitude (e.g., 1 nM - 100 µM)
Compound Transfer
- Employ non-contact dispensing for compound addition to minimize carryover
- Maintain consistent DMSO concentration across all wells (typically <1%)
- Include randomization schemes to mitigate plate position effects
Assay Incubation and Readout
- Incubate plates under appropriate environmental conditions
- Measure endpoint or kinetic signals using plate readers
- Record raw data for subsequent analysis
Data Normalization
- Normalize raw data using plate-based controls:
- Apply correction algorithms (B-score, Z-score) to remove systematic row/column effects [31]
Curve Fitting and Parameter Estimation
- Fit normalized concentration-response data to Hill equation (Equation 1)
- Estimate key parameters: AC₅₀, E_max, Hill slope (h), and baseline (E₀)
- Assess curve fit quality using R² or similar goodness-of-fit metrics
Hit Classification
- Classify compounds based on curve shape and efficacy
- Prioritize full agonists/antagonists with well-defined AC₅₀ values
- Exclude promiscuous inhibitors and cytotoxic compounds using counter-screens
Troubleshooting Notes
- Poor curve fits often result from inadequate concentration range or insufficient asymptote definition [20]
- AC₅₀ estimates are most reliable when the concentration range defines both upper and lower response levels [20]
- Increasing replicate measurements (n=3-5) significantly improves parameter estimation precision [20]
Protocol 2: Active-Matrix Digital Microfluidics (AM-DMF) for High-Throughput Screening
This protocol describes the use of AM-DMF technology for high-throughput droplet-based screening applications [17].
Materials and Reagents
- AM-DMF device (TFT-based active matrix)
- Aqueous samples (compounds, cells, reagents)
- Immersion oil (filler fluid)
- Surface coatings (e.g., fluorocarbon layers) to reduce fouling
- Cleaning solutions (ethanol, detergents)
Procedure
- Device Preparation
- Clean AM-DMF device surface with appropriate solvents
- Apply hydrophobic and/or antifouling coatings if required
- Fill device with immersion oil to reduce evaporation and facilitate droplet movement
Droplet Generation and Loading
- Dispense nanoliter-scale aqueous samples onto device
- Generate droplets of precise volumes using electrode actuation patterns
- Verify droplet size and consistency through imaging
Droplet Manipulation
- Program electrode activation sequences for droplet transport
- Implement mixing protocols through rapid droplet merging and splitting
- Perform dilution steps using controlled droplet combinations
Assay Execution
- Merge compound, target, and detection reagent droplets
- Incubate for appropriate time with temperature control
- Measure endpoint or kinetic signals using integrated detection
Data Collection and Analysis
- Use integrated sensors (impedance, optical) for real-time monitoring
- Record droplet positions and assay results
- Analyze data using custom or commercial software
Technical Considerations
- Electrode design and driving waveforms significantly impact droplet manipulation reliability [17]
- Integration of sensing capabilities (e.g., impedance, optical) enables real-time droplet tracking and analysis [17]
- Biofouling remains a challenge and requires appropriate surface treatments or device passivation [17]
Visualization of HTS Workflows
HTS Experimental Workflow
HTS Experimental Workflow
Quantitative HTS Data Analysis
Quantitative HTS Data Analysis
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for HTS
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Compound Libraries | Source of chemical diversity for screening | Include diversity-oriented synthesis compounds, natural products, FDA-approved drugs [30] |
| Cell Lines | Biological system for phenotypic or target-based screening | Use engineered lines with reporter constructs for specific pathways; primary cells for physiological relevance |
| Detection Reagents | Generate measurable signals from biological activity | Luminescence for sensitivity, fluorescence for homogeneity, absorbance for cost-effectiveness |
| Assay Kits | Optimized reagent combinations for specific targets | Provide standardized protocols and controls; ensure reproducibility across screens |
| Surface Coatings | Modify substrate properties for cell attachment or reduce fouling | Extracellular matrix proteins for cell-based assays; PEG or fluorocarbon for microfluidics [17] |
| Immersion Oils | Filler fluid for digital microfluidics | Enable droplet actuation; prevent evaporation; must be immiscible with aqueous samples [17] |
High-Throughput Screening platforms have evolved from simple microtiter plate-based systems to sophisticated architectures incorporating microfluidics, automation, and advanced data analytics. The integration of quantitative approaches that generate concentration-response data and miniaturized technologies like active-matrix digital microfluidics is driving increased information content and efficiency in drug discovery.
The future of HTS lies in the continued convergence of biology, engineering, and data science. Artificial intelligence is already being integrated into platforms like AM-DMF to increase the efficiency and reliability of complex workflows [17]. Similarly, 3D cell models and organ-on-chip technologies are providing more physiologically relevant screening environments [23]. As these technologies mature, HTS will continue to transform from a simple hit identification tool to an integrated platform for understanding complex biological systems and advancing personalized medicine.
Concentration Gradient Generators (CGGs) for Rapid, Accurate Dose-Response Studies
Concentration Gradient Generators (CGGs) represent a transformative microfluidic technology that enables the precise generation of concentration gradients for dose-response studies in drug discovery research. Traditional methods for creating drug dilutions, such as manual pipetting and serial dilution, are not only time-consuming and labor-intensive but also prone to cumulative errors, which can significantly affect the determination of key pharmacological parameters like the half-maximal inhibitory concentration (IC₅₀) [7]. Microfluidic CGGs address these limitations by leveraging the unique behavior of fluids at the microscale, allowing for the rapid, accurate, and high-throughput creation of concentration gradients [34] [7]. This capability is crucial for applications ranging from high-throughput drug screening and antimicrobial susceptibility testing (AST) to personalized medicine, as it systematically evaluates the optimal concentration of a single drug or the most effective drug combinations [35] [7]. By integrating CGGs with on-chip cell culture arrays, these platforms facilitate automated assay workflows, reduce manual errors, and enhance experimental efficiency, thereby accelerating the drug development process [36].
Theoretical Foundations and Operating Principles
The operation of microfluidic CGGs is governed by the fundamental principles of fluid dynamics at low Reynolds numbers (Re), where laminar flow predominates, and viscous forces far exceed inertial forces [34] [23]. In this regime, fluids flow in parallel streams without turbulence, and mixing occurs primarily through molecular diffusion at the interface between adjacent fluid streams [34].
Two primary types of CGGs have been developed based on their mixing mechanisms:
- Passive CGGs: These generators rely on channel geometry and hydrodynamic resistance to control fluid mixing without external fields. A classic example is the "Christmas tree" design, which uses a network of bifurcating and recombining channels to perform serial dilutions, generating a linear concentration gradient across multiple output channels [34] [37]. The final concentration at each output is determined by the principle of flow resistance, analogous to Ohm's law in electric circuits. The volumetric flow rate (Q) is related to the pressure drop (ΔP) and hydraulic resistance (R) by ΔP = Q × R. By designing channels with specific resistance ratios, the desired flow rate ratios—and thus concentration ratios—can be precisely achieved [37].
- Active CGGs: These systems utilize external physical fields (e.g., magnetic, acoustic, electric) to precisely control fluid mixing, enabling the generation of dynamic and complex (nonlinear) concentration gradients [34]. This allows for more sophisticated simulations of in vivo conditions.
A critical advancement is the development of flowless diffusional μ-CGGs. Unlike conventional systems that require continuous fluid flow, these devices generate shear-free concentration gradients via diffusion alone within a microfluidic grid connecting source and sink reservoirs. This design is particularly beneficial for cell-based assays, as it eliminates shear stress that can influence cellular behavior [36].
Key Experimental Protocols
Protocol 1: High-Throughput Cancer Drug Screening Using a Laminar Flow-Based CGG
This protocol details the use of a pressure-driven CGG for the cytotoxicity assessment of chemotherapeutic agents [7].
Materials and Reagents
- Microfluidic Device: Fabricated from Cycle Olefin Polymer (COP) via hot embossing [7].
- Cell Line: Human bladder cancer cells (T24) [37].
- Drugs of Interest: e.g., Cisplatin, Gemcitabine [37].
- Staining Reagents: Fluorescein for gradient validation; CellTracker Green CMFDA or propidium iodide (PI) for live/dead cell staining [7].
- Buffer: Phosphate-buffered saline (PBS) or cell culture medium.
Procedure
- Device Priming: Flush all microchannels with a buffer solution, such as PBS, to remove air bubbles and ensure proper wetting of the channels. Use a syringe pump to maintain a steady flow during this process.
- Gradient Validation: Before cell-based experiments, validate the generated concentration gradient. Introduce a fluorescein solution into the drug inlet and PBS into the buffer inlet. After allowing the gradient to stabilize (typically within 30 seconds [7]), capture the fluorescence profile across the output channels using a fluorescence microscope. Confirm that the measured concentrations conform to the theoretical values (e.g., R² > 0.99 [7]).
- On-Chip Cell Culture: Seed T24 cells embedded in a 3D fibrin gel into the cell culture chambers of the device. Allow the cells to attach and stabilize under a continuous flow of fresh culture medium for 24-48 hours.
- Drug Exposure: Introduce the drug solution and the cell culture medium into their respective inlets. Apply a constant pressure to drive the flow, generating a stable concentration gradient across the parallel cell culture chambers. Maintain the drug exposure for a predetermined period (e.g., 24-72 hours).
- Viability Assessment: Terminate the drug flow and introduce a live/dead cell stain (e.g., CellTracker Green and PI) into the chambers. Incubate according to the staining protocol.
- Imaging and Analysis: Image each cell chamber using a fluorescence microscope or a high-content imaging system. Quantify the viability of the cells (e.g., the ratio of live to dead cells) in each chamber to determine the response at each drug concentration.
- Data Fitting: Plot cell viability against drug concentration and fit a dose-response curve (e.g., a sigmoidal model) to determine the IC₅₀ value.
Protocol 2: Flowless Diffusional Gradient Assay for Antimicrobial Susceptibility Testing (AST)
This protocol leverages a flowless CGG for shear-free, high-throughput AST, which is particularly useful for studying bacterial responses to antibiotic gradients [36].
Materials and Reagents
- Flowless μ-CGG Device: Fabricated in Polydimethylsiloxane (PDMS) via soft lithography from a PMMA mold [36].
- Bacterial Strain: e.g., Antibiotic-resistant Escherichia coli [35].
- Antibiotics: e.g., Tetracycline, Ciprofloxacin, Amikacin [35].
- Growth Medium: Suitable liquid broth for the bacterial strain (e.g., LB broth).
- Fluorescent Tracer: Such as fluorescein, for characterizing gradient generation.
Procedure
- Device Preparation: Sterilize the PDMS device using UV light or ethanol. Subsequently, flush the microchannels with sterile ultrapure water to remove any residual sterilization agents and prepare the device for use.
- Gradient Characterization: Pipette a fluorescent tracer solution into the source reservoir and PBS into the sink reservoir. Monitor the diffusion and establishment of the gradient over time using time-lapse fluorescence microscopy. This step determines the characteristic time required for gradient stabilization, which is influenced by the device's geometry and the solute's diffusivity [36].
- Bacterial Inoculation: Load a suspension of log-phase bacteria in growth medium into the central microfluidic grid or designated cell culture chambers.
- Assay Initiation: Carefully add the antibiotic solution to the source reservoir and fresh growth medium to the sink reservoir. The device will passively generate a stable, diffusion-based concentration gradient across the cell culture area without any applied flow.
- Incubation and Monitoring: Incubate the device at the appropriate temperature (e.g., 37°C). Monitor bacterial growth or inhibition at different positions within the gradient over 12-24 hours using time-lapse microscopy, for instance, by tracking optical density or a fluorescent viability marker.
- Endpoint Analysis: Determine the Minimum Inhibitory Concentration (MIC) by identifying the lowest antibiotic concentration in the gradient that completely inhibits visible bacterial growth at the end of the incubation period [35]. For combinatorial screening, this process can be repeated with multiple antibiotics loaded into different source inlets to generate combinatorial gradients [36] [35].
Data Presentation and Analysis
Performance Comparison of Microfluidic CGG Technologies
Table 1: Comparative analysis of major CGG types for dose-response studies.
| CGG Type | Gradient Profile | Throughput | Key Advantages | Inherent Limitations | Typical Stabilization Time |
|---|---|---|---|---|---|
| Passive (Christmas Tree) [34] [7] | Linear, Logarithmic | High | Simple structure, fast response, high reproducibility | Limited to pre-set gradient shapes, requires continuous flow | ~30 seconds [7] |
| Active (Field-Based) [34] | Dynamic, Nonlinear | Medium | Highly flexible, enables complex gradients | Requires complex external control systems | Millisecond to second scale (adjustable) |
| Flowless Diffusional [36] | User-defined via geometry | High | Shear-free, no pumps needed, simple operation | Slow gradient establishment, difficult to change quickly | Minutes to hours (diffusion-dependent) |
| 3D-Printed Multi-Drug [35] | Symmetric multi-drug combinations | Medium for 3+ drugs | Enables 3D fluidic routing for complex drug combinations | Complex fabrication, limited to 3D printing resolution | Similar to flow-based systems |
Key Reagents and Materials for CGG Experiments
Table 2: Essential research reagents and materials for conducting CGG-based dose-response studies.
| Item Name | Function/Application | Example Specifications |
|---|---|---|
| PDMS (Polydimethylsiloxane) [36] [37] | Elastomeric material for device fabrication; biocompatible and gas-permeable. | Sylgard 184, mixed 10:1 base:curing agent [36] |
| COP (Cycle Olefin Polymer) [7] | Thermoplastic for high-throughput devices; excellent optical clarity and low autofluorescence. | Zeonor 1020R [7] |
| Fluorescein [7] [37] | Fluorescent tracer for quantitative validation of concentration gradients. | High-purity, prepared in buffer at low micromolar concentrations [37] |
| 3D Cell Culture Matrix [37] | Hydrogel for embedding cells to mimic a more physiologically relevant tumor microenvironment. | Fibrin gel, Matrigel, or other biocompatible hydrogels |
| Viability Stains [7] | Fluorescent probes for distinguishing live and dead cells in endpoint analysis. | CellTracker Green CMFDA (live), Propidium Iodide (dead) [7] |
Workflow and System Integration
The following diagram illustrates the standard workflow for a CGG-based dose-response study, from device design to data analysis.
CGG Dose-Response Workflow
The "Christmas tree" structure is a fundamental and widely used design for passive CGGs. The following diagram details its operational principle.
Christmas Tree CGG Principle
Concentration Gradient Generators have firmly established themselves as a critical enabling technology in modern high-throughput drug discovery. Their ability to perform rapid (e.g., within 30 seconds [7]) and highly accurate generation of concentration gradients dramatically improves the efficiency of dose-response characterization, a cornerstone of pharmaceutical development [38]. The technology's miniaturization leads to a significant reduction in the consumption of precious reagents and cells, while its capacity for integration and automation minimizes manual errors and enhances experimental reproducibility [34] [23].
Future developments in the field are likely to focus on increasing the intelligence and closed-loop control capabilities of CGG systems [34]. The integration of artificial intelligence (AI) with active-matrix digital microfluidics is already showing promise for optimizing complex droplet handling and workflow automation [17]. Furthermore, the trend toward more accessible fabrication methods, such as 3D printing, and the development of novel, biocompatible materials will continue to lower the barrier for adoption and enable more complex biological simulations, such as multi-organ-on-a-chip platforms [35] [23]. As these technologies mature, CGG-based platforms are poised to become indispensable tools for achieving the goals of precision medicine, enabling the rapid identification of optimal, patient-specific therapeutic regimens.
Organ-on-a-Chip and Microphysiological Systems for Predictive Toxicity Testing
The escalating costs and high failure rates of conventional drug development have underscored the critical need for more predictive preclinical models. On average, developing a single new medicine takes 10 to 15 years and costs approximately $2.6 billion, with only 12% of new molecular entities that enter clinical trials ultimately receiving regulatory approval [39]. This inefficiency stems partly from the limited predictive value of existing preclinical tools, particularly for human-specific responses. Traditional 2D cell culture models lack physiological relevance, while animal models often suffer from interspecies differences that restrict human predictivity [40]. Organ-on-a-Chip (OoC) technology, also known as microphysiological systems (MPS), represents a transformative approach that bridges this gap by recreating organ-level functionality in vitro through microfluidic devices lined with living human cells, subject to organ-specific biomechanical cues and fluid flow [41].
The integration of MPS into predictive toxicology aligns with the FDA's plan to phase out animal testing and embraces a "quick win, fast fail" paradigm in pharmaceutical development [40] [39]. By providing human-relevant data early in the drug discovery pipeline, OoC technologies enable researchers to identify potential toxicity issues sooner, de-risk candidate selection, and ultimately improve clinical success rates. These systems combine microfluidic perfusion, 3D tissue architecture, and patient-derived cells to create living, human-relevant models that detect effects manifesting only in humans—positioning MPS as indispensable tools for modern predictive toxicology [40].
Technology Platforms for High-Throughput Toxicity Assessment
The transition of OoC technology from academic research to industrial application necessitates platforms capable of higher throughput and robust, reproducible operation. Recent advancements have yielded several commercial systems specifically designed to meet these demands within drug development workflows.
Table 1: Commercial High-Throughput Organ-on-Chip Platforms for Predictive Toxicology
| Platform Name | Vendor/Developer | Throughput Capability | Key Technological Features | Primary Toxicity Applications |
|---|---|---|---|---|
| AVA Emulation System | Emulate | 96 independent Organ-Chips per run | 3-in-1 platform with microfluidic control, automated imaging, self-contained incubator; Chip-Array consumable | Liver and kidney safety assessment, immunotoxicity, DILI prediction [42] |
| PhysioMimix Core | CN Bio | Up to 288 samples per controller (6 plates) | PDMS-free multi-chip plates; adjustable recirculating flow; compatible with single- and multi-organ studies | Safety toxicology, ADME, disease modeling [40] |
| OrganoPlate | MIMETAS | 40-96 chips per plate | Microfluidic 3D culture in standard well plate format; no artificial membranes; gravity-driven flow | Barrier integrity, transport, migration assays [39] |
| PREDICT96-ALI | Draper Laboratory | 96 chips per plate | Membrane-based platform; designed for air-liquid interface tissues | Respiratory toxicity, inhalation toxicology [39] |
The AVA Emulation System represents a significant advancement in throughput, combining microfluidic control for 96 Organ-Chip "Emulations" with automated imaging and a self-contained incubator. This system achieves a four-fold reduction in consumable spend and up to 50% fewer cells and media per sample compared to previous generation technology, while reducing hands-on lab time by more than half [42]. Similarly, the PhysioMimix Core system offers exceptional flexibility with the capability to run up to 6 plates simultaneously, accommodating 6-288 samples per controller, and supporting studies lasting up to 4 weeks while maintaining microtissue viability and function [40].
For specialized applications, platforms like the Chip-R1 Rigid Chip from Emulate address specific toxicology challenges with minimally drug-absorbing plastics, making it particularly suitable for ADME and toxicology applications where compound absorption by traditional PDMS materials could compromise results [42]. The modified design also enables physiologically relevant shear stress application, critical for immune cell recruitment studies and vascular toxicity assessment.
Application Protocols: Predictive Toxicity Assessment Using Organ-Chip Systems
Protocol 1: Nephrotoxicity Screening Using Kidney-on-Chip
Background and Principle: Drug-induced kidney injury represents a major cause of drug attrition and post-market withdrawals. Traditional 2D renal cell cultures lack the tubular structure and fluid flow dynamics essential for proper kidney function, limiting their predictive value. The kidney-on-chip model recreated by researchers like Dr. Samira Musam at Duke University leverages induced pluripotent stem cell (iPSC)-derived kidney cells in a microfluidic environment that reproduces nephron-relevant structure, fluid flow, and molecular transport for mechanistic interrogation of nephrotoxicity [43].
Table 2: Key Reagents and Materials for Kidney-on-Chip Nephrotoxicity Screening
| Research Reagent Solution | Function/Application | Specific Example/Properties |
|---|---|---|
| iPSC-derived podocytes and proximal tubule cells | Recreate functional kidney nephron components | Patient-specific cells for personalized toxicity assessment; express appropriate transporters and receptors |
| Specialized renal extracellular matrix | Provide physiological 3D microenvironment for kidney cells | Collagen-IV based hydrogel with appropriate stiffness (≈2-5 kPa) |
| Microfluidic chip with porous membrane | Enable tissue-tissue interface and basal-apical polarity | Chip-S1 stretchable chip or similar with 7 µm pores for cell communication |
| perfusion medium with physiological renal components | Support kidney cell viability and function | Contains albumin, glucose, electrolytes at physiological concentrations |
| Effluent collection system | Enable biomarker analysis and drug metabolism assessment | Automated fraction collector for time-stamped sampling |
Experimental Workflow:
- Differentiation and seeding: Differentiate iPSCs into kidney progenitor cells using established protocols involving CHIR99021 and FGF9 treatment over 7-9 days. Seed the resulting cells (approximately 2×10^6 cells/mL) into the renal ECM-filled microfluidic channel of the organ chip.
- Maturation under flow: Initiate perfusion of renal medium at 60-100 µL/hour to apply physiological shear stress (≈0.5-2 dyne/cm²) and promote tissue maturation over 10-14 days.
- Validation of functionality: Assess barrier function through TEER measurements (expect >200 Ω×cm² for mature tubules), albumin uptake (FITC-albumin assay), and expression of key transporters (OCT2, MATE1, OAT1 via qPCR).
- Compound exposure: Introduce nephrotoxins (e.g., cisplatin, gentamicin, tenofovir) or novel drug candidates at clinically relevant concentrations (typically 1-100 µM) through the perfusion medium for 24-72 hours. Include a parallel vascular channel for systemic exposure modeling when available.
- Endpoint assessment: Quantify multiple toxicity markers including LDH release (general cytotoxicity), KIM-1 and NGAL expression (specific kidney injury biomarkers), caspase-3 activity (apoptosis), and morphological changes via immunofluorescence (ZO-1, γH2AX).
- Data analysis and prediction: Compare biomarker levels to established nephrotoxin positive controls, apply multi-parameter toxicity scoring, and correlate with known clinical nephrotoxicity profiles.
This kidney-on-chip platform has demonstrated concordance with known nephrotoxins, enabled detection of off-target effects and cardio-renal complications, and revealed patient-to-patient variability in susceptibility, positioning it as an actionable tool for predictive toxicology [43].
Protocol 2: Hepatotoxicity Assessment Using Liver-Chip
Background and Principle: Drug-induced liver injury (DILI) remains the leading cause of acute liver failure and post-market drug withdrawals. The liver-chip model developed by companies such as Emulate and CN Bio incorporates primary human hepatocytes in a 3D microenvironment with continuous perfusion and non-parenchymal cell types (Kupffer cells, liver sinusoidal endothelial cells) to better predict human hepatotoxicity.
Experimental Workflow:
- Chip preparation and cell seeding: Coat chip membranes with collagen I (50 µg/mL) for 1 hour at 37°C. Seed primary human hepatocytes (1.2×10^6 cells/mL) into the parenchymal channel and liver sinusoidal endothelial cells (0.6×10^6 cells/mL) into the vascular channel, allowing attachment for 6 hours before initiating low flow (30 µL/hour).
- Tissue maturation: Gradually increase flow rate to 100 µL/hour over 48 hours to promote hepatocyte polarization and albumin synthesis. Co-culture with Kupffer cells (0.2×10^6 cells/mL) can be introduced at this stage for enhanced inflammatory response modeling.
- Functional validation: Assess hepatic functionality through albumin secretion (≥10 µg/day/10^6 cells), urea production (≥50 µg/day/10^6 cells), CYP450 activity (using substrate cocktails like Luciferin-IPA for CYP3A4), and bile canaliculi formation (using CDCFDA secretion assay).
- Compound exposure: Introduce test compounds (typically 3-5 concentrations across expected clinical range) through the vascular channel for 3-7 days, with daily medium renewal. Include positive controls (e.g., acetaminophen, troglitazone) and vehicle controls in each experiment.
- High-content analysis: Monitor multiple hepatotoxicity endpoints including ATP depletion (cell viability), ALT/AST release (hepatocellular damage), GSH depletion (oxidative stress), lipid accumulation (Oil Red O staining), and phosphotidylserine exposure (apoptosis).
- Transcriptomic profiling: For mechanistic insights, perform RNA sequencing on chip contents to identify toxicity pathways (e.g., oxidative stress, endoplasmic reticulum stress, steatotic pathways).
Industry validation studies, including those by Boehringer Ingelheim and Daiichi Sankyo, have demonstrated the liver-chip's capability for cross-species DILI prediction and comparative liver toxicity assessment, showing superior predictivity compared to conventional hepatocyte models [42].
Case Studies and Validation Data
Bone Marrow Toxicity Assessment
Drug-induced myelosuppression represents a significant dose-limiting toxicity for many chemotherapeutic agents and other drug classes. Traditional assessment relies heavily on animal models, which often poorly predict human hematological toxicity due to species-specific differences in drug metabolism and bone marrow physiology. Researchers from the Wyss Institute at Harvard University developed a Bone Marrow-on-Chip that recapitulates the complex bone marrow architecture by housing hematopoietic progenitor cells and stromal cells within a 3D extracellular matrix adjacent to a perfused vascular channel lined with endothelial cells [41].
Experimental Outcomes:
- The chip accurately recapitulated clinical hematologic toxicities, showing lineage-specific depletion after exposure to chemotherapeutic agents (5-fluorouracil, cisplatin) and radiation at clinically relevant doses.
- When seeded with patient-derived cells from individuals with Shwachman-Diamond syndrome, the chip reproduced hallmark disease features including impaired neutrophil maturation, enabling study of patient-specific pathophysiology.
- The platform maintained multilineage differentiation potential for over four weeks, significantly longer than static cultures, enabling chronic toxicity assessment.
- The system demonstrated utility for personalized risk assessment, showing variable toxicity responses across donor-derived cells that mirrored clinical susceptibility patterns.
This bone marrow surrogate provides an accessible, human-relevant platform for predicting marrow toxicity, studying disease mechanisms, and testing patient-specific treatment regimens—effectively bridging the gap between conventional in vitro models and human clinical outcomes [41].
Multi-Organ Toxicity Assessment
For compounds with potential systemic toxicity, multi-organ MPS platforms enable assessment of inter-organ crosstalk and metabolite-mediated toxicity. Companies including CN Bio and TissUse GmbH have developed interconnected multi-organ systems that model complex physiological interactions [40] [39].
Table 3: Quantitative Performance Data of Organ-on-Chip Platforms in Predictive Toxicology
| Platform/Model | Toxicity Endpoint | Predictive Performance | Reference Compounds Tested | Comparison to Conventional Models |
|---|---|---|---|---|
| Liver-Chip (Emulate) | Drug-induced liver injury (DILI) | 87% concordance with clinical DILI | 27 compounds (12 hepatotoxins, 15 non-hepatotoxins) | Superior to primary hepatocytes (47%) and animal models (53%) [42] |
| Kidney-Chip (UCB) | Antisense oligonucleotide toxicity | Correctly identified 4/4 nephrotoxic compounds | 8 antisense oligonucleotides | Enabled de-risking of novel therapeutic modality [42] |
| Alveolus Lung-Chip (Boehringer Ingelheim) | Antibody drug conjugate (ADC) safety | Identified patient risk factors for ADC toxicity | Multiple ADCs with different warheads | Provided human-specific safety insights not available from animal models [42] |
| Bone Marrow-Chip (Wyss Institute) | Chemotherapy-induced myelosuppression | Reproduced clinical lineage-specific toxicity patterns | 5-fluorouracil, cisplatin, radiation | Recapitulated patient-specific vulnerabilities [41] |
Integrated Liver-Kidney System Protocol:
- Individual organ maturation: Culture liver chips (primary hepatocytes + non-parenchymal cells) and kidney chips (proximal tubule cells) separately for 7 days to establish mature phenotypes.
- System interconnection: Connect liver and kidney chips via microfluidic circulatory network at physiologically relevant flow rates (liver: 100 µL/hour, kidney: 60 µL/hour) using specialized coupling plates.
- Circulatory establishment: Allow 24-48 hours for system stabilization and establishment of metabolic cross-talk.
- Compound administration: Introduce parent compound through the "systemic circulation" at therapeutically relevant concentrations.
- Temporal monitoring: Collect sequential samples from circulatory medium to track parent compound depletion and metabolite formation (via LC-MS).
- Organ-specific assessment: Evaluate liver-specific toxicity (ALT/AST release, CYP inhibition) and kidney-specific toxicity (KIM-1, NGAL release) after 72-96 hours of exposure.
- Mechanistic analysis: Correlate metabolite profiles with tissue-specific injury markers to identify potential mechanisms of inter-organ toxicity.
This approach proved particularly valuable for compounds requiring hepatic activation to toxic metabolites, where single-organ models would fail to detect nephrotoxicity. The system also enabled organ-specific clearance calculations and more accurate prediction of human pharmacokinetic parameters than static culture systems [40].
Implementation Considerations for Drug Discovery Workflows
Integration with Existing Preclinical Pipelines
Successful implementation of OoC technology for predictive toxicity testing requires strategic integration with established drug discovery workflows. Based on industry adoption patterns, the most effective approach involves complementary use with existing models rather than outright replacement [40].
Staged Integration Strategy:
- Tier 1 - Early screening: Implement liver-chip models for lead optimization phase to assess potential hepatotoxicity before animal studies, focusing on compounds with structural alerts or previous toxicity concerns.
- Tier 2 - Mechanistic investigation: Utilize specialized organ chips (kidney, bone marrow, CNS) for compounds showing organ-specific signals in animal studies or for patient populations at particular risk (e.g., renal impairment).
- Tier 3 - Advanced modeling: Employ multi-organ systems for compounds with complex metabolism, suspected metabolite-mediated toxicity, or narrow therapeutic indices.
This tiered approach maximizes resource efficiency while progressively building confidence in OoC-derived data. Companies like Pfizer have successfully implemented this strategy, using a Lymph Node-Chip for predicting antigen-specific immune responses—a major advancement for preclinical immunotoxicity testing [42].
Analytical Methods and Data Integration
The richness of OoC systems necessitates sophisticated analytical approaches to fully leverage their predictive potential. A typical 7-day experiment on platforms like the AVA Emulation System can generate >30,000 time-stamped data points from daily imaging and effluent assays, with post-takedown omics pushing the total into the millions [42]. This data richness provides a multi-modal foundation for machine learning approaches to toxicity prediction.
Essential Analytical Modalities:
- High-content imaging: Automated brightfield and fluorescence microscopy for morphological assessment and cellular health tracking.
- Effluent analysis: Multiplexed biomarker quantification (Luminex, MSD) for organ-specific injury markers.
- Metabolomic profiling: LC-MS based quantification of parent compound depletion and metabolite formation.
- Transcriptomic analysis: RNA sequencing from chip contents for pathway analysis and mechanistic insights.
- Functional assessment: TEER measurements for barrier integrity, enzymatic activity assays for metabolic competence.
The integration of these diverse data streams through computational approaches enables the development of multi-parameter toxicity signatures that show improved predictivity compared to single endpoints. Furthermore, the emergence of standardized data formats and analysis pipelines, as showcased at the 2025 MPS World Summit, is addressing previous challenges in data comparability across platforms and laboratories [42].
Organ-on-Chip technology has transitioned from proof-of-concept demonstrations to robust tools capable of generating human-relevant toxicity data for drug development decisions. The field has reached a critical maturation point, evidenced by the growing adoption by pharmaceutical companies and the inclusion of MPS data in regulatory submissions [42] [40]. As the technology continues to evolve, several trends are shaping its future in predictive toxicology.
The ongoing development of patient-specific models using iPSC-derived cells promises to address inter-individual variability in drug responses and enable toxicity assessment in vulnerable populations [41]. The integration of immune system components into OoC models is expanding the scope of assessable toxicities to include immunotoxicity and immuno-mediated organ injury. Furthermore, advances in instrumentation and automation, exemplified by platforms like the AVA Emulation System and PhysioMimix Core, are addressing throughput limitations that previously restricted widespread industrial adoption [42] [40].
For researchers implementing these systems, success depends on selecting the appropriate platform for specific toxicity questions, implementing robust analytical methods, and strategically integrating OoC data within existing decision frameworks. When properly deployed, Organ-on-Chip technology provides a powerful approach to de-risk drug candidates, reduce late-stage attrition, and ultimately deliver safer therapeutics to patients—positioning MPS as indispensable tools for 21st-century predictive toxicology.
Droplet Microfluidics for Single-Cell Analysis and Digital PCR
Droplet microfluidics has emerged as a breakthrough technology that is revolutionizing single-cell analysis and digital PCR (dPCR), providing powerful tools for high-throughput drug discovery research [44]. By compartmentalizing individual cells or nucleic acid molecules into picoliter to nanoliter droplets, this approach enables unprecedented resolution in studying cellular heterogeneity and absolute quantification of target genes [44] [45]. The technology's capacity to perform millions of parallel experiments in isolated microreactors aligns perfectly with the pharmaceutical industry's need for efficient screening methodologies to reduce drug development costs and timelines [44] [46]. This application note details practical protocols and implementation guidelines for leveraging droplet microfluidics in drug discovery pipelines.
Fundamental Principles of Droplet Microfluidics
Droplet microfluidics utilizes immiscible phases (typically oil and water) to generate monodisperse droplets at rates of hundreds to thousands per second [47]. The technology leverages three primary channel geometries for droplet generation [44] [47]:
- T-Junction: Simple perpendicular intersection where dispersed phase is pinched off by continuous phase shear forces
- Flow Focusing: Dispersed phase is focused and pinched by continuous phase from both sides
- Co-Flow: Concentric arrangement where droplets form due to shear stress along coaxial geometry
The Capillary number (Ca = ηU/σ), representing the ratio of viscous to interfacial forces, governs droplet formation dynamics and must be optimized for stable operation [47].
Comparative Technology Assessment
Table 1: Comparison of Single-Cell Isolation Technologies
| Method | Throughput | Cell Viability | Cost | Automation | Key Applications |
|---|---|---|---|---|---|
| Droplet Microfluidics | Very high (kHz rates) | High (>95%) | Moderate | High | Single-cell omics, antibody screening |
| Fluorescence-Activated Cell Sorting (FACS) | High | Moderate | Very high | Yes | Population sorting, surface protein analysis |
| Microwell Arrays | Moderate | High | Low to moderate | Limited | Cell-cell interactions, secreted factors |
| Laser Capture Microdissection | Low | Variable | High | No | Tissue pathology, spatial omics |
| Manual Micromanipulation | Very low | High | Moderate | No | Rare cell isolation |
Table 2: Digital PCR Platforms and Specifications
| Platform Type | Partition Volume | Partition Number | Absolute Quantification | Detection Limit | Multiplexing Capacity |
|---|---|---|---|---|---|
| Droplet-based dPCR | 0.5-10 nL | 20,000-100,000 | Yes | 0.001% | 2-6 colors |
| Chip-based dPCR | 1-50 nL | 5,000-30,000 | Yes | 0.01% | 2-4 colors |
| Quantitative PCR | 10-50 µL | 1 | No (relative) | 0.1-1% | 4-6 colors |
Application Protocols
Protocol 1: Single-Cell Encapsulation and Viability Screening for Compound Libraries
Objective: High-throughput assessment of compound toxicity and mechanism of action at single-cell resolution.
Materials:
- Microfluidic droplet generator (flow-focusing or T-junction design)
- Biocompatible fluorinated oil (e.g., FluoOil 135) with 1-2% surfactant (e.g., FluoSurf)
- Cell suspension (0.5-2 × 10⁶ cells/mL in appropriate medium)
- Compound library in DMSO (100-500 nL aliquots)
- Fluorescent viability markers (Calcein-AM, propidium iodide, or similar)
Procedure:
Device Preparation:
- Flush channels with surfactant-containing oil phase (30 min, 200 µL)
- Treat channels with Fluo-ST1 for hydrophobic surface modification if needed [47]
- Verify droplet generation stability with buffer solution (5 min)
Cell Preparation:
- Harvest and wash cells 2× with appropriate buffer
- Resuspend at 1 × 10⁶ cells/mL density (optimized for Poisson distribution)
- Add viability markers according to manufacturer specifications
- Keep cells on ice until loading into device
Droplet Generation:
- Load cell suspension into dispersed phase syringe
- Set oil:aqueous flow rate ratio to 3:1 to 5:1 (typical range)
- Adjust absolute flow rates to achieve desired droplet size (20-50 µm diameter)
- Monitor droplet formation stability for 2-3 minutes before collection
Compound Exposure:
- Merge compound-containing droplets with cell-containing droplets using electrofusion or passive merging geometries [47]
- Incubate emulsion at 37°C, 5% CO₂ for designated time (4-72 hours)
- Maintain emulsion stability by adding supplemental surfactant if needed
Analysis:
- Flow droplets through detection channel at 100-1000 droplets/second
- Measure fluorescence emission using 488 nm (viability) and 561 nm (cytotoxicity) lasers
- Sort droplets based on fluorescence criteria using dielectrophoresis or piezoelectric sorting
Troubleshooting:
- Droplet coalescence: Increase surfactant concentration or optimize flow rates
- Low single-cell encapsulation: Adjust cell density using Poisson distribution calculations
- Reduced cell viability: Minimize shear stress by optimizing channel dimensions and flow rates
Protocol 2: Single-Cell RNA Sequencing for Transcriptomic Profiling in Drug Response
Objective: Identify heterogeneous cellular responses to drug candidates through whole-transcriptome analysis.
Materials:
- High-throughput droplet scRNA-seq system (e.g., 10X Genomics)
- Single cell suspension at 100-1,000 cells/µL
- Barcoded beads with oligo-dT primers
- Cell lysis buffer (containing detergent and RNase inhibitors)
- Reverse transcription reagents
- Library preparation kit
Procedure:
Device Setup:
- Use commercial scRNA-seq droplet system or custom flow-focusing design
- Verify three-phase operation: cells, beads, and oil
- Optimize flow rates for single-cell/bead co-encapsulation (typically 3-5 kHz generation rate)
Sample Preparation:
- Prepare single-cell suspension with >90% viability
- Remove cell aggregates through 40 µm filtration
- Count and adjust concentration to target ~10,000 cells/recovery
Droplet Generation and Barcoding:
- Co-encapsulate single cells with barcoded beads and lysis buffer
- Collect emulsion into PCR tubes or microcentrifuge tubes
- Incubate at 53°C for 45 minutes to complete cell lysis and mRNA capture
Reverse Transcription and Library Prep:
- Break droplets using perfluorooctanol or equivalent breaking agent
- Perform reverse transcription directly in broken emulsion
- Purify cDNA using SPRI beads or equivalent magnetic beads
- Amplify cDNA with 10-12 PCR cycles
- Fragment and size-select cDNA for library construction
Sequencing and Analysis:
- Sequence libraries on appropriate Illumina platform
- Process data using Cell Ranger or equivalent pipeline
- Perform differential expression analysis between treatment conditions
Protocol 3: Droplet Digital PCR for Pharmacogenomic Biomarker Quantification
Objective: Absolute quantification of low-frequency genetic variants and copy number variations in drug target genes.
Materials:
- Droplet generator chip or commercial ddPCR system
- Evagreen or TaqMan probe-based ddPCR supermix
- Target-specific primers and probes
- Restriction enzymes (if genomic DNA template)
- Droplet reading instrument or flow cytometer
Procedure:
Reaction Setup:
- Prepare 20 µL PCR mix containing 1× ddPCR supermix, 900 nM primers, 250 nM probe, and 1-100 ng template DNA
- Include no-template controls and positive controls for each assay
- Vortex and centrifuge briefly to mix components
Droplet Generation:
- Load sample into sample well and oil into oil well of droplet generator cartridge
- Generate 20,000-40,000 droplets per sample following manufacturer protocols
- Transfer droplets to 96-well PCR plate using pipette with wide-bore tips
- Seal plate with foil heat seal
Thermal Cycling:
Droplet Reading:
- Load plate into droplet reader
- Measure fluorescence in each droplet using appropriate filter sets
- Set threshold between positive and negative populations using controls
Data Analysis:
- Apply Poisson correction to calculate absolute copy number
- Calculate confidence intervals based on partition number
- For rare variant detection, ensure sufficient partitions for desired sensitivity
Validation:
- Perform replicate measurements (minimum n=3)
- Establish limit of detection and limit of quantification using serial dilutions
- Compare with orthogonal method (e.g., qPCR or NGS) for concordance
Essential Research Reagent Solutions
Table 3: Key Reagents for Droplet Microfluidics Applications
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| Surfactants | FluoSurf-C, FluoSurf-O, PFPE-PEG | Stabilize droplets, prevent coalescence | Critical for thermocycling compatibility in ddPCR |
| Oil Phase | FluoOil 135, FluoOil 200, HFE-7500 | Continuous phase for emulsion formation | Fluorinated oils offer superior oxygen permeability |
| Surface Treatments | Fluo-ST1, Fluo-ST3 | Modify channel wettability | Covalent bonding to PDMS or glass surfaces |
| Barcoded Beads | 10X GemCode, Dolomite beads | Single-cell RNA capture | Oligo-dT primers with cell barcodes |
| Detection Chemistries | Evagreen, TaqMan probes, Molecular Beacons | Fluorescent detection in droplets | Evagreen offers cost-efficiency; TaqMan provides specificity |
Workflow Visualization
Diagram 1: Integrated Workflow for Single-Cell Analysis and Digital PCR in Drug Discovery. This workflow highlights the parallel pathways for cellular and molecular analyses enabled by droplet microfluidics technology.
Diagram 2: Drug Discovery Pipeline Applications. This diagram illustrates how droplet microfluidics technologies integrate across various stages of pharmaceutical development.
Implementation Considerations for Drug Discovery
Integration with Existing Workflows
Successful implementation of droplet microfluidics in drug discovery requires strategic integration with established screening platforms:
- Automation Compatibility: Design droplet systems compatible with liquid handling robots for library screening
- Data Management: Implement robust data analysis pipelines for high-dimensional single-cell data
- Quality Control: Establish routine monitoring of droplet size distribution and encapsulation efficiency
- Scalability: Plan for scale-up from proof-of-concept (100s compounds) to full library screening (100,000s compounds)
Technical Challenges and Solutions
Table 4: Common Technical Challenges and Mitigation Strategies
| Challenge | Impact on Drug Discovery | Solution Approaches |
|---|---|---|
| Droplet coalescence | Data loss, cross-contamination | Optimize surfactant type and concentration [47] |
| Cell viability maintenance | Reduced assay sensitivity | Minimize shear stress, use biocompatible oils [48] |
| Low encapsulation efficiency | Increased reagent costs, reduced throughput | Poisson optimization, active encapsulation methods |
| Multiplexing limitations | Reduced information content per experiment | Spectral barcoding, sequential labeling |
| Data integration complexity | Difficulty translating to clinical decisions | Computational pipelines, machine learning approaches |
Future Perspectives
Droplet microfluidics continues to evolve with emerging trends focusing on increased multiplexing, spatial resolution, and functional readouts. Integration with mass spectrometry for single-cell proteomics and CRISPR screening in complex co-culture models represents the next frontier in drug discovery applications [49]. The development of standardized commercial platforms is making the technology more accessible across the pharmaceutical industry, potentially reducing barriers to adoption for routine screening applications.
As droplet-based approaches become more integrated with organ-on-chip technologies and AI-driven analytics, they are poised to transform early drug discovery by providing unprecedented resolution on compound effects in biologically relevant models. The continued miniaturization and automation of these platforms will further enhance their utility in pharmaceutical research and development pipelines.
Synthesizing Drug Carriers and Nanoparticles using Microfluidic Reactors
The synthesis of nanoparticles (NPs) for drug delivery has garnered significant interest due to their wide-ranging applications in the pharmaceutical industry. Controlling key NP characteristics, such as size, polydispersity, zeta potential, drug release, and encapsulation efficiency, is critical for their performance in biomedical applications [50]. Microfluidic technology, which manipulates small volumes of fluids (microliter to picoliter) within channels less than 1 millimeter wide, offers a superior alternative to conventional bulk synthesis methods [23]. This platform provides unparalleled control over the reaction environment, leading to the production of highly uniform nanomaterials with tunable properties, which are crucial for drug delivery, diagnostics, and catalysis [51].
In the context of high-throughput drug discovery research, microfluidic reactors represent a transformative tool. They facilitate the precise fabrication of advanced drug carriers, including lipid-based nanoparticles, polymeric particles, and inorganic nanoparticles, with enhanced reproducibility and batch-to-batch consistency [51] [52]. Unlike traditional methods, which often lack the resolution to control local reactant concentrations and lead to undesirable polydispersity, microfluidics employs laminar flow to establish stable and predictable flow and concentration profiles [51]. The miniaturized format of these reactors enables high-throughput screening using minimal reagent volumes, making them ideal for synthesizing novel materials from complex or costly precursors [51] [1].
Fundamental Principles and Advantages
Microfluidic synthesis operates on core principles that govern fluid behavior at the microscale. Laminar flow—where fluids move in smooth, parallel layers with low Reynolds number—allows for precise fluid control without turbulence. Mixing occurs primarily through molecular diffusion, while forces like capillarity and electrokinetics can be harnessed for pump-less fluid movement [23]. These principles enable rapid heat and mass transfer due to a high surface-area-to-volume ratio, enhancing reaction kinetics and uniformity [51].
The advantages of microfluidic reactors over conventional bulk methods are substantial:
- Precision and Control: Fine-tuning of flow rates, concentrations, and mixing times allows exact manipulation of NP characteristics like size, morphology, and composition [51] [52].
- Enhanced Reproducibility: Continuous-flow reactors facilitate rapid and homogeneous mixing, significantly improving particle size uniformity and batch-to-batch consistency [51]. This is critical for industrial scale-up and clinical translation, where high batch-to-batch variability is a major bottleneck [52].
- Reduced Consumption: Microfluidic devices operate with small volumes, reducing reagent consumption and waste generation, which is particularly beneficial when using expensive or rare precursors [51] [1].
- High-Throughput Capabilities: Automated and integrated systems can synthesize and screen large NP libraries, accelerating the discovery and optimization of drug carriers [51] [53].
Table 1: Comparison of Nanoparticle Synthesis Methods
| Feature | Conventional Bulk Methods | Microfluidic Reactors |
|---|---|---|
| Mixing Efficiency | Low; relies on turbulent mixing | High; rapid, diffusion-dominated mixing |
| Particle Size Control | Broad size distribution (high polydispersity) | Narrow size distribution (low polydispersity) |
| Batch-to-Batch Reproducibility | Low variability | High reproducibility |
| Reagent Consumption | High volume | Minimal volume (µL to pL) |
| Process Control | Limited control over reaction parameters | Precise control of flow rates, temperature, and mixing |
| Scalability | Easy to scale up, but with quality loss | Challenges in scaling, often via numbering-up |
| Throughput | Low to moderate | High, with parallelization |
Microfluidic Synthesis Platforms and Methods
Microfluidic platforms for NP synthesis are broadly classified into passive and active methods. Passive methods rely solely on channel geometry and fluid dynamics to control reactions, without external energy input. In contrast, active methods utilize external energy sources—such as thermal, electrical, electromagnetic, or acoustic inputs—to enhance mixing and control [50].
Droplet-Based Microfluidics
Droplet-based microfluidics transforms a continuous stream into discrete, picoliter-to-nanoliter droplets, which serve as isolated reaction vessels [51]. Common geometries for droplet generation include T-junction, flow-focusing, and co-flow designs [51]. In this system, an aqueous dispersed phase and an oil-based continuous phase are introduced, generating monodisperse droplets where nanoparticle synthesis can occur. The droplet size and generation frequency are dictated by the flow rate ratios of the phases and the channel geometry [53]. A key advantage is the ability to perform massive numbers of parallel experiments, making it ideal for high-throughput screening of nanoparticle formulations [53].
Diagram 1: Droplet-based synthesis and screening workflow.
Continuous-Flow Microfluidics
Continuous-flow microfluidics involves the constant pumping and mixing of a single-phase stream within microchannels. These systems offer precise control over experimental parameters like flow rates, concentration, and temperature, ensuring consistent material size and morphology [51]. Common mixer geometries include T-shaped, Y-shaped, spiral, and staggered herringbone micromixers (SHM) [51]. While simple T- and Y-shaped designs rely on molecular diffusion and have low mixing efficiency, advanced structures like SHMs induce chaotic advection to enhance mixing, leading to more reproducible synthesis conditions [51]. This method is particularly suited for the high-throughput, continuous production of nanoparticles, such as lipid nanoparticles (LNPs) for drug and gene delivery [51] [52].
Protocols for Synthesizing Key Drug Carriers
Protocol: Synthesis of Lipid Nanoparticles (LNPs)
Lipid-based nanomedicines, including liposomes and solid lipid nanoparticles (SLNs), are among the most widely approved nanomedicines [52]. This protocol describes their synthesis using a staggered herringbone mixer (SHM).
Research Reagent Solutions:
- Lipid Stock Solution: Dissolve phospholipid (e.g., DSPC), cholesterol, and PEG-lipid in ethanol at a defined molar ratio. This is the organic phase.
- Aqueous Buffer Solution: Prepare an aqueous phase, typically a citrate or phosphate buffer at pH 4.0-7.4. For loaded drugs, dissolve the hydrophilic active ingredient in this buffer.
Experimental Procedure:
- Device Priming: Load the syringes containing the organic and aqueous phases into syringe pumps. Connect the syringes to the inlets of the SHM device using PTFE tubing. Prime the device and tubing with the respective solutions to remove air bubbles.
- Setting Flow Rates: Set the syringe pumps to the desired flow rates. The Total Flow Rate (TFR) and Flow Rate Ratio (FRR) are critical. A typical TFR is 0.5-10 mL/min, with an FRR (aqueous-to-organic) of 3:1. These parameters control nanoparticle size and polydispersity.
- Initiation of Synthesis: Start the pumps simultaneously. The solutions meet at the junction and are mixed rapidly within the SHM due to chaotic advection. Nanoparticle self-assembly occurs almost instantaneously.
- Collection: Collect the effluent stream from the outlet in a vial. The resulting suspension contains formed LNPs.
- Post-Processing: Dialyze the collected suspension against a neutral buffer (e.g., PBS, pH 7.4) for 12-24 hours to remove residual ethanol and for buffer exchange. Finally, sterilize the LNP formulation by filtration through a 0.22 µm membrane.
Table 2: Key Parameters for LNP Synthesis in a Staggered Herringbone Mixer
| Parameter | Typical Range | Impact on Critical Quality Attributes (CQAs) |
|---|---|---|
| Total Flow Rate (TFR) | 0.5 - 10 mL/min | Higher TFR generally leads to smaller particle size due to faster mixing. |
| Flow Rate Ratio (FRR - Aqueous:Organic) | 2:1 to 5:1 | A higher aqueous ratio typically results in smaller particles. |
| Total Lipid Concentration | 5 - 25 mM | Affects particle size and encapsulation efficiency; high concentrations may increase viscosity and size. |
| Aqueous Phase pH | 4.0 - 7.4 | Can influence the ionization state of lipids and the encapsulated drug, impacting stability and encapsulation. |
| Mixer Geometry | Staggered Herringbone | Induces chaotic advection for highly efficient mixing, producing uniform particles with low polydispersity. |
Protocol: Synthesis of Polymeric Nanoparticles using Droplet Microfluidics
This protocol details the synthesis of monodisperse polymeric nanoparticles, such as PLGA NPs, using a flow-focusing droplet generator.
Research Reagent Solutions:
- Dispersed Phase: Dissolve the polymer (e.g., PLGA) and a hydrophobic drug in a water-immiscible organic solvent (e.g., dichloromethane, DCM).
- Continuous Phase: Prepare an aqueous surfactant solution (e.g., 1-2% w/v PVA in water) to stabilize the formed droplets.
Experimental Procedure:
- Device Setup: Load the dispersed and continuous phases into separate syringes. Mount the syringes on precision syringe pumps and connect them to the respective inlets of the flow-focusing device.
- Droplet Generation: Set the flow rates. A typical flow rate for the continuous phase is 500-2000 µL/h, and for the dispersed phase, 100-500 µL/h. This will generate a stable stream of monodisperse droplets.
- Solvent Evaporation: Direct the outlet stream containing the droplets into a collection vial. Gently stir the collection vial under a fume hood or apply a mild vacuum to allow the organic solvent to evaporate over several hours. As the solvent diffuses out, the polymer precipitates, forming solid nanoparticles.
- Washing and Concentration: Centrifuge the nanoparticle suspension at high speed (e.g., 20,000 x g for 20 minutes) to pellet the particles. Carefully remove the supernatant and resuspend the pellet in pure water or buffer. Repeat this washing step 2-3 times to remove residual surfactant and unencapsulated drug.
- Characterization: The final nanoparticles can be characterized for size (Dynamic Light Scattering), morphology (Electron Microscopy), and drug loading (HPLC).
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful synthesis relies on a set of key reagents and materials. The table below details essential components for formulating lipid and polymeric nanoparticles.
Table 3: Research Reagent Solutions for Microfluidic Nanoparticle Synthesis
| Reagent/Material | Function | Example Components | Application Notes |
|---|---|---|---|
| Phospholipids | Primary structural lipid for bilayer formation. | DSPC, DPPC, Phosphatidylcholine | Provides membrane integrity and biocompatibility. Select based on phase transition temperature (Tm). |
| Sterols | Modulates membrane fluidity and stability. | Cholesterol | Incorporated into lipid bilayers (e.g., liposomes) to prevent leakage and improve in vivo stability. |
| PEG-Lipids | Confers "stealth" properties to reduce immune clearance. | DMG-PEG, DSPE-PEG | Added in small molar ratios (1-5%) to prolong circulation half-life by reducing opsonization. |
| Surfactants | Stabilizes emulsions and droplets; prevents coalescence. | PVA, Poloxamer 188, Span 80, Tween 80 | Critical for droplet-based synthesis and for stabilizing nanoemulsions. Biocompatibility is key for in vivo use. |
| Biodegradable Polymers | Forms the nanoparticle matrix for controlled drug release. | PLGA, PLA, PEG-PLGA | The choice of polymer and its molecular weight determines drug release kinetics and nanoparticle degradation. |
| Edge Activators | Imparts flexibility and deformability to lipid vesicles. | Sodium cholate, Tween 80, Span 80 | Essential component for creating ultra-deformable Transferosomes for enhanced penetration [52]. |
| Aqueous Buffer | Serves as the hydration medium and controls pH. | Citrate Buffer (pH ~4), Phosphate Buffered Saline (PBS, pH 7.4) | pH can be critical for ionizable lipids (used in mRNA LNPs) and for drug stability/solubility. |
| Organic Solvent | Dissolves hydrophobic materials (polymers, lipids). | Ethanol, Isopropanol, Dichloromethane (DCM) | Must be miscible/immiscible with the aqueous phase depending on the method. Must be removed post-synthesis. |
High-Throughput Screening and Optimization in Drug Discovery
Microfluidic reactors are uniquely positioned to accelerate high-throughput screening (HTS) in drug discovery. They enable the rapid generation and testing of vast libraries of nanoparticle formulations with minimal reagent consumption [7] [53]. A key application is in antibody discovery, where droplet microfluidics can encapsulate single B-cells and assay components in picoliter droplets, allowing for the screening of millions of cells to identify rare, antigen-specific antibodies at kilohertz rates [53].
Furthermore, microfluidic concentration gradient generators (CGGs) are powerful tools for high-throughput drug screening. These devices leverage laminar flow characteristics to create precise, stable concentration gradients of drugs or formulations across a cell culture chamber, enabling rapid assessment of cytotoxicity and therapeutic efficacy [7]. This allows researchers to systematically evaluate optimal concentrations of single drugs or the most effective drug combinations, a crucial step in precision medicine [7].
Diagram 2: High-throughput formulation screening and optimization logic.
Microfluidic reactors have firmly established themselves as a powerful and versatile platform for the synthesis of drug carriers and nanoparticles. Their ability to exert precise control over the reaction environment translates directly into superior products with well-defined Critical Quality Attributes (CQAs), addressing the key limitations of traditional batch synthesis [51] [52]. The integration of these systems into high-throughput drug discovery workflows enables the rapid optimization of nanomedicines, accelerating the path from concept to clinical application.
The future of this field lies in increased automation and intelligence. The convergence of microfluidics with artificial intelligence (AI) and machine learning is creating intelligent platforms capable of self-optimization [50] [51]. AI algorithms can analyze complex datasets from synthesis parameters and performance outcomes to predict optimal formulations and control the process in real-time [51]. Furthermore, the trend toward more robust and scalable fabrication methods, alongside the exploration of sustainable materials, will be critical for overcoming current challenges in industrial adoption [23] [52]. As these innovations mature, microfluidic reactors are poised to become the standard for the on-demand production of personalized nanotherapeutics, fundamentally transforming the landscape of pharmaceutical research and development.
Navigating Practical Challenges: A Guide to Optimizing Device Performance and Reliability
The evolution of microfluidic devices has revolutionized high-throughput drug discovery research, enabling the rapid screening of compounds with minimal reagent use and increased experimental control. The performance of these devices is intrinsically linked to the materials from which they are fabricated. Polydimethylsiloxane (PDMS), various synthetic polymers, and glass represent the most prevalent materials, each offering a distinct set of physicochemical properties that dictate their suitability for specific biological assays. This application note provides a structured comparison of these materials, supplemented with detailed protocols, to guide researchers in selecting the optimal substrate for their microfluidic-based drug discovery pipelines. The choice of material directly influences critical parameters such as biochemical compatibility, optical performance, and manufacturing scalability, all of which are paramount for generating reliable, high-quality data.
Material Properties and Comparative Analysis
Selecting a material requires a fundamental understanding of how its intrinsic properties align with the technical demands of an assay. Below is a comparative analysis of key properties relevant to biological applications.
Table 1: Comparative Properties of PDMS, Polymers, and Glass for Biological Assays
| Property | PDMS | Polymers (e.g., PLA, PMMA) | Glass (e.g., Borosilicate) |
|---|---|---|---|
| Optical Transparency | High (∼90% transmittance 390-780 nm) [54] | Variable (e.g., PMMA: High) | Very High (Excellent across visible-UV) [55] |
| Biocompatibility | High; mild foreign body reaction [54] [56] | Variable (Requires validation; some require surface modification) [55] | High, but stiff implants can cause glial reaction [56] |
| Young's Modulus | 0.36–0.87 MPa (Flexible, hyperelastic) [54] | 1–3 GPa (e.g., PLA: Rigid) [57] | ∼50 GPa (Rigid, brittle) [54] |
| Gas Permeability | High (Ideal for cell culture) [54] | Low to Moderate | Impermeable |
| Surface Hydrophobicity | Hydrophobic (Contact angle ~108°) [54] | Variable | Hydrophilic |
| Protein/Biomolecule Absorption | High (Can absorb small molecules) [54] | Low to Moderate (Material-dependent) | Low |
| Fabrication Complexity | Low (Soft lithography, rapid prototyping) [54] [58] | Moderate (Injection molding, 3D printing) [58] | High (Photolithography, etching) [58] |
| Typical Assay Suitability | Cell culture, organ-on-chip, particle synthesis [54] | Disposable microfluidics, diagnostic cartridges [58] | High-resolution imaging, capillary electrophoresis [56] |
Detailed Material Profiles and Applications
Polydimethylsiloxane (PDMS)
PDMS is a silicone-based elastomer that has become a cornerstone material in academic research for prototyping microfluidic devices, particularly those involving living cells.
- Key Advantages: Its exceptional optical transparency facilitates high-resolution microscopy and real-time observation of biological processes within microchannels [54]. A critical property for cell-based assays is its high gas permeability, which allows for efficient oxygen and carbon dioxide exchange, essential for long-term cell culture and viability within microdevices [54]. Furthermore, its well-established biocompatibility and flexibility make it suitable for creating dynamic environments and interfacing with soft biological tissues [54] [56].
- Key Limitations: The inherent hydrophobicity of PDMS can impede the flow of aqueous solutions and lead to non-specific adsorption of proteins and small molecules, which can skew experimental results in drug discovery assays [54]. While its elasticity is beneficial, it can limit the resolution of high-pressure applications.
Specialty Polymers (PLA, PMMA, and MPC Polymers)
A broad range of synthetic polymers is available, offering a spectrum of properties tailored for specific applications.
- Polylactic Acid (PLA): As a biodegradable polymer, PLA is increasingly used to fabricate scaffolds in tissue engineering and for environmentally conscious, disposable devices. Its biodegradability can be tuned through copolymerization, for instance, by introducing thionoester linkages to enhance its degradation profile [59].
- PMMA and Resins: Polymers like PMMA are prized for their excellent optical clarity and are often used in commercial diagnostic devices. Recent advances have utilized consumer-grade 3D printing resins in maskless photolithography to create masters for PDMS molding, significantly reducing the cost and iteration time for microfabrication [58].
- Bioinspired Polymers: Polymers like poly(2-methacryloyloxyethyl phosphorylcholine) (MPC) are engineered to mimic the outer surface of cell membranes. These polymers dramatically suppress protein adsorption and cell adhesion, making them exceptionally useful for creating anti-fouling surfaces in diagnostic devices and implants that contact blood [59].
Glass
Glass remains the gold standard for applications requiring ultimate precision and chemical inertness.
- Key Advantages: Its superior optical transparency and low autofluorescence make it the material of choice for high-resolution imaging techniques like Total Internal Reflection Fluorescence (TIRF) microscopy. Its chemical inertness and low biomolecule adsorption prevent experimental artifacts in sensitive biochemical assays, and its high rigidity allows for the fabrication of precise, stable channel geometries [56].
- Key Limitations: The primary drawback of glass in biological interfaces is its high stiffness and density, which can trigger significant glial activation and tissue response when implanted, as demonstrated by its comparison to softer PDMS fibers [56]. The fabrication of glass microdevices is also complex, time-consuming, and requires specialized equipment, making rapid prototyping challenging [58].
Experimental Protocols
Protocol: Rapid Prototyping of a PDMS Microfluidic Device via Soft Lithography
This protocol outlines the creation of a master mold using a cost-effective maskless photolithography technique and subsequent replication in PDMS for cell culture applications [58].
The Scientist's Toolkit: Key Reagents and Equipment
| Item | Function/Explanation |
|---|---|
| Sylgard 184 Kit | Two-part PDMS elastomer; the standard material for soft lithography due to its optical and mechanical properties [58]. |
| TMSPMA | Adhesion promoter; a silane applied to glass slides to ensure UV resin adheres during mold fabrication [58]. |
| Consumer UV Resin | A low-cost alternative to SU-8 photoresist for creating the master mold [58]. |
| Spin Coater | Instrument used to spread resin into a thin, uniform film on a slide, controlling feature height [58]. |
| Microscope with DMD | A fluorescence microscope with a Digital Micromirror Device repurposed for maskless UV pattern projection [58]. |
| Oxygen Plasma Cleaner | Treats the surface of cured PDMS to make it permanently hydrophilic for improved aqueous flow [54]. |
Procedure
- Master Mold Fabrication:
- Clean a standard glass microscope slide and coat it with TMSPMA to promote resin adhesion.
- Spin-coat a layer of UV-curable resin onto the slide. The rotational speed (RPM) determines the final thickness of the features. A calibration print is recommended to establish the RPM-height relationship.
- Place the coated slide on the microscope stage of a DMD-equipped system. Project the UV light pattern (e.g., a channel network design) onto the resin for the required exposure time to cure the pattern.
- Develop the mold by washing away the uncured resin with isopropanol, leaving behind the cured microstructures. The resulting mold can be reused numerous times.
PDMS Replica Molding:
- Mix the PDMS base and curing agent from the Sylgard 184 kit at a 10:1 (w/w) ratio. Degas the mixture under vacuum to remove bubbles.
- Pour the PDMS over the master mold and cure it in an oven at 70°C for at least 2 hours.
- Once cured, peel off the PDMS replica from the master mold. Use a biopsy punch to create inlet and outlet ports.
Device Bonding and Surface Treatment:
- Treat the PDMS slab and a clean glass slide (or another PDMS slab) in an oxygen plasma cleaner. Immediately bring the activated surfaces into contact to form an irreversible seal.
- To mitigate hydrophobicity, the channels can be rendered permanently hydrophilic through this plasma treatment or by using physisorption techniques like layer-by-layer deposition of polymers [54].
Protocol: Surface Modification of PDMS for Reduced Protein Adsorption
The hydrophobic PDMS surface readily adsorbs proteins, which can be detrimental to many biological assays. This protocol describes a simple physisorption method to create a protein-resistant surface [54].
Procedure
- Prepare a 1 mg/mL solution of a bioinspired polymer like poly(2-methacryloyloxyethyl phosphorylcholine) (MPC) in a buffer such as phosphate-buffered saline (PBS) [59].
- After oxygen plasma treatment of the PDMS device (which temporarily makes it hydrophilic), immediately flush the channels with the MPC polymer solution.
- Incubate the device at room temperature for 1-2 hours to allow the polymer to adsorb onto the surface.
- Rinse the channels thoroughly with PBS or deionized water to remove any unbound polymer. The modified surface will now exhibit significantly reduced non-specific protein adsorption.
Protocol: Assessing Biocompatibility via In Vitro Cell Assay
Evaluating the cytotoxicity of a material or its extracts is a critical step in validating its use for biological assays. This protocol utilizes the MTT assay, a common colorimetric method for assessing cell metabolic activity [55].
Procedure
- Material Extraction: Sterilize the material (e.g., a piece of PDMS, polymer, or glass) under UV light. Immerse it in a cell culture medium (e.g., DMEM) at a standard surface-area-to-volume ratio (e.g., 3 cm²/mL). Incubate at 37°C for 24 hours to create a conditioned extract.
- Cell Seeding: Seed a relevant cell line (e.g., NIH/3T3 fibroblasts) in a 96-well plate at a density that will reach 80% confluency and allow them to adhere overnight.
- Exposure and Incubation: Replace the culture medium in the test wells with the material-conditioned extract. Include control wells with fresh medium and wells with a known cytotoxic agent as a positive control. Incubate the plate for 24-48 hours.
- MTT Assay: Add MTT reagent to each well and incubate for 2-4 hours. Living cells with active metabolism will reduce the yellow MTT to purple formazan crystals.
- Solubilization and Measurement: Carefully remove the medium, dissolve the formazan crystals in a solvent like DMSO, and measure the absorbance at 570 nm using a plate reader. The cell viability is expressed as a percentage of the absorbance in the control wells.
The following decision workflow synthesizes the key selection criteria to guide researchers in choosing the most appropriate material for their specific biological assay within a drug discovery context.
Figure 1: A decision workflow for selecting materials for biological assays. This chart guides users through key questions based on their primary experimental requirements, leading to a material recommendation.
There is no single "best" material for all biological assays; the optimal choice is a deliberate compromise based on the specific demands of the experiment. PDMS is unparalleled for rapid prototyping and applications requiring gas-permeable, flexible devices for cell culture. Glass provides unmatched chemical stability and optical performance for sensitive biochemical assays and high-resolution imaging. The diverse class of synthetic polymers offers scalable, cost-effective solutions for disposable diagnostics and can be engineered with specialized properties, such as biodegradability or extreme anti-fouling characteristics. By applying the comparative data, protocols, and the selection workflow provided, researchers can make informed decisions to enhance the reliability and throughput of their microfluidic-based drug discovery research.
The transition from prototype to mass-produced microfluidic devices represents a critical pathway in advancing high-throughput drug discovery research. While academic laboratories have successfully utilized versatile prototyping methods for novel device development, these approaches often face significant challenges when scaled for industrial applications requiring thousands of identical, reliable chips. The divergence between fabrication needs for initial research versus commercial production necessitates a thorough understanding of available technologies, their limitations, and appropriate implementation protocols. This application note examines the current state of microfluidic fabrication, providing structured comparisons and detailed methodologies to guide researchers and development professionals in selecting and optimizing manufacturing approaches for drug screening applications.
Comparative Analysis of Fabrication Technologies
The selection of appropriate fabrication methodologies requires careful consideration of technical specifications, material properties, and scalability requirements. The table below provides a quantitative comparison of primary fabrication technologies used in microfluidic device production.
Table 1: Technical Comparison of Microfluidic Fabrication Methods
| Fabrication Method | Resolution (μm) | Throughput | Common Materials | Capital Cost | Relative Cost per Device | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|---|---|
| Soft Lithography (PDMS) | 1-100 [9] [60] | Low-medium | PDMS, Sylgard 184 [9] [60] | Low | Medium | Excellent biocompatibility, gas permeability, optical clarity [9] [60] | Limited scalability, manual process, hydrophobic recovery [9] [60] |
| Stereolithography (SLA) | 10-200 [61] [60] | Medium | Photopolymer resins [61] [60] | Medium | Low-medium | High complexity geometries, fast prototyping [60] | Limited material options, potential biocompatibility concerns [60] |
| Injection Molding | 10-500 [60] | High | Thermoplastics (PMMA, PS, COC, PC) [9] [62] [60] | High | Very low (at volume) | Excellent for mass production, high reproducibility [62] [60] | High initial tooling cost, limited design flexibility [60] |
| Laser Micromachining | 10-500 [63] | Medium | Polymers, glass [63] | Medium-high | Medium | No masks required, suitable for thermoplastics [63] | Tapered channel profiles, thermal damage potential [63] |
Experimental Protocols
Protocol: Standard PDMS Soft Lithography for Prototyping
This protocol details the creation of microfluidic devices using PDMS soft lithography, the predominant method for academic prototyping [9] [60]. The process generates devices suitable for a wide range of drug screening applications, including organ-on-chip systems and high-throughput screening platforms [9] [10].
Materials and Equipment:
- SU-8 photoresist (e.g., SU-8 2050 or 2075)
- Silicon wafers (4-inch diameter, prime grade)
- PDMS elastomer kit (Sylgard 184, Dow Corning)
- Plasma treatment system (e.g., Harrick Plasma Cleaner)
- Spin coater
- UV exposure system with appropriate photomask
- Hotplate or oven (65-70°C)
- Desiccator
- Scotch tape
- Acetone and isopropanol for cleaning
- Curing oven (65-70°C)
Procedure:
Master Mold Fabrication
- Clean silicon wafer with acetone and isopropanol, followed by oxygen plasma treatment (100 W, 1 minute).
- Dehydrate wafer on hotplate at 150°C for 5-10 minutes.
- Pour SU-8 photoresist onto wafer center and spin coat using parameters appropriate for desired channel height (e.g., 1000 rpm for 30 seconds for ~100 μm height).
- Perform soft bake on hotplate according to SU-8 manufacturer specifications (typically 65°C for 3 minutes, then 95°C for 6-10 minutes).
- Expose photoresist to UV light through photomask with desired channel patterns using appropriate exposure dose (typically 150-400 mJ/cm²).
- Perform post-exposure bake on hotplate (65°C for 1-2 minutes, then 95°C for 3-7 minutes).
- Develop in SU-8 developer with gentle agitation until features are fully developed (2-6 minutes).
- Rinse with fresh developer and isopropanol, then hard bake at 150°C for 10-15 minutes.
- Silanize master mold with vaporized tridecafluoro-1,1,2,2-tetrahydrooctyl-trichlorosilane in desiccator for 1 hour to prevent PDMS adhesion.
PDMS Device Fabrication
- Mix PDMS base and curing agent at 10:1 ratio by weight and stir thoroughly.
- Degas mixture in desiccator until all bubbles are removed (approximately 30 minutes).
- Pour PDMS over master mold to desired thickness (typically 3-5 mm).
- Cure at 65-70°C for at least 4 hours (or 2 hours at 85°C).
- Carefully peel cured PDMS from master mold.
- Cut individual devices and punch inlets/outlets using biopsy punches (typically 0.5-1.5 mm diameter).
- Clean PDMS and glass slide with oxygen plasma (100 W, 45 seconds).
- Immediately bring activated surfaces into contact to form irreversible bond.
- Anneal bonded devices at 65-70°C for 10-15 minutes to strengthen bond.
Surface Treatment (Optional)
- For enhanced cell adhesion, treat PDMS channels with oxygen plasma followed by incubation with extracellular matrix proteins (e.g., fibronectin at 10 μg/mL for 1 hour at 37°C) [9].
- For reduced hydrophobic recovery, extract unreacted oligomers by soaking in cyclohexane for 1 hour prior to plasma treatment [9].
Troubleshooting Tips:
- Incomplete bonding: Ensure plasma chamber is clean and humidity is controlled; use fresh plasma-treated surfaces.
- Channel collapse: Optimize PDMS thickness (≥3 mm) and aspect ratio (width:height < 10:1) for critical structures.
- Bubble formation: Degas PDMS thoroughly before curing; prime channels with ethanol before introducing aqueous solutions.
Protocol: Validation of Microfluidic Device for Concentration Gradient Generation
This protocol validates the performance of fabricated microfluidic devices for drug screening applications by assessing their ability to generate precise concentration gradients, a critical requirement for high-throughput drug screening [7] [64].
Materials and Equipment:
- Fabricated microfluidic device
- Syringe pumps with precise flow rate control
- Fluorescent dyes (e.g., FITC-dextran, 70 kDa)
- Phosphate Buffered Saline (PBS)
- Inverted fluorescence microscope with camera
- Image analysis software (e.g., ImageJ, MATLAB)
Procedure:
Device Preparation and Priming
- Connect device inlets to syringe pumps via tubing.
- Prime all channels with PBS to remove air bubbles and ensure complete wetting.
- Prepare two solutions: (1) PBS only and (2) PBS with fluorescent dye at known concentration (e.g., 10 μM FITC-dextran).
Gradient Generation and Imaging
- Load solutions into separate syringes and mount on syringe pumps.
- Set flow rates to achieve desired residence time (typically 0.5-5 μL/min per inlet).
- Initiate flow simultaneously from all inlets.
- Allow system to stabilize for approximately 30 seconds [7].
- Capture fluorescence images at multiple locations along the gradient channel using consistent exposure settings.
- Repeat for at least three different flow rates to verify flow-independent performance.
Data Analysis and Validation
- Quantify fluorescence intensity across the gradient width using image analysis software.
- Normalize intensities to maximum and minimum values from control channels.
- Compare experimental gradient profiles to theoretical predictions based on device design.
- Calculate coefficient of variation (CV) between replicates to assess reproducibility (target CV < 5%).
- For drug screening applications, validate with actual drug solutions and confirm biological response correlates with expected concentration profile.
Validation Parameters:
- Gradient linearity: R² > 0.95 for linear gradients
- Reproducibility: CV < 5% between replicates
- Stability: <5% intensity fluctuation over 30 minutes of operation
- Biological correlation: IC₅₀ values within 2.5% of traditional methods [7]
Fabrication Workflow and Decision Pathway
The following diagram illustrates the key decision points and workflow for selecting appropriate fabrication methods based on research and production requirements:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of microfluidic fabrication requires specific materials and reagents optimized for each manufacturing approach. The table below details essential solutions for microfluidic device fabrication and application in drug discovery research.
Table 2: Essential Research Reagents for Microfluidic Fabrication and Applications
| Reagent/Material | Function/Application | Key Considerations | Example Suppliers |
|---|---|---|---|
| PDMS (Sylgard 184) | Elastomer for soft lithography; biocompatible, gas permeable devices [9] [60] | Base:curing agent ratio affects mechanical properties; requires surface treatment for hydrophilic applications [9] | Dow Corning, Ellsworth Adhesives |
| SU-8 Photoresist | Negative photoresist for creating high-aspect-ratio master molds [60] | Viscosity determines feature height; requires optimized exposure and development protocols [60] | Kayaku Advanced Materials, Gersteltec |
| Trichloro(1H,1H,2H,2H-perfluorooctyl)silane | Mold surface treatment to prevent PDMS adhesion during demolding [60] | Apply via vapor deposition in desiccator; handle in fume hood due to toxicity | Sigma-Aldrich, Fisher Scientific |
| Extracellular Matrix Proteins (Fibronectin, Collagen) | Surface functionalization for enhanced cell adhesion in biological assays [9] | Coating concentration and time affect cell attachment and function; validate for specific cell types [9] | Corning, Thermo Fisher Scientific |
| Photopolymer Resins | Materials for SLA/DLP 3D printing of microfluidic devices [61] [60] | Select based on biocompatibility, transparency, and resolution requirements; may require post-curing [61] [60] | Formlabs, B9Creations, BEGO |
| Thermoplastic Polymers (PMMA, COC, PS) | Rigid substrates for injection molding and mass production [9] [62] | Selected for optical clarity, chemical resistance, and biocompatibility; may require surface modification [9] | Tekni-Plex, Sigma-Aldrich, TOPAS |
The successful transition of microfluidic devices from research prototypes to mass-produced platforms for high-throughput drug discovery requires careful navigation of fabrication hurdles. While PDMS-based soft lithography remains the gold standard for prototyping due to its exceptional biocompatibility and handling properties, emerging technologies including advanced 3D printing and high-throughput injection molding offer compelling pathways to industrialization. By understanding the capabilities, limitations, and appropriate applications of each fabrication method, researchers and development professionals can effectively bridge the gap between innovative device concepts and robust, scalable production systems. The continued advancement of these fabrication technologies promises to accelerate drug discovery pipelines through more physiologically relevant screening platforms and enhanced experimental throughput.
Polydimethylsiloxane (PDMS) remains a dominant material in academic microfluidics and high-throughput drug discovery research due to its exceptional optical transparency, gas permeability, biocompatibility, and ease of prototyping [65] [66]. These properties make it particularly valuable for organ-on-a-chip (OoC) platforms and high-throughput screening systems that require real-time imaging and physiological gas exchange [65] [67]. However, its inherent material characteristics—specifically, uncontrolled gas permeability, absorption of small hydrophobic molecules, and potential for autofluorescence—pose significant challenges for quantitative bioassays and drug discovery applications [65] [67] [66]. This application note details these limitations within drug discovery workflows and provides validated protocols to mitigate them, ensuring data reliability and reproducibility.
The Gas Permeability Challenge
The Dual Nature of Gas Permeability
PDMS is highly permeable to gases like oxygen (O₂) and carbon dioxide (CO₂) [66]. This property is crucial for maintaining cell viability in prolonged cultures within OoC devices by allowing passive gas exchange [65] [67]. However, this same permeability becomes a significant drawback for applications requiring precise control over the dissolved gas concentrations in the culture medium.
Uncontrolled permeation can lead to:
- Evaporation of water vapor: This alters medium osmolarity and concentrate solutes, potentially stressing cells and invalidating drug response data [66].
- Oxygen gradients: In devices with high cell density or metabolic activity, oxygen diffusion through PDMS can create unintended gradients, affecting cellular phenotypes and drug sensitivities [65].
Table 1: Quantitative Permeability of PDMS to Various Gases
| Gas | Permeability (Barrer) | Impact on Drug Discovery Assays |
|---|---|---|
| O₂ (Oxygen) | ~500-600 [65] | Alters cellular metabolic activity, hypoxia responses, and drug efficacy. |
| CO₂ (Carbon Dioxide) | ~2,700-3,200 [65] | Disrupts medium pH balance, affecting cell health and enzyme function. |
| H₂O (Water Vapor) | High [66] | Evaporation increases osmolarity, stressing cells and skewing assay results. |
Experimental Protocol: Quantifying Evaporation in a Microfluidic Culture System
This protocol measures medium evaporation rates in a PDMS device to correct for osmolarity shifts.
Workflow Overview:
Materials:
- PDMS devices (Sylgard 184, 10:1 base:curing agent ratio)
- Analytical balance (accuracy ±0.1 mg)
- Humidified CO₂ incubator (set to 37°C, 5% CO₂)
- Culture medium or ultrapure water
Procedure:
- Device Preparation: Fabricate and sterilize PDMS devices. Bond to a glass substrate and ensure all inlets/outlets are sealed with tape or plugs.
- Baseline Weight: Weigh the empty, dry device (W_device).
- Device Filling: Completely fill the device's microchannels with the test fluid (culture medium or water) using a syringe, avoiding bubbles. Wipe away any fluid on the external surfaces.
- Initial Weight: Weigh the filled device immediately (W_initial).
- Incubation and Monitoring: Place the device on a tray inside the pre-equilibrated incubator. If possible, place the entire tray on an analytical balance inside the incubator for continuous monitoring. Otherwise, remove the device briefly at predetermined time points (e.g., 6, 12, 24, 48 hours), weigh it (W_t), and return it promptly.
- Data Analysis: Calculate the fluid loss over time. The evaporation rate (µL/h) can be derived from the mass loss, assuming a fluid density of ~1 g/mL.
Mitigation Strategies:
- Humidified Enclosures: Place the entire microfluidic system within a custom-built, humidified chamber to minimize the vapor pressure gradient.
- Medium Overlays: For reservoir-based systems, add a layer of sterile, immiscible oil (e.g., mineral oil) over the medium to create a physical vapor barrier.
- Alternative Materials: For assays highly sensitive to osmolarity, consider using alternative, less permeable thermoplastics like cycle olefin polymer (COP) for critical components [7].
The Small Molecule Absorption Problem
Impact on Drug Pharmacokinetics and Assay Reliability
The porous, hydrophobic nature of PDMS causes it to absorb small, hydrophobic molecules from the medium [65] [67] [66]. In drug discovery, this non-specific absorption leads to:
- Unintended drug dosing: The effective concentration of a drug exposed to cells decreases unpredictably over time, invalidating IC₅₀ and EC₅₀ calculations [7] [67].
- Analytical interference: Absorption of fluorescent dyes or reporter molecules quenches signals, leading to false negatives in high-throughput screening [66].
Table 2: Absorption of Common Drug Classes into PDMS
| Drug Molecule/Class | Log P | Reported Absorption | Suggested Correction Method |
|---|---|---|---|
| Small Hydrophobic Drugs | >2 | High absorption, rapid concentration loss [67]. | Lipophilic coating (e.g., Silicone-PEG). |
| Proteins/Peptides | N/A (Hydrophilic) | Low absorption, minimal impact [66]. | Plasma treatment for sustained hydrophilicity. |
| Fluorescent Dyes | Varies | Significant absorption quenches signal [66]. | Pre-saturate device or use alternative materials. |
Experimental Protocol: Characterizing Small Molecule Absorption
This protocol quantifies the absorption kinetics of a fluorescent model drug (e.g., Rhodamine B) into PDMS.
Workflow Overview:
Materials:
- PDMS microchannels (standard 10:1 ratio)
- Model drug solution (e.g., 10 µM Rhodamine B in PBS)
- Fluorescence plate reader or microspectrophotometer
- Syringe pump for precise flow control
Procedure:
- Device Preparation: Fabricate simple PDMS microchannels bonded to glass.
- Pre-saturation (Optional): To distinguish between surface adsorption and bulk absorption, pre-saturate the PDMS by flowing a high-concentration dye solution (e.g., 100 µM Rhodamine B) for several hours, followed by extensive washing with PBS until the effluent is clear.
- Absorption Experiment: Load the model drug solution into the device using a syringe pump at a very low flow rate (e.g., 0.5 µL/min) to ensure sufficient residence time for absorption. Collect the effluent at regular time intervals (e.g., every 5 minutes for 1 hour) into a 96-well plate.
- Concentration Measurement: Measure the fluorescence intensity of each collected sample using a plate reader. Compare these values to the intensity of the initial input solution and a control experiment run in a glass capillary or a COP device [7].
- Data Analysis: Plot the normalized effluent concentration (C/C₀) over time. Fit the data to a first-order exponential decay model to determine the absorption time constant.
Mitigation Strategies:
- Surface Coatings:
- Lipophilic Coatings: Treat the PDMS surface with proprietary lipophilic coatings to create a barrier that prevents absorption [67].
- Silicone-PEG Copolymers: Modify PDMS with PDMS-PEG block copolymers to decrease nonspecific adsorption while maintaining biocompatibility [67].
- Protein Passivation: Pre-incubate channels with bovine serum albumin (BSA) or serum to passivate absorption sites (note: this may be temporary).
- Material Selection: For critical dose-response assays, use glass or Norland Optical Adhesive (NOA) chips, which exhibit significantly lower absorption [68] [67]. NOA has a high Young's modulus (~1.7 GPa) and lower compliance, making it suitable for high-pressure applications [68].
Autofluorescence and Optical Interference
Impact on Sensitive Detection Modalities
While PDMS has low autofluorescence in the visible spectrum, it can exhibit significant background noise in ultraviolet (UV) and blue light excitation ranges [66]. This autofluorescence interferes with common fluorescent dyes like DAPI, FITC, and GFP, leading to a reduced signal-to-noise ratio. This is particularly detrimental in high-throughput drug screening that relies on sensitive detection of weak fluorescent signals from single cells or low-abundance biomarkers [67].
Experimental Protocol: Mapping PDMS Autofluorescence Profile
This protocol characterizes the autofluorescence signature of a PDMS device to identify optimal imaging wavelengths.
Materials:
- Cured PDMS samples (with varying base-to-crosslinker ratios)
- Confocal or fluorescence microscope
- Standard set of fluorescence filter cubes (DAPI, FITC, TRITC, Cy5)
Procedure:
- Sample Preparation: Prepare thin PDMS slabs (e.g., ~1 mm thick) using the standard fabrication protocol. Ensure samples are clean and free of dust.
- Background Imaging: Place a PDMS sample on the microscope. Without adding any fluorescent dyes, acquire images using each standard filter cube set (DAPI, FITC, TRITC, Cy5). Use identical exposure times, gain, and laser power/intensity settings for all samples to allow direct comparison.
- Signal Quantification: Measure the average pixel intensity within a defined region of interest (ROI) in each channel. This value represents the autofluorescence background.
- Threshold Setting: For each channel, set a detection threshold that is at least 3 standard deviations above the mean autofluorescence background intensity.
Mitigation Strategies:
- Spectral Shifting: Design assays using fluorophores with excitation/emission spectra in the red and far-red regions (e.g., Cy5, Cy7), where PDMS autofluorescence is minimal.
- Optical Clearing: If UV excitation is unavoidable, use optical clearing methods or select PDMS types (like PDMS RTV-615) known for lower autofluorescence [66].
- Image Processing: Employ background subtraction algorithms during image analysis, using the baseline autofluorescence values obtained from this protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Mitigating PDMS Limitations
| Reagent/Material | Function/Benefit | Example Use Case |
|---|---|---|
| Sylgard 184 | Standard PDMS elastomer; tunable mechanical properties by adjusting base:crosslinker ratio [66]. | General prototyping of OoC and microfluidic devices. |
| Norland Optical Adhesive (NOA) | Rigid, low-compliance optical adhesive; alternative to PDMS with low molecule absorption [68]. | Fabricating devices for precise pharmacokinetic studies. |
| Cycle Olefin Polymer (COP) | Thermoplastic with high chemical resistance, low autofluorescence, and low water absorption [7]. | High-throughput drug screening requiring high signal-to-noise ratio. |
| Trichloro(1H,1H,2H,2H-perfluorooctyl)silane (PFOTS) | Silanizing agent used to create release layers on molds for easy PDMS demolding [68]. | Fabrication of complex 3D PDMS structures from 3D-printed molds. |
| PEG-based Silicone Copolymers | Surface modification agent; reduces absorption of hydrophobic molecules [67]. | Coating PDMS channels for accurate small molecule drug dosing assays. |
| Lipophilic Coating Reagents | Commercial coatings that create a barrier to prevent small molecule absorption into PDMS [67]. | Pretreating OoC devices before introducing expensive drug candidates. |
PDMS continues to be an invaluable material for microfluidic-based high-throughput drug discovery. By understanding its limitations—gas permeability, small molecule absorption, and autofluorescence—and implementing the detailed characterization and mitigation protocols outlined in this application note, researchers can significantly enhance the reliability and quantitative accuracy of their data. Strategic material selection, combined with surface engineering and rigorous experimental controls, allows for the continued exploitation of PDMS's benefits while minimizing its drawbacks, thereby accelerating robust drug discovery pipelines.
Robust fluid control is a foundational requirement for achieving reliable and reproducible results in high-throughput drug discovery research using microfluidic devices. Clogging and bubble formation represent two of the most pervasive challenges in microfluidic systems, capable of compromising experimental integrity, disrupting automated screening workflows, and yielding misleading data in critical assays ranging from single-cell analysis to organoid-based drug screening [69] [70]. These issues become particularly detrimental in long-term, unattended experiments common in pharmaceutical development pipelines, where system failures can result in substantial losses of time and valuable biological samples [71].
This application note provides a structured framework for understanding, preventing, and addressing clogging and bubble formation within microfluidic systems tailored for drug discovery applications. By integrating foundational principles with practical protocols and quantitative comparisons, we equip researchers with the methodologies necessary to maintain fluidic integrity throughout their experimental workflows, thereby enhancing the reliability of data generated for target validation, lead optimization, and preclinical assessment.
Understanding the Challenges
Clogging: Origins and Impacts
Clogging in microfluidic channels occurs when particulates, cell aggregates, or precipitates obstruct the flow path, leading to increased fluidic resistance, pressure fluctuations, and ultimately, complete flow cessation. In drug discovery contexts, clogs can arise from multiple sources:
- Cell Debris and Aggregates: During single-cell analysis or perfusion cultures, cells entering inlet channels or shedding debris can accumulate at constrictions [69].
- Protein Precipitation: Certain drug compounds or biological reagents may precipitate under specific buffer conditions, forming crystalline structures that block channels [4].
- Matrix Materials: Hydrogels like Matrigel, used for 3D cell culture and organoid models, can prematurely polymerize and adhere to channel walls if not handled with precise temperature control [71].
The consequences of clogging extend beyond simple flow interruption. In systems employing syringe pumps, which deliver a fixed flow rate, a partial clog causes a significant pressure increase within the chip, potentially leading to device failure or delamination [70]. Furthermore, clogging creates unpredictable flow patterns that undermine the quantitative nature of drug response assays, particularly in systems testing combinatorial drug treatments or temporal sequences where precise concentration control is paramount [71].
Bubble Formation: Mechanisms and Consequences
Bubble formation represents an equally formidable challenge in microfluidic systems, with origins ranging from fluid switching and temperature fluctuations to the permeation of gases through porous device materials like PDMS [70]. The issues caused by bubbles can be categorized as follows:
- Flow Instability: Bubbles moving within fluidic pathways or undergoing expansion/contraction in response to pressure changes introduce significant flow rate instability, compromising the delivery of precise drug concentrations [70].
- Increased Compliance: Trapped air bubbles act as compressible volumes that absorb pressure changes, increasing the time required for the system to reach pressure equilibrium and degrading fluidic responsiveness—a critical parameter in dynamic stimulation experiments [70].
- Experimental Interference: The air-liquid interface of bubbles presents interfacial tension that can apply shear stress to cells, induce protein aggregation, and even damage chemical surface functionalizations essential for specific assay types [70]. In organoid culture systems, bubbles can disrupt the surrounding extracellular matrix and impair normal growth and development [71].
Prevention Strategies and System Design
A proactive approach to fluid control begins with strategic system design and the implementation of preventive measures tailored to the specific application.
Microfluidic Chip Design
The architecture of the microfluidic device itself plays a crucial role in mitigating clogging and bubble accumulation. Design considerations include:
- Acute Angle Avoidance: Channel geometries featuring sudden expansions or acute angles promote bubble trapping and create stagnation points where cells and particulates can accumulate. Implementing gradual transitions with rounded corners facilitates smooth fluid flow and reduces adhesion sites [70].
- Cultivation Chamber Optimization: For cell-based assays, the dimensions of cultivation chambers and supply channels must be carefully balanced. Channels should be sufficiently wide to prevent clogging during cell loading, while chamber heights may be designed to physically constrain cells without causing damage [69]. For organoid cultures, which can reach diameters of 500 μm, chamber heights must accommodate this size while maintaining adequate nutrient supply [71].
- Bubble-Trapping Structures: Incorporating dedicated architectural features, such as bypass channels or hydrophobic vents, can strategically isolate and remove bubbles before they enter critical regions of the device [70].
Fluidic Path Preparation and Maintenance
Proper preparation of the fluidic path significantly reduces the incidence of both clogging and bubble formation:
- Liquid Degassing: Degassing buffers and culture media prior to introduction into the microfluidic system removes dissolved gases that would otherwise nucleate into bubbles, particularly when solutions are heated to physiological temperatures during experiments [70].
- Surface Passivation: Treating channel walls with surface-active agents like Pluronic or bovine serum albumin (BSA) can reduce non-specific adsorption of cells, proteins, and drug molecules that might otherwise initiate clogging [69].
- Leak Prevention: Ensuring leak-free connections throughout the fluidic path is fundamental. Using Teflon tape on threaded fittings and regularly inspecting seals prevents air ingress, a common source of bubble introduction [70].
Table 1: Comparative Analysis of Preventive Measures for Clogging and Bubble Formation
| Preventive Measure | Implementation Complexity | Effectiveness Against Clogging | Effectiveness Against Bubbles | Key Applications in Drug Discovery |
|---|---|---|---|---|
| Chip Design Optimization | High | High | Medium | Long-term organoid culture, single-cell analysis |
| Liquid Degassing | Low | Low | High | All perfusion-based systems, temperature-sensitive assays |
| Surface Passivation | Medium | High | Low | Protein crystallization, ligand-binding studies |
| Injection Loops | Medium | Medium | High | High-throughput compound screening, sequential drug addition |
| Leak-Free Fittings | Low | Low | High | All pressure-driven systems, prolonged experiments |
Experimental Protocols
Protocol for Degassing and Priming Microfluidic Systems
Purpose: To remove dissolved gases from aqueous solutions and establish a bubble-free fluidic path prior to experimental operation.
Materials:
- Vacuum desiccator or chamber
- Vacuum pump
- Source of heat (e.g., water bath)
- Pressure-based flow controller or syringe pump
- Microfluidic device and associated tubing
- Degassed buffer (e.g., phosphate-buffered saline, culture medium)
Procedure:
- Solution Degassing: Place the buffer or culture medium in a vacuum desiccator. Apply vacuum (approximately 25-30 inHg) for 30-45 minutes while gently stirring if possible. Alternatively, heat the medium to 37°C while applying vacuum to accelerate gas removal.
- System Priming: Connect the degassed solution to the microfluidic system via the flow controller. With all outlets open, gradually increase the pressure to 50-100 mbar, allowing the liquid to slowly displace the air within the tubing and channels.
- Bubble Dissolution: If bubbles persist trapped within the device, temporarily increase the inlet pressure to 200-300 mbar for 5-10 seconds, then return to the operating pressure. The increased pressure forces dissolution of small air bubbles into the surrounding liquid.
- System Verification: Visually inspect all channels and chambers under magnification to confirm the absence of bubbles. Verify stable flow by monitoring the meniscus movement at the outlet or by tracking beads if available.
Protocol for Clog Mitigation in Cell-Based Assays
Purpose: To prevent channel obstruction during the introduction and cultivation of cells within microfluidic devices.
Materials:
- Cell suspension at appropriate density
- Cell strainer (30-40 μm mesh)
- Pressure-based flow controller
- Microfluidic device with appropriate chamber design
- Surface passivation solution (e.g., 1% Pluronic F-127)
Procedure:
- Sample Preparation: Gently dissociate cells to minimize aggregation and filter the cell suspension through a sterile mesh strainer to remove large aggregates that could obstruct inlet channels.
- Surface Treatment: Prior to cell introduction, flush the microfluidic device with surface passivation solution for 15-30 minutes, then rinse with cell-compatible buffer to create a non-adhesive surface along the main flow channels.
- Controlled Cell Loading: For hydrodynamic cell trapping designs, introduce the filtered cell suspension at a low flow rate (e.g., 1-2 μL/min) to ensure controlled entry into cultivation chambers without over-pressurization.
- Post-Loading Rinse: Once cells are trapped in the designated chambers, switch to fresh medium perfusion at the desired operational flow rate to remove any non-trapped cells from the main channels that might otherwise serve as nucleation points for future clogs.
Fluid Control Preparation Workflow
Troubleshooting and Corrective Actions
Despite rigorous prevention, clogging and bubble formation may still occur during extended experiments. The following systematic approaches enable researchers to resolve these issues with minimal experimental disruption.
Bubble Removal Techniques
When bubbles are detected within the microfluidic path, implement the following escalation strategy:
- Pressure Pulses: Using a pressure-based flow controller, apply a square-wave pressure signal (e.g., cycling between operational pressure and 2x operational pressure at 1-2 Hz frequency for 10-20 seconds). The alternating forces help detach bubbles adhered to channel walls [70].
- Surfactant Introduction: If pressure pulses alone prove insufficient, flush the system with a buffer containing a mild surfactant such as 0.1% Tween-20 or 0.5% BSA. These compounds reduce interfacial tension, facilitating bubble dissolution and detachment. Note that surfactants may interfere with certain biological assays and should be used judiciously.
- Backpressure Application: For persistently trapped bubbles, apply pressure simultaneously at all inlets of the microfluidic chip for several minutes. This technique increases gas solubility in the surrounding liquid, forcing dissolution of the bubble over time [70].
Table 2: Troubleshooting Guide for Common Fluid Control Issues
| Problem | Primary Cause | Immediate Corrective Action | Long-Term Solution |
|---|---|---|---|
| Frequent channel clogging | Cell aggregates or precipitates | Reverse flow briefly if possible | Implement pre-filtration of samples; optimize channel dimensions |
| Bubbles at junction points | Air ingress at fittings | Check and seal all connections | Use Teflon tape on threaded fittings; employ degassing methods |
| Flow rate instability | Compliance from trapped bubbles | Apply pressure pulses to mobilize bubbles | Integrate inline bubble traps; switch to less gas-permeable materials |
| Gradual pressure increase | Partial clog developing | Flush with cleaning solution (e.g., 1M NaOH) | Increase channel cross-section; implement more frequent passivation |
| Sudden flow cessation | Complete channel blockage | Attempt backflush procedure | Redesign critical regions with redundant paths; add pre-column filters |
Clog Resolution Methods
Addressing established clogs requires careful intervention to restore flow without damaging the microfluidic device or biological samples:
- Backflushing: Reverse the flow direction temporarily by applying pressure at the outlet while opening the inlet to waste. This approach can dislodge recently formed clogs without introducing additional stresses to cultured cells in separate compartments.
- Chemical Dissolution: For precipitates or crystalline clogs, identify a compatible solvent that can dissolve the obstruction without damaging the device or any biological components. For example, dilute sodium hydroxide (0.1-0.5M) can effectively dissolve proteinaceous clogs.
- Pressure Surge: As a last resort before device abandonment, apply a short, high-pressure pulse (3-5x operational pressure) for no more than 1-2 seconds. This approach carries risk of device failure but may successfully clear obstructions in robust chips.
Troubleshooting Decision Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of robust fluid control requires specific materials and reagents selected for their functional properties in preventing and addressing clogging and bubble formation.
Table 3: Essential Research Reagent Solutions for Fluid Control
| Reagent/Material | Primary Function | Application Protocol | Compatibility Notes |
|---|---|---|---|
| Pluronic F-127 | Surface passivation to reduce protein and cell adhesion | Flush device with 0.1-1% solution for 30 min before experiment | Compatible with most cell types; may interfere with certain protein assays |
| Tween-20 | Surfactant for reducing bubble adhesion and interfacial tension | Add at 0.01-0.1% to running buffers | Avoid in membrane protein studies; can affect cell viability at high concentrations |
| Degassed Buffer | Prevention of bubble nucleation from dissolved gases | Prepare using vacuum degassing immediately before use | Essential for all perfusion systems; maintain in sealed containers |
| Sodium Hydroxide (0.5M) | Cleaning agent for dissolving organic clogs and residues | Flush system for 15-30 min between experimental runs | Incompatible with living cells; rinse thoroughly before reintroducing biologicals |
| Bubble Trap Module | Physical removal of bubbles from fluidic path | Install inline between pressure source and device | Select appropriate volume for flow rate; may add compliance to system |
| Inline Filter | Removal of particulates from samples prior to injection | Place between sample reservoir and device inlet | Choose pore size based on smallest channel dimension; replace regularly |
Ensuring robust fluid control through comprehensive management of clogging and bubble formation is not merely a technical consideration but a fundamental requirement for generating reliable, reproducible data in microfluidics-based drug discovery research. By integrating strategic device design, preventive maintenance protocols, and systematic troubleshooting methodologies, researchers can significantly enhance the operational reliability of their microfluidic platforms. The protocols and guidelines presented herein provide a structured approach to maintaining fluidic integrity across diverse applications—from single-cell analysis and protein crystallization to complex organoid-based drug screening—thereby supporting the advancement of microfluidic technologies as robust tools in the pharmaceutical development pipeline.
The adoption of microfluidic technologies in high-throughput drug discovery represents a paradigm shift, enabling the miniaturization of assays and a significant increase in experimental throughput [4]. These systems provide a valuable tool for various applications throughout the drug discovery and development pipeline, from initial target selection to lead identification and preclinical testing. The core advantage lies in their ability to precisely manipulate fluids within microscale channels, integrating multiple components such as pumps, valves, mixers, and heaters to perform experiments using minimal reagents and achieving fast reaction times [4]. The integration of these technologies with existing laboratory workflows and data management systems is critical for maximizing their potential, reducing manual error, and ensuring the generation of reliable, high-quality data.
Automation Solutions for Microfluidic Workflows
Advanced Microfluidic Platforms
Recent advancements have led to the development of sophisticated, automated microfluidic platforms specifically designed for complex, gel-based 3D cell cultures, such as organoids. These systems address previous limitations of compatibility with extracellular matrices like Matrigel and low throughput.
Key Platform Features: An automated, high-throughput microfluidic 3D organoid culture and analysis system has been developed to facilitate preclinical research. This system provides combinatorial and dynamic drug treatments to hundreds of cultures in parallel and enables real-time analysis of organoids [71]. Its design includes a 200-well array for culturing organoids, with each well unit serving as a culture chamber for 3D structures grown within a gel matrix. The platform is engineered to accommodate large, mature organoids (averaging around 500 μm in diameter) with chamber heights of approximately 610 μm, which is significantly larger than most conventional microfluidic devices [71].
Fluidic Control and Automation: A key component is a reversibly clamped two-layer chamber chip. A second, multiplexer control device, composed of a system of fluidic channels and valves, provides automated, programmable fluidic flow to the valve-less culture device [71]. This automation allows for the application of dynamic conditions, such as temporally-modified drug treatments, which have been shown in validation screens on human-derived pancreatic tumor organoids to be more effective in vitro than constant-dose monotherapy or combination therapy [71]. This level of automation standardizes timing of media and drug delivery, limiting human error and enabling the execution of complex, preprogrammed experiments that would be infeasible with manual pipetting.
Integration with Broader Laboratory Automation
The philosophy of automation in drug discovery is expanding from standalone devices to integrated systems. The focus is on creating tools that are ergonomic, accessible, and can fit into existing workflows rather than forcing workflows to adapt around them [72]. This includes:
- Benchtop Automation Systems: For liquid handling tasks, companies are developing systems that offer a balance of simplicity and capability. For instance, walk-up automation that any researcher can use without extensive training empowers scientists to save time on repetitive tasks like pipetting, freeing them for analysis and strategic thinking [72].
- Robotics and Closed-Loop Systems: The integration of microfluidics with robotics is creating closed-loop design–make–test–learn cycles. One AI-driven drug discovery company, for example, launched an integrated AI-powered platform linking generative-AI design software with a robotics-driven "AutomationStudio" to synthesize and test candidate molecules automatically [73]. This represents the cutting edge of workflow integration.
Research Reagent Solutions for Automated Microfluidic Screening
Successful integration requires the use of specific reagents and materials compatible with microfluidic systems and the biological models used. The following table details key solutions for automated organoid-based screening.
Table 1: Essential Research Reagent Solutions for Automated Microfluidic Organoid Screening
| Reagent/Material | Function in the Workflow |
|---|---|
| Extracellular Matrix (e.g., Matrigel) | Provides a physiologically relevant 3D scaffold for organoid growth, delivering both mechanical support and essential biochemical cues [71]. |
| Patient-Derived Tumor Organoids | Serve as biologically relevant, personalized tumor models that retain the heterogeneity and characteristics of the parent tumor for ex vivo therapeutic testing [71]. |
| Fluorescent Cellular Protein Markers | Enable continuous, time-dependent, live-cell analysis of cell reactions, viability, and proliferation within the microfluidic device via fluorescence microscopy [71]. |
| Precursor Cells (e.g., Primary Cancer Cells) | Are seeded into the matrix to develop into mature organoids directly on the platform, allowing for the entire lifecycle to be monitored under controlled conditions [71]. |
| Drug Cocktails & Signaling Molecules | The solutions preloaded into the automated multiplexer device to be delivered in precise temporal sequences and combinations to the cultured organoids [71]. |
Data Management and Integration Solutions
The automation of microfluidic systems generates vast amounts of data, making robust data management and analysis platforms essential for deriving meaningful insights.
The Data Challenge and AI Integration
A significant challenge in modern drug discovery is dealing with fragmented, siloed data and inconsistent metadata, which creates barriers to automation and AI delivering full value [72]. The industry is responding with a focus on:
- Data Traceability: For AI to be effective, it is critical to capture more than just results; every experimental condition and state must be recorded to provide quality data for models to learn from [72]. This ensures transparency and builds trust in AI-driven decisions, which is essential for partners and regulators [72].
- Foundational Models: Companies are applying foundation models to extract features from complex data, such as imaging. For example, large-scale AI models trained on thousands of histopathology and multiplex imaging slides can identify new biomarkers and link them to clinical outcomes [72].
Software Platforms for Data Handling
Several software solutions are emerging to address these data management needs. The following table compares key platforms relevant to a microfluidic and automation-driven discovery environment.
Table 2: Comparison of Data Handling and AI Software Platforms
| Software Platform | Key Data & AI Capabilities | Relevance to Integrated Workflows |
|---|---|---|
| Cenevo | Unites sample management (Mosaic) and digital R&D (Labguru) platforms; embeds an AI Assistant for smarter search and workflow generation [72]. | Helps laboratories connect data, instruments, and processes, providing a structured data landscape for AI applications [72]. |
| Sonrai Analytics | Integrates complex imaging, multi-omic, and clinical data into a single analytical framework with advanced, transparent AI pipelines [72]. | Supports the analysis of multi-modal datasets generated by microfluidic platforms, uncovering links between molecular features and disease [72]. |
| deepmirror | Generative AI engine for molecule generation and property prediction; supports prediction of protein-drug binding complexes; user-friendly for chemists [74]. | Accelerates hit-to-lead optimization, seamlessly connecting data analysis with design in an automated discovery cycle [74]. |
| Schrödinger | Integrates quantum chemical methods with machine learning; cloud-based platform for high-capacity molecular simulation [73] [74]. | Provides powerful in silico validation for compounds and targets identified in high-throughput microfluidic screens. |
Experimental Protocols
Protocol: Automated Dynamic Drug Screening on Patient-Derived Tumor Organoids
This protocol describes a methodology for using an automated microfluidic platform to perform dynamic and combinatorial drug screening on patient-derived tumor organoids, based on the system validated by [71].
Key Experiment Cited: Automated microfluidic platform for dynamic and combinatorial drug screening of tumor organoids [71].
1. Platform Setup and Priming: - Assemble the two-layer microfluidic device by reversibly clamping the fluidic channel layer over the 200-well chamber array. - Connect the assembled culture device to the automated multiplexer control device via fluidic tubing. - Preload the multiplexer's solution vials with the required media, drug stocks, and staining solutions. Ensure the multiplexer's solenoid valves are connected to the control software.
2. Device Loading with Extracellular Matrix and Cells: - Unclamp and separate the fluidic channel layer from the well array. - Manually pipette a mixture of temperature-sensitive Matrigel (or other hydrogel) and suspended patient-derived primary tumor cells into each well of the array. This manual pipetting step is feasible due to the valve-less, non-permanently bonded design. - Re-clamp the fluidic layers together and place the entire assembly onto the stage of a programmable microscope equipped with an environmental chamber (maintained at 37°C and 5% CO₂).
3. Organoid Culture and Monitoring: - Using the control software, program the multiplexer to perfuse culture media through the channels over the wells at defined intervals to supply nutrients. - Allow organoids to develop from single cells over a period of days to weeks. Monitor growth, morphology, and express fluorescent protein markers in 3D using time-lapse phase-contrast and fluorescence deconvolution microscopy.
4. Programmable Drug Treatment: - Design the dynamic treatment regimen in the control software (e.g., via a tab-delimited text file). This can include sequences for single drugs, combinations, or complex temporal profiles where concentration and duration are varied over time. - Initiate the preprogrammed experiment. The multiplexer device will automatically switch between the preloaded solutions, delivering the precise fluidic sequences to the 20 independent channel subsets, each servicing 10 individual chamber units. - Continue real-time imaging throughout the drug treatment phase to capture organoid response kinetics.
5. Endpoint Analysis and Harvesting: - After the experiment, terminate fluidic flow and imaging. - Unclamp the device to separate the layers, exposing the well array. - Harvest organoids from the gel matrix for subsequent downstream analysis, such as genomic sequencing, further expansion, or grafting.
Workflow Visualization
The following diagram illustrates the integrated workflow of the automated microfluidic screening platform, from setup to data analysis.
Proving Efficacy: Validating Microfluidic Platforms Against Traditional Drug Discovery Methods
The integration of microfluidic technology into high-throughput drug discovery represents a paradigm shift, offering unprecedented capabilities for miniaturization, automation, and physiological relevance. However, the transition of these platforms from research tools to validated components of the drug development pipeline necessitates rigorous benchmarking of their performance against established standards. Performance benchmarking ensures that data generated from microfluidic systems is reliable, reproducible, and translatable to clinical outcomes. This document provides detailed application notes and protocols for benchmarking the key metrics of accuracy, reproducibility, and scalability for microfluidic devices within high-throughput drug discovery research. The core advantages of microfluidic systems that require benchmarking include their ability to significantly reduce reagent volumes (from 100–200 µl in conventional 96-well plates to 50 nl in microchambers), integrate 3D cell cultures that better mimic the physiological microenvironment, and provide dynamic control over fluidic conditions for more predictive assays [9] [75].
Quantitative Performance Metrics for Microfluidic HTS
To ensure data quality and platform reliability, specific quantitative metrics must be evaluated. The table below summarizes the core performance metrics essential for benchmarking microfluidic High-Throughput Screening (HTS) platforms.
Table 1: Key Performance Metrics for Benchmarking Microfluidic HTS Platforms
| Metric Category | Specific Metric | Definition/Measurement Method | Benchmark Target/Industry Standard |
|---|---|---|---|
| Accuracy | Coefficient of Variation (CV) for cell viability | (Standard Deviation / Mean) of replicate measurements expressed as a percentage [75] | CV < 10% for robust assays [75] |
| Z'-factor for assay quality | 1 - (3*(σp + σn) / |μp - μn|), where p=positive control, n=negative control [75] | Z' > 0.5 indicates an excellent assay [75] | |
| Predictive Value for in vivo efficacy | Correlation coefficient between in vitro IC50 and in vivo therapeutic efficacy [9] | High positive correlation (R² > 0.6) desired [9] | |
| Reproducibility | Intra-device CV | CV of results across multiple chambers or units on the same device [9] | CV < 15% [9] |
| Inter-device CV | CV of results across multiple independently fabricated devices [9] | CV < 20% [9] | |
| Inter-operator CV | CV of results when the assay is performed by different trained personnel [76] | CV < 15% [76] | |
| Inter-laboratory CV | CV of results when the protocol is executed in different laboratories [77] | CV < 25-30% [77] | |
| Scalability | Throughput (samples/day) | Number of individual experiments or data points generated per day [76] | Droplet systems: > 100,000 samples/day [76] |
| Batch-to-Batch Uniformity | Size and PDI of nanoparticles synthesized across different production batches [78] | PDI < 0.2 indicates a highly uniform distribution [78] | |
| Manufacturing Consistency | Percentage of devices that function as intended without defects [9] | > 95% yield for functional devices [9] |
Experimental Protocols for Benchmarking
Protocol 1: Benchmarking Assay Performance and Accuracy
Aim: To quantify the accuracy and robustness of a cell-based drug screening assay on a microfluidic platform using the Z'-factor.
Materials:
- Microfluidic Device: PDMS-based device with 96 or more parallel cell culture chambers [9] [75].
- Cell Line: A relevant, stable cell line (e.g., Caco-2 for adhesion studies) [9].
- Reagents: Cell culture medium, positive control drug (e.g., a known cytotoxic compound like staurosporine), negative control (vehicle, e.g., DMSO), live/dead cell staining kit (e.g., Calcein AM/EthD-1) [75].
- Equipment: Inverted fluorescence microscope with an automated stage, environmental chamber for temperature and CO2 control, precision syringe pumps for fluid handling [9] [76].
Procedure:
- Device Preparation: Sterilize the microfluidic device (e.g., via UV light or ethanol flush). Coat the device channels and chambers with an extracellular matrix protein (e.g., fibronectin) to enhance cell adhesion [9].
- Cell Seeding: Prepare a single-cell suspension at an optimized density. Use a syringe pump to introduce the cell suspension into the device at a low, constant flow rate to ensure uniform cell distribution across all chambers. Allow cells to adhere and grow for 24-48 hours under standard culture conditions [9] [75].
- Control Treatment:
- Identify a set of chambers for positive controls and another set for negative controls.
- Perfuse the positive control chambers with a medium containing a high concentration of the cytotoxic drug.
- Perfuse the negative control chambers with a medium containing only the vehicle.
- Incubate for a predetermined period (e.g., 24 hours).
- Viability Staining and Imaging: Introduce the live/dead stain mixture into all channels. After incubation, acquire high-resolution fluorescence images from each chamber for both positive and negative control sets using an automated microscope.
- Image and Data Analysis:
- Use image analysis software (e.g., ImageJ, CellProfiler) to count the number of live (green) and dead (red) cells in each chamber.
- Calculate the percentage of cell viability for each chamber: (Number of live cells / Total number of cells) * 100.
- For the positive control set, calculate the mean (μp) and standard deviation (σp) of cell viability.
- For the negative control set, calculate the mean (μn) and standard deviation (σn) of cell viability.
- Compute the Z'-factor: 1 - [3*(σp + σn) / \|μp - μn\|] [75].
Interpretation: A Z'-factor > 0.5 indicates an excellent assay with a large dynamic range and low variability. A Z'-factor between 0 and 0.5 is considered marginal, while a Z'-factor < 0 indicates a non-viable assay that is not suitable for screening [75].
Protocol 2: Benchmarking Device Reproducibility and Scalability
Aim: To assess the intra-device, inter-device, and inter-laboratory reproducibility of a microfluidic drug screening assay, and to evaluate the scalability of nanoparticle synthesis.
Materials:
- Multiple Microfluidic Devices: At least three devices from the same fabrication batch and three from different batches [9].
- Standardized Reagent Kits: Pre-aliquoted and quality-controlled stocks of cells, media, and control drugs to be shared across testing sites [77].
- Lipid Nanoparticle (LNP) Synthesis Setup: A staggered herringbone micromixer (SHM) chip, syringe pumps, lipid solution in alcohol, and an aqueous buffer [78].
Procedure: Part A: Reproducibility of a Cell-Based Assay
- Intra- and Inter-Device Testing: A single operator performs the drug screening assay described in Protocol 1 on one device, measuring results from 10 internal chambers (intra-device). The operator then repeats the identical assay on at least two additional devices from the same fabrication batch (inter-device).
- Inter-Laboratory Testing: Ship standardized reagent kits and devices to two or more partner laboratories. Each laboratory follows the same written protocol to perform the assay on multiple devices.
- Data Analysis: Calculate the Coefficient of Variation (CV) for the measured outcome (e.g., IC50 value, cell viability) for each reproducibility level:
- Intra-device CV: CV across the 10 chambers of one device.
- Inter-device CV: CV of the mean results from each device within the same batch.
- Inter-laboratory CV: CV of the mean results reported by each laboratory [77].
Part B: Scalability of Nanoparticle Synthesis
- Microfluidic Synthesis: Use a syringe pump to simultaneously inject a lipid solution and an aqueous buffer into the SHM chip at a defined Flow Rate Ratio (FRR). Collect the resulting LNP suspension at the outlet [78].
- Batch-to-Batch Testing: Repeat the synthesis process multiple times (n≥5) over different days to create multiple batches.
- Characterization: For each batch, use dynamic light scattering (DLS) to measure the average particle size (Z-average) and the Polydispersity Index (PDI).
- Data Analysis: Calculate the mean particle size and PDI across all batches. A PDI < 0.2 indicates a highly monodisperse and reproducible synthesis process, which is critical for scalable production [78].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Microfluidic HTS
| Item Name | Function/Application | Critical Parameters & Notes |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Elastomeric polymer used for rapid prototyping of microfluidic devices [9] [75]. | Gas permeability for cell culture; requires surface modification (e.g., plasma oxidation, fibronectin coating) for cell adhesion [9]. |
| Extracellular Matrix (ECM) Proteins (Fibronectin, Collagen) | Coating substrates to promote cell adhesion and growth in microchannels [9]. | Fibronectin adsorption on PDMS can increase cell adhesion to levels comparable to treated polystyrene [9]. |
| Staggered Herringbone Micromixer (SHM) | Passive mixer for efficient nanoprecipitation and synthesis of lipid nanoparticles (LNPs) [78]. | Provides highly efficient mixing; optimal design is critical for controlling LNP size and polydispersity [78]. |
| Precision Syringe Pumps | To control the flow of fluids (cells, drugs, reagents) through microchannels at defined rates [76]. | Essential for generating stable concentration gradients and for reproducible droplet generation in emulsion-based systems [76]. |
| Z'-factor Assay Kit | A standardized set of positive and negative controls for quantifying assay robustness [75]. | Contains a known cytotoxic agent (positive control) and vehicle (negative control). |
Workflow and Data Analysis Diagrams
Diagram 1: Microfluidic HTS Benchmarking Workflow. This diagram outlines the logical flow for systematically benchmarking a microfluidic High-Throughput Screening (HTS) platform, from initial preparation to final validation, including an iterative feedback loop for process improvement.
Rigorous benchmarking grounded in standardized protocols and quantitative metrics is the cornerstone for establishing credibility and ensuring the translational success of microfluidic platforms in drug discovery. By systematically evaluating accuracy, reproducibility, and scalability as outlined in these application notes, researchers can not only optimize their own systems but also generate data that is comparable and reliable across the scientific community. This practice is critical for accelerating the adoption of microfluidic technologies, ultimately leading to more efficient and predictive drug development pipelines.
In the field of high-throughput drug discovery, the half-maximal inhibitory concentration (IC50) is a critical parameter for quantifying the potency of a drug candidate [79]. It represents the concentration required to inhibit a specific biological process by 50%, serving as a key benchmark for evaluating the efficacy of potential therapeutics, including antitumor agents [79] [80]. Traditional methods for IC50 determination, such as enzyme-linked immunosorbent assays (ELISA) and colorimetric kits (e.g., CCK-8, MTT), often face limitations including the use of endpoint measurements, potential interference from assay reagents, and poor performance with certain cell types [79] [80]. These factors can introduce significant deviation from theoretical dose-response curves, reducing the accuracy and predictive power of preclinical data.
The integration of advanced microfluidic platforms within drug discovery workflows presents a powerful strategy to overcome these limitations [21]. Microfluidic systems, including organ-on-chip (OoC) and lab-on-chip (LoC) devices, enable high-throughput screening with dramatic reductions in reagent consumption and offer superior physiological relevance by recapitulating human tissue environments and incorporating dynamic flow conditions [21]. This application note details a case study utilizing a novel, label-free surface plasmon resonance (SPR) imaging platform integrated within a microfluidic format. This approach allows for real-time, high-throughput monitoring of drug-induced cytotoxicity based on cell adhesion changes, achieving highly accurate IC50 values with minimal deviation from theoretical models [79].
Experimental Protocols and Methodologies
Fabrication of Nanowire Array Sensor (NAS) Chips
The core of the sensing platform is a gold-coated periodic nanowire array sensor (NAS) fabricated via compression-injection molding, which ensures high chip-to-chip uniformity critical for reproducible high-throughput screening [79].
- Master Template Preparation: A 5x5 array of 400 nm-period nanoridge structures was fabricated on a Ni–Co mold using electron beam lithography followed by electroplating. The master template contained 25 individual nanoslit arrays [79].
- Replication Process: Large-area plastic nanostructure chips were mass-produced on polycarbonate substrates using compression-injection molding with the master template. The resulting nanowire structures had a periodicity of 400 nm [79].
- Metal Deposition and Assembly: A 50 nm-thick gold layer was deposited onto the nanowire arrays via electron-beam evaporation. The final NAS biochip was assembled by stacking double-sided tape, a poly(methyl methacrylate) (PMMA) layer, and the NAS substrate [79].
- Surface Treatment: Prior to cell experiments, assembled biochips were sterilized and rendered hydrophilic via oxygen plasma treatment (200 W, 120 s) to promote efficient cell attachment [79].
Cell Culture, Seeding, and Drug Treatment
This protocol was applied to lung cancer (CL1-0, A549), liver cancer (Huh-7), and breast cancer (MCF-7) cell lines to evaluate the cytotoxicity of doxorubicin [79].
- Cell Culture: Maintain cells in appropriate culture media (e.g., RPMI-1640 for CL1-0 cells) supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin at 37°C in a 5% CO₂ atmosphere [79].
- Cell Seeding on NAS: Detach cells, count, and seed onto the oxygen plasma-treated NAS biochips at an optimized density (e.g., 5 x 10⁴ cells per well) to ensure consistent monolayer formation. Allow cells to adhere for a predetermined time [79].
- Drug Treatment: Prepare a serial dilution of the drug (e.g., doxorubicin) in complete culture medium. At the time of treatment, replace the medium on the NAS biochips with medium containing the drug at various concentrations. Include vehicle-only controls for normalization [79].
Contrast SPR Imaging and Data Acquisition
The reflection-mode SPR imaging system detects changes in cell adhesion by monitoring spectral shifts at the SPR dip [79].
- Imaging System Setup: The system comprises a coaxial linear white LED light source, a 40 nm bandpass filter centered at 580 nm, and a scientific CMOS (sCMOS) camera for image capture [79].
- Image Capture Protocol:
- Acquire a baseline SPR image after initial cell seeding.
- Capture a second image immediately after drug administration.
- Capture a final image 24 hours post-treatment [79].
- Self-Referencing Analysis: For each region of interest (ROI), calculate the spectral contrast value (γ) at each time point using the formula derived from the red (R) and green (G) channel intensities [79]:
γ = (I_G - I_R) / (I_G + I_R)The change in γ over time reflects the drug-induced alteration in cell attachment [79].
Data Analysis and IC50 Calculation
The following workflow converts raw imaging data into a quantitative IC50 value.
- Signal Normalization: Normalize the spectral contrast values (γ) from the 24-hour time point against the values from the time point immediately after drug addition for each drug concentration.
- Dose-Response Curve Fitting: Plot the normalized cell attachment (expressed as a percentage) against the logarithm of the drug concentration. Fit the data points to a standard four-parameter logistic (4PL) nonlinear regression model:
Y = Bottom + (Top - Bottom) / (1 + 10^((LogIC50 - X) * HillSlope))where Y is the response, and X is the log(concentration). - IC50 Determination: The IC50 value is derived directly from the fitted curve as the concentration at which the response is halfway between the top (maximum attachment, control) and bottom (minimum attachment) plateaus [79].
Key Findings and Data Presentation
Quantitative Performance of SPR Imaging vs. Traditional Assays
The contrast SPR imaging platform demonstrated superior performance and reliability compared to conventional methods.
Table 1: Comparison of IC50 Values and Key Parameters for Doxorubicin Cytotoxicity Assessment Using Different Methodologies on CL1-0 and MCF-7 Cell Lines
| Cell Line | Methodology | Reported IC50 | Key Advantages | Noted Limitations |
|---|---|---|---|---|
| CL1-0 | Contrast SPR Imaging | Successfully Quantified [79] | Label-free, real-time, high-throughput, based on physiological adhesion [79] | Requires specialized NAS chips and imaging system [79] |
| CL1-0 | Cell Staining Assay | Aligned with SPR data [79] | Considered a reliable standard [79] | End-point assay, may miss dynamic responses [79] |
| CL1-0 | CCK-8 Assay | Not Specifically Reported [79] | Simple, affordable [79] | Failed to quantitatively assess MCF-7; potential reagent interference [79] |
| MCF-7 | Contrast SPR Imaging | Successfully Quantified [79] | Enabled accurate quantification where CCK-8 failed [79] | Requires specialized NAS chips and imaging system [79] |
| MCF-7 | CCK-8 Assay | Failed to Quantify [79] | — | Inability to assess quantitative cytotoxic effects on this cell line [79] |
The data confirms that the SPR imaging platform reliably quantified IC50 values for cell lines where the enzymatic CCK-8 assay failed, highlighting its robustness and broader applicability [79]. The methodology's foundation in monitoring cell adhesion, a direct physiological response to cytotoxic insult (apoptosis and necrosis), minimizes artifacts that can cause deviation in theoretical values [79].
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful implementation of this microfluidic IC50 determination platform relies on several key reagents and materials.
Table 2: Key Research Reagent Solutions for Microfluidic IC50 Determination via SPR Imaging
| Item | Function / Rationale | Specific Examples / Notes |
|---|---|---|
| Gold-coated NAS Chips | The core sensor; nanostructure generates a sensitive and quantifiable SPR dip shift in response to changes in cell adhesion [79]. | 400 nm periodicity; 50 nm gold coating; fabricated via injection molding for high uniformity [79]. |
| Cell Culture Reagents | To maintain and prepare cells for the assay, ensuring consistency and viability. | Standard media (e.g., RPMI-1640), fetal bovine serum, penicillin-streptomycin, trypsin/EDTA [79]. |
| Therapeutic Compounds | The agents whose potency is being evaluated. | e.g., Doxorubicin; prepare a serial dilution in culture medium for dose-response testing [79]. |
| Primary Antibodies | For validation and multiplexing via techniques like in-cell Western [80]. | Target-specific antibodies (e.g., against phosphorylated proteins) to provide mechanistic insights alongside IC50 data [80]. |
| Fluorescently-Labeled Secondary Antibodies | Enable detection for complementary validation assays. | Used in in-cell Western for multiplex analysis; conjugated to fluorophores like AzureSpectra [80]. |
| Fixation and Permeabilization Buffers | Preserve cellular architecture and allow antibody entry for immunodetection assays [80]. | Used when combining the platform with endpoint validation methods like in-cell Western [80]. |
Visualizing Workflows and System Relationships
Experimental Workflow for IC50 Determination
The following diagram outlines the key steps in the IC50 determination process using the NAS-based SPR platform.
Relationship Between Microfluidic Platforms and IC50 Determination
This diagram conceptualizes how the NAS-SPR platform fits into the broader ecosystem of microfluidic technologies for drug discovery.
This case study demonstrates that the nanostructure-enhanced SPR imaging platform enables accurate, label-free, and high-throughput IC50 determination, effectively minimizing deviations from theoretical values encountered with traditional enzymatic assays. Its success lies in directly measuring a physiologically relevant parameter—cell adhesion—in real-time and within a scalable microfluidic format. The convergence of such label-free biosensing technologies with advanced microfluidic systems like organ-on-chip and droplet platforms is poised to significantly accelerate the drug discovery pipeline. These integrated approaches provide more predictive, human-relevant potency data earlier in the development process, thereby reducing late-stage attrition and fostering the delivery of more effective therapeutics.
The relentless pursuit of efficiency in drug discovery is driving the adoption of advanced screening technologies. For decades, multi-well plates have been the standard tool for early-stage research. However, the emergence of sophisticated microfluidic platforms presents a compelling alternative, promising significant gains in throughput, cost-effectiveness, and data quality. This application note provides a comparative analysis of modern high-throughput microfluidic systems against traditional well-plate methods, contextualized within drug discovery research. We present quantitative data, detailed protocols, and essential toolkits to guide researchers in evaluating and implementing these transformative technologies.
Quantitative Comparative Analysis
The following tables summarize a direct comparison of key performance indicators between microfluidic systems and traditional well-plate methods, based on current market data and technological capabilities.
Table 1: Overall Performance and Market Metrics
| Metric | Traditional Well-Plates | Microfluidic/HTS Platforms | Reference / Notes |
|---|---|---|---|
| Global Market Size (2025) | ~Part of HTS Market | USD 24.6 Billion (Microfluidic Devices) | [81] |
| Market Growth Rate (CAGR) | ~8.7% (Overall HTS Market) | 12.2% (Microfluidic Devices) | [82] [81] |
| Sample Consumption | ~Microliter (μL) range | 200x less than a 96-well plate (Nanoliter to Picoliter) | [26] |
| Assay Time | ~2 hours (for a given reaction) | ~2.5 minutes (due to higher surface-to-volume ratio) | [26] |
Table 2: Technology and Data Quality Comparison
| Aspect | Traditional Well-Plates | Microfluidic/HTS Platforms |
|---|---|---|
| Screening Technology | Ultra-High-Throughput Screening, Cell-Based Assays | Lab-on-a-Chip (LoC), Organ-on-a-Chip (OoC), Droplet Microfluidics |
| Throughput | High (Thousands to millions of compounds) | Ultra-High (Extreme parallelization with droplets) |
| Physiological Relevance | Static 2D cell cultures, limited mimicry of in vivo conditions | High; dynamic fluid flow, 3D cell models, human organ mimicry (OoC) |
| Data Quality & Content | Population-average data (e.g., from plate readers) | Single-cell resolution, continuous, time-lapsed tracking possible |
| Key Applications | Primary and secondary screening, toxicology | High-throughput screening, personalized medicine, complex disease modeling |
Featured Microfluidic Platforms and Experimental Protocols
High-Throughput Organ-on-Chip (HT-OoC) Screening
Platforms like the OrganoPlate (MIMETAS) have been adapted for high-throughput experimentation by scaling into standard well-plate formats (e.g., 40-, 64-, or 96-independent chips per plate) [39]. These systems enable the cultivation of perfused 3D tissue models without artificial membranes, providing direct access to both apical and basolateral sides of the culture.
Protocol 1: 3D Tubule Formation and Barrier Integrity Assay in an OrganoPlate
Research Reagent Solutions:
- Extracellular Matrix (ECM): Collagen I, Matrigel, or other optimized hydrogels.
- Cell Suspension: Endothelial cells (e.g., HUVECs) and/or epithelial cells relevant to the target organ.
- Culture Medium: Cell-type specific medium, such as Endothelial Cell Growth Medium.
- Fluorescent Tracers: FITC-Dextran (e.g., 70 kDa for barrier integrity assessment).
- Assay Reagents: PrestoBlue/MTT for viability, specific substrates for enzymatic activity.
Procedure:
- Chip Priming: Following manufacturer instructions, prime the ECM channel of the OrganoPlate with a sterile PBS solution to prepare the surface for hydrogel loading.
- Hydrogel Loading: Mix the selected ECM hydrogel with cells if desired for embedded 3D culture. Using a positive displacement pipette, carefully load the ECM-cell mixture into the designated gel-inlet channel. Allow the hydrogel to polymerize in a 37°C incubator for 15-30 minutes.
- Perfusion Channel Seeding: Introduce a concentrated suspension of endothelial cells into the two perfusion channels. Allow cells to adhere to the gel-facing sides of the channels for 1-2 hours under static conditions.
- Continuous Perfusion: Place the OrganoPlate on a rocker platform inside a 37°C, 5% CO₂ incubator. The rocking motion induces bidirectional perfusion, ensuring continuous nutrient supply and waste removal.
- Tubule Formation & Validation: Monitor tubule formation over 2-5 days using brightfield and fluorescence microscopy. To assess barrier integrity, add a fluorescent tracer (e.g., FITC-Dextran) to one perfusion channel and measure its appearance in the opposite channel over time.
- Compound Screening: Introduce candidate drug compounds or stimuli directly into the perfusion medium. Automated liquid handlers can be integrated for high-throughput addition to all chips on the plate in parallel.
- Endpoint Analysis: Post-treatment, assess viability (e.g., PrestoBlue), morphology (imaging), and specific functional endpoints (e.g., cytokine release, transporter activity).
Droplet-Based Microfluidic Screening
Droplet microfluidics encapsulates single cells and reagents in picoliter-volume droplets, acting as millions of independent microreactors. This technology is ideal for massive parallelization in screening applications, such as antibody discovery or enzyme evolution [83] [26].
Protocol 2: High-Throughput Single-Cell Cytotoxicity Screening via Droplet Microfluidics
Research Reagent Solutions:
- Oil Phase: Fluorinated oil with a biocompatible surfactant (e.g., 2% RAN Biotechnologies Surfactant).
- Aqueous Phase 1: Cell suspension in growth medium at a optimized concentration (~1-5 million cells/mL).
- Aqueous Phase 2: Drug library compounds diluted in medium containing a fluorescent viability dye (e.g., Calcein AM for live cells, Propidium Iodide for dead cells).
- Lysis Buffer: An internal lysis buffer for intracellular content analysis (optional).
Procedure:
- Droplet Generation: Load the oil and two aqueous phases into separate syringes on a droplet generator chip (e.g., a flow-focusing device). Use precision syringe pumps to control flow rates. Typical rates are ~5000 μL/hr for the oil phase and ~1000 μL/hr for each aqueous phase to generate stable, monodisperse droplets (~50-100 μm diameter).
- Incubation & Merging: Collect the emulsion (droplets in oil) in a syringe or tubing and incubate at 37°C for 30-60 minutes to allow for initial cell-drug interaction. For multi-step assays, a droplet pairing and merging step can be incorporated using electrocoalescence to add a second reagent.
- Incubation for Endpoint Readout: Further incubate the emulsion for several hours to days to allow for cytotoxic effects to manifest.
- Re-injection and Analysis: Re-inject the emulsion into an analysis chip. As droplets flow single-file past a laser-induced fluorescence (LIF) detector, measure the fluorescence intensity in multiple channels (e.g., green for Calcein AM, red for Propidium Iodide).
- Sorting (Optional): Based on the fluorescence signal, activate a dielectrophoretic or acoustic sorter to deflect and collect droplets containing cells with a desired phenotype (e.g., live cells in the presence of a cytotoxic drug).
- Data Collection: Use the sorted populations for downstream analysis (e.g., sequencing) or simply count the ratio of live/dead droplets from the fluorescence data to generate dose-response curves for each compound.
Workflow and Signaling Visualization
The fundamental difference in workflow and data acquisition between the two technologies is illustrated below.
Microfluidic vs Well Plate Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for High-Throughput Microfluidic Screening
| Item | Function | Example Application |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Elastomer for rapid prototyping of chips; biocompatible, gas-permeable. | Organ-on-Chip devices, custom microfluidic circuits. |
| Biocompatible Fluorinated Oils & Surfactants | Forms the continuous phase in droplet microfluidics; prevents droplet coalescence. | Generation of stable water-in-oil emulsions for single-cell assays. |
| Optimized Hydrogels (e.g., Collagen I) | Provides a 3D extracellular matrix (ECM) for cell growth and tissue formation. | Creating physiological 3D tissue models in OrganoPlates and other OoC platforms. |
| Viability/Cytotoxicity Dyes (e.g., Calcein AM/PI) | Fluorescent markers for distinguishing live and dead cells within micro-environments. | Real-time monitoring of cell health in response to compounds in droplets or OoC. |
| Primary Cells & Organoids | Biologically relevant human cell sources offering superior physiological mimicry. | Establishing patient-specific or disease-specific models for screening. |
| Integrated Biosensors | Transduce biological/chemical changes (e.g., pH, metabolites) into optical/electrical signals. | Real-time, label-free monitoring of cellular responses within microchannels. |
The transition from traditional well-plates to advanced microfluidic systems represents a paradigm shift in high-throughput screening. The quantitative data and protocols presented herein demonstrate that microfluidics offers unambiguous advantages in reducing reagent consumption and assay time by orders of magnitude while simultaneously enhancing data quality through physiologically relevant models and single-cell resolution. For drug discovery researchers, the adoption of these platforms, despite a steeper initial learning curve, is a strategic move towards more predictive, efficient, and cost-effective research and development.
Regulatory and Standardization Considerations for Clinical Translation
The translation of microfluidic devices from research prototypes to clinically approved tools for high-throughput drug discovery presents a complex interplay of regulatory compliance and standardization challenges. These miniaturized systems, which manipulate fluids at the microscale (10−6–10−9 liters), offer transformative potential for pharmaceutical research through reduced reagent consumption, faster assay times, and enhanced analytical sensitivity [84] [1]. However, their multidisciplinary nature—integrating biology, fluid dynamics, material science, and electronics—creates unique regulatory hurdles that must be navigated for successful clinical implementation [84]. This document outlines the current regulatory frameworks, standardization initiatives, and practical protocols to facilitate the clinical translation of microfluidic devices within drug discovery pipelines.
The commercialization pathway for microfluidic devices typically spans 3-5 years from laboratory prototyping to market entry, with regulatory strategy requiring early integration into the development process [84]. Key challenges include the complexity of cartridge integration involving multiple reaction chambers, biosensors, and microchannels; manufacturing scalability while maintaining quality and consistency; and evolving regulatory expectations specific to microfluidic technologies [84] [85]. Recent developments, including the FDA's new regulatory science tool for microfluidics leakage testing (anticipated 2023-2025) and standardization roadmaps for organ-on-chip technology (January 2025), signal progress toward more standardized evaluation frameworks [86] [87].
Regulatory Frameworks and Compliance Strategies
Global Regulatory Landscape
Microfluidic diagnostic devices fall under the purview of various international regulatory agencies with distinct but converging requirements. In the United States, the Food and Drug Administration (FDA) Center for Devices and Radiological Health (CDRH) has reported a 400% increase in medical device submissions incorporating microfluidics from 2013 to 2018, prompting specialized regulatory development [86]. The FDA's "breakthrough devices program" offers an expedited pathway for innovative microfluidic technologies that demonstrate potential for unmet medical needs, while the recently developed Microfluidics Program aims to address knowledge gaps through consistent assessment protocols [88] [86].
The European Union operates under the Medical Device Regulation (MDR) framework, with notified bodies requiring compliance with relevant ISO standards. The European Commission's Joint Research Centre has actively contributed to creating a CEN-CENELEC Focus Group specifically for organ-on-chip standardization, recognizing the technology's potential for personalized medicine and animal-free testing [87]. Asia's regulatory landscape varies by country, with China's National Medical Products Administration (NMPA) and Japan's Pharmaceutical and Medical Devices Agency (PMDA) implementing increasingly stringent review processes [84].
The Medical Device Single Audit Program (MDSAP) allows manufacturers to undergo a single regulatory audit accepted by multiple participating countries, potentially streamlining the approval process for international markets [84]. However, regulatory bodies continue to enforce strict validation processes that can delay market entry, particularly for devices involving complex biochemical interactions [88].
Key Regulatory Hurdles and Solutions
Device Validation Complexity: Microfluidic-based diagnostic devices must demonstrate analytical, clinical, and scientific validity, requiring robust experimental designs and comprehensive data packages [85]. Solution: Implement a phased validation approach beginning with analytical performance verification during prototyping, followed by pre-clinical and clinical validation using statistically powered sample sizes.
Material Biocompatibility and Manufacturing Constraints: Scaling up production while ensuring compliance with material biocompatibility standards remains challenging, particularly for novel polymers and integrated biosensors [85]. Solution: Early material selection guided by ISO 10993-1 biological evaluation of medical devices standard, with manufacturing process validation under quality management systems such as ISO 13485.
Post-Market Surveillance Requirements: Regulatory agencies increasingly expect continuous monitoring of device performance through structured post-market surveillance programs [85]. Solution: Implement a comprehensive post-market surveillance system including unique device identification (UDI) tracking, customer feedback mechanisms, and periodic safety updates.
Table 1: Global Regulatory Agencies and Key Requirements for Microfluidic Devices
| Regulatory Agency | Key Requirements | Special Programs | Relevant Standards |
|---|---|---|---|
| U.S. FDA | Premarket notification [510(k)] or Premarket Approval (PMA); Quality System Regulation (21 CFR Part 820) | Breakthrough Devices Program; Microfluidics Program for leakage testing | ISO 13485; ISO 14971; CLIA regulations for IVDs |
| European CE Marking | Technical documentation per MDR; Clinical evaluation; Post-market surveillance | CEN-CENELEC Focus Group on Organ-on-Chip | ISO 13485; ISO 14971; EN ISO 10993-1 |
| China NMPA | Registration testing; Clinical trial approval; Technical review | - | GB/T standards; YY standards (medical devices) |
| Japan PMDA | Marketing authorization; QMS conformity assessment | - | JIS Q 13485; JPAL (Japan Pharmacopoeia) |
| MDSAP Participants | Single audit accepted by Australia, Brazil, Canada, Japan, United States | Medical Device Single Audit Program (MDSAP) | ISO 13485; jurisdiction-specific requirements |
Standardization Initiatives and Implementation
Current Standardization Landscape
Standardization efforts for microfluidic technologies have accelerated in response to the growing recognition of their potential in drug discovery and clinical applications. The International Organization for Standardization (ISO) has established a new Subcommittee on 'Microphysiological systems and Organ-on-Chip' (ISO/TC 276/SC2) under Technical Committee 276 - Biotechnology, signaling formal international recognition of the need for standardized approaches [87]. This development is particularly relevant for high-throughput drug discovery applications, where reproducibility across platforms is essential for reliable data generation.
The standardization roadmap published by the CEN-CENELEC Focus Group in January 2025 identifies key priority areas including material characterization methods, biocompatibility assessment protocols, performance verification frameworks, and data interoperability standards [87]. These efforts aim to establish consensus on critical quality attributes and performance metrics that will enable more straightforward regulatory evaluation and technology adoption.
Manufacturing Standards and Scalability
Transitioning from laboratory prototyping to industrial-scale production presents significant standardization challenges. The manufacturing process chain for microfluidic cartridges encompasses concept development, laboratory prototyping, pre-clinical validation, clinical validation, and finally mass production, with each stage requiring different manufacturing approaches and quality controls [84].
For initial prototyping (5-50 chips), manufacturing processes must be flexible and rapid to facilitate design validation. At the pre-clinical and clinical study stage (100-1000 chips), devices must demonstrate scalability using production-grade materials and processes, with design locked to ensure consistency. For mass production (>10,000 parts), automated manufacturing becomes essential to achieve the required consistency and cost-effectiveness [84]. Beyond 20,000 parts, full automation is typically necessary to maintain quality while controlling costs.
Table 2: Manufacturing Methods for Microfluidic Devices
| Fabrication Method | Resolution | Throughput | Cost | Best Application | Key Limitations |
|---|---|---|---|---|---|
| Soft Lithography (PDMS) | High (<1 µm) | Low | Low to moderate | Prototyping, organ-on-chip models | Scalability, absorption of small molecules |
| Injection Molding | Moderate (~10 µm) | High | High (tooling) | Mass production | High initial tooling cost |
| 3D Printing | Moderate (~50 µm) | Low to moderate | Moderate | Complex geometries, customization | Surface roughness, limited material choice |
| Laser Cutting | Moderate (~20 µm) | Moderate | Low to moderate | Rapid prototyping | Material limitations |
| Photolithography | Very high (<0.5 µm) | Low | High | High-feature density chips | Complex processing, expensive |
Experimental Protocols for Regulatory Compliance
Microfluidic Device Leakage Testing Protocol
Background: Device leakage has emerged as a significant failure mode in microfluidic devices, potentially contributing to inaccurate results, cross-contamination, and device malfunction. The FDA's Microfluidics Program is developing standardized test methods and protocols for leakage testing expected to be available between 2023-2025, with a potential standard established shortly thereafter [86]. This protocol aligns with anticipated regulatory expectations.
Materials and Equipment:
- Microfluidic device(s) for testing
- Pressure source (syringe pump or pressure controller)
- Pressure sensor (0.1% full-scale accuracy recommended)
- Test fluid (deionized water or simulated biofluid)
- Collection reservoir
- Environmental chamber (if temperature control required)
- Data acquisition system
Procedure:
- Preparation: Condition devices and test fluids to standard temperature (23±2°C) unless specific use conditions dictate otherwise.
- Setup: Connect the pressure source to the device inlet and the pressure sensor to monitor internal pressure. Place outlet into collection reservoir to measure potential leakage.
- Pressure Ramp Test: Gradually increase pressure from 0 to 150% of maximum expected operating pressure (or until device failure) at a rate of 10-20 kPa/min while monitoring for leakage.
- Hold Test: Apply 110% of maximum expected operating pressure for 24 hours while monitoring pressure decay (>5% decay indicates potential leakage).
- Cyclic Fatigue Test: Subject device to 10,000 pressure cycles from 0 to 100% operating pressure at a frequency of 0.5-1 Hz.
- Analysis: Inspect for visible leakage, measure pressure decay rates, and quantify any fluid loss gravimetrically.
Acceptance Criteria: No visible leakage; pressure decay <2% during hold test; no structural failure during pressure ramp; consistent performance through cyclic testing.
Analytical Validation for Drug Screening Applications
Background: Microfluidic devices used in high-throughput drug screening must demonstrate reliability in generating concentration gradients and assessing cell viability. This protocol validates device performance for cancer drug screening applications, based on established methodologies [7].
Materials and Equipment:
- Microfluidic concentration gradient generator (MCGG) device
- Syringe pumps (minimum of 2)
- Cell culture reagents (appropriate medium, staining solutions)
- Anticancer drugs for testing
- Cell viability assay kit (e.g., MTT, Calcein-AM)
- Microscopy system for analysis
- Statistical analysis software
Procedure:
- Device Priming: Prime all microfluidic channels with appropriate buffer or culture medium to remove air bubbles and condition surfaces.
- Gradient Verification:
- Prepare two solutions: buffer and drug solution at maximum concentration.
- Infuse simultaneously at determined flow rates (typically 1-10 µL/min).
- Collect output from different gradient outlets and measure concentration using appropriate analytical method (HPLC, fluorescence, etc.).
- Compare measured concentrations to theoretical values.
- Cell-based Validation:
- Seed appropriate cancer cells in device chambers or in separate plates for exposure to device-generated concentrations.
- Apply drug gradients generated by device to cells for predetermined exposure time.
- Assess cell viability using standardized assay.
- Compare results to conventional dilution methods.
- Data Analysis:
- Calculate IC50 values for tested drugs.
- Determine coefficient of variation for replicate measurements.
- Assess linearity of dose-response relationships.
Acceptance Criteria: Generated concentrations within ±10% of theoretical values; IC50 values within ±15% of reference method; coefficient of variation <15% for replicate measurements; linear dose-response with R² >0.95.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Microfluidic Device Development and Testing
| Material/Category | Function | Examples | Key Considerations |
|---|---|---|---|
| Elastomers | Device fabrication; flexible substrates | PDMS, Ecoflex | Biocompatibility, gas permeability, solvent resistance [63] |
| Thermoplastics | Mass-produced device components | COP, PMMA, PS | Optical properties, biocompatibility, manufacturing scalability [84] [7] |
| Hydrogels | 3D cell culture; tissue barriers | PEG, alginate, PAA, Matrigel | Porosity, mechanical properties, biochemical functionality [63] |
| Surface Modifiers | Control surface properties; prevent fouling | PEG-silanes, pluronics, BSA | Stability, impact on assay components, uniformity |
| Biosensors | Analytic detection; real-time monitoring | Fluorescent probes, electrochemical sensors, SPR chips | Compatibility with detection system, stability, sensitivity |
| Validation Reagents | Performance verification | Reference standards, control materials | Traceability, stability, commutability |
Workflow Visualization
Regulatory Pathway for Microfluidic Devices
Standardization Implementation Framework
The successful clinical translation of microfluidic devices for high-throughput drug discovery requires meticulous attention to evolving regulatory expectations and standardization initiatives. By integrating compliance strategies early in the development process—from material selection and manufacturing scalability to comprehensive performance validation—researchers can navigate the complex pathway from prototype to approved product more efficiently. The experimental protocols provided herein offer practical methodologies for addressing key regulatory concerns, particularly device integrity and analytical reliability.
Future directions in microfluidic regulatory science will likely include increased standardization of organ-on-chip platforms following the January 2025 roadmap, implementation of the FDA's leakage testing protocols once finalized, and greater harmonization of international requirements through programs like MDSAP. Additionally, the integration of artificial intelligence for quality control and data analysis presents both opportunities and regulatory considerations that will shape the next generation of microfluidic devices for drug discovery. By proactively addressing these regulatory and standardization considerations, researchers can accelerate the translation of innovative microfluidic technologies from bench to bedside, ultimately enhancing the efficiency and effectiveness of drug development pipelines.
The pharmaceutical industry is undergoing a significant transformation, driven by the integration of microfluidic technologies into the drug discovery pipeline. These systems, which manipulate fluids at the microscale, have evolved from academic curiosities to essential tools that address critical inefficiencies in traditional drug development. With nearly 90% of clinical trial candidates failing to reach FDA approval, the industry faces immense pressure to improve predictive accuracy in preclinical stages [89]. Microfluidic platforms answer this challenge by providing human-relevant models that bridge the gap between animal studies and human clinical outcomes, enabling more confident decision-making before committing to costly clinical trials.
The commercial landscape for microfluidic systems has expanded dramatically, with the global market projected to grow from USD 41.92 billion in 2025 to approximately USD 73.85 billion by 2030, representing a compound annual growth rate (CAGR) of ~11.99% [90]. This growth is fueled by the technology's ability to perform high-throughput screening with minimal reagent consumption, create physiologically relevant organ-on-a-chip models, and enable personalized medicine approaches through patient-derived tissue cultures. This review examines the commercial systems demonstrating tangible impact, their experimental protocols, and the quantitative evidence supporting their adoption across the pharmaceutical industry.
Commercially Available Platforms and Their Impact
Integrated Organ-on-a-Chip Workstations
Self-contained organ-on-a-chip workstations represent the most advanced commercial microfluidic platforms for drug discovery. These systems integrate microfluidic culture, environmental control, and real-time imaging into unified workflows that generate human-relevant data at scales suitable for industrial application.
The AVA Emulation System (Emulate) exemplifies this category as the first self-contained workstation designed specifically for organ-on-a-chip applications. The platform supports up to 96 simultaneous Organ-Chip Emulations, dramatically increasing throughput while reducing the cost per sample by more than 75% compared to earlier systems [89]. This scalability addresses one of the most significant historical barriers to adoption in pharmaceutical settings. The system's impact is demonstrated through its inclusion in the FDA's ISTAND program after a landmark 2022 study showed its Liver-Chip could accurately predict drug-induced liver injury—a major cause of clinical trial failures and post-market withdrawals [89]. Pharmaceutical companies like Moderna have utilized this platform to pre-screen lipid nanoparticles for safety, demonstrating its utility in accelerating development timelines for novel therapeutic modalities.
Another impactful system is the automated microfluidic platform for tumor organoid culture described in Nature Communications, which enables dynamic and combinatorial drug screening of patient-derived samples [71]. This system addresses the technical challenges of working with temperature-sensitive matrices like Matrigel through a unique two-part, valve-less design that prevents clogging while accommodating large organoids (up to 500μm diameter). The platform's ability to maintain 200 individual culture wells under 20 independently controlled experimental conditions has proven particularly valuable for personalized oncology applications, where tumor organoids from individual patients can be screened against numerous treatment regimens simultaneously [71].
Partnership-Driven Innovation Platforms
Beyond standalone commercial systems, collaborative partnerships between pharmaceutical companies and microfluidics specialists are producing next-generation platforms tailored to specific drug discovery challenges.
The Pfizer-Neofluidics partnership is developing a first-of-its-kind microfluidic platform to study dynamic PK and PD profiles in vitro [91]. This system aims to overcome the limitations of static culture systems by simulating human pharmacokinetic profiles, allowing researchers to answer critical questions about how long a molecule needs to stay above a certain exposure level to be effective, and how to tailor molecular properties to achieve desired exposure profiles [91]. Such capabilities represent a potential game-changer for optimizing dosing regimens before advancing to animal studies or human trials.
These partnership-driven platforms often incorporate advanced fluid control systems with programmable solenoid valves and custom software that enable complex, temporal drug exposure profiles impossible to achieve with traditional well-plate formats. The ability to model human drug PK profiles in a laboratory setting provides unprecedented control, reduces uncertainty, and improves experimental efficiency—factors that collectively address the pharmaceutical industry's need for more predictive preclinical models [91].
Table 1: Commercial Microfluidic Platforms for Drug Discovery
| Platform/System | Key Features | Throughput | Primary Applications | Demonstrated Impact |
|---|---|---|---|---|
| AVA Emulation System (Emulate) | Integrated environmental control, real-time imaging, automated workflows | 96 simultaneous organ-chip emulations | Liver toxicity testing, drug safety assessment | 75% reduction in cost per sample; FDA ISTAND program qualification [89] |
| Automated Tumor Organoid Platform | Valve-less design, Matrigel compatibility, dynamic fluid control | 200 culture wells, 20 experimental conditions | Personalized oncology, combination therapy screening | Successful sequential drug screening on pancreatic tumor organoids [71] |
| Pfizer-Neofluidics Platform | Dynamic PK/PD profiling, programmable exposure regimens | Not specified | Pharmacokinetic optimization, dose regimen selection | Enables simulation of human PK profiles before animal studies [91] |
Quantitative Impact Assessment
The adoption of microfluidic systems in drug discovery is delivering measurable improvements across key development metrics. Industry data indicates that microfluidic-enabled workflows can accelerate early-stage drug testing processes by approximately 40% while generating significant cost savings through reduced reagent consumption and higher throughput [92]. The quantitative benefits extend beyond speed and efficiency to improved predictive accuracy, which has far greater implications for overall development success.
In personalized therapeutic applications, microfluidic systems have demonstrated a 25% increase in personalized treatment plans based on their ability to analyze individual genetic profiles or patient-derived tissue samples to customize drug regimens [92]. This capability is particularly valuable in oncology, where platforms capable of dynamic drug screening have revealed that temporally-modified drug treatments can be more effective than constant-dose monotherapy or combination therapy in vitro [71]. Such findings would be extremely difficult to discover using traditional screening methods.
The commercial impact is further evidenced by market growth projections across specific application segments. The point-of-care diagnostics segment, heavily reliant on microfluidic technologies, shows a 30% reduction in diagnostic turnaround time and a 20% decrease in testing costs [92]. Meanwhile, the organ-on-chip segment is poised for substantial expansion as these systems become increasingly integrated into standard preclinical workflows, with the broader microfluidics market anticipated to reach USD 110.40 billion by 2034, according to Precedence Research [90].
Table 2: Quantitative Impact of Microfluidic Systems in Drug Discovery
| Performance Metric | Traditional Methods | Microfluidic-Enabled Approach | Improvement | Source |
|---|---|---|---|---|
| Early-stage testing timeline | Baseline | Accelerated processes | ~40% acceleration | [92] |
| Personalized treatment planning | Standard regimens | Patient-specific optimization | 25% increase in personalized plans | [92] |
| Diagnostic turnaround time | Centralized lab testing | Point-of-care testing | 30% reduction | [92] |
| Diagnostic testing costs | Conventional methods | Microfluidic POC devices | 20% cost reduction | [92] |
| Cost per organ-chip sample | Early-generation systems | AVA Emulation System | >75% reduction | [89] |
Experimental Protocols and Methodologies
Protocol: Automated Tumor Organoid Screening
The following protocol adapts the methodology from the Nature Communications automated microfluidic platform for dynamic drug screening of tumor organoids [71]:
Research Reagent Solutions and Essential Materials:
- Patient-derived tumor tissue: Source material for organoid generation
- Matrigel: Extracellular matrix for 3D organoid culture
- Organoid culture medium: Cell-type specific nutrient medium with growth factors
- Drug compounds: Lyophilized or concentrated stock solutions
- Viability assay reagents: Fluorescent markers (e.g., Calcein-AM, propidium iodide)
- Microfluidic device: Two-part chamber chip (200-well array) and multiplexer control device
- Programmable microscope: With environmental chamber for continuous imaging
Procedure:
- Organoid Preparation: Dissociate patient-derived tumor tissue into single cells and suspend in Matrigel at a concentration of 500-1000 cells/μL. Pipette 2μL droplets of the cell-Matrigel suspension into each well of the microfluidic chamber device.
- Device Assembly: Align the fluidic channel layer over the chamber array and secure using the clamping system. Connect the assembled device to the multiplexer control system.
- Culture Establishment: Program the multiplexer to perfuse organoid culture medium through all channels at 50μL/hour. Place the entire system in the programmable microscope environmental chamber (37°C, 5% CO₂) and culture for 5-7 days until organoids reach 200-400μm diameter.
- Drug Treatment Programming: Prepare drug solutions at 100x final concentration. Program the multiplexer software to deliver desired concentration gradients, combinations, or temporal sequences to different channel subsets. For sequential treatments, program switching times based on preliminary PK data.
- Real-time Viability Monitoring: Acquire phase contrast and fluorescence images every 6 hours using automated microscopy. Use multipoint imaging to cover all 200 wells. Analyze organoid size, morphology, and viability marker fluorescence.
- Endpoint Analysis: After 72-120 hours of treatment, disassemble the chamber device and harvest organoids for secondary analysis (genomics, histology, etc.) by carefully extracting Matrigel plugs from individual wells.
Protocol: Liver-Chip Toxicity Assessment
This protocol summarizes the approach used with commercial liver-chip systems for predictive toxicity screening [89]:
Research Reagent Solutions and Essential Materials:
- Primary human hepatocytes: Drug metabolism functionality
- Liver sinusoidal endothelial cells: Vascular interface
- Chip-specific culture media: Separate formulations for parenchymal and vascular channels
- Test compounds: 1000x stock solutions in DMSO
- Cytotoxicity assay reagents: LDH, ATP content, albumin secretion kits
- Liver-Chip devices: Commercial chips (e.g., Emulate Liver-Chip) or equivalent
- Perfusion system: Automated fluid handling with precise flow control
Procedure:
- Chip Seeding: Introduce primary human hepatocytes into the parenchymal channel at 6×10⁶ cells/mL density. After 4-6 hour attachment, seed liver sinusoidal endothelial cells into the vascular channel at 2×10⁶ cells/mL density.
- Tissue Maturation: Perfuse both channels with appropriate media at 30-60μL/hour for 5-7 days to establish mature tissue phenotypes and stable barrier function.
- Compound Exposure: Dilute test compounds to therapeutic concentrations (typically 1-100μM) in culture medium. Perfuse compounds through the vascular channel for 7 days, maintaining vehicle controls in parallel chips.
- Biomarker Sampling: Collect effluent daily from the vascular channel for biomarker analysis (albumin, urea, LDH). Sample volume should not exceed 20% of total channel volume.
- Viability Assessment: At day 7, measure intracellular ATP content using bioluminescence assays. Perform immunostaining for tissue architecture markers (ZO-1, albumin) and damage markers (cleaved caspase-3).
- Data Analysis: Compare all treated chips to vehicle controls using standardized effect size calculations. Compounds showing >50% reduction in albumin secretion with >2-fold increase in LDH release are flagged as hepatotoxic.
Implementation Workflows
The integration of commercial microfluidic systems follows structured workflows that maximize their predictive value while ensuring operational efficiency. The following diagram illustrates the standard operational workflow for microfluidic-based drug screening:
Diagram 1: Microfluidic Drug Screening Workflow. This standardized workflow enables systematic compound evaluation from tissue establishment to data-driven decisions.
For organ-on-chip systems specifically, the experimental workflow incorporates additional steps for tissue-functional validation:
Diagram 2: Organ-on-Chip Experimental Workflow. This specialized workflow emphasizes functional validation before experimental use, ensuring physiological relevance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of microfluidic systems requires specific research reagents and materials optimized for microscale environments. The following table details essential components:
Table 3: Essential Research Reagents and Materials for Microfluidic Drug Discovery
| Reagent/Material | Function/Application | Key Considerations | Commercial Sources/Examples |
|---|---|---|---|
| PDMS (Polydimethylsiloxane) | Device fabrication, rapid prototyping | Gas permeability, absorbs small molecules | Sylgard 184 (Dow), RTV615 (Momentive) |
| Thermoplastic Polymers | Mass-produced devices (COP, COC, PMMA) | Optical clarity, chemical resistance | Zeonor (COP), Topas (COC), PMMA |
| Extracellular Matrices | 3D cell culture support | Batch variability, temperature sensitivity | Matrigel (Corning), Collagen I, Fibrin |
| Primary Human Cells | Physiologically relevant models | Donor variability, limited expansion | Commercial vendors (Lonza, PromoCell) |
| Microfluidic Perfusion Media | Continuous nutrient delivery | Optimized for flow conditions, reduced evaporation | Custom formulations (Gibco, Thermo) |
| Oxygen-Sensitive Probes | Microenvironment monitoring | Compatibility with imaging systems | Image-iT (Thermo), Luxcel probes |
| Programmable Solenoid Valves | Fluidic control and automation | Precision, response time, reliability | Bio-Chem Fluidics, The Lee Company |
| Organ-Chip Specific Antibodies | Tissue characterization | Validation under flow conditions | Commercial (Abcam, R&D Systems) with chip validation |
The commercial adoption of microfluidic systems in drug discovery is transitioning from specialized applications to mainstream implementation. Current trends indicate several key directions for future development. AI-driven design and analysis is emerging as a powerful combination, with machine learning algorithms increasingly used to optimize device geometries and analyze complex phenotypic data [90] [23]. The integration of microfluidics with electronic sensors and actuators will enable more sophisticated real-time monitoring of tissue barrier function and metabolic activity [90]. Additionally, regulatory acceptance continues to grow, with platforms like the Emulate Liver-Chip achieving inclusion in the FDA's ISTAND program, paving the way for broader qualification of microfluidic systems as recognized drug development tools [89].
The long-term trajectory points toward increasing automation and accessibility, with systems becoming more user-friendly while supporting increasingly complex biological models. Between 2035 and 2050, the market is projected to reach USD 250-400 billion, with strong uptake across pharmaceutical, diagnostic, and environmental applications [90]. As these systems become more integrated with digital platforms and data analytics, they will likely evolve from specialized tools to central components in a connected drug discovery ecosystem.
In conclusion, commercial microfluidic systems have demonstrated tangible impact through improved predictive accuracy, accelerated timelines, and cost reduction. Platforms for organ-on-chip applications, tumor organoid screening, and PK/PD modeling are generating human-relevant data that informs critical development decisions. While challenges remain in standardization and implementation complexity, the continued evolution of these systems promises to reshape drug discovery paradigms, ultimately contributing to more efficient development of safer, more effective therapeutics.
Conclusion
Microfluidic technology has unequivocally established itself as a cornerstone of modern, high-throughput drug discovery. By enabling precise manipulation of fluids at the microscale, these systems offer unparalleled advantages in speed, cost-efficiency, and biological relevance over traditional methods. The integration of advanced platforms like organ-on-chip models and droplet generators is paving the way for more physiologically accurate screening and the advancement of personalized medicine. Future progress hinges on overcoming material limitations, streamlining mass production, and fostering greater integration with artificial intelligence for data analysis and experimental design. As these innovations converge, microfluidics is poised to dramatically accelerate the entire pharmaceutical development pipeline, from initial screening to clinical application, ultimately delivering safer and more effective therapies to patients faster.
References
- 1. Revolutionizing drug discovery and development [https://japsonline.com/abstract.php?article_id=4605&sts=2]
- 2. Microfluidics: A general overview of microfluidics [https://elveflow.com/microfluidic-reviews/a-general-overview-of-microfluidics/]
- 3. Microfluidics in biomedicine: Heart-on-chip platforms for ... [https://www.sciencedirect.com/science/article/abs/pii/S177322472500574X]
- 4. Microfluidics for Drug Discovery and Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC2700821/]
- 5. Microfluidic Drug Discovery [https://www.fluigent.com/microfluidic-oem/applications/drug-discovery/]
- 6. Laminar flow and capillary flow in microfluidic chips [https://elveflow.com/microfluidic-reviews/laminar-flow-capillary-flow/]
- 7. Microfluidic device for high-throughput cancer drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725103537]
- 8. Diffusion Mechanism - an overview [https://www.sciencedirect.com/topics/engineering/diffusion-mechanism]
- 9. Microfluidic cell chips for high-throughput drug screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4870726/]
- 10. Microfluidics in High-Throughput Drug Screening: Organ- ... [https://www.mdpi.com/2079-6374/14/1/55]
- 11. Understanding Capillarity in Physics and Its Applications [https://www.ai-futureschool.com/en/physics/understanding-capillarity-in-physics.php]
- 12. Capillary Force - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/capillary-force]
- 13. The Evolution of High - Throughput Screening in Drug Discovery [https://www.linkedin.com/pulse/evolution-high-throughput-screening-drug-discovery-pavan-kumar-puram-3w4wc]
- 14. Origin and evolution of high screening - PMC throughput [https://pmc.ncbi.nlm.nih.gov/articles/PMC1978279/]
- 15. High content screening in microfluidic devices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3156449/]
- 16. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 17. Active-matrix digital microfluidics for high-throughput ... [https://www.nature.com/articles/s44287-025-00230-1]
- 18. High throughput fluorescence imaging approaches for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4863443/]
- 19. Hypothesis Testing in High-Throughput Screening for Drug ... [https://www.sciencedirect.com/science/article/pii/S2472555222076304]
- 20. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 21. Microfluidics drug discovery and biomedical research [https://microfluidics-innovation-center.com/reviews/advances-in-microfluidics-drug-discovery-and-biomedical-research/]
- 22. Transforming Drug Discovery with Miniaturized Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944397/]
- 23. Microfluidics in 2025: Applications, Trends & How It Work [https://eden-microfluidics.com/news-events/microfluidics-overview/]
- 24. Microfluidic technologies for drug discovery and development [https://www.sciencedirect.com/science/article/abs/pii/S0165614721000791]
- 25. A Microfluidics-Based Ultrahigh-Throughput Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489886/]
- 26. Microfluidics Statistics and Facts (2025) [https://media.market.us/microfluidics-statistics/]
- 27. Microfluidics Market Size & Growth Forecast to 2029 [https://www.marketsandmarkets.com/Market-Reports/microfluidics-market-1305.html]
- 28. 2025 life sciences outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-life-sciences-executive-outlook.html]
- 29. Microfluidic Devices for Drug Delivery Systems and Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5852599/]
- 30. High throughput screening in modern drug discovery [https://www.drugdiscoverynews.com/high-throughput-screening-in-modern-drug-discovery-16695]
- 31. Identifying Actives from HTS Data Sets: Practical ... [https://www.sciencedirect.com/science/article/pii/S2472555222077371]
- 32. Top High Throughput Screening Software for Labs | Trends [https://www.scispot.com/blog/top-high-throughput-screening-software-for-labs]
- 33. A User Guide for High-Throughput Workflows - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10722570/]
- 34. A comprehensive review of concentration gradient ... [https://www.sciencedirect.com/science/article/abs/pii/S0255270125003046]
- 35. 3D microfluidic gradient generator for combination ... [https://www.nature.com/articles/s41378-020-00200-7]
- 36. A high-throughput flowless microfluidic single and multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11338633/]
- 37. Multi-layered Microfluidic Drug Screening Platform ... [https://link.springer.com/article/10.1007/s13206-024-00154-2]
- 38. Dose-response characterization: A key to success in drug ... [https://pubmed.ncbi.nlm.nih.gov/40626332/]
- 39. State-of-the-art in high throughput organ-on-chip for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149869/]
- 40. PhysioMimix® Core Microphysiological System MPS [https://cn-bio.com/physiomimix-core/]
- 41. Using Organ-on-a-Chip Technology to Unlock Patient ... [https://emulatebio.com/using-organ-on-a-chip-technology-to-unlock-patient-derived-precision-medicine/]
- 42. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 43. September 19, 2025: Human Organ Chip Models for ... [https://sites.nicholas.duke.edu/envhealth/seminars-symposia/fall-2025-seminar-series/september-19-2025-human-organ-chip-models-for-nephrotoxicity-screening-and-biomedical-applications/]
- 44. Droplet Microfluidics for Advanced Single‐Cell Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11970111/]
- 45. Droplet-based digital PCR (ddPCR) and its applications [https://www.sciencedirect.com/science/article/abs/pii/S0165993622003806]
- 46. Microfluidic Devices for Drug Assays [https://www.mdpi.com/2571-5135/7/2/18]
- 47. Droplet-Based Microfluidics : An Intuitive Design Guideline [https://eden-microfluidics.com/news-events/droplet-based-microfluidics-a-design-guideline/]
- 48. Droplets microfluidics platform—A tool for single cell research [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1121870/full]
- 49. Recent advances in droplet microfluidics for single-cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993623000195]
- 50. Advances in nanoparticle synthesis assisted by microfluidics [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00194c]
- 51. Harnessing Microfluidics for the Effective and Precise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566220/]
- 52. Microfluidic Manufacture of Lipid-Based Nanomedicines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9506151/]
- 53. Recent Advances in Antibody Discovery Using Ultrahigh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293579/]
- 54. Properties and Applications of PDMS for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8788510/]
- 55. The Assessment of Bioactivity and Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471625/]
- 56. Polydimethylsiloxane as a more biocompatible alternative ... [https://www.nature.com/articles/s41598-023-43297-2]
- 57. Polymers, Volume 17, Issue 22 (November-2 2025) [https://www.mdpi.com/2073-4360/17/22]
- 58. low-cost and rapid-iteration microfabrication for biology [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00181a]
- 59. Articles in 2025 | Polymer Journal [https://www.nature.com/pj/articles?year=2025]
- 60. From Soft Lithography to 3D Printing: Current Status and ... [https://www.mdpi.com/2073-4360/17/4/455]
- 61. Advancements and challenges in SLA-based microfluidic ... [https://www.sciencedirect.com/science/article/pii/S0264127525006744]
- 62. Overcoming Challenges in Point of Care Diagnostics [https://eden-microfluidics.com/news-events/flexdym-overcoming-challenges-in-point-of-care-diagnostics/]
- 63. Microfluidic technologies for wearable and implantable ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00499c]
- 64. The impact of microfluidics in high-throughput drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9142169/]
- 65. The Impact of Polydimethylsiloxane (PDMS) in Engineering [https://www.mdpi.com/2311-5521/10/2/41]
- 66. PDMS: The Versatile Polymer for Microfluidic Chips [https://elveflow.com/microfluidic-reviews/the-polydimethylsiloxane-pdms-and-microfluidics/]
- 67. Recent Progress in PDMS-Based Microfluidics Toward ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852457/]
- 68. Comparison of PDMS and NOA Microfluidic Chips [https://www.mdpi.com/2072-666X/14/11/2033]
- 69. How to Perform a Microfluidic Cultivation Experiment—A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8699335/]
- 70. Air bubbles and microfluidics, how to deal with it [https://elveflow.com/microfluidic-reviews/air-bubbles-and-microfluidics/]
- 71. Automated microfluidic platform for dynamic and ... [https://www.nature.com/articles/s41467-020-19058-4]
- 72. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 73. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 74. Top Drug Discovery Software Solutions to Watch in 2025 [https://www.deepmirror.ai/post/top-drug-discovery-software-solutions-to-watch-in-2025]
- 75. Recent advances in microfluidics for drug screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6870548/]
- 76. Microfluidics for High Throughput Screening of Biological ... [https://link.springer.com/article/10.1007/s44174-024-00169-1]
- 77. Benchmarking compound activity prediction for real-world ... [https://www.nature.com/articles/s42004-024-01204-4]
- 78. Recent Development of Drug Delivery Systems through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8880124/]
- 79. Determination of Half-Maximal Inhibitory Concentration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489899/]
- 80. In-cell Western Assays for IC50 Determination [https://azurebiosystems.com/blog/in-cell-western-assays-for-ic50-determination/]
- 81. Microfluidic Devices Market Size and Trends Report, 2032 [https://www.psmarketresearch.com/market-analysis/microfluidic-devices-market]
- 82. High Throughput Screening Market Size, Share Report [https://www.thebusinessresearchcompany.com/report/high-throughput-screening-hts-global-market-report]
- 83. Emerging Trends in Microfluidics [https://elveflow.com/microfluidic-reviews/emerging-trends-in-microfluidics/]
- 84. Perspectives in translating microfluidic devices from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8933055/]
- 85. The Regulatory Landscape and Future Outlook of ... [https://www.regulatorymedicaldevice.com/2025/03/Microfluidic-Based-Diagnostic-Devices.html]
- 86. FDA Developing New Regulatory Tool for Screening ... [https://www.exponent.com/article/fda-developing-new-regulatory-tool-screening-microfluidics-devices]
- 87. Setting out a roadmap for standardisation of organ-on-chip ... [https://joint-research-centre.ec.europa.eu/jrc-news-and-updates/setting-out-roadmap-standardisation-organ-chip-technology-2025-01-13_en]
- 88. Microfluidic Devices Market Outlook: Regulations, Smart ... [https://www.linkedin.com/pulse/microfluidic-devices-market-outlook-regulations-smart-seldc/]
- 89. Ushering in a New Era of Human-Relevant Drug Discovery [https://emulatebio.com/insights-into-the-ava-emulation-system-ushering-in-a-new-era-of-human-relevant-drug-discovery/]
- 90. The Microfluidic device industry: Growth outlook 2025 – 2050 [https://www.medicalmicromolding.com/the-microfluidic-device-industry-growth-outlook-2025-2050/]
- 91. How an Advance in Microfluidics Can Speed Up Drug ... [https://www.pfizer.com/news/articles/better_faster_smaller_how_an_advance_in_microfluidics_can_speed_up_drug_discovery]
- 92. Microfluidic Devices in the Real World: 5 Uses You'll ... [https://www.linkedin.com/pulse/microfluidic-devices-real-world-5-uses-youll-actually-see-yddee/]