Strategies for Enhancing Nanoparticle Structural Stability in Systemic Circulation: A Comprehensive Guide for Drug Development
This article provides a comprehensive examination of strategies to improve the structural stability of nanoparticles during systemic circulation, a critical factor for successful drug delivery.
Strategies for Enhancing Nanoparticle Structural Stability in Systemic Circulation: A Comprehensive Guide for Drug Development
Abstract
This article provides a comprehensive examination of strategies to improve the structural stability of nanoparticles during systemic circulation, a critical factor for successful drug delivery. Targeted at researchers, scientists, and drug development professionals, it explores the fundamental principles governing nanoparticle stability, advanced engineering methodologies, systematic optimization approaches, and rigorous validation techniques. The content synthesizes current scientific understanding with practical applications, addressing key challenges such as protein corona formation, biological barrier navigation, and maintaining colloidal integrity to enhance therapeutic efficacy and safety profiles of nanomedicines.
Understanding Nanoparticle Stability: Fundamental Principles and Circulation Challenges
Defining Nanoparticle Stability in Physiological Environments
For researchers in drug development, defining and ensuring nanoparticle stability in physiological environments is a critical hurdle in translating nanomedicines from the lab to the clinic. Stability here extends beyond simple aggregation resistance; it encompasses the preservation of structural integrity, surface functionality, and therapeutic payload throughout systemic circulation to achieve the desired biodistribution and efficacy. This guide addresses common challenges and provides targeted troubleshooting strategies to improve nanoparticle performance in circulation research.
Troubleshooting Guides & FAQs
Troubleshooting Common Stability Issues
This section addresses frequent problems encountered when testing nanoparticles in biological media.
Problem 1: Rapid Aggregation in Physiological Buffers Nanoparticles are stable in pure water but aggregate immediately upon addition to phosphate-buffered saline (PBS) or cell culture media.
| Possible Cause | Investigation | Solution |
|---|---|---|
| Insufficient steric stabilization | Measure hydrodynamic size & PDI via DLS in water vs. PBS [1]. | Introduce a dense PEG coating to provide steric hindrance [1] [2]. |
| Low surface charge magnitude | Measure zeta potential. A value between -10 mV and +10 mV indicates poor electrostatic stabilization [3]. | Modify surface chemistry to increase charge. Aim for a zeta potential magnitude > 20 mV for moderate stability [3]. |
| Surface protein fouling | Incubate with serum, then re-measure size and zeta potential [1]. | Use higher density or different topology (e.g., cyclic) PEG coatings to better resist protein adsorption [1] [2]. |
Problem 2: Short Systemic Circulation Lifetime Nanoparticles are cleared rapidly from the blood in in vivo models, limiting tumor accumulation.
| Possible Cause | Investigation | Solution |
|---|---|---|
| Protein corona formation | Isolate nanoparticles after blood contact and analyze corona composition via proteomics [4]. | Tune nanoparticle elasticity; intermediate elasticity (75-700 kPa) favors adsorption of ApoA1, which correlates with longer circulation [4]. |
| Surface charge is too positive | Measure zeta potential at physiological pH. | Aim for a neutral or slightly negative surface charge to reduce non-specific cellular uptake [1] [5]. |
| Poor stealth coating stability | Use a ligand exchange or encapsulation method that forms a stable, covalent bond with the nanoparticle core (e.g., siloxane bonds) [1]. | Optimize surface chemistry for a dense, stable PEG layer to minimize opsonization and macrophage uptake [1] [6]. |
Problem 3: Loss of Functionality After Surface Modification Targeting ligands (e.g., antibodies, peptides) lose activity or become masked after conjugation.
| Possible Cause | Investigation | Solution |
|---|---|---|
| Non-specific protein adsorption | Test binding to the target antigen in a serum-free buffer vs. serum-containing media. | Use efficient blocking agents (e.g., BSA) and high-density PEG spacers to minimize non-specific binding [7]. |
| Improper conjugation chemistry | Use techniques like FTIR or fluorescence tagging to confirm ligand attachment [1]. | Employ controlled, site-specific conjugation chemistries (e.g., thiol-maleimide) and avoid EDC crosslinking when both amine and carboxyl groups are present to prevent crosslinking [1] [7]. |
| Aggregation during conjugation | Monitor hydrodynamic size before and after each conjugation step [7]. | Optimize the antibody-to-nanoparticle ratio and maintain an optimal pH (often 7-8) during conjugation [7]. |
Frequently Asked Questions (FAQs)
Q1: What does "nanoparticle stability" truly mean in the context of physiological environments? It is a multi-faceted concept. Beyond just resisting aggregation, it includes [8]:
- Chemical Stability: The core composition and crystal structure must not degrade.
- Surface Stability: The surface chemistry, charge, and conjugated ligands must remain functional and unaltered.
- Functional Stability: The nanoparticle's ability to deliver its payload to the intended target must be preserved throughout its circulation time.
Q2: How can I accurately monitor nanoparticle stability in my experiments? A combination of techniques is essential. The table below outlines key methods.
Table: Key Techniques for Monitoring Nanoparticle Stability
| Technique | What It Measures | Application in Stability Testing |
|---|---|---|
| Dynamic Light Scattering (DLS) | Hydrodynamic diameter and Polydispersity Index (PDI) [9] [3] | Track size increase over time in biological media to monitor aggregation [1] [3]. |
| Zeta Potential | Surface charge and colloidal stability [3] | A stable zeta potential in serum indicates resistance to protein fouling. A shift towards zero suggests instability [1]. |
| UV-Vis Spectroscopy | Optical properties (for plasmonic NPs) [3] | A shift or broadening of the plasmon peak indicates aggregation [2]. |
| Transmission Electron Microscopy (TEM) | Core size, shape, and morphology [3] | Confirm DLS data and visually identify aggregation or changes in core structure [1]. |
Q3: My nanoparticles are stable in PBS but aggregate in cell culture media. Why? Cell culture media contains ions and proteins. ions can neutralize surface charge (reducing electrostatic stabilization), and proteins can adsorb to the surface, bridging particles together. Enhancing steric stabilization with a robust PEG layer is the most effective countermeasure [1] [8].
Q4: How does nanoparticle elasticity influence blood circulation time? A non-monotonic relationship exists. Nanoparticles with intermediate elasticity (e.g., ~75 kPa to 700 kPa) have shown the longest circulation lifetimes. This is because their elasticity influences the composition of the protein corona that forms upon entering the blood, specifically enriching in apolipoprotein A-I (ApoA1), which is associated with reduced macrophage uptake and prolonged circulation [4].
Experimental Protocols & Methodologies
Core Protocol: Engineering Hydrophilic, Functionalized Iron Oxide Nanoparticles
This protocol, based on a published approach, details the creation of nanoparticles with long-term stability in biological media [1].
1. Ligand Exchange with Triethoxysilylpropylsuccinic Anhydride (SAS)
- Starting Material: Begin with oleic acid-coated iron oxide nanoparticles (NP-OA) synthesized via thermal decomposition.
- Reaction: Disperse NP-OA in anhydrous toluene. Add triethoxysilylpropylsuccinic anhydride (SAS) and react under inert atmosphere with stirring.
- Mechanism: The anhydride group of SAS binds to the nanoparticle surface, displacing oleic acid. Concurrently, ethoxysilane groups hydrolyze and condense, forming a cross-linked siloxane network that anchors the coating to the surface.
- Purification: Precipitate the resulting SAS-coated nanoparticles (NP-SAS) and wash with ethanol to remove unreacted species.
2. PEGylation via EDC Coupling
- Reaction: Disperse NP-SAS in MES buffer. Add amine-functionalized PEG (MW = 2,000 Da) and N,N'-dicyclohexylcarbodiimide (DCC) as a coupling agent.
- Mechanism: DCC activates the free carboxyl groups on the NP-SAS surface, enabling the formation of amide bonds with the terminal amines of the PEG chains.
- Purification: Dialyze the final product (NP-SAS-PEG-NH2) extensively against water to remove coupling reagents and unbound PEG.
3. Validation and Stability Assessment
- Confirm Coating: Use FTIR to verify the disappearance of oleic acid peaks and the appearance of characteristic siloxane (~1031 cm⁻¹) and PEG (C-O-C, ~1112 cm⁻¹) bands [1].
- Quantify Functionality: Use a colorimetric assay (e.g., with SPDP) to quantify the number of surface amine groups (approximately 70 per nanoparticle was reported) [1].
- Test Stability: Incubate NP-SAS-PEG-NH2 in PBS, DMEM+10% FBS, and pure FBS. Monitor the hydrodynamic size by DLS for at least 15 days. Stable nanoparticles will show no significant size increase or precipitation [1].
Methodology: Investigating the Elasticity-Protein Corona Relationship
This methodology outlines how to isolate and study the effect of nanoparticle elasticity on protein corona formation and systemic circulation [4].
1. Synthesis of Core-Shell Nanoparticles with Tunable Elasticity
- Core Fabrication: Synthesize hydrogel nanoparticles (nanogels) with varying crosslinking densities (monomer-to-crosslinker ratios) to create cores with different elasticities (e.g., 75 kPa to 1700 kPa). Use bulk hydrogel measurements to assign Young's modulus.
- Shell Formation: Coat all nanogel cores with an identical PEGylated lipid bilayer (e.g., DOPC:DSPE-PEG2000, 90:10 mass ratio) to standardize surface chemistry.
- Characterization: Use Cryo-EM/TEM to confirm core-shell structure and DLS to ensure consistent hydrodynamic size and zeta potential across all samples.
2. In Vitro Protein Corona Analysis
- Incubation: Incubate a standardized amount of each nanoparticle type (differing only in core elasticity) in mouse plasma for a set time (e.g., 1 hour).
- Corona Isolation: Separate the nanoparticle-protein corona complexes from unbound plasma proteins via centrifugation and careful washing.
- Protein Identification and Quantification: Digest the corona proteins and analyze via liquid chromatography-mass spectrometry (LC-MS/MS). Identify and relatively quantify the proteins present.
3. In Vivo Circulation Lifetime Study
- Animal Model: Administer the different nanoparticle formulations to mouse models (e.g., via tail vein injection).
- Pharmacokinetic Sampling: Collect blood samples at multiple time points post-injection.
- Quantification: Measure nanoparticle concentration in blood over time using a relevant technique (e.g., fluorescence, radiolabeling, or elemental analysis for metal cores).
- Correlation: Plot systemic circulation lifetime versus nanoparticle elasticity and correlate with the relative abundance of specific corona proteins (e.g., ApoA1) identified in the in vitro study.
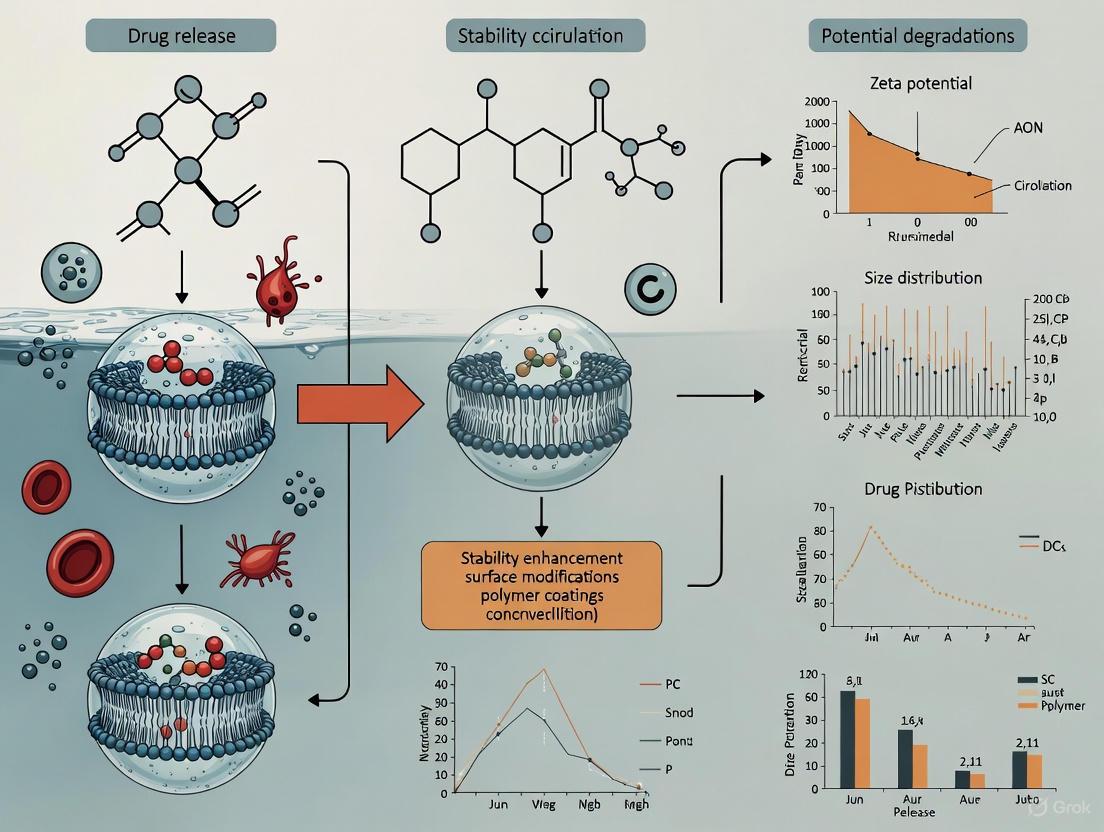
Essential Diagrams
Diagram 1: Mechanism of Nanoparticle Stabilization
Mechanism of Nanoparticle Stabilization\ This diagram illustrates the two primary mechanisms to prevent nanoparticle aggregation: creating a physical barrier with a dense PEG layer (steric stabilization) and increasing electrostatic repulsion between particles by modifying surface charge (electrostatic stabilization).
Diagram 2: Elasticity-Circulation Relationship
Elasticity-Circulation Relationship\ This flowchart shows how tuning nanoparticle elasticity to an intermediate range leads to the formation of a specific protein corona, enriched in ApoA1, which in turn promotes a longer systemic circulation lifetime.
The Scientist's Toolkit
Table: Key Research Reagents and Materials for Nanoparticle Stability
| Reagent/Material | Function in Stability Research | Key Considerations |
|---|---|---|
| Poly(ethylene glycol) (PEG) | A "stealth" polymer that provides steric hindrance, reducing protein adsorption and aggregation [1] [2]. | Density and topology (linear vs. cyclic) matter. Cyclic PEG can offer superior stability without chemisorption [2]. |
| Triethoxysilylpropylsuccinic Anhydride (SAS) | A coupling agent that forms a stable, cross-linked siloxane coating on oxide nanoparticles, providing anchor points for PEG [1]. | Creates a robust, hydrophilic base layer for further functionalization. |
| Apolipoprotein A-I (ApoA1) | A specific plasma protein whose adsorption is correlated with prolonged nanoparticle circulation [4]. | Not a reagent to add, but a biomarker to track. Enrichment on nanoparticles indicates a favorable corona. |
| Dicyclohexylcarbodiimide (DCC) | A coupling reagent used to covalently link carboxyl groups on nanoparticles to amine-functionalized PEG [1]. | Handle with care; ensures stable amide bond formation. Requires anhydrous conditions. |
| BSA (Bovine Serum Albumin) | Used as a blocking agent to passivate nanoparticle surfaces and minimize non-specific binding in assays and in vivo [7]. | A common "dysopsonin" that can help reduce uptake by immune cells [6]. |
Key Biological Barriers to Circulation Longevity
For researchers in drug development, the systemic circulation lifetime of nanoparticles (NPs) is a critical determinant of therapeutic efficacy. A longer circulation time increases the probability of NPs reaching their intended target tissue. However, a complex array of biological barriers actively works to clear these particles from the bloodstream. This guide details the primary biological hurdles and provides evidence-based troubleshooting strategies to overcome them, directly supporting the broader thesis of improving nanoparticle structural stability in circulation research.
Frequently Asked Questions (FAQs)
FAQ 1: What is the most significant biological event that determines nanoparticle circulation time? The formation of a protein corona is arguably the most critical event. Within minutes of entering the bloodstream, nanoparticles are coated by a layer of adsorbed plasma proteins. This corona defines the nanoparticle's "biological identity" to immune cells, overriding its synthetic surface properties. The composition of this corona directly influences opsonization—the process that marks the nanoparticle for clearance by phagocytic cells in the liver and spleen [4].
FAQ 2: How does nanoparticle elasticity influence their physiological fate? Recent evidence demonstrates that nanoparticle elasticity has a non-monotonic relationship with systemic circulation lifetime. This means that neither the softest nor the stiffest particles perform best. Instead, particles with intermediate elasticity (in the range of 75–700 kPa) have been shown to exhibit the longest circulation times. This is because elasticity selectively influences the adsorption of specific plasma proteins, such as apolipoprotein A-I (ApoA1), whose presence correlates strongly with prolonged circulation [4].
FAQ 3: Beyond the protein corona, what other aging-related barriers affect circulation? The integrity of the body's physiological barriers, including the endothelium that lines blood vessels, decreases with age. This is due to age-related loss of homeostasis, changes in gene expression, and morphological alterations in cells and tissues [10]. Furthermore, the aging process is associated with chronic, low-grade inflammation ("inflammaging") and immunosenescence (the decline of immune function), which can alter how the body interacts with and clears nanoparticles [11] [12].
FAQ 4: Are there biological factors more important than nanoparticle design? Yes. A large-scale study on aging revealed that lifestyle and environmental factors (e.g., smoking, physical activity, socioeconomic status) have a significantly greater impact on health and mortality than genetic predisposition. This suggests that the patient's overall health and physiological status, which are shaped by these factors, could profoundly influence the performance and distribution of nanomedicines [13].
Troubleshooting Common Experimental Issues
Problem 1: Rapid Clearance of Nanoparticles from Circulation
Potential Causes and Solutions:
Cause: Protein Corona-Induced Opsonization. The nanoparticle surface is optimized for stealth but still adsorbs opsonic proteins (e.g., immunoglobulins, complement factors) that promote phagocytosis [4].
- Solution: Re-evaluate surface chemistry and elasticity. A high-density PEGylated surface can selectively suppress the adsorption of certain plasma proteins. Furthermore, tuning nanoparticle elasticity to an intermediate range (e.g., 75-700 kPa) has been shown to promote the enrichment of ApoA1 in the corona, which is associated with longer circulation [4].
Cause: Poor Barrier Integrity in Disease Models. If using an animal model with underlying inflammation or metabolic disease, the vascular endothelium may be more "leaky" or adhesive, facilitating nanoparticle extravasation or immune cell binding.
Problem 2: High Variability in Circulation Longevity Between Batches
Potential Causes and Solutions:
- Cause: Inconsistent Nanoparticle Elasticity. Even with tight control over size and surface charge, batch-to-batch variations in core cross-linking density or material composition can lead to significant differences in elasticity, which in turn alters the protein corona and circulation fate [4].
- Solution: Implement a standardized quantitative measure of nanoparticle elasticity (e.g., Atomic Force Microscopy) as a critical quality control check before in vivo studies. Ensure your synthesis protocol produces particles with consistent mechanical properties.
Problem 3: Failure in Active Targeting
Potential Causes and Solutions:
- Cause: Protein Corona Masking. The protein corona can sterically shield targeting ligands (e.g., antibodies, peptides) conjugated to the nanoparticle surface, preventing their interaction with the intended receptor on target cells [4].
- Solution: Design the targeting strategy with the corona in mind. Consider the density and spacer length of the targeting ligands to mitigate masking effects. Pre-forming the corona in vitro with a curated protein mixture is an advanced strategy to create a more predictable biological identity.
Table 1: The Impact of Nanoparticle Elasticity on Physiological Fate
| Elasticity (Young's Modulus) | Core Composition (Example) | Key Corona Protein Observed | Relative Circulation Lifetime | Key Cellular Interaction |
|---|---|---|---|---|
| 45 kPa (Soft) | Liposome | Low ApoA1 | Short | High uptake by phagocytes |
| 75 kPa – 700 kPa (Intermediate) | Polyacrylamide Hydrogel | High ApoA1 | Longest | Reduced cellular uptake |
| 760 MPa (Stiff) | PLGA (Poly(lactic-co-glycolic acid)) | Low ApoA1 | Short | High uptake by phagocytes |
Source: Data adapted from [4]. This study used core-shell nanoparticles with an identical PEGylated lipid bilayer shell, isolating elasticity as the sole variable.
Table 2: Key Research Reagent Solutions for Circulation Studies
| Reagent / Material | Function in Experiment | Key Consideration |
|---|---|---|
| DSPE-PEG2000 | A lipid-PEG conjugate used to create a stealth ("steric stabilization") layer on nanoparticle surfaces, reducing protein adsorption and opsonization. | PEG density is critical; too low offers insufficient protection, too high can cause unexpected immune responses. |
| Apolipoprotein A-I (ApoA1) | Not a reagent, but a key biomarker. Its preferential adsorption on nanoparticles of intermediate elasticity is a strong positive indicator of prolonged circulation. | Monitor ApoA1 presence in the protein corona via techniques like SDS-PAGE or mass spectrometry as a performance marker. |
| Model Nanoparticles (Core-Shell) | Systems with a hydrogel core and lipid shell allow independent tuning of core elasticity and surface chemistry, perfect for mechanistic studies. | Ensures that differences in circulation are due to elasticity and not other physicochemical parameters [4]. |
Detailed Experimental Protocols
Protocol 1: Isolating and Analyzing the Protein Corona
Objective: To characterize the composition of the protein corona formed on nanoparticles after exposure to biological fluids, a key determinant of their biological fate [4].
Methodology:
- Incubation: Incubate a standardized concentration of your purified nanoparticles (e.g., 1 mg/mL) in mouse or human plasma (e.g., 50% v/v in PBS) for a predetermined time (e.g., 0.5 - 60 minutes) at 37°C.
- Isolation: Separate the nanoparticle-protein corona complexes from unbound proteins. This is typically achieved by centrifugation (for large/dense particles) or size-exclusion chromatography for a cleaner separation.
- Washing: Gently wash the pellet or fractions containing the complexes with a mild buffer (e.g., PBS) to remove loosely associated proteins.
- Elution & Denaturation: Dissociate the proteins from the nanoparticle surface using a denaturing buffer (e.g., Laemmli buffer for SDS-PAGE or RIPA buffer for mass spectrometry).
- Analysis:
- SDS-PAGE: For a quick profile of the total protein corona.
- Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS): For a comprehensive, quantitative identification of all adsorbed proteins and their relative abundances.
Protocol 2: Evaluating the Impact of Elasticity In Vivo
Objective: To systematically determine the relationship between nanoparticle elasticity and systemic circulation lifetime.
Methodology:
- Nanoparticle Fabrication: Synthesize a series of core-shell nanoparticles with identical size, surface charge, and surface chemistry (e.g., PEGylated lipid bilayer) but with cores of varying elasticity (e.g., from ~50 kPa to >1 GPa). Core materials can range from soft hydrogels to stiff polymers like PLGA [4].
- Characterization: Confirm that all batches are monodisperse and matched for hydrodynamic diameter and zeta potential. Measure core elasticity via Atomic Force Microscopy.
- In Vivo Tracking: Administer the nanoparticles intravenously to animal models (e.g., mice). Collect blood samples at multiple time points post-injection (e.g., 5 min, 30 min, 1h, 2h, 4h, 8h, 24h).
- Quantification: Measure nanoparticle concentration in the blood over time. This can be done by labeling particles with a fluorescent dye (e.g., DiR) and using in vivo imaging systems (IVIS) or by extracting blood and measuring fluorescence with a plate reader. Calculate pharmacokinetic parameters like half-life (t1/2).
Visualizing Key Concepts
Protein Corona Formation and Its Consequences
Experimental Workflow for Circulation Longevity Studies
The Critical Role of Protein Corona in Determining Biological Identity
Technical Support Center
Troubleshooting Guides
| Problem Description | Possible Causes | Recommended Solutions | Key References |
|---|---|---|---|
| Unexpectedly low transfection efficiency with LNPs despite high cellular uptake. | Protein corona-induced rerouting of LNPs to lysosomal degradation, compromising endosomal escape and cargo delivery [14]. | Pre-form a protein corona with specific proteins (e.g., ApoE) to promote desired intracellular trafficking. Optimize LNP surface chemistry to recruit beneficial corona proteins [14]. | Nature Communications (2025) [14] |
| Rapid clearance of nanoparticles by the immune system and short circulation time. | Opsonins (e.g., immunoglobulins, complement proteins) in the hard corona promote recognition and uptake by phagocytic cells [15] [16]. | Employ PEGylation or use surface modifications with zwitterionic groups (e.g., α-glutamyl) to create stealth properties and reduce opsonin adsorption [16]. | Biomedicines (2021) [16] |
| Inconsistent cellular targeting and unpredictable biodistribution. | Dynamic and variable composition of the protein corona, which is highly influenced by the biological medium and NP physicochemical properties [15] [17]. | Use machine learning models to predict the functional composition of the corona based on NP parameters. Standardize incubation conditions (e.g., plasma concentration, time) during pre-coating [18]. | PNAS (2020) [18] |
| Aggregation of nanoparticles in biological fluids (e.g., blood plasma). | Nanoparticle surface is screened by proteins and salts, overcoming electrostatic repulsion and leading to aggregation. This is common with citrate-capped particles [19]. | Use sterically bulky polymeric capping agents (e.g., BPEI, PEG) instead of small molecules (e.g., citrate, tannic acid) to enhance colloidal stability [19]. | nanoComposix (2018) [19] |
| Loss of catalytic or optical activity of functional nanoparticles. | Conformational changes in proteins adsorbed on the corona, or the corona itself shielding the active surface of the nanoparticle [15] [8]. | Design experiments to understand the hard corona composition. Consider engineering the corona to preserve specific active crystal facets or optical properties [15] [8]. | J. Phys. Chem. C (2019) [8] |
Frequently Asked Questions (FAQs)
Q1: What is the difference between the "hard" and "soft" protein corona, and which one is more critical for determining biological identity?
The hard corona is a tightly bound layer of proteins with high affinity for the nanoparticle surface, characterized by slow exchange rates and relative stability. The soft corona consists of proteins that are loosely bound, often to the hard corona itself, with rapid exchange rates [16]. The hard corona is generally considered more critical as it is more stable and defines the initial identity of the nanoparticle that cells encounter, directly influencing cellular recognition and uptake [16].
Q2: How can I isolate the protein corona from my nanoparticles for analysis, especially for soft nanoparticles like Lipid Nanoparticles (LNPs)?
Isolating the intact corona from soft nanoparticles is challenging due to their low density and similarity to endogenous biological particles. Standard centrifugation can cause aggregation or disruption [14]. A recommended method is continuous density gradient ultracentrifugation (DGC) with extended centrifugation times (e.g., 16-24 hours). This approach gently separates protein-LNP complexes from denser plasma proteins and endogenous particles based on buoyant density, allowing for a cleaner isolation suitable for downstream mass spectrometry analysis [14].
Q3: Can I prevent protein corona formation altogether to maintain my nanoparticle's synthetic identity?
Completely preventing corona formation is extremely difficult and may not be desirable, as the corona mediates key biological interactions. The primary strategy is to engineer a stealth corona that directs favorable biological outcomes. While PEGylation is the gold standard for reducing opsonization and prolonging circulation, it does not fully prevent corona formation [16]. Advanced strategies, such as conjugating zwitterionic groups (e.g., α-glutamyl) to PEG termini, have shown improved stealth properties and reduced protein adsorption compared to conventional PEG [16].
Q4: How does the protein corona affect the stability of my nanoparticle formulation?
The protein corona can have dual effects on stability. It can prevent aggregation by providing steric stabilization; for instance, BSA adsorption has been shown to prevent the aggregation of iron oxide nanoparticles [15]. Conversely, it can induce aggregation if the adsorbed proteins cause bridging between particles. Furthermore, for certain materials like silver nanoparticles, proteins in the corona can influence the release of ions (e.g., by acting as a silver ion "sink"), thereby altering the nanoparticle's chemical stability and dissolution rate [15] [19].
Q5: Are there computational tools to predict the protein corona composition to guide nanoparticle design?
Yes, traditional linear models perform poorly for this complex task. However, machine learning (ML), particularly Random Forest (RF) models, has emerged as a powerful tool. By integrating meta-analysis of existing data, ML can quantitatively predict the functional composition of the protein corona (e.g., relative abundance of immune proteins, apolipoproteins) based on a nanoparticle's physicochemical properties and experimental conditions with high accuracy (R² > 0.75). This can then be used to predict downstream biological responses like cellular uptake by macrophages [18].
Data Presentation
| Parameter | Influence on Protein Corona | Impact on Biological Identity & Stability |
|---|---|---|
| Size | Thicker corona on larger nanoparticles; influences protein binding capacity [15]. | Affects biodistribution, macrophage uptake, and circulation time. |
| Surface Charge | Positively charged NPs often adsorb more proteins, particularly those with negative charge [15]. | Influences colloidal stability, cellular internalization, and potential cytotoxicity. |
| Surface Chemistry | The most critical factor. Determines affinity for specific protein groups. Hydrophobicity and functional groups (e.g., -COOH, -NH₂) dictate binding [18]. | Directs organ targeting (e.g., ApoE binding for liver targeting), immune response, and blood circulation half-life. |
| Shape | Proteins retain more stable structure on spherical NPs compared to high-curvature nanostructures (e.g., rods) [15]. | Alters interaction with cell membranes and internalization pathways. |
| Incubation Conditions (pH, Time, Temp) | Alters protein conformation and binding kinetics; longer time leads to more stable hard corona [15]. | Defines the maturity and stability of the corona, affecting the reproducibility of in-vivo outcomes. |
| Functional Protein Category | Example Proteins | Common Biological Consequences |
|---|---|---|
| Apolipoproteins | ApoE, ApoA-I | Facilitates targeting to specific tissues (e.g., liver via LDL receptor binding); can enhance cellular uptake [15] [14]. |
| Immune Proteins | Immunoglobulins (IgG), Complement Proteins | Acts as opsonins, promoting recognition and clearance by the mononuclear phagocyte system (MPS), reducing circulation time [18]. |
| Coagulation Factors | Fibrinogen, Vitronectin | May trigger thrombotic responses or influence adhesion to vascular endothelial cells [14]. |
| Acute Phase Proteins | C-reactive Protein, Alpha-2-Macroglobulin | Modulates inflammatory responses; can either promote or suppress immune cell uptake [14]. |
| "Stealth" Proteins | Clusterin, Serum Albumin | Can confer stealth properties by reducing phagocytosis and increasing circulation time [18]. |
Experimental Protocols
This protocol is designed to minimize co-isolation of endogenous nanoparticles and preserve the integrity of the soft LNP-corona complex.
- LNP Incubation: Inculate your LNP formulation with human blood plasma (or other relevant biofluid) at a physiologically relevant concentration and temperature (e.g., 37°C) for a desired time (e.g., 1 hour) to allow corona formation.
- Gradient Preparation: Prepare a continuous density gradient (e.g., iodixanol gradient) in an ultracentrifuge tube. The density should range to accommodate the buoyant density of LNPs (typically low).
- Sample Loading: Carefully layer the LNP-plasma incubation mixture on top of the pre-formed density gradient.
- Ultracentrifugation: Centrifuge the samples at high speed (e.g., ~100,000 - 200,000 × g) for an extended period (16-24 hours at 4°C). This prolonged run is critical for effective separation from endogenous particles.
- Fraction Collection: After centrifugation, carefully fractionate the gradient from the top. The protein-LNP complexes will band at their buoyant density.
- Corona Characterization:
- Mass Spectrometry: Analyze the fractions via label-free quantitative mass spectrometry to identify and quantify the proteins in the corona. Normalize to the protein composition in the plasma control alone.
- Dynamic Light Scattering (DLS): Measure the hydrodynamic diameter and polydispersity of the fractions to confirm LNP size and monodispersity.
- Functional Assays: Use the isolated LNP-corona complexes in downstream cell culture experiments (e.g., uptake, transfection efficiency) to link corona composition to biological function.
This protocol directly tests the functional consequence of the protein corona on mRNA delivery.
- Corona Pre-formation: Create two sets of LNPs:
- Experimental Group: Pre-incubate LNPs with a selected protein (e.g., Vitronectin) or full plasma to form a corona.
- Control Group: Bare LNPs in buffer.
- Cell Treatment: Treat human liver cells (e.g., HepG2) with both groups of LNPs. Use a consistent nanoparticle concentration based on particle number.
- Uptake Measurement: After a few hours, measure cellular uptake using flow cytometry (if LNPs are fluorescently labeled) or other suitable methods.
- Expression Analysis: After 24-48 hours, measure mRNA expression levels using techniques like qRT-PCR or fluorescence microscopy (if the mRNA encodes a reporter protein like GFP).
- Data Interpretation: Correlate uptake data with expression data. A key finding may be that certain corona proteins increase uptake but do not enhance, or even decrease, functional mRNA expression, indicating corona-induced trafficking to degradative pathways rather than productive endosomal escape [14].
Mandatory Visualization
Diagram 1: Protein Corona Impact on LNP Transfection
Diagram 2: Machine Learning Prediction of Corona & Bio-Effects
The Scientist's Toolkit
Essential Research Reagent Solutions
| Item | Function / Application in Corona Research |
|---|---|
| Gold Nanoparticles (AuNPs) | Commonly used model nanoparticles due to their unique optical properties (Surface Plasmon Resonance) which shift upon protein binding, allowing for real-time monitoring of corona formation [15]. |
| PEGylated Lipids | Used in LNP formulations to provide a steric barrier, reducing non-specific protein adsorption and opsonization, thereby prolonging circulation time. A key tool for creating stealth nanoparticles [14] [16]. |
| Apolipoprotein E (ApoE) | A critical functional protein in the corona. Its adsorption onto LNPs is a known mechanism for hepatocyte targeting via the LDL receptor. Used in pre-coating experiments to direct liver-specific delivery [14]. |
| Density Gradient Media (e.g., Iodixanol) | Essential for isolating intact protein-LNP complexes from biological fluids using ultracentrifugation, enabling proteomic analysis of the corona without contamination from endogenous particles [14]. |
| Random Forest Machine Learning Models | A computational tool used to accurately predict the functional composition of the protein corona and subsequent cellular recognition based on nanoparticle parameters, guiding rational NP design before synthesis [18]. |
Impact of Physicochemical Properties on Stability and Fate
Troubleshooting Guides
FAQ 1: How do the core physicochemical properties of a nanoparticle influence its stability in biological fluids?
Answer: The core physicochemical properties of a nanoparticle are fundamental determinants of its stability in circulation. Instability can lead to premature drug release, aggregation, or rapid clearance, undermining therapeutic efficacy. The following properties are critical:
- Size and Surface Charge: Nanoparticles must be designed with a negative surface charge to prevent accelerated blood clearance (ABC), a phenomenon where particles are rapidly cleared from the blood by the kidney and liver [20]. In contrast, a positive surface charge can increase cell affinity and uptake in diseased tissues via the Enhanced Permeation and Retention (EPR) effect, but it must be carefully balanced against circulation time [20].
- Surface Chemistry and Corona Formation: Upon injection into the bloodstream, nanoparticles are rapidly coated by proteins and lipids, forming a "corona". The composition of this corona is dictated by the nanoparticle's original surface chemistry and electrical charge, and it defines the biological identity that the immune system interacts with [20]. This corona can trigger opsonization, leading to phagocytosis and clearance.
- Mechanical Properties (Stiffness): The material composition (e.g., polymeric vs. metallic) determines nanoparticle stiffness. Softer nanoparticles (like lipidic ones) can deform more easily but may have a lower rate of cellular uptake compared to stiffer metal or silica nanoparticles [20].
Table 1: Impact of Key Physicochemical Properties on Stability and Fate
| Property | Impact on Stability & Fate | Consequence of Poor Control |
|---|---|---|
| Size | Determines the pathway and efficiency of cellular uptake (endocytosis) [20]. Influences circulation time and tissue penetration. | Off-target effects; accelerated clearance; reduced cellular internalization. |
| Surface Charge (Zeta Potential) | Affects particle affinity for cell membranes and protein corona composition [20]. A high zeta potential (positive or negative) prevents aggregation [21]. | Aggregation in suspension; opsonization and rapid clearance by the mononuclear phagocyte system (MPS). |
| Surface Chemistry / Ligands | Directs active targeting to specific cells; can be engineered for "stealth" properties (e.g., using PEG) to evade immune detection [20]. | Non-specific binding; immune recognition; failure to reach the target site. |
| Hydrophobicity | Influences the interaction with biological membranes and serum proteins [20]. | Increased protein adsorption, leading to opsonization and aggregation. |
FAQ 2: My nanoparticle formulation is aggregating in serum. What are the primary causes and solutions?
Answer: Aggregation is a primary indicator of instability and is often caused by particle collisions that overcome repulsive forces [8]. In serum, this is exacerbated by interactions with proteins and ions.
Causes and Solutions:
- Cause: Unfavorable Surface Charge. A low zeta potential (near neutral) reduces the electrostatic repulsion between particles, allowing them to agglomerate [21].
- Solution: Modify the surface chemistry to increase the zeta potential. This can be achieved by introducing charged functional groups or using stabilizers that provide steric hindrance [8].
- Cause: High Nanoparticle Concentration. A high particle density increases the collision frequency, raising the probability of aggregation [22].
- Solution: Follow recommended concentration guidelines and use a sonicator to disperse nanoparticles evenly before introduction into biological media [22].
- Cause: Non-Specific Protein Binding. Proteins in serum can bridge between nanoparticles, causing them to clump together [20].
- Solution: Incorporate stabilizing agents like polyethylene glycol (PEG) or use blocking agents such as Bovine Serum Albumin (BSA) after conjugation to shield the surface from non-specific interactions [22].
FAQ 3: What advanced analytical techniques can I use to quantitatively monitor nanoparticle stability in complex biological media like plasma?
Answer: Conventional dynamic light scattering (DLS) can be unreliable in biological fluids due to interference from plasma proteins and other components [23]. More sophisticated techniques are required for accurate analysis.
Recommended Technique: Size-Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS)
- Methodology: This technique separates nanoparticles from biological matrix components (like free proteins) before analysis. The dual-angle light scattering detector then provides absolute measurements of molecular weight and radius of gyration without relying on column calibration standards [23].
- Application: SEC-MALS can elucidate degradation kinetics and physical property changes of nanoparticles in pure human serum and plasma. For instance, it has been used to discover that even a trace impurity (~1%) in a lipid component (ALC-0315) can greatly diminish mRNA-LNP stability in serum [23].
- Protocol Outline:
- Sample Preparation: Incubate your nanoparticle formulation (e.g., mRNA-LNPs) in human plasma or serum for designated time points.
- Chromatographic Separation: Use a dual-column configuration to attenuate interference from plasma components.
- On-line Detection: Pass the eluent through a MALS detector and a refractive index (RI) detector.
- Data Analysis: Software calculates the absolute molar mass and size of the nanoparticles in the solution, allowing you to track changes in integrity over time [23].
The following workflow diagram illustrates the experimental protocol for analyzing nanoparticle stability using SEC-MALS:
FAQ 4: How does the "protein corona" form and how does it alter the intended fate of nanoparticles in the body?
Answer: The protein corona is a dynamic layer of biomolecules that adsorbs spontaneously onto a nanoparticle's surface upon contact with biological fluids [20]. This process fundamentally alters the nanoparticle's biological identity.
- Formation Mechanism: The formation is driven by the physicochemical properties of the nanoparticle, including its surface chemistry, electrical charge, and hydrophobicity [20]. The Vroman effect describes the competitive and time-dependent exchange of proteins on the surface, where proteins with high abundance and mobility adsorb first, and are later replaced by proteins with higher affinity.
- Impact on Fate:
- Altered Cellular Recognition: The corona, not the synthetic nanoparticle surface, is what cells "see." It can mask targeting ligands, rendering them ineffective, or create new, unintended biological interactions.
- Shift in Pharmacokinetics: A corona rich in opsonins (proteins that mark particles for phagocytosis) leads to rapid clearance by macrophages in the liver and spleen. Conversely, a corona rich in "dysopsonins" (like albumin) can promote longer circulation times [20].
- Changed Biodistribution: The ultimate destination of the nanoparticle in the body is largely dictated by the composition of the hard protein corona that forms within the first few minutes of entering circulation.
FAQ 5: What are the critical steps for conjugating biomolecules to nanoparticles without compromising stability?
Answer: Successful conjugation requires optimizing reaction conditions to maintain nanoparticle dispersion and biomolecule activity.
- Optimize pH: The pH of the conjugation buffer significantly impacts binding efficiency. For example, antibody conjugation to gold nanoparticles typically works best at a pH near or slightly above the isoelectric point of the antibody, often around pH 7-8 [22].
- Prevent Aggregation: Adjust the concentration of nanoparticles to prevent crowding and aggregation during the reaction. Sonication prior to conjugation is recommended [22].
- Determine Optimal Ratio: An inadequate or excessive amount of antibody (or other biomolecule) can hinder conjugation efficiency and lead to unbound particles that disrupt assays. Use precise ratios as suggested in conjugation kits or determined empirically [22].
- Use Stabilizers: After conjugation, incorporate stabilizing agents like BSA or PEG to enhance shelf life and prevent non-specific binding in diagnostic applications [22].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Nanoparticle Stability and Fate Experiments
| Reagent / Material | Function in Experiment | Key Consideration |
|---|---|---|
| Polyethylene Glycol (PEG) | A "stealth" polymer conjugated to nanoparticle surfaces to reduce protein adsorption (opsonization) and prolong circulation time [20]. | PEG density and chain length are critical for creating an effective hydration barrier. |
| HEPES or Phosphate Buffers | Provide a stable pH environment for conjugation reactions and stability studies [22]. | Buffer capacity and ionic strength must be optimized to prevent nanoparticle aggregation. |
| Bovine Serum Albumin (BSA) | Used as a blocking agent to passivate nanoparticle surfaces and prevent non-specific binding in assays and in vivo [22]. | High-purity grades are essential to avoid introducing contaminants. |
| Size-Exclusion Chromatography (SEC) Columns | For purifying conjugated nanoparticles from unreacted reagents and for analyzing stability in complex media via SEC-MALS [23]. | Column pore size must be selected to match the hydrodynamic size of the nanoparticle. |
| Stimuli-Responsive Polymers (e.g., pH-sensitive) | Used to design "smart" nanoparticles that release their cargo in response to specific biological stimuli (e.g., low tumor pH) [20]. | The trigger mechanism (pH, ROS, enzyme) must be highly specific to the target microenvironment. |
| HEPA-Filtered Local Exhaust Ventilation | An engineering control (e.g., fume hood, glove box) to protect researchers from inhaling airborne nanoparticles during synthesis and handling [24] [25]. | Required when handling dry powder nanomaterials to minimize inhalation exposure risk. |
For researchers in drug development, the journey of an intravenously injected nanoparticle is a race against time and the body's sophisticated defense systems. The therapeutic promise of nanocarriers—spatial and temporal controlled drug delivery—is often compromised by their rapid destabilization and clearance from the bloodstream [26] [27]. Achieving successful delivery requires navigating a series of biological barriers, where processes like aggregation, opsonization, and phagocytic clearance can prematurely eliminate nanoparticles before reaching their target site [26]. This guide provides targeted troubleshooting methodologies to diagnose and overcome these destabilization mechanisms, framed within the thesis that rational design and precise characterization are paramount for improving nanoparticle structural stability in systemic circulation.
Troubleshooting Guide: Key Issues and Solutions
FAQ 1: My nanoparticle formulations are aggregating in biological media. How can I prevent this?
- Problem: Nanoparticles aggregate when introduced into blood serum or plasma, leading to increased particle size, potential capillary blockade, and altered biodistribution.
- Diagnosis & Solution:
- Verify Concentration: Aggregation often occurs when nanoparticle concentration is too high. Follow recommended concentration guidelines and use sonication to disperse particles evenly before use [28].
- Optimize Surface Chemistry: Incorporate steric stabilizers. Poly(ethylene glycol) (PEG) is the gold-standard for creating a hydrophilic, steric barrier that reduces interparticle attraction and aggregation [26] [27]. A common practice is to use PEG-conjugated lipids (e.g., DSPE-PEG2000) in the nanoparticle shell [4].
- Employ Blocking Agents: After synthesis and conjugation, use blocking agents like Bovine Serum Albumin (BSA) or casein to coat the surface and minimize non-specific interactions that lead to aggregation [28] [29].
FAQ 2: My nanoparticles are being cleared from the blood circulation too quickly. What is the mechanism and how can I extend their circulation lifetime?
- Problem: Rapid clearance of nanoparticles, primarily by the Mononuclear Phonuclear Phagocytic System (MPS), limits their ability to reach the target tissue.
- Diagnosis & Solution:
- Understand Opsonization: The primary mechanism for rapid clearance is opsonization, where blood serum proteins (opsonins) adsorb to the nanoparticle surface, tagging them for phagocytosis [26] [27]. Common opsonins include immunoglobulins, complement proteins (C3, C4, C5), albumin, and apolipoproteins [26].
- Implement "Stealth" Coating: The most effective strategy is PEGylation—grafting, entrapping, or adsorbing PEG chains onto the nanoparticle surface. This creates a steric shield that reduces opsonin protein adsorption and MPS recognition, significantly prolonging circulation half-life [27].
- Consider Nanoparticle Elasticity: Recent evidence indicates that nanoparticle elasticity non-monotonically affects systemic circulation lifetime, correlating with the composition of the protein corona. Tuning elasticity (e.g., to an intermediate range of 75–700 kPa) can promote the adsorption of specific proteins like Apolipoprotein A-I (ApoA1), which is strongly correlated with longer blood circulation times [4].
FAQ 3: I am getting inconsistent results in my diagnostic assay. Could nanoparticle conjugation be the issue?
- Problem: Inconsistent signal, high background, or false positives in nanoparticle-based diagnostics (e.g., lateral flow assays, ELISA).
- Diagnosis & Solution:
- Check Conjugation Buffer pH: The pH of the conjugation buffer significantly impacts biomolecule binding efficiency. For antibody conjugations with gold nanoparticles, a pH around 7-8 is generally optimal. Use dedicated conjugation buffers to maintain stable pH and molecule integrity [28].
- Optimize Antibody-to-Nanoparticle Ratio: Inadequate or excessive antibody amounts can hinder conjugation efficiency and assay performance. Use precise ratio suggestions provided by kit manufacturers or determine the optimal ratio empirically [28].
- Prevent Non-Specific Binding: Use blocking agents like BSA or PEG in the assay incubation steps to prevent nanoparticles from attaching to unintended molecules, which causes high background and false positives [28] [29].
Experimental Protocols for Stability Assessment
Protocol 1: Analyzing Protein Corona Composition
Objective: To isolate and identify proteins adsorbed onto nanoparticles after incubation in plasma, providing insight into opsonization potential.
Materials: Nanoparticle sample, mouse or human plasma, ultracentrifuge, phosphate-buffered saline (PBS), sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) system, mass spectrometry.
Method:
- Incubation: Incubate your nanoparticle sample (e.g., 1 mg/mL) in plasma (e.g., 50% v/v in PBS) for a predetermined time (e.g., 1 hour) at 37°C [4].
- Isolation of Corona-Coated Nanoparticles: Ultracentrifuge the mixture (e.g., at 100,000 × g for 1 hour) to pellet the nanoparticles with their hard protein corona.
- Washing: Carefully remove the supernatant and gently wash the pellet with PBS to remove loosely associated proteins. Repeat centrifugation.
- Protein Elution & Analysis: Re-suspend the pellet in SDS-PAGE loading buffer to elute the corona proteins. Analyze via:
- SDS-PAGE: For a gross profile of corona proteins.
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS): For precise identification of individual corona proteins, such as ApoA1, whose abundance can be correlated with circulation lifetime [4].
Protocol 2: Evaluating In Vivo Circulation Lifetime
Objective: To quantitatively measure the pharmacokinetic profile and blood circulation half-life of nanoparticles.
Materials: Fluorescently or radio-labeled nanoparticles, animal model (e.g., mouse), IV injection setup, blood collection equipment, fluorescence spectrometer or gamma counter.
Method:
- Dosing: Intravenously inject a known dose of labeled nanoparticles into the animal model (e.g., via tail vein).
- Serial Blood Sampling: Collect small blood samples (e.g., 10-20 µL) from the retro-orbital plexus or tail vein at multiple time points post-injection (e.g., 0.5, 1, 2, 4, 8, 24 hours).
- Processing: Lyse the blood samples and isolate the plasma fraction by centrifugation.
- Quantification: Measure the signal (fluorescence or radioactivity) in each plasma sample and compare it to a standard curve of the injected formulation.
- Pharmacokinetic Analysis: Plot nanoparticle concentration in blood versus time. Calculate key parameters like circulation half-life (t1/2) and area under the curve (AUC) to compare the performance of different formulations [4] [27].
Data Presentation: Quantitative Relationships
Table 1: Impact of Nanoparticle Physicochemical Properties on Stability and Clearance
| Property | Effect on Aggregation | Effect on Opsonization | Impact on Circulation Lifetime |
|---|---|---|---|
| Size | Larger particles (>200 nm) are more prone to sedimentation and aggregation. | Optimal size for avoiding MPS is reported to be 10-100 nm [26]. | Smaller sizes (within optimal range) generally show longer circulation [26]. |
| Surface Charge | Highly charged surfaces (positive or negative) can cause electrostatic aggregation in high-salt media. | Neutral or slightly negative surfaces tend to reduce opsonin adsorption [26] [27]. | Neutral, "stealth" surfaces significantly prolong half-life compared to charged ones [27]. |
| Surface Chemistry (PEGylation) | Reduces aggregation by steric hindrance. | Dramatically reduces opsonization by forming a hydrophilic shield [27]. | Can increase circulation half-life from minutes to hours or days [27]. |
| Elasticity | Softer particles may be more prone to deformation and fusion under stress. | Non-monotonically affects protein corona composition; intermediate elasticity (75-700 kPa) enriches for ApoA1 [4]. | Shows a non-monotonic relationship; maximum lifetime correlated with intermediate elasticity and high ApoA1 adsorption [4]. |
Table 2: Key Opsonins and Their Roles in Nanoparticle Clearance
| Opsonin | Function in Clearance | Note |
|---|---|---|
| Immunoglobulins (IgG, IgM) | Bind to foreign surfaces and engage Fc receptors on macrophages. | Major initiators of phagocytosis [27]. |
| Complement Proteins (C3, C4, C5) | Form "membrane attack complex" and tag particles for phagocytosis. | A key part of the innate immune response to nanoparticles [27]. |
| Apolipoprotein A-I (ApoA1) | Main protein component of HDL. | Recent studies show its enrichment in the corona is strongly correlated with longer systemic circulation lifetime [4]. |
| Fibrinogen | Acute phase protein; adsorption can trigger inflammatory responses. | High adsorption may lead to platelet aggregation and immune activation [26]. |
Visualization of Mechanisms and Workflows
Diagram: Protein Corona Formation and MPS Clearance
Diagram: Experimental Workflow for Stability Testing
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Nanoparticle Stabilization and Characterization
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| DSPE-PEG2000 | A PEG-conjugated lipid used to create a sterically stabilizing "stealth" coating on lipid and polymeric nanoparticles. | PEG density and chain length are critical for effective protein repulsion [4] [27]. |
| BSA (Bovine Serum Albumin) | Used as a blocking agent to passivate surfaces and minimize non-specific binding in assays and formulations. | Can be chemically modified (e.g., BSA-c) to better overcome charge-based interactions [29]. |
| Poloxamers/Poloxamines (e.g., Pluronic F127, Poloxamine 908) | Non-ionic surfactants that can be adsorbed onto nanoparticles to reduce opsonization and MPS uptake. | An alternative to PEGylation; their effectiveness depends on the copolymer chain arrangement [27]. |
| Tunable Resistive Pulse Sensing (TRPS) | A high-resolution, single-particle technique for characterizing size, concentration, and zeta potential. | Crucial for accurately analyzing polydisperse samples and detecting nanoparticle subpopulations that may aggregate [30]. |
| Apolipoprotein A-I (ApoA1) | A specific plasma protein whose corona abundance is a potential biomarker for predicting nanoparticle circulation time. | Enrichment in the protein corona on nanoparticles of intermediate elasticity correlates with longer circulation [4]. |
Engineering Stable Nanoparticles: Design Strategies and Advanced Materials
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary mechanism by which PEGylation confers "stealth" properties to nanoparticles?
PEGylation creates a hydrophilic, steric barrier around the nanoparticle that reduces nonspecific interactions with blood components. The flexible PEG chains form a hydrated shield through hydrogen bonding with water molecules. This shield minimizes opsonization—the adsorption of proteins that mark particles for clearance by the Mononuclear Phagocyte System (MPS)—thereby prolonging circulation time. The stealth effect is influenced by PEG conformation, which transitions from a "mushroom" state at low density to an extended "brush" state at high surface density, with the latter providing more effective shielding [31] [32].
FAQ 2: What is the "PEG Dilemma," and how does it impact drug delivery efficacy?
The "PEG Dilemma" refers to the paradoxical challenge where the same PEG coating that provides beneficial stealth properties can also create a physical barrier that hinders the cellular uptake of nanoparticles by the target cells. This steric hindrance can prevent the nanoparticle from interacting with cellular receptors, thereby reducing the internalization and efficacy of the delivered therapeutic, especially for agents that require intracellular activity (e.g., DNA, RNA, certain chemotherapeutics) [33] [34]. Furthermore, PEG can trigger immune responses, such as the production of anti-PEG antibodies, which exacerbate this problem by accelerating blood clearance upon repeated administration [34] [35].
FAQ 3: What are the key structural parameters of PEG that influence nanoparticle performance?
The immunological safety and performance of PEGylated nanoparticles are highly dependent on several structural parameters of the PEG-lipid conjugate [35]:
- PEG Chain Length: Has a biphasic effect; both very short and very long chains are more likely to induce the Accelerated Blood Clearance (ABC) phenomenon.
- PEG Density (Surface Coverage): Also exhibits a biphasic effect, where both very low and very high densities can impact stealth properties and immunogenicity.
- PEG Architecture: Branched PEG conjugates often confer superior stealth properties compared to linear PEGs.
- Terminal Functional Group: The chemical group at the end of the PEG chain (e.g., methoxy, carboxyl, amine) can significantly impact immunogenicity and clearance rate.
- Lipid Anchor Structure: The hydrophobicity and length of the lipid moiety (e.g., DSPE, ceramide) anchoring the PEG to the nanoparticle influence stability and pharmacokinetics.
FAQ 4: What are the main alternatives being explored to overcome the limitations of traditional PEGylation?
Researchers are developing advanced strategies to move beyond the limitations of conventional PEG coatings [33] [35] [32]:
- Sheddable PEG Coatings: PEG is attached via linkers that are cleaved in response to specific stimuli in the tumor microenvironment (TME), such as low pH or overexpressed enzymes (e.g., matrix metalloproteinases). This allows the particle to shed its stealth coat upon reaching the target, facilitating cellular uptake.
- Alternative Polymers: Hydrophilic polymers like poly(oxazoline) (POZ), polyvinyl alcohol (PVA), and poly(glycerol) are being investigated as potential replacements for PEG to avoid anti-PEG immune responses.
- Zwitterionic Coatings: Materials that possess both positive and negative charges, creating a super-hydrophilic surface that resists protein adsorption effectively.
- Biomimetic Coatings: Using natural cell membranes (e.g., from red blood cells or leukocytes) to cloak nanoparticles, providing innate biocompatibility and active targeting capabilities [36].
Troubleshooting Guide: Common Experimental Challenges
Challenge 1: Reduced Cellular Uptake of PEGylated Nanoparticles
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| High efficacy in vitro but low efficacy in vivo. | Steric hindrance from PEG shield preventing interaction with target cell receptors [34]. | Implement a sheddable PEG strategy. Use a pH-sensitive (e.g., hydrazone bond) or enzyme-cleavable (e.g., MMP-2 sensitive peptide linker) covalent bond between the PEG and nanoparticle core [33]. |
| Confirmed long circulation half-life but poor tumor regression. | The PEG coating remains intact, creating a barrier to cellular internalization. | Optimize PEG surface density. A lower density might reduce steric hindrance while maintaining sufficient stealth properties; however, balance is key to avoid opsonization [31]. |
| Poor transfection (for gene delivery) despite good tumor accumulation. | PEG interferes with intracellular processes post-internalization [34]. | Functionalize PEG terminal groups with targeting ligands (e.g., peptides, antibodies) to promote receptor-mediated endocytosis, overcoming the non-specific blocking effect [33] [37]. |
Challenge 2: Accelerated Blood Clearance (ABC Phenomenon) Upon Repeated Dosing
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| First dose shows prolonged circulation, but second dose is rapidly cleared. | Anti-PEG IgM antibodies produced after the first dose bind to the second dose, promoting opsonization and clearance by macrophages in the liver and spleen [34] [35]. | Adjust the injection schedule. The ABC phenomenon is most pronounced with dosing intervals of 3-7 days and attenuates by 4 weeks [34]. |
| Reduced Area Under the Curve (AUC) for subsequent doses. | The ABC phenomenon has an inverse relationship with the first dose quantity; very low first doses optimally induce anti-PEG IgM [34]. | Use a high first dose (e.g., 5 µmol/kg) to induce B-cell anergy or tolerance, reducing the anti-PEG antibody response [34]. |
| Increased hepatic and splenic accumulation of the second dose. | Anti-PEG antibodies trigger complement activation and Fc-receptor-mediated phagocytosis. | Modify PEG structure. Utilize branched PEG architectures or carefully optimize PEG chain length and density to make the coating less immunogenic [38] [35]. |
Challenge 3: Complement Activation-Related Pseudoallergy (CARPA)
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Acute hypersensitivity reactions (e.g., skin flushing, hypotension) in animal models or patients shortly after infusion. | PEGylated nanoparticles activating the complement system, leading to the release of anaphylatoxins (C3a, C5a) [35] [32]. | Pre-medicate with corticosteroids and antihistamines to mitigate inflammatory reactions. |
| Batch-to-batch variability in reaction severity. | Factors like PEG surface density, conjugation chemistry, and nanoparticle charge influence complement activation [32]. | Control nanoparticle surface charge. Avoid highly negative or positive charges. A near-neutral zeta potential is generally desired for stealth properties [31]. |
| Reactions occur even with low levels of anti-PEG antibodies. | Activation can occur via the lectin pathway or alternative pathway, independent of antibodies, especially with high molecular weight PEGs [32]. | Consider alternative stealth polymers like POZ or PVA for new formulations if PEG-specific issues persist [35]. |
Experimental Protocols
Protocol 1: Evaluating the Protein Corona and Opsonization
Objective: To analyze the profile of serum proteins that adsorb onto PEGylated nanoparticles, which defines their biological identity and fate.
Materials:
- Purified PEGylated nanoparticle formulation (and non-PEGylated control)
- Complete cell culture medium supplemented with Fetal Bovine Serum (FBS) or human plasma
- Ultracentrifuge
- SDS-PAGE gel electrophoresis system
- Mass Spectrometry (MS) equipment
- Dynamic Light Scattering (DLS) and Zeta Potential instruments
Methodology:
- Incubation: Incubate a standardized concentration of nanoparticles (e.g., 1 mg/mL) in 50% FBS or human plasma at 37°C for 1 hour to simulate in vivo conditions [33].
- Isolation of Corona-Coated NPs: Separate the nanoparticles from unbound proteins by ultracentrifugation (e.g., 100,000 g for 1 hour). Gently wash the pellet with PBS to remove loosely associated proteins.
- Protein Elution: Resuspend the nanoparticle pellet in a strong denaturing buffer (e.g., Laemmli buffer) to elute the hard corona proteins.
- Analysis:
- SDS-PAGE: Run the eluted proteins on a gel to visualize and compare the total protein amount and pattern between PEGylated and non-PEGylated formulations [34].
- Mass Spectrometry: Identify the specific proteins present in the corona to understand which opsonins or dysopsonins are adsorbed [33].
- DLS/Zeta Potential: Measure the hydrodynamic diameter and surface charge of the nanoparticles before and after corona formation. A significant change indicates substantial protein adsorption [37].
Protocol 2: Assessing Cellular Uptake In Vitro
Objective: To quantify and visualize the internalization of nanoparticles into target cells, evaluating the impact of PEGylation.
Materials:
- Fluorescently labeled PEGylated and non-PEGylated nanoparticles
- Target cell line (e.g., HeLa, MCF-7)
- Cell culture plates and standard media
- Flow Cytometer
- Confocal Microscope
- Inhibitors (e.g., chloroquine for endocytosis inhibition)
Methodology:
- Cell Seeding: Seed cells in multi-well plates (e.g., 24-well for flow cytometry, glass-bottom dishes for microscopy) and culture until 70-80% confluency.
- Dosing: Treat cells with a consistent concentration of fluorescent nanoparticles in serum-containing media. Include wells for negative controls (no nanoparticles) and pharmacological inhibitors if studying uptake mechanisms.
- Incubation: Incubate for a predetermined time (e.g., 2-4 hours) at 37°C.
- Washing: Thoroughly wash cells with PBS to remove non-internalized nanoparticles.
- Analysis:
- Flow Cytometry: Trypsinize and resuspend cells in PBS. Analyze the fluorescence intensity of the cell population using a flow cytometer. A rightward shift in fluorescence indicates nanoparticle uptake. Compare PEGylated and non-PEGylated formulations [34].
- Confocal Microscopy: Fix cells (e.g., with 4% PFA), stain actin cytoskeleton (e.g., phalloidin) and nuclei (e.g., DAPI). Use a confocal microscope to obtain z-stack images and confirm intracellular localization of nanoparticles versus surface binding [37].
Signaling Pathways and Experimental Workflows
PEGylated Nanoparticle Journey and Clearance Pathways
Experimental Workflow for Protein Corona Analysis
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Experimentation | Key Consideration |
|---|---|---|
| Heterobifunctional PEG Linkers (e.g., MAL-PEG-NHS) | Enable site-specific, covalent conjugation of PEG to nanoparticles or proteins. The different terminal groups (e.g., Maleimide, NHS Ester) react with specific residues (thiols, amines) [39]. | Crucial for controlling PEG orientation and density. Choice of linker determines conjugation chemistry and stability. |
| PEG-DSPE (Distearoylphosphatidylethanolamine) | A common PEG-lipid conjugate used for post-insertion or co-formulation into lipid nanoparticles and liposomes. The DSPE anchor provides stable incorporation into lipid bilayers [35] [31]. | A workhorse for creating stealth liposomal formulations. The length of the PEG chain and the lipid anchor affect stability and pharmacokinetics. |
| Acid-Labile Linkers (e.g., hydrazone, vinyl ether) | Used to create sheddable PEG coatings. Stable at neutral blood pH but cleave rapidly in the acidic environment of endosomes/lysosomes (pH ~5.0), facilitating intracellular drug release [33]. | Key for resolving the "PEG dilemma". Enables the design of stimuli-responsive nanoparticles that shed PEG upon cellular internalization. |
| Aminosilanes (e.g., APTES) | Used as crosslinkers for the surface functionalization of inorganic nanoparticles (e.g., silica, metal oxides). Introduce primary amine groups for subsequent bioconjugation with activated PEG [37]. | Essential for creating a stable functional layer on specific nanomaterial surfaces as a first step towards PEGylation. |
| Dynamic Light Scattering (DLS) / Zeta Potential Analyzer | Instruments to characterize the core physicochemical properties of nanoparticles: hydrodynamic size, size distribution (PDI), and surface charge (Zeta Potential) before and after PEGylation [37]. | Mandatory for quality control. Confirms successful PEGylation (often a slight size increase, shift towards neutral zeta potential) and colloidal stability. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical factors for ensuring the structural stability of cell membrane-coated nanoparticles (CMCNPs) in circulation?
The structural stability of CMCNPs is governed by a combination of core design, membrane integrity, and surface properties. Key factors include:
- Nanoparticle Core Elasticity: The stiffness of the core material significantly impacts circulation time. Studies using core-shell nanoparticles with identical PEGylated lipid shells but cores of different elasticity (45 kPa to 760 MPa) have revealed a non-monotonic relationship. Nanoparticles with intermediate elasticity (75–700 kPa) demonstrated the longest systemic circulation lifetime, which was strongly correlated with the specific composition of the adsorbed protein corona [4].
- Membrane Protein Integrity and Retention: The functionality of the coating relies on preserving the natural proteins and lipids from the source cell membrane during extraction and fusion. The extraction method (e.g., hypotonic lysis, sonication) and purification process (e.g., differential centrifugation) are critical to maintaining a intact membrane structure with full biological function [40] [41].
- Protein Corona Formation: Upon entering the bloodstream, nanoparticles are rapidly coated by plasma proteins, creating a "biological identity." The elasticity and surface chemistry of the nanoparticle determine the composition of this corona. For instance, a higher relative abundance of apolipoprotein A-I (ApoA1) in the corona is strongly correlated with an extended circulation lifetime [4] [42].
FAQ 2: How can I troubleshoot poor targeting efficiency of my biomimetic nanoparticles in vivo?
Poor targeting often stems from issues with margination, adhesion, or off-target clearance.
- Margination: This is the process of particles moving from the center of blood flow to the vessel wall. The "4S" parameters are crucial:
- Size: Larger nanoparticles (e.g., >100 nm) marginate more efficiently than smaller ones [43].
- Shape: Non-spherical particles with higher aspect ratios marginate more quickly than spherical ones [43].
- Stiffness: Stiffer particles tend to marginate better than soft, highly deformable ones [43].
- Surface Functionalization: A stealth coating like PEG can reduce non-specific interactions and prolong circulation, allowing more time for margination to occur [43] [4].
- Cellular Uptake by Immune Cells: If your nanoparticles are being cleared by the mononuclear phagocyte system (MPS) before reaching the target, consider the source of your cell membrane. For example, red blood cell (RBC) membranes are excellent for immune evasion due to CD47 proteins that signal "don't-eat-me," while macrophage membranes possess inherent tropism to inflammatory sites [40] [41].
FAQ 3: My biomimetic nanoparticles are aggregating during synthesis or storage. What are the probable causes and solutions?
Aggregation can be addressed by optimizing the synthesis conditions and characterizing colloidal stability.
- Cause: Incorrect Zeta Potential. A low zeta potential (typically between -10 mV and +10 mV) indicates insufficient electrostatic repulsion between particles, leading to aggregation.
- Solution: Aim for a high zeta potential, either highly positive or highly negative. For example, a chitosan-based nanosystem with a zeta potential of +73 mV demonstrated excellent stability, facilitating efficient interaction with negatively charged cell membranes [44].
- Cause: Membrane Fusion Process. The process of coating the synthetic core with the cell membrane vesicle must be controlled.
- Solution: Use optimized fusion methods like extrusion or sonication. Ensure the size of the core nanoparticle and the cell membrane vesicle are compatible for a uniform coating. Always characterize the final product's hydrodynamic diameter and polydispersity index (PDI) using dynamic light scattering; a PDI below 0.3 is generally considered acceptable for a monodisperse population [40] [41].
FAQ 4: Are there methods to actively control the delivery and release of payloads from these nanoparticles?
Yes, beyond passive targeting, bio-inspired designs can incorporate active triggering mechanisms.
- Stimuli-Responsive Cores: Use polymer cores that degrade in response to specific stimuli in the target microenvironment. Common triggers include:
- External Triggers: Incorporate functional materials that respond to external fields.
Troubleshooting Guides
Issue 1: Short Circulation Half-Life and Rapid Clearance
| Symptom | Possible Cause | Solution | Key Experimental Check |
|---|---|---|---|
| Nanoparticles rapidly disappear from bloodstream in animal models. | Insufficient stealth properties; recognition by immune system. | Use RBC membrane or platelet membrane coating; increase PEG density on surface. | Analyze protein corona composition via SDS-PAGE; check for ApoA1 enrichment [4]. |
| Suboptimal elasticity; too stiff or too soft. | Tune core material (e.g., hydrogel cross-linking density) to achieve intermediate elasticity (~75-700 kPa) [4]. | Use atomic force microscopy (AFM) to measure nanoparticle stiffness. | |
| Incomplete cell membrane coating; exposed synthetic core. | Optimize membrane fusion protocol (e.g., extrusion pressure, sonication time). | Verify coating via Cryo-EM/TEM to visualize core-shell structure [4]. |
Issue 2: Low Targeting Specificity and Accumulation at Disease Site
| Symptom | Possible Cause | Solution | Key Experimental Check |
|---|---|---|---|
| Low signal/load at target site despite long circulation. | Poor margination in blood flow. | Adjust the "4S" parameters: increase size, use non-spherical shapes, increase stiffness [43]. | Use microfluidic devices with blood flow to observe margination behavior in vitro [42]. |
| Loss of targeting membrane protein function during coating process. | Use gentler extraction methods (e.g., hypotonic lysis); avoid harsh detergents. | Confirm retention of key proteins (e.g., CD47) via Western blot or flow cytometry [40] [41]. | |
| Protein corona masking targeting ligands. | Consider "self" markers from cell membranes that are less masked. | Perform cell binding assays after pre-incubation in plasma to simulate corona formation [4]. |
Issue 3: Inconsistent Batch-to-Batch Performance
| Symptom | Possible Cause | Solution | Key Experimental Check |
|---|---|---|---|
| High variability in size, coating efficiency, or in vivo results. | Lack of standardized protocol for membrane extraction and fusion. | Strictly control cell source, lysis conditions, and purification steps (e.g., differential centrifugation) [41]. | Characterize each batch of membrane vesicles for size and protein content before fusion. |
| High polydispersity of final CMCNP product. | Optimize and control the extrusion process; use filters with defined pore sizes. | Measure hydrodynamic diameter and PDI via DLS; aim for PDI <0.3 [44]. | |
| Instability during storage. | Lyophilize with appropriate cryoprotectants (e.g., sucrose, trehalose) and store at -80°C. | Monitor size and zeta potential after reconstitution and over time. |
Quantitative Data for Biomimetic Nanoparticle Design
Table 1: Key Physicochemical Properties and Their Target Ranges for Circulation Stability
| Parameter | Optimal Range for Circulation | Impact on Fate | Characterization Technique | ||||
|---|---|---|---|---|---|---|---|
| Size | 100 - 150 nm | Avoids renal clearance; enhances margination [43]. | Dynamic Light Scattering (DLS) | ||||
| Zeta Potential | > | +20 | mV or <-20 | mV | Prevents aggregation; influences protein corona [44]. | Zetasizer | |
| Elasticity (Young's Modulus) | 75 - 700 kPa | Maximizes circulation lifetime; influences protein corona (e.g., ApoA1) [4]. | Atomic Force Microscopy (AFM) | ||||
| PEG Density | 5 - 10 mol% | Reduces opsonization and MPS uptake [4]. | NMR Spectroscopy, Colorimetric assays | ||||
| Membrane Protein Retention | >80% (vs. source cell) | Preserves biological targeting and "self" signaling [41]. | Western Blot, Flow Cytometry |
Table 2: Comparison of Cell Membrane Sources for Camouflage
| Membrane Source | Key Advantages | Potential Challenges | Ideal Application |
|---|---|---|---|
| Red Blood Cell (RBC) | Long circulation (CD47-mediated); simple isolation [40] [41]. | Lacks active targeting ligands. | Long-circulating "stealth" platforms; oxygen delivery. |
| Platelet (PLT) | Natural affinity to damaged vasculature and pathogens [40]. | Risk of initiating thrombotic events. | Targeted delivery to sites of vascular injury (e.g., atherosclerosis). |
| Macrophage | Innate tropism to inflammatory and tumor sites [40] [41]. | May be actively recruited to off-target inflamed tissues. | Therapy for inflammatory diseases, cancer. |
| Stem Cell (e.g., MSC) | Homing to injury and tumor sites; secretes reparative factors [40]. | Complex cell culture; risk of ectopic tissue formation (for whole cells, not membranes). | Regenerative medicine; myocardial infarction. |
| Cancer Cell | Homologous targeting to parent tumor [41]. | Source is tumor cell line, requiring careful safety checks. | Cancer therapy; personalized vaccines. |
Experimental Protocols
Protocol 1: Preparation of RBC Membrane-Coated Polymeric Nanoparticles
This protocol details the synthesis of biomimetic nanoparticles using red blood cell membranes for prolonged circulation [40] [41].
Materials:
- Source cells (e.g., Fresh whole blood)
- Hypotonic Lysing Buffer (e.g., 0.25x PBS)
- Protease Inhibitor Cocktail
- Poly(lactic-co-glycolic acid) (PLGA) nanoparticles
- Extruder and polycarbonate membranes (e.g., 400 nm, 200 nm, 100 nm pores)
Procedure:
- Membrane Extraction:
- Isolate RBCs from whole blood via centrifugation (3,000 rpm for 10 min at 4°C).
- Wash RBCs 3x in cold PBS to remove plasma and serum proteins.
- Lyse RBCs in hypotonic lysing buffer with protease inhibitors for 30-60 min on ice.
- Centrifuge at 12,000 g for 45 min at 4°C to pellet the membrane fraction. Discard the supernatant (hemoglobin).
- Wash the membrane pellet repeatedly with PBS until it appears pale pink or white.
- Membrane Vesiculation:
- Resuspend the purified RBC membrane pellet in PBS.
- Sonicate the suspension or subject it to multiple freeze-thaw cycles to form membrane vesicles.
- Extrude the vesicle suspension through a 400 nm polycarbonate membrane 11 times to obtain uniformly sized vesicles.
- Fusion with Nanoparticle Core:
- Mix the prepared RBC membrane vesicles with your pre-synthesized core nanoparticles (e.g., PLGA NPs) at a predetermined protein-to-polymer mass ratio (e.g., 1:1).
- Co-extrude the mixture through a 100-200 nm polycarbonate membrane for 21+ times. The physical force facilitates the fusion of the membrane onto the core.
- Purification:
- Purify the final RBC membrane-coated nanoparticles from free membranes and aggregates using density gradient centrifugation or size exclusion chromatography.
- Store the final product in PBS at 4°C or lyophilize for long-term storage.
Validation:
- Size and PDI: Use DLS to confirm a uniform, monomodal distribution.
- Zeta Potential: Should shift towards the zeta potential of pure RBC membranes (approx. -15 to -20 mV).
- Morphology: Visualize the core-shell structure using Cryo-electron microscopy [4].
- Protein Retention: Confirm the presence of key proteins like CD47 via Western Blot.
Protocol 2: Evaluating Protein Corona Formation and Its Impact
This protocol assesses the "biological identity" of nanoparticles after exposure to plasma, which dictates their in vivo fate [4].
Materials:
- Nanoparticle sample
- Mouse or human plasma
- Ultracentrifuge
- SDS-PAGE equipment
- Mass Spectrometry (for detailed analysis)
Procedure:
- Incubation:
- Incubate a fixed concentration of your nanoparticles (e.g., 1 mg/mL) in 50-100% plasma at 37°C for 1 hour to simulate in vivo conditions.
- Corona Isolation:
- Centrifuge the nanoparticle-protein corona complex at high speed (e.g., 16,000 g for 30 min) to pellet the complexes.
- Carefully remove the plasma supernatant.
- Gently wash the pellet with cold PBS to remove loosely associated proteins. Repeat this step 2-3 times.
- Analysis:
- SDS-PAGE: Re-suspend the final pellet in SDS loading buffer, boil, and run on a polyacrylamide gel. Stain with Coomassie Blue to visualize the protein profile. Compare bands between nanoparticles of different elasticity.
- Mass Spectrometry (LC-MS/MS): For precise identification, digest the proteins in the corona pellet with trypsin and analyze via LC-MS/MS to identify and quantify the relative abundance of specific proteins like ApoA1.
Visualization of Concepts and Workflows
Diagram: Relationship Between Nanoparticle Properties, Protein Corona, and In Vivo Fate
Diagram: Workflow for Synthesizing Cell Membrane-Coated Nanoparticles
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Biomimetic Nanoparticle Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| DOPC / DSPE-PEG2000 Lipids | Forms a stealth, PEGylated lipid bilayer shell; standardizes surface chemistry across different cores [4]. | Creating a consistent outer shell to isolate the effects of core elasticity. |
| PLGA Polymer | Biodegradable, FDA-approved polymer for creating the nanoparticle core [40] [45]. | Fabricating drug-loaded nanoparticle cores for membrane coating. |
| Chitosan | A natural, biocompatible cationic polysaccharide that enhances cell membrane interaction and penetration [45] [44]. | Forming stable nanosystems for brain delivery; component in hybrid NPs. |
| Acrylamide / Bis-Acrylamide | Monomer and crosslinker for synthesizing hydrogel cores with tunable elasticity [4]. | Systematically producing nanoparticles with a range of stiffness values. |
| Protease Inhibitor Cocktail | Preserves membrane protein integrity during the extraction and purification process. | Added to buffers during cell membrane isolation to prevent protein degradation. |
| Polycarbonate Extrusion Membranes | Used to control the size of membrane vesicles and for the fusion process with core nanoparticles. | Creating uniformly sized membrane vesicles and final CMCNPs. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What are the primary factors that cause rapid clearance of nanocarriers from systemic circulation? The primary factor is opsonization, where plasma proteins (opsonins) bind to the nanoparticle surface, marking them for clearance by macrophages of the mononuclear phagocyte system (MPS). This significantly shortens circulation time and reduces the fraction of the administered dose that reaches the therapeutic target. Surface characteristics such as charge and hydrophobicity are key determinants of opsonization. [46]
Q2: Besides PEGylation, what are some emerging strategies to prolong nanocarrier circulation time? Several advanced strategies are being developed to complement or provide alternatives to PEGylation. These include:
- Surface modification with "self" markers such as the CD47 protein, which signals macrophages to avoid phagocytosis.
- Modulation of mechanical properties, making particles more flexible to improve margination and circulation.
- Engineering particle morphology to optimize size and shape for hydrodynamic performance.
- Red blood cell hitchhiking, where nanocarriers attach to red blood cells to evade immune recognition. [46]
Q3: How does cholesterol incorporation enhance the stability of liposomal formulations? Cholesterol is a critical component that integrates into the phospholipid bilayer of liposomes. Its role in promoting stability is multifaceted; it controls membrane fluidity, reduces permeability, increases membrane strength and elasticity, modulates the phospholipid phase transition temperature (Tm), enhances drug retention, improves phospholipid packing, and contributes to stability in plasma. [47]
Q4: What makes cubosomes a promising nanocarrier system, particularly for drug delivery? Cubosomes are promising due to their unique non-lamellar, honeycombed (cavernous) structures that form two internal aqueous channels and a large interfacial area. This structure provides distinct advantages, including high drug payload capacity due to a high internal surface area, relatively simple preparation methods, the biodegradability of lipid components, and the ability to encapsulate hydrophobic, hydrophilic, and amphiphilic substances. [48]
Q5: Which parameters and tools are essential for adequately measuring the dispersion stability of nanoparticles in a suspension? Dispersion stability is a foundational parameter in ecotoxicological and formulation studies. It can be suitably assessed by monitoring several factors over time: (a) surface charge (zeta potential), (b) sedimentation events, and (c) the presence and size of agglomerates. Useful and complementary techniques for these measurements include Dynamic Light Scattering (DLS) for particle size, zeta potential analyzers, UV-Vis spectroscopy, fluorescence spectroscopy, and Scanning Electron Microscopy (SEM). [49]
Troubleshooting Common Experimental Issues
Problem: Short Circulation Half-Life of Liposomes
| Issue | Potential Cause | Solution | Key Parameters to Monitor | ||
|---|---|---|---|---|---|
| Rapid clearance by MPS | Opsonization due to hydrophobic or charged surface | PEGylate surface using DSPE-PEG2000; Optimize PEG density and chain length | Circulation half-life in vivo; Zeta potential (aim for near-neutral) | ||
| Drug leakage | Permeable membrane | Incorporate cholesterol (30-50 mol%) to improve bilayer packing | Drug retention rate in serum; Membrane phase transition temperature (Tm) | ||
| Particle aggregation | Unstable dispersion | Optimize lipid composition; Include 5-10% charged lipid (e.g., DOTAP, DPSE-PEG) | Zeta potential (> | ±30 | mV for electrostatic stability); Hydrodynamic diameter via DLS |
Problem: Physical Instability of Cubosome Dispersions
| Issue | Potential Cause | Solution | Key Parameters to Monitor |
|---|---|---|---|
| Loss of cubic structure | Lipid composition or degradation | Optimize monoglyceride (e.g., GMO) to polymer stabilizer (e.g., Pluronic F127) ratio | Cryo-TEM imaging; SAXS to confirm cubic phase |
| Instability in plasma | Interaction with lipoproteins/albumin | Use a PEGylated stabilizer in formulation; Consider pre-incubation with plasma proteins | Particle size distribution via DLS/NTA; Structural integrity via SAXS over time |
| Particle size growth | Agglomeration | Use high-energy homogenization (top-down) or controlled precipitation (bottom-up) | Hydrodynamic diameter and PDI via DLS; Agglomeration state via SEM |
Problem: Poor Dispersion Stability of Nanoparticles in Biological Media
| Issue | Potential Cause | Solution | Key Parameters to Monitor |
|---|---|---|---|
| Agglomeration in electrolyte-rich media | Colloidal instability; Shielded surface charge | Use steric stabilizers (e.g., Poloxamers, Polysorbates); Adjust pH away from isoelectric point | Zeta potential in target media; Hydrodynamic diameter over 24-72 hours |
| Sedimentation | Large agglomerates form | Use sonication/probe ultrasonication prior to use; Optimize concentration | Sedimentation rate via visual inspection/UV-Vis; Particle concentration via NTA |
Experimental Protocols for Key Characterizations
Protocol 1: Assessing Nanoparticle Dispersion Stability
This protocol outlines a standardized method for evaluating the stability of nanoparticle dispersions over time, which is critical for predicting performance in biological applications. [49]
1. Sample Preparation:
- Prepare nanoparticle dispersions in the relevant media (e.g., de-ionized water, phosphate-buffered saline (PBS), or cell culture medium).
- Subject the dispersion to sonication using a probe sonicator (e.g., 100 W for 5-10 minutes in an ice bath) to ensure a uniform initial state.
2. Stability Monitoring Over Time (e.g., 0, 24, 48, 72 hours):
- Surface Charge: Measure the zeta potential (in mV) using a Zetasizer. A high absolute zeta potential (>|±30| mV) typically indicates good electrostatic stability.
- Particle Size Distribution: Determine the hydrodynamic diameter and polydispersity index (PDI) via Dynamic Light Scattering (DLS). An increasing size over time suggests agglomeration.
- Sedimentation: Visually document sedimentation in vials or use UV-Vis spectroscopy to monitor the change in absorbance at a specific wavelength (e.g., 500 nm) at the top of the dispersion.
- Imaging: Use Scanning Electron Microscopy (SEM) to visually confirm the presence and morphology of agglomerates.
Protocol 2: Determining In Vitro Drug Release Profile
1. Dialysis Method:
- Place a known volume of the drug-loaded nanocarrier dispersion into a dialysis bag (appropriate MWCO).
- Immerse the bag in a large volume of release medium (e.g., PBS at pH 7.4 or a buffer with surfactants to maintain sink conditions) under gentle agitation.
- Maintain the system at 37°C.
2. Sampling and Analysis:
- At predetermined time intervals, withdraw a aliquot from the external release medium.
- Replace with an equal volume of fresh pre-warmed medium to maintain sink conditions.
- Analyze the drug concentration in the aliquots using a validated method (e.g., HPLC or UV-Vis spectroscopy).
- Calculate the cumulative percentage of drug released and plot against time to generate the release profile.
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function & Application |
|---|---|
| DSPE-PEG2000 | A phospholipid-PEG conjugate used for PEGylating lipid-based nanocarriers (liposomes, cubosomes) to reduce opsonization and prolong circulation half-life. [46] |
| Cholesterol | Incorporated into liposomal bilayers to modulate membrane fluidity, reduce permeability, enhance physical stability, and improve drug retention. [47] |
| Pluronic F127 | A non-ionic tri-block copolymer commonly used as a stabilizer in the preparation of cubosomes to prevent aggregation and maintain the cubic phase structure. [48] |
| Glycerol Monooleate (GMO) | A monoglyceride that is a principal lipid component for forming the bicontinuous cubic liquid crystalline structure of cubosomes. [48] |
| Dynamic Light Scattering (DLS) / Zetasizer | An essential instrument for characterizing the hydrodynamic diameter, size distribution (PDI), and zeta potential of nanoparticle dispersions. [49] |
Experimental Workflow and Signaling Pathways
Nanocarrier Stability Assessment Workflow
Strategies to Prolong Nanocarrier Circulation
Troubleshooting Guide: Common Experimental Issues
Q1: My lipid-polymer hybrid nanoparticles (LPHNs) are showing aggregation and poor colloidal stability. What could be the cause? A: This is often related to insufficient steric or electrostatic stabilization. To resolve this:
- Verify stabilizer selection and concentration: Ensure you are using an appropriate steric stabilizer like Polyethylene Glycol (PEG) at a sufficient concentration. Inadequate stabilizer can lead to particle coalescence [50].
- Check zeta potential: Measure the zeta potential of your nanoparticles. A high absolute value (typically > ±30 mV) indicates good electrostatic stabilization, preventing aggregation. A low value suggests your formulation is unstable [51].
- Review processing parameters: High pressure or temperature during manufacturing (e.g., from high-pressure homogenization) can sometimes induce physical instability or crystallinity changes in the nanoparticles [51].
Q2: I am observing a high burst release of the encapsulated peptide from my polymeric nanoparticles. How can I achieve a more controlled release profile? A: A high burst release typically indicates poor entrapment or weak association of the drug with the polymer matrix.
- Optimize polymer selection: Switch to or blend with polymers that have a slower degradation rate. Poly(lactic-co-glycolic acid) (PLGA) with a higher ratio of lactic acid (LA) to glycolic acid (GA) degrades more slowly, offering better release control [50].
- Consider a hybrid system: A core-shell Lipid-Polymer Hybrid Nanoparticle (LPHN) structure is specifically designed to mitigate this issue. The polymeric core provides a stable, controlled-release reservoir, while the lipid shell acts as an additional barrier, reducing the initial burst release [50].
- Adjust formulation parameters: Increase polymer molecular weight or modify the drug-to-polymer ratio to create a denser matrix that slows drug diffusion.
Q3: What are the primary stability concerns for nanosuspensions during storage, and how can I mitigate them? A: The high surface energy of nanoparticles makes them prone to physical instability over time [51].
- Prevent Ostwald Ripening: This is a process where smaller particles dissolve and re-deposit onto larger particles, leading to crystal growth. It can be mitigated by using a narrow initial particle size distribution and selecting a stabilizer that effectively adsorbs to the particle surface, creating a barrier [51].
- Avoid Sedimentation and Agglomeration: While slower sedimentation is a benefit of nanonization, it can still occur. Using viscosifiers in the suspension or transforming the nanosuspension into a dry solid (e.g., via lyophilization) are common strategies to enhance long-term stability [51].
Q4: When should I choose a lipid-polymer hybrid system over a pure lipid or pure polymer nanoparticle? A: LPHNs are advantageous when you need to combine the benefits of both systems while mitigating their individual weaknesses. Select LPHNs if your project requires [50]:
- Enhanced structural stability compared to liposomes or other lipid-based carriers.
- Superior biocompatibility and cellular uptake compared to some polymeric nanoparticles.
- High encapsulation efficiency for both hydrophobic and hydrophilic macromolecules (like peptides/proteins).
- Tunable and controlled drug release kinetics.
Material Selection Data for Nanoparticle Stability
The following table summarizes key properties of different nanocarrier systems that influence their structural stability in circulation.
Table 1: Comparative Analysis of Nanocarrier Systems for Structural Stability
| Material System | Key Advantages for Stability | Key Stability Challenges | Recommended Applications |
|---|---|---|---|
| Lipid-based (e.g., Liposomes, SLNs) | Excellent biocompatibility; Facile surface functionalization [50] | Low structural stability; Premature drug leakage; Poor encapsulation of macromolecules [50] | Delivery of small molecules; Fusogenic applications requiring membrane fusion |
| Polymer-based (e.g., PLGA, PLA) | Rigid matrix provides high stability; Excellent control over drug release profile [50] | Potential biocompatibility concerns; Polymer degradation can affect stability; Use of toxic organic solvents in preparation [50] | Sustained/controlled release delivery; Delivery of hydrophobic drugs |
| Lipid-Polymer Hybrid (LPHNs) | Combines structural stability of polymers with biocompatibility of lipids; Reduced burst release; Enhanced encapsulation efficiency [50] | More complex manufacturing process; Requires optimization of multiple material components [50] | Oral delivery of peptides/proteins (e.g., insulin); Targeted delivery requiring high stability and biocompatibility |
| Drug Nanocrystals | High drug loading; Improved dissolution rate [51] | Particle agglomeration and crystal growth (Ostwald Ripening); Sensitive to changes in the dispersion medium [51] | Delivery of poorly water-soluble drugs via oral or pulmonary routes |
Table 2: Quantitative Stability Targets for Parenteral Nanosuspensions
For injectable formulations, specific quantitative benchmarks are critical for safety and efficacy. The table below outlines key parameters to monitor.
| Parameter | Target Value | Rationale & Characterization Technique | |
|---|---|---|---|
| Particle Size Growth | Maintain initial size distribution (e.g., PDI < 0.2) | Particle growth can indicate instability. Use Dynamic Light Scattering (DLS) for hydrodynamic diameter and Polydispersity Index (PDI) [51]. | |
| Formation of Large Particles | No particles > 5 μm detected | Larger particles in IV injections can cause capillary blockade and embolism. Use Light Obscuration or Liquid Particle Counting [51]. | |
| Zeta Potential | > | ±30 mV | A high absolute zeta potential ensures electrostatic stabilization, preventing aggregation. Measured via Electrophoretic Light Scattering [51]. |
| Crystallinity Change | Maintain desired crystalline/amorphous state | Changes in crystallinity can alter dissolution and stability. Use Differential Scanning Calorimetry (DSC) and X-ray Diffraction (XRD) [51]. |
Experimental Protocols for Stability Assessment
Protocol 1: Assessing In Vitro Serum Stability
Objective: To evaluate the colloidal stability of nanoparticles in a biologically relevant medium, simulating the circulatory system.
- Preparation: Dilute the nanoparticle formulation (e.g., LPHNs, liposomes) in fetal bovine serum (FBS) or phosphate-buffered saline (PBS) with 10% FBS to a specific concentration.
- Incubation: Incubate the mixture at 37°C under gentle agitation to mimic physiological conditions.
- Sampling: Withdraw aliquots at predetermined time points (e.g., 0, 1, 2, 4, 8, 24 hours).
- Analysis: Analyze each sample for:
- Particle Size and PDI: Using Dynamic Light Scattering (DLS). An increase indicates aggregation or protein corona-induced growth [51].
- Zeta Potential: Using Electrophoretic Light Scattering. A change towards neutral values suggests surface coating by serum proteins, which could lead to opsonization [51].
- Interpretation: A formulation that maintains its original size distribution and a moderately negative zeta potential over 24 hours is considered to have good serum stability.
Protocol 2: Preparation of Lipid-Polymer Hybrid Nanoparticles (LPHNs) via Nanoprecipitation
Objective: To fabricate core-shell LPHNs in a reproducible, one-step process.
- Organic Phase: Dissolve the polymer (e.g., PLGA, 50 mg) and a lipophilic stabilizer (e.g., PEG-b-PLA, 10 mg) in a water-miscible organic solvent such as acetone or acetonitrile (20 mL).
- Aqueous Phase: Prepare an aqueous solution (40 mL) containing lipids (e.g., lecithin, 20 mg) and a stabilizer (e.g., sodium cholate, 0.5% w/v). Heat this solution to 40-50°C to ensure lipids are fully dispersed.
- Nanoprecipitation: Under magnetic stirring (500-1000 rpm), rapidly inject the organic phase into the aqueous phase using a syringe pump or manual injection.
- Solvent Removal: Stir the resulting milky suspension for 2-4 hours at room temperature to allow for complete evaporation of the organic solvent. Alternatively, use reduced pressure.
- Purification: Concentrate and purify the nanoparticles by centrifugation or ultrafiltration. Resuspend the pellet in the desired buffer (e.g., PBS) for further characterization [50].
Experimental Workflow and Material Selection Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Lipid-Polymer Hybrid Nanoparticle Development
| Research Reagent | Primary Function in Formulation |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer forming the core; provides structural integrity and controls drug release kinetics [50]. |
| PEG-lipid (e.g., DSPE-PEG) | Lipid conjugated to polyethylene glycol; used as a steric stabilizer to reduce protein adsorption (opsonization) and prolong circulation time [50]. |
| Lecithin | A natural phospholipid; a key component of the lipid shell, providing biocompatibility and enhancing cellular uptake [50]. |
| Poloxamer 188 | A non-ionic triblock copolymer surfactant; used as a stabilizer to prevent nanoparticle aggregation during and after synthesis [51]. |
| Trehalose | A disaccharide cryoprotectant; used to stabilize nanoparticles during lyophilization (freeze-drying) by forming a glassy matrix, preventing fusion and aggregation [51]. |
| DSPC (Distearoylphosphatidylcholine) | A saturated phospholipid with a high phase transition temperature; contributes to the formation of a rigid and stable lipid bilayer shell in LPHNs [50]. |
Green Synthesis Methods for Improved Biocompatibility and Stability
Troubleshooting Guides
Troubleshooting Green Synthesis with Plant Extracts
Table 1: Common Issues in Plant-Mediated Green Synthesis
| Problem | Possible Root Cause | Solution | Preventive Measures |
|---|---|---|---|
| Irregular Size & Shape [52] | Non-standardized plant extract; variable phytochemical composition. | Standardize extract by quantifying key bioactive compounds (e.g., total phenolic content) [52]. | Use plants from the same geographical source and harvest season; characterize extract beforehand [52]. |
| Rapid Aggregation & Low Stability [53] [52] | Inefficient capping by phytochemicals; weak stabilization. | Optimize reaction pH and temperature; increase plant extract to metal salt ratio [52]. | Use plant extracts rich in stabilizing agents (e.g., flavonoids, terpenoids) [53] [52]. |
| Low Synthesis Yield [52] | Insufficient reaction time; suboptimal temperature. | Extend reaction time; increase temperature within a moderate range (e.g., 60-80°C) [52]. | Monitor color change visually and via UV-Vis spectroscopy to determine optimal reaction endpoint [53]. |
| Poor Reproducibility [52] | Batch-to-batch variation in plant extract composition. | Document plant source, growth stage, and extraction protocol meticulously [52]. | Create a large, homogenized batch of plant extract for a full set of experiments [52]. |
| High Toxicity/Cytotoxicity | Residual bioactive phytochemicals on NP surface. | Purify synthesized nanoparticles via repeated centrifugation and washing [54]. | Select plant extracts known for biocompatibility and test different purification methods [54] [55]. |
Troubleshooting Biocompatibility and Circulation Stability
Table 2: Addressing Biocompatibility and In Vivo Performance Issues
| Problem | Possible Root Cause | Solution | Preventive Measures |
|---|---|---|---|
| Short Systemic Circulation Lifetime [4] | Nanoparticle elasticity is not optimized for prolonged circulation. | Tune nanoparticle elasticity; intermediate ranges (e.g., 75-700 kPa) show longer circulation in models [4]. | Design nanoparticles with tunable, intermediate elasticity and screen in vitro for protein corona composition [4]. |
| Unfavorable Protein Corona Formation [4] | Nanoparticle surface promotes adsorption of opsonins that trigger immune clearance. | Engineer surface with "stealth" coatings like PEG; modulate elasticity to recruit specific proteins like ApoA1 [4]. | Pre-coat nanoparticles with a pre-formed corona of dysopsonic proteins (e.g., ApoA1) during synthesis [4]. |
| Uptake by Reticuloendothelial System (RES) | Surface properties lead to opsonization and clearance by liver/spleen macrophages. | Functionalize surface with hydrophilic polymers (e.g., PEG) to reduce protein adsorption and improve stealth properties [54] [4]. | Optimize surface charge to near-neutral zeta-potential and ensure small, uniform size (<150 nm) [54]. |
| Inflammatory or Immune Response [54] | Material composition or surface properties trigger innate immune recognition (e.g., for some metal NPs). | Use biodegradable and biocompatible materials (e.g., PLGA, chitosan); employ green synthesis for better biocompatibility [54] [55]. | Select materials with known low immunogenicity (e.g., PEG, PLGA) and leverage green synthesis to create bio-friendly surfaces [54] [53]. |
Frequently Asked Questions (FAQs)
Synthesis & Optimization
Q1: What are the primary advantages of green synthesis over chemical methods for biomedical nanoparticles?
Green synthesis is eco-friendly, cost-effective, and utilizes non-toxic reagents. It often uses plant extracts or microorganisms where bioactive compounds (e.g., phenolics, terpenoids) act as reducing and capping agents. This process can result in nanoparticles with enhanced biocompatibility and stability, which are critical for biomedical applications like drug delivery and diagnostics [53] [56] [55].
Q2: Which factors most significantly influence the size and shape of green-synthesized nanoparticles?
Key factors include [53] [52]:
- Phytochemical Composition: The type and concentration of reducing agents in the plant extract.
- Reaction pH: Influences the reduction rate and nucleation of metal ions.
- Temperature: Higher temperatures often accelerate reduction and affect particle growth.
- Reaction Time: Insufficient time can lead to incomplete reduction, while excessive time may cause aggregation.
- Concentration of Metal Salt and Extract: The ratio directly impacts nucleation and growth dynamics.
Q3: How can I improve the batch-to-batch reproducibility of plant-mediated nanoparticle synthesis?
Reproducibility requires strict standardization [52]:
- Source Control: Use the same plant species, organ (leaf, root), geographical source, and harvest season.
- Extraction Protocol: Standardize the solvent, temperature, duration, and solid-to-liquid ratio for extraction.
- Characterization: Pre-characterize plant extracts for key phytochemicals to ensure consistency before synthesis.
Characterization & Biocompatibility
Q4: What are the essential characterization techniques for green-synthesized nanoparticles intended for drug delivery?
A core set of techniques is mandatory [53]:
- UV-Vis Spectroscopy: Confirms nanoparticle formation via Surface Plasmon Resonance.
- Dynamic Light Scattering (DLS): Determines hydrodynamic size distribution and polydispersity index.
- Zeta Potential: Measures surface charge, indicating colloidal stability.
- Electron Microscopy (SEM/TEM): Reveals detailed morphology, size, and shape.
- FTIR Spectroscopy: Identifies functional groups from phytochemicals capping the nanoparticles.
Q5: Why is nanoparticle elasticity important for systemic circulation, and how can I measure it?
Nanoparticle elasticity directly impacts blood circulation lifetime. Studies show a non-monotonic relationship, where nanoparticles with intermediate elasticity (e.g., 75-700 kPa) have the longest circulation times. This is because elasticity influences the composition of the protein corona, particularly the enrichment of Apolipoprotein A-I (ApoA1), which is associated with prolonged circulation [4]. Techniques like Atomic Force Microscopy (AFM) can be used to measure the nanomechanical properties (Young's modulus) of nanoparticles [4].
Q6: What is the role of the protein corona, and how does green synthesis affect it?
Upon entering a biological fluid, nanoparticles are immediately coated with proteins, forming a "protein corona." This corona defines the nanoparticle's biological identity, influencing its interaction with cells, immune response, and biodistribution [4]. Green-synthesized nanoparticles, by virtue of their bio-derived capping agents, may form a more biocompatible corona. Furthermore, the core material's elasticity—which can be tuned during synthesis—has been shown to be a critical factor in determining corona composition, independent of surface chemistry [4].
Experimental Protocols
Detailed Protocol: Plant-Mediated Synthesis of Silver Nanoparticles (AgNPs)
This protocol is adapted for reproducibility and high biocompatibility, suitable for subsequent drug loading and circulation studies [53] [52].
1. Reagent Preparation:
- Plant Extract: Wash 10 g of fresh plant leaves (e.g., Azadirachta indica) thoroughly. Boil in 100 mL deionized water for 20 min. Filter the solution through Whatman No. 1 filter paper. The extract can be stored at 4°C for short-term use.
- Metal Salt Solution: Prepare a 1 mM aqueous solution of Silver Nitrate (AgNO₃) in deionized water. Store in a dark bottle.
2. Synthesis Procedure:
- Add 5 mL of plant extract dropwise to 95 mL of the 1 mM AgNO₃ solution under constant magnetic stirring (500 rpm) at room temperature.
- Observe the color change from colorless to brownish-yellow, indicating the formation of AgNPs.
- Continue stirring for 2 hours to ensure complete reaction.
- Critical Step: Record the exact parameters: plant source, extract concentration, pH, temperature, and reaction time.
3. Purification and Recovery:
- Centrifuge the reaction mixture at 15,000 rpm for 30 minutes.
- Discard the supernatant and re-disperse the pellet in deionized water. Repeat this washing process three times to remove any unreacted phytochemicals or silver ions.
- Re-suspend the final pellet in 10 mL of deionized water or a suitable buffer (e.g., PBS for biological studies).
- Lyophilize a portion of the purified NPs for long-term storage and characterization.
4. Characterization:
- UV-Vis: Scan from 300-600 nm; a peak between 400-450 nm confirms AgNP synthesis.
- DLS & Zeta Potential: Measure hydrodynamic size, PDI, and surface charge.
- TEM: Confirm size, shape, and monodispersity.
- FTIR: Analyze the capping agents on the NP surface.
Detailed Protocol: Evaluating the Role of Elasticity on Circulation
This protocol outlines a method to correlate nanoparticle elasticity with protein corona formation and systemic circulation lifetime, a key aspect of stability research [4].
1. Model Nanoparticle Preparation:
- Synthesize a series of core-shell nanoparticles with identical size, shape, and surface chemistry (e.g., PEGylated lipid bilayer shell) but varying core elasticity. This can be achieved by using hydrogel cores with different cross-linking densities [4].
- Include controls: a soft nanoparticle (e.g., liposome, ~45 kPa) and a stiff nanoparticle (e.g., PLGA, ~760 MPa) [4].
- Characterize all nanoparticles to ensure uniformity in hydrodynamic diameter and surface charge.
2. In Vitro Protein Corona Analysis:
- Incubate each type of nanoparticle with mouse plasma (or human plasma) at a physiological temperature (37°C) for a set time (e.g., 1 hour).
- Isolate the nanoparticle-protein corona complexes via ultracentrifugation.
- Wash the complexes gently to remove loosely associated proteins.
- Elute the hard corona proteins and identify/quantify them using techniques like SDS-PAGE and Liquid Chromatography-Mass Spectrometry (LC-MS).
- Data Analysis: Correlate the abundance of specific proteins (e.g., ApoA1) with nanoparticle elasticity.
3. In Vivo Circulation Lifetime Study:
- Label the different elasticity nanoparticles with a near-infrared (NIR) dye.
- Administer the nanoparticles intravenously to mouse models (e.g., BALB/c mice) at a standardized dose.
- Collect blood samples at predetermined time intervals (e.g., 0.5, 1, 2, 4, 8, 12, 24 hours) post-injection.
- Measure the fluorescence intensity in the blood samples to determine the concentration of nanoparticles remaining in circulation over time.
- Calculate pharmacokinetic parameters like half-life (t₁/₂).
- Correlation: Plot circulation lifetime against nanoparticle elasticity and against the relative abundance of key corona proteins (e.g., ApoA1) identified in the in vitro study.
Diagrams
Green Synthesis Workflow
Elasticity-Circulation Relationship
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for Green Synthesis and Stability Research
| Category | Item / Reagent | Function & Application Notes |
|---|---|---|
| Green Synthesis | Plant Material (e.g., leaves, roots) | Source of phytochemicals (phenolics, flavonoids) that act as reducing and capping agents. Select based on documented bioactivity [53] [52]. |
| Metal Salts (e.g., AgNO₃, HAuCl₄, ZnAc₂) | Precursors for forming metallic nanoparticles (Ag, Au, ZnO). Use high-purity grades [53] [52]. | |
| Solvents (Deionized Water, Ethanol) | Extraction medium. Water is preferred for its green and non-toxic properties [55]. | |
| Nanoparticle Engineering | PEGylated Lipids (e.g., DSPE-PEG2000) | Used to create a stealth lipid bilayer shell on nanoparticles to reduce protein adsorption and improve circulation time [4]. |
| Polymeric Cores (e.g., PLGA, Polyacrylamide) | Used to fabricate nanoparticles with tunable elasticity. Cross-linking density can be adjusted to modulate stiffness [4]. | |
| Characterization | DLS/Zeta Potential Analyzer | Essential instrument for measuring hydrodynamic size, size distribution (PDI), and surface charge, which predicts colloidal stability [53] [4]. |
| UV-Vis Spectrophotometer | Used for initial confirmation of nanoparticle synthesis via Surface Plasmon Resonance absorption measurement [53]. | |
| Transmission Electron Microscope (TEM) | Provides high-resolution imaging of core nanoparticle size, shape, and morphology [53] [4]. | |
| Stability & Biocompatibility Assays | Animal Plasma/Serum (e.g., Mouse, Human) | Used for in vitro protein corona formation studies to predict in vivo behavior [4]. |
| Cell Lines (e.g., Macrophages, HEK293) | For in vitro cytotoxicity (MTT assay) and cellular uptake studies to preliminarily assess biocompatibility [54]. |
Optimization Frameworks and Stability Enhancement Protocols
Systematic Optimization Using Design of Experiments (DoE) Methodology
FAQs: DoE in Nanoparticle Formulation
Q1: What are the key factors to investigate when using DoE for nanoparticle stability? The liquid-to-solid lipid ratio (Liq:So) and the proportion of total lipids to surfactants (TL:Sur) are statistically significant predictors for optimizing particle size stability [57]. These factors should be included as primary factors in your experimental design.
Q2: How can I quantitatively define "stability" as a response factor in my DoE? You can define stability using a time-based unit (days). A formulation is considered stable at a given measurement point if it meets three criteria simultaneously [57]:
- Z-average variation is under 8%.
- Polydispersity Index (PdI) is under 0.2.
- The sample mean particle size does not deviate by more than 5.0% within three consecutive readings. The stability endpoint is recorded as the number of days elapsed until the prior measurement before these criteria are no longer met [57].
Q3: Why is my DoE model for nanoparticle stability not statistically significant? The choice of how you measure the response factor is critical. Using simple particle size variation (ΔZ-average in nanometers) over a fixed period may not yield a significant model due to the different root causes of instability (e.g., aggregation vs. Ostwald ripening) [57]. A quadratic model using stability-in-days has been shown to provide a significant fit (p < 0.05) with high predictive accuracy (R² of 81.37%) [57].
Q4: What is a common mistake when setting up a DoE for failure analysis? A common mistake is testing too many variables at once. To effectively pinpoint the cause of a problem, you should test one variable or solution at a time. This minimizes complications and makes it easier to identify the most effective fix [58].
Q5: How many experimental runs are needed for a reliable DoE? You must test enough units to achieve a statistically significant result. For formulation DoE, a Central Composite Design (CCD) with 14 runs, including a center point in sextuplicate, has been successfully used [57]. For failure testing, a rule of thumb is that to validate a solution for an issue with a failure rate of p, you should test at least n = 3/p units with zero observed failures [58].
Troubleshooting Guides
Problem: Unpredictable Nanoparticle Aggregation During Storage
| # | Problem Description | Possible Cause | Solution |
|---|---|---|---|
| 2.1 | Rapid particle growth and increased PdI within days of preparation. | Suboptimal liquid-to-solid lipid ratio, leading to matrix instability and Ostwald ripening [57]. | Use a CCD to model the effect of Liq:So and TL:Sur ratios. The contour plot of the model will identify a stable zone, often at higher solid lipid content [57]. |
| 2.2 | Failed DoE model; unable to identify significant factors affecting stability. | Using an inappropriate response factor (e.g., Z-average change alone) that does not accurately capture the stability phenomenon [57]. | Adopt a multi-parameter stability measure (size variation, PdI, reading quality) expressed in days as your DoE response factor [57]. |
| 2.3 | DoE results are not reproducible in scaled-up production. | Kitting or assembly errors during the DoE, where units are built with the wrong configuration [58]. | Practice hyper-vigilance during the assembly of test units. Keep impeccable records and perform in-person validation to ensure the correct parts are used for each configuration [58]. |
Experimental Protocols & Data
Protocol: DoE for Nanostructured Lipid Carrier (NLC) Optimization
1. Objective: To optimize NLC formulation for maximum particle size stability using a Central Composite Design (CCD) [57].
2. Experimental Design:
- Design Type: Central Composite Design (CCD) [57].
- Factors (Predictors): Liquid-to-Solid Lipid Ratio (Liq:So), Total Lipids-to-Surfactants Ratio (TL:Sur) [57].
- Response Factor: Particle Size Stability (in days), determined by the criteria in FAQ #2 [57].
- Number of Runs: 14 experiments, including a center point in sextuplicate to test reproducibility [57].
3. Methodology (Adapted Solvent Injection Technique):
- Prepare NLCs using a solvent injection method.
- Use a natural seed butter (e.g., tucuman butter) as the solid lipid and a resin oil (e.g., copaiba oil) as the liquid lipid to accentuate instability for model testing [57].
- After preparation, measure the particle size (Z-average) and PdI of each formulation weekly for 28 days using Dynamic Light Scattering (DLS) [57].
- For each measurement, record the three parameters (Z-average variation, PdI, and reading deviation) to determine the stability endpoint for each formulation [57].
4. Data Analysis:
- Analyze the data using multiple linear regression.
- Fit the data to both linear and quadratic models.
- Select the quadratic model if it shows a higher regression coefficient (R²) and a statistically significant p-value (p < 0.05) [57].
- Use the resulting model and its contour plot to identify the factor level combinations that predict the highest stability [57].
Quantitative Data from a DoE Study on NLC Stability
The table below summarizes experimental data and results from a published DoE study optimizing NLC stability [57].
Table 1: Central Composite Design and Response Data for NLC Optimization
| Experiment No. | Factor A: Liq:So | Factor B: TL:Sur | Response: Stability (Days) |
|---|---|---|---|
| 1 | 2.000 | 1.000 | 28 |
| 2 | 0.189 | 1.750 | 21 |
| 3 | 1.250 | 2.810 | 21 |
| 4 | 0.500 | 1.000 | 21 |
| 5 | 1.250 | 1.750 | 7 |
| 6 | 1.250 | 1.750 | 7 |
| 7 | 1.250 | 1.750 | 14 |
| 8 | 1.250 | 1.750 | 7 |
| 9 | 1.250 | 0.690 | 21 |
| 10 | 0.500 | 2.500 | 28 |
| 11 | 1.250 | 1.750 | 14 |
| 12 | 1.250 | 1.750 | 14 |
| 13 | 2.000 | 2.500 | 28 |
| 14 | 2.311 | 1.750 | 21 |
Table 2: Statistical Parameters for the DoE Quadratic Model [57]
| Statistical Parameter | Value for Stability (Days) Model |
|---|---|
| R² (Regression Coefficient) | 81.37% |
| Adjusted R² | 69.72% |
| p-value | 0.001 |
| F-value | 16.77 |
| Standard Deviation | 4.19 |
Experimental Workflow Visualization
DoE for Nanoparticle Stability
Research Reagent Solutions
Table 3: Essential Materials for Lipid Nanoparticle Formulation and Characterization
| Reagent / Material | Function in Experiment |
|---|---|
| Solid Lipid (e.g., Tucuman Butter) | Forms the solid crystalline matrix of the nanostructured lipid carrier (NLC), providing structure [57]. |
| Liquid Lipid (e.g., Copaiba Oil) | Incorporated into the solid matrix to create imperfections, increasing drug loading capacity and potentially influencing stability [57]. |
| Surfactants (Types vary) | Stabilizes the lipid-water interface during and after nanoparticle formation, preventing aggregation. The ratio to total lipids (TL:Sur) is a critical factor [57]. |
| Solvent (for injection method) | Dissolves lipids for the preparation process via solvent injection, a simple and efficient laboratory method [57]. |
| Dynamic Light Scattering (DLS) Instrument | Measures particle size (Z-average), size distribution, and Polydispersity Index (PdI) for stability assessment [57]. |
| Central Composite Design (CCD) Software | Generates the set of experimental runs, randomizes the order, and performs multiple linear regression analysis on the resulting data [57]. |
FAQs on Critical Quality Attributes (CQAs) for Nanoparticle Stability
1. What are the most critical attributes to control for ensuring nanoparticle stability in circulation? The most critical attributes are size, size distribution (polydispersity), surface charge (zeta potential), and surface chemistry [59] [60]. Stability is defined as the preservation of these key nanostructure properties, which directly influence biological behavior [8]. Maintaining these CQAs is essential to prevent aggregation, ensure consistent drug release profiles, and achieve the desired circulation time and targeting efficiency [59] [60].
2. How does nanoparticle size influence performance in drug delivery? Size is a primary determinant of a nanoparticle's fate in vivo. It critically impacts the circulation half-life, biodistribution, and the ability to extravasate at target sites like tumors through the Enhanced Permeability and Retention (EPR) effect [60]. Precise size control is necessary because it is directly related to the nanoparticle's surface area, energy, and its interactions with biological components [8].
3. Why is surface charge (zeta potential) a key CQA? Zeta potential indicates the surface charge and colloidal stability of a nanoparticle suspension [8]. A high absolute value of zeta potential (typically > |±20| mV) suggests strong electrostatic repulsion between particles, which helps prevent aggregation during storage and in biological fluids [8]. Surface charge also significantly influences interactions with cell membranes and plasma proteins, which can affect toxicity and targeting [60].
4. What are the biggest challenges in controlling CQAs during development? The main challenges include the complexity of nanoparticles as multi-component 3D constructs and the lack of a single analytical method to fully characterize them [59] [60]. Subtle variations in composition or manufacturing can drastically alter the CQAs and the final product's performance. Furthermore, characterizing CQAs in complex biological matrices (e.g., plasma) is particularly challenging due to the formation of a protein corona that can mask the nanoparticle's original properties [59].
Troubleshooting Guides
Issue 1: Nanoparticle Aggregation During Storage or in Biological Media
Potential Causes and Solutions:
- Cause: Inadequate Surface Charge. Low zeta potential reduces electrostatic repulsion.
- Cause: Suboptimal pH or Ionic Strength.
- Solution: Ensure the pH of the formulation buffer is appropriate. For example, antibody conjugations often work best at a pH of 7-8. Use buffers designed for conjugation to maintain molecule integrity and prevent aggregation triggered by environmental shifts [61].
- Cause: High Nanoparticle Concentration.
- Solution: Follow recommended concentration guidelines. If aggregation occurs, dilute the sample or use a sonicator to disperse nanoparticles evenly before use [61].
- Cause: Interaction with Biological Components.
Issue 2: Inconsistent Sizing Data Between Different Characterization Techniques
Potential Causes and Solutions:
- Cause: Use of Non-Orthogonal Techniques. Different techniques measure different aspects of size (e.g., hydrodynamic radius vs. molecular weight).
- Solution: Employ an orthogonal and complementary characterization approach [59]. Use a suite of techniques based on different physical principles to get a comprehensive understanding. For instance, use Dynamic Light Scattering (DLS) for hydrodynamic size, Analytical Ultracentrifugation (AUC) for molecular weight and density, and Transmission Electron Microscopy (TEM) for direct visualization of core morphology [59].
- Cause: Presence of Aggregates or Impurities.
- Solution: Incorporate fractionation techniques like Size Exclusion Chromatography (SEC) or Asymmetric Flow Field-Flow Fractionation (AF4) coupled with multiple detectors to separate and analyze different populations within the sample [59].
Issue 3: High Polydispersity Indicating a Heterogeneous Product
Potential Causes and Solutions:
- Cause: Uncontrolled Synthesis or Conjugation Process.
- Solution: Optimize and tightly control critical process parameters (CPPs) such as reaction time, temperature, and reagent addition rates. Reproducible, scalable manufacturing processes are essential for a consistent product [60].
- Cause: Incomplete or Variable Drug Loading.
Issue 4: Rapid Clearance from Circulation
Potential Causes and Solutions:
- Cause: Unfavorable Surface Charge Leading to Opsonization.
- Solution: Engineer a near-neutral or slightly negative surface charge using hydrophilic polymers like PEG. This "stealth" effect reduces opsonization and uptake by the mononuclear phagocyte system (MPS), prolonging circulation time [60].
- Cause: Large Size or Broad Size Distribution.
- Solution: Control particle size to within an optimal range (typically 10-100 nm) and minimize polydispersity to ensure uniform hemodynamic properties and avoid filtration by the spleen or capture in the liver [60].
Experimental Protocols for CQA Analysis
Protocol 1: Orthogonal Characterization of Nanoparticle Size and Molecular Weight
Method: A multi-step, incremental complexity approach as deployed for the characterization of AZD0466, a drug-dendrimer conjugate [59].
Workflow:
- Pre-screening (Batch Mode):
- Technique: Dynamic Light Scattering (DLS).
- Procedure: Measure the hydrodynamic diameter and polydispersity index (PDI) of the nanoparticle sample in a standard buffer. This provides a quick assessment of colloidal stability and size distribution.
- Advanced Fractionation and Sizing:
- Technique: Size Exclusion Chromatography (SEC) or Asymmetric Flow Field-Flow Fractionation (AF4) coupled with multi-angle light scattering (MALS), DLS, and refractive index (RI) detectors.
- Procedure: Inject the sample onto the column (SEC) or channel (AF4). The fractionation system separates nanoparticles based on size. The coupled detectors provide absolute molecular weight (from MALS), hydrodynamic size (from online DLS), and concentration (from RI) for each fraction.
- High-Resolution Analysis:
- Technique: Analytical Ultracentrifugation (AUC).
- Procedure: Subject the nanoparticle sample to high centrifugal forces. Monitor the sedimentation behavior to determine the sedimentation coefficient, which provides information on molecular weight, density, and conformation without the need for a stationary phase.
- Morphology Assessment:
- Technique: Transmission Electron Microscopy (TEM).
- Procedure: Deposit a diluted sample onto a carbon-coated grid, stain if necessary, and image under high vacuum. This provides direct, high-resolution information on the core size, shape, and morphology.
Protocol 2: Assessing Physical Stability and Drug Release in Biological Media
Method: Evaluating stability and drug release profiles in the presence of plasma proteins to predict in vivo performance [59].
Workflow:
- Sample Incubation:
- Incubate the nanoparticle formulation (e.g., AZD0466) with human plasma or a simulated biological fluid at 37°C under gentle agitation for a predetermined time (e.g., 1, 6, 24 hours).
- Analysis of Physical Stability:
- Technique: DLS, AF4, or AUC.
- Procedure: At each time point, withdraw an aliquot. Analyze changes in particle size, size distribution, and molecular weight using the orthogonal techniques described in Protocol 1. An increase in size or a shift in the size distribution profile indicates aggregation or protein corona formation.
- Analysis of Drug Release:
- Technique: Dialysis or centrifugation followed by HPLC/UV-Vis.
- Procedure: Separate the released free drug from the nanoparticle conjugate (e.g., via centrifugation using a molecular weight cutoff filter). Quantify the amount of free drug in the filtrate using a validated analytical method like HPLC. This provides a drug release kinetic profile.
Table 1: Target Ranges and Measurement Techniques for Key CQAs
| Critical Quality Attribute (CQA) | Target or Acceptable Range | Key Measurement Techniques | Impact on Performance | ||
|---|---|---|---|---|---|
| Size & Size Distribution | • Drug delivery: ~10-100 nm [60]• Narrow PDI is critical | • DLS (hydrodynamic size) [59] [8]• SEC/AF4-MALS (absolute size)• TEM (core morphology) [59] [8]• AUC [59] | • Circulation time, biodistribution, EPR effect, targeting [60] | ||
| Surface Charge (Zeta Potential) | • > | ±20 | mV for good colloidal stability [8]• Near-neutral for stealth properties | • Zeta potential analysis [8] | • Colloidal stability, protein corona formation, cellular uptake, potential toxicity [8] [60] |
| Drug Loading & Release | • High loading capacity• Controlled, sustained release profile | • HPLC/UV-Vis (loading & release) [59]• Dialysis methods | • Therapeutic efficacy, dosing frequency, safety profile [60] | ||
| Surface Chemistry & Morphology | • Consistent surface functionalization• Defined morphology | • TEM [59]• Small-Angle Neutron Scattering (SANS) [59]• X-ray Photoelectron Spectroscopy (XPS) [8] | • Biocompatibility, stealth properties, targeting capability, drug release kinetics [59] [60] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents for Nanoparticle Formulation and CQA Control
| Reagent / Material | Function / Purpose | Example Use Case |
|---|---|---|
| PEG (Polyethylene Glycol) | Provides "stealth" properties by steric stabilization; reduces opsonization and MPS uptake, thereby prolonging circulation half-life [60]. | Grafting to nanoparticle surface to improve stability in biological fluids. |
| BSA (Bovine Serum Albumin) | Used as a blocking agent to prevent non-specific binding in diagnostics [61]. Also used as a carrier for hydrophobic drugs (e.g., in Abraxane) [60]. | Added during conjugation steps or assay development to reduce background noise. |
| Stabilizing Agents (e.g., PVP, Poloxamers) | Prevent nanoparticle aggregation during synthesis and storage by providing steric or electrostatic stabilization [8]. | Included in formulation buffers to maintain colloidal stability. |
| Functional Ligands (e.g., Antibodies, Peptides, Folate) | Enable active targeting of nanoparticles to specific cells or tissues (e.g., receptors overexpressed on cancer cells) [60]. | Conjugated to nanoparticle surface for targeted drug delivery. |
| High-Purity Buffers | Maintain optimal pH and ionic strength for conjugation reactions and long-term storage stability [61]. | Used during bioconjugation to ensure efficient binding and maintain biomolecule integrity. |
Strategies for Minimizing Protein Corona Formation and Manipulation
This technical support center provides practical guidance for researchers working to control protein corona formation on nanoparticles, a critical factor in improving nanoparticle structural stability and efficacy in circulation.
Frequently Asked Questions
How does nanoparticle elasticity influence protein corona formation and circulation lifetime? Research shows that nanoparticle elasticity has a non-monotonic relationship with systemic circulation lifetime. Using core-shell nanoparticles with identical PEGylated lipid bilayer shells but cores of different elasticity (45 kPa to 760 MPa), scientists observed that intermediate elasticity nanoparticles (75-700 kPa) showed the longest circulation times. This correlates with the preferential adsorption of apolipoprotein A-I (ApoA1) on particles of intermediate elasticity, which strongly correlates with extended blood circulation. Surface chemistry had less impact than elasticity, suggesting elasticity is a dominant factor [4].
What are the key challenges in isolating and studying the protein corona on lipid nanoparticles (LNPs)? The main challenges include:
- Separation difficulties: LNPs have similar size and composition to endogenous particles in biofluids (e.g., exosomes, lipoproteins), making clean isolation problematic [14].
- Low density: LNPs are buoyant in common buffers and cannot be pelleted with standard centrifugation without risking aggregation or disruption [14].
- Methodological artifacts: Techniques requiring nanoparticle modification (e.g., photoaffinity-based, magnetic-based) may alter corona formation, while methods relying on PEG targeting may be biased by PEG desorption [14].
Can we exploit protein corona formation for beneficial outcomes rather than preventing it? Yes, strategic manipulation of protein corona is a promising approach. Studies with chitosan-based nanoparticles demonstrated that corona formation can be controlled to improve biodistribution. Nanoparticles with specifically engineered coronas showed low liver uptake and notable heart blood pool accumulation, indicating longer circulation times - favorable for drug delivery applications [62].
Troubleshooting Guide
Protein Corona Interference with Cellular Uptake and Transfection
Table 1: Troubleshooting Protein Corona Effects on Delivery Efficiency
| Observed Problem | Potential Cause | Solutions to Consider |
|---|---|---|
| High cellular uptake but low protein expression from mRNA-LNPs | Protein corona redirecting intracellular trafficking to lysosomal compartments, hindering endosomal escape [14] | - Pre-form corona with selected proteins- Modify LNP surface chemistry to influence corona composition- Incorporate endosomolytic lipids to improve escape |
| Rapid clearance from circulation | Corona contains opsonins that promote immune recognition and clearance [62] | - Optimize nanoparticle elasticity (aim for intermediate range)- Use hydrophilic polymer coatings (e.g., PEG, dextran)- Engineer surface to preferentially adsorb "stealth" proteins |
| Inconsistent corona formation between experiments | Variable incubation conditions or isolation methods | - Standardize protein source and concentration- Control temperature and time of incubation- Validate corona isolation efficiency |
Experimental Workflow for Protein Corona Isolation
The following diagram illustrates a refined density gradient ultracentrifugation workflow for effective isolation of protein corona on lipid nanoparticles:
Detailed Protocol:
- Incubation: Incubate LNPs with human blood plasma (or other biofluid) at 37°C for 1 hour to allow corona formation [14] [62].
- Gradient Preparation: Prepare continuous density gradient medium in ultracentrifugation tubes.
- Sample Loading: Carefully load the protein-LNP complex mixture onto the pre-formed gradient.
- Ultracentrifugation: Centrifuge at approximately 160,000 × g for 16-24 hours at 4°C. This extended duration is crucial for effective separation from endogenous particles [14].
- Fraction Collection: Gently fractionate the gradient from the top, collecting the LNP-containing bands.
- Washing: Wash collected fractions with phosphate buffer (pH 7.4) to remove loosely associated proteins (soft corona) if analyzing the hard corona only [62].
- Analysis: Proceed with proteomic analysis (LC-MS/MS) to identify corona proteins, normalizing to protein composition in the biofluid alone [14].
Surface Coating Strategies to Minimize Corona Formation
The Scientist's Toolkit
Table 2: Essential Research Reagents for Protein Corona Studies
| Reagent/Category | Specific Examples | Function in Corona Research |
|---|---|---|
| Ionizable Lipids | C12-200, DLin-MC3-DMA | Form core LNP structure; influence protein adsorption based on pKa and charge [63] |
| PEGylated Lipids | DMG-PEG2000, DSPE-PEG2000 | Provide stealth properties, reduce opsonization, improve circulation time [63] |
| Structural Lipids | DSPC, DOPE, Cholesterol | Maintain nanoparticle integrity; cholesterol enhances stability [63] |
| Polymeric Coatings | Chitosan, Carboxymethyl Dextran (CMD), Thiolated Dextran (TD) | Form polyelectrolyte complexes (PECs) that can be engineered to control corona composition [62] |
| Hydrogel Cores | Polyacrylamide-based cores of varying crosslink density | Enable controlled modulation of nanoparticle elasticity without changing surface chemistry [4] |
Key Methodological Considerations
- Include Proper Controls: Always run parallel experiments with plasma/serum alone to distinguish proteins truly associated with LNPs from those bound to endogenous particles [14].
- Standardize Corona Washing: For "hard corona" analysis, implement consistent washing procedures (typically 2× with PBS, pH 7.4) to remove loosely associated proteins [62].
- Validate Nanoparticle Integrity: After corona isolation, check that LNPs remain intact and non-aggregated using dynamic light scattering [14].
- Consider Physiological Relevance: Use human plasma rather than depleted sources when possible to capture biologically relevant interactions with apolipoproteins and other proteins [14].
Frequently Asked Questions (FAQs)
How does nanoparticle elasticity influence circulation time?
Nanoparticle elasticity is a crucial, tunable property that significantly impacts biological performance. Tuning elasticity can lead to enhanced blood circulation times by helping nanoparticles avoid rapid interception by the body's defense cells, particularly hepatic macrophages (Kupffer cells). Softer, more elastic particles can exhibit prolonged circulation, which is a prerequisite for effective drug delivery to pathological sites [64] [65].
My nanoparticles are being cleared from the blood too quickly. Could elasticity be a factor?
Yes, rapid clearance is a common challenge. The liver's Kupffer cells are highly efficient at scavenging rigid colloidal particles from the bloodstream. If your nanoparticles are too rigid, they are likely being recognized and removed by these cells within minutes. Modulating elasticity towards a softer, more deformable character is a recognized strategy to confer longevity, allowing particles to remain in circulation for hours instead of minutes [65].
What are the key strategies for modulating nanoparticle elasticity?
Elasticity can be engineered through several design parameters:
- Composition: The choice of polymer or lipid directly influences intrinsic material properties.
- Crosslinking Density: This is a primary control lever; reducing the degree of crosslinking within a particle generally increases its deformability.
- Structural Design: Architectural features, such as a hollow core or a layered shell, can be leveraged to enhance overall particle softness [64].
How does elasticity compare to other physicochemical properties like size and charge?
While size, charge, and surface chemistry are well-studied and critical, focusing on them alone is often insufficient to overcome complex biological barriers. Elasticity is gaining recognition as an equally important, independent parameter. Optimizing elasticity can work in concert with these other properties to improve a nanoparticle's ability to navigate biological hydrogels like the extracellular matrix, which is essential for reaching target tissues [64].
Are there trade-offs when optimizing for elasticity?
Potentially, yes. A key consideration is that the optimal properties for one biological stage may be detrimental for another. For instance, while a specific surface modification like PEGylation can aid in penetrating mucus barriers, it might simultaneously reduce cellular uptake. The therapeutic goal must guide the design, as elasticity must be tuned in accordance with specific needs, balancing circulation time, barrier penetration, and eventual drug release [64] [65].
Troubleshooting Guides
Problem: Short Circulation Half-Life
Potential Cause and Solution:
- Cause: Nanoparticles are too rigid, leading to rapid recognition and phagocytosis by Kupffer cells in the liver [65].
- Solution:
- Reduce Crosslinking: If using crosslinked polymers (e.g., in hydrogel nanoparticles), systematically lower the crosslinker density during synthesis.
- Softer Materials: Formulate nanoparticles using inherently softer, more deformable materials (e.g., certain liposomes or low-modulus polymers).
- Biomimetic Camouflage: Coat particles with mimicking strategies derived from the body's own cells or pathogens, which often have soft, stealth-like properties to evade immune detection [65].
Experimental Protocol: Modulating Crosslinking Density
- Synthesis: Prepare a series of polymeric nanoparticles (e.g., based on chitosan or PEG-PLA) with identical composition and size but varying concentrations of a crosslinker like genipin or glutaraldehyde.
- Elasticity Measurement: Characterize the mechanical properties of each batch using Atomic Force Microscopy (AFM) to determine their Young's modulus.
- In Vivo Testing: Administer the different batches to an animal model (e.g., mice) and track their blood concentration over time using fluorescence or radiolabeling.
- Analysis: Correlate the measured Young's modulus with the calculated circulation half-life. Expect to see a trend where a lower modulus (softer particles) correlates with a longer half-life [64].
Problem: Poor Penetration into Target Tissues
Potential Cause and Solution:
- Cause: Nanoparticles cannot deform to navigate the dense, mesh-like structure of biological hydrogels like the tumor extracellular matrix (ECM) or mucus [64].
- Solution: Engineer highly deformable (elastic) nanoparticles. Their ability to change shape allows them to squeeze through pores in the hydrogel network that are smaller than the particle's original diameter.
Experimental Protocol: Assessing ECM Permeation In Vitro
- Model Setup: Create a 3D hydrogel barrier in a transwell system. This hydrogel could be collagen (to mimic ECM) or mucin (to mimic mucus).
- Particle Preparation: Use two batches of nanoparticles of the same size and surface charge but different elasticity (e.g., soft liposomes vs. rigid polystyrene beads).
- Permeation Study: Place the nanoparticles on top of the hydrogel barrier and measure the quantity that passes through to the bottom chamber over several hours using a technique like spectrophotometry.
- Validation: The data should show a higher permeation rate for the more elastic nanoparticles compared to their rigid counterparts [64].
Data Presentation
Table 1: Impact of Nanoparticle Elasticity on Biological Performance
| Elasticity (Young's Modulus) | Circulation Half-Life | Mucus Penetration | ECM Permeation | Cellular Uptake | Key Findings |
|---|---|---|---|---|---|
| High (Rigid) | Short (minutes) | Low | Low | Variable (can be high) | Rapid clearance by Kupffer cells; steric hindrance in hydrogels [64] [65] |
| Low (Soft/Elastic) | Long (hours) | High | High | Variable (can be lower) | Evades immune scavenging; squeezes through hydrogel pores [64] [65] |
| Medium (Tunable) | Medium | Medium | Medium | Dependent on other parameters | Allows for balancing circulation with other functions like drug release and uptake [64] |
Table 2: Common Methods for Elasticity Tuning and Characterization
| Tuning Method | Mechanism | Typical Materials | Key Characterization Technique |
|---|---|---|---|
| Crosslink Density | Varying crosslinker concentration alters polymer network stiffness. | Chitosan, Gelatin, PEG-based hydrogels | Atomic Force Microscopy (AFM) |
| Core-Shell Design | Using a soft shell and a tunable core to control overall deformability. | Liposomes, Polymeric NPs with lipid shells | AFM, Micropipette Aspiration |
| Polymer Choice | Selecting polymers with intrinsically low Young's modulus. | Certain PLGA blends, Liquid Crystal Polymers | Dynamic Mechanical Analysis |
Experimental Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Elasticity-Tuned Nanoparticle Research
| Item | Function in Research | Example Application |
|---|---|---|
| Tunable Crosslinkers | To systematically vary the stiffness of polymeric nanoparticles. | Using different concentrations of genipin to create a stiffness gradient in chitosan nanoparticles. |
| Biomimetic Coatings | To confer "self" properties and reduce immune recognition, complementing elasticity. | Coating particles with CD47-mimetic peptides or macrophage membrane vesicles. |
| Placebo/"Dummy" Particles | To saturate Kupffer cells temporarily, allowing a test dose of therapeutic nanoparticles to circulate longer. | Pre-injecting empty liposomes before administering drug-loaded, elasticity-optimized nanoparticles [65]. |
| Atomic Force Microscope | The key instrument for directly measuring the mechanical properties (Young's modulus) of individual nanoparticles. | Quantifying the elasticity of different formulation batches to confirm tuning success. |
| Fluorescent Tags | To label nanoparticles for tracking and quantification in complex biological environments. | Measuring the penetration of soft vs. rigid particles through a 3D mucus or ECM model over time. |
Stabilizing Ligand Integration and Targeting Moiety Preservation
For researchers in drug development, maintaining the structural integrity of nanoparticles (NPs) in circulation is paramount to therapeutic efficacy. A nanoparticle's journey in the bloodstream is challenging, and the stability of its surface ligands—which ensure colloidal stability, prevent opsonization, and enable targeted delivery—directly dictates its success. This technical support center addresses the key experimental challenges in preserving ligand integration and targeting moiety function, providing targeted troubleshooting guides and detailed protocols to enhance the robustness of your nano-formulations.
FAQ: Ligand and Targeting MoietY Stability
Why is ligand stability critical for inorganic nanoparticles in biomedical applications?
Ligands are not merely passive coatings; they are dynamic components that govern the nanoparticle's identity and function. Their stability is crucial because they [66]:
- Maintain Colloidal Stability: Ligands prevent nanoparticle aggregation, which can alter biodistribution and cause toxicity.
- Govern Biological Interactions: The surface chemistry (charge, hydrophobicity, functional groups) dictates interactions with proteins (forming the protein corona), cellular uptake, biodistribution, and clearance.
- Ensure Targeting Fidelity: Ligands are often used to conjugate targeting moieties (e.g., antibodies). Their instability can lead to the loss of this targeting capability, rendering the nanoparticle non-specific.
What are the common mechanisms of ligand instability I should anticipate in my experiments?
Ligand instability can arise from multiple fronts, both during storage and in biological environments [66]:
- Ligand Desorption: The spontaneous dissociation of ligands from the nanoparticle surface into the solution, driven by weak binding affinity or dynamic equilibrium.
- Chemical Degradation: The molecular structure of the ligand itself can be degraded by hydrolysis or oxidation, especially under storage conditions or in the presence of reactive oxygen species (ROS) in vivo.
- Biomolecule-Induced Displacement: Upon injection, biomolecules like proteins and lipids can competitively adsorb onto the nanoparticle surface, displacing the original ligands.
- Enzymatic Degradation: Specific enzymes in biological fluids can cleave and degrade certain types of organic ligands.
How can I improve the stability of targeting antibodies conjugated to my nanoparticles?
A primary concern is the random orientation of antibodies, which can block their antigen-binding sites. A advanced method to ensure proper orientation and preserve avidity is directional conjugation via the Fc moiety. This protocol involves [67]:
- Mild Oxidation: The glycosyl groups exclusively located on the Fc region of the antibody are oxidized to generate aldehyde groups.
- Linker Attachment: An aminooxy-PEG-dibenzocyclooctyne heterobifunctional linker is reacted with the newly formed aldehydes on the Fc region.
- Click Conjugation: The modified antibodies are then conjugated to azide-functionalized nanoparticles using metal-free click chemistry. This method ensures the antigen-binding Fab regions remain free and functional, maximizing the targeting efficiency of your nanoparticle-antibody conjugates [67].
Troubleshooting Guide: Ligand Instability
| Problem Phenomenon | Potential Root Cause | Recommended Solution |
|---|---|---|
| Nanoparticle Aggregation in buffer or serum | Ligand desorption or degradation, leading to loss of colloidal stability [66]. | Increase ligand binding affinity (e.g., use multidentate ligands); perform stability tests in relevant biological media [66]. |
| Loss of Targeting Specificity in cellular assays | Random antibody orientation or detachment of targeting moieties [67] [66]. | Implement directional conjugation protocols (e.g., Fc-targeted click chemistry); characterize ligand density pre-/post-incubation [67]. |
| Uncontrolled Drug Release or premature payload leakage | Instability of the nanoparticle core or surface coating in physiological conditions [68]. | Optimize nanoparticle composition; use stimulus-responsive materials designed for specific disease microenvironments (e.g., low pH, enzymes) [68]. |
| High Non-Specific Cellular Uptake | Formation of a protein corona that masks targeting ligands and confers a new, non-specific biological identity [66]. | Engineer "stealth" surfaces (e.g., with PEG); use ligands that resist protein adsorption. |
Quantitative Stability Metrics and Characterization
To objectively assess stability, researchers must move beyond qualitative observations and employ quantitative metrics. The following table outlines key attributes and corresponding characterization techniques.
Table 1: Critical Quality Attributes (CQAs) and Characterization Methods for Nanoparticle Stability Assessment [8] [5] [66]
| Critical Quality Attribute | Definition & Impact on Stability | Quantitative Characterization Techniques | ||
|---|---|---|---|---|
| Aggregation State | Preservation of primary nanoparticles; aggregation alters biodistribution and efficacy [8]. | Dynamic Light Scattering (DLS), Localized Surface Plasmon Resonance (LSPR) [8]. | ||
| Size & Distribution | Nanoparticle diameter and polydispersity; affects circulation time and targeting [5]. | DLS, Transmission Electron Microscopy (TEM), Scanning Electron Microscopy (SEM) [8]. | ||
| Surface Charge (Zeta Potential) | Indicator of colloidal stability; high magnitude ( | ζ | > 30 mV) typically suggests good stability [5]. | Zeta Potential Measurement [8]. |
| Ligand Density & Conformation | Number and spatial arrangement of ligands on the surface; directly influences biological interactions [66]. | Nuclear Magnetic Resonance (NMR), X-ray Photoelectron Spectroscopy (XPS), Isothermal Titration Calorimetry (ITC) [66]. | ||
| Surface Chemistry | Chemical identity and functionality of the surface coating [8]. | XPS, Fourier-Transform Infrared Spectroscopy (FTIR) [8]. | ||
| Drug Loading/Release | Capacity to encapsulate and controllably release a therapeutic payload [5]. | HPLC, UV-Vis Spectroscopy [5]. |
Experimental Protocols for Stability Evaluation
Protocol 1: Evaluating Colloidal Stability in Physiological Buffers
This protocol assesses the nanoparticle's resistance to aggregation in conditions mimicking in vivo environments.
- Sample Preparation: Dilute the nanoparticle suspension in commonly used buffers such as phosphate-buffered saline (PBS), with or without serum, to a standard concentration (e.g., 0.1-1 mg/mL).
- Incubation: Incubate the samples at 37°C under gentle agitation to simulate physiological temperature and flow.
- Time-Point Measurement: At predetermined time points (e.g., 0, 1, 4, 24, 48 hours), withdraw aliquots.
- Analysis: Measure the hydrodynamic diameter and zeta potential via DLS. A significant increase in size over time indicates aggregation and poor colloidal stability [8] [66].
Protocol 2: Confirming Targeting Moiety Integrity and Function
This protocol verifies that conjugated antibodies or other targeting ligands remain functional after nanoparticle formulation and storage.
- Direct Binding Assay (ELISA):
- Immobilize the target antigen on an ELISA plate.
- Incubate with your nanoparticle-conjugate and relevant controls (e.g., bare nanoparticles, free antibody).
- Use a detection antibody (e.g., against the Fc region of the targeting antibody) or a label specific to the nanoparticle to measure binding.
- Interpretation: A strong signal from the conjugate, comparable to the free antibody, indicates preserved binding function [67].
- Cell-Based Binding and Uptake Assay:
- Use cell lines that express (positive) and do not express (negative) the target receptor.
- Incubate the cells with the targeted nanoparticles and non-targeted controls.
- Analyze using flow cytometry or confocal microscopy.
- Interpretation: Significantly higher association with the target-positive cells, compared to controls and target-negative cells, confirms specific targeting [67].
Visualizing Instability Mechanisms and Workflows
The following diagrams illustrate key concepts and experimental pathways for evaluating nanoparticle stability.
Ligand Instability Mechanisms
Ligand Stability Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Ligand Stabilization and Conjugation
| Reagent / Material | Primary Function in Stabilization & Targeting | Key Considerations |
|---|---|---|
| Multidentate Ligands (e.g., dithiols, tripods) | Enhance binding affinity to the nanoparticle core, reducing desorption rates [66]. | Can be synthetically complex; may require custom synthesis. |
| PEG-based Linkers | Provide a hydrophilic stealth layer, reducing protein adsorption and improving circulation time [69] [67]. | PEG length can affect shielding and pharmacokinetics; consider potential anti-PEG immunity. |
| Heterobifunctional Crosslinkers (e.g., Aminooxy-PEG-DBCO) | Enable controlled, directional conjugation (e.g., via Fc glycosylation) to preserve bioactivity [67]. | Reaction conditions (pH, temperature) are critical for efficiency. |
| Stimuli-Responsive Lipids/Polymers | Promote controlled drug release in specific microenvironments (e.g., low pH, high ROS) [70]. | Must be matched to the target pathology's microenvironment. |
| Inorganic Ligands (e.g., S²⁻, metal chalcogenides) | Form highly stable, conductive coatings; useful for electronic or catalytic applications [69]. | May not be biocompatible; typically used for non-biological applications. |
Assessment Methods and Comparative Analysis of Nanoparticle Stability
FAQs: Core Principles and Applications
Q1: How do DLS, SMLS, and Cryo-EM complement each other in nanoparticle stability assessment? These techniques provide information at different structural hierarchies and physical scales. DLS is a rapid, solution-based technique ideal for measuring a nanoparticle's hydrodynamic diameter and assessing aggregation state in real-time by analyzing the fluctuation of scattered light [71] [72]. SMLS, which includes techniques like Nanoparticle Tracking Analysis (NTA), directly tracks the Brownian motion of individual particles to determine size distribution and concentration, offering higher resolution for polydisperse samples [72] [73]. Cryo-EM visualizes nanoparticles in a near-native, vitrified state, providing direct, high-resolution images of particle morphology, internal structure (e.g., lamellar vs. cubic phases in lipid nanoparticles), and detailed aggregation characteristics [74] [72]. Using them together provides a comprehensive profile from ensemble size (DLS) to particle-by-particle concentration (SMLS) and ultimate structural validation (Cryo-EM).
Q2: What is the critical advantage of Cryo-EM over traditional electron microscopy for soft nanoparticles? The key advantage is the preservation of native structure. Traditional EM often requires sample dehydration, chemical fixation, and heavy metal staining, which can distort or collapse soft, hydrated nanostructures like liposomes or hydrogels [75] [74]. Cryo-EM involves ultra-rapid vitrification ("flash-freezing"), which traps nanoparticles in a thin layer of amorphous ice. This process minimizes artifacts, allowing researchers to observe the true size, shape, and internal architecture of nanoparticles as they exist in solution [75] [74] [72].
Q3: My DLS results show a single peak, but my Cryo-EM images reveal multiple particle sizes and shapes. Why the discrepancy? This is a common scenario highlighting the limitations of DLS for heterogeneous samples. DLS reports an intensity-weighted hydrodynamic diameter and is heavily biased towards larger particles in a mixture because larger particles scatter light more intensely [72]. A small population of aggregates or oversized particles can dominate the signal, masking the presence of smaller, more numerous species. Cryo-EM provides a direct visual assessment, revealing morphological heterogeneity, contaminants, or complex structures that DLS cannot resolve. This discrepancy underscores the importance of using orthogonal techniques to validate nanoparticle homogeneity.
Q4: What sample purity is required for successful single-particle Cryo-EM analysis? For high-resolution single-particle Cryo-EM, sample purity must be exceptionally high, typically >99% [76]. The sample should be monodisperse, meaning the particles are uniform in size, shape, and composition. Even minor contaminants can hinder data processing and 3D reconstruction. Techniques like size-exclusion chromatography (SEC) are critical as a final purification step to achieve this monodispersity and remove aggregated material [77] [78].
Troubleshooting Guides
Dynamic Light Scattering (DLS)
Table: Troubleshooting Common DLS Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor Polydispersity Index (PDI) | Sample aggregation or contamination. | Filter sample and buffers through a 0.22 µm or 0.1 µm filter. Optimize buffer conditions (pH, salt) to improve stability [76]. |
| Unreliable or Fluctuating Size Readings | Presence of dust or air bubbles. | Centrifuge sample briefly before loading. Ensure cuvettes are clean and properly filled without bubbles. |
| Signal-to-Noise Ratio Too Low | Sample concentration is too low or the particles are too small. | Increase sample concentration within the instrument's linear range. Use a higher-power laser if available. |
| Multiple Peaks in Size Distribution | Genuine sample heterogeneity or the presence of protein aggregates. | Use a complementary technique like AF4-NTA or Cryo-EM to deconvolute the populations [71]. Further purify the sample via SEC. |
Cryo-Electron Microscopy (Cryo-EM)
Table: Troubleshooting Cryo-EM Sample Preparation
| Problem | Potential Cause | Solution |
|---|---|---|
| Empty or Broken Ice | Blotting time too long or too much blot force. | Optimize blotting time and force empirically. Use a glow-discharged grid to improve hydrophilic sample spread [76] [79]. |
| Preferential Orientation | Particle adsorption to the air-water interface. | Test different grid types (e.g., gold vs. copper). Use additives like detergents or amphipols to shield hydrophobic patches [78]. |
| Thick, Vitreous Ice | Insufficient blotting or high humidity during plunge-freezing. | Decrease blot time, adjust humidity settings on the vitrobot, ensure proper ethane temperature [76]. |
| Particle Denaturation or Disruption | Destructive forces at the air-water interface. | Use affinity grids or continuous carbon supports to protect particles [77]. Increase sample concentration slightly. |
| Sample Aggregation on Grid | Interaction with grid surface or buffer incompatibility. | Change grid type (e.g., to graphene oxide). Perform a final buffer exchange into a compatible, additive-free buffer right before grid preparation [78] [76]. |
Optimizing Data Collection Efficiency: When using automated data collection software like EPU, the choice of acquisition mode impacts speed and potential beam-induced motion. The Faster acquisition mode, which uses image/beam shift to collect multiple micrographs per stage movement, can increase data collection speed nearly fivefold without compromising resolution compared to the Accurate mode, which mechanically centers each hole [79]. For many standard samples, the Faster mode with counted super-resolution, binning 2, and TIFF output file format is recommended for an optimal balance of speed and data quality [79].
Experimental Protocols
Protocol: Sample Preparation for Cryo-EM Grids
This protocol is adapted for a standard protein or nanoparticle sample [76] [79].
- Grid Preparation: Use holey carbon grids (e.g., Quantifoil, 1.2/1.3 µm holes, 300 mesh). Glow-discharge the grids for 30-60 seconds at 15-30 mA to render the surface hydrophilic.
- Sample Application: Load a 3-4 µL aliquot of your sample (e.g., 3.5-4.0 mg/mL for proteins like apoferritin) onto the glow-discharged grid within a controlled-environment vitrobot (e.g., FEI Vitrobot Mark IV, >90% humidity, 4°C).
- Blotting and Vitrification: Blot away excess liquid with filter paper for a defined time (e.g., 4 seconds, blot force zero). Immediately after blotting, plunge-freeze the grid rapidly into liquid ethane cooled by liquid nitrogen. The goal is to form a thin, vitreous (non-crystalline) ice layer.
- Storage: Clip the grid into an autogrid ring and store it under liquid nitrogen until data collection.
Protocol: Negative Stain TEM for Rapid Sample Screening
This quick protocol allows for the assessment of sample quality, monodispersity, and concentration before committing to cryo-EM [78] [76].
- Grid Preparation: Glow-discharge a continuous carbon-coated grid.
- Sample Application: Apply 3-4 µL of sample to the grid. Let it adsorb for approximately 1 minute.
- Staining: Blot away the sample and wash the grid by placing it on a droplet of ultrapure water. Blot again and apply 3-4 µL of a heavy metal stain (e.g., 1-2% uranyl acetate) for 20-30 seconds.
- Drying and Imaging: Blot away the excess stain completely and allow the grid to air-dry for several minutes. The grid is now ready for imaging in a TEM at room temperature.
Workflow and Relationship Diagrams
Diagram 1: Integrated nanoparticle characterization workflow. This diagram outlines the logical progression for comprehensively characterizing nanoparticles, showing how DLS and SMLS provide initial solution-based data, which informs the sample preparation and screening steps for Cryo-EM, ultimately leading to high-resolution structural data. Feedback loops are essential for optimizing the initial formulation.
Research Reagent Solutions
Table: Essential Materials for Nanoparticle Characterization
| Reagent / Material | Function / Application | Example in Context |
|---|---|---|
| Lipids for LNPs (e.g., DODMA, DSPC, DMG-PEG2000, Cholesterol) | Form the structural and functional components of lipid nanoparticles for mRNA/drug delivery [73]. | Used in a molar ratio of 50:10:1.5:38.5 to create stable, immunogenic LNP-mRNA vaccine formulations [73]. |
| Holey Carbon Grids (e.g., Quantifoil) | Support the vitrified sample layer for Cryo-EM, with holes that allow imaging without background interference from the grid itself [79]. | Quantifoil grids (1.2/1.3, 300 mesh Copper) are standard for preparing Apoferritin and other protein samples [79]. |
| Heavy Metal Stains (e.g., Uranyl Acetate) | Provide contrast in negative stain TEM by embedding dehydrated samples, revealing particle outline and distribution [78] [76]. | A 1-2% uranyl acetate solution is applied for 20-30 seconds to visualize sample quality before Cryo-EM [78]. |
| Amphipols | Amphipathic polymers used to stabilize membrane proteins in solution by replacing detergents, forming a belt around hydrophobic domains [78]. | Crucial for solving high-resolution structures of membrane proteins like TRPV1 by Cryo-EM [78]. |
| Size Exclusion Chromatography (SEC) Columns | Final purification step to isolate monodisperse populations of nanoparticles or protein complexes and remove aggregates [77] [78]. | A symmetric elution profile from an SEC column is a key indicator of sample monodispersity suitable for Cryo-EM [78]. |
| Microfluidic Device | Enables reproducible and rapid mixing of organic and aqueous phases for the formation of uniform lipid nanoparticles (LNPs) [73]. | Used at a 1:3 organic-to-aqueous flow ratio to produce LNP-mRNA formulations with high encapsulation efficiency and low PDI [73]. |
In Vitro and In Vivo Stability Evaluation Protocols
For researchers in drug development, evaluating the structural stability of nanoparticles in circulation is paramount for predicting their efficacy and safety. A robust stability protocol confirms that a nanoparticle maintains its structural integrity and designed functionality from the vial to the vascular system. This guide provides detailed, actionable methodologies and troubleshooting advice to standardize your stability evaluation process, ensuring reliable and reproducible data for your research.
Key Evaluation Protocols & Data Presentation
Quantitative Stability Parameters Table
The following table summarizes the core parameters and acceptance criteria for a comprehensive stability assessment, integrating principles from general in vivo assay validation [80] and nanoparticle-specific research [4].
Table 1: Key Parameters for Nanoparticle Stability Evaluation
| Evaluation Parameter | In Vitro Assay Method | Typical Acceptance Criterion | Link to In Vivo Performance |
|---|---|---|---|
| Size & PDI | Dynamic Light Scattering (DLS) | ΔDiameter < 10%; PDI < 0.2 | Prevents rapid clearance by RES; ensures extravasation potential [81]. |
| Surface Charge | Zeta Potential Measurement | ΔPotential ∣±5 mV∣ | Indicates colloidal stability; predicts protein corona composition [4]. |
| Drug Release Profile | Dialysis in PBS/Buffer | RSD of release kinetics < 15% | Predicts availability of active pharmaceutical ingredient at target site [82]. |
| Structural Integrity | TEM / Cryo-EM | No visible disintegration or fusion | Directly correlates with circulation lifetime and payload protection [4]. |
| Protein Corona | SDS-PAGE, LC-MS | Consistent protein composition profile | Determines biological identity and subsequent cellular interactions [4]. |
Core In Vivo Validation Parameters
When transitioning to in vivo models, the validation parameters expand to include pharmacological endpoints. The following table outlines the statistical performance measures critical for a validated in vivo assay, as guided by the Assay Guidance Manual [80].
Table 2: Key Performance Measures for In Vivo Assay Validation
| Performance Measure | Stage of Validation | Description and Purpose | Application in Stability |
|---|---|---|---|
| Minimum Significant Difference (MSD) | Pre-study (Single Dose) | Quantifies the smallest difference in effect that is statistically significant. | Determines if a change in a stability endpoint (e.g., circulation time) between nanoparticle batches is real. |
| Minimum Significant Ratio (MSR) | Pre-study (Dose-Response) | Quantifies the smallest ratio in potency that is statistically significant. | Used when evaluating dose-dependent effects on stability, such as carrier-mediated toxicity. |
| Control Charts | In-study | Monitors assay performance over time using maximum and minimum control groups. | Tracks the consistency of baseline in vivo stability data (e.g., of a reference nanoparticle) across multiple experimental runs. |
| Assay Comparison | Cross-study (Method Transfer) | Statistical comparison of results before and after a procedural change or between labs. | Ensures stability protocols yield equivalent results when transferred to a new facility or after a minor protocol change. |
Detailed Experimental Protocols
Protocol: Evaluating Systemic Circulation Lifetime
Objective: To quantitatively measure the blood circulation half-life of nanoparticles, a critical indicator of in vivo stability [4].
Materials:
- Test nanoparticles
- Animal model (e.g., mouse)
- EDTA-coated microtainers
- Phosphate Buffered Saline (PBS)
- Centrifuge
- ELISA plate reader or other relevant detection instrumentation
Methodology:
- Dosing & Sampling: Administer a single dose of nanoparticles via the chosen route (e.g., intravenous). Collect blood samples (e.g., ~50 µL) at pre-determined time intervals (e.g., 0.5, 2, 8, 24, 48 hours) into EDTA-coated tubes to prevent coagulation.
- Plasma Separation: Centrifuge blood samples immediately at 4°C to separate plasma from cellular components.
- Sample Analysis: Isolate nanoparticles from plasma and quantify nanoparticle concentration using a pre-validated method. This could involve:
- Measuring a fluorescent or radioactive tag incorporated into the nanoparticle.
- Using ELISA to detect a specific component of the nanoparticle.
- Data Analysis: Plot the nanoparticle concentration in plasma versus time. Use a non-compartmental pharmacokinetic analysis to calculate key parameters like half-life (t1/2), area under the curve (AUC), and clearance (CL).
Protocol: Isolating and Analyzing the Protein Corona
Objective: To characterize the protein corona that forms on nanoparticles in a biological fluid, as its composition is a major determinant of in vivo stability and fate [4].
Materials:
- Test nanoparticles
- Mouse or human plasma
- Ultracentrifuge or size-exclusion columns
- SDS-PAGE gel apparatus
- Mass Spectrometry (LC-MS/MS) equipment
Methodology:
- Incubation: Incubate a standardized concentration of nanoparticles (e.g., 1 mg/mL) in undiluted plasma for a designated time (e.g., 1 hour) at 37°C with gentle agitation.
- Isolation: Separate the nanoparticle-protein corona complexes from unbound plasma proteins. This is typically achieved via ultracentrifugation (at 100,000 x g for 1-2 hours) or size-exclusion chromatography.
- Washing: Gently wash the pellet (if using centrifugation) with a cold, neutral buffer to remove loosely associated proteins without disrupting the hard corona.
- Protein Elution & Identification: Dissociate the proteins from the nanoparticle surface using a denaturing buffer. Analyze the protein composition using SDS-PAGE for a gross profile and LC-MS/MS for precise protein identification and relative quantification.
Experimental Workflows & Visualization
In Vivo Assay Validation Lifecycle
The following diagram illustrates the continuous cycle of assay validation, ensuring data reliability throughout the research lifecycle [80].
Nanoparticle Stability & Fate Workflow
This workflow outlines the logical pathway from nanoparticle properties to physiological fate, highlighting the central role of the protein corona [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Nanoparticle Stability Evaluation
| Reagent / Material | Function in Stability Evaluation | Key Consideration |
|---|---|---|
| PEGylated Lipids | Forms a hydrophilic stealth layer on nanoparticle surface to reduce opsonization and prolong circulation [4] [81]. | PEG density and chain length are critical; can affect protein corona composition and immunogenicity. |
| Hydrogel Cores (e.g., Polyacrylamide) | Provides a tunable, soft core to study the isolated effect of nanoparticle elasticity on biological fate [4]. | Crosslinking density directly controls elasticity, which non-monotonically impacts circulation time. |
| DOPC & DSPE-PEG2000 | Common lipid components used to form stable, PEGylated lipid bilayer shells for core-shell nanoparticles [4]. | Ratio of DOPC to DSPE-PEG2000 determines PEG density on the nanoparticle surface. |
| Apolipoprotein A-I (ApoA1) | A specific corona protein identified as a biomarker for long circulation lifetime on nanoparticles of intermediate elasticity [4]. | Its relative abundance in the corona can be a key predictive metric for in vivo performance. |
| Plasma/Serum | Used for in vitro incubation studies to simulate protein corona formation under physiological conditions [4]. | Source (human vs. animal) and handling (e.g., freeze-thaw cycles) can significantly alter protein composition. |
Troubleshooting Guides & FAQs
FAQ 1: Our nanoparticles show excellent stability in buffer but aggregate rapidly in serum. What could be the cause?
- Answer: This is a classic sign of colloidal destabilization induced by protein adsorption.
- Troubleshooting Steps:
- Check Surface Charge: Measure the zeta potential of the nanoparticles immediately after serum incubation. A shift towards neutrality indicates surface shielding by proteins, promoting aggregation.
- Increase Stealth Properties: Increase the density or length of PEG chains on the nanoparticle surface. PEG creates a steric barrier that repels proteins and other nanoparticles [4] [81].
- Modify Surface Chemistry: Consider using alternative stealth coatings or adjusting the surface charge to be slightly negative, which is generally less interactive with serum proteins.
FAQ 2: We observed a high and unpredictable variation in circulation half-life between animal subjects. How can we improve the reliability of our in vivo data?
- Answer: High variability often stems from inadequate in vivo assay validation and poor control of experimental conditions [80].
- Troubleshooting Steps:
- Implement Control Charts: Run a standardized reference nanoparticle in every in vivo experiment. Plot its half-life on a control chart to monitor the assay's performance over time and identify outliers [80].
- Review Randomization: Ensure animals are randomly assigned to treatment groups to minimize bias from weight, age, or litter effects. Proper randomization is a fundamental requirement for a validated in vivo assay [80].
- Power Analysis: Conduct a pre-study power analysis to determine the appropriate group size. A sample size that is too small will be unable to detect biologically meaningful effects, leading to irreproducible results [80].
FAQ 3: How significant is nanoparticle elasticity compared to other parameters like size and surface chemistry in determining stability and fate?
- Answer: Recent evidence suggests elasticity is a critically independent parameter. Using core-shell nanoparticles with identical size and surface chemistry but different core elasticity, researchers demonstrated a non-monotonic relationship between elasticity and circulation lifetime, with intermediate elasticity (75–700 kPa) being optimal. This effect was mechanistically linked to a preferential adsorption of ApoA1, a protein beneficial for long circulation [4]. Therefore, elasticity should be considered a primary design parameter alongside size and surface chemistry.
Comparative Analysis of Different Nanoparticle Platforms and Formulations
Troubleshooting Guide: Frequently Asked Questions
FAQ: What are the most common causes of nanoparticle instability during storage, and how can I mitigate them?
Answer: The primary causes of instability are aggregation, drug leakage, and chemical degradation. Your mitigation strategy depends on the nanoparticle platform.
- For Lipid Nanoparticles (LNPs): Refrigerated storage (2°C) in aqueous buffers provides the best long-term stability, preserving gene silencing efficacy for over 150 days. Avoid repeated freeze-thaw cycles, which cause aggregation. For lyophilization, use cryoprotectants like trehalose or sucrose at 5-10% (w/v) concentration to maintain efficacy upon reconstitution [83].
- For Liposomes and Polymer Nanoparticles: Instability can manifest as solute leakage and aggregation. Lyophilization is the preferred long-term storage method. Ensure stringent quality control to monitor drug encapsulation efficiency and particle size distribution over time [84] [83].
FAQ: My nanoparticles are aggregating in biological media. Is this due to my formulation?
Answer: Yes, aggregation in biological fluids is often due to surface-protein interactions. When nanoparticles enter circulation, they are rapidly coated by proteins, forming a "protein corona." This can lead to opsonization and clearance by the immune system.
- Surface Modification is Key: Coating your nanoparticles with polyethylene glycol (PEG) is a standard strategy to create a "stealth" effect, reducing protein adsorption and extending circulation time [84] [85].
- Emerging Alternatives: Be aware that repeated administration of PEGylated nanoparticles can trigger anti-PEG antibodies. Consider investigating non-PEG alternatives, such as zwitterionic polymers or coatings inspired by natural biomolecules, for next-generation formulations [84].
FAQ: I am not seeing the expected therapeutic efficacy in my in vivo models. What could be wrong?
Answer: This is a common translational gap, often stemming from an over-reliance on the Enhanced Permeability and Retention (EPR) effect.
- The EPR Effect is Heterogeneous: The EPR effect, while robust in many animal tumor models, is highly variable and often limited in human patients. Do not assume passive targeting alone will be sufficient [84].
- Re-evaluate Your Targeting Strategy: Move beyond passive targeting. Incorporate active targeting ligands (e.g., antibodies, peptides) on the nanoparticle surface to improve specific cell uptake. Furthermore, consider the biological barriers you need to overcome. For example, if you are working on ocular diseases, design your nanoparticles for enhanced corneal permeability and sustained release to overcome ocular barriers [84] [86].
| Storage Condition | Storage Duration | Impact on Gene Silencing Efficacy | Recommendation |
|---|---|---|---|
| Refrigeration (2°C) | 156 days | Remained most stable | Recommended for aqueous storage |
| Room Temperature (25°C) | 156 days | Significant reduction | Not recommended for long-term storage |
| Freezing (-20°C) | 156 days | Reduced stability vs. refrigeration | Acceptable, but inferior to 2°C |
| Lyophilization (with cryoprotectant) | Short-term (1 week) | Efficacy retained upon reconstitution | Recommended for room-temperature storage |
| Market Segment | Projected Market Share / Growth | Key Insights |
|---|---|---|
| Overall Market | CAGR of 9.4% ($5.1B in 2025 → $15.1B in 2035) | Driven by demand for nanoparticle-based drugs and service providers. |
| By Nanoparticle Type | Organic Nanoparticles dominate the market. | Lipid and polymeric nanoparticles are the most established. |
| Fastest Growing Type | Protein-based Nanoparticles (Highest CAGR segment) | Includes platforms like reconstituted HDL [85]. |
| By Scale of Operation | Clinical-scale manufacturing is the fastest-growing segment. | Indicates a rich pipeline of products moving through development. |
Experimental Protocols for Stability Assessment
Protocol 1: Assessing Long-Term Stability of Lipid Nanoparticles in Aqueous Solution
This methodology is adapted from a study on lipidoid nanoparticle (LNP) stability for siRNA delivery [83].
1. Formulation:
- Prepare LNPs via rapid pipette mixing of lipid and siRNA solutions in a defined molar ratio (e.g., lipidoid:cholesterol:DSPC:PEG-lipid at 50:38.5:10:1.5). Use a sodium citrate buffer (pH ~4) during formation to facilitate electrostatic complexation [83].
2. Storage Conditions:
- Dilute the freshly prepared LNP solution in phosphate-buffered saline (PBS).
- Divide the solution into aliquots and store at different temperatures: -20°C, 2°C (refrigeration), and 25°C (room temperature).
- Monitor the samples over your desired time course (e.g., up to 150 days).
3. Characterization and Analysis:
- Size and Aggregation: Measure the hydrodynamic diameter and polydispersity index (PDI) using Dynamic Light Scattering (DLS) at regular intervals. An increase in size indicates aggregation.
- Entrapment Efficiency: Use a fluorescence-based assay (e.g., Quant-iT RiboGreen). Measure total siRNA fluorescence, then measure fluorescence of unencapsulated siRNA after nanoparticle separation. Calculate percentage entrapped [83].
- In Vitro Efficacy: The most critical test. Treat relevant cell lines (e.g., HeLa cells) with stored LNPs and measure functional output, such as gene silencing efficacy via luciferase assay, compared to fresh LNPs [83].
Protocol 2: Lyophilization and Reconstitution of Nanoparticles
This protocol provides a method for converting aqueous nanoparticle dispersions into a stable dry powder [83].
1. Pre-Lyophilization (Adding Cryoprotectants):
- Add a cryoprotectant sugar (e.g., trehalose or sucrose) to the nanoparticle solution to a final concentration of 5-10% (w/v). This is critical to prevent aggregation and maintain structure during freezing and drying.
2. Freezing and Lyophilization:
- Rapidly freeze the nanoparticle/cryoprotectant solution, either in a -80°C freezer or by immersion in liquid nitrogen.
- Transfer the frozen samples to a freeze-dryer. Lyophilize for approximately 12 hours or until a dry powder is obtained.
3. Reconstitution:
- Reconstitute the lyophilized powder in deionized water or an appropriate aqueous buffer by gentle vortexing.
- Critical Step: Do not reconstitute in buffers containing ethanol, as this requires subsequent dialysis for in vitro or in vivo use. With proper cryoprotectants, reconstitution in aqueous buffer is effective [83].
4. Post-Reconstitution Analysis:
- Characterize the reconstituted nanoparticles for size, PDI, entrapment efficiency, and in vitro efficacy as described in Protocol 1 to confirm stability has been maintained.
Experimental Workflow & Formulation Strategy
Diagram: Workflow for Nanoparticle Stability Testing
Diagram: Strategy for Stable Nanoparticle Formulation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Nanoparticle Formulation and Stability Research
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| Ionizable Lipidoids | Key component for forming lipid nanoparticles; encapsulates nucleic acids (siRNA/mRNA) via electrostatic interactions. | Primary material in potent LNP systems for gene delivery [83]. |
| DSPC (Distearoylphosphatidylcholine) | A structural phospholipid that contributes to the stability and integrity of the lipid bilayer in nanoparticles. | Used in LNP formulations to improve structural stability [83]. |
| PEGylated Lipids | Imparts a "stealth" property to nanoparticles, reducing protein adsorption and extending circulation half-life. | Critical for creating long-circulating nanomedicines like Doxil [84]. |
| Trehalose / Sucrose | Cryoprotectants that protect nanoparticle structure during freeze-drying (lyophilization) and storage. | Added at 5-10% w/v to LNP solutions before lyophilization to enable room-temperature storage [83]. |
| Apolipoprotein A-I (Apo-AI) | The primary protein component of High-Density Lipoproteins (HDL); used to create biomimetic nanoparticles. | Key for synthesizing reconstituted HDL (rHDL) nanoparticles for cardiovascular and drug delivery applications [85]. |
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable polymer used for controlled-release nanoparticle formulations. | Common material for polymer-based nanoparticles that provide sustained drug release [84]. |
Correlating Physicochemical Properties with Pharmacokinetic Performance
FAQs and Troubleshooting Guides
FAQ 1: How does nanoparticle elasticity influence systemic circulation lifetime, and what is the optimal range?
The relationship between nanoparticle elasticity and systemic circulation lifetime is non-monotonic. Research using core-shell nanoparticles with identical surface chemistry but differing core elasticity has demonstrated that an intermediate elasticity range (approximately 75 kPa to 700 kPa) promotes the longest circulation times. Excessively soft (e.g., 45 kPa) or overly stiff (e.g., 760 MPa) nanoparticles are cleared from the blood more rapidly [4].
- Underlying Mechanism: This effect is mediated by the protein corona. Nanoparticles with intermediate elasticity selectively adsorb apolipoprotein A-I (ApoA1) from the blood. The relative abundance of ApoA1 in the corona shows a strong positive correlation with prolonged circulation lifetime, helping to evade clearance by immune cells like Kupffer cells [4] [65].
FAQ 2: Which physicochemical properties most significantly impact the volume of distribution (Vss) and clearance (CL) of small molecules?
For small molecules, lipophilicity is a primary determinant. Studies on xanthine derivatives have established that the distribution coefficient (logD) is a major descriptor influencing variability in volume of distribution (Vss), elimination rate constant (λz), and clearance (CL) [87].
- Additional Influences: Beyond lipophilicity, electronic and structural descriptors also contribute. Clearance and elimination rates have been shown to depend on the energy of the Lowest Unoccupied Molecular Orbital (LUMO) and specific hydration energy descriptors (HEFO), while volume of distribution can be influenced by partial atomic charges on carbon and oxygen atoms (COAR) [87].
FAQ 3: What are the common causes of high background or false positives in pharmacokinetic bridging ELISAs for total drug measurement?
False positives in bridging ELISAs can arise from several specific issues related to sample composition and assay procedure [88].
- Matrix-Induced Bridging: The sample matrix can cause false signals. Dimeric or bivalent target proteins, heterophilic antibodies, or rheumatoid factor can bridge the capture and detection antibodies independently of the drug, creating a false positive signal [88].
- Insufficient Washing: Inadequate washing can fail to remove unbound detection reagents, leading to high background signal. Ensure wells are washed thoroughly according to the protocol [88].
- Antibody Aggregation: Drug or reagent antibody aggregates are more prone to non-specific interactions. Using a new batch of antibodies that have been properly stored can resolve this [88].
FAQ 4: My nanoparticle formulation is rapidly cleared from circulation. Which properties should I investigate first?
When facing rapid clearance, you should systematically troubleshoot these four key physicochemical properties, as they are directly linked to recognition and uptake by the mononuclear phagocyte system (MPS) [4] [8] [20].
- 1. Surface Chemistry: This is the most critical parameter. A dense layer of polyethylene glycol (PEG) is the gold-standard "stealth" coating to reduce protein opsonization and uptake by Kupffer cells. Check the integrity and density of your PEGylation [4] [65].
- 2. Elasticity: As noted in FAQ 1, ensure your nanoparticle's elasticity is within the optimal intermediate range. Both very soft and very hard nanoparticles are cleared more quickly [4].
- 3. Size and Aggregation State: Use Dynamic Light Scattering (DLS) to confirm your nanoparticles exist as primary particles and have not aggregated into larger clusters, which are more readily phagocytosed [8] [20].
- 4. Protein Corona Composition: Characterize the absorbed protein corona. A corona rich in opsonins (e.g., immunoglobulins, complement proteins) promotes clearance, while the presence of ApoA1 is beneficial [4] [20].
Troubleshooting Data and Experimental Challenges
Handling Missing or Problematic Pharmacokinetic Data
Errors in PK data, such as missing sample times or concentrations below the limit of quantification (BLQ), are common and can bias results if mishandled [89].
Table 1: Troubleshooting Common PK Data Issues
| Problem Type | Potential Cause | Recommended Handling Method |
|---|---|---|
| Concentration Data BLQ | Bioanalytical assay limitations; low drug exposure. | Use the M3 method in population PK modeling, which allows for simultaneous modeling of continuous and categorical (BLQ) data. This provides less biased parameter estimates compared to simple omission [89]. |
| Inaccurate Sampling Times | Human error in recording; protocol deviations. | Do not discard the sample. Use the documented time while performing a sensitivity analysis to understand the potential impact of the error on your PK parameters [89]. |
| Missing Covariate Data | Non-compliance; data entry errors. | For continuous covariates (e.g., weight), avoid simple imputation with the median. Consider multiple imputation techniques or model the missing data as a function of other observed variables [89]. |
| High Inter-Subject Variability | Complex biology; unaccounted for covariates. | Perform a thorough covariate analysis using stepwise model building to identify physiological (e.g., weight, renal function) or demographic factors that explain variability in PK parameters [87] [89]. |
Quantitative Structure-Pharmacokinetics Relationship (QSPKR) Modeling Protocol
This protocol outlines the steps to develop a model correlating molecular descriptors with pharmacokinetic parameters [87].
Aim: To predict the pharmacokinetic behavior of new chemical entities based on their easily calculable molecular properties.
Materials & Reagents:
- Software: SYBYL-X, KowWin, MarvinSketch (for descriptor calculation); statistical software (for regression analysis).
- Chemical Compounds: A series of compounds with experimentally determined PK parameters.
- Data: Pharmacokinetic data (e.g., Vss, CL, fu) obtained from in vivo studies.
Experimental Workflow:
Key Steps:
- PK Data Acquisition: Determine pharmacokinetic profiles via in vivo administration (e.g., intravenous to rats). Calculate parameters like volume of distribution at steady state (Vss), clearance (CL), and fraction unbound (fu) using non-compartmental analysis [87].
- Descriptor Generation: Use computational programs to generate a set of molecular descriptors for each compound. Key descriptors often include lipophilicity (logD), electronic properties (e.g., LUMO energy), and structural parameters [87].
- Model Building: Employ multiple linear regression with a forward stepwise inclusion method to identify which descriptors significantly explain the variability in each PK parameter [87].
- Model Validation: Validate the predictive power of the model using techniques like cross-validation, reporting metrics like R² (goodness-of-fit) and Q² (predictive ability) [87].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents for Investigating Nanoparticle PK and Stability
| Research Reagent | Function and Application |
|---|---|
| DSPE-PEG2000 | A phospholipid-polyethylene glycol conjugate used to create a stealth "brush" layer on nanoparticle surfaces. This reduces non-specific protein adsorption (opsonization) and prolongs systemic circulation lifetime [4]. |
| Centrifree Ultrafiltration Devices | Equipped with a 30,000 NMWL membrane, these devices are used to separate free (unbound) drug from protein-bound drug in plasma samples. This is critical for determining the fraction unbound (fu) in PK studies [87]. |
| Apolipoprotein A-I (ApoA1) | A key protein in the protein corona associated with prolonged nanoparticle circulation. It can be used as a reference standard in corona composition analysis to understand the mechanism behind elasticity-dependent PK [4]. |
| Dynamic Light Scattering (DLS) Instrument | The primary tool for measuring the hydrodynamic diameter and aggregation state of nanoparticles in suspension. Monitoring these properties is fundamental to assessing colloidal stability over time [8]. |
| B3LYP/6-311G(d,p) DFT Method | A computational chemistry method used to calculate electronic properties and global reactivity parameters (e.g., HOMO/LUMO energies) of small molecules. These descriptors are vital for building QSPKR models [90]. |
Regulatory Considerations and Standardization of Stability Assessment
Frequently Asked Questions (FAQs)
Q1: What are the key regulatory bodies governing the stability assessment of nanoparticle-based therapeutics? In the United States, the Food and Drug Administration (FDA) is the primary authority that evaluates and approves nanomedicine products, ensuring they meet standards for safety, effectiveness, and quality [91]. In the European Union, the European Commission (EC) provides the foundational legal framework, with guidance from the European Medicines Agency [91]. These regulatory systems are highly influential and often set the benchmark for international regulatory standards [91].
Q2: Why is nanoparticle stability in circulation critical for regulatory approval? Nanoparticle stability directly influences a product's biodistribution, safety, and efficacy, which are core concerns for regulators [60]. Instability can lead to premature drug release, aggregation, or unintended interactions with biological systems, potentially causing immunogenic reactions, toxicity, or loss of therapeutic effect [60] [92]. Demonstrating consistent physical and chemical stability under physiological conditions is therefore essential for approval [60].
Q3: What are the main challenges in the regulatory approval of nanomedicines? Regulatory challenges include the complexity of nanoparticles as multi-component constructs, the need for detailed orthogonal analysis methods, and the requirement for a reproducible scale-up and manufacturing process [60]. Furthermore, minor variations in parameters like size, surface charge, or drug release kinetics can significantly influence safety and efficacy, requiring careful examination in preclinical and clinical studies [60] [92]. There is also a general lack of specific regulatory standards for nanoparticle-based medicines, though efforts are being made to address this [60].
Q4: How does standardization of characterization methods support regulatory submissions? Using standardized and orthogonal characterization methods provides robust, reproducible data that regulators can rely on to assess product quality. Techniques like dynamic light scattering, nanoparticle tracking analysis, and cryogenic transmission electron microscopy offer complementary information on size, distribution, and morphology [93] [94]. A thorough and consistent analytical approach helps to establish critical quality attributes and ensures the product is manufactured consistently, which is a fundamental regulatory requirement [60].
Q5: What physicochemical properties are most critical to monitor for stability assessment? Key properties include [60]:
- Size and size distribution
- Surface charge (zeta potential)
- Drug loading efficiency
- Drug release kinetics
- Particle morphology
- Aggregation state
These properties can change during storage and in the biological environment, affecting the nanoparticle's performance [60] [92].
Troubleshooting Guides
Problem: Nanoparticle Aggregation During Storage or in Biological Media
| Potential Cause | Recommended Investigation | Possible Solution |
|---|---|---|
| Insufficient steric or electrostatic stabilization | Measure zeta potential. Use DLS or NTA to monitor size over time in relevant buffers [60] [93]. | Introduce steric stabilizers (e.g., PEGylation) or optimize surface charge [92]. |
| Interaction with serum proteins | Incubate with serum and analyze size change via DLS and morphology via cryo-TEM [94]. | Engineer surface to be protein-resistant (e.g., PEG coatings) or pre-form a protein corona [60]. |
| Osmotic stress or pH instability | Test stability in different physiological-mimicking buffers (varying pH, ionic strength) [60]. | Reformulate with different excipients or buffers to improve colloidal stability [60]. |
Experimental Protocol: Investigating Serum Protein Interactions
- Incubation: Mix the nanoparticle suspension with fetal bovine serum (FBS) or human plasma at a physiologically relevant ratio (e.g., 1:1) and incubate at 37°C.
- Time-point Sampling: Withdraw samples at predetermined time points (e.g., 0, 1, 2, 4 hours).
- Size Analysis: Dilute the samples appropriately in a suitable buffer and measure the hydrodynamic diameter and polydispersity index using Dynamic Light Scattering [93].
- Visualization: For a detailed morphological assessment, prepare samples for cryo-TEM following standard vitrification procedures to observe the particles in their native state and check for aggregation or corona formation [94].
Problem: Inconsistent or Poorly Reproducible Drug Release Profiles
| Potential Cause | Recommended Investigation | Possible Solution |
|---|---|---|
| Inconsistent drug loading | Measure drug loading efficiency across multiple batches using HPLC or UV-Vis spectroscopy [60]. | Optimize and strictly control the drug loading process (e.g., solvent evaporation, dialysis) [60]. |
| Batch-to-batch variation in nanoparticle size | Use NTA or DLS to rigorously quantify the size distribution of each batch [93] [94]. | Standardize the manufacturing process (e.g., mixing rates, solvent addition speed) to improve reproducibility [60]. |
| Unaccounted-for enzymatic degradation | Perform release studies in the presence of relevant enzymes (e.g., esterases, proteases) [92]. | Switch to more stable polymer/lipid components or incorporate enzyme inhibitors [92]. |
Experimental Protocol: Standardized In Vitro Drug Release Study
- Dialysis: Place a known volume of nanoparticle suspension into a dialysis tube (with an appropriate molecular weight cutoff).
- Sink Conditions: Immerse the tube in a large volume of release medium (e.g., PBS at pH 7.4, with 0.1% w/v Tween 80 to maintain sink conditions) at 37°C with constant agitation.
- Sampling: At regular intervals, withdraw a sample from the external release medium and replace it with fresh medium to maintain the sink condition.
- Analysis: Quantify the drug concentration in the samples using a validated analytical method (e.g., HPLC).
- Data Plotting: Plot the cumulative drug release (%) versus time to generate the release profile.
Experimental Protocols for Key Stability Assessments
Protocol 1: Assessing colloidal stability in simulated biological fluids
- Objective: To evaluate the stability of nanoparticle size and aggregation state in physiologically relevant conditions.
- Materials: Nanoparticle formulation, PBS (pH 7.4), FBS, DLS instrument, NTA instrument (optional).
- Method:
- Dilute the nanoparticle sample in PBS and FBS to a concentration suitable for light scattering measurements.
- Incubate the samples at 37°C.
- Measure the hydrodynamic diameter and PDI using DLS at time zero and after 1, 2, 4, 8, and 24 hours of incubation [93].
- For a more sensitive count-based size distribution, confirm key time points using Nanoparticle Tracking Analysis [93].
Protocol 2: Morphological analysis using Cryo-TEM
- Objective: To directly visualize nanoparticle morphology, internal structure, and state of aggregation in a vitrified, near-native state.
- Materials: Nanoparticle formulation, cryo-TEM instrument, holey carbon grids.
- Method:
- Apply a small volume (e.g., 3-5 µL) of the nanoparticle suspension to a freshly glow-discharged holey carbon grid.
- Blot the grid to create a thin liquid film and immediately plunge-freeze it into liquid ethane using a vitrification device.
- Transfer the grid under liquid nitrogen to the cryo-TEM holder.
- Image the samples at a temperature below -170°C using a transmission electron microscope [94].
- Analyze images for size, shape, lamellarity (for liposomes), and any signs of aggregation or structural defects.
Experimental Workflow and Signaling Pathways
Diagram Title: Nanoparticle Stability Assessment Workflow
Diagram Title: Consequences of Nanoparticle Instability
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Stability Assessment |
|---|---|
| PEGylated Lipids | Provides steric stabilization, reduces opsonization, and prolongs circulation half-life by creating a hydrophilic barrier [60] [92]. |
| Fetal Bovine Serum | Used in in vitro assays to simulate interactions with blood components and study protein corona formation and its impact on stability [60]. |
| Dynamic Light Scattering Instrument | Measures the hydrodynamic diameter and polydispersity index of nanoparticles in suspension to monitor size stability and aggregation [93] [94]. |
| Cryogenic Transmission Electron Microscope | Provides high-resolution, direct visualization of nanoparticle size, morphology, and internal structure in a near-native state; considered a gold standard [94]. |
| Nanoparticle Tracking Analyzer | Provides particle size distribution and concentration estimates by visualizing and tracking the Brownian motion of individual particles [93]. |
| Size Exclusion Chromatography | Separates nanoparticles from free drug or impurities; used to analyze drug loading and assess aggregate formation [94]. |
| Analytical Ultracentrifugation | Analyzes sedimentation behavior to determine particle density, size distribution, and the ratio of full-to-empty particles in formulations like viral vectors [94]. |
Conclusion
Enhancing nanoparticle structural stability in circulation requires a multifaceted approach integrating fundamental understanding of nano-bio interactions with advanced engineering strategies. Key takeaways include the critical role of protein corona management, the emerging importance of nanoparticle elasticity, the value of systematic optimization frameworks like DoE, and the necessity of robust characterization methods. Future directions should focus on developing smart nanoparticles that dynamically adapt to physiological environments, establishing standardized stability protocols for regulatory approval, and creating computational models to predict in vivo performance from in vitro data. These advances will accelerate the clinical translation of nanoparticle-based therapeutics, ultimately improving treatment outcomes across various disease domains.
References
- 1. Functionalized Nanoparticles with Long-Term Stability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2883049/]
- 2. Enhanced dispersion stability of gold nanoparticles by the ... [https://www.nature.com/articles/s41467-020-19947-8]
- 3. Nanoparticle Characterization Techniques [https://nanocomposix.com/pages/nanoparticle-characterization-techniques]
- 4. Nanoparticle elasticity affects systemic circulation lifetime by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9288426/]
- 5. Frequently Asked Questions - Lipid Nanoparticles (LNPs) ... [https://diantpharma.com/?page_id=1308]
- 6. Nanoparticles with High Drug Loading and Circulation ... [https://docs.lib.purdue.edu/open_access_dissertations/1787/]
- 7. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOoqVFMm_oBQyI78Qz7rrk5yKC9wdv75jSWFmA5a05IdzZqAAJs-o]
- 8. What Does Nanoparticle Stability Mean? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6913534/]
- 9. Tips and Tricks for Nanoparticles - Zetasize Materials Talks [https://www.malvernpanalytical.com/en/learn/knowledge-center/insights/tips-tricks-for-nanoparticle-characterization]
- 10. Aging and physiological barriers: mechanisms of ... [https://pubmed.ncbi.nlm.nih.gov/39158744/]
- 11. Exploring the barriers and enablers to healthy longevity [https://www.openaccessgovernment.org/exploring-the-barriers-and-enablers-to-healthy-longevity/193976/]
- 12. Scientists Discover Key Biological Mechanism That ... [https://scitechdaily.com/scientists-discover-key-biological-mechanism-that-promotes-healthy-aging-and-longevity/]
- 13. Lifestyle and environmental factors affect health and ... [https://www.ox.ac.uk/news/2025-02-20-lifestyle-and-environmental-factors-affect-health-and-ageing-more-our-genes]
- 14. Protein corona formed on lipid nanoparticles compromises ... [https://www.nature.com/articles/s41467-025-63726-2]
- 15. Protein Corona as a Result of Interaction ... [https://www.mdpi.com/1422-0067/26/19/9771]
- 16. Impact of Protein Corona on the Biological Identity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8533425/]
- 17. Impact of Protein Corona on the Biological Identity ... [https://pubmed.ncbi.nlm.nih.gov/34680613/]
- 18. Machine learning predicts the functional composition of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7229677/]
- 19. Salt Stability of Nanoparticles - nanoComposix [https://nanocomposix.com/pages/salt-stability-of-nanoparticles]
- 20. Effect of Physico-Chemical Properties of Nanoparticles on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7662525/]
- 21. Nanoparticle classification, physicochemical properties ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01477-8]
- 22. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOopwP8PivG94CNcRZSWWG7ASQhKh0nG28JgfV_Dszoq9MPsw1uvM]
- 23. Quantitative analysis of mRNA-lipid nanoparticle in human... stability [https://pubmed.ncbi.nlm.nih.gov/38499167/]
- 24. Nanotechnology Safety Resources [https://www.acs.org/about/governance/committees/chemical-safety/publications-resources/nanotechnology-safety-resources.html]
- 25. Nanotechnology: Guidelines for Safe Research Practices [https://blink.ucsd.edu/safety/research-lab/nanotechnology.html]
- 26. Design of polymeric nanoparticles for biomedical delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3299918/]
- 27. Opsonization, biodistribution, and pharmacokinetics of ... [https://www.sciencedirect.com/science/article/abs/pii/S037851730500668X]
- 28. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOoqRaZIhSTP10Yks7YIlIrBP9Pp8p_HN00eEa8WcTaAuQZJsmk8u]
- 29. Trouble shooting - AURION [https://aurion.nl/answering-your-question/trouble-shooting/]
- 30. 3 Questions to Ask When Navigating Nanoparticle Analysis ... [https://www.izon.com/news/navigating-nanoparticle-analysis-and-resolution-limits]
- 31. PEGylation as a strategy for improving nanoparticle-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X15002173]
- 32. PEGylation technology: addressing concerns, moving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020137/]
- 33. Beyond PEGylation: nanoparticle surface modulation for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00014-4]
- 34. Questioning the Use of PEGylation for Drug Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4051498/]
- 35. The ultimate guide for PEGylated lipid nanoparticles [https://www.cas.org/resources/cas-insights/ultimate-guide-pegylated-lipid-nanoparticles]
- 36. Stealth missiles with precision guidance [https://www.sciencedirect.com/science/article/pii/S2590006425004922]
- 37. Nanoparticle Surface Functionalization: How to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726445/]
- 38. How Effective is PEGylation as a Stability Enhancement ... [https://nhsjs.com/2025/how-effective-is-pegylation-as-a-stability-enhancement-method/]
- 39. The Art of PEGylation: From Simple Polymer to ... [https://www.mdpi.com/1422-0067/26/7/3102]
- 40. Bio-inspired nanomaterials as novel options for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8205945/]
- 41. Application of Biomimetic SPIONs in Targeted Lung Cancer Therapy: Cell-Membrane Camouflage Technology and Lung Retention Enhancement Strategies [https://www.mdpi.com/1999-4923/17/10/1301]
- 42. The interaction between particles and vascular ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24000383]
- 43. Manipulating nanoparticle transport within blood flow through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5897762/]
- 44. New nanomanufacturing strategy through bioinspired ... [https://www.nature.com/articles/s41598-024-75116-7]
- 45. Inflammation-modulating polymeric nanoparticles: design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271758/]
- 46. Factors that control the circulation time of nanoparticles in blood... [https://pubmed.ncbi.nlm.nih.gov/20618151/]
- 47. : Liposomes , Biomedical Applications, and Structure ... Stability [https://pubmed.ncbi.nlm.nih.gov/34568298/]
- 48. Engineering Nanomedicines for Improved Melanoma Therapy - Page 5 [https://www.medscape.com/viewarticle/734055_5]
- 49. Dispersion stability of nanoparticles in ecotoxicological investigations... [https://link.springer.com/article/10.1007/s11051-011-0298-y]
- 50. Lipid-Polymer Hybrid Nanoparticles as a Smart Drug ... [https://www.mdpi.com/1999-4923/17/6/797]
- 51. Physical and chemical stability of drug nanoparticles [https://www.sciencedirect.com/science/article/abs/pii/S0169409X11000172]
- 52. Green-synthesized metal nanoparticles: a promising ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1637589/full]
- 53. Revisiting the Green Synthesis of Nanoparticles [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444627/]
- 54. Biocompatibility of nanomaterials and their immunological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8357854/]
- 55. Sustainable synthesis of nanomaterials using different ... [https://bnrc.springeropen.com/articles/10.1186/s42269-025-01316-4]
- 56. A review on green synthesis of nanoparticles toward ... [https://www.sciencedirect.com/science/article/pii/S2772826925000161]
- 57. Applying Particle Size Stability as a Response Factor in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223868/]
- 58. Guide to DOEs (Design of Experiments) - Instrumental [https://instrumental.com/build-better-handbook/guide-to-does]
- 59. In depth characterization of physicochemical critical quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10157317/]
- 60. Challenges in Development of Nanoparticle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326161/]
- 61. Top Troubleshooting Tips for Nanoparticle Conjugation ... [https://hiyka.com/tutorials/top-troubleshooting-tips-for-nanoparticle-conjugation-and-application-in-diagnostics/?srsltid=AfmBOoqZF5-W1lwFjKweS1S_RGgCK66xTOq35xMTD_YzT2-5L7I142LE]
- 62. Controlling evolution of protein corona [https://www.nature.com/articles/s41598-020-66572-y]
- 63. Recent Advances in Lipid Nanoparticles and Their Safety ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510967/]
- 64. The Role of Nanoparticle Elasticity on Biological Hydrogel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196392/]
- 65. A brief history of long circulating nanoparticles [https://www.sciencedirect.com/science/article/pii/S0169409X22002861]
- 66. Review (In)stability of ligands at the surface of inorganic ... [https://www.sciencedirect.com/science/article/abs/pii/S1748013222001438]
- 67. Directional conjugation of monoclonal antibodies to ... [https://www.nature.com/articles/s41596-025-01272-3]
- 68. A review of current nanoparticle and targeting moieties for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3619023/]
- 69. Ligands of Nanoparticles and Their Influence on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510505/]
- 70. Nanoparticle Drug Delivery Systems for Atherosclerosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463135/]
- 71. Nanoparticle Size Distribution and Stability Assessment Using ... [https://pubmed.ncbi.nlm.nih.gov/38506987/]
- 72. From Dynamic Light Scattering to Super-Resolution ... [https://www.mdpi.com/2304-6732/11/2/101]
- 73. The immunogenic potential of an optimized mRNA lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921523/]
- 74. Super-resolution fluorescence microscopy and cryogenic ... [https://www.sciencedirect.com/science/article/abs/pii/S1748013224004559]
- 75. Comparative Analysis of Electron Microscopy Techniques ... [https://pubmed.ncbi.nlm.nih.gov/40290944/]
- 76. Cryo-EM Sample Prep: 5 Crucial Considerations [https://bitesizebio.com/62619/cryo-em-sample-prep/]
- 77. Challenges and opportunities in cryo-EM single-particle analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC6442032/]
- 78. Chapter 1 – Cryo EM 101 [https://cryoem101.org/chapter-1/]
- 79. Efficient strategies and troubleshooting for single particle ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-025-00025-8]
- 80. In Vivo Assay Guidelines - Assay Guidance Manual - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK92013/]
- 81. Engineering precision nanoparticles for drug delivery [https://www.nature.com/articles/s41573-020-0090-8]
- 82. Generalized in vitro-in vivo relationship (IVIVR) model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3615932/]
- 83. Achieving long-term stability of lipid nanoparticles : examining the... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5221800/]
- 84. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 85. Artificial High Density Lipoprotein Nanoparticles in Cardiovascular... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6695986/]
- 86. Innovative solid lipid nanoparticle formulations for ocular ... [https://www.sciencedirect.com/science/article/pii/S0168365925006133]
- 87. Pharmacokinetics and Quantitative Structure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11597386/]
- 88. Troubleshooting of Pharmacokinetic (PK) Bridging ELISA ... [https://www.antibody-creativebiolabs.com/troubleshooting-of-pharmacokinetic-pk-bridging-elisa-measuring-total-drug.htm]
- 89. Approaches to handling missing or “problematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8099444/]
- 90. Physicochemical properties, pharmacokinetic studies, DFT ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2024.1360719/full]
- 91. Frontiers | Regulatory pathways and guidelines for nanotechnology-enabled health products: a comparative review of EU and US frameworks [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 92. Therapeutic potential and toxicological challenges of metal ... [https://www.sciencedirect.com/science/article/abs/pii/S1549963425000632]
- 93. Nanoparticle Measurement Through Visualization [https://www.americanlaboratory.com/913-Technical-Articles/756-Nanoparticle-Measurement-Through-Visualization/]
- 94. Comparing Analytical Techniques for Nanoparticle ... [https://www.nanoimagingservices.com/about/blog/visualizing-nanomedicines-understanding-your-nanoparticle-formulations]